Abstract
Introduction:
The COVID-19 pandemic has imposed an extraordinary challenge to the health and socio-economic facet of nations globally. Health facilities have encountered tremendous challenges to contain service delivery at all levels. This study aims to assess the trend of health service utilization and challenges faced during the COVID-19 pandemic at primary units in Addis Ababa, Ethiopia.
Method:
A multi-facility-based cross-sectional study was conducted in Addis Ababa between 1 and 30 of August 2020. A mixed-methods design was employed, and both quantitative and qualitative data were collected at 5 health centers. Facilities were selected randomly from 5 sub-cities while interviewees were recruited purposively. A structured questionnaire was used to collect quantitative data from the HMIS units of each facility. Qualitative data was collected using a semi-structured key-informant interview guide. Quantitative data were analyzed using Microsoft Excel, and a 10-month time-series trend was generated. For the qualitative data, qualitative data analysis (QDA-minor) software was used.
Results:
Time-series comparison of the pre-COVID-19 era loads with the COVID-19 period showed that there was an extensive disparity in the service delivery capacity of the health facilities. A huge drop in inpatient flow of some units such as PICT, VCT, FP services, and most sub-units of the OPDs has been recorded following the COVID-19 outbreak. The key-informant interview also revealed that such challenges, as fear of infection and stigma, poor infrastructure, challenges related to human resources, and challenges related to the supply of prevention and treatment inputs were prominently encountered at the health centers.
Conclusion:
The COVID-19 wave has negatively impacted many service delivery points in the study settings. The presence of weak infrastructure, lack of PPEs, fear of the infection and stigma, and staff workload have been mentioned as the predominant challenges faced during the outbreak. Health authorities should arrange multifaceted supports to ensure uninterrupted service delivery at primary healthcare units.
Keywords: Ethiopia, COVID-19, challenges, health service utilization, primary healthcare unit
Introduction
The novel coronavirus, also known as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has brought about devastating consequences in the health, 1,2 economy, 2,3 social life, 4 as well as the health infrastructure, 5,6 globally. First originated in the Chinese city of Wuhan in December 2019, 7 the COVID-19 pandemic has infected over 79.2 million and killed over 1.7 million people during its 1-year surge. 8 The effects on health outcomes could be reflected either directly through imposing morbidity and mortality or indirectly through affecting the healthcare service delivery practice to non-COVID-19 suspect patients.
A significant level of service delivery has been reported to be impacted, especially, during early times owing to the steady spread of the virus across all settings. Despite optimism on the cumulative effects of the pandemic in Sub-Saharan Africa compared to the developed nations, the situation had got much worse expectation of altered health service disruptions attributed to the pre-existing poor health infrastructure and system in the region. Whereas a huge number of essential services have been delayed by the healthcare facilities, 9 -11 patients were also unable to attend follow-ups and acute care visits due to the fear and anxiety they experienced during the pandemic waves. 12 Some health setups have changed their mode of service delivery to accord with preventive strategies and local policies 13 -15 and preparing new protocols that maintain service and reduce contamination. 16
In Ethiopia, following the first COVID-19 reported case in March 2020, the trend curve has exhibited a fluctuating daily tolls overtime with the highest ever figures being 1733 and 2163 cases in August 2020 and April 2021 respectively. As of 15th June 2021, a cumulative 274614 cases and 4264 deaths have been reported. 17 However, both figures showed a remarkable drop in the same month which also was in agreement with the global trend (12% and 2% decline of infection and fatality rates respectively). 17 Though local mobility restrictions are eased in Ethiopia, gatherings above 50 persons are not allowed at all settings, and anyone who suspects to having acquired the virus should report to the ministry of health (MOH) as soon as possible. So far, international travelers without a negative RT-PCR test result are not permitted to boarding a flight for entry, exit or transit, while those who entered the country are expected to stay-home for 2 weeks before mixing with others. 18
Up until now, the government of Ethiopia had tried to continue existing healthcare services along with preventive rules and awareness packages. 19 Nonetheless, some hospitals shrunk their regular roles and shifted to serve as isolation and treatment centers. 20 The decline in the patient flow of selected service units, such as family planning, emergency, and chronic care units has been reported to be an area of concern in the Northeastern part of the country. 21 Paralleling to these were, the spread of false information on the transmission and treatment of the virus, framed COVID-19 related conspiracies, and claims of herbal medicines with presumed effect against the COVID-19 virus. Yet, despite the shortage of medicines and preventive supplies, frontline healthcare workers and Pharmacists have played a substantial role to inform the public and render essential services. 22
The reports documented in the literature often cover high-level settings, where patients are often referred to, after being seen at lower (primary care) units. The situation, during the COVID-19 era, might exhibit a quite distinct pattern at primary care units, at least in terms of patient flow, service quality, availability of inputs, and level of preparedness to combat the pandemic. As patients got scared of attending hospitals and the tendency to cancel elective services and admitting COVID-19 suspects grew at such settings, a remaining plausible option could be to visit local health centers and community pharmacies for potential refills and treating of acute illnesses if not absent at all.
Due to the lack of aggregate findings that depict the magnitude of negative impacts following the COVID-19 wave in Addis Ababa, Ethiopia, the present study has considered the importance of assessing healthcare service delivery practices at primary healthcare units. Taking into account the socio-economic variation in all sub-cities, the study was conducted at 5 health centers to evaluate the presence of potential disparities of service uptake both before and during the pandemic. Besides, the challenges encountered by the health facilities have also been explored.
