Abstract
Objective:
To determine the minimal clinically important difference of the Mini-BESTest in individuals’ post-stroke.
Design:
Prospective cohort study.
Setting:
Outpatient stroke rehabilitation.
Subjects:
Fifty outpatients with stroke with a mean (SD) age of 60.8 (9.4).
Intervention:
Outpatients with stroke were assessed with the Mini-BESTest before and after a course of conventional rehabilitation. Rehabilitation sessions occurred one to two times/week for one hour and treatment duration was 1.3–42 weeks (mean (SD) = 17.4(10.6)).
Main measures:
We used a combination of anchor- and distribution-based approaches including a global rating of change in balance scale completed by physiotherapists and patients, the minimal detectable change with 95% confidence, and the optimal cut-point from receiver operating characteristic curves.
Results:
The average (SD) Mini-BESTest score at admission was 18.2 (6.5) and 22.4 (5.2) at discharge (effect size: 0.7) (P = 0.001). Mean change scores on the Mini-BESTest for patient and physiotherapist ratings of small change were 4.2 and 4.3 points, and 4.7 and 5.3 points for substantial change, respectively. The minimal detectable change with 95% confidence for the Mini-BESTest was 3.2 points. The minimally clinical importance difference was determined to be 4 points for detecting small changes and 5 points for detecting substantial changes.
Conclusions:
A change of 4–5 points on the Mini-BEST is required to be perceptible to clinicians and patients, and beyond measurement error. These values can be used to interpret changes in balance in stroke rehabilitation research and practice.
Keywords: Stroke, Mini-BESTest, MCID
Introduction
Improving mobility and reducing the risk of falls are key rehabilitation goals after stroke. A recent expert panel recommended the Mini-Balance Evaluation Systems test (Mini-BESTest) 1 as part of a minimum data set for measuring balance in adults. 2 However, a key barrier to uptake of the Mini-BESTest is the limited information regarding its psychometric properties across clinical populations. In particular, the minimal clinically important difference, which reflects the amount of improvement that is perceived as important to patients and care providers, was highlighted by clinicians as an important facilitator for outcome measure uptake. 3 To date, Mini-BESTest research in stroke has been limited to reporting of reliability, validity, and ability to discriminate by fall status. 4 There is a need to identify the amount of change on the Mini-BESTest that can be understood as both real and important to patients and clinicians. The aim of this study was to determine the minimal clinically importance difference of the Mini-BESTest in individuals post stroke receiving outpatient rehabilitation.
Methods
This study is part of a single-center, prospective, longitudinal study in which physiotherapists and researchers have partnered in an Integrated Knowledge Translation paradigm, with the purpose of generating new data to improve the utility of the Mini-BESTest in people with stroke. Potential participants were screened by their treating physiotherapist and enrolled as appropriate. Eligibility criteria included: residents of Manitoba, Canada, with a valid provincial health care number who were referred for stroke; stroke patients referred for standing balance assessment; treating physiotherapist observation of instability in transfers or walking; history of falls in the past two years or self-reported problem with balance; lack of other neurological conditions that would significantly affect balance; ability to stand for 10 seconds without physical assistance; a minimum of two weeks of outpatient physiotherapy services anticipated; ability to communicate in and understand English; and ability to follow test instructions and provide informed consent. In line with guidelines for establishing the minimal clinically important difference of outcome measures, a sample size of 50 was targeted. 5
The rehabilitation program was tailored to individual patient needs based on an initial assessment and consistent with Canadian stroke best practice recommendations. 6 The program typically included repetition and practice of lower limb strength training, multiple components of balance with an emphasis on static and dynamic stability and anticipatory control in sitting and standing, progressive functional tasks including walking, and stair climbing, as appropriate. The need for gait aides and lower extremity orthotics was evaluated and devices were modified as necessary. There was a strong emphasis on patients completing home exercises on a daily basis. Parts of each session were used to progress to the home exercises. As part of patient education, fall prevention strategies were also reviewed. Physiotherapy sessions were one hour long and occurred one to two times a week.
