Abstract
Background Context:
When different health care providers use different patient-reported outcome (PRO) instruments, it is challenging to integrate findings that describe particular patient groups or to establish treatment effectiveness across studies. It is therefore critical to develop accurate ways to convert scores between various instruments for clinicians and researchers to make comparisons across health outcomes.
Purpose:
To develop a common metric so that scores on the Oswestry Disability Index (ODI) and scores on the PROMIS Physical Function can be converted interchangeably.
Study Design/Setting:
Data were collected from a prospective study. A single-group linking design was used.
Patient Sample:
The study population included 9020 patients presented to an orthopedic spine clinic from November 2013 to March 2019.
Outcome Measures:
Patients completed the ODI and the PROMIS Pain Interference scale delivered by Computerized Adaptive Testing (CAT) at the same time prior to their visit with a spine clinician.
Methods:
Equipercentile linking methods based on log-linear smoothing approach and non-smoothing approach were used to establish a common metric across the two measures.
Results:
The two measures assess the similar construct of pain. The correlation between the scores of the ODI and the PROMIS PI was .81. The standardized Root Expected Mean Square Difference (REMSD) values for gender, ethnic, and racial groups ranged from 3.55% to 4.81%. Hence, the assumptions for the equipercentile linking method were met. The crosswalk derived linked scores based on the log-linear smoothing method yielded small deviations (Δ = 0.09) from the observed scores. We then identified linked PROMIS-PI scores corresponding to the benchmark ODI scores for the five disability levels and for various categories of patients.
Conclusions:
This study is the first to create crosswalks to interchangeably convert scores between the ODI to the PROMIS-PI in a large population of spine patients using the equipercentile linking method. The results of this study provide confidence in the validity and usefulness of the derived crosswalks based on the equipercentile linking approach. The crosswalks are helpful for comparing new and old studies on the two measures and identifying benchmark scores for various diseases and disability levels.
Keywords: PROMIS, Oswestry Disability Index, equipercentile linking, scale linking, patient-reported outcomes, crosswalk tables
INTRODUCTION
Clinicians and researchers use patient-reported outcome (PRO) instruments to gather reliable and valid information on patient experience and perspectives regarding their health.1 In orthopedic practice, several PRO instruments have been developed to understand patient disability, pain, and treatment response.2 When different health care providers use different PRO instruments, it is challenging to directly harmonize data that describe particular patient groups or to establish treatment effectiveness across studies. It is therefore critical to develop accurate ways to convert scores between various instruments to aid a cooperative research activity in which clinicians and researchers can aggregate existing data across cohorts and projects and expand measurement coverage.
A methodology known as “scale alignment” or “linking” is a comprehensive tool to facilitate the harmonization of data across studies by converting scores across instruments.3 Linking methods may be based on item response theory (IRT), equipercentile linking with different smoothing approaches, and prediction based on regression. A few researchers in orthopedics have applied these techniques to link instruments such as physical function and pain.4–7
The Oswestry Disability Index (ODI) is a widely used spine-specific PRO instrument in orthopedics to assess disability related to back pain and functional improvement from treatment.8 The Patient Reported Outcomes Measurement Information System® (PROMIS®) is a standard set of outcome measures in health care supported by the National Institutes of Health (NIH) beginning in 2004.9 PROMIS is a PRO system of instruments that measure domains of overall well-being, such as physical, mental, and social health across many diseases.10,11 The computerized adaptive testing (CAT) option of PROMIS contributes to high levels of accuracy with reduced patient burden and efficiency of its usage in clinical practice by tailoring relevant questions to each patient and reaching adequate accuracy with a shorter test length.10,11
Compared to the ODI, the PROMIS CAT has better coverage of the full range of pain and function, while taking less time to administer and having less associated patient burden.12,13 One of the most relevant PROMIS domains to the ODI and the spine patients is the Pain Interference domain. Most patients visit the clinic complaining of pain due to spine problems, and previous studies found strong correlation between the ODI and PROMIS-Pain Interference (PROMIS-PI),13–15 indicating the two scales may capture similar constructs. Given the widespread usage of the ODI and the efficiency of PROMIS, and the conversion at many centers to preferentially collect PROMIS CATs due to reduced patient burden, there is value in linking scores of the two measures and creating a score conversion table. It would help the clinical and research community to increase flexibility in data collection by allowing either measure to be used, compare spine patient outcomes in centers that have historically captured scores of one measure and have recently converted to the other measure and, importantly, facilitate accurate comparison of results across studies that have used either ODI or PROMIS to describe spine patient population outcomes. The purpose of the present study is to create a common metric (i.e., crosswalks) for conversion of scores between the ODI and the PROMIS-PI for an orthopedic spine care population.
