Abstract
Introduction:
Hip fracture patients have been severely affected by the COVID-19 pandemic; however, the sub acute effects of a concomitant SARS-CoV-2 infection and the outcomes in highly exposed developing countries are still unknown. Our objective is to describe the morbidity and mortality of elderly patients admitted for a hip fracture during the COVID-19 pandemic in Chile, with a minimum 90-day follow-up. Also, to elucidate predictors for mortality and to compare mortality results with the pre-pandemic era.
Material and Methods:
Multicentric retrospective review of patients admitted for a fragility hip fracture in 3 hospitals during the COVID-19 pandemic, and during the same time in 2019. All clinical information and images were recorded, and patients were followed for a minimum of 90-days. Morbidity and mortality were the primary outcomes. Uni/multivariable models were performed to elucidate predictors for mortality utilizing the Weibull’s regression.
Results:
Three hundred ninety-one cases were included. From the 2020 cohort (162 patients), 24 (15%) had a concomitant SARS-CoV-2 infection. Fourteen patients (58%) tested positive after admission. The COVID-19(+) group had a higher risk of in-hospital, 30-day, and 90-day mortality (p < 0.001). They also had a prolonged hospital stay and presented with more complications and readmissions (p < 0.05). Only COVID-19(+) status and older age were independent predictors for mortality with a HR = 6.5 (p = < 0.001) and 1.09 (p = 0.001), respectively. The 2020 cohort had twice the risk of mortality with a HR = 2.04 (p = 0.002) compared to the 2019 cohort. However, comparing only the COVID-19 (-) patients, there was no difference in mortality risk, with a HR = 1.30 (p = 0.343).
Discussion:
The COVID-19 pandemic has significantly affected healthcare systems and elderly patients.
Conclusions:
Hip fracture patients with a concomitant SARS-CoV-2 virus infection were associated with increased morbidity and mortality throughout the first 3 months. COVID-19 status and older age were significant predictors for mortality. Efforts should be directed into nosocomial infection reduction and prompt surgical management.
Level of evidence:
Level III
Keywords: COVID-19, hip fracture, fragility fracture, survival analysis
Introduction
Since the first reported cases of SARS-CoV-2 virus infection and the coronavirus disease 2019 (COVID-19) in China, the disease has spread rapidly without boundaries and every country in the world has been affected in some magnitude. 1 By the end of 2020, more than 68 million people have been affected worldwide, with over 1.5 million deaths. 2 In particular, Latin America became the world’s most affected geographic area in June 2020, 3 and Chile was not an exception with one of the highest cumulative incidences and an exceptional healthcare overload during the winter season.
Hip fractures are the most severe manifestation of so-called fragility fractures and have been recognized as one of the growing epidemics of the 21st century. 4,5 Their time-sensitive need for intervention and the elderly, frail, high-risk population that they affect have become critical features during the COVID-19 pandemic, especially in highly affected countries and on the verge of collapse health systems.
Several reports have shown an increased 30-day mortality in patients with a hip fracture and concomitant COVID-19 infection. 6 -12 However, the sub-acute effects of the pandemic on this specific population are still unknown. Similarly, the influence of limited access to health care because of the pandemic in patients independently of their COVID-19 status and the disparities of different health systems in Latin America have not been addressed.
Our objective is to describe the effects of the COVID-19 pandemic on morbidity and mortality of elderly patients admitted for a fragility hip fracture in 3 different Chilean hospitals with a minimum 90-day follow-up. We also establish predictors for mortality, including COVID-19 infection, demographics, delay in surgery, and different health care systems.
Materials and Methods
A multicenter cohort study was performed at 3 major hospitals within Santiago, Chile. Ethical institutional review board approval was obtained individually at each center before performing this study. All 3 centers are high complexity referral hospitals, 2 of them of public access and 1 private, representing the mixed public-private Chilean healthcare system. 13 Results were reported in accordance with the STROBE (strengthening the reporting of observational studies in epidemiology) statement and checklist for retrospective studies. 14
We included all patients older than 60 years of age admitted for a fragility hip fracture (femoral neck, pertrochanteric, or subtrochanteric fracture) from March 15th, when a national state of emergency was declared because of the COVID-19 pandemic, until August 30th, 2020 (2020 cohort). All patients were followed for a minimum of 90 days after admission or until the date of their death. Exclusion criteria were patients with a high-energy fracture, femoral shaft, and periprosthetic fractures. Patients from the same period of 2019 were included as a control group, complying with the same inclusion and exclusion criteria, from all 3 hospitals participating in the study (2019 cohort).
