Abstract
Background
Chronic kidney disease (CKD) is a leading cause of morbidity and mortality globally. The risk of CKD is increased in people of African ancestry and with Human Immunodeficiency Virus (HIV) infection.
Methods
We conducted a cross-sectional study investigating the relationship between region of ancestry (East, Central, South or West Africa) and kidney disease in people of sub-Saharan African ancestry with HIV in the UK between May 2018 and February 2020. The primary outcome was renal impairment (estimated glomerular filtration rate [eGFR] of <60 mL/min/1.73 m2). Secondary outcomes were stage 5 CKD (eGFR <15 ml/min/1.73 m2, on dialysis for over 3 months or who had received a kidney transplant), proteinuria (urine protein/creatinine ratio >50 mg/mmol), and biopsy-confirmed HIV-associated nephropathy (HIVAN), focal segmental glomerulosclerosis (FSGS) or arterionephrosclerosis. Multivariable robust Poisson regression estimated the effect of region of African ancestry on kidney disease outcomes.
Findings
Of the 2468 participants (mean age 48.1 [SD 9.8] years, 62% female), 193 had renal impairment, 87 stage 5 CKD, 126 proteinuria, and 43 HIVAN/FSGS or arterionephrosclerosis. After adjusting for demographic characteristics, HIV and several CKD risk factors and with East African ancestry as referent, West African ancestry was associated with renal impairment (prevalence ratio [PR] 2.06 [95% CI 1.40–3.04]) and stage 5 CKD (PR 2.23 [1.23–4.04]), but not with proteinuria (PR 1.27 [0.78–2.05]). West African ancestry (as compared to East/South African ancestry) was also strongly associated with a diagnosis of HIVAN/FSGS or arterionephrosclerosis on kidney biopsy (PR 6.44 [2.42–17.14]).
Interpretation
Our results indicate that people of West African ancestry with HIV are at increased risk of kidney disease. Although we cannot rule out the possibility of residual confounding, geographical region of origin appears to be a strong independent risk factor for CKD as the association did not appear to be explained by several demographic, HIV or renal risk factors.
Keywords: Chronic kidney disease, Africa, Diaspora, Apolipoprotein L1, HIV, Epidemiology, HIVAN
Research in context.
Evidence before this study
Chronic kidney disease (CKD) is an important complication of Human Immunodeficiency Virus (HIV) infection, particularly in people of African ancestry. Among African people with HIV, West-Africans appear at greatest risk of kidney disease although CKD estimates are limited by heterogeneity of studies and measures to define CKD, and availability of data on HIV and traditional CKD risk factors.
Added value of the study
We conducted a study in people of African ancestry with HIV in a single healthcare system. We confirmed that West African ancestry was associated with an increased risk of renal impairment (estimated glomerular filtration rate of <60 mL/min/1.73 m2) and stage 5 CKD (eGFR <15 ml/min/1.73 m2 or requiring permanent renal replacement therapy), and that this was not explained by differences in several demographic, HIV or traditional CKD risk factors. Moreover, participants of West African ancestry were six-fold more likely to be diagnosed with HIV associated nephropathy (HIVAN), focal segmental glomerulosclerosis (FSGS), or arterionephrosclerosis, glomerular pathologies that have been associated with coding variants of the apolipoprotein L1 (APOL1) gene that are highly prevalent in populations of West African ancestry.
Implications of all the available evidence
HIVAN/FSGS disproportionally affects people of West-African ancestry and this may contribute to the high burden of kidney disease in this population. These data suggest that early HIV diagnosis and prompt initiation of ART, already recommended to reduce morbidity and mortality in all people with HIV, may be an important CKD prevention strategy, particularly in populations of West African ancestry.
Alt-text: Unlabelled box
1. Introduction
Chronic kidney disease (CKD) is a common condition characterized by gradual loss of kidney function over time, leading to increased morbidity and mortality. CKD is ranked as the 12th leading cause of death globally, and is particularly common among people living in sub-Saharan Africa [1]. With a population of over one billion [2], sub-Saharan Africa is a vast and heterogenous region with marked genetic diversity, in which urbanization and economic progress contribute to a rapid transition in disease-burden from communicable diseases and childhood illnesses to chronic, non-communicable diseases, including CKD.
HIV is also highly prevalent in sub-Saharan Africa, with the greatest prevalence in East and Southern Africa [3]. The risk of acute kidney injury and CKD is increased in people with HIV; these conditions frequently have a multifactorial etiology including: chronic immune activation as a direct effect of the HIV virus; drug toxicity from antiretroviral therapy (ART) or agents to treat or prevent opportunistic infections; and age-related comorbid kidney disease due to diabetes, hypertension, and cardiovascular disease for example [4]. In addition, common coding variants of apolipoprotein L1 (APOL1) gene were found to be strongly associated with some subsets of CKD in people of African ancestry, especially HIV-associated nephropathy (HIVAN, odds ratio [OR] 29 in African Americans, 89 in South Africans), focal segmental glomerulosclerosis (FSGS, OR 17), and arterionephrosclerosis (OR 2–4) [5], [6], [7], [8]. APOL1 renal risk variants are also associated with steeper decline in estimated glomerular filtration rate (eGFR) [9] and non-diabetic end-stage kidney disease (ESKD, OR 7) [8]. These APOL1 risk variants are found almost exclusively in people of African ancestry, with the highest frequencies reported in West Africans and the lowest in East Africans [4]. Within West Africa, the frequency of the APOL1 risk variants is particularly high among the Yoruba and Igbo-Edo speaking populations of Nigeria, and the Asante in Ghana [5,[7], [8], [9]].
There remains a paucity of reliable population-based data on the prevalence of CKD in African people with HIV. A recent systematic review of CKD in Africans with HIV [10] and a study from the UK Collaborative HIV Cohort (UK CHIC) Study [11] reported the highest prevalence of CKD in people from West Africa. However, the systematic review highlighted several weaknesses in the design of the included studies, a lack of standardized measures of eGFR, and differences in the populations studied and HIV care provided. The UK CHIC study was limited by a lack of information on hypertension, diabetes, and cardiovascular disease, all of which are known risk factors for CKD [11].
In the present study, performed in a setting of universal and free access to healthcare, we sought to further investigate the relationship between region of African ancestry and markers of kidney disease: renal impairment, stage 5 CKD and proteinuria, with adjustment for demographic, HIV, and CKD-associated parameters. As HIVAN is an important cause of CKD in black people with HIV [12], we hypothesized that West African ancestry, a region with the highest prevalence of APOL1 risk alleles, would be associated with renal impairment (particularly stage 5 CKD), proteinuria and HIVAN/FSGS on kidney biopsy.
