Abstract
The purpose of this study was to identify the risk factors for complications of perforator flaps in plantar reconstruction. A systematic review was performed by searching the PubMed, Cochrane Library, MEDLINE, and EMBASE databases from their inception date up to October 2020. Only studies on reconstructing plantar defects with perforator flaps were included, and specific data were required for each patient in the included studies. A total of 14 studies involving 111 flaps were identified and included in the meta‐analysis. Our meta‐analysis identified two risk factors for postoperative complications: flap size over 50 cm2 (risk ratio [RR] = 3.12; P = .02), diabetes mellitus foot (RR = 3.26; P = .03). No significant differences were found regarding heel defects (P = .34), single perforator (P = .57), age older than 60 years (P = .19), chronic aetiology (P = .13), trauma (P = .33), tumour resection (P = .60), ulcer (P = .84), and burn (P = .76). Although more high‐quality studies with adequate sample sizes are needed, this meta‐analysis indicated that flap size over 50 cm2 and diabetes mellitus foot were significant risk factors for postoperative complications of perforator flaps in plantar reconstruction.
Keywords: complication, meta‐analysis, perforator flap, plantar defect, risk factor
1. INTRODUCTION
Reconstruction of plantar defects has always been a difficult problem. The plantar aspect of the foot, as a weight‐bearing part of the human body, has tough skin, thick cuticle, and strong resistance to pressure and wear. 1 , 2 Forefoot and hindfoot are weight‐bearing areas with thicker skin and fat pads to support the body's weight. 3 Non‐weight‐bearing areas include toe and midfoot, which have relatively thin skin that helps maintain balance. 1 One of the main factors in plantar reconstruction is the provision of skin with texture, thickness, and sensitivity similar to plantar skin. 4
Because Koshima and Soeda first reported a perforator flap, the technique of perforator flaps has been widely used for the reconstruction of soft tissue defects. 5 A perforator flap is an axial flap consisting of skin and subcutaneous tissue based on one or more deep arterial perforators. 6 The technique of perforator flaps can obtain thin and flexible flaps with good blood perfusion while retaining the innervation, blood supply, and functionality of the donor site muscles. 7 Thus, the incidence of complications in the donor site can be reduced. 8 In recent years, with the development of perforator flaps, different types and concepts have emerged. 9 , 10 , 11 , 12 , 13
Perforator flaps can repair plantar defects while minimising the risk of complications in the donor site, but the reliability of perforator flaps has not been well verified. As far as we know, there is currently no meta‐analysis performing a risk analysis of complications of perforator flaps in plantar reconstruction, and our study can fill this knowledge gap. In this study, a meta‐analysis was performed to identify the risk factors for complications of perforator flaps in plantar reconstruction.
2. MATERIALS AND METHODS
2.1. Search strategy
A systematic review was performed by searching the PubMed, Cochrane Library, MEDLINE, and EMBASE databases from their inception date up to October 2020 for all literature on reconstructing plantar defects with perforator flaps. The following keywords were used in the search: “Perforator Flap,” “Flap, Perforator,” “Flaps, Perforator,” “Perforator Flaps,” “Plantar,” “Forefoot,” “Midfoot,” “Hindfoot,” “Heel,” and “defect.” References cited in the study were also reviewed in search of other suitable literature.
2.2. Selection criteria
All original studies using perforator flaps to repair plantar defects were included. The location of the defect was limited to the forefoot sole, midfoot sole, and hindfoot sole. Specific data were needed for each patient in the study. Only articles published in English were included. Case reports, letters, purely technical descriptions, comments, guidelines, and reviews were excluded. Data from the same author's studies were reviewed, and duplicates data were deleted.
2.3. Relevant study selection
Two reviewers independently reviewed all possible studies to screen out all eligible studies. First, the two reviewers (F. Y. F. and Z. P. Y.) directly removed unqualified articles that were not related to plantar reconstruction with perforator flaps by reading all the titles and abstracts of the articles. All qualified articles related to plantar reconstruction with perforator flaps were downloaded, and they sought the help of the original author for manuscripts that could not be downloaded. They identified all the studies that were included based on the selection criteria. If the two reviewers had different opinions, the issue was resolved by a more experienced reviewer (X. C. C.).
2.4. Data extraction
Data from the eligible studies were extracted independently by the two reviewers (F. Y. F. and Z. P. Y.). If the two reviewers had different opinions, the issue was resolved by a more experienced reviewer (X. C. C.). The extracted data included the following basic information: number of patients, age, aetiology, location of the defect, type of the flap, preoperative preparation, flap size, dissection plane, number of perforators, donor site, follow‐up time, and complications.
2.5. Quality assessment
Because all the included studies were retrospective studies, the Newcastle‐Ottawa Scale (NOS) was used to assess the risk of bias of each study. 14 The primary indicators of NOS included selection, comparability, and outcome, with a total score of 9. A study with a quality score of ≤5 was considered to be low quality, suggesting a high risk of bias; a study with a quality score of >5 was considered to be high quality, suggesting a low risk of bias. 15
2.6. Data analysis
We used the Revman 5.3 software to perform statistical analysis of the results. The risk ratio (RR) with the Mantel‐Haenszel calculation method was selected and used to compare dichotomous variables, and the corresponding 95% confidence intervals (CIs) were calculated. The chi‐square test was used to estimate heterogeneity. We used a fixed‐effect model when the result showed that the I 2 was less than 50% 16 ; otherwise, a random‐effect model was used. Funnel plots were performed to assess publication bias. P < .05 was considered statistically significant.
3. RESULTS
A total of 258 studies were initially searched from four databases. Then, 132 studies were excluded because they were duplicates, and 126 studies remained. After screening the titles and abstracts, 90 studies that were not related to plantar reconstruction with perforator flaps were deleted. After downloading and reading the full text of the remaining 36 studies, 22 studies were further removed. Figure 1 shows the selection process for eligible studies. Finally, 14 studies 4 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 involving 111 flaps were identified and included in the meta‐analysis (Table 1). The basic characteristics of patients and flaps are shown in Table 2. The quality scores of the included studies are presented in Table 1. One study 19 was considered to be low quality, and the others 4 , 17 , 18 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 were considered to be high quality.
