Abstract
Background:
Understanding the factors that influence hospital mobility, especially in the context of a heightened focus on falls prevention, is needed to improve care.
Objective:
This qualitative study uses a socioecological framework to explore factors that influence hospital mobility in older adults.
Design:
Qualitative Research
Participants:
Semi-structured interviews and focus groups were conducted with medically-ill hospitalized older adults (n=19) and providers (hospitalists, nurses, and physical and occupational therapists (n=48) at 2 hospitals associated with an academic health system.
Approach:
Interview and focus group guides included questions on perceived need for mobility, communication about mobility, hospital mobility culture, and awareness of patients’ walking activity. Data were analyzed thematically and mapped onto the constructs of the socioecological model.
Key Results:
A consistent theme among patients and providers was that “mobility is medicine”. Categories of factors reported to influence hospital walking activity included intrapersonal factors (patients’ health status, fear of falls), interpersonal factors (patient-provider communication about mobility), organizational factors (clarity about provider roles and responsibilities, knowledge of safe patient handling, reliance on physical therapy for mobility), and environmental factors (falls as a never event, patient geographical locations on hospital units). Several of these factors were identified as potentially modifiable targets for intervention. Patients and providers offered recommendations for improving awareness of patient’s ambulatory activity, assigning roles and responsibility for mobility, and enhancing education and communication between patients and providers across disciplines.
Conclusion:
Patients and providers identified salient factors for future early mobility initiatives targeting hospitalized older adults. Consideration of these factors across all stages of intervention development and implementation will enhance impact and sustainability.
Keywords: Hospital, mobility, older adults, interdisciplinary health professions, qualitative
INTRODUCTION
Low mobility is common in the hospital and associated with poor health outcomes.1–8 On average, older adult patients walk fewer than 1200 steps per day and spend over 90% of their hospitalization lying in bed.1,9,10 Increasing the time spent walking during hospitalization has been shown to reduce the risk of death, hospital acquired disability, and the need for post-acute care.5,9,11–13 However, studies over time show persistent low mobility among medically-ill hospitalized patients.1,9,10
Some have suggested that efforts to improve hospital mobility have been set back by Centers for Medicare and Medicaid Services designation of falls as a “never event” in 2008, which stopped hospital payment for injuries related to inpatient falls. Subsequent studies have identified unintended consequences of this policy, including a decrease in hospital mobility, increase in use of physical restraints, and a tendency to focus on measures such as new prevention devices (e.g., bed alarms).14,15 However, there are little data regarding provider perceptions about this designation or how it may have changed their attitudes or behavior around hospital mobility.
In addition to provider and patient perspectives, hospital mobility may depend on many factors, such as patient symptoms, hospital layout, lack of staffing, and tethers.16 We chose the socioecological model (SEM) as our foundational approach to understanding how these various factors impact walking behavior. The SEM is appropriate in this context because it suggests that behavior is a product of multiple influences, namely intrapersonal, interpersonal, organizational, environmental, and policy, all of which impact mobility.17 Using the SEM as a framework, this qualitative study reports on the perspectives of both patients and hospital providers, including physical and occupational therapists who are integral to mobility safety training and evaluation in hospitals, regarding: (1) factors that influence hospital mobility in older adults, and (2) how these factors can inform the design or implementation of hospital walking or mobility programs.
METHODS
Participants
Between March 2018 and May 2018, we recruited a purposive sample of General Medicine patients at an academic tertiary medical center and academic community hospital. Inclusion criteria were community-dwelling older adults aged 60 years or older, able to ambulate with or without assistance of another person or walking aid, and cognitively able to follow instructions (defined as a score of 4 or higher on the Six-Item Screener).18 We included patients who were between hospital days two and seven at the time of screening, a time frame in which most patients would have had an opportunity for walking activity. We attempted to enroll patients with a variety of admission diagnoses and potential mobility constraints (e.g. foley catheters, IVs, sequential compression devices), exposure to physical therapy (PT) and occupational therapy (OT), and baseline need for assistive mobility devices. We aimed to follow the principle of purposive sampling to increase our information power by identifying and selecting cases to document diverse variations in perspectives within a targeted sample.19,20 Patients on respiratory isolation precautions were excluded because of expected limited ambulatory activity outside of their rooms.
We also recruited a purposive sample of hospital providers (physicians, advanced practice providers, nurses, physical therapists, and occupational therapists) from the General Medicine service of the same hospitals from March 2018 to May 2018. We sampled across various levels of professional experience, including medical resident trainees, based on years in practice.
In-depth Interviews
We conducted 1:1 semi-structured interviews with patients and hospitalist physicians. The interview guides were informed by expert opinion and the literature. The included interview guides are part of a larger effort to examine hospital mobility and tracking of walking activity, and we are reporting on the portion that included questions for patients on their experiences with getting up and moving while in the hospital, and for providers on opinions and practices related to mobility (Supplemental Table 1).