METHODS
Data Collection
This study was approved by an University Institutional Review Board. The ODI and PROMIS-PI were administrated via iPad tablets to consecutive patients presenting for spine care at the University Orthopedic Center prospectively from November 2013 to March 2019. Prior to their visit with a spine clinician, patients completed demographic questions, the ODI and the PROMIS-PI as a part of the standard clinical care protocol. Nearly 99% of the patients completed the questionnaires with the rest of the patients refused to complete the questionnaires as part of the standard care. The patient sample possessed a wide range of spinal disorders including vertebral fractures, neck pain, spondylitis, kyphosis, spinal stenosis, spina bifida, and back pain.
Description of Instruments
The ODI has 10 patient-completed questions in which the response options are presented as 6-point Likert scales. Scores range from 0% (no disability) to 100% (most severe disability). We followed the ODI scoring manual that if one section/item is missed (or not applicable) for a patient, this item will be excluded from the total score. The PROMIS-PI v1.1 CAT has a 40-item bank with individually validated and calibrated items regarding how pain interferes with daily activities. Its CAT administration selects the next item based on patients’ responses to previous items. Item response theory (IRT) is used to score each patient’s responses and estimate scale scores. The scale scores are standardized in T scores (Mean = 50; standard deviation [SD] = 10) based on a general population.10,11 Lower scores on the PROMIS-PI are indicative of less pain interference. In this study, the PROMIS-PI T scores were rounded to the nearest integer in order to match the increment of the ODI score for the calculation of percentile ranks.
Analytical Approach
We applied the equipercentile method to link the scale scores of the two measures for patients who experienced back pain and visited a university clinic at least once. Appendix 1a shows the frequency of visit numbers for the patients involved in this study. As the number of visits are unbalanced within the sample, we decided to randomly choose one visit for each participant to form the analytical sample. The distribution of time points selected in analysis can be found in Appendix 1a. We further analyzed and confirmed that the crosswalk linking results were consistent across time points, which allowed us to randomly pool time points for each patient.
The equipercentile approach aligns total scores or scale scores of the two measures with the same percentile ranks to establish a nonlinear linking relationship.16 The prerequisite assumptions for the equipercentile linking are: the similar content of the two measures; a high correlation between the scores of the two measures; the population invariance across subgroups.
Using the equipercentile method to directly link scores may not be sufficiently precise because of sampling or measurement error inherited in score distributions of the two measures. In other words, the responses of some patients in the sample might not be representative of those of the target population so that their scores may not follow the score distribution of the target population. The existence of sampling or measurement error may lead to irregular and unsmoothed patterns on the score distribution. To minimize its impact, we needed to smooth the score distribution. In this study, we used the polynomial log-linear smoothing technique which is widely used to smooth score distributions,17,18 and compared its results with the non-smoothing approach, which directly links the two score distributions without smoothing. We then evaluated the linking effectiveness by comparing the linked scores computed by each method with observed scores in terms of Pearson product-moment correlations, the mean and standard deviation (SD) of the differences between scores. We also plotted both linked and observed scores to graphically illustrate their deviations at each score point.
RESULTS
The study population included 9020 patients with a mean age of 56.5, 51.6% female (Table 1). One hundred and fifty-six patients (1.7%) did not fully complete both measures, leaving 8864 patients as the final sample size for linking (Table 2). Fewer than 2.5% of patients received the highest or lowest possible ODI score and observed PROMIS-PI score. To test linking assumptions, we first inspected the contents of the two measures. The ODI mainly evaluates patients’ levels of back or leg pain, and the PROMIS-PI measures patients levels of pain. Both instruments focus on how much the pain levels may impact patients’ ability to manage in everyday living functions. Along with the strong correlation between the two measures, this supports the assumption that the two measures are assessing the similar health outcome. As shown in Figure 1, the ODI and PROMIS-PI scores are positively correlated, and the Spearman’s correlation proves the strong correlation (= 0.81). The standardized Root Expected Mean Square Difference (REMSD) was used to evaluate population invariance across subgroups. Linking experts recommended using values of less than 8% of SD to support subgroup invariance.19 In this study, the REMSD is 3.80% for gender groups (i.e., Male and Female); 4.81% for ethnic groups (i.e., Hispanic and not Hispanic); 3.55% for racial groups (i.e., Other and White or Caucasian). Based on all the above results, the assumptions for the equipercentile linking are met in this study.
Table 1.
