Abstract
Context
X-linked hypophosphatemia (XLH) is a rare, genetic phosphate-wasting disease resulting in bone, muscular, and dental problems, beginning in childhood and increasing in adulthood.
Objective
This qualitative analysis aimed to explore patient-reported symptoms, complications, and experiences of XLH over the life-course, using data from a large multinational online survey.
Methods
Responses to 2 open-ended questions from 209 adults and 86 children/adolescents (proxy report) with self-reported XLH were analyzed in 8 age groups. Two researchers independently coded and analyzed the responses, using thematic analysis, with differences settled among a multidisciplinary group. Six themes were identified, with age subgroup analysis conducted on the 3 most common, according to coding frequency.
Results
Within theme 1, “Clinical Signs and Symptoms of XLH,” “Pain” was a dominant subtheme across the life-course, but “Skeletal Pathology” dominated the responses of children/adolescents. Within theme 2, “Impacts of Clinical Signs and Symptoms,” interference with “Physical Exertion” and “Emotional Wellbeing” (comprising depression/anxiety in adults and lack of self-esteem in children/adolescents) was reported across all ages. For theme 3, “Negative Treatment Experiences,” “Medication” was problematic for children, with adults reporting lack of “Access to Appropriate Treatment.” Three further themes were identified: “Resilience,” “Positive Treatment Experiences,” and “Information Needs.”
Conclusion
The multiple burdens imposed on people with XLH throughout their lifetime encompassed the physical, emotional, and social, although the most challenging symptoms or complications differed between ages. Burden was further exacerbated by adults’ lack of access to appropriate treatment, illustrating the need for age-appropriate multidisciplinary care.
Keywords: quality of life, rare disease, cross sectional survey, qualitative research
X-linked hypophosphatemia (XLH) is a rare, genetic, phosphate-wasting disease caused by inactivating mutations in the phosphate regulating endopeptidase homolog, X-linked (PHEX) gene, which causes hypophosphatemia and ultimately leads to impaired bone and dental mineralization and suboptimal growth, muscle development, and function [1]. Clinical manifestations of XLH usually begin in early childhood, once infants begin to weight-bear [2]. Phosphate deficit compromises skeletal development, resulting in lower limb deformities and shortened stature, as well as increased propensity for dental abscess [1-3]. As a result, most children with XLH have an abnormal gait, some delayed motor milestones, and experience pain [4]. Overall emotional wellbeing may be affected, and children may have difficulties with attendance and participation in school [5].
With the fusion of the growth plates during puberty, the skeletal deformities become permanent, often requiring corrective surgery [6, 7]. The development of subsequent morbidities has deleterious impacts on multiple body systems into adult life [4, 8]. Even for young adults, musculoskeletal morbidities can include pseudo-fractures, fractures, osteoporosis, osteoarthritis, osteophytes, enthesopathy, and spinal stenosis [9-11]. In a global survey of people with XLH, 44% of adult responders indicated a history of fracture and the mean (SD) age at first fracture was 26.4 (15.7) years; 46% and 27% of respondents reported osteophytes and enthesopathy, respectively, with the frequency of reporting increasing with age [4]. These reports may be an underestimate, as patients may not be aware of having these complications when self-reporting; other adult study populations have reported prevalence of these symptoms in the region of 61% to 85% [11]. These clinical morbidities have considerable impact on mobility, physical functioning, ability to perform daily activities, emotional wellbeing, and social/family/work life [4, 8, 12]. Moreover, pain and quality of life (QOL) physical functioning in adults with XLH was reported as significantly worse when compared with adults with another chronic skeletal disease (axial spondyloarthritis) [13].
A thematic analysis conducted on responses received during a 2018 UK National Institute for Health and Care Excellence online public consultation provided the first analysis of the lived experience of XLH across the lifetime. Asked about the burdens of XLH symptoms and treatment, conventional therapy (phosphate and calcitrol) was frequently reported as a burden for children, along with dosing regimen, adherence, distress, and pain. During adolescence, the burden became increasingly complex and multifactorial, with psychological factors dominating. In adults, the burdens of conventional therapy are discussed with frequency, along with bone deformity and orthopedic surgery, pain, mobility, fatigue, and dental problems [5].
A multinational online “XLH Burden of Disease” survey, completed by adults and children (by proxy) with XLH, was launched in June 2014 across 16 countries. Results of the primary analyses, presented and published in the Journal of the Endocrine Society, have already provided important insights into the impact of living with XLH [4]. However, participant responses to additional bespoke questions were not analyzed. These additional questions allowed participants to provide, in their own words, descriptions of symptoms and complications of XLH that most interfered with their lives, along with the option to report anything else about their experiences of living with XLH. Physicians treating people with XLH have anecdotally reported the importance of understanding the symptoms and complications that are prioritized by patients. The objective of the present analysis was to qualitatively explore the symptoms, complications, and other experiences resulting from XLH reported within the survey and describe specifically how these change over the life-course.
Methods
Data Collection
The survey was designed by Ultragenyx Pharmaceutical Inc., in partnership with the patient advocacy group The XLH Network Inc., and it comprised validated patient-reported outcome measures, details of which are published elsewhere [4], and open-ended bespoke questions, offered in English, German, Portuguese, French, and Spanish. Adults with XLH and caregivers of children with XLH were recruited through the sponsor, The XLH Network Inc., and clinicians. Respondents were asked to confirm diagnosis of XLH and whether a genetic confirmation of diagnosis (PHEX mutation) had been received; diagnosis was not verified with medical records [4]. This manuscript details the qualitative analysis of the responses to the following open-ended questions aimed at adults (18-65 years) and parents/carers of children and adolescents (1-17 years) with XLH:
Q1: “List the three symptoms or complications from XLH that interfere most with your life/with your child’s life”
Q2: “Is there anything else you would like us to know about your disease/your child’s disease?”
Analysis
From the original survey sample (n = 232 adults with XLH; n = 90 parents/carers), participants were excluded from the present analysis if they reported currently taking or having ever taken burosumab [14].
Therefore, the sample for qualitative analysis included 90% of adult survey respondents (n = 209) and 96% of proxy respondents for children and adolescents (n = 86), with 27 responses requiring translation into English (20 French, 6 Spanish, 1 Portuguese).
