Abstract
Context:
Neurofibroma is a benign peripheral nerve sheath tumor. Commonly found in the peripheral soft tissues, it can manifest as a solitary mass or as a component of neurofibromatosis.
Aims:
The purpose of the retrospective cross-sectional study was contributing to the literature by providing data about the prevalence of oral neurofibroma in Central Indian population.
Settings and Design:
Retrospective, cross-sectional study.
Subjects and Methods:
All histopathologically diagnosed cases of oral neurofibroma were retrieved from the archives of our department and were reviewed. All the cases that met the inclusion criteria were reviewed in terms of the year when the patient reported, patient's age, gender, location of the lesion, i.e., soft tissue or intraosseous, clinical appearance, i.e., growth or swelling, histopathologic diagnosis and immunohistochemistry results if available. The results were aggregated and described qualitatively using Microsoft Excel 2013.
Results:
In our retrospective analysis of 20 years (2000–2019), we came across 14 reported cases of oral neurofibroma, in five males and nine females. Two of these cases showed a recurrent nature and one case showed transformation into atypical neurofibroma. Two cases were encountered in the mandible as an intraosseous oral neurofibroma.
Conclusions:
In our study, we found that oral neurofibroma was more common in the third decade with a female predilection. Gingiva was the most common site. Of the 14 cases that were encountered, two cases showed recurrence and one case showed malignant transformation. Hence, in spite of being a benign neoplasm, oral neurofibroma is locally aggressive and should be diagnosed accurately.
Keywords: Central Indian population, intraosseous, oral neurofibroma, orthopantograph, prevalence, quality of life
INTRODUCTION
The neurofibroma is a benign tumor of nerve tissue origin derived from a mixture of cell types which include Schwann cells and perineurial fibroblasts that constitute the nerve sheath.[1] The very first case of solitary neurofibroma of the oral cavity was reported by Bruce in 1954.[2] It is commonly seen in soft tissues, skin being the most common location. Intraorally, tongue is the most common location. Intraosseous occurrence of oral neurofibroma is a rare phenomenon. If it occurs, it is preferably seen in the mandible.[3] Oral neurofibroma can occur in two different forms: A solitary tumor or as a component of neurofibromatosis.[4]
Clinically, oral neurofibromas usually appear as pedunculated or sessile nodule, with slow growth.[5] Pain and paresthesia are the common symptoms due to compression of involved nerve. No gender predilection is reported.[6] In some patients, malignant transformation subsequently occurs.[1]
Microscopy reveals the presence of multiple, relatively well-demarcated fascicles of spindle-shaped nerve cells, most of which are positive for S-100 protein.[7] It appears in the fifth decade of life.[8] Macroscopic appearance is characterized by glistening, tan-white tumor that lacks secondary degenerative changes.[9]
A variant, plexiform oral neurofibroma consists of compact bundle of cells in a highly irregular sinuous pattern giving an appearance of grossly distorted nerve fibers.[6] Surgical removal may result in recurrence. Multiple recurrences are associated with malignant transformation.[1]
After the first documentation of the case by Bruce in 1954, many cases were reported in the literature. We have also come across a number of cases of oral neurofibromas, and hence, the need for an update from the Central Indian population seems to be of paramount importance. With this aim, we report the prevalence of oral neurofibroma in Central Indian population.
SUBJECTS AND METHODS
All diagnosed cases of oral neurofibroma were retrieved from the archives of Department of Oral and Maxillofacial Pathology, Government Dental College and Hospital, Nagpur, India, spanning over a period of 2000–2019.
The inclusion criteria were as follows:
Histopathologically diagnosed cases of oral neurofibroma with complete patient information
Cases of spindle cell lesions with a certainty of neural origin which were confirmed using immunohistochemistry (IHC).
Exclusion criteria
Histopathologically diagnosed cases of oral neurofibroma with incomplete patient information
Cases of spindle cell lesions with no certainty of neural origin.
All cases were signed out by one board certified oral pathologist and reviewed by secondary oral pathologists and residents. The slides retrieved were reviewed by one board certified oral pathologist and one oral pathology resident for the consensus.
