Abstract
Background/Objectives:
Medicare-certified home health agencies are required to offer family caregiver training, but little is known regarding the potential impact of this training on outcomes during home health care. We estimate the proportion of family caregivers assisting Medicare home health patients who have unmet training needs and examine whether these unmet training needs are associated with older adults’ risk of acute care utilization during home health care.
Design:
Observational, nationally representative cohort study.
Setting:
Linked National Health and Aging Trends Study (NHATS), Outcome and Assessment Information Set (OASIS), Medicare Provider of Services file, and Medicare claims data from 2011–2016.
Participants:
1,217 (weighted n=5,870,905) community-living Medicare beneficiaries who received home health care between 2011–2016.
Measurements:
Family caregivers’ unmet training needs measured from OASIS and Medicare claims; home health patients’ acute care utilization (including Emergency Department (ED) use and hospitalization) measured from OASIS.
Results:
Rates of unmet need for training varied by activity, from 8.2% of family caregivers assisting with household chores to 16.0% assisting with self-care tasks. After controlling for older adult and home health provider characteristics, older adults whose family caregivers had an unmet need for training with any caregiving activity were twice as likely to incur acute care utilization during their home health episode (Adjusted Odds Ratio (aOR): 2.01, 95% CI: 1.20–3.38). This relationship held across specific caregiving activities including household chores (aOR: 1.98; 95% CI: 1.13–3.46), medication management (aOR: 2.50; 95% CI: 1.46–4.26), patient supervision (aOR: 2.92; 95% CI: 1.36–6.24), and self-care tasks (aOR: 3.11; 95% CI: 1.62–6.00).
Conclusions and relevance:
Unmet training needs among family caregivers are associated with greater likelihood of acute care utilization among Medicare beneficiaries receiving home health care. Identifying and addressing family caregivers’ training needs may reduce older adults’ risk of acute care utilization during home health care.
Keywords: family caregiving, home health care, acute care utilization, Medicare
INTRODUCTION
Medicare-funded home health care provides eligible beneficiaries with skilled nursing, rehabilitation therapy, and personal care delivered in the home environment. Medicare spending on home health care more than doubled between 2000 and 2016 as utilization increased.1 Older adults who receive home health care have significant social and clinical complexity2 and home health providers are only present in the home intermittently. Thus, executing the home health plan of care is often contingent on help provided by unpaid and family caregivers3—individuals with a close relationship to an older adult for whom they provide regular assistance. Home health providers report that family caregiver assistance is needed in 87% of index home health care episodes.4
In recognition of the critical role family caregivers play in home health care, The Centers for Medicare and Medicaid Services (CMS) revised the Home Health Conditions of Participation in 2017 to require that home health providers offer family caregiver training as needed to enact the plan of care.5 A growing body of evidence suggests that the availability, capacity, and characteristics of family caregivers affect older adults’ health care utilization and outcomes6–10 and that providing training for family caregivers may improve such outcomes.11–16 Yet, fewer than 1 in 10 family caregivers report receiving training.17
More than one-third of family caregivers assisting during a Medicare-funded home health care episode have an identified need for training related to their caregiving role.18 Family caregivers’ identified training needs affect the number of skilled nursing and therapy visits received during home health care.19 However, the scope of caregiver training provided during home health care, and the potential consequences of failing to meet family caregivers’ training needs in this setting, are unknown. Guided by Andersen’s Behavioral Model of Health Services Use, we hypothesized that unmet family caregiver training needs may be linked to greater acute care utilization by increasing the patient’s perceived and actual need for this care, due to the caregiver not having the necessary resources to meet the older adult’s care needs in the home.20
CMS has prioritized reducing unplanned acute care utilization as a critical step towards improving care quality while curtailing costs.21 Medicare beneficiaries receiving post-acute care experience a higher rate of Emergency Department (ED) visits and hospitalization in home health care, compared to skilled nursing or inpatient rehabilitation.22 Therefore, information regarding how unmet family caregiver training needs may affect the risk of acute care utilization during home health care is especially relevant at this time.
This is the first study to examine the relationship between unmet training needs among family caregivers and services utilization of patients in the home health care setting. Drawing on a nationally representative sample of Medicare beneficiaries receiving home health care between 2011–2016, we model the relationship between caregivers’ activity-specific unmet training needs and older adults’ acute care utilization—including ED visits and hospitalization—during the home health care episode. Findings are relevant to ongoing efforts to reduce ED visits and unplanned hospitalization, improve home health care quality, and connect family caregivers with training resources.
METHODS
Data Sources and Analytic Sample
Data for this study were drawn from four linked data sources: the National Health and Aging Trends Study (NHATS), the Outcomes and Assessment Information Set (OASIS), Medicare claims, and Medicare Provider of Services (POS) files. NHATS is an annual, nationally representative survey of Medicare beneficiaries ages 65 and older that collects comprehensive information on participants’ sociodemographic characteristics, health and functional status, and assistance from family and unpaid caregivers via in-person interviews. OASIS is a standardized patient assessment completed by a home health clinician (either a Registered Nurse or Physical Therapist) and submitted to CMS at regular intervals during a Medicare-funded home health episode. OASIS includes information regarding the older adult’s clinical and functional status, plan of care, and receipt of assistance from family caregivers. POS files are publicly-available sources of information on the characteristics of Medicare-certified providers, including home health agencies.