Focus groups
In addition to individual in-depth interviews with hospitalists, four focus groups were conducted to facilitate participation by scheduling at mutually convenient times (one with residents, one with nurses, and two with PTs and OTs from each of the academic and community hospitals), and were led by an expert facilitator, and conducted with a range of seven to eleven participants per group. Group composition consisted of the same health professionals to facilitate greater willingness to communicate.21
The number of interviews and focus groups conducted was based on thematic saturation, defined when no new relevant information was obtained from new participants.22 All interviews and focus groups were audio recorded and transcribed verbatim. This research was approved by the Duke University School of Medicine Institutional Review Board.
Patient-reported measures of falls, walking, and physical activity to assess baseline activity
Patients self-reported on falls over the past 3 months, use of assistive devices, and needing help walking up the stairs, ¼ mile, and across a small room. Participants reported on walking indices at two time points: two weeks prior to admission (retrospective, collected with baseline), and at baseline. Patient-reported physical activity at home was measured using the International Physical Activity Questionnaire,23 and scores were categorized into low activity, moderate activity, and high activity.
Data Analysis
We analyzed transcripts of patients and provider interviews together using a framework analysis (familiarization; identifying a thematic framework; indexing; charting and mapping; and interpretation).24 Familiarization involved the authors’ (JP and LF) review of three patient and provider transcripts to become familiar with the data and to identify initial coding themes. We used a deductive approach to identify themes for the initial coding framework based on a Donabedian framework, which is particularly suited to healthcare research as it categorizes quality of care into three categories (structure, process, and outcomes).25
The first and second authors (JP, LF) conducted line-by-line coding of a single transcript and met to discuss the transcript and modify the initial Donabedian coding framework. Inductive codes included category for patient and provider attitudes, beliefs, and behaviors that affect mobility. Next, the first and second authors conducted line-by-line coding of remaining transcripts using NVivo12. This allowed for detection of deviant cases, coding errors, and examination of coding reliability. Coding included memos for each transcript to annotate coders questions, decisions about the data, and reflections on the coding process. Rigor was also maintained through audit trail, member checking with hospitalists and PT/OTs, and peer review with regular team meetings. After coding was completed, the team met to discuss themes, and sort codes. In the final stage, the team identified major themes and associated quotes to summarize the results. We used the SEM model, well-suited for understanding the importance of dynamic interrelations between a person and his/her environment on hospital mobility, to organize the major themes identified by patients and providers on the intrapersonal, interpersonal, cultural/organizational, and environmental/policy levels.17
RESULTS
We screened 366 patients; 96 patients were eligible to participate, and 32 patients were approached. For feasibility purposes, we approached patients consecutively until we reached our enrollment goal of two to three interviews per day. A total of 19 older hospitalized patients were interviewed before we reached theme saturation (Table 1).
Table 1.
Patient Characteristics (N=19)
| MEAN (SD) OR N (%) | |
|---|---|
| Age | 77 (7.6) |
| Gender, female | 13 (68%) |
| Race, white | 10 (52%) |
| Primary reason for admission | |
| Cardiac | 1 (5%) |
| Pulmonary | 1 (5%) |
| Gastrointestinal | 4 (21%) |
| Infectious | 4 (21%) |
| Weakness/falls | 4 (21%) |
| Other | 5 (26%) |
| Mobility constraints (yes) | |
| Foley catheters | 2 (13%) |
| Intravenous lines | 8 (50%) |
| Sequential compression devices | 13 (81%) |
| Oxygen | 3 (19%) |
| Contact precautions | 1 (5%) |
| Falls risk label (yes) | 11 (58%) |
| Falls precaution order (yes) | 5 (26%) |
| Walk across a room (yes) | 12 (63%) |
| If no, able to 2 weeks ago?; n= 7 | 4 (57%) |
| Fallen in past 3 months (yes) | 8 (42%) |
| Use assistive device (yes) | 11 (56%) |
| Cane (n=11) | 8 (73%) |
| Walker (n=11) | 7 (64%) |
| Rollator (n=11) | 0 (0%) |
| Current function | |
| Help walking up stairs (no) | 8 (42%) |
| Help walking ¼ mile (no) | 5 (26%) |
| Help walking across room (no) | 13 (68%) |
| 2 weeks ago function | |
| Help walking up stairs (no) | 11 (58%) |
| Help walking ¼ mile (no) | 5 (26%) |
| Help walking across room (no) | 13 (68%) |
| No help walking (current/2weeks) | 5 (26%) |
| International physical activity questionnaire score | |
| Low activity | 16 (84%) |
| Moderate activity | 3 (16%) |
| High activity | 0 (0%) |
A total of 48 providers were interviewed. We conducted 10 semi-structured interviews with hospitalists, and 4 focus groups (medical residents only (n=7), nurses (n=9)/certified nursing assistants (n=2) only, and 2 groups with PTs and OTs only (n=9 and n=11, respectively) (Table 2). Of 48 provider respondents, 8 respondents had roles in supervising other staff, or setting institutional policies.