On admission and discharge, treating physiotherapists administered the Mini-BESTest, a 14-item test of dynamic balance. The test is divided into four subcomponents (anticipatory postural adjustments, postural responses, sensory orientation, and dynamic gait) and scored on a three-level ordinal scale with a total score out of 28 points (higher scores indicate better balance). 1 At discharge, both the patients and physiotherapists completed a global rating of change scale to rate the amount of change perceived in the patients’ balance on a 7-point scale: much better (7); a little better/meaningful (6); a little better/not meaningful (5); about the same (4); a little worse/not meaningful (3); a little worse/meaningful (2), and much worse (1). A 7-point global rating of change scale has shown adequate responsiveness, face validity, and clinical relevance with patient satisfaction.7–9
Prior to the study, a comprehensive and established training program based on health professional behavior change theory 10 was administered to treating physiotherapists (N = 5) to increase knowledge, skills, and confidence for administering and scoring the Mini-BESTest, and a pilot inter-rater reliability trial including five patients with stroke was conducted. The Mini-BESTest was administered by the treating physiotherapist and the procedures were video recorded. All physiotherapists scored each patient’s performance from the video on two separate occasions – approximately seven days apart. Intraclass correlation coefficients of 0.95 and 0.93 were obtained for the total score of the Mini-BESTest on sessions 1 and 2, respectively.
A research assistant extracted data from the clinical record on admission date, age, diagnosis, stroke severity, co-morbidities, and fall history. The research assistant also administered the Chedoke McMaster Stroke Assessment, 11 Timed Up and Go Test, 12 and Activities-specific Balance Confidence scale, 13 to describe the sample population. The University of Manitoba Health Research Ethics Board approved this study (ethics reference number: HS19725), and all patients provided written consent. This study was funded by the Health Sciences Centre Foundation, Winnipeg (recipient KM Sibley) and supported in part by the Canada Research Chairs Program (recipients MK Beauchamp and KM Sibley).
Statistical analysis
Descriptive statistics were computed using measures of central tendency and dispersion. Box plot examination showed no outliers in the data. A paired t-test was used to determine if there was a difference in the mean change score between intake and discharge. Cohen’s effect size was also determined. 14 Ceiling and floor effects were examined for the Mini-BESTest total score and considered significant if ⩾15% of participants were at the upper or lower limits of the test score.
The minimal clinically important difference 15 was based on a combination of distribution and anchor-based approaches. For the anchor-based approach, we determined the mean absolute Mini-BESTest change scores for each answer on the global rating of change scale. For the distribution based-approach, we first determined the standard error of measurement calculated as , where Sb is the SD of our sample at intake, and r is the test-retest reliability coefficient. 3 Following, the minimal detectable change with 95% confidence, which refers to the smallest amount of change that falls outside of measurement error, was calculated as . Minimal clinically important difference thresholds were determined by triangulating the estimates from the mean change score on the global rating of change scale with the standard error of measurement for small changes, and with the minimal detectable change for substantial changes. We have used this approach successfully in our other studies.16,17