The analytic sample included 1,217 older adults who participated in the 2011 NHATS and received Medicare-funded home health care within one year of the baseline interview (2011) or a subsequent interview (2012–2015). We pooled NHATS data from 2011–2015 with linked OASIS data and Medicare claims from 2011–2016. For each participant, we matched the OASIS Start of Care filing for the first (index) home health episode during the observation period with the NHATS interview immediately preceding the index home health episode. We then included claims filed for services provided during the 60-day index home health episode. Finally, we used CMS Certification Numbers (unique identifiers assigned to each Medicare-certified provider) present in the claims to link to POS data for each provider, from the year in which the index episode occurred.
We exclusively examined the index home health episode; therefore, each participant appeared in the dataset once. We excluded NHATS participants who did not receive home health care during the observation period as well as those living in congregate settings such as assisted living facilities at the time of the NHATS interview due to the availability of supports that may substitute for or otherwise affect family caregiving. Our sample excluded Medicare Advantage enrollees, as claims data were not available for this population. This study was approved by the Johns Hopkins Bloomberg School of Public Health Institutional Review Board.
Measures
Older Adult and Home Health Provider Characteristics
From NHATS, we measured older adult characteristics prior to the home health care episode which may be considered predisposing characteristics for health care utilization20: sociodemographic factors (age, sex, race, Medicaid-enrollment), health status (self-reported overall health status and prior year hospitalization), and receipt of family caregiver assistance (help with household chores, mobility tasks, and/or self-care tasks). From OASIS, we measured the following older adult characteristics during the home health care episode which may be considered predisposing and need factors for health care utilization20: living arrangement (whether they lived alone), post-acute status (receipt of inpatient care within 14 days of home health care), care intensity (receipt of any respiratory therapy or intravenous treatment), clinical severity, functional impairment, and cognitive impairment.
Clinical severity and functional impairment during home health care were determined from Health Insurance Prospective Payment System (HIPPS) codes.23 These codes are used for home health payment risk adjustment23 and identify home health patients as having little or no, moderate, or significant functional impairment and low, moderate, or significant clinical severity. Cognitive impairment was measured via home health clinician assessment of the older adult.24
From POS, we identified the following home health provider characteristics which may be considered enabling and need factors for health care utilization20: type of ownership (for-profit vs nonprofit), number of full-time equivalent employees, and hospital affiliation (connected to a larger health system). From Medicare claims, we measured care intensity using the number and type of home health visits provided within the 60-day index home health episode. We created count variables for nursing and therapy visits incurred during this timeframe, identifying the type of visit using Healthcare Common Procedure Coding System codes.25, 26 Nursing visits were visits from a Registered Nurse (RN) or Licensed Practical Nurse (LPN) to provide direct care, evaluate the plan of care, or observe/assess patient’s condition. Therapy visits were visits from a Physical Therapist (PT), Occupational Therapist (OT), Speech Language Therapist, or PT or OT Assistant to provide direct care or develop a program of therapy. Because nearly one-fourth (22.4%) of the sample received no therapy visits, we created a binary indicator of receipt of any therapy visits for use in our analyses.
Family Caregivers’ Unmet Training Needs
In OASIS, home health clinicians document whether a patient needs family caregiver assistance with specific activities, whether they receive this assistance, and whether the caregiver needs training in order to provide this assistance.24 For all analyses, we limited our analytic sample to episodes in which the older adult was identified as receiving family caregiver assistance with the given caregiving activity. Caregiver involvement and need for training varies considerably by caregiving activity.4, 18 In this study, we considered caregiving activities during the home health episode for which at least 50% of older adults required family caregiver assistance4 and at least 10% of caregivers had an identified training need.18 These activities were:
Household chores (assisting with meals, housekeeping, laundry, telephone, shopping),
Self-care tasks (assisting with ambulation, bathing, dressing, toileting, eating/feeding),
Medication management (managing and administering medications),
Patient supervision (monitoring to ensure patient’s safety).
We measured family caregivers’ unmet need for training for each caregiving activity using information from both the OASIS and Medicare claims. As part of the OASIS patient assessment, home health clinicians document whether the patient needs family caregiver assistance with specific activities, whether the patient receives this assistance, and whether the caregiver requires additional training in order to provide this assistance.24 We considered the family caregiver to have an identified training need with a given activity if the home health clinician reported that the caregiver was providing assistance but required additional training. From claims data, we determined whether any training had been provided during the older adult’s home health care episode; claims include a count of the number of training visits, defined as visits made by an RN or LPN to offer training/education.26 As the majority of the sample (weighted proportion=67.82%) experienced zero training visits, we created a binary variable equal to “1” if any training visits were received and “0” otherwise.
We then created a binary indicator of unmet need for training, defined as having an identified need for training and not receiving any training visits. There was no unmet need for training if 1) the family caregiver had no identified need for training or 2) the family caregiver received one or more training visits. We measured unmet need for training for each caregiving activity (household chores, self-care tasks, medication management, and patient supervision) and created a composite measure for unmet need for training with any of these four activities.