Methods
Study Setting, Design, and Period
The study was conducted in Addis Ababa, the capital of Ethiopia, and headquarters of the African Union Commission (AUC). It has a total population of over 5.03 million projected for 2020. 23 There are about 103 health centers administered under the city government (AAHB). 24 In the Ethiopian health system, health centers are structured at the lower tier expected to deliver primary healthcare services for about 5000 to 40000 catchment populations. These services may include family planning, minor surgical services, reproductive health, outpatient, antiretroviral therapy (ART), emergency abortion, non-communicable disease follow-up services, and inpatient among others. A cross-sectional study was conducted at 5 health centers located in Addis Ababa. These were; Arada, Lideta, Nifas Silk Lafto Wereda 9, Akaki Kality, and Bulbula health center. The study was conducted between 1 and 30 of August 2020.
Population, Sample Size, and Sampling Technique
The populations in this evaluation considered all the selected departments namely; ART, ANC, OPD, IPT, abortion care, VCT, PICT, delivery, family planning, and immunization. The monthly patient loads from these units were evaluated based on a 10-month time-series trend analysis comparing figures before and during the COVID-19 era. Also, 20 key-informant interviewees (KIIs) were included from selected departments namely; disease prevention, OPD, IPT, and pharmacy units. Health centers were selected with a simple random sampling method while service units were selected purposively with a high likelihood of service disruption and patient load drop as a result of the pandemic. Likely, key-informants were recruited based on presumed involvement in decision making, a saturation of obtaining new insights, and experience of the KIIs to lead the units both before and during the COVID-19 spread.
Data Collection Instrument, Procedure, and Analysis
For the time-series quantitative analysis, a structured data collection format was used to retrieve average monthly loads from health management information system (HMIS) units of each health center. A 10 months review period, starting from September 2019 to July 2020, was considered in this evaluation. Two trained health officers were employed in the quantitative data collection whereas qualitative data was collected by the principal investigator (PI). A semi-structured KII guide was employed to collect the qualitative data. Interviews were undertaken in the Amharic language (official working language in Ethiopia), transcribed verbatim, and back-translated to English. A semi-structured interview-guide was used with broader questions including; what challenges is the health facility facing during the COVID-19 pandemic? What solutions did the facility place to the challenges mentioned? Apart from the efforts done by the facility/organization, which parties do you suggest to engage in tackling the challenges? Do you like to add any idea or more suggestions uncovered? When elaboration was sought in line with quantitative trends or at times of emergent ideas, KIIs were offered with probing questions to further their viewpoints. KIIs were undertaken at respondents’ preferred settings, including offices, waiting rooms, and open spaces. At 2 health centers all, except pharmacists, were interviewed as groups. All the time, the interview/discussions were initiated with friendly introductions, openly explaining purpose of the study, and engaging participants as indispensable part of the healthcare cadre who might have experienced challenges during the pandemic-hence who should have something in mind. The PI doing this qualitative exploration has an earlier experience to carrying out qualitative interviews, transcription, and analysis. Quantitative data were analyzed using Microsoft excel while qualitative data analysis minor (QDA-minor) was used for the qualitative part. Results were presented using trend lines and thematic narrations.
Ethical Approval
Ethical approval to conducting the study was obtained at 2 levels. Initially, ethical clearance and a letter of support were sought from the institutional review board (IRB) of Saint Paul’s Hospital Millennium Medical College (SPHMMC). Next, the city government health bureau of Addis Ababa had reviewed and, issued a letter of support addressed to the respective health facilities. Informed verbal consent was sought from all KIIs and facility representatives. No individual or facility-specific data or identifiers were collected in the process. The analysis was done in aggregate, and figures were presented in trend lines.
