Abstract
Purpose
Endoscopic endonasal balloon-assisted dacryoplasty is a minimally invasive surgical approach that can be applied after failure of dacryocystorhinostomy with recurrence of distal acquired lacrimal obstruction.
Methods
At the Department of Otolaryngology, San Raffaele Hospital, Milan (Italy), from December 2016 to October 2020, 14 patients underwent trans-nasal balloon-assisted dacryoplasty after a failed dacryocystorhinostomy (both external and endoscopic endonasal). The routinary pre-operative work-up included multidisciplinary study of the lacrimal disease, which consisted in primary ophthalmological and otorhinolaryngological visits associated with nasal endoscopy, in which a radiological exam was added if needed. The surgical approach includes pneumatic enlargement of the stenotic rhinostomy, created during the primary dacryocystorhinostomy, using a high-pressure trans-nasal balloon catheter. Anatomical success was considered when the ostium was patent upon irrigation, while functional success was considered as resolution of epiphora or free lacrimal flow on functional test.
Results
Among 14 patients included and after a mean follow-up of 19.5 months (range 13–51 months), anatomic success was achieved in 100% of patients and functional success was achieved in the 85.7% (12/14). Operative time ranged from 9 to 28 min (mean 18 min) and no complications were reported.
Conclusion
Trans-nasal balloon-assisted dacryoplasty is a mini-invasive surgical approach to treat failed dacryocystorhinostomies with reliable and stable outcomes in the long term. The absence of post-surgical complications, high success rate and short operative time are the main features of this innovative procedure.
Keywords: Dacryocystorhinostomy, Ballooning, Balloon dacryoplasty, Nasolacrimal duct obstruction, Revision surgery
Introduction
Distal acquired lacrimal obstruction (DALO) is a common pathology that affects the lacrimal drainage system distal to Rosenmuller’s valve and its main clinical presentation is represented by epiphora or recurrent dacryocystitis [1]. The main etiology for this entity is believed to be idiopathic, also known as primary acquired nasolacrimal duct obstruction (PANDO), even if other causes have been described [2–9].
While in the past decades the approach of choice has been considered external dacryocystorhinostomy (EXT-DCR) [10], a recent review has highlighted that, among all treatments available, endoscopic endonasal dacryocystorhinostomy (END-DCR), similar to EXT-DCR, is associated with higher functional success rates compared to other approaches; accordingly, both can be considered the gold standard techniques for DALO [11, 12]. Nevertheless, it is generally acknowledged that END-DCR provides advantages over EXT-DCR, such as less operative time, morbidity, post-operative complications, and absence of external scar, which, however, frequently presents optimal esthetic outcomes [13–15].
Overall, END-DCR and EXT-DCR have a surgical failure rate of 10% that can be distinguished as early failure, mainly caused by inadequate surgery, or late failure, which can have multifactorial causes. In particular, the most common reasons for unsuccessful DCRs are excessive cicatricial ostium closure or granulation tissue formation, inadequate osteotomy/sac opening, internal ostium stenosis, common canalicular obstruction and sump syndrome [16]. Excluding the last two reasons, which require specific ophthalmological management, the others determine intranasal ostium stenosis which is mainly treated either with an endoscopic or external approach [17]. However, even if no significant difference has been noted, over the past few years, the END-DCR has gained popularity among clinicians for revision surgeries because, using endoscopic instrumentation, it provides a direct identification of the cause for the surgical failure and permits its rectification [18]. In addition, several endoscopic mini-invasive approaches have been proposed, with particular attention to balloon-assisted endoscopic dacryoplasty (balloon END-DCP), which is a high-pressure balloon catheter system introduced through the nose and used to restore the lacrimal pathway in revision cases of distal acquired obstruction [19]. In fact, although a trans-canalicular balloon-assisted approach has been previously described, its potential damage to the canalicular system has limited its application in favor of endoscopic approaches [20].
The aim of this study is to analyze the long-term outcomes of our series of patients who underwent balloon-assisted endoscopic dacryoplasty as revision surgery for recurrence of distal acquired lacrimal obstruction (Table 1).
Table 1.
Characteristics of the 14 patients included in the study
| Patient characteristics | Total (%) |
|---|---|
| Age | |
| ≥ 60 y | 8 (57) |
| < 60 y | 6 (43) |
| Gender | |
| Male | 1 (7) |
| Female | 13 (93) |
| Affected eye | |
| Left | 7 (50) |
| Right | 7 (50) |
| Previous surgery | |
| EXT-DCR | 4 (29) |
| END-DCR | 10 (71) |
| Time between 1st and 2nd surgery (months) | |
| < 12 | 7 (50) |
| ≥ 12–24 < | 4 (29) |
| ≥ 24 | 3 (21) |
Methods
In this analysis, we included patients who underwent, at the Department of Otolaryngology of San Raffaele Hospital in Milan (Italy), between December 2016 and October 2020, endonasal endoscopic balloon dacryoplasty (balloon END-DCP) after a failed EXT-DCR or END-DCR.