Acute Care Utilization
We constructed a binary indicator of acute care utilization for each home health patient from OASIS data. We identified whether each patient had any OASIS files indicating Emergency Department (ED) visit or hospitalization during their home health episode. These included filings which indicated resumption of home health care following an acute care hospital stay, discharge to an acute care hospital during the home health episode, and ED visit (with or without hospital admission) during the home health episode.
Statistical Analysis
We used weighted, multivariable logistic regressions to model the adjusted odds of acute care utilization among older adults during a home health care episode, as a function of family caregivers’ unmet training needs. All models adjusted for a range of covariates: older adults’ sociodemographic characteristics, health status and family caregiver assistance before and during home health care, home health care intensity, and home health provider characteristics. All models were weighted to provide nationally representative estimates and account for the NHATS complex survey design. All analyses were performed using Stata 14 (StataCorp LLC, College Station, TX). This research was approved by the Johns Hopkins Bloomberg School of Public Health Institutional Review Board.
RESULTS
The sample for this study included 1,217 (weighted n=5,870,905) community-dwelling Medicare beneficiaries receiving home health care between 2011–2016 (Table 1). The average age of participants was 79.8 years, 19.6% were non-white, 16.7% were Medicaid-enrolled, and 71.0% were admitted to home health care following a hospitalization. Among family caregivers assisting during a home health care episode, unmet need for training varied by activity, from 8.2% of those assisting with household chores to 16.0% of those assisting with medication management or self-care tasks (Figure 1).
Table 1.
Characteristics of Community-Dwelling Older Adults Receiving Family Caregiver Assistance during Medicare Home Health Care between 2011–2016 (n=1,217 unweighted, n=5,870,905 weighted)a
| % (n) or Mean ± SE | |
|---|---|
| Older Adult Characteristics | |
| Age | 79.8 ± 0.29 |
| Male sex | 40.5% (468) |
| Non-white race | 19.6% (401) |
| Medicaid-enrolled | 16.7% (250) |
| Prior to Home Health Care | |
| Self-rated health: | |
| Excellent/very good | 26.4% (285) |
| Good | 31.7% (381) |
| Fair/poor | 41.9% (551) |
| Hospitalized in past year | 30.1% (560) |
| Receives functional assistance with: | |
| None | 40.1% (421) |
| Household chores | 27.1% (318) |
| Mobility | 7.4% (109) |
| Self-care | 25.4% (369) |
| During Home Health Care | |
| Incurs acute care utilization | 15.2% (195) |
| Lives alone | 32.8% (400) |
| Post-acute | 71.0% (794) |
| Clinical severity | |
| Low | 26.5% (331) |
| Moderate | 41.1% (485) |
| High | 32.4% (401) |
| Functional impairment | |
| None/low | 17.2% (190) |
| Moderate | 62.4% (762) |
| High | 20.4% (265) |
| Cognitive impairment | 44.1% (605) |
| Care Intensity During Home Health Care | |
| Receipt of any respiratory therapy | 10.5% (137) |
| Receipt of any IV treatment | 2.1% (24) |
| Number of nursing visits received | 7.2 ± 0.26 |
| Receipt of any therapy visits | 77.6% (945) |
| Home Health Provider Characteristics | |
| Nonprofit | 46.2% (455) |
| Number of full-time equivalent employees | 98.4 ± 20.1 |
| Affiliated with an acute care hospital | 15.7% (151) |
Data are drawn from National Health and Aging Trends Study (NHATS) and linked Outcomes and Assessment Information Set (OASIS), Medicare claims data, and Provider of Services data for 1,217 Medicare beneficiaries receiving family caregiver assistance during a home health episode between 2011–2016. Percentages are weighted to account for NHATS survey design and to produce nationally representative estimates.
Figure 1. Rates of Unmet Need for Training among Family Caregivers to Medicare Beneficiaries Receiving Home Health Care, by Activity (n=1,217 unweighted, n=5,870,905 weighted)a,b.