Demographics
| Variables | Number |
|---|---|
| Sample Size | 9020 |
| Age at visit (mean +− SD, range) (yr) | 56.5 ± 16.8, 11.1-98.5 |
| Female (%) | 51.6% |
| Race(%) | |
| American Indian and Alaska Native | 0.8% |
| Asian | 1.2% |
| Black or African American | 1.1% |
| Native Hawaiian and Other Pacific Islander | 0.4% |
| Other | 5.8% |
| Patient Refused | 0.8% |
| Unknown | 0.03% |
| White or Caucasian | 89.7% |
| NA | 0.2% |
| Ethnicity | |
| Hispanic/ Latino | 6.3% |
| Not Hispanic/ Latino | 92.4% |
| Patient Opts Out | 1.0% |
| Unknown/ Information Not Available | 0.02% |
| NA | 0.3% |
Table 2.
Descriptive Statistics for the Two Measures for the Selected Sample
| ODI | PROMIS-PI | |
|---|---|---|
| Sample Size | 8864 | 8864 |
| Mean | 34.3 | 62.3 |
| Median | 32 | 63 |
| SD | 18.7 | 7.8 |
| Minimum | 0 | 39 |
| Maximum | 100 | 84 |
| Interquartile range | [20, 48] | [57, 67] |
Figure 1.
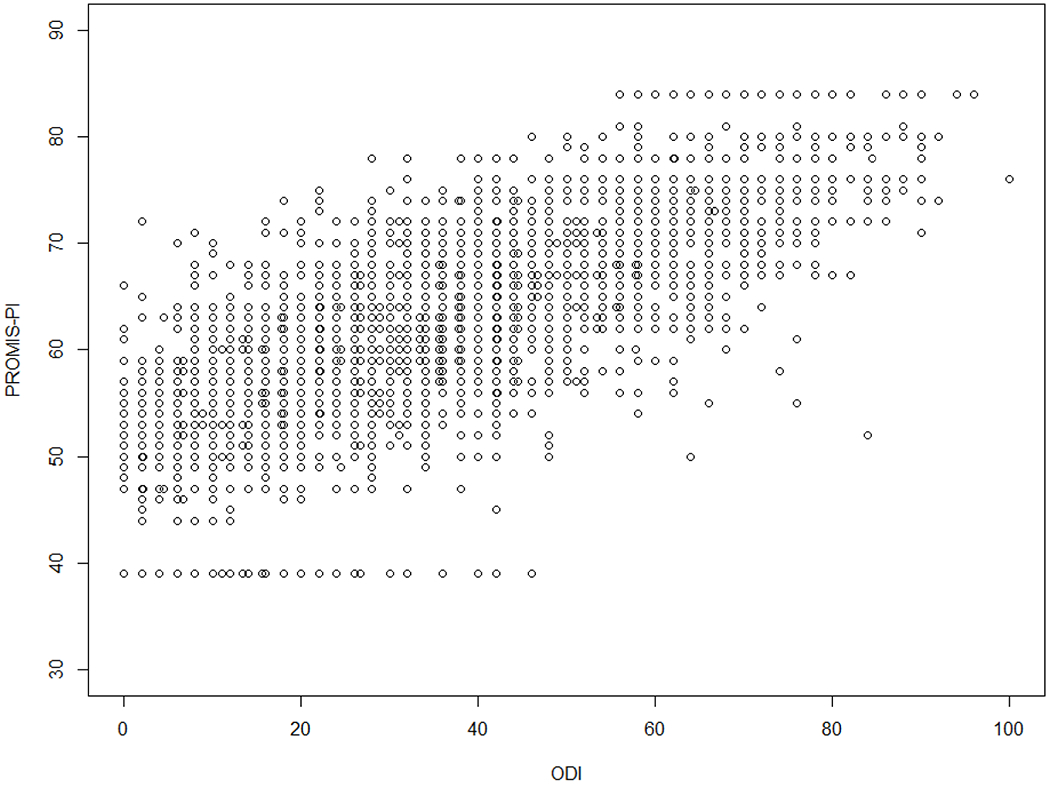
The scatterplot for the ODI and PROMIS-PI scores among the analytical sample
We examined score distributions of the two measures (Figure 2). Although both score distributions are generally normal, there are irregular patterns at some score points. To reduce the impact of these irregularities on the linking relationship, it is necessary to smooth their score distributions before linking them. To achieve this, we first fit polynomial functions to the log of the score distribution of each measure. Second, we followed linking experts’20 suggestions on the likelihood ratio chi-square test results for model comparison and the differences between the fitted and the raw distribution to select the appropriate polynomial degree of smoothing for each measure. We then linked the two smoothed score distributions based on the equipercentile linking procedure. For comparison, we also linked the two unsmoothed score distributions.
Figure 2.