FIGURE 1.
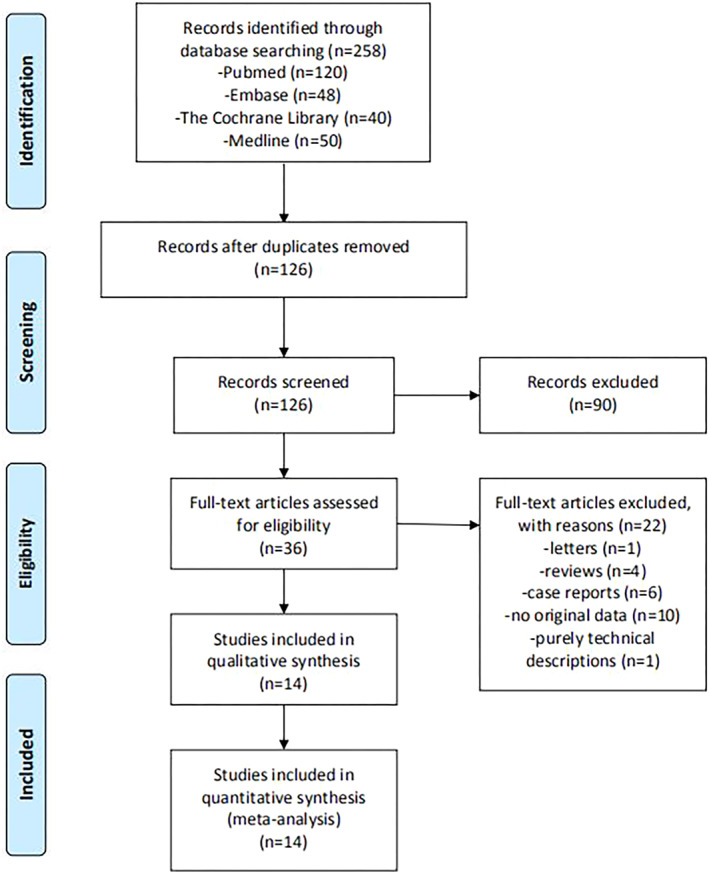
Flow diagram of the selection process for eligible studies
TABLE 1.
Overview of included studies
| Study | No. of cases | Mean age (y) | Type of flaps | Surgical technique | Donor site | Mean follow‐up (mo) | Complications | Quality score | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Preoperative preparation | Mean size (cm2) | Dissection | No. of perforators | ||||||||
| Zheng et al 17 | 7 | 19.6 | PAP; pedicled | Doppler | 27.2 | ND | ND | Direct suturing | ND | No significant complications | 6 |
| Scaglioni et al 4 | 28 | 54.4 | MPAP; pedicled (n = 26), free (n = 2) | Doppler | 21.9 | Suprafascial | One (n = 26), three (n = 2) | A split‐thickness skin graft | 9 | Total lost (n = 1) | 7 |
| Woo et al 18 | 10 | 64.9 | TDAP; free | Doppler, CT angiography | 50.0 | ND | ND | ND | 11.4 | Partial flap loss (n = 1), venous congestion (n = 1) | 7 |
| Balan et al 19 | 2 | 46.5 | MSAP; free | Doppler | 104 | Subfascial | ND | Graft | ND | No significant complications | 5 |
| Cho et al 20 | 5 | 61.2 | LCAP; free | Doppler | 12.9 | Suprafascial | One | A split‐thickness skin graft | 24.2 | No significant complications | 7 |
| Kim et al 21 | 5 | 56.4 | TDAP; free | CT angiography | 56.8 | ND | ND | Primary closure | 15.2 | Partial necrosis (n = 1), venous congestion (n = 1) | 6 |
| Song et al 22 | 4 | 26.25 | MPAP, FPMAP; pedicled | Doppler | 19.1 | Subfascial | ND | A split‐thickness skin graft | 16 | Skin graft necrosis (n = 1) | 7 |
| Valentin et al 23 | 7 | 64.7 | PMAP, CDAP; pedicled | ND | ND | ND | ND | Directly closed (n = 2), a skin graft (n = 5) | 9.9 | Delayed healing (n = 1) | 7 |
| Akhtar et al 24 | 7 | 39.9 |
PTAP; pedicled |
Doppler | 41.5 | Subfascial | ND | A split‐thickness skin graft | ND | Complete flap loss (n = 1), epidermolysis (n = 1), mild venous congestion (n = 1) | 6 |
| Georgescu et al 25 | 3 | 47 | PAP; pedicled | Doppler | ND | ND | ND | ND | ND | Partial superficial necrosis (n = 1) | 6 |
| Kim et al 26 | 8 | 53.9 | MPAP (n = 5), LPAP (n = 3); pedicled | Doppler | ND | Suprafascial | One (n = 7), two (n = 1) | ND | 13 | Venous congestion (n = 1) | 6 |
| Kim et al 27 | 9 | 48.1 | MSAP; free | Doppler | 72.1 | Subfascial | One (n = 5), two (n = 4) | Primary closure (n = 6), a split‐thickness skin graft (n = 3) | ND | Partial flap loss (n = 1), venous insufficiency (n = 1) | 7 |
| Bhattacharya et al 28 | 8 | 50.3 | PTAP (n = 5), PAP (n = 3); pedicled | Doppler | 167.0 | Subfascial | ND | A split‐thickness skin graft | ND | Marginal necrosis (n = 1) | 7 |
| Koshima et al 29 | 8 | 33.3 | ALTP (n = 7), AMTP (n = 1); free | Doppler | 161.6 | Suprafascial | ND | ND | ND | No significant complications | 6 |
Abbreviations: ALTP, anterolateral thigh perforator; AMTP, anteromedial thigh perforator; CDAP, common digital artery perforator; CT, computed tomographic; FPMAP, first plantar metatarsal artery perforator; LCAP, lateral calcaneal artery perforator; LPAP, lateral plantar artery perforator; MPAP, medial plantar artery perforator; MSAP, medial sural artery perforator; ND, not determined; PAP, peroneal artery perforator; PMAP, plantar metatarsal artery perforator; PTAP, posterior tibial artery perforator; TDAP, thoracodorsal artery perforator.