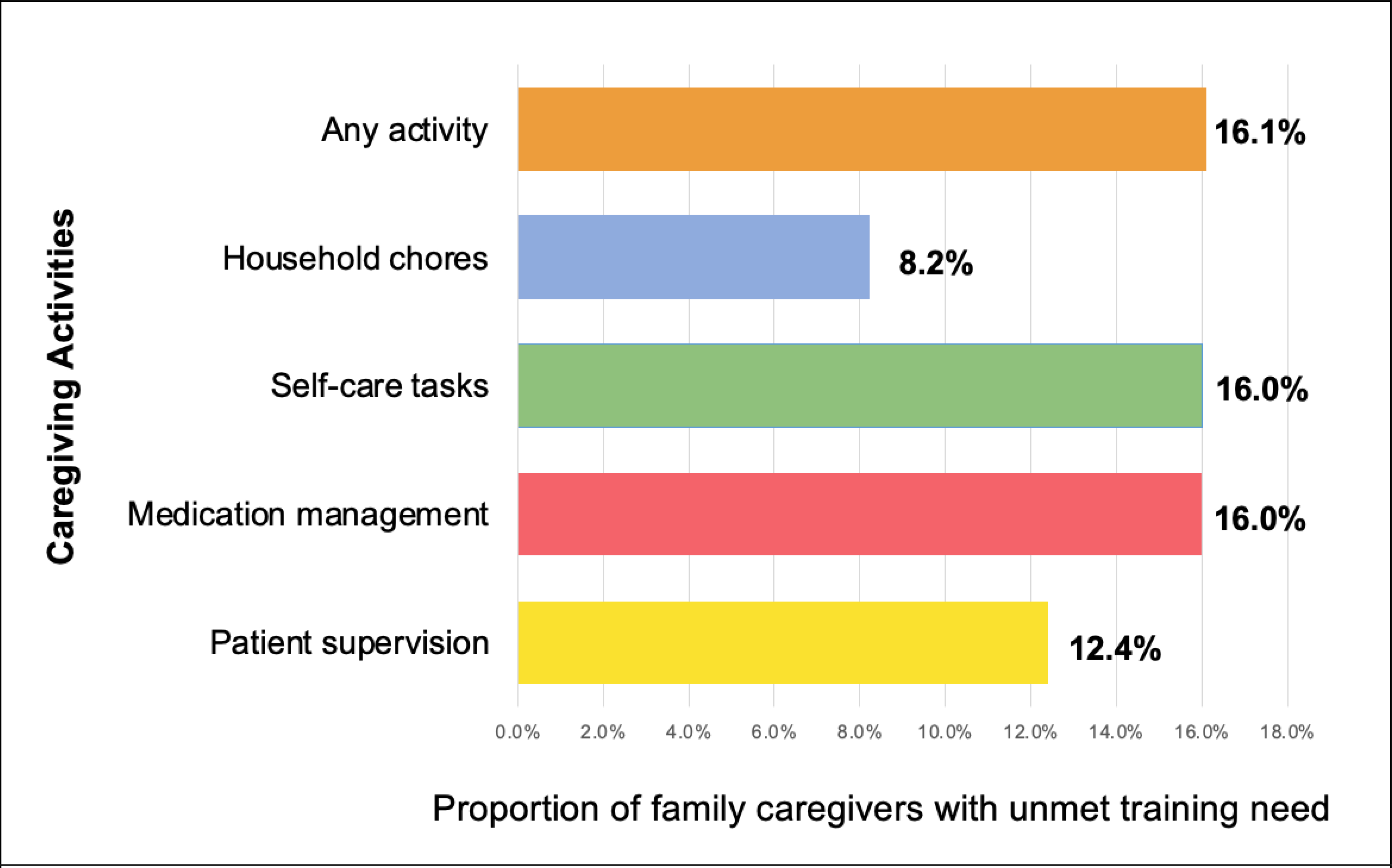
a) Data are drawn from National Health and Aging Trends Study (NHATS) and linked Outcomes and Assessment Information Set (OASIS), Medicare claims data, and Provider of Services data for 1,217 Medicare beneficiaries receiving family caregiver assistance during a home health episode between 2011–2016. Proportions are weighted to account for complex survey design.
b) Bars represent the proportion of family caregivers assisting during a Medicare-funded home health episode who have an unmet need for training, by caregiving activity.
Among community-dwelling Medicare beneficiaries receiving home health care, 15.2% experienced acute care utilization during their index home health episode (Table 1). Older adults receiving family caregiver assistance were more likely to experience acute care utilization if the family caregiver had one or more unmet needs for training (Figure 2). After controlling for older adult and home health provider characteristics, older adults whose family caregiver had unmet need(s) for training on any activity were twice as likely to experience acute care utilization (Adjusted Odds Ratio (aOR): 2.01, 95% CI: 1.20–3.38). Older adults whose family caregivers had unmet training needs with respect to specific activities experienced a two- to three-fold greater likelihood of acute care utilization. Likelihood of acute care utilization was higher among older adults whose family caregivers had unmet need for training with household chores (aOR: 1.98; 95% CI: 1.13–3.46), medication management (aOR: 2.50; 95% CI: 1.46–4.26), patient supervision (aOR: 2.92; 95% CI: 1.36–6.24), and self-care tasks (aOR: 3.11; 95% CI: 1.62–6.00). (For full regression results, see Supplementary Tables S1–S5.)
Figure 2. Comparative Adjusted Odds of Acute Care Utilization among Medicare Beneficiaries Receiving Home Health Care Whose Family Caregivers Do (Versus Do Not) have Unmet Need for Training (n=1,217 unweighted, n=5,870,905 weighted)a,b.