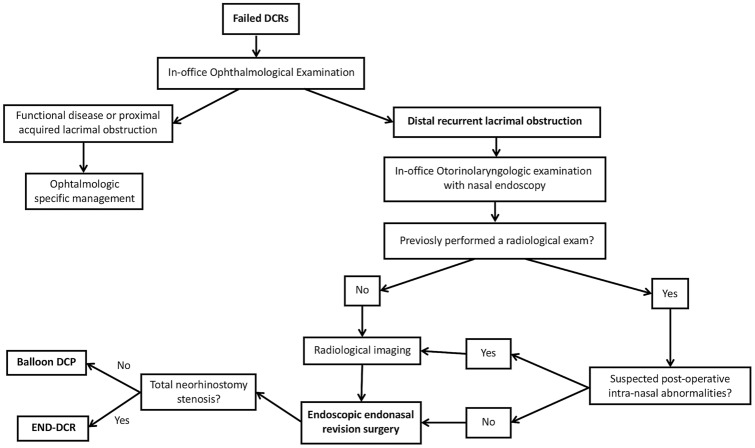
All patients presented recurrent epiphora due to distal acquired lacrimal obstruction after a primary DCR (both END or EXT) and received a diagnosis on the site of obstruction made by multidisciplinary agreement between an otolaryngologist and ophthalmologist. In particular, the diagnostic work-up for failed dacryocystorhinostomy (Fig. 1) is initially based on ophthalmologic examination that differentiates canalicular disease or pump failure, which is treated accordingly by an ophthalmologist, to distal recurrent obstruction. In fact, when a neorhinostomy closure is detected, in-office otorhinolaryngologic examination with 30 ° rigid nasal endoscopes is mandatory to directly visualize the nasal cavities and to better define the potential cause of the surgical failure. Pre-operative radiological imaging, particularly maxilla-facial CT scan, was not always requested since in our END-DCR series, we always performed it before the primary approach to treat any possible nasal comorbidity during the primary surgery [21]. However, in case of suspected novel nasal pathologies or absence of radiological examination, particularly after an EXT-DCR for which it is not always requested, a pre-operative radiological imaging (MRI or CT) was performed to detect and treat any endonasal pathology that could have influenced the final outcome. When complete examination of the nasal-lacrimal condition was achieved, two different surgical techniques were proposed, standard END-DCR or endonasal endoscopic balloon-assisted dacryoplasty, depending on the endonasal characteristics. In particular, the applicability of balloon END-DCP has been standardized in patients with internal ostium stenosis with a tiny neorhinostomy highlighted on high-pressure lacrimal irrigation and visualized on nasal endoscopy; additionally, the procedure was proposed if no adjunctive endonasal procedures were needed.
Fig. 1.
Diagnostic work-up for failed DCRs. DCR: dacryocystorhinostomy; END-DCR: endoscopic endonasal dacryocystorhinostomy; CT: computed tomography
All primary surgeries of the patients were treated for idiopathic distal obstruction, also known as primary acquired nasolacrimal duct obstruction (PANDO).
Exclusion criteria included other causes of NLDO such as malignancy, bone disease, previous radiotherapy, Down’s syndrome, sarcoidosis and granulomatosis with polyangiitis (GPA).
Informed consent was obtained from each patient for treatment and use of de-identified clinical data for study purposes. We obtained approval from the institutional review board (IRB) of San Raffaele Hospital for this clinical review study, which was conducted according to the ethical standards established in the 1964 Declaration of Helsinki, as revised in 2000.
Surgical technique
All procedures were performed by the same two surgeons, one ophthalmologist and one otolaryngologist (M.T. and G.R.A), under general anesthesia following our previous description of this surgical approach. Nasal cavities were treated with local oxymetazoline hydrochloride-soaked gauze; subsequently, the inferior lacrimal punctum was dilated by the ophthalmologist with a Bowman’s lacrimal probe that was inserted into the canalicular system down the stenotic lacrimal ostium. The tip of this probe was used as a surgical guide to allow direct endonasal endoscopic visualization of the stenotic point. Using an endoscopic endonasal approach, an 8 mm balloon catheter was gently introduced into the closed nasal neorhinostomy created during the primary DCR. Subsequently, the catheter, connected to an inflation device, determines enlargement of the rhinostomy using a balloon system which was inflated to 12 atm (1.216 × 106 Pa) for 3 cycles of at least 20 s each (Fig. 2).