All the cases that met inclusion criteria were reviewed in terms of the year when the patient reported, patient's age, gender, location of the lesion, i.e., intraosseous or soft tissue, clinical appearance, i.e., growth or swelling, histopathologic diagnosis and IHC results if available. The results were aggregated and described qualitatively using Microsoft Excel 2013. Data regarding two cases of recurrence were recorded under the above-mentioned terms as a separate table.
RESULTS
A total of 14 cases of oral neurofibroma were reported over the past two decades (2000-2019). Twelve of these which did not show any recurrence are depicted in Table 1.
Table 1.
Review of cases of neurofibromas of Central Indian Population without recurrence
| Years | Age (years) | Gender | Types of presentation | Location | IHC performed | Recurrence |
|---|---|---|---|---|---|---|
| 2003 | 14 | Female | Soft-tissue growth | Lower left mandibular body region | No | No |
| 2003 | 40 | Female | Soft-tissue swelling | Left maxillary alveolar ridge extending onto the palate | No | No |
| 2007 | 21 | Female | Swelling in the lower left posterior region | Body of mandible | No | No |
| 2008 | 17 | Female | Gingival overgrowth | Maxillary anterior gingiva | No | No |
| 2013 | 10 | Female | Soft-tissue swelling | Maxillary right posterior region | No | No |
| 2013 | 18 | Male | Soft-tissue growth | Mandibular right posterior lingual gingiva | No | No |
| 2014 | 56 | Female | Soft-tissue swelling | Floor of the mouth right side | No | No |
| 2014 | 20 | Male | Soft-tissue Swelling | Mandibular left lingual gingiva | No | No |
| 2016 | 35 | Female | Solitary sessile growth | Interdental gingiva w.r.t. 14, 15 tooth | No | No |
| 2018 | 25 | Female | Intraosseous growth | Left mandibular ramus | Yes. S-100 and CD-34 positivity | No |
| 2018 | 30 | Male | Soft tissue swelling | Left anterior region of gingiva w.r.t 22, 23 | No | No |
| 2018 | 47 | Male | Swelling | Mandibular left buccal vestibule | No | No |
IHC: Immunohistochemistry
One case of juvenile patient which recurred once was shown in Table 2. Moreover, a case of multiple recurrences in a male patient is shown in Table 3.
Table 2.
Neurofibroma with recurrence in a juvenile patient
| Year when reported | Age when reported | Gender | Site | IHC performed | Final diagnosis |
|---|---|---|---|---|---|
| 2013 | 14 | Female | Swelling in the maxillary anterior gingiva | No | Neurofibroma |
| 2017 | 18 | No | Recurrent neurofibroma |
IHC: Immunohistochemistry
Table 3.
A case of multiple recurrences
| Year when reported | Age when reported | Gender | Site | IHC performed | Final diagnosis |
|---|---|---|---|---|---|
| 2010 | 38 | Male | Posterior mandible | Yes (Vimentin +) | Neurofibroma |
| 2012 | 39 | No | Recurrent neurofibroma | ||
| 2015 | 42 | No | Recurrent neurofibroma | ||
| 2016 | 43 | No | Recurrent neurofibroma | ||
| 2017 | 44 | Yes (Vimentin+, S-100+, Ki-67+, MIB1 +) | Atypical neurofibroma |
IHC: Immunohistochemistry
Of these 14 cases, five were males and nine were females. Hence, there was a slight female predilection. These cases occurred over a wide age range from 10 years to maximum of 56 years, with a mean age of 30 years. Lesional presentation varied from soft-tissue growth to soft and hard-tissue swelling. Of these 14 cases, five cases were seen as a growth on the maxillary gingival region (two anterior and three posterior). Four cases were seen on the mandibular gingival region (two anterior lingual gingiva and two posterior buccal gingiva). One case occurred on the floor of the mouth. Two cases were intraosseous in the mandibular ramus region. Two cases showed recurrence and one case showed subsequent malignant transformation into atypical neurofibroma.