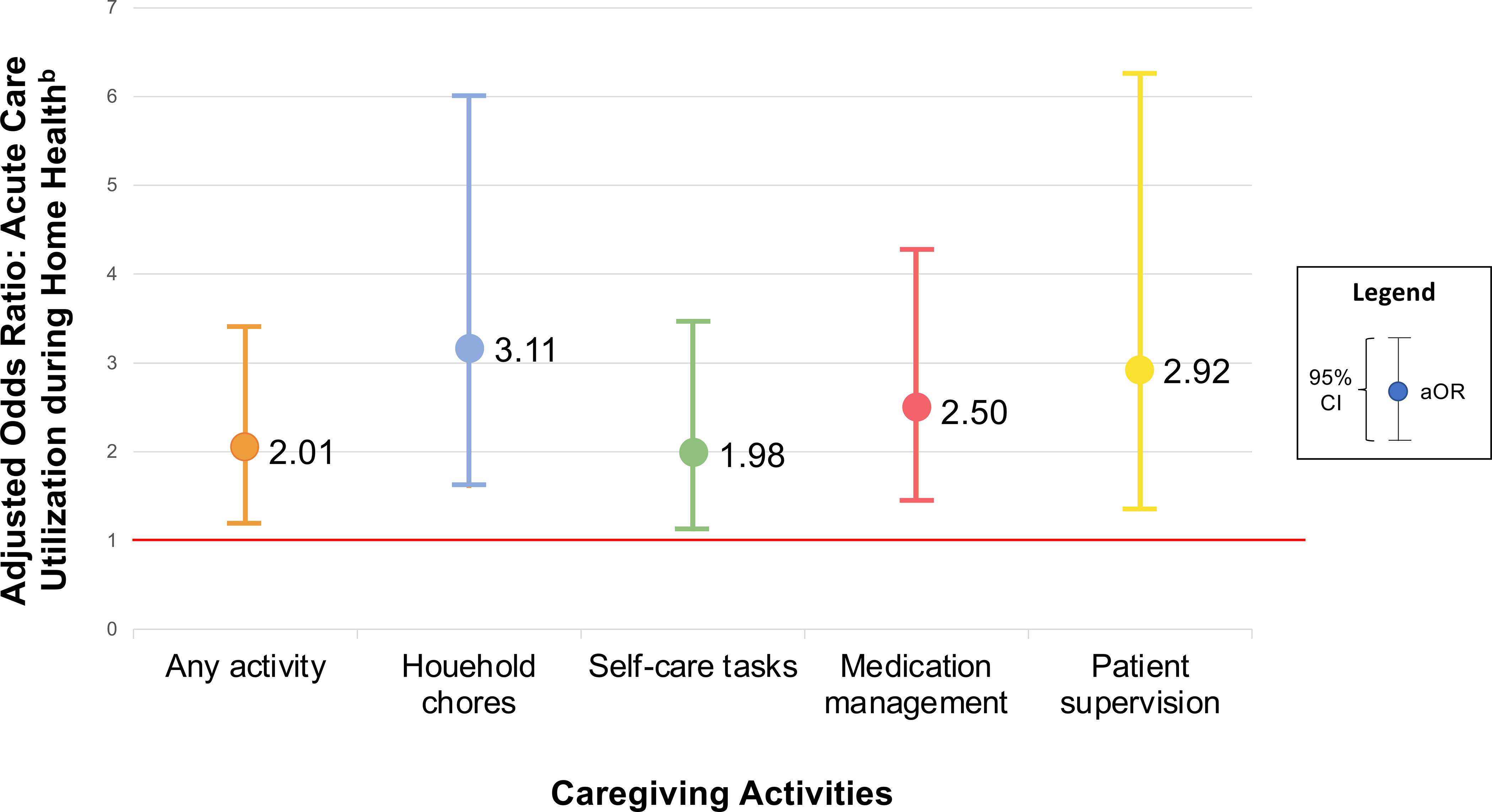
a) Data are drawn from National Health and Aging Trends Study (NHATS) and linked Outcomes and Assessment Information Set (OASIS), Medicare claims data, and Provider of Services data for 1,217 Medicare beneficiaries receiving family caregiver assistance during a home health episode between 2011–2016.
b) Adjusted for: measures of older adults’ sociodemographic characteristics (age, sex, race, Medicaid-enrollment), health status (self-reported health status and prior year hospitalization), and receipt of family caregiver assistance (help with household chores, mobility tasks, or self-care tasks) prior to home health; older adults’ living arrangement (whether they lived alone), post-acute status (whether they received inpatient care within 14 days of home health care), care intensity (receipt of any respiratory therapy or any IV treatment, number of nursing visits received, receipt of any therapy visits), clinical severity, functional impairment, and cognitive impairment during home health; and home health provider non-profit status, number of full-time equivalent employees, and affiliation with any acute care hospital.
DISCUSSION
Older adults whose family caregivers were identified as having an unmet need for training were twice as likely to experience acute care utilization during their home health care episode. This relationship persisted across specific caregiving activities: those whose family caregivers had an unmet training need with respect to patient supervision or self-care tasks experienced three times higher odds of acute care utilization, while those whose family caregivers had an unmet training need with respect to household chores or medication management experienced two times higher odds of acute care utilization. Findings collectively indicate that family caregiver capacity and the adequacy of training they receive may affect older adults’ outcomes and risk of acute care utilization during a home health care episode and suggest benefits from better supporting caregivers’ training needs.
Health care delivery reform efforts aimed at improving outcomes and reducing costs for older adults have emphasized the importance of averting ED visits and unplanned hospitalizations from post-acute settings.12, 21, 28, 29 Factors associated with risk of ED visit or hospitalization from home health care have been reported to include the quality of cross-setting communication between clinicians,30 rural location,31 older adult’s dementia status,32 patients’ prior acute care use,33, 34 and the length of the home health episode.35 These factors are largely out of home health providers’ direct control and have more modest effects than the relationships observed in this study. In comparison, family caregiver training is not only amenable to intervention by home health providers, but required under new Medicare Conditions of Participation.5 Findings highlight the importance of responding to caregivers’ individual needs and suggest that targeted training interventions, delivered to those with the greatest need for education, could positively affect patient outcomes. Prior work identifies factors which increase family caregivers’ likelihood of needing training during home health care, including recent escalation in older adults’ care needs, less caregiving experience, and assisting with nursing/medical tasks.18 Unfortunately, a revised home health patient assessment instrument implemented in 2019 (OASIS-D), no longer solicits clinicians’ judgment regarding caregiver training needs at the start of care.36 This change could potentially hamper clinicians’ ability to identify those most in need of training related to caregiving activities.