Table 2.
Provider Characteristics (N=48)
| MEAN (SD) OR N (%) | |
|---|---|
| Age | 37.0 (10.1) |
| Gender, female | 40 (83%) |
| Race, white | 30 (63%) |
| Clinical service | |
| Hospitalists | 10 (21%) |
| Nurses/Certified nursing assistants | 11 (23%) |
| Medical Residents | 7 (15%) |
| PT and OT | 20 (42%) |
| Clinical years of service (median, (IQR)) | |
| Hospitalists | 7 years (5-10), range 1-15 years |
| Nurses | 2.5 years (1.5-25.5), range 0.3 – 40 years |
| PT and OT | 13.5 years (2-19.5), range 1-32 years |
PT and OT = Physical Therapy and Occupational Therapy
IQR= Interquartile range
A consistent theme among patients and providers was that “mobility is medicine”, a phrase that came directly from the voice of participants when discussing their belief that mobility is a treatment that patients can receive to improve their health. The majority of patient and provider themes mapped to the Donabedian process category. However, we used the SEM framework to organize and describe the results to better understand how the person-environment interrelationship influences mobility. The Donabedian factors of structure and process typically mapped to the SEM domains of organizational and interpersonal factors, respectively. Overall nine themes were identified at multiple levels of the SEM; three at the intrapersonal level (patient health status, fear of falls, motivating factors), one at the interpersonal level (communication), three at the organizational/cultural level (roles and responsibility, moving safely, available time and resources) and two at the environmental level (falls as a never event, patient geographic locations) (Figure 1).
Figure 1.
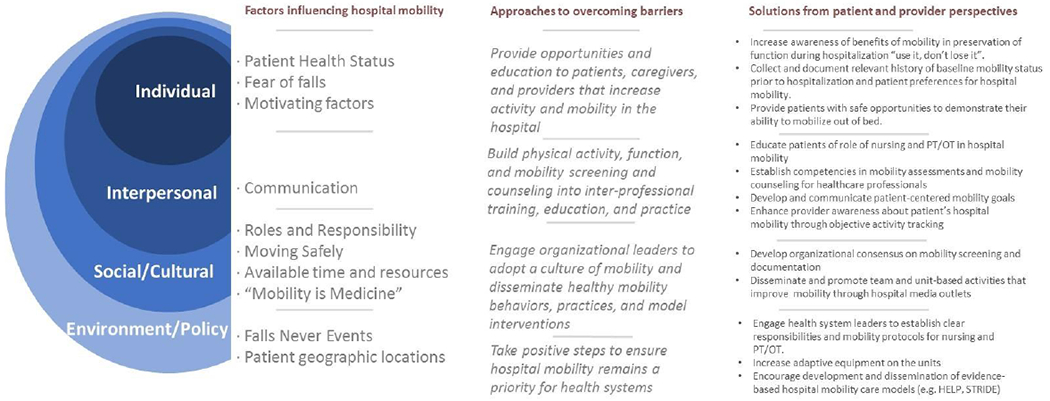
Socio-Ecological Model based themes, approaches, and solutions for understanding and improving hospital mobility
Patient perspectives on factors that influence mobility
The first SEM level identifies the biological and personal history factors that influence knowledge and behaviors, in this case related to hospital mobility. At this intrapersonal level, many patients reported that their current health condition was a significant barrier to mobility in the hospital (Table 3). Most patients perceived that they were not allowed to move without a nurse or someone to help them because of clear instructions or bed alarms. Some patients were concerned about falling and thus were not motivated to get up out of bed (Table 3). Other patients, such as those who felt they were able to move freely reported negative feelings due to loss of autonomy (Table 3).
Table 3.