DISCUSSION
After the first description of neurofibroma by Bruce in 1954, considerable research was done in the arena of neural tumors for their nomenclature. Bernier suggested that nomenclature of neurogenic fibroma is quite confusing due to the complexity in their background. Thus multiple names were applied to benign tumors of nerve sheath such as neurofibroma, perineural fibroblastoma, neurilemmoma, schwannoma, peripheral glioma, fibroma of nerve sheath and neuroma.[2]
Oral neurofibroma is seen either as a solitary lesion or as a part of generalized syndrome of neurofibromatoses.[1] Whenever an oral neurofibroma is present, it is wise to determine by general physical examination if von Recklinghausen disease or neurofibromatosis is present.
Table 1 shows the incidence of oral neurofibroma among the Central Indian population over a period of 20 years, i.e., 2000–2019. A total of 14 cases of this rare neoplasm were reported. Two of these also showed recurrence.
According to the literature, the mean age of the patient is in the fifth decade of life.[8] In our findings, the age ranged from a minimum of 10 years to a maximum of 56 years, with a mean age of 30 years.
In WHO's blue book, no sex predilection is mentioned. In our data, slight different findings were observed. Of the 14 cases, five were male and nine were female showing a slight female predilection.
Clinically, oral neurofibroma presents as a slow growth sessile or pedunculated. In our cases, the lesional presentations varied ranging from soft-tissue growth to hard and soft-tissue swelling with no other intraoral findings.