The effect of unmet family caregiver training needs on older adults’ service use has not been previously studied. Existing knowledge relating to family caregiver training interventions is limited to outpatient primary and specialty care settings and primarily examines caregiver outcomes (e.g. depressive symptoms, burden, sense of self-efficacy).12–16, 37, 38 While these outcomes are important, understanding the effects of family caregiver training for patient services use offers a more direct “return on investment” argument to motivate an increased deployment of resources for family caregiver training and support. Our study reveals one potential avenue by which investment in family caregiver training may be cost-effective for integrated health systems and/or payers: through reductions in acute care utilization among home health care patients.
Family caregivers have traditionally been deemed “informal” providers of care and, as a result, rarely integrated into the care team or offered adequate training and support.11, 39–41 Our findings demonstrate the importance of collaboration between family caregivers and health care providers in determining patient outcomes. Family caregivers, like other care team members, may benefit from training to ensure that they have the requisite knowledge and skills to provide appropriate care. Ongoing efforts to develop family caregiver training interventions are promising;13, 14, 16 yet few programs are designed for specific care delivery settings, such as home health care.15, 38 Gaps in reimbursement40, 42 and educational curricula to prepare health care professionals for triadic interactions with both patients and family caregivers41 pose further barriers to identifying and addressing caregiver training needs. The development of embedded training programs designed for implementation in care delivery settings would facilitate improved support of family caregivers, in turn contributing to improved care quality and outcomes for high-need older adults.
Limitations and Strengths
Several limitations merit comment. This is an observational study and we cannot comment on causal relationships given the potential existence of unobserved confounders. Due to our reliance on claims data to ascertain receipt of training, our sample is limited to Medicare Fee-for-Service enrollees and findings may not be applicable to Medicare Advantage enrollees. We rely on the OASIS, the only available national source of data on family caregiver factors during home health care, but research on the reliability and validity of OASIS items is limited.27 We are not aware of evidence demonstrating the psychometric properties of items relating to caregiver training needs. As our sample focuses on index home health episodes, findings may not be reflective of later episodes in a sustained period of home health care utilization.
Our sample size is constrained to older adults who participated in a national survey. Future studies should extend analyses to larger samples of individuals receiving home health care; a larger sample could be valuable in facilitating analyses which consider ED use and hospitalization separately and test for differences between these outcomes. Despite these limitations, our paper has multiple notable strengths: we examine a nationally representative sample of Medicare beneficiaries; we draw on clinician reports of family caregivers’ specific training needs, measured during the home health care episode; and we control for a range of factors that may affect patients’ risk of ED visit and hospitalization at the older adult, home health care episode, and home health provider levels.
Conclusion
The unmet training needs of family caregivers are associated with greater likelihood of acute care utilization among older adults receiving home health care. Findings substantiate recent policy efforts to expand family caregiver access to training in care delivery settings and suggest that appropriate training of family caregivers may mitigate hospitalization risk among older adults receiving home health care.
Supplementary Material
SUPPLEMENTARY MATERIAL: Supplementary tables S1–S5 include results of weighted, multivariable logistic regressions modelling patients’ adjusted odds of acute care utilization during home health as a function of unmet family caregiver training needs.
KEY POINTS:
Among family caregivers assisting an older adult during Medicare home health care, 16% have an unmet need for training related to their caregiving role.
Medicare home health patients are twice as likely to visit the hospital if receiving help from a family caregiver with an unmet training need.
Investing in family caregiver training access during home health care could potentially improve outcomes and/or reduce costs for major payers like Medicare.
Why does this matter?
During home health care, systematically identifying and meeting family caregivers’ training needs may improve care outcomes for older patients.
ACKNOWLEDGEMENTS
Funding sources: This work was supported by the National Institute on Aging under Grant R01AG047859 and by the Agency for Health Care Research and Quality under Grant T32HS0000029.
Footnotes
Conflicts of interest: Authors have no conflicts of interest to disclose.