TABLE 2.
The basic characteristics of patients and flaps
| Features | No. of cases (%) |
|---|---|
| Age (y) | |
| <20 | 10 (9.0) |
| ≥20, <40 | 18 (16.2) |
| ≥40, <60 | 43 (38.7) |
| ≥60 | 40 (36.0) |
| Flap size (cm2) | |
| <25 | 31 (33.3) |
| ≥25, <50 | 25 (26.9) |
| ≥50, <75 | 15 (16.1) |
| ≥75, <100 | 6 (6.5) |
| ≥100 | 16 (17.2) |
| Aetiology | |
| Acute aetiology | 77 (70.6) |
| Chronic aetiology | 32 (29.4) |
| Location of plantar defect | |
| Forefoot | 15 (19.2) |
| Midfoot | 4 (5.1) |
| Hindfoot | 59 (75.6) |
| Preoperative preparation | |
| Doppler | 89 (85.6) |
| CT angiography | 5 (4.8) |
| Both | 10 (9.6) |
| Type of flaps | |
| Free flaps | 41 (36.9) |
| Pedicled flaps | 70 (63.1) |
| No. of perforators | |
| One | 43 (86.0) |
| Two | 5 (10.0) |
| Three | 2 (4.0) |
| Dissection plane | |
| Suprafascial | 49 (62.0) |
| Subfascial | 30 (38.0) |
| Donor site | |
| Primary closure | 20 (24.4) |
| Skin graft | 62 (75.6) |
3.1. Overview of practices
3.1.1. Age
The mean age of the patients was 49.3 ± 19.1 years (range, 6‐84 years). In 36.0% of cases (n = 40), the patients were over 60 years old (Table 2).
3.1.2. Aetiology
Causes of plantar defects were divided into acute and chronic causes (Table 2). Acute causes were those that can cause plantar defects in a short period of time, and chronic causes were those that require a period of development to cause plantar defects. Acute causes (n = 77, 70.6%) included trauma, tumour resection, vascular malformation resection, and burn; chronic causes (n = 32, 29.4%) included ulcer and diabetes mellitus foot. The proportion of all specific causes is shown in Figure 2. Tumour resection (37.6%) was the most common cause of plantar defects, followed by trauma (27.5%).
FIGURE 2.
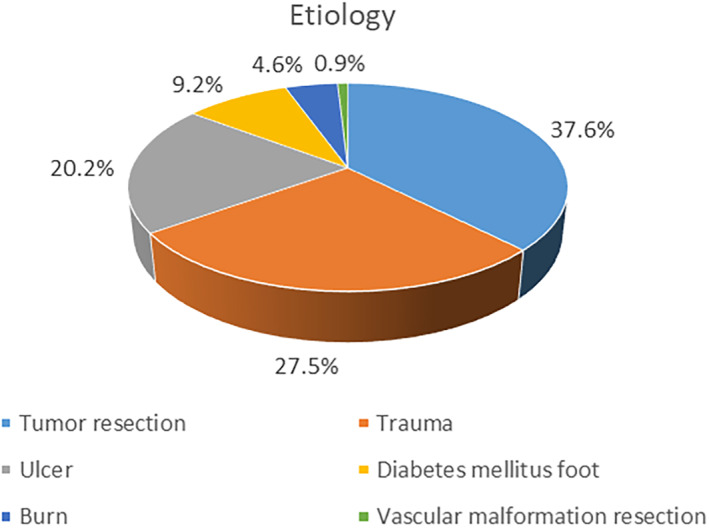
Distribution of causes (in percent)
3.1.3. Location of the defect
In this meta‐analysis, we observed that most plantar defects were at the hindfoot (n = 59, 75.6%), followed by the forefoot (n = 15, 19.2%) and the midfoot (n = 4, 5.1%) (Table 2).
3.1.4. Preoperative preparation
In our study, we observed that most cases (n = 89, 85.6%) used only Doppler ultrasound preoperatively to look for perforators. Surgeons used only CT angiography before operating in 4.8% of cases (n = 5). Besides, Doppler ultrasound and CT angiography were used in 9.6% of cases (n = 10) (Table 2).
3.1.5. Type of flaps
There were two types of perforator flaps for repairing plantar defects: pedicled flaps (n = 70, 63.1%) and free flaps (n = 41, 36.9%) (Table 2). According to the source of perforators, the commonly used pedicled perforator flaps included medial plantar artery perforator (n = 31, 27.9%), peroneal artery perforator (n = 13, 11.7%), posterior tibial artery perforator (n = 12, 10.8%), and lateral plantar artery perforator (n = 3, 2.7%); besides, plantar metatarsal artery perforator flaps and common digital artery perforator flaps were also reported. The most common free perforator flaps were thoracodorsal artery perforator (n = 15, 13.5%), followed by medial sural artery perforator (n = 11, 9.9%), anterolateral thigh perforator (n = 7, 6.3%), lateral calcaneal artery perforator (n = 5, 4.5%), and anteromedial thigh perforator (n = 1, 0.9%).
3.1.6. Flap size
The average size of the flaps was 59.2 ± 60.4 cm2 (range, 6.25‐360 cm2). In 36.8% of the flaps (n = 37), the size was greater than 50 cm2 (Table 2).
3.1.7. Dissection plane
The dissection plane was suprafascial in 62.0% of cases (n = 49), and 38.0% of cases (n = 30) were dissected to the subfascial plane (Table 2).