Electronic charts were used to collect all clinical notes and images, including patient demographics, surgery reports, discharge summaries, emergency consultations, follow-up appointments, and postoperative x-rays. The following clinical data was collected: age, gender, comorbidities, modified Charlson Comorbidity Score Index (CCI), 15,16 American Society of Anesthesiologists (ASA) score, laboratory on admission including SARS-CoV-2 test results, type of fracture, treatment received, time from admission to surgery and length of hospital stay (LOS) (in days). Medical or surgical complications, emergency consults or readmissions within 30 days after discharge, and mortality were also recorded (in-hospital, 30-day, and 90-day mortality). Mortality information is centralized and accessible in Chile, ensuring a reliable and complete set of information at the time of review.
Patients were classified into COVID-19 positive (+) or COVID-19 negative (-) groups based on their SARS-CoV-2 real-time reverse transcriptase-polymerase chain reaction (rRT-PCR) status and/or clinical symptoms. Seventy-eight percent of patients had at least 1 SARS-CoV-2 PCR test during their hospitalization (127 of 162 patients) along with all symptomatic cases. Cases with at least 1 positive test (23 cases) during their clinical course, as well as patients who tested negative but had highly suggestive symptoms and a Computed Tomography (CT) scan with a compatible COVID-19 pneumonia (1 case), were considered part of the COVID-19 (+) group. Patients with negative tests (103 of 162 cases) and patients not tested but without any suggestive symptoms and an uneventful clinical course on retrospective analysis (35 of 162 cases) were considered part of the COVID-19 (-) group. Patients were re-tested in case of in-hospital contact with a positive subject or if there was any change in their symptoms.
All patients were managed by an orthogeriatric team during their hospital stay and were initially considered for surgery unless their medical condition needed stabilization. Displaced femoral neck fractures were treated with a total hybrid arthroplasty or cemented (bipolar) hemiarthroplasty. Non-displaced femoral neck fractures were treated with osteosynthesis versus hip arthroplasty if a significant posterior tilt was observed. 17 Pertrochanteric fractures were treated with reduction and fixation with a cephalomedullary nail or a sliding hip screw. All subtrochanteric fractures (defined as fractures up to 5 cm below the lesser trochanter) were treated with long cephalomedullary nail fixation. All surgeries were performed as per standard clinical pathway, and even though operating room access was overall limited for non-urgent conditions, the orthopaedic surgery service continued to provide care to all patients presenting with a hip fracture to the emergency department in all 3 centers. Patients were encouraged to mobilize early with weight-bearing as tolerated as per routine hip fracture surgery protocols, favoring early discharge. Antibiotic and deep venous thrombosis prophylaxis were used in all cases. Patients were followed at 3 and 6 weeks after discharge and bi-monthly after that.
Statistical Analysis
Statistical analysis was conducted using SPSS version 21 (SPSS, Chicago, IL, USA) and STATA 16/SE (Stata Corp LLC, Texas, USA). The primary outcome was mortality, assessed as in hospital, 30-day, and 90-day mortality. The 2020 cohort’s secondary outcomes were: length of hospital stay, postoperative complications, and emergency consults or readmissions within 30 days after discharge. The Chi-Squared and Fisher Exact tests were used to compare categorical data, while the independent samples t-test or the Mann-Whitney test was utilized for numerical data after normality verification. Similarly, variables were expressed as number of patients (n) and percentage (%), mean and standard deviation (SD), or, alternatively, median and interquartile range (IQR).
Kaplan-Meier curves were utilized for the survival analysis, and values were expressed with their 95% confidence intervals (CI). Survival probabilities were explored, adjusting to a Weibull’s distribution. 18,19 Hazard Ratios (HR) with their 95%CI were considered to assess for mortality predictors in univariable and multivariable analyzes, utilizing the Weibull’s regression. 18,19 Multivariable models were selected from variables with a significant association in the univariable analysis at alpha <0.2. Variables included in the analysis were: gender, age, CCI, ASA score, COVID-19 status, time from admission to surgery (in days), and being treated in a public vs. private hospital.
The mortality of patients from the 2020 and 2019 cohorts was also compared. In parallel, the 2020 and 2019 cohorts were contrasted removing the COVID-19 (+) patients to analyze the effects of the pandemic in the COVID-19 (-) patients. A p-value < 0.05 was considered to be significant.
Results
A total of 391 cases were included, 162 patients in the 2020 cohort and 229 in the 2019 cohort. There was no difference in gender, age, CCI, ASA score, or fracture type within the 2 cohorts (Table 1).
Table 1.