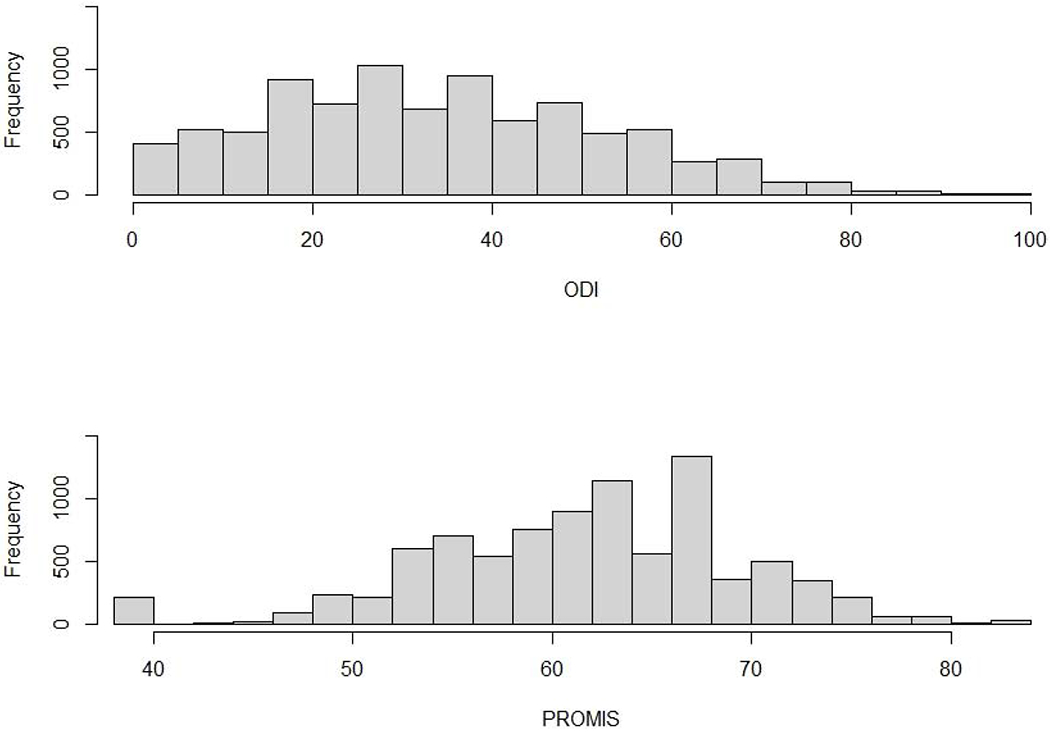
The score distributions of the ODI and PROMIS-PI among the analytical sample
The two linking function graphs (left panel in Figure 3) show a consistent trend, but the log-linear smoothing approach yields a smooth, less choppy function than the unsmoothed linking function. The smooth log-linear function helps to eliminate the impact of sampling or measurement error. With regard to the linking standard error (right panel in Figure 3), although the log-linear smoothed function had a relatively high standard error at a low score point, it yielded smaller standard error across the entire score range compared with the standard error of the unsmoothed linking function. The high standard error associated with the low score point is probably due to the small number of patients reporting very low scores.
Figure 3.
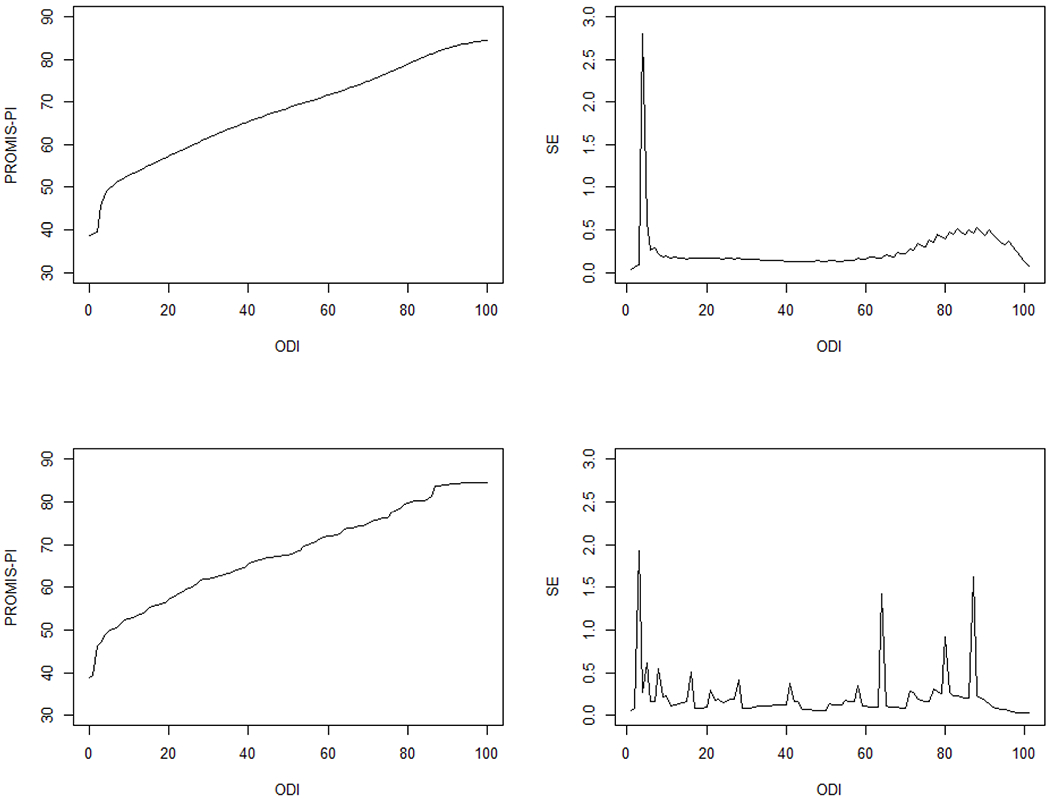
The linking functions and linking standard errors of the log-linear smoothing method (upper panel) and the non-smoothing method (bottom panel).