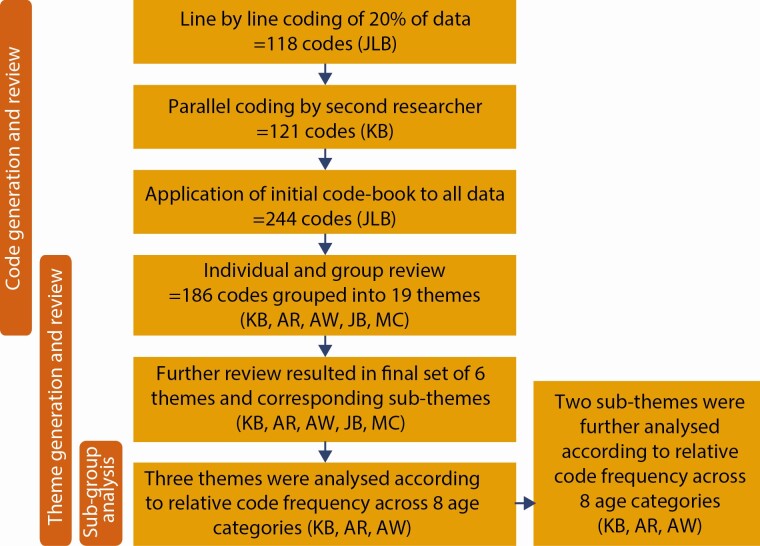
The responses collected in MS Office Excel were uploaded into NVivo software v12 [15] and analyzed by a multidisciplinary team of physicians and researchers, using hybrid deductive and inductive thematic analysis [16, 17]. All responses from both questions were analyzed together due to the rich variety of information provided in answer to the 2 questions, relating to symptoms, complications, and other experiences. The analysis stages comprised (Fig. 1): (1) Familiarization with data involving an initial read through of individual participant responses, noting early codes and emerging themes; (2) code generation and review involving the creation, merging and renaming of codes; (3) theme generation and review focusing on perceived meaning and patterns in the data at the more explicit or semantic level; and (4) subgroup analysis of the 3 main themes according to 8 predefined age groups (1-4, 5-12, 13-17, 18-29, 30-39, 40-49, 50-59, 60 + years). This provided a quantification of the content [18] according to the number of code references assigned under the themes or subthemes, reported as frequencies and reported descriptively. Parallel coding of 20% of the data by a second researcher and review of codes by the team aimed to facilitate open discussion about the interpretation and meaning of the responses, which can potentially improve the consistency or reliability of the coding and analysis [19]. Quotes are accompanied with ID number, sex, and age group to highlight diversity of the sample.
Figure 1.
Process of qualitative data analysis.
Results
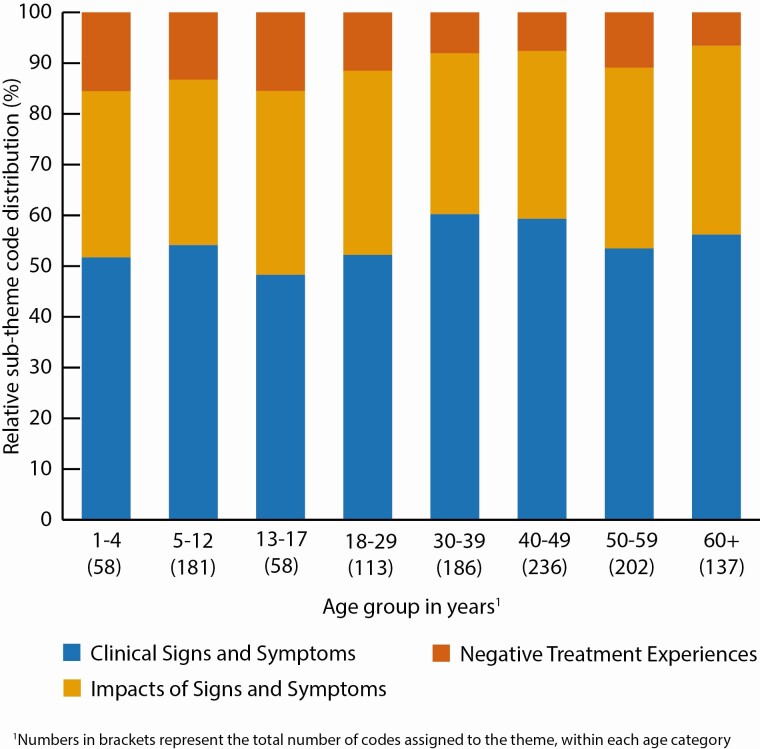
Table 1 illustrates the demographics of the respondents. The majority of the 295 adults and children were based in the United States (59%, n = 174) and female (70%, n = 207), with the 40-49 years category forming the largest age group (21%, n = 61) followed by 5-12 years (17%, n = 51). Fig. 2 outlines 6 themes, subthemes, and codes. Participants reported a myriad of symptoms, complications, and consequences of XLH that interfered with their lives. These were grouped together according to 3 main themes (1)“Clinical Signs and Symptoms of XLH,” (2)“Impacts of Clinical Signs and Symptoms,” and (3) “Negative Treatment Experiences,” which together comprised 95% (n = 1171) of total code references. These themes were present across all ages (Fig. 3) and subgroup analysis was conducted according to the quantification of codes grouped under each theme and presentation of their relative distribution across each age category. Due to the inductive nature of the analysis, 3 additional themes were also identified, which explored wider patient-reported experiences of living with XLH: (4) “Resilience,” (5)“Positive Treatment Experiences,” and (6)“Information Needs.” These themes accounted for a minority of total code references (n = 65); therefore, subgroup analysis by age was not deemed appropriate.
Table 1.
Participants With XLH—Demographics
| Age group (years) | Sex (n) | Region (n) | |||||
|---|---|---|---|---|---|---|---|
| Female | Male | Total | USA | EU | Rest of world | Total | |
| 1-4 | 5 | 10 | 15 | 7 | 2 | 6 | 15 |
| 5-12 | 29 | 22 | 51 | 25 | 13 | 13 | 51 |
| 13-17 | 13 | 6 | 19 | 9 | 6 | 4 | 19 |
| 18-29 | 17 | 10 | 27 | 18 | 3 | 6 | 27 |
| 30-39 | 36 | 9 | 45 | 25 | 11 | 9 | 45 |
| 40-49 | 48 | 13 | 61 | 39 | 16 | 6 | 61 |
| 50-59 | 33 | 13 | 46 | 28 | 15 | 3 | 46 |
| 60+ | 26 | 5 | 31 | 23 | 4 | 4 | 31 |
| Total | 207 | 88 | 295 | 174 | 70 | 51 | 295 |
Figure 2.
Themes, subthemes, and codes.
Figure 3.