Patients Demographics and Surgery Details.
| 2020 Cohort (n = 162) | 2019 Cohort (n = 229) | p-value | |
|---|---|---|---|
| Gender (n; %) | |||
| Female | 139 (86%) | 184 (80%) | 0.161^ |
| Male | 23 (14%) | 45 (20%) | |
| Age (median; IQR) | 82 years (75-88) | 83.5 years (77-89) | 0.122* |
| Charlson Comorbidity Index (median; IQR) | 1 (0-2) | 1 (0-2) | 0.651* |
| ASA score (median; IQR) | 2 (2-2) | 2 (2-2) | 0.483* |
| Type of fracture (n, %) | |||
| Femoral neck | 68 (42%) | 97 (42%) | 0.368^ |
| Intertrochanteric | 89 (55%) | 118 (52%) | |
| Subtrochanteric | 5 (3%) | 14 (6%) | |
| Side (n, %) | |||
| Left | 72 (44%) | 106 (46%) | 0.718^ |
| Right | 90 (56%) | 123 (54%) | |
| Treatment (n, %) | |||
| Non-operative | 3 (2%) | 3 (1%) | 0.695^ |
| Operative | 159 (98%) | 226 (99%) | |
| Internal fixation | 97 (61%) | 140 (62%) | |
| Hemiarthroplasty | 29 (18%) | 23 (10%) | |
| Total hip arthroplasty | 33 (21%) | 63 (28%) |
Abbreviations: ASA, American Society of Anesthesiologists; IQR, interquartile range.
* Mann Whitney Test.
^ Chi-square or Fisher’s test.
2020 Cohort
From 162 patients, 24 (15%) were classified as COVID (+) and 138 (85%) as COVID (-) (Table 2). No difference was observed in patients’ demographics or fracture type; however, more patients developed a SARS-CoV-2 infection in the public hospitals (22/110; 20%) compared to the private one (2/52; 4%) (p = 0.007). Patients were followed for a median of 130 days (IQR 100-153). In addition, COVID-19 (+) patients were also followed for a minimum of 90 days after their SARS-CoV-2 infection if alive (median: 48 days; IQR 18-141). Three patients did not undergo surgical treatment; all of them died during their hospitalization because of their coexisting medical conditions and COVID-19 infection (5, 10, and 18 days after admission).
Table 2.
Patients From the 2020 Cohort.
| COVID (+) (n = 24) | COVID (-) (n = 138) | p-value | |
|---|---|---|---|
| Gender (n; %) | |||
| Female | 20 (83%) | 119 (86%) | 0.707^ |
| Male | 4 (17%) | 19 (14%) | |
| Age (median; IQR) | 81 years (75-88) | 81 years (77-89) | 0.370* |
| Charlson comorbidity index (Median; IQR) | 2 (0-3) | 1 (0-2) | 0.05* |
| Comorbidities (n; %) | |||
| Diabetes | 4 (17%) | 34 (25%) | 0.395^ |
| Coexisting lung disease | 2 (8%) | 15 (11%) | 1^ |
| Cardiopathy | 5 (21%) | 24 (17%) | 0.773^ |
| Hypertension | 14 (58%) | 79 (57%) | 0.921^ |
| Active smoking (n; %) | 4 (17%) | 17 (12%) | 0.520^ |
| ASA score (median; IQR) | 2 (2-3) | 2 (2-2) | 0.035* |
| Type of fracture (n, %) | |||
| Femoral neck | 8 (33%) | 60 (43%) | 0.637^ |
| Intertrochanteric | 15 (63%) | 74 (54%) | |
| Subtrochanteric | 1 (4%) | 4 (3%) | |
| Side (n, %) | |||
| Left | 10 (42%) | 62 (45%) | 0.827^ |
| Right | 14 (58%) | 76 (75%) | |
| Time from admission to surgery (Days, median; IQR) | 5 days (3-8) | 3 days (1-6) | 0.017^ |
| Treatment (n, %) | |||
| Non-operative | 3 (13%) | 0 | 0.003^ |
| Operative | 21 (87%) | 138 (100%) | 0.385^ |
| Internal fixation | 15 (71%) | 82 (59%) | |
| Hemiarthroplasty | 4 (19%) | 25 (18%) | |
| Total hip arthroplasty | 2 (10%) | 31 (23%) | |
| Type of hospital being treated at (n; %) | |||
| Private | 2 (8%) | 50 (36%) | 0.007^ |
| Public | 22 (92%) | 88 (64%) |
Abbreviations: ASA, American Society of Anesthesiologists; IQR, interquartile range.
* Mann Whitney Test.
^ Chi-square or Fisher’s test.