We found that the correlation, mean difference, and SD of difference between observed and crosswalk derived scores are very similar for the non-smoothing and smoothing methods (Table 3). The strong correlations indicate the consistency between the observed and linked scores. The small mean differences and similar SDs of difference also speak to the validity and effectiveness of the crosswalk tables. We also found adequate equivalence between the crosswalk-derived PROMIS-PI scores and the observed mean scores at each ODI score point (Figure 4), which further suggests the effectiveness of the crosswalks.
Table 3.
Comparison Between the Non-Smoothing and Log-Linear Smoothing Technique
| Method | Correlation | Mean Difference | SD |
|---|---|---|---|
| Log-linear Smoothing | 0.80 | 0.09 | 4.93 |
| Non-smoothing | 0.81 | −0.03 | 4.82 |
Figure 4.
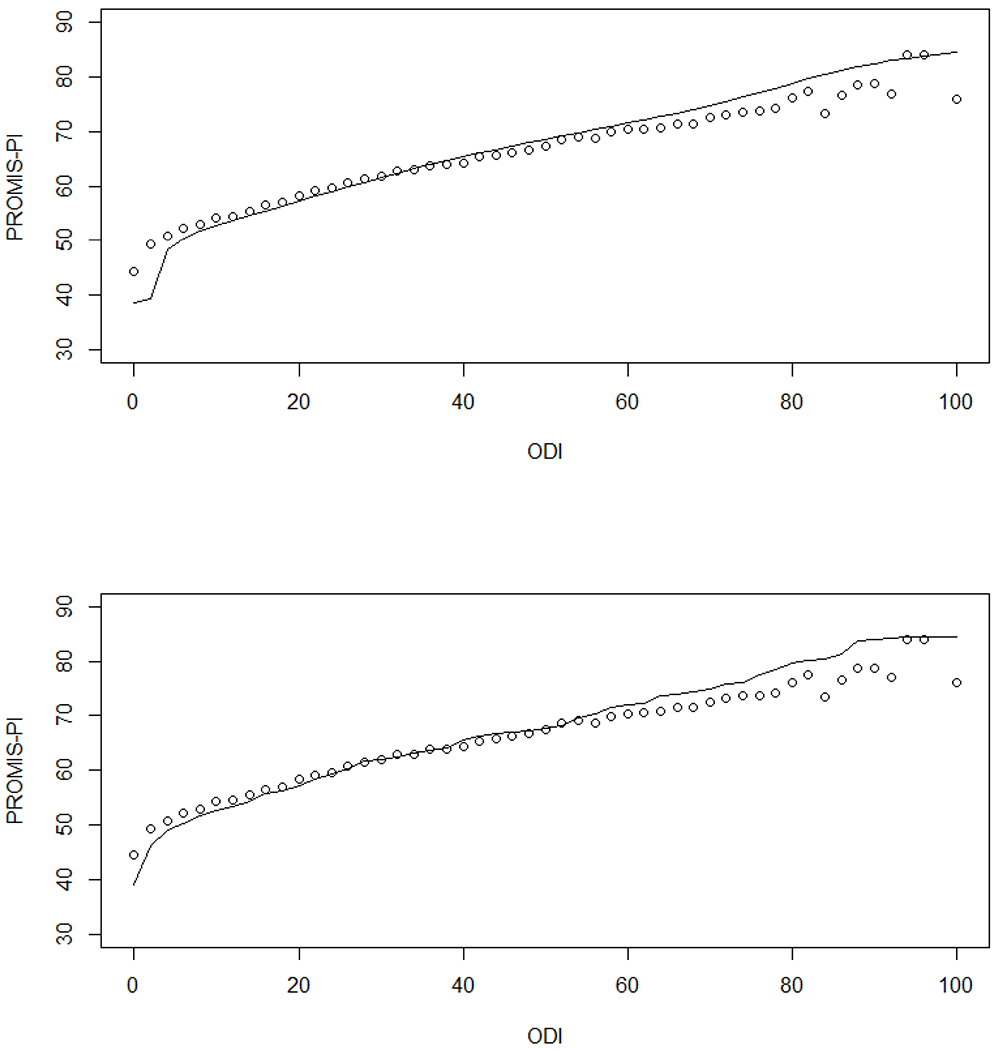
The difference between the actual mean PROMIS-PI scores and the crosswalk derived PROMIS-PI scores. Upper panel: the log-linear presmoothing approach; Bottom panel: the non-smoothing approach.