Results
Health Service Utilization at Health Centers
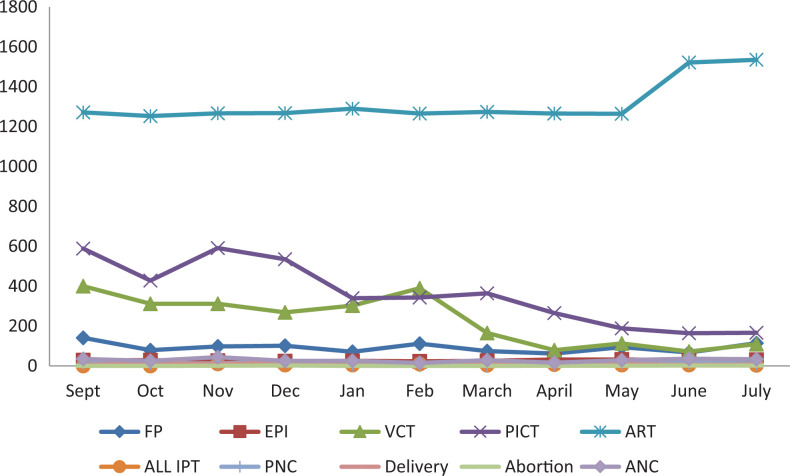
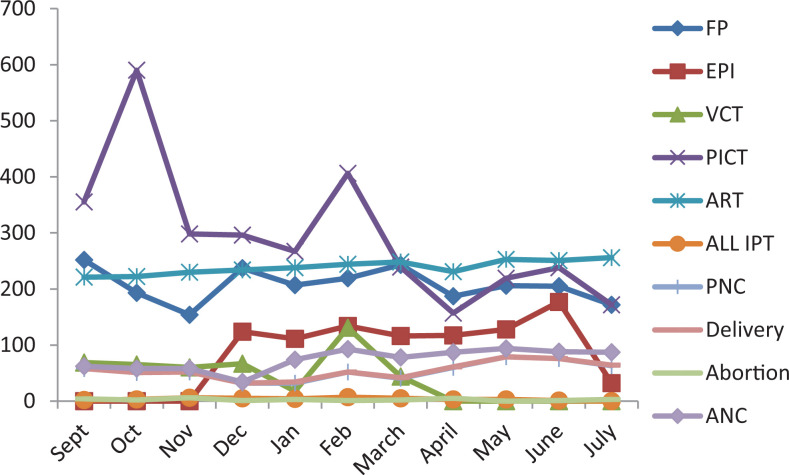
The rate of service utilization over 10 months was reviewed in one of the health centers in the Arada sub-city. Antiretroviral therapy (ART) service delivery showed a steady flow of patients after the COVID-19 pandemic with a substantial increase after May. Provider initiated counseling and testing (PICT) showed a downward sloping curve since December. On the other hand, voluntarily counseling and testing services showed a marked decrease from February. Delivery and Post-natal care service uptake have also diminished since January. Other services, such as emergency abortion, expanded program of immunization (EPI), and prenatal care services did not show a notable change during the outbreak (Figure 1).
Figure 1.
Service utilization trend at different departments during pre and post COVID-19 pandemic, August 2020 (Health center 1, Arada sub-city). Abbreviations: FP, family planning; EPI, expanded program of immunization; VCT, voluntary counseling, and testing; PICT, provider initiated counseling, and testing; ART, antiretroviral therapy; IPT, inpatient; PNC, postnatal care; ANC, antenatal care.
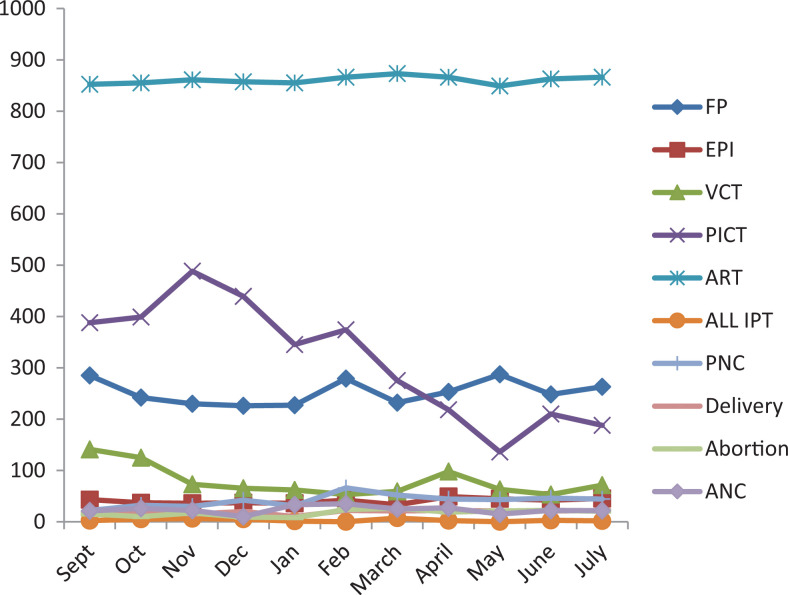
An inspection of antiretroviral therapy (ART) service utilization at a health center in the Lideta sub-city showed no deviation from the usual number of cases over the review period. Provider initiated counseling and testing (PICT) services showed a significant depression since February. Emergency abortion visits were lower in December and January. There was no that change in inpatient admissions, ante-natal care (ANC) post-natal care (PNC), and delivery services that occurred in the health center (Figure 2).
Figure 2.
Service utilization trend at different departments before and during COVID-19 pandemic, August 2020 (Health center 2, Lideta sub-city).