From the COVID-19 (+) group, 21 patients (87.5%) developed respiratory symptoms and/or fever. Ten (42%) of these patients tested positive in admission laboratory, while 14 (58%) tested positive during the following days, at a median of 6 days (IQR 1-18 days). Patients that were COVID-19 (+) were considered to have a higher ASA classification but similar CCI. Time from admission to surgery was longer in the COVID-19 (+) patients (5 vs. 3 days, p = 0.017).
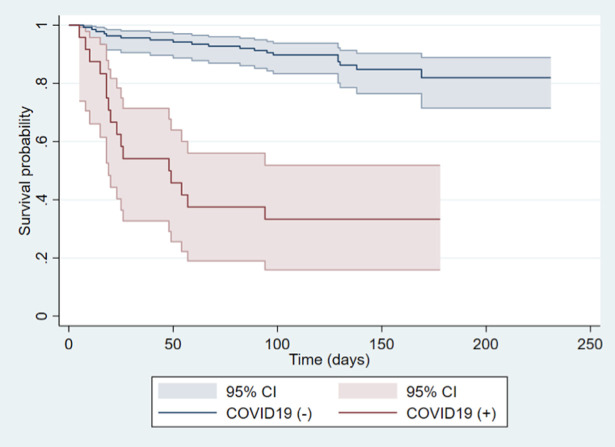
Overall mortality in the 2020 cohort was 21% (35/162 patients), with 67% (16/24) of COVID-19 (+) and 14% (19/138) of COVID-19 (-) patients dying during follow-up (p = < 0.001). The COVID-19 (+) group had a higher risk of in-hospital, 30-day, and 90-day mortality than the COVID-19 (-) group. Similarly, COVID-19 (+) patients had a longer hospital stay (12.5 vs. 6.5 days, p = 0.001), as well as an increased rate of postoperative medical complications (83% vs. % 39%, respectively. p = < 0.001) and emergency consultations or readmissions after discharge (25% vs. 8%, p = < 0.001) (Tables 3 and 4). Kaplan-Meier curves revealed a survival for the COVID-19 (+) patients of 54.2% (95%CI 32-71) at 30 days and 37.5% (95%CI 19-56) at 90 days. In contrast, COVID-19 (-) patients showed a survival of 95.7% (95%CI 90-98) at 30 days and 91.3% (95%CI 85-95) at 90 days, with a significant difference between the two groups (HR = 8.54, 95%CI 4-16; p = < 0.001) (Figure 1).
Table 3.
Outcomes for the 2020 Cohort.
| COVID (+), (n = 24) | COVID (-), (n = 138) | OR (95%CI) | p-value | |
|---|---|---|---|---|
| In-hospital mortality (n, %) | 10 (42%) | 4 (3%) | 23.9 (95%CI 6-86) | <0.001^ |
| 30-days mortality (n, %) | 11 (46%) | 6 (4%) | 18.6 (95%CI 6-58) | <0.001^ |
| 90-days mortality (n, %) | 15 (63%) | 13 (9%) | 16 (95%CI 6-43) | <0.001^ |
| Length of hospital stay (Days, median; IQR) | 12.5 days (IQR 7-23) | 6.5 days (IQR 4-11) | 0.001* | |
| Postoperative medical complications (n of patients, %) | 20 (83%) | 54 (39%) | 7.7 (95%CI 2-23) | <0.001^ |
| Emergency consultations or readmissions (n, %) | 6 (25%) | 11 (8%) | 3.8 (95%CI 1.2-12) | 0.023^ |
Abbreviations: OR, odds ratio; CI, confidence interval.
* Mann Whitney Test.
^ Chi-square or Fisher’s test.
Table 4.
Complications in the 2020 Cohort.
| COVID (+) (n = 24) | COVID (-) (n = 138) | |
|---|---|---|
| Postoperative periprosthetic fracture | 0 case | 1 case |
| Postoperative hematoma | 0 case | 2 cases |
| Peri-prosthetic/Peri-implant joint infection | 2 cases | 0 case |
| Wound dehiscence | 1 case | 0 case |
| Hardware failure | 1 case | 0 case |
| Medical complications | ||
| Postoperative delirium | 8 cases | 32 cases |
| Urinary tract infection | 3 cases | 11 cases |
| Pneumonia | 11 cases | 4 cases |
| DVT/PE | 3 cases | 5 cases |
| Acute renal failure | 3 cases | 8 cases |
| Gastrointestinal bleeding | 0 case | 1 case |
| Congestive heart failure | 0 case | 1 case |
| Electrolyte imbalance | 6 cases | 10 cases |
| Hypertensive crisis | 0 case | 1 case |
| Intestinal obstruction | 0 case | 1 case |
| Respiratory failure | 2 cases | 1 case |
| Cerebrovascular infartc | 0 case | 1 case |
| Atrial fibrillation | 0 case | 3 cases |
Abbreviations: DVT, deep venous thrombosis; PE, Pulmonary embolism.