Fig. 2.
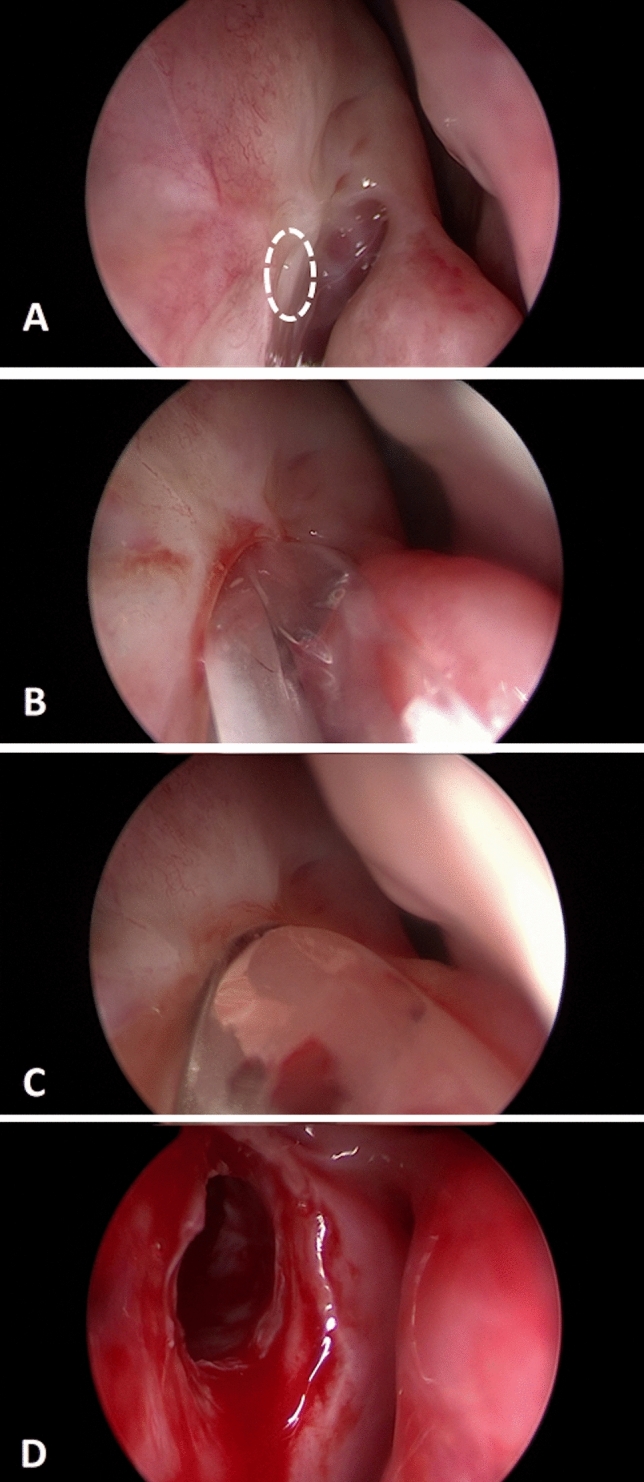
Endoscopic endonasal balloon-DCP: A Stenotic neorhinostomy (dashed white circle); B Trans-nasal introduction of the balloon catheter into the stenotic neorhinostomy; C Complete inflation of the catheter; D Enlarged neorhinostomy
No nasal packing was placed post-operative, although bicanalicular silicone stenting was placed in selected cases (2/14) of primary post-operative extensive fibrosis. All cases were prescribed oral antibiotics (amoxicillin + clavulanate), antibiotic-steroid eye drops for 7 days, periodic nasal washes, and use of local emollient ointment. Follow-up visits were done on days 1 and 7, once a week for the first month, and then once a month for 3 months and every 6 months for 1 year, similar to our previous data on END-DCR [14].
All post-surgical clinical visits consisted of a nasal endoscopy and lacrimal pathway irrigation (Figs. 3 and 4). Anatomical success was defined if a patent ostium on irrigation was achieved, whereas functional success was defined as absence of tearing symptoms (less than Munk 1) [22] and free lacrimal flow on functional test.
Fig. 3.