Relative distribution of the code frequencies within the 3 main themes, analyzed by age group.
Theme 1: Clinical Signs and Symptoms of XLH
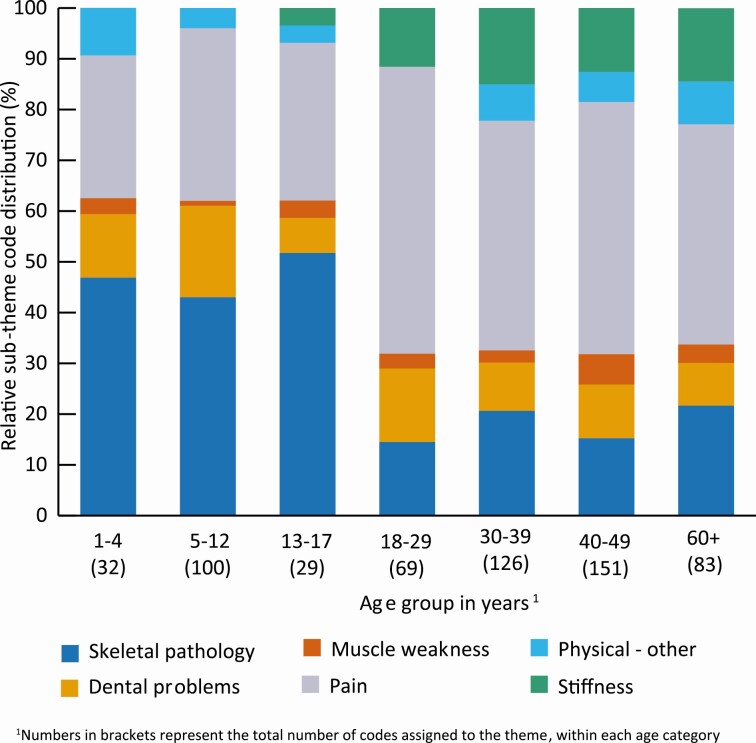
The theme of “Clinical Signs and Symptoms of XLH” comprised 6 subthemes: “Pain,” “Skeletal Pathology,” “Dental Problems,” “Stiffness,” “Muscle Weakness,” and “Other Physical Complications,” most of them featuring across the life-course (Fig. 4). However, their relative distribution (according to code reference frequency) varied by age category. For children (1-4 and 5-12 years) and adolescents (13-17 years), the subtheme of “Skeletal Pathology” (eg, bone/ joint impairments, short stature) dominated (43%-52%) as illustrated:
Figure 4.
Theme 1: Clinical signs and symptoms of XLH, relative distribution of subthemes, analyzed by age.
Bones are so weak won’t hold rods and they have had to be removed. Cannot put more back in (ID 252, M, 5-12).
Her bowed legs and waddle gait make it difficult to run with other children (ID279, F, 1-4).
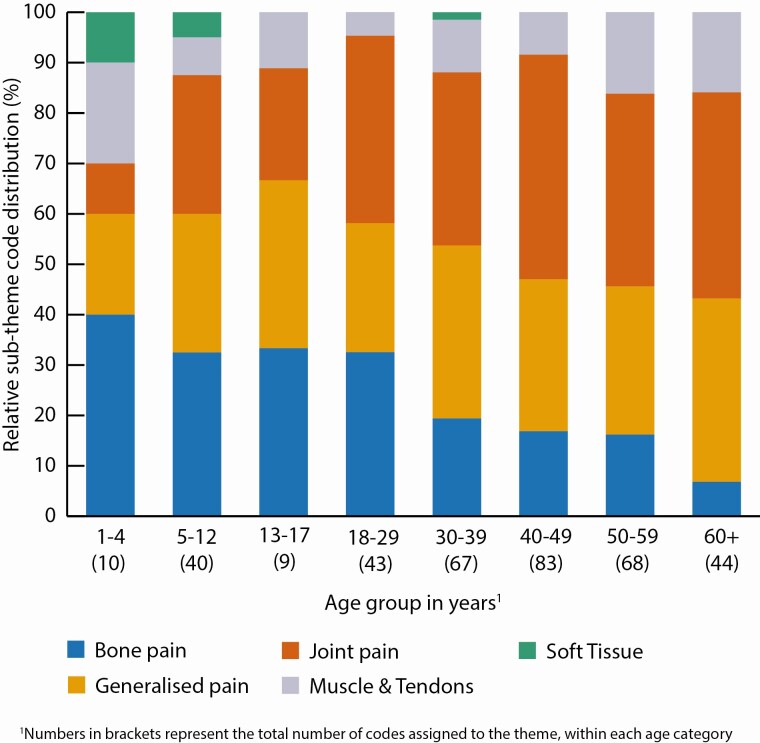
Problems relating to “Skeletal Pathology” were less frequently reported by adults (14%-22% relative code frequency across adult age groups), in comparison to reports of “Pain” (43%-57%), the most frequently reported symptom. “Pain” was also reported frequently in the child and adolescent proxy respondents (28%-34%), but less frequently than skeletal pathology. According to further subgroup analysis conducted on this subtheme (Fig. 5), in children and adolescents, the pain most frequently reported was bone pain (33%-40%). In adults, joint pain became more prominent than bone pain (34%-45%). Some respondents provided details of pain triggers, such as physical activity, weather changes, or menstruation as illustrated below:
Figure 5.
Pain subtheme (Theme 1), relative code frequency distribution, analyzed by age.
The only pain I feel daily is joint pain in my legs and back when I wake up in the mornings, and knee pain from my left leg being slightly more curved, even after the osteotomy. The severe pain throughout my entire legs, however, occurs regularly with menstruation, and more irregularly with weather change and after extensive walking (ID149, F, 18-29).
The pain in her legs during running and after she is done (ID243, F, 5-12).
The subtheme of “Dental Problems” was present throughout the life-course (7%-18%) (Fig. 4), described by respondents as abscesses, loss of teeth, and tooth pain, which often required excessive and costly dental work.
Loss of teeth/constant gum abscesses ongoing from 10 years old (ID 175, M, 30-39).
“Stiffness” was a subtheme that started to feature in adolescent proxy responses (3%) and increased notably in adult responses (12%-15%), with reports from young adults a similar frequency to those in the oldest age group (Fig. 4). The reports were often mentioned alongside pain, particularly in the older adults; however, 1 respondent stressed the uniqueness of stiffness.
My issues are with stiffness NOT pain. Stiffness is on both right and left legs and feet. One side is not more stiff than the other (ID78, F, 60+).