2. Methods
2.1. Subject enrolment and demographic data
The genetic markers of kidney disease progression in people of African ancestry (GEN-AFRICA) study is a cross-sectional study designed to investigate genetic factors associated with CKD in the United Kingdom. The GEN-AFRICA study enrolled consenting adults of African ancestry with HIV at 15 HIV clinics and three dialysis/kidney transplantation centers across England between May 2018 and February 2020. There were no exclusion criteria. Demographic data, including country of birth of both parents, clinical information, HIV status and comorbid conditions, were collected from participants using questionnaires and corroborated through review of clinical records. Laboratory data, including nadir and most recent CD4 cell count, viral hepatitis status (hepatitis B surface antigen and anti-hepatitis C antibody) and HIV viral load were obtained from electronic patient records. Renal function, including serum creatinine and urine protein creatinine ratio (uPCR), was measured in local laboratories. If a renal biopsy had ever been performed, a copy of the histopathology report, where available, was obtained. The study was approved by an NHS Research Ethics Committee and Health Research Authority (18/LO/0234 and 239895).
The exposure in the presented analyses was region of sub-Saharan African ancestry (East, South, Central and West Africa) as defined by the African Union [13], with the exception that Angola was included in the Central rather than South region. Participants of Caribbean, North African, or mixed African ancestry were excluded. eGFR was calculated utilizing the CKD Epidemiology Collaboration (CKD-EPI-Cr) equation [14] with and without application of the correction factor for black ethnicity The primary outcome was renal impairment was defined as an eGFR <60 mL/min/1.73 m2 [15,16]. Participants were stratified by eGFR based on Kidney Disease: Improving Global Outcomes (KDIGO) CKD guidelines [17] and those with eGFR <15 mL/min/1.73 m2 who were on dialysis for over three months or who had received a kidney transplant were categorized as having stage 5 CKD. Renal biopsy reports were reviewed and adjudicated by a renal physician (JB) and, in case of discrepancy, a histopathologist to identify cases of HIVAN, (primary) FSGS and arterionephrosclerosis, a common cause of CKD in people of African ancestry [18]. Diabetes mellitus and hypertension were predominantly self-reported diagnoses; medical records were reviewed for those reporting but not on treatment for these conditions to verify the diagnosis. Additionally, diabetes cases were ascertained through review of medical records of those with glycosuria.
2.2. Statistical methods
Baseline characteristics of the study population, stratified by region of ancestry and by eGFR (greater or less than 60 mL/min/1.73m2), were compared using Х2 for categorical variables, and Kruskal-Wallis tests or ANOVA for continuous variables, as appropriate. Robust Poisson regression was used to quantify the association between each covariate and kidney disease status. It was decided a priori that age and sex would be included in the minimally adjusted model, followed by HIV factors (nadir and current CD4 cell count, and prior AIDS). The fully adjusted model also included renal factors (diabetes and cardiovascular disease). As hypertension is on the causal kidney disease pathway, hypertension was excluded as a factor in the primary and secondary outcomes analyses (we conducted sensitivity analyses that included hypertension in the multivariable models). The association between region of ancestry and secondary outcomes: (1) stage 5 CKD, (2) proteinuria (uPCR >50 mg/mmol [approximately 500 mg/g], excluding those with stage 5 CKD) and (3) biopsy-confirmed HIVAN/FSGS/arterionephrosclerosis was also investigated. East African region of ancestry was used as referent for all analyses except for biopsy-confirmed HIVAN/FSGS/arterionephrosclerosis, where East and South African ancestry were combined as referent. As diabetic nephropathy is an important cause of CKD, we performed a further sensitivity analysis excluding participants with diabetes. Finally, interaction analyses were performed to examine whether diabetes, hypertension or cardiovascular disease modified the association between region of African ancestry and renal impairment. All statistical analyses were done using STATA v16 (StataCorp, College Station, Tx). The study was reported according to STROBE guidelines.
2.3. Role of funding sources
This study was supported by the Medical Research Council (UK) Confidence in Concept scheme (MC_PC_17164). The project has been supported in part the National Institutes of Health and the National Cancer Institute Intramural Research Program (CAW).
3. Results
Of the 3026 individuals enrolled in the GEN-AFRICA cohort, 2468 (81.6%) reported sub-Saharan African ancestry with both parents born in the same sub-Saharan region and were included in the current analyses. The characteristics of these participants at the time of enrolment are shown in Table 1. Participants were predominantly women (62%) and had a mean age of 48.1 (SD 9.8) years, and generally long-standing and well-controlled HIV. The prevalence of diabetes, cardiovascular disease and proteinuria was similar across all four sub-Saharan African regions while hypertension was more common among Central and West Africans. Among the 2,281participants with proteinuria data (and no stage 5 CKD), 77.9%, 16.7%, 5.5% had no proteinuria, uPCR 15–49 mg/mmol, and uPCR>50 mg/mmol, respectively. Exposure to antiretroviral drugs was generally similar across all regions (Table S3).