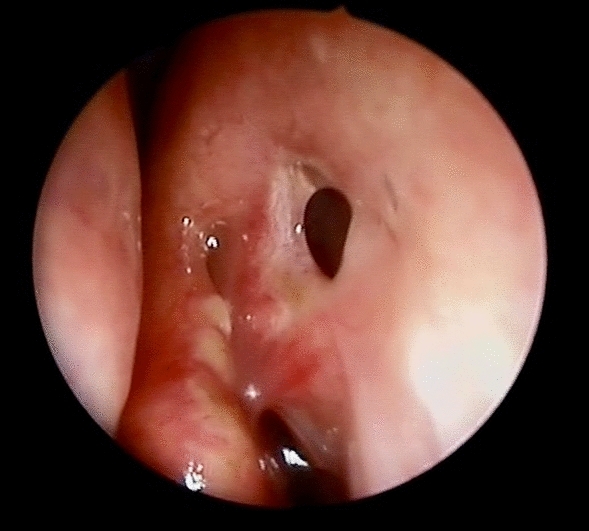
Post-surgical follow-up: 28th post-operative day in patient A
Fig. 4.
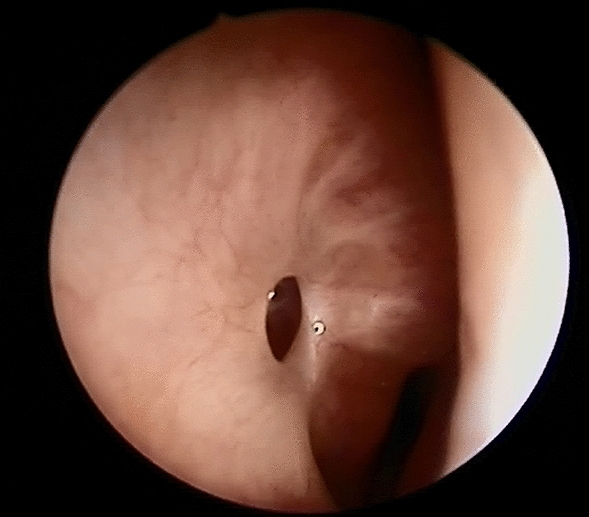
Long-term post-operative follow-up: 12 months after surgery in patient B
Results
A total of 14 patients (13 females and 1 male) underwent 14 balloon dilatations for recurrence of epiphora after a failed EXT-DCR or END-DCR, 50% were left neorhinostomy closures and 50% right closures (Table 1). Considering all the revision END-DCRs performed in our institution between December 2016 and October 2020, 41% (14/34) were treated with the balloon dilation, whereas 59% were treated in a standard endoscopic approach due to total neorhinostomy closure and excessive fibrosis, previous radiotherapy, and concomitant sarcoidosis or granulomatosis with polyangiitis.
In the included patients of this paper, several causes of primary surgical failure were detected, which included development of sinonasal synechiae close to the neorhinostomy (9/14), formation of foreign body granuloma (3/14), and fibrosis formation (2/14). All patients treated did not report any antecedent or concomitant episodes of acute dacryocystitis. Mean age was 58.4 years (range 38–75 years) and the main comorbidities were hypertension (n = 4), glaucoma (n = 1), chronic kidney disease (n = 1), and aortic valve stenosis (n = 1). In four patients (29%), a primary EXT-DCR was performed, while the remaining ten patients (71%) underwent primary END-DCR. The mean duration between primary and secondary surgical approach ranged from 3 to 48 months (mean 15.7 months), whereas the mean time to symptomatologic relapse was 6.5 months. All procedures were unilateral with a mean surgical duration of 18 min (9–28 min); the mean follow-up length was 19.5 months (range 13–51 months).
At last follow-up, anatomic success rate was obtained in 100% of cases, whereas functional success was achieved in 85.7% (12/14 patients). Among failed cases, recurrences were encountered within the first month and, to date, due to COVID-19 pandemic, no other treatment has been proposed. No significant complications such as bleeding, infection or bone necrosis were noted.
Discussion
END-DCR and EXT-DCR have recently gained the role of treatments of choice, as primary approaches, for DALO since they provide reliable and stable outcomes over the years [11]. Conversely, little is known about the best management for recurrent cases, which represent approximately 10% of treated patients.
To the best of our knowledge, this work represents one of the first studies analyzing long-term outcomes of balloon END-DCP and proposes a reproducible decision-making work-up for patients affected with recurrent distal acquired lacrimal obstruction after END-DCR or EXT-DCR (Fig. 1).