3.1.8. Number of perforators
Single perforator was retained in 86.0% of perforator flaps (n = 43), two in 10.0% (n = 5), and three in 4.0% (n = 2) (Table 2).
3.1.9. Donor site
The defect of the donor site was covered by a skin graft in most cases (n = 62, 75.6%), and the donor site was closed by primary closure in 24.4% of cases (n = 20) (Table 2). When covering the donor site with a skin graft, most surgeons used a split‐thickness skin graft.
3.1.10. Complications
Complications of perforator flaps are shown in Table 3. The following conditions were considered postoperative complications and included in our study: flap necrosis and related causes; wound dehiscence, incomplete wound coverage, poor healing, and related causes; hematoma, infection, and related causes. Complications related to recipient and donor sites were included in the analysis. We found complications in 13.5% of cases (n = 15). In our study, the most common flap‐related complication was partial necrosis (n = 5, 4.5%), followed by venous congestion (n = 4, 3.6%), complete necrosis (n = 2, 1.8%), epidermolysis (n = 1, 0.9%), venous insufficiency (n = 1, 0.9%), and delayed healing (n = 1, 0.9%). We observed that donor‐site‐related complication was skin graft necrosis (n = 1, 0.9%).
TABLE 3.
Complications of perforator flaps
| Complications | No. of cases (%) a |
|---|---|
| Partial necrosis | 5 (4.5) |
| Complete necrosis | 2 (1.8) |
| Venous congestion | 4 (3.6) |
| Epidermolysis | 1 (0.9) |
| Venous insufficiency | 1 (0.9) |
| Delayed healing | 1 (0.9) |
n = 111 cases.
3.2. Meta‐analysis of risk factors
3.2.1. Flap size over 50 cm2
A total of four studies describing flap size were included in the pooled analysis. The analysis showed no heterogeneity (Chi2 = 1.48, P = .69, I 2 = 0%); thus, a fixed‐effect model was used. The pooled analysis showed a significantly increased risk of complications for flap size greater than 50 cm2 compared with flap size less than 50 cm2 (RR = 3.12, 95% CI = 1.18‐8.23, P = .02) (Figure 3).
FIGURE 3.
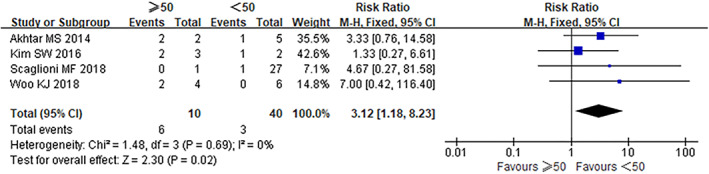
Forest plot for complication risk analysis of flap size over 50 cm2
3.2.2. Aetiology
A total of six studies were included to compare the risk of complications between chronic and acute aetiology. The analysis showed no heterogeneity (Chi2 = 2.92, P = .71, I 2 = 0%); thus, a fixed‐effect model was used. This analysis showed no significant difference in the risk of complications between chronic and acute aetiology (RR = 1.86, 95% CI = 0.84‐4.13, P = .13) (Figure 4). Besides, we performed pooled analyses for complication risk of specific causes, including diabetes mellitus foot, trauma, tumour resection, ulcer, and burn (Table 4). The results showed a significantly increased risk of complications for diabetic foot compared with non‐diabetic foot (RR = 3.26, 95% CI = 1.14‐9.28, P = .03) (Figure 5), while no significant differences were observed regarding other causes.
FIGURE 4.
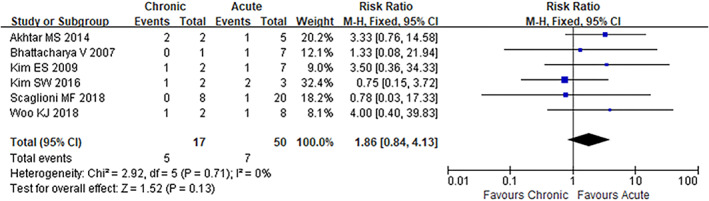
Forest plot for complication risk analysis of chronic aetiology
TABLE 4.
Pooled analysis of specific causes
| Cause | Studies | RR | 95%CI | Heterogeneity test P value and I 2 value | |
|---|---|---|---|---|---|
| Diabetic foot | 4 | 3.26 | (1.14‐9.28) | P = .03 | I 2 = 0% |
| Trauma | 5 | 0.65 | (0.28‐1.54) | P = .33 | I 2 = 37% |
| Tumour resection | 3 | 1.42 | (0.39‐5.22) | P = .60 | I 2 = 41% |
| Ulcer | 3 | 0.87 | (0.23‐3.29) | P = .84 | I 2 = 0% |
| Burn | 3 | 0.84 | (0.28‐2.53) | P = .76 | I 2 = 21% |
Abbreviations: CI, confidence interval; RR, risk ratio.
FIGURE 5.
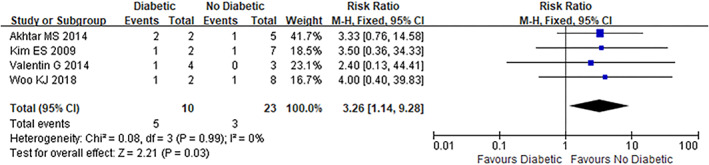
Forest plot for complication risk analysis of diabetic foot
3.2.3. Heel defects
Four studies reporting both heel defects and non‐heel defects were included in this analysis. The analysis showed no heterogeneity (Chi2 = 2.90, P = .41, I 2 = 0%); thus, a fixed‐effect model was used. There was no significant difference in the risk of complications between heel defects and non‐heel defects (RR = 0.56, 95% CI = 0.17‐1.87, P = .34) (Figure 6).
FIGURE 6.