The receiver operating characteristic curve was also used to determine the minimal clinically important difference using the Mini-BESTest as the diagnostic test for discriminating between improved and unchanged patients based on the global rating of change scale. The sample was divided into groups based on the global rating of change scores: patients with any improvement (global rating of change scale: a little better, much better) vs. those who were unchanged (global rating of change: about the same, a little better but not meaningful change). The data point closest to the upper left corner of the curve, the point that optimizes sensitivity and specificity, was chosen as the optimal threshold for detection of a change, with the area under the curve of the receiver operating characteristic reflecting the measure’s accuracy. An area under the curve of 0.7 or greater was considered acceptable accuracy by convention. 5
Weighted kappa was used to determine the inter-rater agreement between patient and physiotherapist global rating of change scores. To interpret the kappa statistics, the following criteria were used: no agreement = <0.0, poor agreement = 0.0–0.20, fair agreement = 0.21–0.40, good agreement = 0.41–0.60, very good agreement = 0.61–0.80, and excellent agreement = 0.81–1.00. 18 Spearman’s rho and Kendall’s tau-b were used for the correlations between anchor and physiotherapist global rating of change scores. Interpretation of the correlations were as follows: negligible = 0.0–0.10, weak = 0.11–0.39, moderate = 0.40–0.69, strong = 0.70–0.89, and very strong = 0.90–1.00. 19
Results
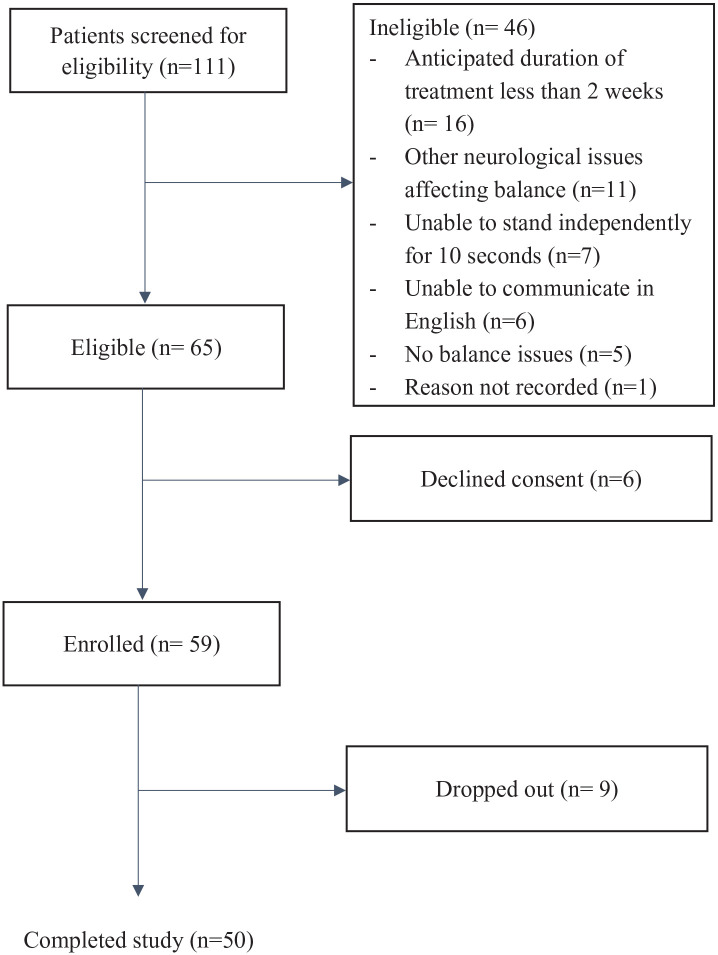
A flowchart of participant recruitment is provided in Figure 1. Fifty patients with stroke (mean (SD) age 60.8 (9.4) years, men = 34/50) participated in the study (Table 1). Treatment duration varied from 1.3 to 42 weeks (mean (SD) = 17.4 (10.6)) and on average patients completed 91% of the treatment proposed.
Figure 1.
Participant recruitment flowchart.
Table 1.
Sociodemographic and clinical characteristics of the participants (n = 50).
| Characteristics | |
|---|---|
| Age (years), mean (SD) | 60.8 (9.4) |
| Men, n | 34 |
| Type of stroke, n | |
| Hemorrhagic | 11 |
| Ischemic | 10 |
| Unknown | 29 |
| Right side affected, n | 34 |
| Time between stroke and admission (days), mean (SD) | 124.4 (106.5) |
| Min/max | 16/459 |
| Treatment duration (days), mean (SD) | 121.8 (74.3) |
| Min/max | 9/294 |
| Number of physiotherapy sessions offered, mean (SD) | 17.3 (13.2) |
| Min/max | 4/69 |
| Number of physiotherapy sessions attended, mean (SD) | 15.5 (11.8) |
| Min/max | 4/58 |
| CMSA | |
| Foot, mean | 5.2 |
| Median | 5 |
| Leg, mean | 5.6 |
| Median | 6 |
| Comorbidities, n | |
| Cardiac | 43 |
| Diabetes | 15 |
| Mobility and balance tests at intake, mean (SD) | |
| Mini-BESTest total score | 18.2 (6.5) |
| TUG time (seconds) | 14.2 (8.7) |
| TUG dual-task time (seconds) | 17.9 (10.7) |
| ABC scale score (%) | 61.6 (21.2) |
| Mean change in the Mini-BESTest | |
| Intake | 18.3 (0.9) |
| Discharge | 22.4 (0.7) |
SD: standard deviation; CMSA: Chedoke-McMaster stroke assessment: 7-point scale impairment inventory, from most impairment (one flaccid paralysis) to no impairment (seven normal movement); TUG: timed up and go; Mini-BESTest: mini balance evaluation systems test; ABC: activities-specific balance confidence scale.