Note. The solid line represents the crosswalk derived PROMIS-PI scores, the dots represent the actual mean PROMIS-PI scores at each ODI score, and the distance between the solid line and each dot refer to the residuals.
Considering the small linking standard error and the small deviations of the linked scores from the observed scores, we created crosswalks based on the log-linear smoothing method. In addition to the ODI to PROMIS-PI crosswalk, we also created the PROMTS to ODI crosswalk. Both crosswalks are presented in Appendix 1b. The crosswalks allow us to interpret PROMIS-PI scores based on the benchmark ODI scores for the five disability levels8 proposed by the authors of the ODI as shown in Table 4. Moreover, another ODI cut-off score of 40%, which can be converted to a PROMIS-PI score of 65.4, is used to divide patients into having a low or high ODI score.21 Finally, we converted the weighted ODI mean scores for various categories of patients, which were calculated from pooled data for a systematic review of the ODI studies by Fairbank and Pynsent,8 to the PROMIS-PI scores (Table 5).
Table 4.
Disability Levels, the Corresponding ODI Scores and Linked PROMIS-PI Scores
| Category | ODI | Crosswalk Derived PROMIS-PI score |
|---|---|---|
| Minimal disability | 0-20 | 38.7-57.2 |
| Moderate disability | 21-40 | 57.7-65.4 |
| Severe disability | 41-60 | 65.7-71.5 |
| Crippled | 61-80 | 71.9-78.8 |
| Completely bedbound | 81-100 | 79.3-84.4 |
Note. The categories and the ODI scores were extracted from Fairbanks and Pynsent.1
Table 5.
The Weighted Mean ODI Scores of Various Spine Diseases and Their Linked PROMIS-PI Scores
| Category | Mean ODI Score | Crosswalk Derived PROMIS-PI Score |
|---|---|---|
| “Normal” population | 10.19 | 52.7 |
| Pelvic fractures | 13.26 | 54.1 |
| Idiopathic scoliosis | 13.81 | 54.6 |
| Neck pain | 21 | 57.7 |
| Spondylolisthesis | 26.63 | 60.3 |
| Primary back pain | 27 | 60.3 |
| Psychiatric patients | 30.8 | 62.0 |
| Neurogenic claudication | 36.65 | 64.3 |
| Chronic back pain | 43.3 | 66.4 |
| PID/Sciatica | 44.65 | 67.0 |
| Fibromyalgia | 44.83 | 67.0 |
| Metastases | 48.04 | 67.9 |
Note. The categories and the ODI scores were extracted from Fairbanks and Pynsent.1 The crosswalk derived PROMIS-PI scores were selected corresponding to the nearest ODI integer score. Linearity is assumed for this conversion of the means.
DISCUSSION
The ODI, a disease-specific measure, and PROMIS-PI, a generic health outcome measure, are both commonly used scales to assess levels of pain and function for spine patients and further evaluate orthopedic treatment. Due to the increasing usage of both measures and their similarities, it is beneficial to connect the two common measures and make their scores comparable. This study successfully linked the scores of the two measures and created crosswalks for the conversion of their scores. The crosswalks would help clinicians and researchers to identify an equivalent score between the two measures for spine patients. Moreover, as the ODI has been used longer than PROMIS-PI for spine patients, the crosswalks can be used to integrate PROMIS PI studies with previous ODI studies. Linking two measures is not meant to suggest the superiority of one measure over another but rather that they can be treated as interchangeable. The crosswalk table provides the interpretability of both measures on a common metric for further group-level analysis and the flexibility of using either measure. For example, researchers can use this crosswalk to compute clinically critical values of each measures based on the reference values of the other measure. For clinicians who want to harmonize existing data for a prospective data collection purpose and for an integrative data analysis, the crosswalks can provide scores for both measures with collecting data of only one measure.