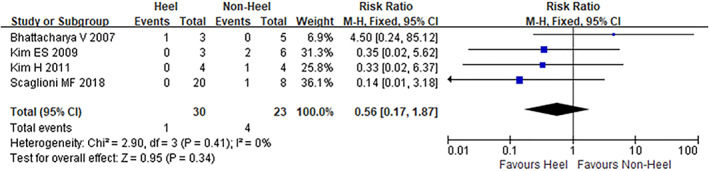
Forest plot for complication risk analysis of heel defects
3.2.4. Single perforator
Three studies were included to compare the risk of complications between single perforator and multiple perforators. This analysis showed no heterogeneity (Chi2 = 0.23, P = .89, I 2 = 0%); thus, a fixed‐effect model was used. No significant difference was found in the risk of complications between single perforator and multiple perforators (RR = 0.64, 95% CI = 0.14‐2.99, P = .57) (Figure 7).
FIGURE 7.
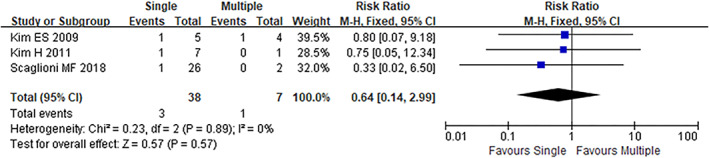
Forest plot for complication risk analysis of single perforator
3.2.5. Age older than 60 years
In this pooled analysis, we evaluated a total of eight studies. The analysis showed no heterogeneity (Chi2 = 4.76, P = .69, I 2 = 0%); thus, a fixed‐effect model was used. There was no significant difference in the risk of complications between patients aged older than, and younger than 60 years (RR = 1.67, 95% CI = 0.78‐3.60, P = .19) (Figure 8).
FIGURE 8.
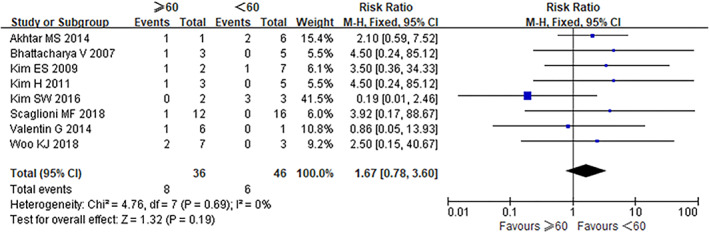
Forest plot for complication risk analysis of age older than 60 years
3.2.6. Assessment of publication bias
Figure 9 shows a funnel plot for flap size over 50 cm2, and Figure 10 for the diabetic foot. These funnel plots are relatively symmetrical, suggesting a low possibility of any publication bias.
FIGURE 9.
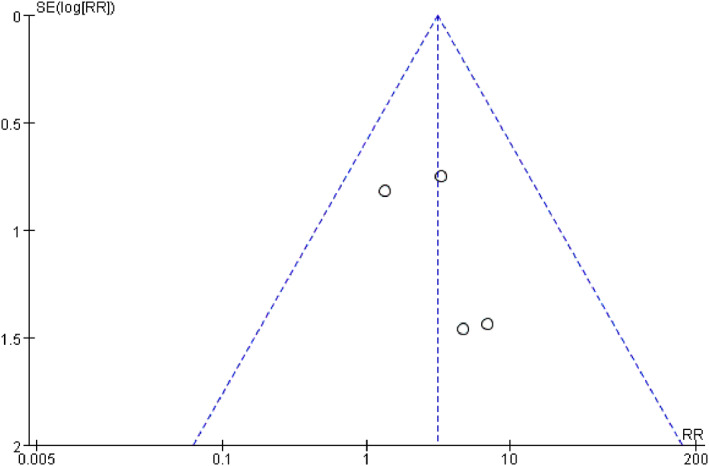
Funnel plot for complication risk analysis of flap size over 50 cm2
FIGURE 10.
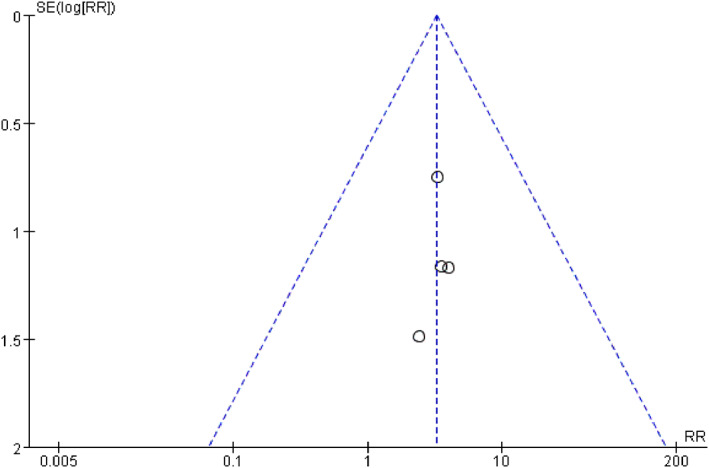
Funnel plot for complication risk analysis of diabetic foot
4. DISCUSSION
Koshima and Soeda 5 first reported the use of an inferior epigastric artery skin flap without rectus abdominis muscle in 1989. Kroll and Rosenfield 30 reported that the blood supply stability of perforator flaps was similar to that of musculocutaneous flaps, but the incidence of donor‐site‐related complications was reduced by retaining muscle tissue. Although many new types and concepts of perforator flaps have been described, perforator flaps are generally divided into pedicled perforator flaps and free perforator flaps. 31 , 32 Pedicled perforator flaps avoid microsurgical techniques and save operating time.
The special anatomical structure of the plantar foot makes plantar defects seriously affect the normal life of the patients. 33 It is a challenging problem for surgeons to repair plantar defects and restore normal functions. Many types of flaps are used to reconstruct plantar defects, but few can support the weight of the human body. So far, perforator flaps have been widely used in the repair of defects various in location and size, 34 , 35 and have been successfully used to repair plantar defects. As far as we know, up until now, no meta‐analysis has focused on the risk factors for complications of perforator flaps in plantar reconstruction.