Theme 2: Impacts of Clinical Signs and Symptoms of XLH
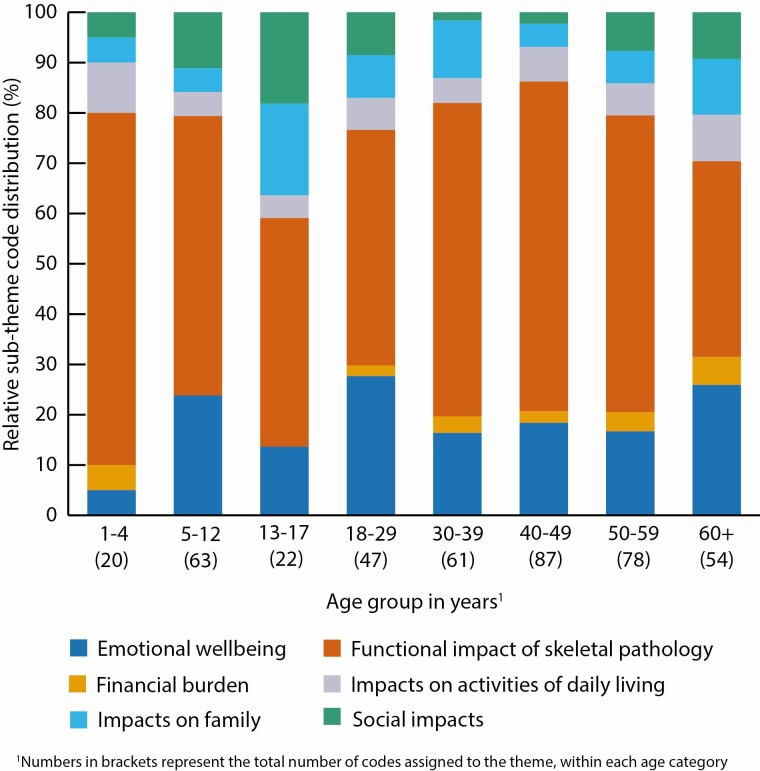
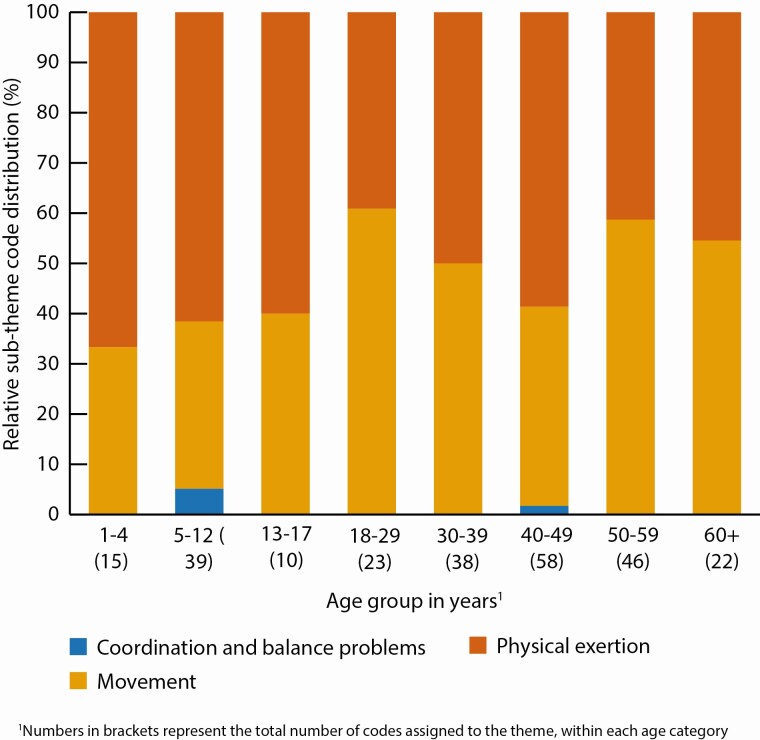
Theme 2, “Impacts of Clinical Signs and Symptoms of XLH,” contained the subthemes of: “Functional Impact of Skeletal Pathology,” “Emotional Wellbeing,” “Financial Burden,” “Impacts on Daily Living,” “Impacts on Family,” and “Social Impacts” (Fig. 6). The “Functional Impacts of Skeletal Pathology” was the most frequently reported subtheme across all age groups (39%-70% relative code frequency across ages). Further subgroup analysis undertaken by age (Fig. 7) identified that in children and adolescents, “Physical Exertion” (60%-67%), such as difficulties with running and excessive fatigue and tiredness, were reported more frequently than impact on “Movement”(33%-40%).
Figure 6.
Theme 2: Impacts of clinical signs and symptoms of XLH, relative distribution of subthemes, analyzed by age.
Figure 7.
Functional impacts of skeletal pathology subtheme (Theme 2), relative code frequency distribution, analyzed by age.
Difficulty running and sometimes walking without tripping over pigeon-toed feet. Gets tired and in pain when we walk too far (ID288, M, 1-4).
In adults, impact on “Movement” (40%-61%) was reported with similar frequency to “Physical Exertion” (39%-59%).
Limited range of motion in hips - just can’t do things I used to be able to do. This didn’t start until my early 30’s (ID79, F, 30-39).
The subtheme of “Emotional Wellbeing” was identified across all age groups (5%-28%) (Fig. 6), although the particular complications differed according to age. Proxy responses for both children and adolescents described lack of self-esteem or being self-conscious.
We’re dealing most with self-esteem right now “I can’t run as fast as so-and-so,” “I’m slower than everyone else,” “I want to be taller” (ID256, F, 5-1).
Multiple emotional difficulties were reported across adulthood, including depression, anxiety, and frustration. Young adults (18-29 years) also described worries about the future.
I feel stuck in a cycle of diminishing activity due to pain and stiffness that leads to weight gain and depression (ID19, F, 50-59).
Sadness because my legs hurt all the time and I never have fun anymore because of it (ID133, F, 30-39).
The subtheme of “Social Impacts” was less frequently reported relative to some of the other subthemes (2%-18%) but was of clear concern to some respondents (Fig. 6). These were most notable in the descriptions of the adolescents (18%), particularly in relation to feeling different from peers. They reported teasing and bullying either due to physical appearance, or the inability to do the same activities as peers.
Feeling down when excluded from vigorous activities, because peers think he is too slow or not able (ID 218, M, 13-17).
While not so frequently reported relative to the other subthemes, adults also described difficulties in intimate relationships and social isolation.