The linking between the two scales met the conceptual and statistical assumptions for the linking analysis. Before linking the scores, we used the log-linear smoothing method with appropriately selected polynomial degree to smooth the two score distributions. Then we applied the equipercentile approach to link the smoothed and unsmoothed score distributions of the two measures, respectively. After comparing the two approaches through a series of statistical modeling, we decided to use the polynomial log-linear smoothing approach to create the bidirectional crosswalks (ODI to PROMIS vs PROMIS to ODI). The effectiveness of the crosswalks was supported by the consistency between the crosswalk derived and observed scores. According to previous studies on the psychometric properties of the ODI, it tends to have ceiling and floor effect, which may limit differentiation within patients at extremely high and low disability, respectively.22 However, in the current study sample, the ceiling (0.01%) and floor (1.86%) effect was small probably due to a very large sample size. Hence, the ODI had a better coverage of the extreme scores in this linking study.
This study also provides the corresponding PROMIS-PI scores for the benchmark ODI values of various disability levels and the mean ODI scores of various spine diseases. These linked PROMIS-PI scores would inform clinicians and researchers who use PROMIS-PI about the critical values from historical spine studies or clinical practices. Finally, this study has examined the consistency of linking relationships across multiple time points and included data of each time point into analysis. Hence, the crosswalks created from the linking function of this study have taken the longitudinal effect into account, providing sufficient justification for their usefulness.
Despite the strength and value of the present study to researchers and clinicians, there are some limitations. First, we did not use a nationally representative sample of the US population; all participants in this study were spine patients. But the ODI is mainly used to collect information from spine patients so it is reasonable to build the linking relationship between the two measures for this specific patient population. While there is some evidence that linking relationships for patient-reported pain interference replicate across different patient populations,23 we caution users against using these crosswalks for other patient groups. Second, the sample in this study is a mix of patients receiving various medical treatments in the spine clinic. Future research can be conducted to examine whether the treatment effect or the various spine disease levels may impact the linking relationship. Third, the data collection of this study is completed in a single center. It might be impacted by factors specific to the local area, diversity of patients and the community. However, as the analytical sample size of this study is very large (N = 8864), it should to some extent represent the spine patients in similar clinic practices. Fourth, although the effectiveness of the crosswalk table has been verified by the consistency of observed and crosswalk-derived T scores, a future study may use another sample to verify the external validity of this crosswalk table. Fifth, this study applied the commonly used polynomial log-linear smoothing method. Other smoothing methods (e.g., kernel equating method) can be further explored and used to conduct the equipercentile linking. Finally, to compute a conversion table or to verify the current crosswalk tables, a future study may use a proportion of the sample data to develop a model to predict the PROMIS PI scores based on the ODI scores and then use the remaining data to validate the model. Another similar and promising method is calibrated projection,24 which applies a two-dimensional IRT model to responses of the two measures and projects scores of one dimension to the other.
To our knowledge, this study is the first to create crosswalks for the conversion of scores between the ODI and the PROMIS-PI in a large population of spine patients. The results of this study provide confidence in the effectiveness and usefulness of the derived crosswalks based on the equipercentile linking method. The crosswalks are helpful for comparing new and old studies on the two measures and identifying benchmark scores for various diseases and disability levels for spine patients.
Supplementary Material
Acknowledgement:
This study was funded by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health under award number U01AR067138.
Abbreviations:
- CAT
Computerized Adaptive Testing
- IRT
Item response theory
- NIH
National Institutes of Health
- ODI
Oswestry Disability Index
- PI
Pain Interference
- PRO
Patient-Reported Outcome
- PROMIS
Patient-Reported Outcomes Measurement Information System
- REMSD
Root Expected Mean Square Difference
- SD
Standard Deviation
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest:
None.
Financial Disclosure:
None.