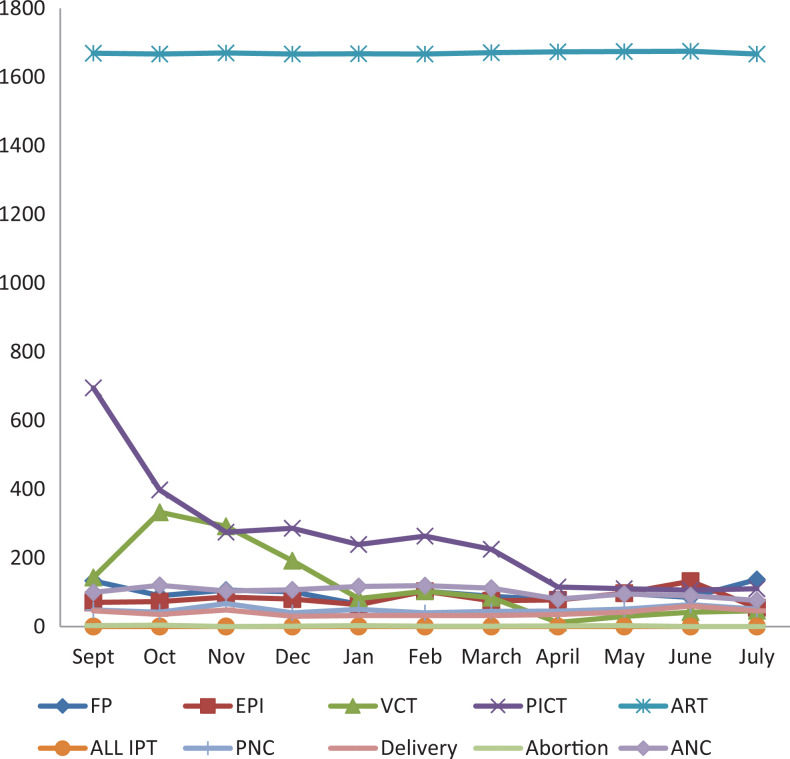
In a similar fashion as earlier, ART services in the Nifas Silk Lafto sub-city were found to retain a consistent trend. On the other hand, PICT, VCT, and family planning (FP) services also dropped in March and the subsequent months. Utilization of most health care services, such as FP, EPI, and VCT showed a significant fall during January (Figure 3).
Figure 3.
Service utilization trend at different departments before and during the COVID-19 pandemic, August 2020 (Health center 3, Nifas Silk Lafto sub-city).
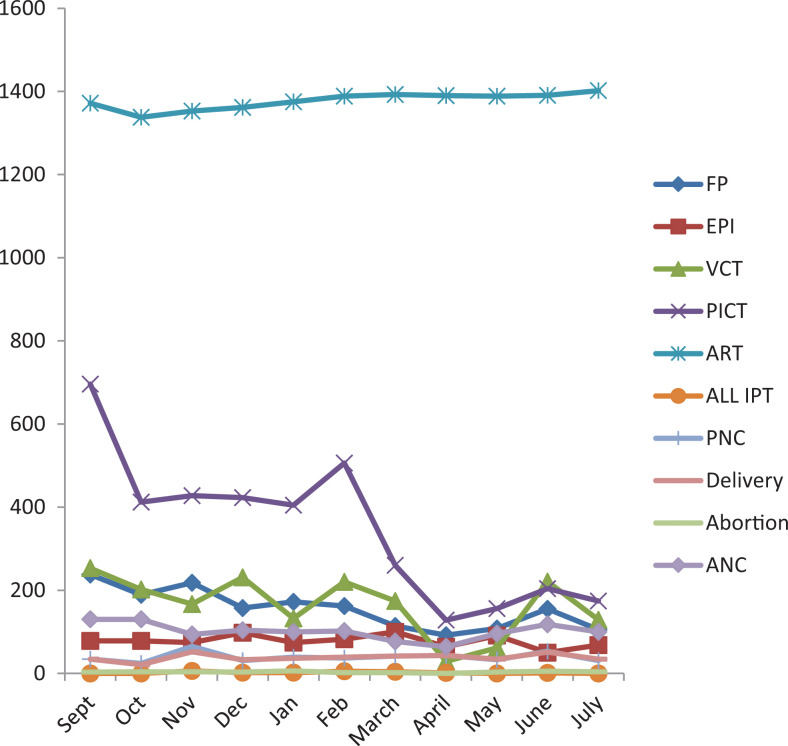
A review of health service utilization in one of the health centers in the Kality sub-city showed that most of the services at VCT, ART, inpatient, prenatal care, emergency abortion, delivery, and post-natal care units were not affected during the COVID-19 pandemic. An extensive fall in family planning uptake was noted early since December with a gradual decrease in the COVID-19 period. In contrast, an inspection of PICT service delivery revealed that a substantial decrement, in the number of uptakes, was recorded from February onward (Figure 4).
Figure 4.
Service utilization trend at different departments before and during the COVID-19 pandemic (Health center 4, Akaki Kality sub-city).
Figure 5 below shows the trend of service uptake at different departments of a health center in the Bole sub-city. Even though ART programs sustained a steady patient flow throughout the review period, PICT service experienced a maximum disruption due to the pandemic since its ever peak in February. Some services, such as antenatal care, delivery, postnatal care, and EPI showed a consistent flow after March to the end, except for EPI programs with a radical fall in the summer season. Services on VCT and FP were found to exhibit a downward sloping curve since February and March respectively with VCT lowest ever in the number of monthly visits after April (Figure 5).
Figure 5.
Service utilization trend at different departments before and during the COVID-19 pandemic, August 2020 (Health center 5, Bole sub-city).