As soon as a relationship becomes serious and information about my genetic condition is shared, such as the fact that I will pass this condition on to all my female children, complications arise with the relationship (ID90, M, 18-29).
The subtheme “Impacts on Family” (5%-18%) related to the genetic nature of the condition and sadness and frustration that multiple generations of family members had XLH, and the untold impacts on the siblings who did not have XLH.
Two of my three children have XLH and that has taken a toll, physically and emotionally (ID09, F, 60+).
One proxy respondent of an adolescent listed her own experiences of living with XLH as one of the complications interfering most in her child’s life.
Having a mother with XLH pain (ID211, F, 13-17).
Some described the anguish caused by this reality and one man felt strongly that his choice not to have children was a moral one. Some women were concerned about the physical burden of pregnancy and birth.
I worry about the stress of pregnancy on my joints, especially my hips and knees (ID139, F, 18-29).
Theme 3: Negative Treatment Experiences
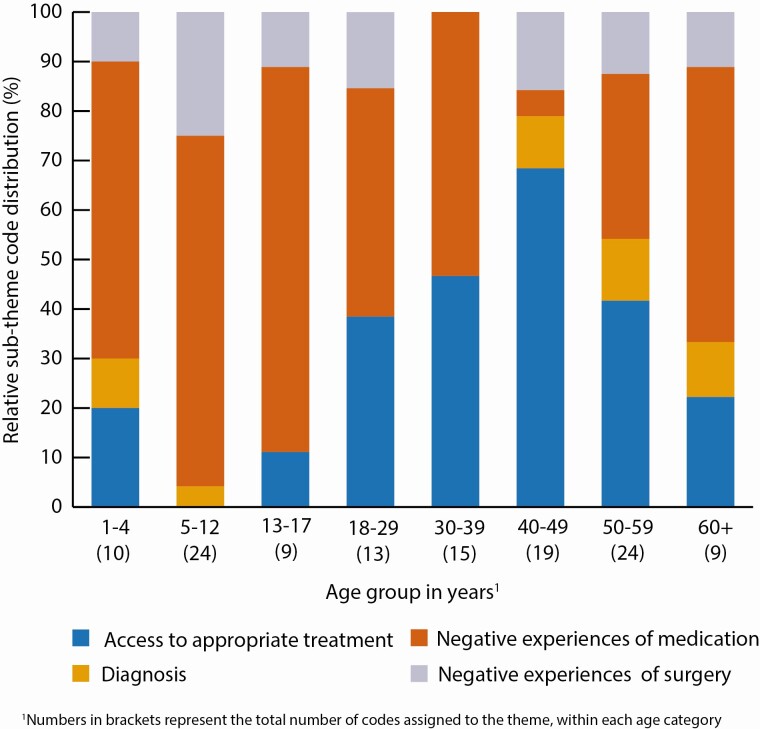
The theme “Negative Treatment Experiences” comprised the 4 subthemes of: “Access to Appropriate Treatment,” “Diagnosis,” “Negative Experiences of Medication” and “Negative Experiences of Surgery” (Fig. 8). “Negative Experiences of Medication” were reported across all ages, most notably in children and adolescents (60%-78%), but also featuring in the responses of adults (5%-56%). Child and adolescent proxy respondents described the challenges of frequent medication doses, while adults tended to focus on describing side effects from conventional medication.
Figure 8.
Theme 3: Negative treatment experiences, relative distribution of subthemes, analyzed by age.
Medical care every 6 hours- phosphate (ID 258, F, 5-12).
In order to avoid the chronic diarrhoea during work or social functions, I skip my medication (ID139, F, 18-29).
Issues relating to “Access to Appropriate Treatment” were reported frequently in adults (22%-68%). Respondents described their frustration and anguish due to the perceived lack of knowledge, interest, and understanding among doctors and dentists about XLH and suitable treatment. Although some child and adolescent proxy respondents commented on this issue, it was minimal in comparison to complaints about medication.
After we turned 18, our doctors, who we considered practically family, did not help us, or guide us, to where or what we needed to do as adults with XLH (ID170, F, 30-39).
My daughter also reports a flashing pain which the doctor says is in her head (ID266, F, 13-17).
With the exception of 1 age category (30-39 years), “Negative Experiences of Surgery” were reported to some degree across all age categories (0%-25%). Respondents described the burden of frequent and serious operations or complications resulting from surgery.
Pain due to recent growth plate stapling-2 weeks ago. Loss of range of motion following 8-plate surgeries (ID 231, F, 5-12).
The operations I had to straighten my right leg caused nerve damage, I think this is why I take more painkillers and feel worse (ID37, F, 18-29).
Some respondents, mainly in the older age groups, described challenges in receiving an XLH diagnosis, resulting in “misdiagnosis” and/or being “diagnosed late.”
I feel like I get treated for this issue, or that issue, with no connection between them (ID50, M, 40-49).
Theme 4: Resilience
The theme “Resilience” comprised 2 subthemes: “Coping Strategies” and “Accustomed to the Condition.” Participants described a range of “Coping Strategies”; some of these were psychological in terms of working to maintain a positive attitude in the face of extreme adversity.
I may be dissatisfied but overall, I’m a very happy person who loves life and makes the most of it (ID86, F, 60+).
Despite being ridiculed while growing up, short stature, and pain that interfered with relationships and job opportunities, 1 respondent stated:
Despite issues of chronic pain, limited range of motion, reduced recreational activities I try to maintain an attitude of acceptance, minimize depression and focus on being a compassionate and kind human being. Meditation and some daily walking with my dog also provide emotional benefits (ID 73, M, 60+).
Other strategies described by respondents related to making efforts to stay active.
I participate in non-weight bearing water sports regularly and I feel this has helped relieve pain and stiffness and kept my muscles strong (ID86, F, 60+).
The subtheme of “Accustomed to the Condition” was also identified as an alternative form of resilience, as respondents described making adaptions to deal with their lifelong condition.
There is never a time when I am pain free. I have learned how to deal with it but it is frustrating (ID45, F, 40-49).
Theme 5: Positive Experiences of Treatment
Due to the nature of the research questions, the majority of participants described “Negative Treatment Experiences” as previously reported (theme 3). However, some respondents provided positive feedback. These were subthemed as “Positive Aspects of Conventional Treatment” and “Positive Experiences of Alternative Therapies.” As part of the subtheme of “Positive Aspects of Conventional Treatment,” some participants described how conventional medication and surgery had improved their symptoms:
After the corrective procedure performed in June 2012, my son is doing well and acting like a normal child (ID234, M, 13-17).