The results of our study indicated that flap size over 50 cm2 increased the risk of postoperative complications. The risk of complications of large perforator flaps may be related to insufficient blood perfusion, and maintaining good blood perfusion of the flaps is a challenge that many surgeons face. When a large perforator flap is needed, obtaining a good appearance and normal function of the donor site is also a problem. The donor site of a large pedicled perforator flap may look good for older patients with sagging skin but maybe ugly for younger patients with delicate skin. Therefore, free flaps from other parts of the body may be a better option for repairing extensive plantar defects. 36 , 37 , 38 When flap size is over 50 cm2, we recommend that surgeons fully consider all treatments and then choose the most appropriate one based on the patient's condition and the surgeon's experience and ability.
According to our study, diabetic foot increased the risk of postoperative complications compared with non‐diabetic foot. Because of problems such as vascular disease, neuropathy, and immunopathy, diabetic patients are at greater risk of limb ischaemia, often with severe soft tissue defects. 39 , 40 In diabetic patients, reduced tissue perfusion can be secondary to injury in the macrocirculation or microcirculation. 41 Diabetic patients are susceptible to serious infections, making wound healing more difficult. 42 Increasing blood perfusion and avoiding infection when reconstructing plantar defects in diabetic patients is a challenge that surgeons face. For intractable diabetic foot, surgeons need to consider all possible methods and choose the best method. Combination therapy can be used if necessary.
The heel bears the force of standing and walking, and the reconstruction of the heel is a challenging problem. In our study, most defects were at the heel, and heel defects did not increase the risk of postoperative complications compared with other plantar defects.
About 400 perforators are connecting the epidermis in the human body, and each perforator can be used to design a pedicled perforator flap. 32 The more perforators a flap retains, the better the flap's blood supply; however, too many perforators may limit the movement of the flap and pedicle rotation. 43 According to the results of our study, a single perforator did not increase the risk of complications compared with multiple perforators. The data included in our study were limited and more high‐quality studies are needed to validate our findings. Chang et al 44 described that the size of perforator flaps, including a single perforator, should be limited to 8 cm by 20 cm. If a larger perforator flap is required, the flap may need to retain two or more perforators. Surgeons should determine the number of perforators that need to be retained based on the size of the perforator flap, distance of movement, and angle of pedicle rotation.
The results of the meta‐analysis showed that patients aged older than 60 years did not increase the risk of complications. However, older patients are more likely to have diseases that affect prognosis, such as diabetes, nerve disease, vascular disease, and infection. Research by Sanak et al 45 showed that age was not an independent variable that increased the risk of microvascular reconstruction, while the time of surgery, the American Society of Anaesthesiologists (ASA) risk score, and the location of reconstruction were related to the success rate of free tissue transfer. For older patients, surgeons should deal with the underlying disease before surgery and make reconstruction decisions based on the specific physical condition of the patients.
In our research, chronic causes included ulcer and diabetes mellitus foot; acute causes included trauma, tumour resection, vascular malformation resection, and burn. This analysis showed no significant difference in the risk of complications between chronic and acute causes. Our study also analysed the relationship between specific causes and complications. Trauma, ulcer, tumour resection, and burn did not increase the risk of postoperative complications, while diabetes mellitus foot had an increased risk of complications. It should be noted that different causes require different treatment methods. Treatment for plantar tumours should be chosen based on the size, location, and depth of the tumour. In the case of a malignant tumour, extended excision is necessary. 1 For plantar defects caused by acute trauma, a thorough debridement should be performed and then treatment should be determined according to the specific situation. 27 The common causes of ulcer are venous disease, arterial disease, and nerve disease. Because many factors can cause ulcer, multidisciplinary knowledge is needed to assess patients, identify the aetiology, and choose the optimal treatment. 46 In addition to the assessment, treatment, and repair of burn wounds, surgeons should also pay attention to anti‐shock, improve breathing, prevent infection, and replenish nutrition.
In our study, the dissection plane was suprafascial in most cases. Because of the lack of relevant studies, this meta‐analysis was unable to analyse the correlation between the dissection plane and complications. Brunetti et al 47 suggested that dissection and separation of perforators at the subfascial plane would be preferred to obtain flaps of the limbs. Through the subfascial approach, perforators can be observed more clearly and flaps can be raised more quickly. Research by Chen et al 48 showed that less sensory disturbance of donor site and higher patient satisfaction follow suprafascial anterolateral thigh flap.
Most donor site defects were repaired with skin grafts, followed by primary closures. When covering the donor site with a skin graft, most surgeons used a split‐thickness skin graft. When the donor site defect is small, surgeons prefer primary closure. For older patients with sagging skin, large defects in the donor site may also be repaired by primary closure. For donor site defects that cannot be closed by primary closure, the use of skin grafts is a good choice. Most surgeons used split‐thickness skin grafts because they are tough, soft, resistant to friction, and strong in vitality.
The present meta‐analysis has the following limitations that must be taken into account: (a) Only studies published in English were included; thus, our study may have lost data on important studies published in other languages. (b) Surgical procedures in different studies were performed by doctors at different levels of operation, and there may be potential bias. (c) Because of the insufficient sample size in the included studies, there may be bias. (d) Because of limited studies included, data on skeletonisation of perforators, pedicle rotation, pedicle length were lacking. (e) All the included studies were retrospective studies, and a randomised controlled trial can validate and complement our findings.
5. CONCLUSION
This meta‐analysis identified two risk factors‐namely, flap size over 50 cm2 and diabetes mellitus foot‐for postoperative complications of perforator flaps in plantar reconstruction. Surgeons should consider the two risk factors before operating, and choose the best option for reconstruction based on the patient's specific situation and the doctor's experience. More high‐quality studies with adequate sample sizes are needed to validate and complement our findings.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
ACKNOWLEDGEMENTS
All authors were involved in the study design and the writing of the article and have no financial interest to declare in relation to the content of this article.