Patient and Provider Perspectives on Factors that Influence Mobility
| Themes | Quotes |
|---|---|
| PATIENTS | |
| Intrapersonal | |
| Patient Health Status | “Well I think they didn’t have me mobile because of my heart and my lungs. They’ve had me on monitors.” |
| Fear of falls | “But my leg been giving out on me because sometimes I can walk and sometimes I can’t. If I were walking it’d just give out. …it made me sit in a chair. I was scared.” |
| Losing autonomy | “When I’m getting ready to go to bed and I’ve got to go to the bathroom and then I got to pick up the phone and call and have somebody come to hold my hand when I go to the bathroom. …Yes, it’s irritating and plus the fact you won’t ever be able to say you can do it yourself if they keep taking it away from you and because they’re afraid they’re going to have somebody injured”. |
| Interpersonal | |
| Communication |
“Yes, they say I should you know walk around the nurse’s station or something like that, yes… they encourage me to, the doctor. It helps me. It helps me to get up and walk…The physical therapists, the nurses, the doctors; all of them.” “Well they haven’t talked to me too much about moving around since I been in here.” |
| Organizational | |
| Moving safely | “I could walk more but they don’t want me to go by myself yet. Because they’re afraid I might fall.” “They were overly cautious but that’s because we’re in the hospital.” |
| PROVIDERS | |
| Intrapersonal | |
| Patient Health Status | “Some patients, you know, all that they could do prior to coming in was to get out of bed to a chair. Well that’s the benchmark, that’s what they need to do while they’re here in the hospital. For patients that are independent ambulators, they need to be independently ambulating.” [Hospitalist] |
| Interpersonal | |
| Communication |
“I think that has a lot to do with doctors a lot of times, just randomly ordering consults and not really looking at our assessment because you go like PT is coming to see them like for what? They’re walking around the hallways.” [Nurse] “We can make recommendations, but really we would have usually been consulted right when they first came in or if they were up mobilizing with nursing they might not have had that decline to begin with and we wouldn’t have been needed.” [PT and OT] “I think a lot of my fellow hospitalists will say the same thing. That’s the biggest thing they look for in PT notes is the discharge recommendation. So I don’t even know if they do put ambulation time in that PT note because it’s too long to go through.” [Hospitalist] |
| Organizational | |
| Roles and Responsibility |
“I think that there, in all honesty, is a general hesitation because we have such a high falls risk population that a lot of times especially maybe less experienced nurses will want to wait until there’s been a PT consult to kind of verify what’s the best way to move this person and that person may not even be on the agenda for a PT consult so then they sit in the bed these two or three days” [Nurse] “Physical therapy is used to doing this, that’s who should be doing this because I have other things to do besides try to figure out a plan of why somebody’s not being as mobile and stuff.” [Nurse] “We are lacking both human resources, physical resources, we may know that someone needs to use a walker, but we can’t get a walker unless PT brings it to the room”. [Nurse] |
| Environmental | |
| Falls Never Event | “We still think that even the fall risk patients should get out of bed to a chair but I think even with that, when they get that falls risk thing put on we become less confident that we can encourage safe mobility. I think then, we tend to rely more on physical therapists” [Hospitalist] |
| Patient Geographic Location | “It’s just a culture commitment as buy in from like the nursing, the patients, the physicians, physical therapists that are on the unit and they have like, this goal towards mobility…they’re committed to it and it’s worked.” [Resident]. |
The second SEM level, interpersonal, examines how relationships influence mobility behaviors. From the patient’s perspective, advice and the assistance to get up and walk was inconsistent and confusing. Several patients reported that doctors, nurses, PTs and OTs recommended that they get up or sit at the bedside and move (Table 3). However, patients who had lower functional status due to long-term or short-term health conditions reported that they had not been up or could not recall being asked about getting out of bed (Table 3). For some patients, doctors recommended that they get up and walk, but were also told they were not allowed to walk by nursing staff.
The organizational SEM levels examine cultural factors that help create a climate for hospital mobility. Patients and caregivers understood that the hospital staff was concerned about their safety (Table 3). Having equipment such as walkers and assistance from staff helped patients feel safe when moving around. Some patients perceived that walking with family members was discouraged because they did not have adequate training to ensure patient safety.
Provider perspectives on factors that influence mobility
Hospitalists, nurses, physical therapists, and occupational therapists interviewed all reported that the hospital culture emphasizes falls prevention ahead of mobility in older patients.
At the intrapersonal level, hospitalists reported that patient health condition was a significant barrier to mobility. When patients felt sick, tired, and in pain, they did not want to get up and move. Hospitalists, in concordance with PTs and OTs, also discussed the importance of assessing patients’ mobility prior to hospitalization to set a realistic expectation for mobility while in the hospital and at discharge (Table 3).
Communication among providers through the electronic health record (EHR) was reported to be a challenging interpersonal barrier to mobility. Nurses noted that other providers are not reading their documented assessments of mobility to help identify early the patients needing mobility support (Table 3). PTs and OTs reported experiencing delays in orders for consult, which prevented them from effectively triaging patients to prevent or mitigate deconditioning in at-risk patients (Table 3). PT and OT notes in the EHR were described by hospitalists, residents, and nurses as lengthy and complex, which made it difficult for doctors and nurses to access and understand the pertinent information efficiently. Physicians also acknowledged typically only reviewing the PT and OT notes for discharge recommendations and instructions (Table 3).