Table 1.
Demographic and clinical characteristics of the study participants stratified by African region of ancestry.
| Region of African Ancestry |
||||||||
|---|---|---|---|---|---|---|---|---|
| All | East | South | Central | West | p value | |||
| N = 2468 | N = 585 | N = 810 | N = 168 | N = 905 | ||||
| Age (years) | Mean (SD) | 48.1 (9.8) | 49.1 (9.7) | 48.3 (9.9) | 47.8 (10.2) | 47.2 (9.8) | 0.002 | |
| Female sex | n (%) | 1531 (62.0) | 377 (64.4) | 562 (69.4) | 95 (56.5) | 497 (54.9) | <0.001 | |
| Time since HIV diagnosis (years) | Mean (SD) | 14.1 (6.3) | 16.6 (7.2) | 14.9 (5.3) | 14.5 (6.3) | 11.5 (5.6) | <0.001 | |
| Nadir CD4 (cells/mm3) | Median (IQR) | 194 (78–329) | 182 (80–319) | 200 (85–335) | 182 (47–302) | 196 (76–351) | 0.21 | |
| Current CD4 (cells/mm3) | Median (IQR) | 551 (396–719) | 534 (376–706) | 599 (430–763) | 511 (355–645) | 531 (390–705) | <0.001 | |
| HIV viral load (<200 copies/mL) | n (%) | 2302 (93.3) | 553 (94.5) | 766 (94.6) | 152 (90.5) | 831 (91.8) | 0.03 | |
| On ART | n (%) | 2444 (99.0) | 581 (99.3) | 806 (99.5) | 167 (99.4) | 890 (98.3) | 0.07 | |
| Time since ART initiation (years) | median (IQR) | 10.9 (6.4–14.9) | 12.6 (7.5–18.1) | 12.4 (7.5–15.5) | 11.4 (6.9–15.8) | 9 (5.1–12.6) | <0.001 | |
| Mode of HIV acquisition | <0.001 | |||||||
| Heterosexual | n (%) | 2150 (87.1) | 484 (82.7) | 724 (89.4) | 151 (89.9) | 791 (87.4) | ||
| MSM | n (%) | 32 (1.3) | 8 (1.4) | 7 (0.9) | 0 (0.0) | 17 (1.9) | ||
| Vertical | n (%) | 107 (4.3) | 26 (4.4) | 37 (4.6) | 5 (3.0) | 39 (4.3) | ||
| Blood products | n (%) | 20 (0.8) | 4 (0.7) | 3 (0.4) | 1 (0.6) | 12 (1.3) | ||
| Unknown | n (%) | 159 (6.4) | 63 (10.8) | 39 (4.8) | 11 (6.5) | 46 (5.1) | ||
| Prior AIDS | n (%) | 615 (25.7) | 169 (29.9) | 231 (29.2) | 36 (22.0) | 179 (20.5) | <0.001 | |
| HBsAg positive | n (%) | 151 (6.2) | 25 (4.4) | 33 (4.1) | 17 (10.2) | 76 (8.5) | <0.001 | |
| Anti-HCV positive* | n (%) | 30 (1.3) | 4 (0.7) | 9 (1.2) | 7 (4.3) | 10 (1.1) | 0.003 | |
| Diabetes | n (%) | 249 (10.2) | 63 (10.9) | 82 (10.2) | 15 (8.9) | 89 (9.9) | 0.88 | |
| Hypertension | n (%) | 826 (33.5) | 184 (31.6) | 240 (29.7) | 62 (36.9) | 340 (37.6) | 0.003 | |
| Cardiovascular diseaseƗ | n (%) | 109 (4.4) | 26 (4.4) | 32 (4) | 12 (7.2) | 29 (4.3) | 0.32 | |
| BMI (kg/m2) | Mean (SD) | 29.5 (6.2) | 29.0 (5.9) | 30.7 (6.4) | 29.7 (5.7) | 29.6 (5.7) | <0.001 | |
| eGFR (60 mL/min/1.73m2⁎⁎) | <0.001 | |||||||
| >90 | n (%) | 1605 (65.0) | 410 (70.1) | 550 (67.9) | 115 (68.5) | 530 (58.6) | ||
| 60–90 | n (%) | 670 (27.1) | 140 (23.9) | 217 (26.8) | 42 (25.0) | 271 (29.9) | ||
| 30–59 | n (%) | 92 (3.7) | 16 (2.7) | 26 (3.2) | 4 (2.4) | 46 (5.1) | ||
| 15–29 | n (%) | 14 (0.6) | 3 (0.5) | 3 (0.4) | 2 (1.2) | 6 (0.7) | ||
| <15 (Stage 5 CKD⁎⁎⁎) | n (%) | 87 (3.5) | 16 (2.7) | 14 (1.7) | 5 (3.0) | 52 (5.7) | ||
| uPCR^ (mg/mmol) | 0.90 | |||||||
| <15 | n (%) | 1776 (77.9) | 429 (77.6) | 584 (77.8) | 123 (77.9) | 640 (78.1) | ||
| 15–49 | n (%) | 380 (16.7) | 100 (18.1) | 120 (16.0) | 26 (16.5) | 134 (16.4) | ||
| 50–99 | n (%) | 65 (2.9) | 11 (2.0) | 23 (3.1) | 5 (3.2) | 26 (3.2) | ||
| ≥100 | n (%) | 60 (2.6) | 13 (2.4) | 24 (3.2) | 4 (2.5) | 19 (2.3) | ||
ART=antiretroviral therapy; MSM=men who have sex with men; AIDS=acquired immunodeficiency syndrome; HBsAg=hepatitis B surface antigen; Anti-HCV=hepatitis C virus antibody; BMI=body mass index; uPCR=urine protein/creatinine ratio; SD=standard deviation; IQR=interquartile range.
There are no missing data for age, sex, mode of HIV acquisition, ART and eGFR; 0.2% of participants lack data for time since HIV diagnosis, 0.3% for current CD4 cell count, 5.5% for nadir CD4 cell count, 8.9% for time since ART initiation, 3% of for prior AIDS, 0.9% for diabetes, 0.2% for hypertension, 1.4% for HBsAg, 2.8% for anti-HCV, and 5% for uPCR (mainly those with stage 5 CKD).
ƗCardiovascular disease = composite of any previous history of myocardial infarction, coronary artery disease, peripheral vascular disease, stroke, heart failure and cardiomyopathy.
Hepatitis C RNA: detectable N = 4, undetectable N = 24, not available N = 2.
estimated glomerular filtration rate calculated with CKD EPI formula with correction of black ethnicity included.
Stage 5 CKD=eGFR <15 mL/min/1.73m2 and those on dialysis for over three months or had a kidney transplant.
uPCR does not include participants with stage 5 CKD (eGFR <15 mL/min/1.73m2 and those on dialysis or had a kidney transplant).
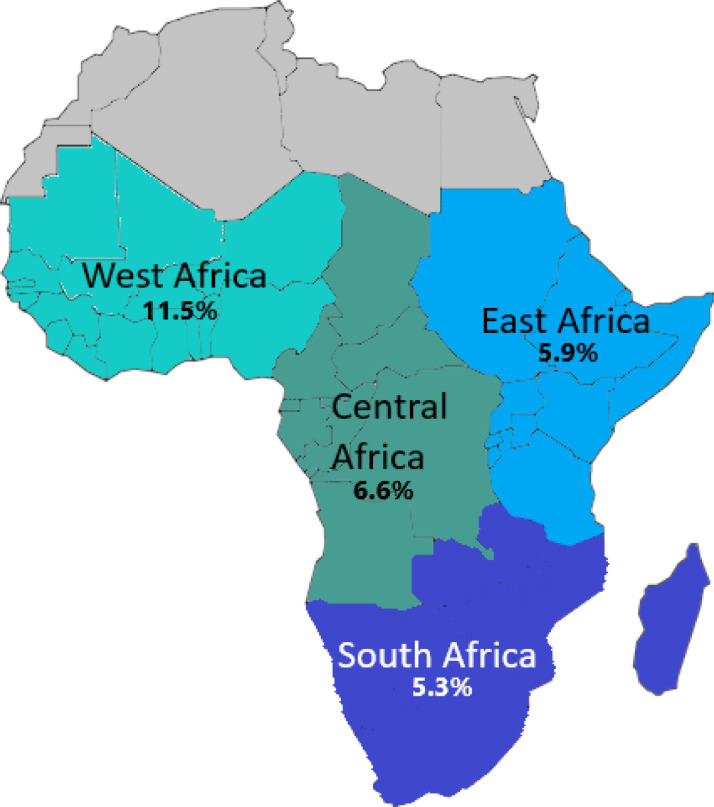
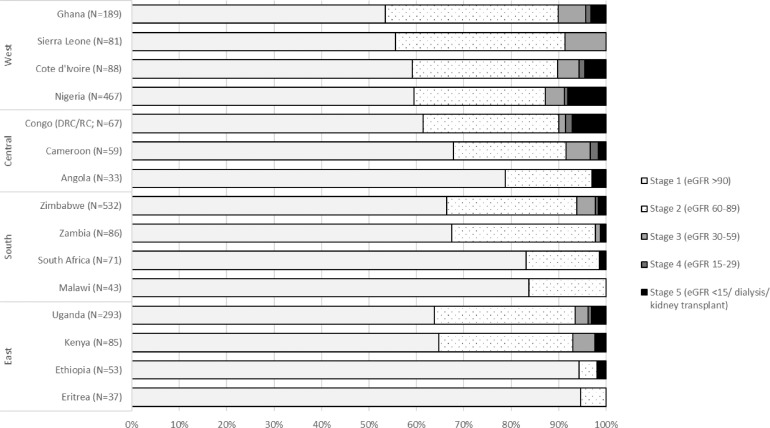
One hundred and ninety-three participants (7.8%) had renal impairment, with the highest prevalence in those of West African ancestry (11.5%) and the lowest in those of South African ancestry (5.3%, Fig. 1). Among participants with renal impairment, 89.1% had hypertension and 26.6% had diabetes. Overall prevalence of hepatitis B (surface antigen) and hepatitis C (anti-HCV) was 6.2% and 1.3% respectively; anti-HCV was more common in those with renal impairment (4.4% vs 1.0%). The characteristics of those with and without renal impairment are shown in Table S2. When stratified by ancestral country, participants with the highest prevalence of renal impairment mostly originated from West Africa, with rates of 13%, 10%, 10% and 9% in those with ancestral roots in Nigeria, Cote d'Ivoire, Ghana and Sierra Leone respectively (Fig. 2, Table S7). Forty-three participants had a biopsy-confirmed diagnosis of HIVAN (N = 36), FSGS (N = 4) or arterionephrosclerosis (N = 3); 1 (2.3%), 6 (14%), 4 (9.3%) and 32 (74.4%) of these occurred in individuals of East, South, Central and West African ancestry (Fig. S1, Table S1).