Revision surgeries for distal lacrimal obstruction is challenging for the oculoplastic and otorhinolaryngologic surgeon since several factors may concur and, not uncommonly, multiple causes for failure may be noted [16, 23]. In the last century, different approaches have been proposed, but external and endoscopic dacryocystorhinostomies still remain the treatments of choice; nevertheless, recent studies highlighted several advantages in revision cases of endoscopic approaches over the external one, rendering endonasal surgery more popular [18, 24, 25]. In fact, apart from the avoidance of a cutaneous scar and preservation of the orbicularis muscle, the endoscopic approach allows direct access to the stenotic lacrimal tract. This improves the possibility to address the specific cause of DCR failure and treat any concurrent pathologies which EXT-DCR may not allow [26]. As a result, more encouraging END-DCR outcomes have been reported compared to traditional external approach in revision surgeries [27, 28].
In recent years, a balloon-assisted dacryoplasty approach has been described for revision cases and represents a valid mini-invasive procedure in which a pneumatic force (the balloon catheter) determines an enlargement of the stenotic tract with no bone exposure and, consequently, less fibrosis or granulation tissue [29, 30]. This innovative technical approach was first delivered through a trans-canalicular manner [31]. However, on one hand, this could cause potential canalicular damage due to manipulation of the proximal lacrimal drainage system [20], while on the other does not usually provide reliable outcomes compared to standard techniques [32]. As a result, an endoscopic endonasal balloon-assisted dacryoplasty has been described in few patients and applied either to revisions or primary cases, with encouraging outcomes: in fact, in this way the mini-invasive technique has been merged with direct visualization of the stenotic tract through endoscopic visualization and treatment [32, 33].
Our results demonstrate that, after mean follow-up of 19.5 months and no adverse events, balloon-END-DCP provides reliable and stable outcomes with anatomical success of 100% and functional success of 85.7%, which is slightly decreased compared to our preliminary results at 6.4 months [19]. In fact, as demonstrated by Allon et al., a mean follow-up of 18 months is required to define the result as being stable for revision surgeries, since late neorhinostomy closure can occur [34]. Compared to our previous work, the present data represent the longest follow-up described for balloon END-DCP, with a functional success rate comparable to or even better than the long-term results of END-DCR revision cases. In particular, our previously reported revision END-DCRs with a powered approach has demonstrated, among 96 patients, a functional success rate of 85.1% at mean follow-up of 38 months [14], whereas Ali et al. [27] described 23 cases of revision END-DCR with a mean follow-up of 26.4 months reporting an anatomical and functional success rates of 91.3% and 86.9%, respectively, both data in line with our END-DCP results. Conversely, another revision END-DCR case-series made by Allon et al. [17] presented lower success, with yearly rates, from immediate to 5 years, of 93.3%, 75.5%, 71.1%, 68.9%, 68.9%, and 68.9%, respectively. Even if dichotomous compared to the work of Ali et al., the difference noted with the latter study can be explained by the less invasiveness and bone exposure of balloon END-DCP compared to standard END-DCR, which is also demonstrated by the reduced surgical time and the possibility to perform the balloon-END-DCP in local anesthesia [19]. Another reason for the lower surgical successes of Allon et al. can be explained by the long follow-up period and larger cohort size.
Nevertheless, it is noteworthy that the mini-invasive balloon END-DCP can be applied in a highly selected patients with subtotal internal ostium stenosis through which the balloon catheter can be placed and dilated in the lacrimal pathway; in fact, if a total neorhinostomy closure is detected, END-DCR should be considered the treatment of choice. However, one of the major drawbacks of this balloon device is the high equipment cost (140–170 euros for a powered approach vs 500–1200 euros for the balloon device), which could influence its applicability in lower-income countries.
Due to the limited number of publications on balloon END-DCP, comparison of our data with other similar studies is difficult. In fact, only Silbert et al. reported a success rate of 92% in 97 patients who underwent balloon END-DCP that, however, were treated as primary surgeries; in only 3 cases, it was subsequently applied as a revision technique, with success in only 1 of 3 patients. However, the difference of the technical primary surgery (END-DCR/EXT-DCR vs balloon END-DCP) makes these results incomparable.
Finally, considering post-surgical therapy, different possibilities have been discussed in the literature, both for post-operative medical therapy and bicanalicular stenting. Nevertheless, with the current data available regarding END-DCR, no difference is noted regarding either lacrimal stenting [34–36] or medical therapies (e.g., mitomycin C, oral antibiotics (ABT), nasal steroids or ocular steroids) [37–40]. As a result, in our series, we do not apply mitomycin C, but we do prescribe post-operative oral ABT and antibiotic-steroid eye drops; bicanalicular stenting was placed in only selected patients (2/14) in which extensive fibrosis was noted as failure of the primary surgical approach.
The present study has some limitations: first, the retrospective design and the small number of patients involved are the main limitations of this study; second, the feasibility of balloon END-DCP depends on the dimension of the previous neorhinostomy so that complete stenosis makes the procedure more difficult to perform. As a result, the described outcomes could be hypothetically influenced by the selection bias of patients with favorable stenosis of the neorhinostomy.