Theme 6: Information Needs
This theme is comprised of 3 subthemes. One of these, “Disease and Treatment Information,” related to the information needs of respondents themselves. Some participants had specific questions about how to manage the condition on a daily basis, such as the role of exercise and weight management.
More information on the other metabolic aspects of this disease which affect adults eg, glucose intolerance and weight gain (ID15, F, 60+).
Others discussed the desire to find out about specialist doctors in their area and explore treatment options, either for the first time, or returning in adulthood.
I am not currently being treated for XLH but would be interested in finding a specialist (ID46, F, 30-39).
Some expressed frustration due to “Lack of Awareness Among Others” about living with a rare condition. Other spoke about “The Role of Research” in terms of the requirements for more research and the desire to participate in trials, which was difficult for some due to low kidney function (a side effect of conventional therapy).
Hopefully research will provide them [children] with many treatment options if they need it (ID122, F, 30-39).
One respondent stressed how the disease was all-encompassing and highlighted the limitations of patient-reported outcome measures for adequately capturing the full experience of living with XLH.
This questionnaire, which I was glad to help with, does not even come close to building a model to construct a phenomenology of XLH. The experience of the disease, testing, surgeries, other treatments, and the social ramifications are beyond the scope of the questions that were asked (ID81, M, 60+).
Discussion
This qualitative study draws upon data generated from the largest survey undertaken to date of people with XLH [4]. Thematic analysis of responses to 2 open-ended survey questions from adults with XLH and proxy respondents for children and adolescents, identified that pain and skeletal pathology were the symptoms most frequently reported as interfering most in their lives. The symptoms negatively impacted the lives of people with XLH, regardless of age, and have all-encompassing impacts on QOL, physical activity, psychological distress, family, and social life. Child proxy respondents described daily routines that are dominated by repeated medication doses, ongoing painful surgeries, and for adults, lack of access to appropriate treatment dominated.
The proxy respondents of children and adolescents indicated most concern with skeletal pathology, particularly with the skeletal deformities and shortened stature. This supports previously published data from this survey, showing a high prevalence of lower limb deformities in children and adolescents, with bowing of the tibia and/or fibula reported for 72% (65/90), bowing of the femur reported for 63% (57/90), and knock-knees (genu valgum) in 32% (29/90) [4]. Short stature is a known consequence in children with XLH, and data has demonstrated that, despite use of conventional treatment, growth rates progressively decline during early childhood, remaining behind healthy peers [20, 21]. Pain, particularly bone pain, was also reported with high frequency for children and adolescents, corroborating the pain research published elsewhere [4, 22]. For example, this survey data has previously reported that 80% of children and adolescents had experienced bone or joint pain and 60% had muscle pain, in the year prior to taking the survey [4].
Our analysis has highlighted how the impacts of skeletal pathology resulted in significant impairments to walking, running, and playing sports, corroborating several other studies using patient-reported measures of mobility and physical function [4, 22]. Problems with physical exertion, combined with concerns with physical bodily appearance, unsurprisingly contribute to the emotional distress felt by children and adolescents, differentiating them from their peers during a time in life where appearance plays a key role in developing a sense of self [23]. Self-esteem was singled out as a particular concern, corroborating other research with young people with different types of physical impairments, which showed the effects of minor physical disabilities on self-esteem related to physical competence were large [24]. The qualitative analysis of statements received during the 2018 National Institute for Health and Care Excellence online public consultation showed a quarter of the adolescent statements were related to psychological burden such as self-esteem, confidence, and distress [5]. The statements regarding children frequently reported the burden of conventional medication, something also identified in our survey responses, in terms of dosing regime and multiple painful surgeries.
In adults with XLH, our survey data suggests that multiple symptoms and complications still exist, but their profile differs. While skeletal pathology is frequently reported, pain dominates, echoing other XLH studies [4, 12, 25], but here the focus is on joint pain. In previously published data from this survey, 67% of the adult sample reported pain medication use at least once a week, yet the mean scores for pain severity and worst pain in the past 24 hours indicated that they continued to suffer with moderate pain [4]. In a previous multi-country (UK, Finland, France, Germany, and Luxembourg) qualitative interview study, adult participants with XLH described experiencing pain on a daily basis. Pain severity ranged from mild to extremely severe and typically varied from day to day, but most participants reported a constant base level of pain even during milder periods [12]. The reports of joint pain may relate to the development of osteoarthritis as adults get older. Data from adults with XLH in a clinical trial with moderate to severe baseline pain suggested corresponding high rates of multiple musculoskeletal morbidities such as osteoarthritis, enthesopathy, as well as fractures and pseudo-fractures [9]. Therefore, it is likely that the joint pain identified in adults in the current analysis is related to multiple morbidities.
Dental problems, including dental pain, also existed across the life-course and preventative work in childhood may prevent dental pathology in adulthood. As well as pain, this analysis identified a distinct concept of stiffness, described as causing significant interference on life beginning in young adulthood. This aligns with other studies that have also highlighted patient-reported stiffness for XLH to be notably higher than population normative scores, even as a young adult [4, 16]. However, we should not assume this concept is unimportant to children and adolescents, who may well struggle to communicate the difference between pain and stiffness. For example, in a recent consultation exercise with 4 young people with XLH, pain was described as “achy” [26].
Our findings also suggest that the cumulative burden of the childhood emotional consequences of living with XLH, combined with an ever-increasing physical burden into adulthood, can manifest as depression, anxiety, and isolation. This is supported by the literature; for example, a study of routine clinical record data from the UK highlighted that the odds of depression occurring in people with XLH was 3 times greater than matched controls without XLH (OR 2.95; 95% CI, 1.47-5.92; P < 0.01) [27]. Previously published longitudinal abstract data also hints at the risks of impending anxiety that may develop over time among adults living with XLH [28].
Furthermore, our survey findings highlight problematic access to treatment for adults, unlike children and adolescents, which no doubt contributes to worries about the future and anxiety. With this cumulation of experiences throughout life, it is perhaps not surprising that some of our survey participants described becoming accustomed to their condition and using various coping strategies. A large population-based study identified that among those with chronic illness, optimism, and resilience appeared to be more important to those facing severe limitations to daily activities, than those who were not, suggesting that positive psychological appraisals play a key role in maintaining wellbeing when faced with debilitating illnesses [29]. Resilience can be defined as the ability to adapt one’s responses in the face of adversity and the associated stressors, and is a concept influenced by psychological, biological, and environmental factors [30]. Cal and colleagues, in their narrative systematic review of resilience and chronic diseases, suggested that people scoring lower on measures of resilience have less capacity to deal with the stressors and challenges of becoming ill [31]. Our study did not set out to explore this relationship in the survey data; however, our findings do highlight a need to support people with the psychological and emotional challenges they face, in addition to managing the clinical signs and symptoms of XLH.