Fig. 1.
Regions of sub-Saharan Africa (East, Central, West, South) and prevalence of renal impairment (eGFR <60 ml/min/1.73m2) by region of ancestry of the study participants.
Fig. 2.
Proportion of participants with eGFR stages 1–5, by country of ancestry
Proportion of participants in each country of ancestry with estimated glomerular filtration rate >90, 60–89, 30–59, 15–29 and <15 mLmin/1.73 m2. Data are restricted to participants with both parents born in the same country, and to countries with at least N = 10 individuals.
In univariable analysis, region of African ancestry, age, female sex, nadir CD4 count, current CD4 count, mode of HIV acquisition, prior AIDS, anti-HCV, hypertension, diabetes, and cardiovascular disease were all associated with renal impairment. In the fully adjusted model, participants of West African ancestry had double the odds (PR 2.06, 95% confidence interval [CI] 1.40 – 3.04) of renal impairment as compared to those of East African ancestry which was quite similar to the univariable estimate. Age, current and nadir CD4 cell count, anti-HCV, prior AIDS, diabetes, and cardiovascular disease also remained associated with renal impairment in these adjusted analyses (Table 2). When hypertension was included in the final model for renal impairment, the association between renal impairment and West African ancestry attenuated but remained significant (PR 1.68, 95% CI 1.16–2.44).
Table 2.
Factors associated with renal impairment (eGFR <60 mL/min/1.73m2), n = 193.
| Univariate |
Adjusted for age and sex |
Adjusted for HIV factors |
Adjusted for renal factors |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PR | 95% CI | p value | PR | 95% CI | p value | PR | 95% CI | p value | PR | 95% CI | p value | |||
| African Region of Ancestry | <0.001 | <0.001 | <0.001 | <0.001 | ||||||||||
| East | 1 | 1 | 1 | 1 | ||||||||||
| South | 0.89 | 0.58–1.37 | 0.59 | 0.94 | 0.61–1.44 | 0.76 | 0.87 | 0.54–1.41 | 0.58 | 0.90 | 0.56–1.44 | 0.67 | ||
| Central | 1.09 | 0.57–2.11 | 0.79 | 1.10 | 0.58–2.10 | 0.76 | 0.85 | 0.40–1.82 | 0.68 | 0.69 | 0.29–1.68 | 0.41 | ||
| West | 1.92 | 1.33–2.78 | 0.001 | 2.04 | 1.12–2.93 | <0.001 | 2.00 | 1.35–2.96 | 0.001 | 2.06 | 1.40–3.04 | <0.001 | ||
| Age (per 1 year increment) | 1.05 | 1.04–1.07 | <0.001 | 1.05 | 1.04–1.07 | <0.001 | 1.05 | 1.03–1.06 | <0.001 | 1.04 | 1.02–1.06 | <0.001 | ||
| Sex (Female vs. male) | 0.62 | 0.47–0.81 | <0.001 | 0.77 | 0.53–1.01 | 0.06 | 0.97 | 0.71–1.31 | 0.83 | 0.97 | 0.72–1.32 | 0.87 | ||
| Time since HIV diagnosis (5 years increments) | 1.05 | 0.95–1.17 | 0.31 | |||||||||||
| Nadir CD4 (50 cell/mm3 increment) | 0.88 | 0.8/3–0.93 | <0.001 | 0.94 | 0.89–0.99 | 0.03 | 0.95 | 0.90–1.00 | 0.05 | |||||
| Current CD4 (50 cell/mm3 increment) | 0.93 | 0.90–0.97 | <0.001 | 0.96 | 0.92–1.00 | 0.06 | 0.95 | 0.92–0.99 | 0.007 | |||||
| On ART | 0.62 | 0.21–1.81 | 0.38 | |||||||||||
| HIV viral load (<200 copies/mL) | 1.09 | 0.62–1.91 | 0.77 | |||||||||||
| Mode of HIV Acquisition | 0.26 | |||||||||||||
| Heterosexual | 1 | |||||||||||||
| MSM | 1.61 | 0.64–4.07 | 0.32 | |||||||||||
| Vertical | 0.48 | 0.19–1.27 | 0.14 | |||||||||||
| Blood products | 1.93 | 0.67–5.54 | 0.22 | |||||||||||
| Unknown | 1.21 | 0.73–2.01 | 0.45 | |||||||||||
| Prior AIDS | 1.76 | 1.33–2.32 | <0.001 | 1.66 | 1.19–2.29 | 0.003 | 1.52 | 1.09–2.11 | 0.01 | |||||
| HBsAg (positive) | 0.96 | 0.53–1.73 | 0.89 | |||||||||||
| Anti-HCV (Positive) | 3.63 | 1.97–6.69 | <0.001 | 3.48 | 1.84–6.57 | <0.001 | 2.97 | 1.44–6.14 | 0.003 | |||||
| Diabetes | 3.20 | 2.38–4.30 | <0.001 | 2.15 | 1.52–3.03 | <0.001 | ||||||||
| Hypertension | 16.24 | 10.40–25.35 | <0.001 | |||||||||||
| Cardiovascular disease | 3.83 | 2.71–5.40 | <0.001 | 2.94 | 1.98–4.35 | <0.001 | ||||||||
| BMI (kg/m2) | ||||||||||||||
| <18.5 | 1.64 | 0.44–6.12 | 0.46 | |||||||||||
| 18.5–24.99 | 1 | |||||||||||||
| 25–30 | 0.82 | 0.56–1.91 | 0.30 | |||||||||||
| >=30 | 0.84 | 0.59–1.20 | 0.34 | |||||||||||
ART=antiretroviral therapy; MSM=men who have sex with men; AIDS=acquired immunodeficiency syndrome; HBsAg=hepatitis B surface antigen; Anti-HCV=hepatitis C virus antibody; BMI=body mass index; PR=prevalence ratio; CI=confidence interval.