Although both patients and providers reported a belief that “mobility is medicine”, at the organizational level there was a general sense of helplessness regarding solutions to the problem. Lack of clarity regarding roles and responsibilities was described as a significant barrier to mobility for hospitalized older patients. Hospitalists and nurses considered PT as having the primary responsibility for hospital mobility (Table 3). Nurses and nurse assistants reported that whereas they want to walk their patients they either lack time because it is not part of their workflow, or lack the necessary equipment because PT and OT have to evaluate the patient first before they can get the mobility equipment in the room (Table 3). PT and OT observed that nurses could have greater role in patient mobility, but that there is a general lack of knowledge on the part of nursing staff regarding best practices for safe mobility. Nurses also reported that they feel PT and OT should be responsible for mobility, because they are specifically trained for that role (Table 3). Finally, there was a general sense among PTs and OTs that nurses and doctors do not have a clear understanding of the PT and OT role regarding patient mobility. PT and OT perceive they are viewed as the “walking team” or “discharge recommendation team”, however, they describe that their role is to perform screening and assessments, and provide recommendations for treatment. There was the sense among PT and OT that limited resources are not being used efficiently. For example, patients who are able to walk independently were referred to PT and/or OT, which takes time away from patients who are at greater risk of deconditioning.
In an environment where fall prevention is a priority, all providers, and particularly nurses, acknowledged that in many instances, risk reduction is prioritized over mobility. Providers across the various disciplines reported the belief that the focus on falls prevention created a cultural reliance on PT and OT to walk patients in the hospital (Table 3). Another environmental factor that influenced mobility was the physical distribution of patients. Medical Residents reported that the value of mobility in treatment is central to the culture on some services such as orthopedics and pulmonary in which patients are clustered together on a single unit (Table 3). However, PT and OT reported that general medicine patients are geographically distributed throughout the hospital, and mobility may not be a priority on all services.
DISCUSSION
There are key studies in the literature over the past 5 years that elucidate factors that influence mobility in hospitalized older adults.16,26, 27 They include nursing perceived lack of training and time to mobilize patients, poor patient-provider communication about mobility, perception that rehabilitation therapists should have primary role in mobilizing patients, challenges in defining mobility tasks, and focus on falls prevention. Our findings corroborate with this published evidence and we uniquely apply the SEM framework to explore the factors that influence hospital mobility in the falls as a “never event” era and to make recommendations for overcoming process and system-level barriers (Figure 1). Here we discuss application of this framework to organize reported factors influencing mobility and implications for designing or implementing hospital walking or mobility programs.
There was consensus among patients and providers that mobility during hospitalization is important, and both groups used the term “use it or lose it” to express this sentiment. In our sample over half the patients reported being able to walk across the room without needing help prior to hospitalization, and patients feeling able to move expressed frustration and dissatisfaction about the lack of opportunities to walk during their hospital stays. Hospitalists, PT, and OT wanted better collection and documentation of relevant history of baseline mobility status prior to hospitalization and patient preferences for hospital mobility. These recommendations align with the strategies endorsed by the Quality and Performance Measurement Committee (QPMC) of the American Geriatrics Society (AGS) and the Institute for Healthcare Initiatives Age Friendly Health System to use standard, validated mobility assessments and screening upon admission.28,29
When designing and implementing a mobility program, training of nursing staff to determine the appropriate patient handling and mobility equipment or device needed to safely move or mobilize the patient should be a key component. In general nurses in our study expressed desire for increased training in safe mobility.30 Nurse-driven mobility interventions, where nurses conduct assessments and nursing assistants perform ambulation can be successful in limiting functional decline and reducing length of stay.31 PTs and OTs also expressed a desire to see nursing have a more prominent role and increased responsibility for walking patients, a recommendation that is also supported by the QPMC and AGS.28 PT and OT have been the pillar of most walking activity in the hospital, leading to reflexive consultation of PTs, overuse and delays in appropriate care. Given that it is not standard of practice, PTs and OTs expressed frustration at the widespread misconception that they have to “clear” patients before they can safely move out of bed, often leading to inappropriate timing of consults. Only about 50% of older adults are seen by PTs and OTs within the first three days of hospitalization.32 Further, nurses, PTs and OTs can carry high patients loads (average PT and OT load of 8 patients per day in our hospitals). With those constraints, in health systems that employ an opt-in approach for PT and OT rehabilitation consults, it is imperative to focus on inter-disciplinary coordination as part of a mobility program to address challenging interpersonal factors related to the roles and responsibilities of mobility safety.