REFERENCES
- 1.March 2017 Report to the Congress. Washington, DC: Medicare Payment Advisory Commission. 2017. http://medpac.gov/docs/default-source/reports/mar17_entirereport.pdf. [Google Scholar]
- 2.Home Health Chartbook 2018:Prepared for the Alliance for Home Health Quality and Innovation. Alliance for Home Health Quality and Innovation & Avalere Health; 2018. http://ahhqi.org/images/uploads/AHHQI_2018_Chartbook_09.21.2018.pdf. [Google Scholar]
- 3.Arbaje AI, Hughes A, Werner N, et al. Information management goals and process failures during home visits for middle-aged and older adults receiving skilled home healthcare services after hospital discharge: a multisite, qualitative study. BMJ Qual Saf. 2019;28(2):111–120. doi: 10.1136/bmjqs-2018-008163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Burgdorf J, Arbaje A, & Wolff JL. Older Adult Factors Associated With Identified Need for Family Caregiver Assistance During Home Health Care. Home Health Care Management & Practice. 2019; 32(2): 67–75. doi: 10.1177/1084822319876608 [DOI] [Google Scholar]
- 5.Medicare and Medicaid Program: Conditions of Participation for Home Health Agencies. Washington, DC: Centers for Medicare and Medicaid Services; 2017. https://www.federalregister.gov/documents/2017/01/13/2017-00283/medicare-and-medicaid-program-conditions-of-participation-for-home-health-agencies. [PubMed] [Google Scholar]
- 6.Wolff JL, Nicholas LH, Willink A, Mulcahy J, Davis K, Kasper JD. Medicare Spending and the Adequacy of Support With Daily Activities in Community-Living Older Adults With Disability: An Observational Study. Ann Intern Med. June 2019;170(12):837–844. doi: 10.7326/M18-2467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wolff JL, Mulcahy J, Roth DL, et al. Long-Term Nursing Home Entry: A Prognostic Model for Older Adults with a Family or Unpaid Caregiver. J Am Geriatr Soc. 2018;66(10):1887–1894. doi: 10.1111/jgs.15447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hoffman GJ, Hays RD, Wallace SP, Shapiro MF, Yakusheva O, Ettner SL. Receipt of Caregiving and Fall Risk in US Community-dwelling Older Adults. Med Care. 2017;55(4):371–378. doi: 10.1097/MLR.0000000000000677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gaugler JE, Yu F, Krichbaum K, Wyman JF. Predictors of nursing home admission for persons with dementia. Review. Med Care. 2009;47(2):191–8. doi: 10.1097/MLR.0b013e31818457ce [DOI] [PubMed] [Google Scholar]
- 10.Burgdorf J, Mulcahy J, Amjad H, Kasper JD, Covinsky K, Wolff JL. Family Caregiver Factors Associated With Emergency Department Utilization Among Community-Living Older Adults With Disabilities. J Prim Care Community Health. 2019;doi: 10.1177/2150132719875636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Academies of Sciences, Engineering, and Medicine. (2016). Families Caring for an Aging America. Washington, DC: The National Academies Press. 10.17226/23606. [DOI] [PubMed] [Google Scholar]
- 12.Nuckols TK, Keeler E, Morton S, et al. Economic Evaluation of Quality Improvement Interventions Designed to Prevent Hospital Readmission: A Systematic Review and Meta-analysis. JAMA Intern Med. 2017;177(7):975–985. doi: 10.1001/jamainternmed.2017.1136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Teri L, Logsdon RG, McCurry SM, Pike KC, McGough EL. Translating an Evidence-based Multicomponent Intervention for Older Adults With Dementia and Caregivers. Gerontologist. 2018;doi: 10.1093/geront/gny122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Van Houtven CH, Oddone EZ, Hastings SN, et al. Helping Invested Families Improve Veterans’ Experiences Study (HI-FIVES): study design and methodology. Contemp Clin Trials. 2014;38(2):260–9. doi: 10.1016/j.cct.2014.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Burns R, Nichols LO, Martindale-Adams J, Graney MJ, Lummus A. Primary care interventions for dementia caregivers: 2-year outcomes from the REACH study. Gerontologist. 2003;43(4):547–55. doi: 10.1093/geront/43.4.547 [DOI] [PubMed] [Google Scholar]
- 16.Van Houtven CH, Smith VA, Lindquist JH, et al. Family Caregiver Skills Training to Improve Experiences of Care: a Randomized Clinical Trial. J Gen Intern Med. 2019;doi: 10.1007/s11606-019-05209-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Burgdorf J, Roth DL, Riffin C, Wolff JL. Factors Associated with Receipt of Training Among Caregivers of Older Adults. JAMA Intern Med. 2019; 179 (6), 833–835. doi: 10.1001/jamainternmed.2018.8694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Burgdorf JG, Arbaje AI, Wolff JL. Training Needs Among Family Caregivers Assisting During Home Health, as Identified by Home Health Clinicians. J Am Med Dir Assoc. 2020; doi: 10.1016/j.jamda.2020.05.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Burgdorf JG, Stuart EA, Arbaje AI, Wolff JL. Family Caregiver Training Needs and Medicare Home Health Visit Utilization. Med Care (forthcoming). 2021; January 21. doi: 10.1097/MLR.0000000000001487. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Andersen R Revisiting the Behavioral Model and Access to Health Care: Does It Matter? J Health Soc Behav. 1995; March, 36(1):1–10. [PubMed] [Google Scholar]
- 21.Hospital Readmissions Reduction Program (HRRP). Washington, DC: Centers for Medicare and Medicaid Services. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/HRRP/Hospital-Readmission-Reduction-Program [Google Scholar]