The average (SD) Mini-BESTest score at admission was 18.2 (6.5) and 22.4 (5.2) at discharge (effect size: 0.7) and this difference was statistically significant (P = 0.001). The Mini-BESTest showed no floor or ceiling effects. At admission, 2 (2.9%) participants scored 5, and 1 (1.4%) participant scored 27. At discharge, 1 (1.4%) participant scored 7 and 5 (7.2%) scored 27.
The interrater reliability of the global rating of change scale ratings between patients and physiotherapists showed no agreement, weighted kappa = 0.06 (probability value = 0.54,), 95% CI (-.131, .256). The correlation between global rating of change score and change in the Mini-BESTest was 0.33 (P = 0.020) for therapists, and 0.09 (P = 0.519) for patients.
The minimal clinically important difference for small (4 points) and substantial change (5 points) was similar for both patient and physiotherapist perception and aligned well with the distribution-based minimal detectable change (Table 2).
Table 2.
Meaningful change estimates for the Mini-BESTest based on patient and physiotherapist ratings using the global rating scale and distribution-based methods (n = 50).
| Mini-BESTest component | Global rating of change scale collapsed, mean (SD) | SEM | MDC95 | MCID small change* | MCID substantial change* | ||
|---|---|---|---|---|---|---|---|
| About the same | A little better | Much better | |||||
| Anticipatory patient | 0.7 (0.8) | 0.4 (0.7) | 0.9 (0.9) | 0.4 | 1.0 | 1 | 1 |
| Therapist | 0.4 (0.7) | 0.8 (0.9) | 0.7 (0.8) | 1 | 1 | ||
| Reactive patient | 0.7 (1.2) | 1.1 (1.6) | 1.1 (1.2) | 0.7 | 1.8 | 1 | 2 |
| Therapist | 0.1 (0.3) | 1.2 (1.2) | 1.2 (1.6) | 1 | 2 | ||
| Sensory patient | 0.3 (0.7) | 0.6 (1.0) | 0.6 (0.7) | 0.4 | 1.0 | 1 | 1 |
| Therapist | 0.1 (0.9) | 0.6 (0.8) | 0.7 (0.7) | 1 | 1 | ||
| Dynamic patient | 2.1 (1.3) | 1.4 (1.9) | 2.0 (2.3) | 1.0 | 2.6 | 2 | 3 |
| Therapist | 0.7 (1.7) | 1.5 (1.4) | 2.6 (2.3) | 2 | 3 | ||
| Total score patient | 3.8 (2.3) | 3.5 (3.8) | 4.7 (3.9) | 1.1 | 3.2 | 4 | 5 |
| Therapist | 1.3 (2.8) | 4.2 (2.6) | 5.2 (4.1) | 4 | 5 | ||
SEM: minimal clinically important difference; MDC: minimal detectable change; MCID: minimal clinically important difference.
Global Rating Change scale collapsed: about the same (a little better/not meaningful and about the same); a little better/meaningful and much better.
The minimal clinically important difference value for small change was selected as the larger of either the anchor-based estimate for small change (about the same and a little better) or the distribution-based standard error of measurement, rounded to the nearest whole number. The minimal clinically important difference value for substantial change was selected as the larger of either the anchor-based estimate for substantial change (much better) or the distribution-based MDC95, rounded to the nearest whole number.