Conclusion
Considering revision surgeries after END-DCR and EXT-DCR, balloon END-DCP is a mini-invasive procedure with reliable and stable outcomes in long-term that can be considered an option in patients with internal ostium stenosis. The reduced operatory time and absence of post-operative complications are the main advantages of this approach over revision DCRs. Future prospective studies are needed to compare balloon END-DCP to other surgical approaches in the management of recurrent distal lacrimal obstruction.
Author contributions
AV and PI made substantial contributions to conception, design and acquisition of data, drafted the article and revised it critically for important intellectual content, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved; MT, AGR and MB made substantial contributions to conception of the data, revised it critically for important intellectual content, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data availability
Upon reasonable request.
Declarations
Conflict of interest
None of the authors have any conflict of interest.
Ethical approval
Approval was obtained from the ethics committee of the institutional review board (IRB) of San Raffaele Hospital for this clinical review study (April 2019), which was conducted according to the ethical standards established in the 1964 Declaration of Helsinki, as revised in 2000.
Consent to participate and for publication
Informed consent was obtained from each patient for treatment and use of de-identified clinical data for study purposes.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Alessandro Vinciguerra and Matteo Trimarchi equally contributed as first author.
References
- 1.Ali MJ, Paulsen F. Etiopathogenesis of primary acquired nasolacrimal duct obstruction: what we know and what we need to know. Ophthalmic Plast Reconstr Surg. 2019 doi: 10.1097/IOP.0000000000001310. [DOI] [PubMed] [Google Scholar]
- 2.Ali MJ. Iodine-131 therapy and nasolacrimal duct obstructions: what we know and what we need to know. Ophthalmic Plast Reconstr Surg. 2016;32(4):243–248. doi: 10.1097/IOP.0000000000000647. [DOI] [PubMed] [Google Scholar]
- 3.Morassi ML, Trimarchi M, Nicolai P, et al. Cocaina, ANCA e granulomatosi di Wegener. Pathologica. 2001;93(5):581–583. [PubMed] [Google Scholar]
- 4.Woog JJ. The incidence of symptomatic acquired lacrimal outflow obstruction among residents of Olmsted County, Minnesota, 1976–2000 (an American Ophthalmological Society thesis) Trans Am Ophthalmol Soc. 2007;105:649–666. [PMC free article] [PubMed] [Google Scholar]
- 5.Krishna Y, Coupland SE. Lacrimal Sac Tumors—a review. Asia Pac J Ophthalmol. 2017;6(2):173–178. doi: 10.22608/APO.201713. [DOI] [PubMed] [Google Scholar]
- 6.Ramberg I, Toft PB, Heegaard S. Carcinomas of the lacrimal drainage system. Surv Ophthalmol. 2020;65(6):691–707. doi: 10.1016/j.survophthal.2020.04.001. [DOI] [PubMed] [Google Scholar]
- 7.Vinciguerra A, Rampi A, Giordano Resti A, Barbieri D, Bussi M, Trimarchi M. Melanoma of the lacrimal drainage system: a systematic review. Head Neck. 2021 doi: 10.1002/hed.26705. [DOI] [PubMed] [Google Scholar]
- 8.Trimarchi M, Bondi S, Della Torre E, Terreni MR, Bussi M. Palate perforation differentiates cocaine-induced midline destructive lesions from granulomatosis with polyangiitis La perforazione del palato differenzia le lesioni destruenti della linea mediana indotte da cocaina dalla granulomatosi con poliangioite. ACTA Otorhinolaryngol Ital. 2017;37:281–285. doi: 10.14639/0392-100X-1586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Resti AG, Bertazzoni G, Trimarchi M. Nasolacrimal duct obstruction secondary to dental impaction. Eur J Ophthalmol. 2013;24(4):611–613. doi: 10.5301/ejo.5000410. [DOI] [PubMed] [Google Scholar]
- 10.Sobel RK, Aakalu VK, Wladis EJ, Bilyk JR, Yen MT, Mawn LA. A comparison of endonasal dacryocystorhinostomy and external dacryocystorhinostomy: a report by the American Academy of Ophthalmology. Ophthalmology. 2019 doi: 10.1016/j.ophtha.2019.06.009. [DOI] [PubMed] [Google Scholar]