Most common intraoral location of neurofibroma is the tongue. In our findings, site predilection also showed variations. Four cases were seen in the maxillary gingival region, five cases in the mandibular gingival region and one on the floor of the mouth and two cases as intraosseous swelling. With time many cases of neurofibroma at unusual locations such as lips, floor of mouth and articular disc of temporomandibular joint has been reported.[13,14,15]
Occasionally, oral neurofibromas are located within the jaws and are called central variety of neurofibroma.[9] These cases are, however, very rare. In our data, two out of the 14 cases presented as an intraosseous growth. Case of solitary neurofibroma of maxillary sinus and pterygopalatine fossa which are clinically silent locations have also been reported in the literature.[16]
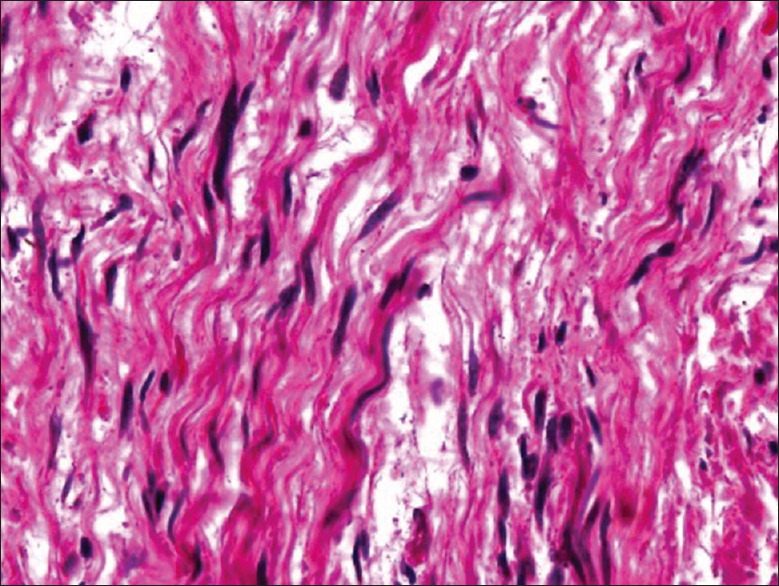
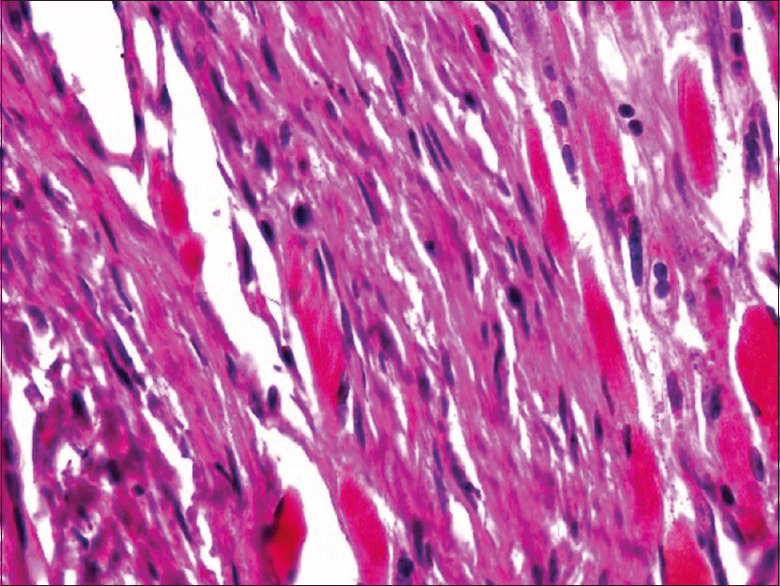
The WHO blue book, 2017 describes histopathology of oral neurofibroma as unencapsulated tumors with the lesional cells arranged in fascicles intermixed with fine collagen bundles and mast cells. These cells are ovoid to spindled cells with undulating pointy nuclei with thin cytoplasmic processes extending into stroma.[8] Our cases also showed a similar histopathologic picture [Figures 1–4]. However, mast cells were not seen in any case.
Figure 1.
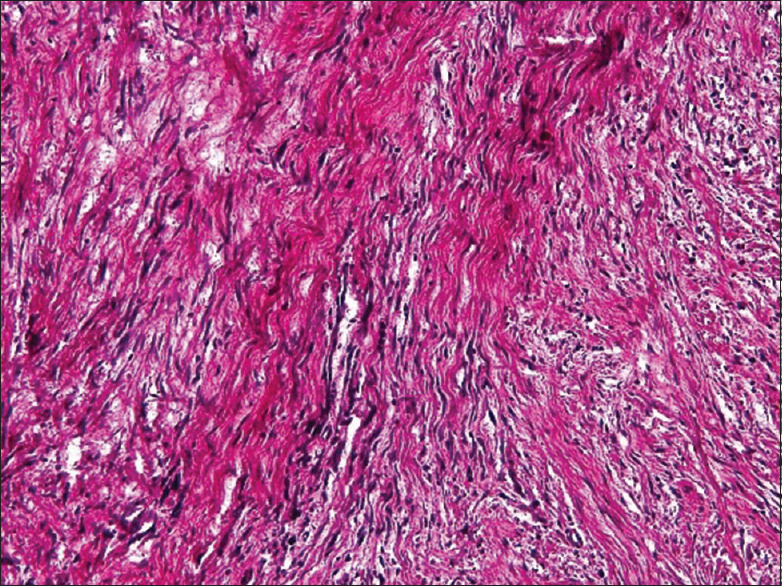
Highly cellular tumor mass with spindle shaped cells and thin, wavy, hair-like nuclei characteristic of neurofibroma
Figure 4.