In secondary analyses, West African ancestry was also associated with stage 5 CKD (PR 2.23, 95% CI 1.23–4.04) (Tables 3A and S4) but not with proteinuria (excluding stage 5 CKD, Tables 3A and S5). However, when hypertension was included in the final model for stage 5 CKD, West African ancestry was no longer associated with stage 5 CKD (PR 1.49, 95% CI 0.89–2.52) (Table 3B).
Table 3.
Secondary outcomes (A) and sensitivity analyses (B).
| Univariate |
Multivariable Х |
||||||
|---|---|---|---|---|---|---|---|
| PR | 95% CI | p value | PR | 95% CI | p value | ||
| A.Secondary Analyses | |||||||
| Stage 5 CKD*(n = 87) | |||||||
| African Region of Ancestry | <0.001 | 0.001 | |||||
| East | 1 | 1 | |||||
| South | 0.63 | 0.31–1.28 | 0.21 | 0.69 | 0.31–1.54 | 0.36 | |
| Central | 1.09 | 0.40–2.93 | 0.87 | 1.03 | 0.34–3.13 | 0.96 | |
| West | 2.11 | 1.21–3.64 | 0.01 | 2.23 | 1.23–4.04 | 0.009 | |
| Biopsy-confirmed HIVAN/FSGS and arterionephrosclerosis (n = 43) | |||||||
| African Region of Ancestry | <0.001 | 0.001 | |||||
| East/South | 1 | 1 | |||||
| Central | 4.74 | 1.40–16.04 | 0.01 | 4.47 | 1.20–16.69 | 0.03 | |
| West | 7.05 | 3.12–15.90 | <0.001 | 6.44 | 2.42–17.14 | <0.001 | |
| Proteinuria†(n = 126) | |||||||
| African Region of Ancestry | 0.47 | ||||||
| East | 1 | ||||||
| South | 1.43 | 0.91–2.37 | 0.11 | ||||
| Central | 1.31 | 0.62–2.77 | 0.48 | ||||
| West | 1.27 | 0.78–2.05 | 0.34 | ||||
| B. Sensitivity Analyses | |||||||
| eGFR<60 ml/min/1.72m2 with additional adjustment for hypertension (n = 193) | |||||||
| African Region of Ancestry | <0.001 | <0.001 | |||||
| East | 1 | 1 | |||||
| South | 0.89 | 0.58–1.37 | 0.59 | 0.93 | 0.59–1.47 | 0.76 | |
| Central | 1.09 | 0.57–2.11 | 0.79 | 0.67 | 0.30–1.47 | 0.32 | |
| West | 1.92 | 1.33–2.78 | 0.001 | 1.68 | 1.16–2.44 | 0.006 | |
| Stage 5 CKD*with additional adjustment for hypertension (n = 87) | |||||||
| African Region of Ancestry | <0.001 | 0.03 | |||||
| East | 1 | 1 | |||||
| South | 0.63 | 0.31–1.28 | 0.21 | 0.59 | 0.28–1.27 | 0.18 | |
| Central | 1.09 | 0.40–2.93 | 0.87 | 0.73 | 0.26–2.05 | 0.55 | |
| West | 2.11 | 1.21–3.64 | 0.01 | 1.49 | 0.89–2.52 | 0.13 | |
| eGFR without correction for ethnicity К (n = 193) | |||||||
| African Region of Ancestry | <0.001 | <0.001 | |||||
| East | 1 | 1 | |||||
| South | 1.12 | 0.80–1.57 | 0.51 | 1.10 | 0.77–1.58 | 0.60 | |
| Central | 1.16 | 0.69–1.96 | 0.58 | 1.01 | 0.56–1.82 | 0.98 | |
| West | 1.89 | 1.40–2.55 | <0.001 | 2.03 | 1.49–2.75 | <0.001 | |
| Participants without diabetes (n = 2197) | |||||||
| African Region of Ancestry | <0.001 | <0.001 | |||||
| East | 1 | 1 | |||||
| South | 0.87 | 0.51–1.47 | 0.6 | 0.87 | 0.49–1.54 | 0.64 | |
| Central | 1.42 | 0.70–2.91 | 0.34 | 1.08 | 0.49–2.38 | 0.85 | |
| West | 2.13 | 1.37–3.32 | 0.001 | 2.11 | 1.32–3.36 | 0.002 | |
ART=antiretroviral therapy; MSM=men who have sex with men; AIDS=acquired immunodeficiency syndrome; HBsAg=hepatitis B surface antigen; Anti-HCV=hepatitis C virus antibody; BMI=body mass index; PR=prevalence ratio; CI=confidence interval.
К eGFR based on CKD-EPI equation, excluding correction for African American ethnicity.
Multivariable model for Stage 5 CKD and for eGFR without correction for ethnicity adjusted for age, sex, nadir CD4, current CD4, diabetes, cardiovascular disease and hepatitis C virus antibody; multivariable model for biopsy-confirmed HIVAN/FSGS and arterionephrosclerosis adjusted for age, sex, nadir CD4, current CD4, cardiovascular disease and hepatitis C virus antibody; multivariable model for eGFR<60 ml/min/1.72m2 with adjusting for hypertension adjusted for age, sex, nadir CD4, current CD4, prior AIDS, diabetes, hypertension, cardiovascular disease and hepatitis C virus antibody; multivariable model for individuals without diabetes adjusted for age, sex, nadir CD4, current CD4, prior AIDS, cardiovascular disease and hepatitis C virus antibody.
Stage 5 CKD=eGFR <15 mL/min/1.73 m2 and those on dialysis for over three months or had a kidney transplant.
Proteinuria=uPCR >50 mg/mmol [approximately 500 mg/g] (excluding those with Stage 5 CKD).
Compared to East and South African ancestry, West African ancestry was also strongly associated with biopsy-confirmed HIVAN/FSGS/arterionephrosclerosis (PR 6.44, 95% CI 2.42–17.14) (Tables 3A and S6). In additional sensitivity analyses, the risk of renal impairment remained similar when correction for ethnicity was excluded in eGFR calculations, and in models that excluded participants with diabetes (Table 3B). There was no evidence of interaction between region of African ancestry and renal impairment with diabetes (p values 0.12–0.87), hypertension (p values 0.25–0.72) or cardiovascular disease (p values 0.09–0.91).
4. Discussion
To our knowledge, GEN-AFRICA is the first pan-African diaspora cohort, allowing for direct comparison of markers of kidney disease, CKD risk factors and a biopsy diagnosis of HIVAN/FSGS and arterionephrosclerosis in the setting of HIV across regions of African ancestry. Consistent with the findings of a recent meta-analysis [10] and the UK CHIC study [11], the highest prevalence of renal impairment was observed in individuals of West African ancestry and the lowest prevalence in those from the South African region. West Africans remained at higher risk of renal impairment and stage 5 CKD after adjusting for demographic, HIV, and CKD risk factors (except for hypertension, which is on the causal pathway for CKD). West African ancestry was also strongly associated with having HIVAN/FSGS and arterionephrosclerosis. By contrast, although proteinuria was common, we observed no association between region of ancestry and proteinuria.