Physical and occupational therapy are a limited resource in many hospitals that is not being used efficiently. Especially for functionally independent patients, it is critical to make organizational changes that will use a team or system-based approach for appropriate assessments and to support safe mobility.33 Special consideration should be made to enhance EHR-embedded screening tools and EHR documentation of mobility to standardize data elements into easily extractable fields that can be used for development of triaging reports or chart analysis.33–36 Additionally, both hospitalists and nurses expressed a lack of awareness of how much their patients were moving in the hospital, partly because there is limited walking data early during hospitalization to appropriately inform providers of a patient’s mobility needs.28 One possible way to enhance provider awareness is through use of mobile health technology, such as physical activity monitors, to objectively measure and report patient mobility data (e.g., step counts, time out of bed) to providers.37
Patients in our sample expressed that an institutional focus on falls prevention was a major barrier to achieving a culture of “mobility is medicine”. Our study uniquely added perspectives from PTs and OTs, which were particularly enlightening about roles, responsibilities, and recommendations for enhanced multi-disciplinary mobility safety training. Since the CMS designation of falls as a “never event”, our organization has developed an increasing reliance PT and OT consultations resulting in staffing pressures. Further, nurses perceive an “unwritten rule” requiring clearance from PTs and OTs prior to safely mobilizing patients. One possible solution to overcome this imposing environmental barrier is broad dissemination of evidence-based walking programs such as STRIDE, HELP, MOVE ON, and Walk FOR, which have been linked to reduced discharges to skilled nursing facilities, delirium, length of stay, and hospital-acquired disability.11,38–40 Importantly, these programs incorporate rehabilitation assistants, certified nursing assistants or volunteers to supervise the walks and have not been associated with an increase in falls risk. At the environmental level, special consideration should be made by health system leadership to establish clear responsibilities and mobility protocols for PT, OT, and nursing when designing or disseminating hospital walking programs.
Limitations
Though this study innovatively applies the SEM model to understand factors influencing hospital mobility, which allowed for a deeper understanding of the barriers and facilitators of patient walking activity, there are several limitations. Involvement of a single health system limits generalizability of the findings. To mitigate this, we sampled from both a tertiary and community academic hospital, patients in our sample had a range of admission diagnoses and baseline mobility, and providers had diverse years of experience, all of which allowed us to elicit more diverse perspectives. Perspectives are limited to only those who participated in the interviews and may not fully represent the whole population. Nursing assistant roles and responsibilities differ from those of nursing, and their perspectives should be investigated more fully. Perspectives from family members are also largely missing, and warrants future investigation. However, a strength of this research lies in the inclusion of PTs and OTs in addition to hospitalists and nurses in middle managerial roles. We focused on interviewing providers in these roles because of a growing body of evidence that emphasizes the importance of these middle managerial roles in implementing new practices. 41,42 While the respondents tended to focus on process issues, those wishing to implement walking programs also need to consider structure and outcome issues including physical layout, staffing levels, required mobility metrics and incentives. Future qualitative work that includes the perspectives of a broad range of organizational leaders is also needed to better understand the programmatic barriers and financial implications to implementing and disseminating evidence-based mobility models.
Conclusions
While several personal factors influenced hospital mobility, modifiable interpersonal, organizational, and environmental factors were identified as potential targets for intervention. Patients and providers recommended improving awareness of patient’s baseline ambulatory activity, assigning roles and responsibility for mobility, and enhancing education and communication between patients and inter-professional providers. When designing or implementing hospital mobility interventions to mitigate hospital-associated disability, consideration of these salient factors and recommendations may enhance impact and sustainability.
Supplementary Material
Supplementary Table S1. Patient and Provider Interview Guides
Impact Statement.
We certify that this work is novel. This qualitative study examines the factors that influence hospital mobility, especially in the context of a heightened focus on falls prevention. We also discuss application of a socioecological framework for designing or implementing hospital walking or mobility programs.
Key Point:
Socioecological factors influence hospital mobility in “falls as a never event” era.
Modifiable interpersonal, cultural, and organizational factors are targets for intervention.
Why does this matter: Patient and frontline provider perspectives inform approaches to overcoming process and system-level mobility barriers.
ACKNOWLEDGEMENTS
Sponsors: This work was supported by the Duke Older Americans Independence Center (NIA P30 AG028716–01); The Duke Cancer Institute as part of the P30-CA014236 (Office of Cancer Centers, NCI); The Durham Center of Innovation to Accelerate Discovery and Practice Transformation (ADAPT) at the Durham VA Health Care System (CIN 13-410; Hastings); and NIA K24 AG049077-02 (Colon-Emeric).
Role of Sponsor Support: The funding sources had no role in the design and conduct of the study; analysis or interpretation of the data; preparation or final approval of the manuscript before publication, and decision to submit the manuscript for publication.
Footnotes
Conflict of Interests: The authors have no conflicts.
Publisher's Disclaimer: Disclaimer: The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of Duke University or the Department of Veterans Affairs.
Prior Presentations: This work was accepted to the American Geriatrics Society Annual Meeting, Long Beach, CA 2020 (meeting cancelled due to COVID-19 pandemic, abstract published: Pavon, J., L. Fish, C. Colon-Emeric, K. Hall, M. Morey, A. Pastva, and S. Hastings. “Towards “mobility is medicine”: a qualitative study of socioecological factors influencing hospital mobility in older adults.” In Journal of the American Geriatrics Society, 68:S244–45. WILEY, 2020).