A total of 23 (46%) patients perceived an improvement, of those, 6 (mean change = 4) patients improved based on the minimal clinically important difference for small change, and 17 (mean change = 8.1) for substantial change. The area under the curve for the Mini-BESTest based on the patients’ perception of change was not significantly better than chance. The receiver operating characteristic curve analysis for change in the Mini-BESTest total score according to physiotherapist perception showed adequate discrimination between patients that improved and those with small or no change (area under the curve = 0.774, 95% CI = 0.59–0.95; probability value = 0.011) with an optimum cut-off value of ⩾1 point (95% sensitivity; 56% specificity) (Figure 2). Table 3 shows a comparison of the number of patients that improved based on the MCID for small and substantial changes and based on the receiver operating characteristic curve.
Figure 2.
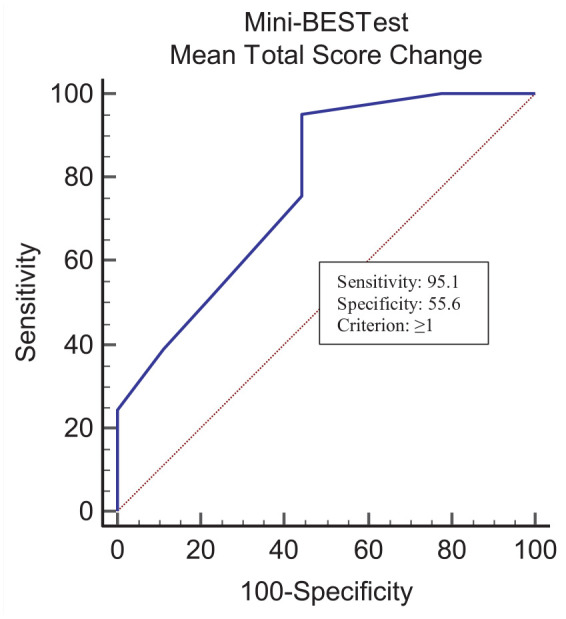
Receiver operating characteristic curve for discrimination between improved and unchanged participants on the Mini-BESTest according to physiotherapist perception.
Table 3.
Total number of patients classified as improved based on the minimal clinically important difference (MCID) value obtained from different methods (n = 50).
| Methods | Cut-off value | Number of patients that improved |
|---|---|---|
| MCID substantial change | ⩾5 | 17 |
| MCID small change | 4 | 6 |
| *ROC curve | ⩾1 | 44 |
Receiver operating characteristic curve, sensitivity 95.1% and specificity 55.6%.
Discussion
This is the first study to provide estimates of clinically meaningful change for the Mini-BESTest in people with stroke. We determined that a change of 4–5 points on the Mini-BESTest reflects the minimal clinically important difference for people with stroke attending outpatient rehabilitation. This information is critical for increasing the interpretability of the Mini-BESTest in stroke rehabilitation research and practice.
A challenge in identifying the optimal minimal clinically important difference value is deciding how much change is needed to be considered “important,” and for whom. Although there was poor agreement between physiotherapists and patients in their perception of change, it is reassuring that our minimal clinically important difference estimates for perceived important change are similar for both patients and physiotherapists. In terms of how much change is needed to constitute a minimal clinically important difference, we have provided estimates for both small change and substantial change to account for different applications and contexts. For example, if forming the basis of a power calculation for a clinical trial, the smallest possible difference threshold is preferable, whereas in clinical practice when evaluating change in individual patients, a more considerable change threshold can be selected. Thus, we have recommended a minimal clinically important difference of 4 points for detecting small changes on the Mini-BESTest in individuals with stroke, and 5 points for substantial change.
Based on the receiver operating characteristic curve, a change of 1-point on the Mini-BESTest was able to identify patients rated as substantially improved by physiotherapists, with acceptable accuracy but with relatively low specificity (55.6%). It is important to note that this change of 1-point in the Mini-BESTest total score is lower than the minimal clinically important difference estimates obtained based on the patient and physiotherapist-rated anchors, as well as below our distribution-based estimate for real change beyond measurement error. Therefore, we would caution against using this value obtained from the receiver operating characteristic curve as a minimal clinical important difference and suggest the values in Table 2 instead. Indeed, the fact that the standard error of measurement aligns with mean change in Mini-BESTest for patient- and physiotherapist-reported “small change,” and that the minimal detectable change aligns well with perceived substantial change, increases our confidence in these estimates. We have also provided the corresponding estimates for minimal clinically important difference values for each of the Mini-BESTest sub-scores (range of 1–3 points depending on the sub-scale), as clinicians may wish to target an individual sub-system of balance in their clinical practice.