The increased risk of renal impairment in West Africans may relate to the high prevalence of renal risk variants (G1, G2) of the APOL1 gene that confer protection against trypanosomiasis but increase the risk of glomerular scarring, especially in the setting of viral infections such as HIV [6]. As Nigerian ancestry was predominant among the West Africans enrolled in our cohort, the observed increased risk of renal impairment among West Africans may relate to the high prevalence of APOL1 G1/G2 variants in this population. Indeed, a majority (over 70%) of HIVAN/FSGS/arterionephrosclerosis, each of which has been associated with APOL1 high risk genotypes, was diagnosed in West Africans, mostly of Nigerian ancestry. The greater burden of renal impairment and stage 5 CKD in those of West African ancestry may, at least in part, be due to HIVAN/FSGS. As ART, a higher CD4 cell count and suppressed HIV viral load have all been associated with a reduced incidence of HIVAN [18,19], our findings suggest that early HIV diagnosis followed by prompt initiation of fully suppressive ART may be an important CKD prevention strategy.
Contrasting with our findings, a recent study of kidney disease in predominantly HIV negative Africans found the lowest prevalence of CKD, defined as an eGFR <60 mL/min/1.73 m2 and/or albuminuria >3 mg/mmol, in West Africans and highest prevalence in South Africans [20]. This was a large population-based study of CKD prevalence (AWI-Gen study) conducted in six discrete locations in East, South and West Africa. The AWI-Gen study recruited from two rural areas in West Africa: Burkina Faso (Nanoro) and Ghana (Navrango), each with a known low prevalence of HIV, CKD and APOL1 risk variants [5,21]. This study is therefore unable to account for differences in CKD prevalence in relation to regional variability in the prevalence of APOL1 risk variants. Rather, the higher prevalence of CKD in the South African sites may reflect a different stage of epidemiological transition from rural to urban lifestyle; the South African sites in AWI-Gen were semi-rural to urban areas with higher prevalence of CKD risk factors including diabetes and hypertension.
Proteinuria was not associated with region of African ancestry. This finding was surprising given that studies have shown APOL1 renal risk genotypes to be associated with more frequent and earlier onset of proteinuria [22], [23], [24], [25]. Proteinuria is an important risk factor for CKD progression with a higher prevalence generally among people of African ancestry [26,27] and it is likely that participants with severe proteinuria have progressed to stage 5 CKD in our study. As we excluded participants with Stage 5 CKD from the proteinuria analyses, this may explain the lack of association with region of African ancestry. As most participants had well controlled HIV, it is possible that the lack of association between proteinuria and CKD is due to past rather than current renal injury (e.g. prior to HIV diagnosis/control). It is also possible that the HIV virus itself, exposure to ART or other medications, or traditional CKD risk factors such as diabetes and hypertension were the predominant causes of proteinuria rather than APOL1-associated glomerular disease.
The strengths of this study include the large number of participants who are representative of people of African ancestry currently living with HIV in the UK. In addition, our study included a substantial number (n = 87) of people with stage 5 CKD who, in the absence of renal replacement therapy, would be missing from most studies conducted in Africa. Consistent with other studies from sub-Saharan Africa, our study included a higher proportion of females (by contrast, most US studies have a predominance of African American males). The limitations include the cross-sectional design and use of a single creatinine time point to calculate eGFR which may not accurately reflect CKD status; however, as almost all participants were clinically well and recruited during routine outpatient visits, it is likely that most had stable kidney function. The CKD-EPI equation, which is a creatinine-based equation, has not been widely validated in African populations, and the use of the adjustment for ethnicity, while arguable given the high BMI of our participants, remains contentious [27]; this issue is currently being investigated by the African Research into Kidney Diseases (ARK) study [28]. However, in our study, analyses of stage 5 CKD support the findings of the primary outcome suggesting that the association between region of ancestry and renal impairment is real. We did not investigate the associations between specific ART medications and CKD as tenofovir disoproxil fumarate (TDF), atazanavir and lopinavir are generally avoided in people with CKD [11,29], and have no information on markers of renal tubular (dys)function, hence we are unable to account for the effects of some ART medications that may lead to reduced tubular creatinine secretion [30]. We also have incomplete data on anti-hypertensive medications and are unable to exclude that differential use of angiotensin converting enzyme inhibitors or angiotensin II receptor antagonist may have affected the severity of proteinuria in different regions.
We lacked information on other factors that may contribute to renal impairment in Africa including infections such as malaria and schistosomiasis, environmental exposure to heavy metals, or data on current use of non-steroidal anti-inflammatory drugs and prior use of antimicrobial treatments and prophylaxis. A small number of recruitment centers were renal centers, and thus our sample includes a higher proportion of people with stage 5 CKD, meaning our study is unable to provide true prevalence estimates. Finally, although we had a sizeable cohort with broad representation from across sub-Saharan Africa, the Central African cohort was small, the East, South and West African regions were over-represented by people of Ugandan, Zimbabwean and Nigerian ancestry, and there was substantial heterogeneity in prevalence of renal impairment and stage 5 CKD within regions. Our data show that in a setting where healthcare is universally accessible, there was an increased burden of kidney disease among those of West African ancestry. Consistent with the known distribution of APOL1 risk alleles, we observed a particularly strong association between West African ancestry and HIVAN/FSGS and arterionephrosclerosis. Genetic analyses in the GEN-AFRICA cohort are currently being undertaken; if these confirm that APOL1 high risk genotypes are a major driver of the increased risk of kidney disease in West Africans with HIV, early HIV diagnosis and prompt initiation of ART will be even more important CKD prevention strategies. This cohort is well placed to help further examine the complex interactions between genes and the environment that ultimately promote the development of CKD.
Contributors
The study was designed by FAP. LH, JF, JB, AC, RV, RJ, DP, MH, RH, JB and FAP were site principal investigators and coordinated recruitment and data collection at their sites. BSS, EBR and LC assisted with logistic and governance aspects. JB preformed a review of all kidney biopsy reports with assistance from Catherine Horsfield. RH and FAP performed the analyses with input from CAS and CAW. RH, KB, CAS, CAW and FAP interpreted the findings. RH wrote the first draft of the manuscript with input from CAS, CAW and FAP. RH and FP verified the underlying data. All authors revised and approved the final version of the manuscript.
Data sharing statement
The database contains personal and sensitive information and is therefore not publicly available. Access to the study data and/or samples is governed by the National Health Service data access policy and those of King's College Hospital NHS Foundation Trust, the study sponsor. The Gen-AFRICA cohort is open to collaborations, and all requests from researchers who meet the criteria for access to fully anonymized patient level data will be considered. Concepts can be submitted for review to the principal investigator (Prof. Frank Post; email: frank.post@kcl.ac.uk).
Funding
This study was supported by the Medical Research Council (UK) Confidence in Concept scheme (MC_PC_17164). The project has been supported in part the National Institutes of Health and the National Cancer Institute Intramural Research Program (CAW) and under contract HHSN26120080001E. The content of this publication does not necessarily reflect the view or policy of the Department of Health and Human Services, nor does mention of trade names, commercial products or organizations imply endorsement by the government.