REFERENCES
- 1.Brown CJ, Redden DT, Flood KL, Allman RM. The underrecognized epidemic of low mobility during hospitalization of older adults. J Am Geriatr Soc. 2009. September;57(9):1660–1665. [DOI] [PubMed] [Google Scholar]
- 2.Covinsky KE, Pierluissi E, Johnston CB. Hospitalization-associated disability: “She was probably able to ambulate, but I’m not sure”. JAMA. 2011; 306(16):1782–1793. [DOI] [PubMed] [Google Scholar]
- 3.Covinsky KE, Palmer RM, Fortinsky RH, et al. Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: increased vulnerability with age. J Am Geriatr Soc. 2003; 51(4):451–458. [DOI] [PubMed] [Google Scholar]
- 4.Fortinsky RH, Covinsky KE, Palmer RM, Landefeld CS. Effects of functional status changes before and during hospitalization on nursing home admission of older adults. J Gerontol A Biol Sci Med Sci. 1999; 54:M521–M526. [DOI] [PubMed] [Google Scholar]
- 5.Ostir GV, Berges IM, Kuo YF, Goodwin JS, Fisher SR, Guralnik JM Mobility activity and its value as a prognostic indicator of survival in hospitalized older adults. J Am Geriatr Soc. 2013; 61(4):551–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fisher SR, Goodwin JS, Protas EJ, Kuo YF, Graham JE, Ottenbacher KJ, Ostir GV. Ambulatory activity of older adults hospitalized with acute medical illness. J Am Geriatr Soc. 2011. January;59(1):91–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fisher SR, Kuo YF, Graham JE, Ottenbacher KJ, Ostir GV. Early ambulation and length of stay in older adults hospitalized for acute illness. Arch Intern Med. 2010;170(21):1942–1943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shadmi E, Zisberg A. In-hospital mobility and length of stay. Arch Intern Med. 2011. July 25;171(14):1298. [DOI] [PubMed] [Google Scholar]
- 9.Pavon JM, Sloane RJ, Pieper CF, et al. Accelerometer-Measured Hospital Physical Activity and Hospital-Acquired Disability in Older Adults. J Am Geriatr Soc. 2020. February;68(2):261–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Greysen SR, Patel MS. Web Exclusive. Annals for Hospitalists Inpatient Notes - Bedrest Is Toxic-Why Mobility Matters in the Hospital. Ann Intern Med. 2018. July 17;169(2):HO2–HO3. [DOI] [PubMed] [Google Scholar]
- 11.Hastings SN, Sloane R, Morey MC, Pavon JM, Hoenig H. Assisted early mobility for hospitalized older veterans: preliminary data from the STRIDE program. J Am Geriatr Soc. 2014. November;62(11):2180–2184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Agmon M, Zisberg A, Gil E, Rand D, Gur-Yaish N, Azriel M. Association Between 900 Steps a Day and Functional Decline in Older Hospitalized Patients. JAMA Intern Med. 2017. February 1;177(2):272–274. [DOI] [PubMed] [Google Scholar]
- 13.Sallis R, Roddy-Sturm Y, Chijioke E, et al. Stepping toward discharge: Level of ambulation in hospitalized patients. J Hosp Med. 2015;10(6):384–389. [DOI] [PubMed] [Google Scholar]
- 14.Fehlberg EA, Lucero RJ, Weaver MT, et al. Impact of the CMS No-Pay Policy on Hospital-Acquired Fall Prevention Related Practice Patterns. Innov Aging. 2017;1(3):igx036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Inouye SK, Brown CJ, Tinetti ME. Medicare nonpayment, hospital falls, and unintended consequences. N Engl J Med. 2009; 360:2390–2393. [DOI] [PubMed] [Google Scholar]
- 16.Brown CJ, Williams BR, Woodby LL, Davis LL, Allman RM. Barriers to mobility during hospitalization from the perspective of older patients and their nurses and physicians. J Hosp Med. 2007; 2(5): 305–313. [DOI] [PubMed] [Google Scholar]
- 17.Bronfenbrenner Urie (1979). The Ecology of Human Development: Experiments by Nature and Design. Cambridge, MA: Harvard University Press. ISBN 0-674-22457-4. [Google Scholar]
- 18.Callahan CM, Unverzagt FW, Hui SL, Perkins AJ, Hendrie HC. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med Care. 2002; September;40(9):771–781. [DOI] [PubMed] [Google Scholar]
- 19.Palinkas LA, Horwitz SM, Green CA, Wisdom JP, Duan N, Hoagwood K. Purposeful Sampling for Qualitative Data Collection and Analysis in Mixed Method Implementation Research. Adm Policy Ment Health. 2015. September;42(5):533–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Malterud K, Siersma VD, Guassora AD. Sample Size in Qualitative Interview Studies: Guided by Information Power. Qual Health Res. 2016. November;26(13):1753–1760. [DOI] [PubMed] [Google Scholar]
- 21.Stewart DW, & Shamdasani PN (2015). Focus groups: Theory and practice (Vol. 20). Los Angeles, Calif: SAGE. [Google Scholar]
- 22.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. International Journal for Quality in Health Care. 2007; 19 (6) 349–357. [DOI] [PubMed] [Google Scholar]