In this study, a correlation of 0.33 was obtained for physiotherapist-reported global rating of change and change in Mini-BESTest but was negligible for the patient-reported anchor. This makes sense given the lack of agreement between physiotherapists and patients with respect to perceived change, and resulted in only 46% (n = 23) of the patients perceiving improvement. A review of studies in patients with balance disorders reveals minimal clinically important difference values in the range of 10%–17% of the total score, consistent with the results of the present study.20–22 A small change of 4 points represents a variation of about 14% in the Mini-BESTest total score, and a substantial change of 5 points, represents a change of 17%. This corresponds to an effect size of 0.7 (standard deviations), which is considered to be clinically relevant. 23 In general, our data suggest that patients with stroke may be weighting different factors or values more strongly in their rating of balance change after therapy, or that they may have had difficulty reflecting on their change over time. The physiotherapists may have also been biased toward a positive change rating as they are actively invested in improving patient function. This would be an important area for future research to ensure that the goals of patients with stroke are being met in rehabilitation.
Our data has some limitations. Because patients were enrolled in a rehabilitation program, most patients improved and we are only able to provide minimal clinically important difference values for improvement; estimates for decline may differ. For our distribution-based estimates of standard error of measurement and minimal detectable change, we used test-retest reliability coefficients from a previous study in stroke. 4 The minimal clinically important difference values reported in this study may not be generalizable to other stroke populations with different mobility levels, for example, among inpatients with stroke.
In summary, our study found that for individuals with stroke attending outpatient rehabilitation, a change of 4–5 points on the Mini-BESTest total score is required to be beyond measurement error and perceptible to both patients and clinicians. These values can be used to interpret the results of rehabilitative interventions designed to improve balance and fall risk in individuals with stroke.
Clinical messages.
For people undergoing post-stroke rehabilitation, a minimal clinically important difference of 4 points for detecting small and 5 points for substantial changes is recommended on the Mini-BESTest.
Minimal clinically important difference of 1–3 points on the Mini-BESTest sub-scores might help clinicians to assess change in individual balance subsystems.
Acknowledgments
We thank Fedra Salias, Lynne Clark, Melissa Vilaykeo, Mona Maida, Shelley Kowalchuk, and Vanessa Ellis for data collection support and all participants for volunteering for this study.
Footnotes
Author contributions: All authors analyzed and interpreted data, critically revised, and approved the final manuscript. In addition, KM Sibley conceptualized and designed the study, and obtained funding. MK Beauchamp co-led the conceptualization and design of the study and led data analysis and manuscript development. R Niebuhr and P Roche coordinated data collection and R Kirkwood contributed to data analysis and manuscript development.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was undertaken, in part, thanks to funding from the Canada Research Chairs Program (recipients: MK Beauchamp and KM Sibley) and by the Health Sciences Centre Foundation, Winnipeg (recipient: KM Sibley).
ORCID iDs: Kathryn M Sibley  https://orcid.org/0000-0002-6212-5437
https://orcid.org/0000-0002-6212-5437
References
- 1. Franchignoni F, Horak F, Godi M, et al. Using psychometric techniques to improve the balance evaluation systems test: the mini-BESTest. J Rehabil Med 2010; 42(4): 323–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sibley KM, Howe T, Lamb SE, et al. Recommendations for a core outcome set for measuring standing balance in adult populations: a consensus-based approach. PLoS One 2015; 10(3): e0120568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Haley SM, Fragala-Pinkham MA. Interpreting change scores of tests and measures used in physical therapy. Phys Ther 2006; 86(5): 735–743. [PubMed] [Google Scholar]
- 4. Tsang CS, Liao LR, Chung RC, et al. Psychometric properties of the mini-balance evaluation systems test (Mini-BESTest) in community-dwelling individuals with chronic stroke. Phys Ther 2013; 93(8): 1102–1115. [DOI] [PubMed] [Google Scholar]
- 5. Terwee CB, Bot SD, de Boer MR, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol 2007; 60(1): 34–42. [DOI] [PubMed] [Google Scholar]
- 6. Practices CSB, Balance and mobility, https://www.strokebestpractices.ca/recommendations/stroke-rehabilitation/mobility-balance-and-transfers (accessed 9 December 2019).