Declaration of Competing Interest
Dr Hung has nothing to disclose.
Dr Santana-Suarez has nothing to disclose.
Dr Binns-Roemer has nothing to disclose.
Dr Campbell has nothing to disclose.
Dr Bramham has nothing to disclose.
Dr Hamzah has nothing to disclose.
Dr Fox has nothing to disclose.
Dr Burns has nothing to disclose.
Dr Clarke reports personal fees from Advisory boards & conference travel from Gilead Sciences, personal fees from Advisory boards from ViiV Healthcare, outside the submitted work.
Dr Vincent has nothing to disclose.
Dr Jones has nothing to disclose.
Dr Price has nothing to disclose.
Dr Onyago has nothing to disclose.
Dr Harber has nothing to disclose.
Dr Hilton has nothing to disclose.
Dr Booth has nothing to disclose.
Dr Sabin has nothing to disclose.
Dr Winkler has nothing to disclose.
Dr Post reports grants from Medical Research Council UK, grants, personal fees and non-financial support from Gilead, grants personal fees and non-financial support from ViiV, grants and personal fees from MSD, grants and personal fees from Janssen, during the conduct of the study.
Acknowledgments
The authors would like to thank the study participants and all members of the GEN-AFRICA study group (appendix).
This paper was presented in abstract for at the Conference on Retroviruses and Opportunistic Infections (CROI-virtual, 2020).
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.eclinm.2021.101006.
Appendix
Genetic markers of chronic kidney disease in people of African ancestry with HIV (GEN-AFRICA) Study Group
Barts Health NHS Trust, London (John Booth [PI], Anele Waters, James Hand, Chris Clarke, Sarah Murphy, Maurice Murphy); Brighton and Sussex University Hospitals, Brighton (Marion Campbell, Amanda Clarke [PI], Celia Richardson, Alyson Knott, Gemma Weir, Rebecca Cleig, Helena Soviarova, Lisa Barbour, Tanya Adams, Vicky Kennard, Vittorio Trevitt); Chelsea and Westminster Hospital, London (Rachael Jones [PI], Alexandra Schoolmeester, Serah Duro; Guy's and St Thomas’ Hospital, London (Rachel Hilton [PI], Julie Fox, May Rabuya, Lisa Hamzah, Deborah Jordan, Teresa Solano, Hiromi Uzu, Karen Williams, Julianne Lwanga, Linda Ekaette Reid-Amoruso, Hannah Gamlen, Robert J. Stocker, Fiona Ryan, Anele Waters, Karina Mahiouz, Tess Cheetham, Claire Williams, Achyuta Nori, Caroline Thomas, Sivaraj Venkateshwaran, Jessica Doctor, Andrea Berlanga); King's College Hospital, London (Frank Post [CI], Beatriz Santana-Suarez, Leigh McQueen, Priya Bhagwandin, Lucy Campbell, Bee Barbini, Emily Wandolo, Tim Appleby, Deborah Jordan, Lois Driver, Sophy Parr, Hongbo Deng, Julie Barber, Andrew Crowe, Chris Taylor, Mary Poulton, Vida Boateng, Marie-Pierre Klein, Caitlin O'Brien, Samuel Ohene-Adomako, Christian Buckingham, Daniel Trotman, Killian Quinn, Kate Flanagan, Verity Sullivan, Holly Middleditch, Itty Samuel, Elizabeth Hamlyn, Candice McDonald, Ana Canoso, Emeka Agbasi, Maria Liskova, Sarah Barber, Amanda Samarawickrama, Zoe Ottaway, Claire Norcross, Amelia Oliveira, Kate Bramham); Leeds Teaching Hospitals NHS Trust, Leeds (Jane Minton [PI], Gary Lamont, Ruby Cross, Gaushiya Saiyad, Shadia Ahmed, Rebecca Ashworth, Nicola Window, J Murira, Khine Phyu); North Manchester General Hospital, Manchester (Andrew Ustianowski [PI], Gabriella Lindergard, Jonathan Shaw, Sarah Holland, Claire Fox, Jan Flaherty, Margaret-Anne Bevan, Valerie George); South Tees Hospitals NHS Foundation Trust, Middlesbrough (David Chadwick [PI], Marie Branch, Pauline Lambert, Adele Craggs); Mortimer Market center, Central and NorthWest London NHS Foundation Trust, London (Sarah Pett [PI], Hinal Lukha, Nina Vora, Marzia Fiorino, Maria Muller Nunez, Deirdre Sally, James E. Burns, Erica Pool, Rebecca Matthews); Newcastle upon Tyne Hospitals, Newcastle (David Ashley Price [PI], Tara Stothard, Bijal Patel, Ian McVittie, Ciara Kennedy, Uli Shwab, Brendan Payne, Sarah Duncan, Jill Dixon, Mathias Schmid, Adam Evans, Christopher Duncan, Ewan Hunter, Yusri Taha, Natasha Astill); National Cancer Institute, Frederick, USA (Cheryl Winkler, Elizabeth Binns- Roemer, Victor David); North Middlesex University Hospital, London (Jonathan Ainsworth, Rachel Vincent [PI]); Queen Elizabeth Hospital, Woolwich (Stephen Kegg [PI], Chloe Saad, Sarah Skinner, Hocine Azzoug, Judith Russell, Tarik Moussaoui, Celia Richardson, Emily Mabonga, Donna Ward, J. Francoise, W. Larbi, Sue Mitchell, A. Manning, V. Russell); Royal Free London Hospital, London (Fiona Burns [PI], Mark Harber, Nnenna Ngwu, Jonathan Edwards, Nargis Hemat, Tom Fernandez, Filippo Ferro, Jorge Ferreira, Alice Nightingale, Tasha Oakes-Monger, Darwin Matila, Pedro Nogueira, Victoria Mutagwanya); St. Georges University Hospitals, London (Catherine Cosgrove [PI], Lisa Hamzah, Catherine Emily Isitt, Helen Webb, Joyce Popoola, Kate Korley, Mark Mencias, Patricia Ribeiro, Rajeshwar Ramkhelawn, Sandra Oliva Lara, Sara Sajijad); Imperial College Healthcare NHS Trust, London (Alan Winston [PI], Amber Shaw, Claire Petersen, Kyle Ring); University Hospital Lewisham, London (Melanie Rosenvinge [PI], Chloe Saad, Sarah Skinner, Thembi Moyo, Faith Odong, Katherine Gantert, Tina Ibe); Africa Advocacy Foundation (Denis Onyango); UK CHIC cohort (Caroline Sabin [PI], Teresa Hill).