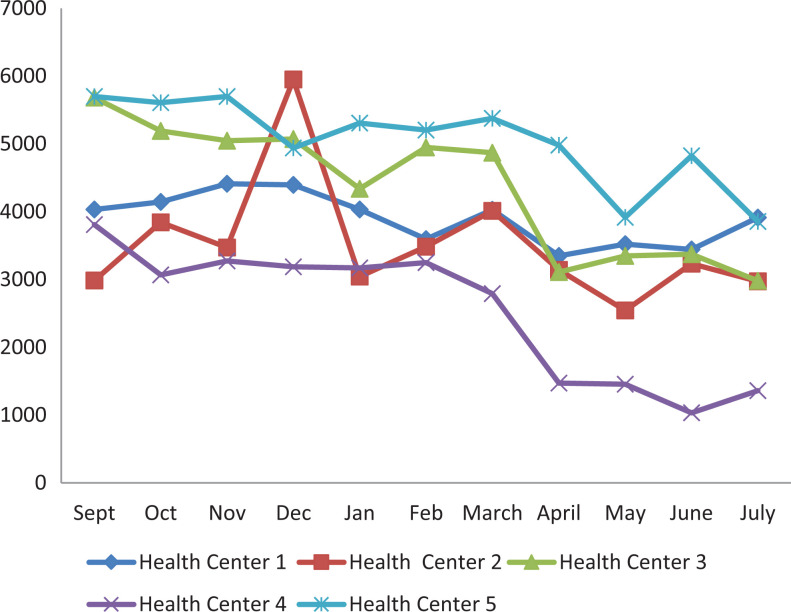
An additional interest in the present study was also to compare the relative change in the trend of outpatient service utilization per the selected health facilities. The lowest number of outpatient visits in health center 1 was recorded in February and April even though decline started to occur early in December. Though highest ever number of visits in December, patient flow in health center 2 plunged significantly in the next months until the end of the review period. Inspection of outpatient flows for the third health center showed that a sudden fall was apparent in January. Meanwhile, a sharp drop in the number of cases was noted in the months following March. In the same manner, the health centers reported a quite low number of outpatient visits in March, followed by a prominently shrunk flow from April onward. Considering health center 5, a sustained number of visits were noted until March as compared to the same figure in December. Nonetheless, this number has tended to decline in the months to follow with the lowest record in May and July (Figure 6).
Figure 6.
Service utilization trend at outpatient departments of health centers before and during the COVID-19 pandemic.
Challenges Faced During the COVID-19 Pandemic
Key-Informants and Themes
All of the 20 key-informants (KIs) (9 females and 11 males) were successfully interviewed to explore challenges encountered at the selected health centers. KIs were of in the age range 30 to 52 years with an overall work experience of 6 to 28 years, and a diverse professional mix namely; pharmacists, clinical nurses and public health officers. Further, all interviewees were department or unit leaders of either the pharmaceutical care and supply chain management, disease prevention and health promotion, inpatient, and outpatient medical services or any combination.
The key-informant interviews have revealed that a multitude of challenges had faced the public health facilities and patients during the COVID-19 pandemic. Through a thematic content analysis, challenges related to 9 individual sub-themes have been identified. These were; patients fear of the COVID-19 infection, increased new/undiagnosed chronic cases in the facility, shortage of staff and increased workload, lack of supplies and medications, lack of facility space, the possibility for high transmission of the COVID-19, a challenge from “suspect stay at home” rules, lack of incentives to health professionals, and frustration and stigma of health professionals. Four main themes namely; challenges related to fear of infection and stigma, poor infrastructure, challenges related to human resources, and challenges related to the supply of prevention and treatment inputs were generated.
Challenges Related to Fear of Infection and Stigma
The key informants in the current study mentioned that patients’ fear of acquiring the COVID-19 infection at the health facilities was one major reason for poor patient flows in case of new infections and follow-up visits for chronic illnesses. This challenge was also highly pronounced during the early months of the pandemic they claimed. On the other hand, some patients and health professionals were reported to have experienced stigma, especially, following recovery from the COVID-19 infection and being suspected of working in high-risk areas. They said that the stigma and discrimination by some community members (for example renters and neighbors) and staff (even from close colleagues) caused frustration in their daily practices.
Poor Facility Infrastructure
One main foundation for the increased morbidity and mortality of patients from the COVID-19 pandemic would be the fact that the health system of the country is poor, particularly, in terms of infrastructure. The key informants rose that new cases have been coming to some health centers from remote “kebeles or woredas” while existing (catchment) populations were missing from follow-ups. This was so because some hospitals were being prioritized as COVID-19 treatment centers. High potential for a person to person transmission of the virus, the occurrence of the outbreak amid the physical year, limited facility budget, shortage of mechanical ventilators, and an already existing lack of facility space have played a synergistic role augmenting for poor outcomes prevention and management against the COVID-19 at health facilities. A related typical problem highlighted by one key-informant was issues about COVID-19 suspects with chronic illness and staying at home. He discussed that these patients encountered severe challenges to cope up with pandemic and underlying chronic illnesses. Poor infrastructure has necessitated the stay home rules for suspected individuals with COVID-19. Yet, the number of health professionals was inadequate at most health facilities, which in turn, might be a risk for potential viral transmission to family and increased morbidity and mortality of those with comorbid conditions.
Challenges Related to Human Resource and Workload
Also in link with the challenges mentioned so far, the pandemic has tested the capacity of all level health facilities in all nations. As witnessed by the interviewees and observed practically, the COVID-19 pandemic has consumed the lives of many health professionals globally and nationally. It was said that some facilities had a small staff before the onset of the outbreak which was exacerbated later, some had their staff reduced due to acquiring the infection, and some were exempted from all clinical practices either due to comorbid condition or advanced ages. These all had led to a decrease in expected service quality, high staff workload, and frustrations. Key-informants have also stated that poor risk incentive packages and lack of continuous training impacted their job motivation negatively.