- 22.March 2019 Report to the Congress. Washington, DC: Medicare Payment Advisory Commission. 2019. http://medpac.gov/docs/default-source/reports/mar19_medpac_entirereport_sec.pdf?sfvrsn=0. [Google Scholar]
- 23.Definition and Uses of Health insurance Prospective Payment System Codes (HIPPS Codes). Washington, DC: CMS Division of Institutional Claims Processing. 2010. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/ProspMedicareFeeSvcPmtGen/Downloads/hippsuses.pdf. [Google Scholar]
- 24.Outcome and Assessment Information Set Guidance Manual. Washington, DC: Centers for Medicare and Medicaid Services. 2016. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HomeHealthQualityInits/Downloads/OASIS-C2-Guidance-Manual-6-17-16.pdf [Google Scholar]
- 25.Home Health Medicare Billing Codes Sheet. Washington, DC: Centers for Medicare and Medicaid Services. 2020. https://www.cgsmedicare.com/hhh/education/materials/pdf/home_health_billing_codes.pdf [Google Scholar]
- 26.Medicare Claims Processing Manual: Chapter 10-Home Health Agency Billing. Washington, DC: Centers for Medicare and Medicaid Services. 2020. https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c10.pdf [Google Scholar]
- 27.O’Connor M, Davitt JK. The Outcome and Assessment Information Set (OASIS): a review of validity and reliability. Home Health Care Serv Q. 2012;31(4):267–301. doi: 10.1080/01621424.2012.703908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Auerbach AD, Kripalani S, Vasilevskis EE, et al. Preventability and Causes of Readmissions in a National Cohort of General Medicine Patients. JAMA Intern Med. 2016;176(4):484–93. doi: 10.1001/jamainternmed.2015.7863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gruneir A, Silver MJ, Rochon PA. Emergency department use by older adults: a literature review on trends, appropriateness, and consequences of unmet health care needs. Med Care Res Rev. 2011;68(2):131–55. doi: 10.1177/1077558710379422 [DOI] [PubMed] [Google Scholar]
- 30.Pesko MF, Gerber LM, Peng TR, Press MJ. Home Health Care: Nurse-Physician Communication, Patient Severity, and Hospital Readmission. Health Serv Res. 2018;53(2):1008–1024. doi: 10.1111/1475-6773.12667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chen HF, Carlson E, Popoola T, Suzuki S. The Impact of Rurality on 30-Day Preventable Readmission, Illness Severity, and Risk of Mortality for Heart Failure Medicare Home Health Beneficiaries. J Rural Health. 2016;32(2):176–87. doi: 10.1111/jrh.12142 [DOI] [PubMed] [Google Scholar]
- 32.Knox S, Downer B, Haas A, Middleton A, Ottenbacher KJ. Dementia Severity Associated With Increased Risk of Potentially Preventable Readmissions During Home Health Care. J Am Med Dir Assoc. 2020;21(4):519–524.e3. doi: 10.1016/j.jamda.2019.09.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lohman MC, Scherer EA, Whiteman KL, Greenberg RL, Bruce ML. Factors Associated With Accelerated Hospitalization and Re-hospitalization Among Medicare Home Health Patients. J Gerontol A Biol Sci Med Sci. 2018;73(9):1280–1286. doi: 10.1093/gerona/glw335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jones CD, Falvey J, Hess E, et al. Predicting Hospital Readmissions from Home Healthcare in Medicare Beneficiaries. J Am Geriatr Soc. 2019;67(12):2505–2510. doi: 10.1111/jgs.16153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.O’Connor M, Hanlon A, Naylor MD, Bowles KH. The impact of home health length of stay and number of skilled nursing visits on hospitalization among Medicare-reimbursed skilled home health beneficiaries. Res Nurs Health. 2015;38(4):257–67. doi: 10.1002/nur.21665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Centers for Medicare and Medicaid Services. Outcome and Assessment Information Set OASIS-D Guidance Manual. 2018. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HomeHealthQualityInits/Downloads/OASIS-D-Guidance-Manual-final.pdf
- 37.Hepburn KW, Tornatore J, Center B, Ostwald SW. Dementia family caregiver training: affecting beliefs about caregiving and caregiver outcomes. J Am Geriatr Soc. 2001;49(4):450–7. doi: 10.1046/j.1532-5415.2001.49090.x [DOI] [PubMed] [Google Scholar]
- 38.Nichols LO, Martindale-Adams J, Burns R, Zuber J, Graney MJ. REACH VA: Moving from Translation to System Implementation. Gerontologist. 2016;56(1):135–44. doi: 10.1093/geront/gnu112 [DOI] [PubMed] [Google Scholar]
- 39.Levine C, Halper D, Peist A, Gould DA. Bridging troubled waters: family caregivers, transitions, and long-term care. Health Aff (Millwood). 2010;29(1):116–24. doi:29/1/11610.1377/hlthaff.2009.0520 [DOI] [PubMed] [Google Scholar]
- 40.Levine C Putting the Spotlight on Invisible Family Caregivers. JAMA Intern Med. 2016;176(3):380–1. doi: 10.1001/jamainternmed.2015.8002 [DOI] [PubMed] [Google Scholar]
- 41.Wolff JL, Feder J, Schulz R. Supporting Family Caregivers of Older Americans. N Engl J Med. 2016;375(26):2513–2515. doi: 10.1056/NEJMp1612351 [DOI] [PubMed] [Google Scholar]
- 42.Transitional Care Management Services. Medicare Learning Network. Washington, DC: Centers for Medicare and Medicaid Services. 2016. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/Transitional-Care-Management-Services-Fact-Sheet-ICN908628.pdf. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
SUPPLEMENTARY MATERIAL: Supplementary tables S1–S5 include results of weighted, multivariable logistic regressions modelling patients’ adjusted odds of acute care utilization during home health as a function of unmet family caregiver training needs.