- 11.Vinciguerra A, Nonis A, Giordano Resti A, Bussi M, Trimarchi M. Best treatments available for distal acquired lacrimal obstruction: a systematic review and meta-analysis. Clin Otolaryngol. 2020;45(4):545–557. doi: 10.1111/coa.13551. [DOI] [PubMed] [Google Scholar]
- 12.Vinciguerra A, Nonis A, Resti AG, Barbieri D, Bussi M, Trimarchi M. Influence of surgical techniques on endoscopic dacryocystorhinostomy: a systematic review and meta-analysis. Otolaryngol Head Neck Surg. 2020 doi: 10.1177/0194599820972677. [DOI] [PubMed] [Google Scholar]
- 13.Sharma V, Martin PA, Benger R, et al. Evaluation of the cosmetic significance of external dacryocystorhinostomy scars. Am J Ophthalmol. 2005;140(3):359.e1–359.e7. doi: 10.1016/j.ajo.2005.11.061. [DOI] [PubMed] [Google Scholar]
- 14.Trimarchi M, Giordano Resti A, Vinciguerra A, Dane G, Bussi M. Dacryocystorhinostomy: Evolution of endoscopic techniques after 498 cases. Eur J Ophthalmol. 2019 doi: 10.1177/1120672119854582. [DOI] [PubMed] [Google Scholar]
- 15.Huang J, Malek J, Chin D, et al. Systematic review and meta-analysis on outcomes for endoscopic versus external dacryocystorhinostomy. Orbit. 2014;33(2):81–90. doi: 10.3109/01676830.2013.842253. [DOI] [PubMed] [Google Scholar]
- 16.Hull S, Lalchan SA, Olver JM. Success rates in powered endonasal revision surgery for failed dacryocystorhinostomy in a tertiary referral center. Ophthalmic Plast Reconstr Surg. 2013;29:267–271. doi: 10.1097/IOP.0b013e3182916556. [DOI] [PubMed] [Google Scholar]
- 17.Allon R, Cohen O, Bavnik Y, Milstein A, Halperin D, Warman M. Long-term outcomes for revision endoscopic dacryocystorhinostomy—the effect of the primary approach. Laryngoscope. 2020 doi: 10.1002/lary.28795. [DOI] [PubMed] [Google Scholar]
- 18.Nair AG, Singh S, Kamal S, Ali MJ. The importance of endoscopy in lacrimal surgery. Expert Rev Ophthalmol. 2018;13(5):257–265. doi: 10.1080/17469899.2018.1520635. [DOI] [Google Scholar]
- 19.Indelicato P, Vinciguerra A, Giordano Resti A, Bussi M, Trimarchi M. Endoscopic endonasal balloon-dacryoplasty in failed dacryocystorhinostomy. Eur J Ophthalmol. 2020 doi: 10.1177/1120672120942692. [DOI] [PubMed] [Google Scholar]
- 20.Mishra AK, Nilakantan A, Mishra S, Mallick A. Comparison of balloon dacryocystorhinostomy with conventional endonasal endoscopic dacryocystorhinostomy for relief of acquired distal nasolacrimal drainage obstruction and its impact on quality of life: a prospective, randomized, controlled study. Med J Armed Forces India. 2018;74(3):255–263. doi: 10.1016/j.mjafi.2017.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Trimarchi M, Giordano Resti A, Bellini C, Forti M, Bussi M. Anastomosis of nasal mucosal and lacrimal sac flaps in endoscopic dacryocystorhinostomy. Eur Arch Otorhinolaryngol. 2009;266(11):1747–1752. doi: 10.1007/s00405-009-1002-z. [DOI] [PubMed] [Google Scholar]
- 22.Munk PL, Lin DT, Morris DC. Epiphora: treatment by means of dacryocystoplasty with balloon dilation of the nasolacrimal drainage apparatus. Radiology. 1990;177:687–690. doi: 10.1148/radiology.177.3.2243969. [DOI] [PubMed] [Google Scholar]
- 23.Welham RAN, Wulc AE. Management of unsuccessful lacrimal surgery. Br J Ophthalmol. 1987;71(2):152–157. doi: 10.1136/bjo.71.2.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yarmohammadi ME, Ghasemi H, Jafari F, Izadi P, Nadoushan MJ, Chin NS. Teamwork endoscopic endonasal surgery in failed external dacryocystorhinostomy. J Ophthalmic Vis Res. 2016;11(3):282–286. doi: 10.4103/2008-322X.188396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.AltinEkin M, KaradenizUgurlu S, Aytogan H, SahinAtik S. Failure in revision dacryocystorhinostomy: a study of surgical technique and etiology. J Craniofac Surg. 2020;31(1):193–196. doi: 10.1097/SCS.0000000000005829. [DOI] [PubMed] [Google Scholar]