Appendix B. Supplementary materials
References
- 1.Roth G.A., Abate D., Abate K.H. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the global burden of disease study 2017. The Lancet. 2018;392(10159):1736–1788. doi: 10.1016/S0140-6736(18)32203-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Population, total - Sub-Saharan Africa | Data. Accessed December 4, 2020. https://data.worldbank.org/indicator/SP.POP.TOTL?locations=ZG
- 3.Dwyer-Lindgren L., Cork M.A., Sligar A. Mapping HIV prevalence in sub-Saharan Africa between 2000 and 2017. Nature. 2019;570(7760):189–193. doi: 10.1038/s41586-019-1200-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Swanepoel C.R., Atta M.G., D'Agati V.D. Kidney disease in the setting of HIV infection: conclusions from a kidney disease: improving global outcomes (KDIGO) controversies conference. Kidney Int. 2018;93(3):545–559. doi: 10.1016/j.kint.2017.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Limou S., Nelson G.W., Kopp J.B., Winkler C.A. APOL1 kidney risk alleles: population genetics and disease associations. Adv Chronic Kidney Dis. 2014;21(5):426–433. doi: 10.1053/j.ackd.2014.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kasembeli A.N., Duarte R., Ramsay M. APOL1 risk variants are strongly associated with HIV-associated nephropathy in black South Africans. J Am Soc Nephrol. 2015;26(11):2882–2890. doi: 10.1681/asn.2014050469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kopp J.B., Nelson G.W., Sampath K. APOL1 genetic variants in focal segmental glomerulosclerosis and HIV-associated nephropathy. J Am Soc Nephrol. 2011;22(11):2129–2137. doi: 10.1681/asn.2011040388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Genovese G., Friedman D.J., Ross M.D. Association of trypanolytic ApoL1 variants with kidney disease in African Americans. Science. 2010;329(5993):841–845. doi: 10.1126/science.1193032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Parsa A., Kao W.H.L., Xie D. APOL1 risk variants, race, and progression of chronic kidney disease. N Engl J Med. 2013;369(23):2183–2196. doi: 10.1056/NEJMoa1310345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ekrikpo U.E., Kengne A.P., Bello A.K. Chronic kidney disease in the global adult HIV-infected population: a systematic review and meta-analysis. PLoS ONE. 2018;13(4) doi: 10.1371/journal.pone.0195443. Reboldi G, ed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jose S., Hamzah L., Jones R. Chronic kidney disease risk in African and Caribbean populations with HIV. J Infect Dis. 2018;218(11):1767–1772. doi: 10.1093/infdis/jiy397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bansi L., Hughes A., Bhagani S. Clinical epidemiology of HIV-associated end-stage renal failure in the UK. Aids. 2009;23(18):2517–2521. doi: 10.1097/QAD.0b013e3283320e12. [DOI] [PubMed] [Google Scholar]
- 13.The six regions of the African Union | West Africa Gateway | Portail de l'Afrique de l'Ouest. Accessed August 4, 2020. http://www.west-africa-brief.org/content/en/six-regions-african-union
- 14.Levey A.S., Stevens L.A. Estimating GFR using the CKD epidemiology collaboration (CKD-EPI) creatinine equation: more accurate GFR estimates, lower CKD prevalence estimates, and better risk predictions. Am J Kidney Dis. 2010;55(4):622–627. doi: 10.1053/j.ajkd.2010.02.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stevens P.E., Levin A. Evaluation and management of chronic kidney disease: synopsis of the kidney disease: improving global outcomes 2012 clinical practice guideline. Ann Intern Med. 2013;158(11):825–830. doi: 10.7326/0003-4819-158-11-201306040-00007. [DOI] [PubMed] [Google Scholar]
- 16.Levey A.S., Coresh J., Balk E. National kidney foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med. 2003;139(2):137–147. doi: 10.7326/0003-4819-139-2-200307150-00013. [DOI] [PubMed] [Google Scholar]
- 17.Official JOurnal Of the InternatiOnal SOciety Of NephrOlOgy KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. [DOI] [PubMed]
- 18.Booth J.W., Hamzah L., Jose S. Clinical characteristics and outcomes of HIV-associated immune complex kidney disease. Nephrol Dial Transplant. 2016;31(12):2099–2107. doi: 10.1093/ndt/gfv436. [DOI] [PubMed] [Google Scholar]
- 19.Lucas G.M., Eustace J.A., Sozio S., Mentari E.K., Appiah K.A., Moore R.D. Highly active antiretroviral therapy and the incidence of HIV-1-associated nephropathy: a 12-year cohort study. AIDS. 2004;18(3):541–546. doi: 10.1097/00002030-200402200-00022. [DOI] [PubMed] [Google Scholar]
- 20.George J.A., Brandenburg J.T., Fabian J. Kidney damage and associated risk factors in rural and urban sub-Saharan Africa (AWI-Gen): a cross-sectional population study. Lancet Glob Health. 2019;7(12):e1632–e1643. doi: 10.1016/S2214-109X(19)30443-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kaboré N.F., Poda A., Zoungrana J. Chronic kidney disease and HIV in the era of antiretroviral treatment: findings from a 10-year cohort study in a west African setting. BMC Nephrol. 2019;20(1) doi: 10.1186/s12882-019-1335-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen T.K., Tin A., Peralta C.A. APOL1 risk variants, incident proteinuria, and subsequent eGFR decline in blacks with hypertension-attributed CKD. Clin J Am Soc Nephrol. 2017;12(11):1771–1777. doi: 10.2215/CJN.01180117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lipkowitz M.S., Freedman B.I., Langefeld C.D. Apolipoprotein L1 gene variants associate with hypertension-attributed nephropathy and the rate of kidney function decline in African Americans. Kidney Int. 2013;83(1):114–120. doi: 10.1038/ki.2012.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Estrella M.M., Wyatt C.M., Pearce C.L. Host APOL1 genotype is independently associated with proteinuria in HIV infection. Kidney Int. 2013;84(4):834–840. doi: 10.1038/ki.2013.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Peralta C.A., Bibbins-Domingo K., Vittinghoff E. APOL1 genotype and race differences in incident albuminuria and renal function decline. J Am Soc Nephrol. 2016;27(3):887–893. doi: 10.1681/ASN.2015020124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mathur R., Dreyer G., Yaqoob M.M., Hull S.A. Ethnic differences in the progression of chronic kidney disease and risk of death in a UK diabetic population: an observational cohort study. BMJ Open. 2018;8:20145. doi: 10.1136/bmjopen-2017-020145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Delanaye P., Mariat C., Maillard N., Jean-Marie K., Cavalier E. Are the creatinine-based equations accurate to estimate glomerular filtration rate in African American populations? Clin J Am Soc Nephrol. 2011;6(4):906–912. doi: 10.2215/CJN.10931210. [DOI] [PubMed] [Google Scholar]
- 28.Kalyesubula R., Fabian J., Nakanga W. How to estimate glomerular filtration rate in sub-Saharan Africa: design and methods of the African Research into kidney diseases (ARK) study. BMC Nephrol. 2020;21(1):20. doi: 10.1186/s12882-020-1688-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mocroft A., Kirk O., Reiss P. Estimated glomerular filtration rate, chronic kidney disease and antiretroviral drug use in HIV-positive patients. AIDS. 2010;24(11):1667–1678. doi: 10.1097/QAD.0b013e328339fe53. [DOI] [PubMed] [Google Scholar]
- 30.Yombi J., Jones R., Pozniak A., Hougardy J.-.M., Post F. Monitoring of kidney function in HIV-positive patients. HIV Med. 2015;16(8):457–467. doi: 10.1111/hiv.12249. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.