Zhang W, Li X, Li X. A systematic review and meta‐analysis of perforator flaps in plantar defects: Risk analysis of complications. Int Wound J. 2021;18:525–535. 10.1111/iwj.13552
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Wang M, Xu Y, Wang J, et al. Surgical Management of Plantar Melanoma: a retrospective study in one center. J Foot Ankle Surg. 2018;57(4):689‐693. [DOI] [PubMed] [Google Scholar]
- 2. Stecco C, Corradin M, Macchi V, et al. Plantar fascia anatomy and its relationship with Achilles tendon and paratenon. J Anat. 2013;223(6):665‐676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Löfstrand JG, Lin C. Reconstruction of defects in the weight‐bearing plantar area using the innervated free medial plantar (instep) flap. Ann Plast Surg. 2018;80(3):245‐251. [DOI] [PubMed] [Google Scholar]
- 4. Scaglioni MF, Rittirsch D, Giovanoli P. Reconstruction of the heel, middle foot sole, and plantar forefoot with the medial plantar artery perforator flap. Plast Reconstr Surg. 2018;141(1):200‐208. [DOI] [PubMed] [Google Scholar]
- 5. Koshima I, Soeda S. Inferior epigastric artery skin flaps without rectus abdominis muscle. Br J Plast Surg. 1989;42(6):645‐648. [DOI] [PubMed] [Google Scholar]
- 6. Wei FC, Celik N. Perforator flap entity. Clin Plast Surg. 2003;30(3):325‐329. [DOI] [PubMed] [Google Scholar]
- 7. Kim JT, Kim SW. Perforator flap versus conventional flap. J Korean Med Sci. 2015;30(5):514‐522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ono S, Hayashi H, Ohi H, Ogawa R. Imaging studies for preoperative planning of perforator flaps. An overview. Clin Plast Surg. 2017;44(1):21‐30. [DOI] [PubMed] [Google Scholar]
- 9. Scaglioni MF, Giuseppe AD, Chang EI. Propeller flap reconstruction of abdominal defects: review of the literature and case report. Microsurgery. 2015;35(1):72‐78. [DOI] [PubMed] [Google Scholar]
- 10. Mardini S, Tsai FC, Wei FC. The thigh as a model for free style free flaps. Clin Plast Surg. 2003;30(3):473‐480. [DOI] [PubMed] [Google Scholar]
- 11. Feng KM, Hsieh CH, Jeng SF. Free‐style puzzle flap: the concept of recycling a perforator flap. Plast Reconstr Surg. 2013;131(2):258‐263. [DOI] [PubMed] [Google Scholar]
- 12. Mohan AT, Sur YJ, Zhu L, et al. The concepts of propeller, perforator, keystone, and other local flaps and their role in the evolution of reconstruction. Plast Reconstr Surg. 2016;138(4):710e‐729e. [DOI] [PubMed] [Google Scholar]
- 13. Maciel‐Miranda A, Morris SF, Hallock GG. Local flaps, including pedicled perforator flaps: anatomy, technique, and applications. Plast Reconstr Surg. 2013;131(6):896e‐911e. [DOI] [PubMed] [Google Scholar]
- 14. Stang A. Critical evaluation of the Newcastle‐Ottawa scale for the assessment of the quality of nonrandomized studies in meta‐analyses. Eur J Epidemiol. 2010;25(9):603‐605. [DOI] [PubMed] [Google Scholar]
- 15. Gu WJ, Wang F, Tang L, Liu JC. Single‐dose etomidate does not increase mortality in patients with sepsis: a systematic review and meta‐analysis of randomized controlled trials and observational studies. Chest. 2015;147(2):335‐346. [DOI] [PubMed] [Google Scholar]
- 16. Bekara F, Herlin C, Somda S, de Runz A, Grolleau JL, Chaput B. Free versus perforator‐pedicled propeller flaps in lower extremity reconstruction: what is the safest coverage? A meta‐analysis. Microsurgery. 2018;38(1):109‐119. [DOI] [PubMed] [Google Scholar]
- 17. Zheng J, Liao H, Li J, et al. Double‐pedicle propeller flap for reconstruction of the foot and ankle: anatomical study and clinical applications. J Int Med Res. 2019;47(10):4775‐4786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Woo K, Park J, Mun G. The lateral calcaneal artery as an alternative recipient vessel option for heel and lateral foot reconstruction. Microsurgery. 2018;38(2):164‐171. [DOI] [PubMed] [Google Scholar]
- 19. Balan JR. Medial sural artery perforator free flap for the reconstruction of leg, foot and ankle defect: an excellent option. ANZ J Surg. 2018;88(3):E132‐E136. [DOI] [PubMed] [Google Scholar]
- 20. Cho SW, Park JU, Kwon ST. Availability of the lateral calcaneal region as a donor site of free flaps. Microsurgery. 2017;37(6):494‐501. [DOI] [PubMed] [Google Scholar]
- 21. Kim SW, Youn DH, Hwang KT, Sung IH, Kim JT, Kim YH. Reconstruction of the lateral malleolus and calcaneus region using free thoracodorsal artery perforator flaps. Microsurgery. 2016;36(3):198‐205. [DOI] [PubMed] [Google Scholar]
- 22. Song D, Yang X, Wu Z, et al. Anatomic basis and clinical application of the distally based medialis pedis flaps. Surg Radiol Anat. 2016;38(2):213‐221. [DOI] [PubMed] [Google Scholar]
- 23. Valentin G, Rodica M, Manuel L. Plantar flaps based on perforators of the plantar metatarsal/common digital arteries. J Reconstr Microsurg. 2014;30(07):469‐474. [DOI] [PubMed] [Google Scholar]
- 24. Akhtar MS, Khurram MF, Choudhary R, Khan AH, Ahmad I. Distally based posterior tibial artery perforator flap for coverage of defects around the ankle, heel and lower third of leg. Eur J Plast Surg. 2014;37(10):547‐554. [Google Scholar]