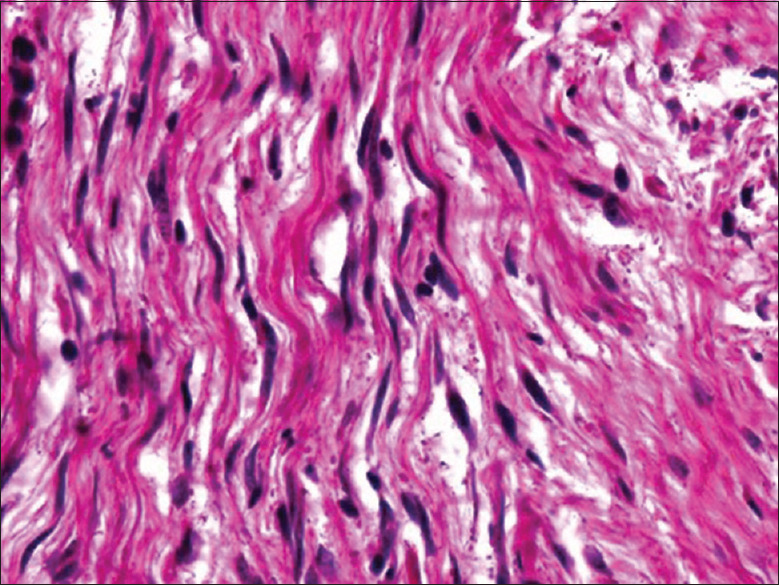
Highly cellular tumor mass with slender, hyperchromatic nuclei
Oral neurofibromas may assume one of the three growth patterns: Localized, diffuse and plexiform. Kamra et al. in their case report demonstrated a plexiform neurofibroma in submandibular gland with small diffuse neurofibroma in floor of the mouth.[27]
Subpopulation of NF are highlighted with S100, GFAP, CD34, BCl2, with SOX10, NFP and Calretinin highlighting the axons specifically.[8] A number of studies to elicit the immunohistochemical reactions of the tumor are done. Marcia et al. examined 22 neurofibromas and concluded that strong positivity for S100 protein was suggestive of abundant Schwann cells. CD 34 positivity was useful for differential diagnosis against palisaded encapsulated neuroma, traumatic neuroma and schwannomas, low immunoreactivity for p53 and Ki67 suggests low potential for aggressiveness and malignant transformation.[28] In our reports, a case of intraosseous neurofibroma showed positivity for S-100 and CD34 which confirmed the diagnosis [Figures 2 and 3]. Another intraosseous case showed positivity for S-100, Vimentin, Ki-67 and MIB1 which confirmed the diagnosis of atypical neurofibroma.
Figure 2.
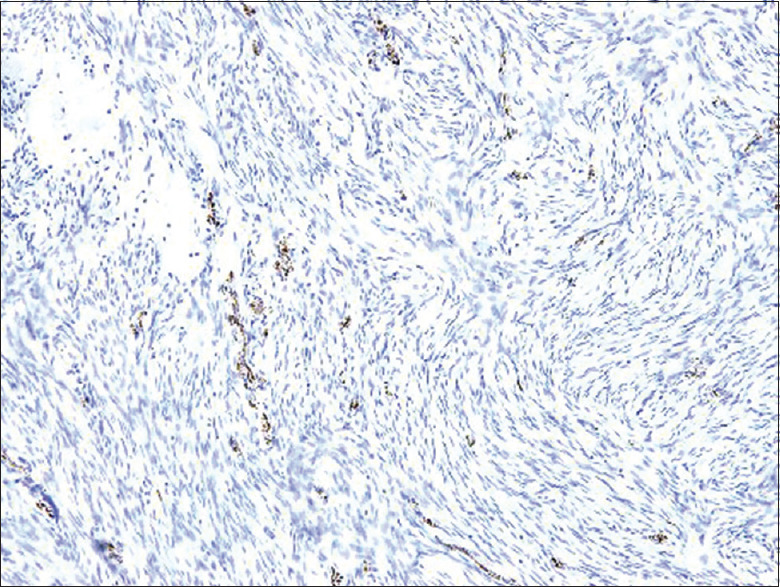
S-100 positivity at 4x
Figure 3.