Figure 1.
Kaplan Meier curve of survival for the COVID-19 (-) and COVID-19 (+) patients from the 2020 cohort.
Predictors for Mortality
The univariable analysis showed that COVID-19 status, age, CCI, ASA score IV, being treated in a public hospital, and a longer period from admission to surgery were risk factors for mortality (Table 5). Multivariable risk analysis found that COVID-19 (+) status and older age were the only independent predictors for mortality with a HR = 6.5 (95%CI 2-14; p = < 0.001) and HR = 1.09 (95%CI 1.03-1.1; p = 0.001), respectively.
Table 5.
Univariable and Multivariable Analyzes.
| Univariable | Multivariable | |||
|---|---|---|---|---|
| Variable | HR (95%CI) | p-value | HR (95%CI) | p-value |
| Gender female (vs. male) | 1.01 (0.39-2.62) | 0.968 | not included | |
| Age | 1.06 (1.02-1.1) | 0.003 | 1.09 (1.03-1.15) | 0.001 |
| Charlson comorbidity index | 1.2 (1.03-1.4) | 0.017 | 1.09 (0.9-1.3) | 0.327 |
| ASA Score (vs. ASA I) | ||||
| ASA II | 0.46 (0.16-1.36) | 0.159 | 0.61 (0.19-1.88) | 0.393 |
| ASA III | 0.71 (0.22-2.38) | 0.586 | 0.58 (0.17-1.99) | 0.391 |
| ASA IV | 5.83 (1.45-23.4) | 0.013 | 2.94 (0.31-27.92) | 0.347 |
| Active smoking status | 0.58 (0.17-1.9) | 0.374 | not included | |
| COVID-19 (+) | 8.54 (4.3-16.7) | <0.001 | 6.51 (2.86-14.8) | <0.001 |
| Time from admission to surgery (days) | 1.08 (1.02-1.1) | 0.006 | 1.04 (0.97-1.12) | 0.246 |
| Public hospital (vs. private) | 2.9 (1.1-7.4) | 0.027 | 1.5 (0.4-4.5) | 0.475 |
Abbreviations: HR, hazard ratio; CI, confidence interval.
2020 vs. 2019 Cohort
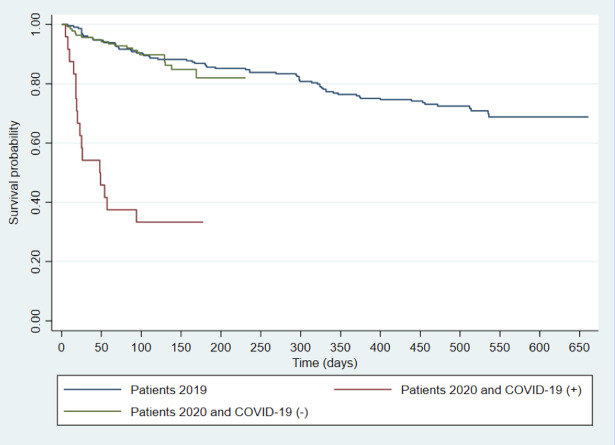
Overall, patients from the 2020 cohort had twice the risk of mortality with a HR = 2.04 (95%CI 1.3-3.2; p = 0.002), compared to the 2019 cohort. Similarly, they presented a higher in-hospital (8.6% vs. 2.2%; p = 0.003), 30-day (10.5% vs. 3.9%; p = 0.010), and 90-day mortality (17.3% vs. 9.2%; p = 0.018), When comparing only the COVID-19 (-) patients from the 2020 cohort to the entire 2019 cohort, there was no difference in mortality risk, with a HR = 1.30 (95%CI 0.75-2.26; p = 0.343) (Figure 2). Likewise, in-hospital (2.9 vs. 2.2%; p = 0.734), 30-day (4.3 vs. 3.9%; p = 0.845), and 90-day mortality (9.4 vs. 9.2%; p = 0.936), showed no statistically significant difference.
Figure 2.
Kaplan Meier curve of survival for the COVID-19 (-) and COVID-19 (+) patients from the 2020 cohort, compared to the 2019 cohort.
Discussion
The COVID-19 pandemic has affected most aspects of our daily lives, with a significant burden to health care systems and an enormous impact on patients, especially the high-risk elderly population. Our results show that Chilean elderly patients with a hip fracture and a concomitant SARS-CoV-2 virus infection were associated with a significantly increased 30 and 90-day mortality, along with poorer outcomes in terms of postoperative complications, length of hospital stay, and postoperative readmissions.