- 25. Georgescu AV, Matei IR, Capota IM. The use of propeller perforator flaps for diabetic limb salvage: a retrospective review of 25 cases. Diabet Foot Ankle. 2012;3(1):18978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kim H, Pyon JK, Lim SY, Mun GH, Bang SI, Oh KS. Perforator‐based Pacman flap in the plantar region. J Foot Ankle Surg. 2011;50(6):747‐750. [DOI] [PubMed] [Google Scholar]
- 27. Kim ES, Hwang JH, Kim KS, Lee SY. Plantar reconstruction using the medial sural artery perforator free flap. Ann Plast Surg. 2009;62(6):679‐684. [DOI] [PubMed] [Google Scholar]
- 28. Bhattacharya V, Reddy GR, Goyal S, Kumar U. Skeletonised retrograde distal perforator Island fasciocutaneous flaps for leg and foot defects. J Plast Reconstr Aesthet Surg. 2007;60(8):892‐897. [DOI] [PubMed] [Google Scholar]
- 29. Koshima I, Fujitsu M, Ushio S, Sugiyama N, Yamashita S. Flow‐through anterior thigh flaps with a short pedicle for reconstruction of lower leg and foot defects. Plast Reconstr Surg. 2005;115(1):155‐162. [PubMed] [Google Scholar]
- 30. Kroll SS, Rosenfield L. Perforator‐based flaps for low posterior midline defects. Plast Reconstr Surg. 1988;81(4):561‐566. [DOI] [PubMed] [Google Scholar]
- 31. Claes KE, Roche NA, Opsomer D, et al. Free flaps for lower limb soft tissue reconstruction in children: systematic review. J Plast Reconstr Aesthet Surg. 2019;72(5):711‐728. [DOI] [PubMed] [Google Scholar]
- 32. Abraham JT, Saint‐Cyr M. Keystone and pedicle perforator flaps in reconstructive surgery: new modifications and applications. Clin Plast Surg. 2017;44(2):385‐402. [DOI] [PubMed] [Google Scholar]
- 33. Lykoudis EG, Seretis K, Lykissas MG. Free sensate medial plantar flap for contralateral plantar forefoot reconstruction with flap reinnervation using end‐to‐side neurorrhaphy: a case report and literature review. Microsurgery. 2012;33(3):227‐231. [DOI] [PubMed] [Google Scholar]
- 34. Chang S, Zhang F, Xu D, et al. Lateral retromalleolar perforator‐based flap: anatomical study and preliminary clinical report for heel coverage. Plast Reconstr Surg. 2007;120(3):697‐704. [DOI] [PubMed] [Google Scholar]
- 35. Bannasch H, Strohm PC, Al Awadi K, et al. Technical refinements of composite thoracodorsal system free flaps for 1‐stage lower extremity reconstruction resulting in reduced donor‐site morbidity. Ann Plast Surg. 2008;60(4):386‐390. [DOI] [PubMed] [Google Scholar]
- 36. Acland RD. Refinements in lower extremity free flap surgery. Clin Plast Surg. 1990;17(4):733‐744. [PubMed] [Google Scholar]
- 37. Wettstein R, Schurch R, Banic A, et al. Review of 197 consecutive free flap reconstructions in the lower extremity. J Plast Reconstr Aesthet Surg. 2008;61(7):772‐776. [DOI] [PubMed] [Google Scholar]
- 38. Godina M. Early microsurgical reconstruction of complex trauma of the extremities. Plast Reconstr Surg. 1986;78(3):285‐292. [DOI] [PubMed] [Google Scholar]
- 39. Ohta M, Ikeda M, Togo T, Suzuki S. Limb salvage of infected diabetic foot ulcers with free deep inferior epigastric perforator flaps. Microsurgery. 2006;26(2):87‐92. [DOI] [PubMed] [Google Scholar]
- 40. Randon C, Vermassen F, Jacobs B, de Ryck F, van Landuyt K, Taes Y. Outcome of arterial reconstruction and free‐flap coverage in diabetic foot ulcers: long‐term results. World J Surg. 2010;34(1):177‐184. [DOI] [PubMed] [Google Scholar]
- 41. Tchanque‐Fossuo CN, Wishy AM, West KIM, Dawson DL, Dahle SE, Carson JG. Reclaiming autologous amputated tissue for limb salvage of a diabetic foot burn with underlying critical limb ischemia. Adv Skin Wound Care. 2018;31(1):596‐600. [DOI] [PubMed] [Google Scholar]
- 42. Özkan Ö, Coşkunfirat OK, Özgentaş HE. Reliability of free‐flap coverage in diabetic foot ulcers. Microsurgery. 2005;25(2):107‐112. [DOI] [PubMed] [Google Scholar]
- 43. Wolff KD. Perforator flaps: the next step in the reconstructive ladder? Br J Oral Maxillofac Surg. 2015;53(9):787‐795. [DOI] [PubMed] [Google Scholar]
- 44. Chang C, Wong C, Wei F. Free‐style free flap. Injury. 2008;39(3):57‐61. [DOI] [PubMed] [Google Scholar]
- 45. Sacak B, Akdeniz ZD, Certel F, et al. Risk assessment for free tissue transfers: is old age a determining factor? J Craniofac Surg. 2015;26(3):856‐859. [DOI] [PubMed] [Google Scholar]
- 46. Agale SV. Chronic leg ulcers: epidemiology, aetiopathogenesis, and management. Ulcers. 2013;2013:1‐9. [Google Scholar]
- 47. Brunetti B, Tenna S, Aveta A, Segreto F, Persichetti P. Free‐style local perforator flaps: versatility of the V‐Y design to reconstruct soft‐tissue defects in the skin cancer population. Plast Reconstr Surg. 2013;132(2):451‐460. [DOI] [PubMed] [Google Scholar]
- 48. Chen YC, Scaglioni MF, Carrillo JL, et al. Suprafascial anterolateral thigh flap harvest: a better way to minimize donor‐site morbidity in head and neck reconstruction. Plast Reconstr Surg. 2016;138(3):689‐698. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