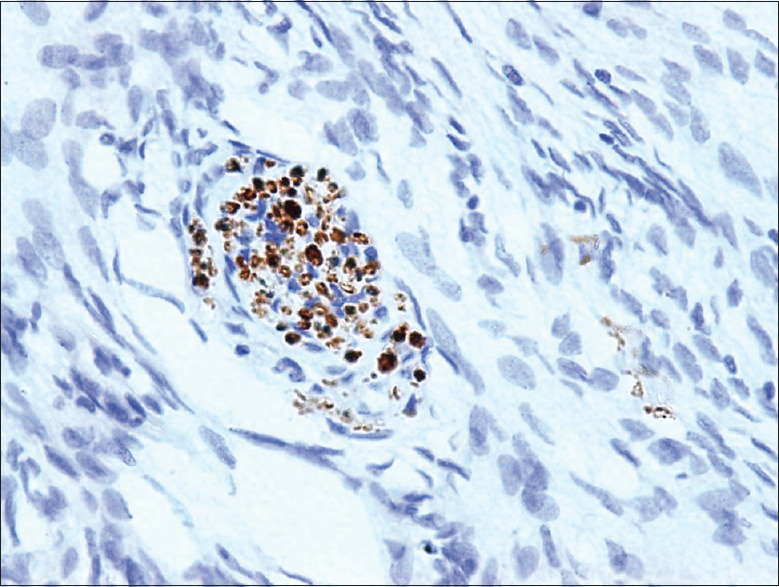
S-100 Focal positive at 40x
Following the first monograph of neurofibroma, a plethora of unusual cases were published in the literature. Johnson et al. in 1959 published a case report of central neurofibroma of the mandible.[10] Gutman et al. in 1961 gave a case report on solitary neurofibroma of the mandible.[11] Baden and Fischer in 1958 described a case of multiple neurofibromas with one on the palate.[12]
HE Simpson et al. in 1963 presented an unusual case where the sensory end organs were elaborated. The biopsy from the tongue and cheek gave unexpected evidence of attempts at production of sensory end organs resembling Meisnner's corpuscles.
Oral neurofibroma involving critical cranial nerves such as inferior alveolar nerve, trigeminal nerve and facial nerve is also reported. These cases stand out from the point of view of cosmetic deformity that they produce. Furthermore, the management is very difficult and requires multidisciplinary approach.[17,18,19]
Literature search revealed many publications of simultaneous occurrence of neurofibromatosis with other anomalies such as bilateral central giant cell granuloma, cherubism, systemic lupus erythematosus, Down's syndrome and even HIV-positive patients. This suggested a need to probe more into the pathogenesis of this tumor. Sujatha and Jatti showed simultaneous occurrence of neurofibromatoses and fibrous dysplasia. Both have café-au-lait spots. Understanding the interrelationship between both is more than an academic exercise and may be of therapeutic importance.[16,20,21,22,23,24]
Shimoyama et al. reported a distinct morphologic type of neurofibroma-lipomatous neurofibroma on the palatal gingiva.[25] Lerman et al. presented a case series of 31 cases of dendritic cell neurofibroma with pseudorosettes exhibiting biphasic population and strong CD57 positivity.[26]
According to the WHO 2017, the recurrence rate of oral neurofibromas is estimated to be 5%. This is in accordance with our findings where, of all cases, only two cases showed recurrence. One case showed malignant transformation into atypical neurofibroma [Figures 5 and 6].
Figure 5.
Highly cellular tumor mass with slender, hyperchromatic nuclei
Figure 6.
Atypical Neurofibroma showing infiltration of normal muscle tissue by the tumor mass
Cosetti et al. conducted an interesting survey of quality of life in patients with neurofibromatosis and found lower QOL in these patients. Psychosocial stressors include disease-related anxiety, personal and financial stress and lack of social support.[29] This indicates that impact of this tumor is way beyond physical deformities.
CONCLUSIONS
Oral neurofibroma is a rare benign neural tumor as confirmed in this study. In our study, we found a female predominance and most cases belonged to the third decade of life and gingiva was the most common site of occurrence. Although rare, cases of intraosseous neurofibroma can be encountered. In our study, two out of 14 cases showed intraosseous occurrence.
This indicates that oral neurofibroma should be considered a radiographic differential diagnosis. Nevertheless, microscopic examination supported by IHC findings remains the mainstay to arrive at a definitive diagnosis. One of the cases in our study showed malignant transformation of oral neurofibroma into atypical neurofibroma after 6 years. This emphasizes the importance of a long-term follow-up.