- 26.Orcutt JC, Hillel A, Weymuller EA. Endoscopic repair of failed dacryocystorhinostomy. Ophthal Plast Reconstr Surg. 1990;6(3):197–202. doi: 10.1097/00002341-199009000-00009. [DOI] [PubMed] [Google Scholar]
- 27.Ali MJ, Psaltis AJ, Wormald PJ. Long-term outcomes in revision powered endoscopic dacryocystorhinostomy. Int Forum Allergy Rhinol. 2014;4(12):1016–1019. doi: 10.1002/alr.21398. [DOI] [PubMed] [Google Scholar]
- 28.Lehmann AE, Scangas GA, Jafari A, Banks CG, Fullerton ZH, Metson R. Predictors of long-term success and failure in primary and revision endoscopic dacryocystorhinostomy. Int Forum Allergy Rhinol. 2020;10(3):374–380. doi: 10.1002/alr.22483. [DOI] [PubMed] [Google Scholar]
- 29.Janssen AG, Mansour K, Krabbe GJ, Van Der Veen S, Helder AH. Dacryocystoplasty: Treatment of epiphora by means of balloon dilation of the obstructed nasolacrimal duct system. Radiology. 1994;193(2):453–456. doi: 10.1148/radiology.193.2.7972762. [DOI] [PubMed] [Google Scholar]
- 30.Indelicato P, Vinciguerra A, Giordano Resti A, Trimarchi M. A case of endonasal balloon-assisted dacryoplasty after failure of endonasal dacryocystorhinostomy. Clin Case Reports. 2020;8(9):1605–1609. doi: 10.1002/ccr3.2956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ali MJ, Naik MN, Honavar SG. Balloon dacryoplasty: ushering the new and routine era in minimally invasive lacrimal surgeries. Int Ophthalmol. 2013;33(2):203–210. doi: 10.1007/s10792-012-9652-z. [DOI] [PubMed] [Google Scholar]
- 32.Lee BJ, Nelson CC, Lewis CD, Perry JD. External dacryocystorhinostomy outcomes in sarcoidosis patients. Ophthal Plast Reconstr Surg. 2012;28(1):47–49. doi: 10.1097/IOP.0b013e3182364ad2. [DOI] [PubMed] [Google Scholar]
- 33.Silbert DI, Matta NS. Outcomes of 9mm balloon-assisted endoscopic dacryocystorhinostomy: Retrospective review of 97 cases. Orbit. 2010;29(3):131–135. doi: 10.3109/01676830.2010.480924. [DOI] [PubMed] [Google Scholar]
- 34.Kim DH, Kim SI, Jin HJ, Kim S, Hwang SH. The clinical efficacy of silicone stents for endoscopic dacryocystorhinostomy: a meta-analysis. Clin Exp Otorhinolaryngol. 2018;11(3):151–157. doi: 10.21053/ceo.2017.01781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kang MG, Shim WS, Shin DK, Kim JY, Lee JE, Jung HJ. A systematic review of benefit of silicone intubation in endoscopic dacryocystorhinostomy. Clin Exp Otorhinolaryngol. 2018;11(2):81–88. doi: 10.21053/ceo.2018.00031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ing EB, Bedi H, Hussain A, et al. Meta-analysis of randomized controlled trials in dacryocystorhinostomy with and without silicone intubation. Can J Ophthalmol. 2018;53(5):466–470. doi: 10.1016/j.jcjo.2017.12.006. [DOI] [PubMed] [Google Scholar]
- 37.Sousa TTS, Schellini SA, Meneghim RLFS, Cataneo AJM. Intra-operative mitomycin-C as adjuvant therapy in external and endonasal dacryocystorhinostomy: systematic review and meta-analysis. Ophthalmol Ther. 2020;9(2):305–319. doi: 10.1007/s40123-020-00253-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nair AG, Ali MJ. Mitomycin-C in dacryocystorhinostomy: From experimentation to implementation and the road ahead: a review. Indian J Ophthalmol. 2015;63(4):335–339. doi: 10.4103/0301-4738.158082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Phelps PO, Abariga SA, Cowling BJ, Selva D, Marcet MM. Antimetabolites as an adjunct to dacryocystorhinostomy for nasolacrimal duct obstruction. Cochrane Database Syst Rev. 2020 doi: 10.1002/14651858.CD012309.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vinciguerra A, Nonis A, Resti AG, Bussi M, Trimarchi M. Impact of post-surgical therapies on endoscopic and external dacryocystorhinostomy: systematic review and meta-analysis. Am J Rhinol Allergy. 2020;34(6):846–856. doi: 10.1177/1945892420945218. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Upon reasonable request.