- 7. Fischer D, Stewart AL, Bloch DA, et al. Capturing the patient’s view of change as a clinical outcome measure. JAMA 1999; 282(12): 1157–1162. [DOI] [PubMed] [Google Scholar]
- 8. Kamper SJ, Maher CG, Mackay G. Global rating of change scales: a review of strengths and weaknesses and considerations for design. J Man Manip Ther 2009; 17(3): 163–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lauridsen HH, Hartvigsen J, Korsholm L, et al. Choice of external criteria in back pain research: does it matter? Recommendations based on analysis of responsiveness. Pain 2007; 131(1–2): 112–120. [DOI] [PubMed] [Google Scholar]
- 10. Sibley KM, Brooks D, Gardner P, et al. Development of a theory-based intervention to increase clinical measurement of reactive balance in adults at risk of falls. J Neurol Phys Ther 2016; 40(2): 100–106. [DOI] [PubMed] [Google Scholar]
- 11. Dang M, Ramsaran KD, Street ME, et al. Estimating the accuracy of the Chedoke-McMaster stroke assessment predictive equations for stroke rehabilitation. Physiother Can 2011; 63(3): 334–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hafsteinsdóttir TB, Rensink M, Schuurmans M. Clinimetric properties of the timed up and go test for patients with stroke: a systematic review. Top Stroke Rehabil 2014; 21(3): 197–210. [DOI] [PubMed] [Google Scholar]
- 13. Powell LE, Myers AM. The Activities-specific balance confidence (ABC) scale. J Gerontol A Biol Sci Med Sci 1995; 50a(1): M28–M34. [DOI] [PubMed] [Google Scholar]
- 14. Lakens D. Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t-tests and ANOVAs. Front Psychol 2013; 4: 863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Revicki D, Hays RD, Cella D, et al. Recommended methods for determining responsiveness and minimally important differences for patient-reported outcomes. J Clin Epidemiol 2008; 61(2): 102–109. [DOI] [PubMed] [Google Scholar]
- 16. Beauchamp MK, Harrison SL, Goldstein RS, et al. Interpretability of change scores in measures of balance in people with COPD. Chest 2016; 149(3): 696–703. [DOI] [PubMed] [Google Scholar]
- 17. Beauchamp MK, Ward RE, Jette AM, et al. Meaningful change estimates for the late-life function and disability instrument in older adults. J Gerontol A Biol Sci Med Sci 2019; 74(4): 556–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Viera AJ, Garrett JM. Understanding interobserver agreement: the kappa statistic. Fam Med 2005; 37(5): 360–363. [PubMed] [Google Scholar]
- 19. Schober P, Boer C, Schwarte LA. Correlation coefficients: appropriate use and interpretation. Anesth Analg 2018; 126(5): 1763–1768. [DOI] [PubMed] [Google Scholar]
- 20. Chinsongkram B, Chaikeeree N, Saengsirisuwan V, et al. Responsiveness of the balance evaluation systems test (BESTest) in people with subacute stroke. Phys Ther 2016; 96(10): 1638–1647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Godi M, Arcolin I, Giardini M, et al. Responsiveness and minimal clinically important difference of the Mini-BESTest in patients with Parkinson’s disease. Gait Posture 2020; 80: 14–19. [DOI] [PubMed] [Google Scholar]
- 22. Godi M, Franchignoni F, Caligari M, et al. Comparison of reliability, validity, and responsiveness of the mini-BESTest and berg balance scale in patients with balance disorders. Phys Ther 2013; 93(2): 158–167. [DOI] [PubMed] [Google Scholar]
- 23. Angst F, Aeschlimann A, Angst J. The minimal clinically important difference raised the significance of outcome effects above the statistical level, with methodological implications for future studies. J Clin Epidemiol 2017; 82: 128–136. [DOI] [PubMed] [Google Scholar]