In spite of being a benign neoplasm, oral neurofibroma is locally aggressive and very rarely can show recurrence and malignant transformation. Hence, every dentist should be sensitized to consider the differential diagnosis of neurofibroma and refer to a specialist if needed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Rajendran R. Shafer's textbook of oral pathology. 7th ed. India: Elsevier; 2009. pp. 202–3. [Google Scholar]
- 2.Bruce KW. Solitary neurofibroma (neurilemmoma, schwannoma) of the oral cavity. Oral Surg Oral Med Oral Pathol. 1954;7:1150–9. doi: 10.1016/0030-4220(54)90307-2. [DOI] [PubMed] [Google Scholar]
- 3.Iqbal A, Tamgadge S, Tamgadge A, Chande M. Intraosseous neurofibroma in a 13-year-old male patient: A case report with review of literature. J Cancer Res Ther. 2018;14:712–5. doi: 10.4103/0973-1482.176173. [DOI] [PubMed] [Google Scholar]
- 4.Papadopoulos H, Zachariades N, Angelopoulos AP. Neurofibroma of the mandible. Review of the literature and report of a case. Int J Oral Surg. 1981;10:293–7. doi: 10.1016/s0300-9785(81)80074-9. [DOI] [PubMed] [Google Scholar]
- 5.Gómez Oliveira G, Fernández-Alba Luengo J, Martín Sastre R, Patiño Seijas B, López-Cedrún Cembranos JL. Neurofibroma plexiforme en mucosa yugal: Presentación de un caso clínico. Med Oral Patol Oral Cir Bucal. 2004;9:253–62. [PubMed] [Google Scholar]
- 6.Depprich R, Singh DD, Reinecke P, Kübler NR, Handschel J. Solitary submucous neurofibroma of the mandible: Review of the literature and report of a rare case. Head Face Med. 2009;5:24. doi: 10.1186/1746-160X-5-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tao Q, Wang Y, Zheng C. Neurofibroma in the left mandible: A case report. Kaohsiung J Med Sci. 2010;26:217–21. doi: 10.1016/S1607-551X(10)70032-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thompson LD, Bullerdiek J, Flucke U, Franchi A. 4th ed. Lyon Cedex 08, France: International Agency on research on cancer; 2017. WHO Classification of Head and Neck Tumors Benign Soft Tissue Tumours; pp. 49–50. [Google Scholar]
- 9.Enzinger FM, Weiss SW, Chandrasekhar B. Soft Tissue Tumors Benign Tumors of Peripheral Nerves. 4th ed. Elsevier Health Sciences; pp. 1122–45. [Google Scholar]
- 10.Johnson HS, Wannamaker GT, Humes JJ, Thompson CW. Central neurofibroma. Oral Surgery, Oral Medicine, Oral Pathology. 1959;12:379–83. doi: 10.1016/0030-4220(59)90194-x. [DOI] [PubMed] [Google Scholar]
- 11.Gutman D, Griffel B, Munk J, Shohat S. Solitary neurofibroma of the mandible. Oral Surg Oral Med Oral Pathol. 1964;17:1–9. doi: 10.1016/0030-4220(64)90304-4. [DOI] [PubMed] [Google Scholar]
- 12.Baden E, Fischer RJ. Multiple neurofibromatosis and neurofibroma of the palate. Report of a case. Oral Surg Oral Med Oral Pathol. 1963;16:1356–64. doi: 10.1016/0030-4220(63)90412-2. [DOI] [PubMed] [Google Scholar]
- 13.Smith TT. Solitary neurofibroma of the larynx. Arch Otolaryngol. 1944;39:144–51. [Google Scholar]
- 14.Maruyama M, Fushiki H, Watanabe Y. Solitary neurofibroma of the floor of the mouth: a case report. Case reports in otolaryngology. 2011 Nov 20;2011 doi: 10.1155/2011/967896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.He Y, Wang J, Zhang Z, Yang H, Fu H. Solitary neurofibroma arising from the infratemporal fossa in a child. J Pediatr Surg. 2011;46:E13–6. doi: 10.1016/j.jpedsurg.2011.03.009. [DOI] [PubMed] [Google Scholar]