None of the respondents in our survey referred to receiving support from a psychologist as part of their treatment plan; however, respondents described varied practical and psychological strategies used to cope with their challenges, emphasizing the role of resilience building among children and young people. Some clinical services in the UK offer a psychology service to teach strategies and skills to young people living with XLH in order to build confidence, particularly during periods of transition such as moving schools. In addition, for adults, psychosocial interventions may be required to address depression and anxiety. Given the inherited nature of the condition, psychological support that addresses the whole family system is also warranted [32].
Our study also highlighted the need for more educational material for people living with XLH, in terms of managing the condition in daily life and increasing access to appropriate treatment. The lack of access to specialist doctors who understand XLH, particularly for adults, corroborates the findings in other research [8, 33]. A recent survey of patient advocacy groups in 11 European countries illustrated high unmet need in a number of countries relating to adequate pain management (Spain, Italy, Finland), physiotherapy (UK, Spain), and support to access the workplace (Finland, Italy) [33]. Moreover, it is our experience that the lack of understanding about XLH in treating physicians can lead to delayed management and results in preventable bone deformities, which may be irreversible. The study results highlight the need for further training and education within the medical community, as well as the need to train multidisciplinary healthcare professionals such as psychologists, occupational therapists, and social workers [8].
Study Strengths and Limitations
The research methodology adopted here is considered a robust and credible approach to qualitative research [34]. The survey was offered in multiple languages and the data used in the analysis were obtained from a large heterogenous sample of participants in terms of age, sex, and country of origin. The process of analysis involved a multidisciplinary team of researchers who conducted parallel coding of a portion of data, cross-checking codes, and discussing the development of themes to prevent individual researcher bias. Two specialist bone physicians were involved in reviewing codes and themes, to facilitate clinical interpretation of the findings. The research demonstrates credibility in its triangulation of data from both the quantification of themes/subthemes, as well as the illustration of rich and varied quotes from a variety of participants [34, 35].
However, there are some study limitations that should be noted. Our sample relied upon recruitment from physicians and patient advocacy groups who may not be representative of the wider XLH population. For example, those with greater disease severity and QOL burden may be more motivated to complete a survey. Secondly, data from children under 18 years relied on proxy reports from parents and carers. This may have resulted in an under- or overestimate of reporting about the severity of issues [36]. For example, 1 carer reported that their child was still too young to tell them about the specific pain or severity. Parents and carers may also be unaware of the full extent of the emotional or mental distress felt by their child.
Future Research Needs
Our findings concur with a recent expert consensus exercise to identify research priorities for rare musculoskeletal diseases, which cited the need for more research into the psychological impacts and support needs of patients and their families, the role of fatigue, as well as disease progression in aging [37]. There is also a need for direct research with children and young people with XLH, rather than via proxy, in order to fully illustrate their experiences.
Conclusion
Taken together, the findings show, from the largest survey to date completed by people with XLH, the multiple burdens imposed across the lifetime of XLH, negatively impacting physical, emotional, and social areas of life. While the symptoms or complications that interfere the most vary between children, adolescents, and adults, understanding these differences may help to guide physicians in deciding care pathways, and inform the population with XLH about disease trajectory. The burden of XLH may be further exacerbated by lack of access to appropriate treatment, particularly for adults, illustrating the need for age-appropriate multidisciplinary care that includes psychological support.
Acknowledgments
Under the direction of the authors, analyst Jacqui Bernarde (JLB) (OPEN Health) also conducted the data analysis.
Sponsorship: The survey was sponsored by Ultragenyx Pharmaceutical Inc. and the analysis sponsored by Kyowa Kirin International. Research design, analysis, and medical writing services provided by OPEN Health were funded by Kyowa Kirin International.
Authors K.B., A.R., and A.W. designed the qualitative study. Authors K.B., A.R., A.W., J.B., and M.C. contributed to the data analysis and interpretation of the study data. All authors critically reviewed the manuscript and approved the final version for submission.
Glossary
Abbreviations
- QOL
quality of life
- XLH
X-linked hypophosphatemia
Additional Information
Disclosures: J.B. and M.C. have received honoraria for serving as an advisory board member or for lectures from Kyowa Kirin International and have received consulting fees for providing clinical input to this study. A.W. and A.R. declare that they are an employees of Kyowa Kirin Services Ltd. K.B. declares that they have no personal, commercial, academic, or financial conflicts of interest.
Data Availability
Some or all datasets generated during and/or analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.
References
- 1. Carpenter TO, Imel EA, Holm IA, Jan de Beur SM, Insogna KL. A clinician’s guide to X-linked hypophosphatemia. J Bone Miner Res. 2011;26(7):1381-1388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Linglart A, Biosse-Duplan M, Briot K, et al. Therapeutic management of hypophosphatemic rickets from infancy to adulthood. Endocr Connect. 2014;3(1):R13-R30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cremonesi I, Nucci C, D’Alessandro G, Alkhamis N, Marchionni S, Piana G. X-linked hypophosphatemic rickets: enamel abnormalities and oral clinical findings. Scanning. 2014;36(4):456-461. [DOI] [PubMed] [Google Scholar]
- 4. Skrinar A, Dvorak-Ewell M, Evins A, et al. The lifelong impact of X-linked hypophosphatemia: results from a burden of disease survey. J Endocr Soc. 2019;3(7):1321-1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ferizović N, Marshall J, Williams AE, et al. Exploring the burden of X-linked hypophosphataemia: an opportunistic qualitative study of patient statements generated during a technology appraisal. Adv Ther. 2020;37(2):770-784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Fucentese SF, Neuhaus TJ, Ramseier LE, Ulrich Exner G. Metabolic and orthopedic management of X-linked vitamin D-resistant hypophosphatemic rickets. J Child Orthop. 2008;2(4):285-291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gizard A, Rothenbuhler A, Pejin Z, et al. Outcomes of orthopedic surgery in a cohort of 49 patients with X-linked hypophosphatemic rickets (XLHR). Endocr Connect. 2017;6(8):566-573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hughes M, Macica C, Meriano C, Doyle M. Giving credence to the experience of X-linked hypophosphatemia in adulthood: an interprofessional mixed-methods study. J Patient Cent Res Rev. 2020;7(2):176-188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Javaid MK, Ward L, Pinedo-Villanueva R, et al. Premature manifestation and accumulation of musculoskeletal- related diseases in adults with X-linked hypophosphatemia (XLH): an analysis of baseline medical history clinical trial data. Poster presented at: American Society for Bone and Mineral Research Annual Meeting;11-15 September 2020; Online.