- 23.Craig CL, Marshall M, Sjostrom AE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003; 35 (8) (2003): 1381–1395. [DOI] [PubMed] [Google Scholar]
- 24.Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology, 2006; 3(2), 77–101. [Google Scholar]
- 25.Donabedian A “The quality of care: How can it be assessed?”. JAMA. 1988; 260 (12): 1743–1748. [DOI] [PubMed] [Google Scholar]
- 26.Hoyer EH, Brotman DJ, Chan KS, Needham DM. Barriers to early mobility of hospitalized general medicine patients: survey development and results. Am J Phys Med Rehabil. 2015; April;94(4):304–312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zisberg A, Agmon M, Gur-Yaish N, Rand D, Hayat Y, Gil E; WALK-FOR team. No one size fits all-the development of a theory-driven intervention to increase in-hospital mobility: the “WALK-FOR” study. BMC Geriatr. 2018. April 13;18(1):91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wald HL, Ramaswamy R, Perskin MH, et al. Quality and Performance Measurement Committee of the American Geriatrics Society. The Case for Mobility Assessment in Hospitalized Older Adults: American Geriatrics Society White Paper Executive Summary. J Am Geriatr Soc. 2019. January;67(1):11–16. [DOI] [PubMed] [Google Scholar]
- 29.Age-Friendly Health Systems: Guide to Using the 4Ms in the Care of Older Adults. April 2019. http://www.ihi.org/Engage/Initiatives/Age-Friendly-HealthSystems/Documents/IHIAgeFriendlyHealthSystems_GuidetoUsing4MsCare.pdf accessed 4/2/2020
- 30.Gillis A, MacDonald B, MacIssac A Nurses’ knowledge, attitudes, and confidence regarding preventing and treating deconditioning in older adults. The Journal of Continuing Education in Nursing. 2008; 39(12): 547–554. [DOI] [PubMed] [Google Scholar]
- 31.Padula CA, Hughes C, Baumhover L. Impact of a nurse-driven mobility protocol on functional decline in hospitalized older adults. J Nurs Care Qual. 2009; 24:325–331. [DOI] [PubMed] [Google Scholar]
- 32.Pavon JM, Sloane RJ, Pieper CF, et al. Physical Activity in the Hospital: Documentation and Influence on Venous Thromboembolism Prophylaxis. J Aging Phys Act. 2019; 17:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hoyer EH, Young DL, Friedman LA, et al. Routine Inpatient Mobility Assessment and Hospital Discharge Planning. JAMA Intern Med. 2019;179(1):118–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pavon JM, Sloane R, Morey MC, Hastings SN. Inpatient Mobility Measures as useful predictors of discharge destination in hospitalized older adults. J Am Geriatr Soc. 2017. January;65(1):224–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Boynton T, Kelly L, Perez A. Banner mobility assessment tool for nurses: Instrument validation. American Nurse Today. 2014; 4(3). 86–92. [Google Scholar]
- 36.Hoyer EH, Friedman M, Lavezza A, et al. Promoting Mobility and Reducing LOS. J. Hosp. Med 2016;5;341–347. [DOI] [PubMed] [Google Scholar]
- 37.Brown CJ, Roth DL, Allman RM. Validation of the use of wireless monitors to measure levels of mobility during hospitalization. J Rehabil Res Dev 2008; 45:551–558. [DOI] [PubMed] [Google Scholar]
- 38.Inouye SK, Bogardus ST Jr, Baker DI, Leo-Summers L, Cooney LM Jr. The Hospital Elder Life Program: a model of care to prevent cognitive and functional decline in older hospitalized patients. Hospital Elder Life Program. Journal of the American Geriatrics Society 2000; 48:1697–1706. [DOI] [PubMed] [Google Scholar]
- 39.Cohen Y, Zisberg A, Chayat Y, et al. Walking for Better Outcomes and Recovery: The Effect of WALK-FOR in Preventing Hospital-Associated Functional Decline Among Older Adults. J Gerontol A Biol Sci Med Sci. 2019. September 15;74(10):1664–1670. [DOI] [PubMed] [Google Scholar]
- 40.Liu B, Moore JE, Almaawiy U., et al. Outcomes of Mobilisation of Vulnerable Elders in Ontario (MOVE ON): A multisite interrupted time series evaluation of an implementation intervention to increase patient mobilisation. Age Ageing. 2018;47:112–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Birken S, Clary A, Tabriz AA, et al. Middle managers’ role in implementing evidence-based practices in healthcare: a systematic review. Implement Sci. 2018. December 12;13(1):149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Urquhart R, Kendell C, Folkes A, Reiman T, Grunfeld E, Porter GA. Making It Happen: Middle Managers’ Roles in Innovation Implementation in Health Care. Worldviews Evid Based Nurs. 2018. December;15(6):414–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table S1. Patient and Provider Interview Guides