Challenges Related to Supply of Prevention and Treatment Inputs
Lack of personal preventive equipment (PPE) was reported in almost all of the health facilities included in this study. The informants mentioned that face masks, body covers, and gloves were in short supply. Likely, medications for chronic illnesses including; insulin, metformin, and enalapril were unavailable for longer times. Even though, availability of respiratory machines (ventilators, cannot be expected at primary healthcare units of Ethiopia, an observation also showed that arrangements of emergency care units like oxygen supply, well-ventilated isolation rooms, and the readily trained team were lacking in the centers. Whereas most of these challenges relate to the preexisting low healthcare infrastructure at these centers, high demand for peculiar inputs such as PPEs and the indirect impact it posed on the supply side (global and local supply chain of health commodities) put a historical mark on the COVID-19 era.
Discussion
The present study has illustrated that most units of the respective health centers have faced drops in client flow following the COVID-19 pandemic. Fears and responses of patients started to draw remarkable attention of the public, particularly, after the virus has been first detected in the country in March 2020. Comparison of the pre-COVID-19 era loads with the COVID-19 period showed that there was a significant disparity in the service delivery capacity of the health facilities. A huge drop in the patient flow of some units such as PICT, VCT, FP services, and OPD visits in most of the units has been recorded. Some services as delivery and Post-natal care (PNC) showed little disruption, particularly, in the latter months of the pandemic. This is partly in agreement with the report by Abdela and his colleagues 21 where family planning and OPD chronic care services faced the highest decline in Northeastern Ethiopia. Among the potential reasons for why PICT services showed an unprecedented fall at the settings would be that providers were engaged on existing medical services, lack of adequate PPEs in all units, patients’ fear to visit facilities at all especially at earlier times of the outbreak, patients’ resistance to link with PICT clinics as a result of perceived poor preventive infrastructures or any combination of these. A similar study in Kenya documented that many clinics did not have masks and sanitizers which affected implementation of COVID-19 guidelines. 25 A study by Pinto and Park (2020) also highlighted that the pandemic has severely impeded HIV testing and linkage care services. 26 Studies in other parts of the world documented impacted services for tuberculosis, 27 cancer cares, 28 ophthalmologic care, 29 dental healthcare, 30 organ donation, 31 and contribution to the mental health burden of the population. 32
A multitude of reasons could be speculated for the severe depression of service uptakes, especially, during the early phases of the outbreak. These may include, but not limited to; lack of adequate information on prevention strategies, uncertainties on the treatment outcomes of the COVID-19, perceived unavailability and ineffectiveness of isolation and treatment programs, as well as perceived severity of the disease especially among the elderly and those with comorbid conditions. Inspecting the trend over the subsequent months, this gap appears to be improved, possibly, due to the reason that people gained more information from peers and media on the mode of transmission, prevention methods, and sign and symptoms of the infection. A report by Desalegn and his colleagues 19 has shown that the public in Addis Ababa had moderate knowledge, an optimistic attitude, and descent practice. As per reports on daily toll or weekly averages, the wave even showed an unprecedented fall in June 2021 following the highest ever peak in April of the same year. 17
Another indirect negative impact of the COVID-19 pandemic was that most services for patients with chronic illness were entirely at lower uptake. The figures from the declining OPD visits in the current study settings showed that little attention was paid to retain follow-up cares especially for non-communicable diseases. Also, as triangulated from key-informant interviews, attention on the COVID-19 has ignored other medical services ominously. This has, partly, been contributed from the health facilities’ side as the poor and existing resources were overwhelmed, and the patients’ side, as patients failed to actively engage in seeking medical care. Although some hospitals have been closed for COVID-19 isolation and treatment centers, 20 patient flows to nearby health centers were not as it would have been expected. According to a study in Australia, patient fear could be a major cause of reduced health facility visits. 33
And, seemingly a paradox to the lower service utilization rates, tracing back of medical histories of those patients visiting the facilities for the first time, and providing adequate service was reported to be a challenging task. This was explained to be attributed to the limited number of medical staff and weak infrastructure. The key-informants also stated that workload on the existing staff was a prominent issue as a result of acquiring the COVID-19 infection and exemption leave of staff with advanced age and comorbidities. Though digitalized technologies have been reported to be an alternative to arrest such challenges in other countries, 34,35 such efforts were non-existent, especially, at such lower healthcare units. A report had also highlighted that integration of mobile care clinics would be ideal to respond against the COVID-19 challenges. 36
The efforts are done to maintain ART programs, however, are appreciated across all settings. The periodic community outreach service in all the primary health units was found to be an exemplar practice that was enhanced further after the COVID-19 outbreak. According to the key-informants, all patients with a higher likelihood of loss to follow-up due to socio-economic issues were identified earlier and enrolled in the community-based follow-up. In the same way, stable patients who were in the regular program, and who were unable to refill their medications were reached by the outreach group. This, possibly, has contributed to the relatively steady number of patients who refilled their ART medications in the subsequent months. In the same fashion, the implementation of appointment spacing models (ASM) whereby stable ART clients receive a 3 to 6 months consumption of drugs was an additional mechanism to sustain such services.