Our series revealed a 15% incidence of COVID-19 disease in elderly patients admitted for a hip fracture, similar to other published reports. 8,20 Furthermore, overall mortality was increased, with a 5-fold mortality rate for COVID-19 (+) patients (67%) when compared to COVID-19 (-) patients (14%). Other reports have addressed early mortality rates in this scenario, with values ranging from 10 to 53% 7 -10,12,20,21 at 30 days. However, most studies report only crude mortality rates, with a short follow-up, especially after the SARS-CoV-2 virus infection, which could influence survival rates and overall outcomes. 20 In contrast, this series showed an increased mortality rate during the first month, with a persistent effect during the second and third months after admission. In fact, 17% of patients died within these 2 timeframes (30 and 90 days), emphasizing the need for a prolonged follow-up in this clinical setting.
Symptomatic patients reached more than 85% in this study, in line with previous reports that have found that an asymptomatic disease course is less frequent in older age groups. 22 On the other hand, more than half of the patients of this series (58%) tested positive for COVID-19 several days after admission, replicating the experiences reported by Dupley et al 23 and the IMPACT-Scot 2 report, among others. 7,9 Consequently, we have to assume that a proportion of these patients may have contracted the virus as a nosocomial infection, which highlights the need for strict preventive measurements, as separate in-hospital cohorts by COVID-19 status and universal PCR testing on admission, especially in high-risk population. 24
Even though the COVID-19 pandemic has affected every country in some magnitude, significant variations exist in infection-wave timing and health systems response or capacity that could differentiate outcomes from various geographic locations. Latin-America has some of the highest COVID-19 rates globally, with this condition being aggravated by poverty and political factors. 25 Chile, in particular, suffered a delayed first wave of infection, with one of the highest cumulative incidences, but a relatively low lethality as a result of intense resource relocation. 26 Slullitel et al 6 reported the effects of social lockdown on an Argentinean cohort of hip fracture patients before and after the COVID-19 pandemic started. Even when all patients tested negative for SARS-CoV-2 virus infection, patients treated during the pandemic were frailer and less mobile, resulting in a higher mortality rate. Pintado et al 27 reported a significant decrease in most emergency department visits except for osteoporotic fractures in a Peruvian trauma center. To our knowledge, this is the only report to date to specifically address mortality in hip fracture patients with a concomitant SARS-CoV-2 infection in a Latin-American country, with comparable results to case series from other locations.
Determining mortality and risk factors for adverse outcomes for patients with COVID-19 and a concurrent hip fracture is of great importance, as it can improve clinical pathways, perioperative management, and resource allocation. The univariable analysis revealed that COVID-19 status (+) (HR = 8.5), older age (HR = 1.06), higher CCI (HR = 1.2), ASA score IV (HR = 5.8), a prolonged time from admission to surgery (HR = 1.08), and being treated in a public hospital (HR = 2.9) were significant risk factors for increased mortality. However, many of these factors might be more related to the risk of contracting the disease (such as the type of hospital being treated in) or the consequence of their medical condition. As a result, the multivariable analysis revealed that only COVID-19 status (+) (HR = 6.5) and older age (HR = 1.09) were significant predictors for mortality.
In this series, COVID-19 (+) patients had not only a higher risk of dying but also had a much higher odds of presenting with a medical complication such as thromboembolic disease, pneumonia, surgical site infection, among others. Similarly, patients’ median length of stay doubled their COVID-19 (-) counterparts. Other reports have shown up to 51% rate of pulmonary complications in patients undergoing surgery with a concurrent SARS-CoV-2 virus infection 28 and up to 31% of thromboembolic events in severely ill patients. 29 Furthermore, this study showed that COVID-19 (+) patients were more likely to be readmitted or to go to the emergency department for complications related to their initial hospitalization or their COVID-19 status, including respiratory failure, among others. Donnelly et al 30 reported that up to 20% of COVID-19 (+) patients were readmitted after an initial discharge in a large multicenter study. Again, these results emphasize the need for a prolonged follow-up, especially in older patients, and that studies focused exclusively on inpatient or 30-day morbidity and mortality may not fully represent the burden of this disease.
When comparing the 2020 cohort to the 2019 cohort, patients treated during the COVID-19 pandemic had twice the hazard of dying, compared to their 2019 counterparts, along with a significant difference in inpatient, 30-day, and 90-day mortality. However, when considering only the COVID-19 (-) patients, we observed a non-statistically significant difference between the two cohorts, favoring a higher mortality risk for the 2020 group. This partially contrasts the results reported by Tripathy et al 31 ; their systematic review showed no significant difference in overall 30-day mortality within the 2020 and 2019 cohorts (9 vs. 6%; p = 0.14).