REFERENCES
- 1.Schalet BD, Kallen MA, Heinemann AW, Deutsch A, Cook KF, Foster L, et al. Using PROMTS Pain Interference Items to Improve Quality Measurement in Inpatient Rehabilitation Facilities. Journal of the American Medical Directors Association. 2018;19(10):846–851. e842. [DOI] [PubMed] [Google Scholar]
- 2.Yee TJ, Smith BW, Joseph JR, Saadeh YS, Nathan JK, Kahn EN, et al. Correlation between the Oswestry Disability Index and the 4-item short forms for physical function and pain interference from PROMIS. Journal of neurosurgery Spine. 2019;31(5):1. [DOI] [PubMed] [Google Scholar]
- 3.Dorans N Linking scores from multiple health outcome instruments. Quality of Life Research. 2007;16(Supplement 1):85–94. [DOI] [PubMed] [Google Scholar]
- 4.Brodke DS, Lawrence BD, Ryan Spiker W, Neese A, Hung M. Converting ODI or SF-36 Physical Function Domain Scores to a PROMIS PF Score. The Spine Journal. 2014;14(11):S50–S50. [Google Scholar]
- 5.van Den Heuvel M 744. Linking Macroscale Connectivity Disruptions with Microscale Measures of Spine Density and Gene Expression. Biological Psychiatry. 2017;81(10):S301–S302. [DOI] [PubMed] [Google Scholar]
- 6.Polascik BA, Hidaka C, Thompson MC, Tong-Ngork S, Wagner JL, Plummer O, et al. Crosswalks Between Knee and Hip Arthroplasty Short Forms: HOOS/KOOS JR and Oxford. Journal of bone and joint surgery American volume. 2020;102(11):983–990. [DOI] [PubMed] [Google Scholar]
- 7.Ghomrawi HMK, Lee Y-y, Herrero C, Joseph A, Padgett D, Westrich G, et al. A Crosswalk Between UCLA and Lower Extremity Activity Scales. Clinical Orthopaedics and Related Research. 2017;475(2):542–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine. 2000;25(22):2940. [DOI] [PubMed] [Google Scholar]
- 9.Pennings J, Devin C, Khan I, Bydon M, Asher A, Archer K. Prediction of Oswestry Disability Index (ODI) using PROMIS-29 in a national sample of lumbar spine surgery patients. Quality of Life Research. 2019;28(10):2839–2850. [DOI] [PubMed] [Google Scholar]
- 10.Cella D, Yount S, Rothrock N, Gershon R, Cook K, Reeve B, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS): Progress of an NIH Roadmap Cooperative Group during Its First Two Years. Medical Care. 2007;45(5):S3–S11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cella D, Riley W, Stone A, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. Journal of Clinical Epidemiology. 2010;63(11): 1179–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brodke DS, Goz V, Voss MW, Lawrence BD, Spiker WR, Hung M. PROMIS PF CAT Outperforms the ODI and SF-36 Physical Function Domain in Spine Patients. Spine. 2017;42(12):921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hung M, Saltzman CL, Voss MW, et al. Responsiveness of the Patient-Reported Outcomes Measurement Information System (PROMIS), Neck Disability Index (NDI) and Oswestry Disability Index (ODI) instruments in patients with spinal disorders. The Spine Journal. 2019;19(1):34–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bernstein DN, Greenstein AS, D’Amore T, Mesfin A. Do PROMIS Physical Function, Pain Interference, and Depression Correlate to the Oswestry Disability Index and Neck Disability Index in Spine Trauma Patients? Spine. 2020;45(11):764. [DOI] [PubMed] [Google Scholar]
- 15.Papuga M, Barnes A. Correlation of PROMIS CAT instruments with Oswestry Disability Index in chiropractic patients. Complementary Therapies in Clinical Practice. 2018;31:85. [DOI] [PubMed] [Google Scholar]
- 16.Kolen MJ, Brennan RL. Test Equating, Scaling, and Linking: Methods and Practices. Vol 27–28. 3rd ed. 2014 ed. New York, NY: 2014. [Google Scholar]
- 17.Holland P, Thayer D. Univariate and bivariate loglinear models for discrete test score distributions. Journal Of Educational And Behavioral Statistics. 2000;25(2): 133–183. [Google Scholar]
- 18.Wang T Standard Errors of Equating for the Percentile Rank–Based Equipercentile Equating With Log-Linear Presmoothing. Journal of Educational and Behavioral Statistics. 2009;34(1):7–23. [Google Scholar]
- 19.Dorans NJ, Holland PW. Population Invariance and the Equatability of Tests: Basic Theory and The Linear Case. Journal of Educational Measurement. 2000;37(4):281–306. [Google Scholar]
- 20.Kolen MJ. Smoothing Methods for Estimating Test Score Distributions. Journal of Educational Measurement. 1991;28(3):257–282. [Google Scholar]
- 21.Sanderson PL, Todd BD, Holt GR, Getty CJ. Compensation, work status, and disability in low back pain patients. Spine. 1995;20(5):554. [DOI] [PubMed] [Google Scholar]
- 22.Brodke DS, Goz V, Lawrence BD, Spiker WR, Neese A, Hung M. Oswestry Disability Index: a psychometric analysis with 1,610 patients. The spine journal. 2016;17(3):321–327. [DOI] [PubMed] [Google Scholar]
- 23.Cook KF, Schalet BD, Kallen MA, Rutsohn JP, Cella D. Establishing a common metric for self-reported pain: linking BPI Pain Interference and SF-36 Bodily Pain Subscale scores to the PROMIS Pain Interference metric. Qual Life Res. 2015;24(10):2305–2318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Thissen D, Varni JW, Stucky BD, Liu Y, Irwin DE, Dewalt DA. Using the PedsQL™ 3.0 asthma module to obtain scores comparable with those of the PROMIS pediatric asthma impact scale (PAIS). Quality of life research. 2011;20(9):1497–1505. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