Apart from evaluating monthly patient loads and drawing comparisons with the pre-COVD-19 era, this study has explored the common challenges that prevailed during the pandemic. Accordingly, 4 main themes namely; challenges related to fear of infection and stigma, poor infrastructure, challenges related to human resources, and challenges related to the supply of prevention and treatment inputs were generated. This was in agreement with other reports. 37 Poor availability of PPEs was among the most mentioned challenges at most of the units. A study from Italy documented that more than two-thirds of the intuitions had trouble getting PPEs. 38
Key-informants also highlighted that “stay at home” rules for COVID-19 suspects posed a challenge to patients with comorbid conditions. This challenge was precipitated by the inadequacy of the health care professionals for home-care deployment, lack of sustained supply of PPEs, and limited health facility infrastructure to admit all COVID-19 suspect patients. They also discussed that health professionals are faced with an increased risk of acquiring the virus because of asymptomatic cases delayed response from treatment centers, poor ventilations of facility environments, the incubation period of the virus, and delay of test results. Nonetheless, temperature measurement was routinely practiced at all health centers.
This study has tried to present a comprehensive report of health service utilization trends at health centers, as the primary healthcare units in the Ethiopian context. The results show the main services that were hampered by the COVID-19 pandemic. It is assumed that health authorities and health professionals will benefit from the update to inform policy and practice. Even though an effort has been made to represent potential variabilities across all sub-cities, the generalizability of findings in this study must be taken with caution. The findings are also limited to the time-period covered by the review, and the dynamics of information, demand and the pandemic curve as well as patients’ behavior might have resulted for an altered trend of the phenomenon. Studies that incorporate additional service units and big data are warranted.
Conclusion
Comparison of the pre-COVID-19 era service utilization with the COVID-19 period showed that there was a substantial disparity in service delivery practice of the health facilities. A huge decline in the patient flow was noted from points such as PICT, VCT, FP, and OPD units. The key-informant interview also revealed that such challenges, as fear of infection and stigma, poor infrastructure, challenges related to human resource, and challenges related to supply of prevention and treatment inputs were prominently encountered at the health facilities following the outbreak.
Acknowledgments
The author would like to thank all the health facility representatives and key-informants who provided their kind cooperation and facilitation in this study. I am indebted to the generous assistance, especially, by Mrs. Zufan, Mr. Amanuel, and Mr. Berhan during my data collection in Lideta sub-city. I also thank SPHMMC for offering the financial support to undertaking this study.
Author Biographies
Tariku Shimels, BPharm, BA, MSc, has a master's in Pharmacoepidemiology and Social Pharmacy. He is a lecturer, and serves as a research coordinator at Saint Paul's Hospital Millennium Medical College, Addis Ababa, Ethiopia. Tariku's research interest include;health service, non-communicable diseases, infectious diseases, drug utilization, economic evaluation, and social determinants of illness and health.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The author received a financial support for this article. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
ORCID iD: Tariku Shimels  https://orcid.org/0000-0001-5212-7597
https://orcid.org/0000-0001-5212-7597
References
- 1. COVIDSurg Collaborative. Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an International Cohort Study. Lancet. 2020;396(10243):27–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Allen S, Julian Z, Coyne-Beasley T, et al. COVID-19’s impact on women: a stakeholder-engagement approach to increase public awareness through virtual town halls. J Public Health Manag Pract. 2020;26(6):534–538. [DOI] [PubMed] [Google Scholar]
- 3. Ritchie LD, Takada D, Morishita T, et al. Economic impact of the first wave of the COVID-19 pandemic on acute care hospitals in Japan. J R Soc Med. 2020;15(12):e0244852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. DeLange Martinez P, Nakayama C, Young HM. Age-friendly cities during a global pandemic. J Gerontol Nurs. 2020;46(12):7–13. [DOI] [PubMed] [Google Scholar]
- 5. Inzitari M, Udina C, Len O, et al. How a Barcelona post-acute facility became a referral center for comprehensive management of subacute patients with COVID-19. J Am Med Dir Assoc. 2020;21(7):954–957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Idris H. Utilization of teleconsultation: mitigation in handling mental disorders in the COVID-19 era. Int J Ment Health Addict. 2020:1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Zhu H, Wei I, Niu P. The novel coronavirus outbreak in Wuhan, China. Global Health Res Policy. 2020;5(1):6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. World Health Organization. COVID-19 Weekly Epidemiologic Update: Global Epidemiological Situation. World Health Organization. 2020:17. [Google Scholar]
- 9. Papautsky EL, Hamlish T. Patient-reported treatment delays in breast cancer care during the COVID-19 pandemic. Breast Cancer Res Treat. 2020;184(1):249–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Panagiotidis E. Nuclear medicine and oncology in the COVID-19 pandemic era. Hell J Nucl Med. 2020;23(Suppl):35–40. [PubMed] [Google Scholar]