Our report has several limitations. It is a retrospective analysis and therefore is subject to different sources of bias, such as selection bias in that we included only patients that were admitted for a hip fracture, while some patients might not have been assessed in the emergency department because of the pandemic. Secondly, given the overall scarcity of resources that affected our health system during the COVID-19 pandemic, the best practices for the management of elderly patients with a hip fracture might not have been achieved, including delays in operative management. Furthermore, 3 different hospitals participated in the study, which may introduce variability among surgical techniques and overall perioperative management of hip fracture patients and COVID-19 (+) subjects. In the same way, protocols were implemented gradually, and therefore, were not applied homogeneously in time or within centers. Similarly, the limited sensitivity of the nasal swab PCR assay 32 and the fact that, initially, not all patients underwent a SARS-CoV-2 virus test may have affected the overall incidence of the COVID-19 disease in this group of patients. Moreover, given the relatively small sample size, it is possible that some differences, including results from the multivariable analysis, were not observed due to type 2 error and lack of study power.
Despite these limitations, our study has strengths to mention. The multicentric nature and the mixture of public and private health, which may reflect most Latin-American countries’ reality, reveal important information about the effects of COVID-19 on this geographic location. Similarly, the 90-day follow-up allowed us to identify an increase in mortality not fully covered by the 30-day assessment carried in other reports.
In conclusion, hip fracture patients with a concomitant SARS-CoV-2 virus infection were associated with a significantly increased mortality and morbidity. COVID-19 status and older age were the only independently significant predictors for mortality during the pandemic and delivered a significant increase in mortality compared to 2019. Efforts should be focused on prompt treatment and strict hospital viral transmission prevention, especially in high-risk geriatric populations.
Acknowledgments
We thank Catalina Vidal, Research Coordinator, and Cristian Velásquez, MD, for their assistance in data collection and processing.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Tomas Zamora, MD  https://orcid.org/0000-0003-3791-0449
https://orcid.org/0000-0003-3791-0449
References
- 1. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi:10.1016/S0140-6736(20)30183-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Johns Hopkins Coronavirus Resource Center. 2020. Accessed December 8, 2020. https://coronavirus.jhu.edu/map.html
- 3. Dyer O. Covid-19 hot spots appear across Latin America. BMJ. 2020;369:m2182. doi:10.1136/bmj.m2182 [DOI] [PubMed] [Google Scholar]
- 4. Hartholt KA, Oudshoorn C, Zielinski SM, et al. The epidemic of hip fractures: are we on the right track? PLoS One. 2011;6(7):e22227. doi:10.1371/journal.pone.0022227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zamora T, Klaber I, Urrutia J. Hip fracture in the elderly. Clin Med Insights Geriatr. 2017;10:1–10. doi:10.1177/1179553017703998 [Google Scholar]
- 6. Slullitel PA, Lucero CM, Soruco ML, et al. Prolonged social lockdown during COVID-19 pandemic and hip fracture epidemiology. Int Orthop. 2020;44(10):1887–1895. doi:10.1007/s00264-020-04769-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kayani B, Onochie E, Patil V, et al. The effects of COVID-19 on perioperative morbidity and mortality in patients with hip fractures. Bone Jt J. 2020;102B(9):1136–1145. doi:10.1302/0301-620X.102B9.BJJ-2020-1127.R1 [DOI] [PubMed] [Google Scholar]
- 8. Lim MA, Pranata R. Coronavirus disease 2019 (COVID-19) markedly increased mortality in patients with hip fracture—a systematic review and meta-analysis. J Clin Orthop Trauma. 2021;12(1):187–193. doi:10.1016/j.jcot.2020.09.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hall AJ, Clement ND, MacLullich AMJ, White TO, Duckworth AD. IMPACT-scot 2 report on COVID-19 in hip fracture patients. Bone Joint J. 2021:1–10. doi:10.1302/0301-620x.103b.bjj-2020-2027.r1 [DOI] [PubMed] [Google Scholar]