- 10. Javaid MK, Imel E, Pinedo-Villanueva R, et al. Real-world evidence of the progressive and cumulative morbidity arising from X-linked hypophosphatemia (XLH) over the adult life course. Paper presented at: American Society for Bone and Mineral Research Annual Meeting; 11-15 September 2020; Online. [Google Scholar]
- 11. Bubbear J, Rylands AJ, Williams A, Bailey KMA, Cheung M. A qualitative thematic analysis to map the most frequent patient-reported symptoms and complications of X-linked hypophosphatemia over the life-course. Poster presented at the: Annual meeting of the American Society for Bone and Mineral Research; 11-15 September 2020; Online. [Google Scholar]
- 12. Lo SH, Lachmann R, Williams A, Piglowska N, Lloyd AJ. Exploring the burden of X-linked hypophosphatemia: a European multi-country qualitative study. Qual Life Res. 2020;29(7):1883-1893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Che H, Roux C, Etcheto A, et al. Impaired quality of life in adults with X-linked hypophosphatemia and skeletal symptoms. Eur J Endocrinol. 2016;174(3):325-333. [DOI] [PubMed] [Google Scholar]
- 14. NICE. Burosumab for treating X-linked hypophosphataemia in children and young people. NICE highly specialised technologies guidance HST8. Published October 10, 2018. www.nice.org.uk/guidance/hst8. Accessed September 15, 2020.
- 15. QSR International Pty Ltd; 2018. NVivo version 12. https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home. Accessed October 29, 2020.
- 16. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77-101. [Google Scholar]
- 17. Attride-Stirling J. Thematic networks: an analytic tool for qualitative research. Qual Res. 2001;1(3):385-405. [Google Scholar]
- 18. Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277-1288. [DOI] [PubMed] [Google Scholar]
- 19. Barbour RS. Checklists for improving rigour in qualitative research: a case of the tail wagging the dog? BMJ. 2001;322(7294):1115-1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mao M, Carpenter TO, Whyte M, et al. Growth curves for children with X-linked hypophosphatemia. J Clin Endocrinol Metab. 2020;105(10): 3243-3249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Nielsen LH, Rahbek ET, Beck-Nielsen SS, Christesen HT. Treatment of hypophosphataemic rickets in children remains a challenge. Dan Med J. 2014;61(7):A4874. [PubMed] [Google Scholar]
- 22. Carpenter TO, Whyte MP, Imel EA, et al. Burosumab therapy in children with X-linked hypophosphatemia. N Engl J Med. 2018;378(21):1987-1998. [DOI] [PubMed] [Google Scholar]
- 23. Anderson FJ. Self-concept and coping in adolescents with a physical disability. Issues Ment Health Nurs. 1982;4(4):257-274. [DOI] [PubMed] [Google Scholar]
- 24. Miyahara M, Piek J. Self-esteem of children and adolescents with physical disabilities: quantitative evidence from meta-analysis. J Dev Phys Disabil. 2006;18(3):219-234. [Google Scholar]
- 25. Ruppe MD, Zhang X, Imel EA, et al. Effect of four monthly doses of a human monoclonal anti-FGF23 antibody (KRN23) on quality of life in X-linked hypophosphatemia. Bone Rep. 2016;5:158-162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Rylands AJ, Williams A, Davies EH, Vincent SA, Bailey KMA. A patient-centric approach to designing a mixed-methods observational study involving adolescents with X-Linked Hypophosphatemia. Poster presented at; ISPOR Europe 2020; 16-19 November 2020; Online. [Google Scholar]
- 27. Hawley S, Shaw NJ, Delmestri A, et al. Characterization of comorbidity in X-linked Hypophosphatemia: A prospective parallel cohort study using the UK CPRD. Poster presented at; Bone Research Society Annual Meeting 2020; 6-8 July 2020; Online. [Google Scholar]
- 28. Cole S, Gray N, Barrett J, et al. Change in patient-reported outcomes of XLH registry participants in the UK: a longitudinal study. Abstract presented at: World Congress on Osteoporosis, Osteoarthritis and Musculoskeletal Diseases; 20 August 2020; Online. [Google Scholar]
- 29. Maguire R, Hanly P, Maguire P. Living well with chronic illness: how social support, loneliness and psychological appraisals relate to well-being in a population-based European sample. J Health Psychol. Published online October 24, 2019. doi: 10.1177/1359105319883923 [DOI] [PubMed] [Google Scholar]
- 30. Rutter M. Implications of resilience concepts for scientific understanding. Ann N Y Acad Sci. 2006;1094:1-12. [DOI] [PubMed] [Google Scholar]
- 31. Cal S, de Sá LR, Glustak ME, Santiago MB. Resilience in chronic diseases: a systematic review. Cogent Psychol. Published online April 15, 2015;2(1):1-9. doi:10.1080/23311908.2015.1024928 [Google Scholar]
- 32. Morison JE, Bromfield LM, Cameron HJ. A therapeutic model for supporting families of children with a chronic illness or disability. Child Adolesc Ment Health. 2003;8(3):125-130. [DOI] [PubMed] [Google Scholar]
- 33. Harvengt P, Seefried L, Perera L. Unmet needs of adults with XLH: results from a survey of European patient organizations. Poster presented at: 10th European Conference on Rare Diseases & Orphan Products; 14-15 May 2020; Online. [Google Scholar]
- 34. Tracy SJ. Qualitative quality: eight “big-tent” criteria for excellent qualitative research. Qual Inq. 2010;16(10):837-851. [Google Scholar]
- 35. Nowell LS, Norris JM, White DE, Moules NJ. Thematic analysis: striving to meet the trustworthiness criteria. Int J Qual Methods. 2017;16(1):160940691773384. [Google Scholar]
- 36. Eiser C, Morse R. Can parents rate their child’s health-related quality of life? Results of a systematic review. Qual Life Res. 2001;10(4):347-357. [DOI] [PubMed] [Google Scholar]
- 37. Mickute G, Staley K, Delaney H, et al. Rare musculoskeletal diseases in adults: a research priority setting partnership with the James Lind Alliance. Orphanet J Rare Dis. 2020;15(1):117. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Some or all datasets generated during and/or analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.