- 16.Boedeker CC, Ridder GJ, Kayser G, Schipper J, Maier W. Solitary neurofibroma of the maxillary sinus and pterygopalatine fossa. Otolaryngol Head Neck Surg. 2005;133:458–9. doi: 10.1016/j.otohns.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 17.Loutfy WG, Ryan DE, Toohill RJ, Meyer GA. Trigeminal nerve neurofibroma: Case report. J Oral Maxillofac Surg. 1990;48:650–4. doi: 10.1016/s0278-2391(10)80486-0. [DOI] [PubMed] [Google Scholar]
- 18.Stewart A, Bailey BM. Neurofibroma of the inferior alveolar nerve: Diagnostic and management difficulties. Br J Oral Maxillofac Surg. 1992;30:56–8. doi: 10.1016/0266-4356(92)90138-9. [DOI] [PubMed] [Google Scholar]
- 19.Rai A, Kumar A. Neurofibroma of facial nerve presenting as parotid mass. J Maxillofac Oral Surg. 2015;14:465–8. doi: 10.1007/s12663-014-0681-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hachach-Haram N, Gerarchi P, Benyon SL, Saggar A, McLellan G, Kirkpatrick WN. Multidisciplinary surgical management of cherubism complicated by neurofibromatosis type 1. J Craniofac Surg. 2011;22:2318–22. doi: 10.1097/SCS.0b013e318232a779. [DOI] [PubMed] [Google Scholar]
- 21.Akyüz SG, Çaltik A, Bülbül M, Erdoğan Ö, Renda R, Demircin G. An unusual pediatric case with neurofibromatosis and systemic lupus erythematosus. Rheumatol Int. 2012;32:2345–7. doi: 10.1007/s00296-011-1966-z. [DOI] [PubMed] [Google Scholar]
- 22.Schaffer R, Goss L, Romer MM, Kalamchi S. Down syndrome and neurofibromatosis: A case report. Spec Care Dentist. 2014;34:313–8. doi: 10.1111/scd.12062. [DOI] [PubMed] [Google Scholar]
- 23.Warhekar AM, Wanjari PV, Chaudhary A, Hada DS, Gupta R. A rare case report of neurofibromatosis I in HIV positive individual. J Clin Diagn Res. 2015;9:ZD20–2. doi: 10.7860/JCDR/2015/12111.5838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sujatha S, Jatti D. Neurofibromatosis and fibrous dysplasia manifesting in the same patient: A rare case report. J Investig Clin Dent. 2015;6:77–80. doi: 10.1111/jicd.12059. [DOI] [PubMed] [Google Scholar]
- 25.Shimoyama T, Kato T, Nasu D, Kaneko T, Horie N, Ide F. Solitary neurofibroma of the oral mucosa: A previously undescribed variant of neurofibroma. J Oral Sci. 2002;44:59–63. doi: 10.2334/josnusd.44.59. [DOI] [PubMed] [Google Scholar]
- 26.Lerman MA, Li CC, Woo SB. Dendritic cell neurofibroma with pseudorosettes: A clinicopathologic and immunohistochemical study of 5 intraoral cases. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;117:221–6. doi: 10.1016/j.oooo.2013.10.009. [DOI] [PubMed] [Google Scholar]
- 27.Kamra HT, Dantkale SS, Birla K, Sakinlawar PW, Bharia PH. Plexiform neurofibroma in the submandibular gland along with small diffuse neurofibroma in the floor of the mouth but without neurofibromatosis-1: A rare case report. Ecancermedicalscience. 2013;7:313. doi: 10.3332/ecancer.2013.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Campos MS, Fontes A, Marocchio LS, Nunes FD, de Sousa SC. Clinicopathologic and immunohistochemical features of oral neurofibroma. Acta Odontol Scand. 2012;70:577–82. doi: 10.3109/00016357.2011.640286. [DOI] [PubMed] [Google Scholar]
- 29.Cosetti MK, Golfinos JG, Roland JT., Jr Quality of Life (QoL) Assessment in Patients with Neurofibromatosis Type 2 (NF2) Otolaryngol Head Neck Surg. 2015;153:599–605. doi: 10.1177/0194599815573002. [DOI] [PubMed] [Google Scholar]