- 11. Park C, Sugand K, Nathwani D, et al. Impact of the COVID-19 pandemic on orthopedic trauma workload in a London level 1 trauma center: the “golden month.” Acta Orthop. 2020;91(5):556–561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Passos L, Prazeres F. Impact on mental health due to COVID-19 pandemic: cross-sectional study in Portugal and Brazil. Int J Environ Res Public Health. 2020;17(18):6794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Patel S, Douglas-Moore J. A reflection on an adapted approach from face-to-face to telephone consultations in our Urology Outpatient Department during the COVID-19 pandemic—a pathway for change to future practice? BJU Int. 2020;126(3):339–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Feroz AS, Khoja A, Saleem S. Equipping community health workers with digital tools for pandemic response in LMICs. Arch Public Health. 2021;79(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. De Biase G, Freeman WD, Bydon M, et al. Telemedicine utilization in neurosurgery during the COVID-19 pandemic: a glimpse into the future? Perspect Med Educ. 2020;4(6):736–744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Pini R, Faggioli G, Vacirca A, et al. Is it possible to safely maintain a regular vascular practice during the COVID-19 Pandemic? Eur J Vasc Endovasc Surg. 2020;60(1):127–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. World Health Organization. Weekly Epidemiological Update on COVID-19 . World Health Organization. Edition 44. June 15, 2021. 1–26. [Google Scholar]
- 18. US Embassy in Ethiopia. COVID-19 Information: entry and exit requirements. Updated June 13, 2021. Accessed June 16, 2021. https://et.usembassy.gov/covid-19-information/
- 19. Desalegn Z, Deyessa N, Teka B, et al. COVID-19 and the public response: knowledge, attitude and practice of the public in mitigating the pandemic in Addis Ababa, Ethiopia. PLoS One. 2021;16(1):e0244780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Abdela SG, van Griensven J, Seife F. Neglecting the effect of covid-19 on neglected tropical diseases: the Ethiopian perspective. Trans R Soc Trop Med Hyg. 2020;114(10):730–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Abdela SG, Berhanu AB, Ferede LM. Essential healthcare services in the face of covid-19 prevention: experiences from a referral hospital in Ethiopia. Am J Trop Med Hyg. 2020;103(3):1198–1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kasahun GG, Kahsay GM, Asayehegn AT, et al. Pharmacy preparedness and response for the prevention and control of coronavirus disease (COVID-19) in Aksum, Ethiopia; a qualitative exploration. BMC Health Serv Res. 2020;20(1):913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. United Nations Population Fund (UNFPA) and Federal Democratic Republic of Ethiopia Population Census Commission. Summary and statistical report of the 2007 population and housing census:population by age and sex. Addis Ababa, Ethiopia. December 2008;1-12.
- 24. Misganaw A, Mariam DH, Araya T., et al. Patterns of mortality in public and private hospitals of Addis Ababa, Ethiopia. BMC Pub Heal. 2012;12:1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lagat H, Sharma M, Kariithi E, et al. Impact of the COVID-19 pandemic on HIV testing and assisted partner notification services, Western Kenya. AIDS Behav. 2020;24(11):3010–3013. doi:10.1007/s10461-020-02938-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Pinto RM, Park S. COVID-19 pandemic disrupts HIV continuum of care and prevention: implications for research and practice concerning community-based organizations and frontline providers. AIDS Behav. 2020;24(9):2486–2489. doi:10.1007/s10461-020-02893-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Abikoye TM. Collateral damage: the impact of the COVID-19 pandemic on the care of a patient with tuberculous neuroretinitis in Lagos, Nigeria. Pan Afr Med J. 2020;35(Suppl 2):135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Abila DB, Ainembabazi P, Wabinga H. COVID-19 pandemic and the widening gap to access cancer services in Uganda. Pan Afr Med J. 2020;35(Suppl 2):140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Agarwal R, Sharma N, Patil A. Impact of COVID-19 pandemic, national lockdown, and unlocking on an apex tertiary care ophthalmic institute. Indian J Ophthalmol. 2020;68(11):2391–2395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ahmadi H, Ebrahimi A, Ghorbani F. The impact of COVID-19 pandemic on dental practice in Iran: a questionnaire-based report. BMC Oral Health. 2020;20(1):354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ahmed O, Brockmeier D, Lee K. Organ donation during the COVID-19 pandemic. Am J Transplant. 2020;20(11):3081–3088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Aho J, Samouti G, Samoutis G. Mental health disorders during the COVID-19 outbreak in Cyprus. Glob Public Health. 2020;13(3):300–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Amukotuwa SA, Bammer R, Maingard J. Where have our patients gone? The impact of COVID-19 on stroke imaging and intervention at an Australian stroke center. J Med Imaging Radiat Oncol. 2020;64(5):607–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Ajibade A, Younas H, Pullan M, Harky A. Telemedicine in cardiovascular surgery during COVID-19 pandemic: a systematic review and our experience. J Card Surg. 2020;35(10):2773–2784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Ameis SH, Lai MC. Coping, fostering resilience, and driving care innovation for Autistic people and their families during the COVID-19 pandemic and beyond. Mol Autism. 2020;11(1):61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Attipoe-Dorcoo S, Delgado R, Gupta A, et al. Mobile health clinic model in the COVID-19 pandemic: lessons learned and opportunities for policy changes and innovation. Int J Equity Health. 2020;19(1):73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Arcot PJ, Kumar K, Mukhopadhyay T, Subramanian A. Potential challenges faced by blood bank services during COVID-19 pandemic and their mitigative measures: the Indian scenario. Transfus Apher Sci. 2020;59(5):102877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Albano D. Impact of coronavirus disease 2019 (COVID-19) emergency on Italian radiologists: a national survey. Psychol Trauma. 2020;30(12): 6635–6644. [DOI] [PMC free article] [PubMed] [Google Scholar]