- 10. LeBrun DG, Konnaris MA, Ghahramani GC, et al. Hip fracture outcomes during the COVID-19 pandemic: early results from New York. J Orthop Trauma. 2020;34(8):403–410. doi:10.1097/BOT.0000000000001849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Egol KA, Konda SR, Bird ML, et al. Increased mortality and major complications in hip fracture care during the COVID-19 pandemic: a New York City perspective. J Orthop Trauma. 2020;34(8):395–402. doi:10.1097/BOT.0000000000001845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Narang A, Chan G, Aframian A, et al. Thirty-day mortality following surgical management of hip fractures during the COVID-19 pandemic: findings from a prospective multi-centre UK study. Int Orthop. 2021;45(1):23–31. doi:10.1007/s00264-020-04739-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. PAHO. Pan American Health Organization. Health in the Americas. Paho; 1998. Accessed January 2, 2021. https://www.paho.org/salud-en-las-americas-2017/ [Google Scholar]
- 14. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–349. doi:10.1016/j.jclinepi.2007.11.008 [DOI] [PubMed] [Google Scholar]
- 15. Quan H, Li B, Couris CM, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011;173(6):676–682. doi:10.1093/aje/kwq433 [DOI] [PubMed] [Google Scholar]
- 16. Neuhaus V, King J, Hageman MG, Ring DC. Charlson comorbidity indices and in-hospital deaths in patients with hip fractures trauma. Clin Orthop Relat Res. 2013;471(5):1712–1719. doi:10.1007/s11999-012-2705-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Palm H, Krasheninnikoff M, Holck K, et al. A new algorithm for hip fracture surgery. Acta Orthop. 2012;83(1):26–30. doi:10.3109/17453674.2011.652887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Carroll KJ. On the use and utility of the Weibull model in the analysis of survival data. Control Clin Trials. 2003;24(6):682–701. doi:10.1016/S0197-2456(03)00072-2 [DOI] [PubMed] [Google Scholar]
- 19. Zhang Z. Parametric regression model for survival data: Weibull regression model as an example. Ann Transl Med. 2016;4(24):484. doi:10.21037/atm.2016.08.45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Clement ND, Ng N, Simpson CJ, et al. The prevalence, mortality, and associated risk factors for developing COVID-19 in hip fracture patients: a systematic review and meta-analysis. Bone Jt Res. 2020;9(12):873–883. doi:10.1302/2046-3758.912.BJR-2020-0473.R1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Cheung ZB, Forsh DA. Early outcomes after hip fracture surgery in COVID-19 patients in New York City. J Orthop. 2020;21:291–296. doi:10.1016/j.jor.2020.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kronbichler A, Kresse D, Yoon S, Lee KH, Effenberger M, Shin J Il. Asymptomatic patients as a source of COVID-19 infections: a systematic review and meta-analysis. Int J Infect Dis. 2020;98:180–186. doi:10.1016/j.ijid.2020.06.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Dupley L, Oputa TJ, Bourne JT, et al. 30-day mortality for fractured neck of femur patients with concurrent COVID-19 infection. Eur J Orthop Surg Traumatol. 2020;31(2):341–347. doi:10.1007/s00590-020-02778-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Van Praet JT, Claeys B, Coene AS, Floré K, Reynders M. Prevention of nosocomial COVID-19: another challenge of the pandemic. Infect Control Hosp Epidemiol. 2020;41(11):1355–1356. doi:10.1017/ice.2020.166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. The Lancet. COVID-19 in Latin America: a humanitarian crisis. Lancet. 2020;396(10261):1463. doi:10.1016/S0140-6736(20)32328-X [DOI] [PubMed] [Google Scholar]
- 26. Garcia PJ, Alarcón A, Bayer A, et al. COVID-19 response in Latin America. Am J Trop Med Hyg. 2020;103(5):1765–1772. doi:10.4269/ajtmh.20-0765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Pintado JF, Gibaja W, Vallejos RA, Rosas W, Guerra-Farfan E, Nuñez JH. How COVID-19 has affected emergent visits to a Latin-American trauma department: experience at a Peruvian National Trauma Referral Center. Injury. 2020;51(12):2834–2839. doi:10.1016/j.injury.2020.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Almaadany FS, Samadov E, Namazov I, et al. Mortality and pulmonary complications in patients undergoing surgery with perioperative sars-cov-2 infection: an International Cohort Study. Lancet. 2020;396(10243):27–38. doi:10.1016/S0140-6736(20)31182-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hasan SS, Radford S, Kow CS, Zaidi STR. Venous thromboembolism in critically ill COVID-19 patients receiving prophylactic or therapeutic anticoagulation: a systematic review and meta-analysis. J Thromb Thrombolysis. 2020;50(4):814–821. doi:10.1007/s11239-020-02235-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Donnelly JP, Wang XQ, Iwashyna TJ, Prescott HC. Readmission and death after initial hospital discharge among patients with COVID-19 in a large multihospital system. JAMA. 2021;325(3):304–306. doi:10.1001/jama.2020.21465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Tripathy SK, Varghese P, Panigrahi S, et al. Thirty-day mortality of patients with hip fracture during COVID-19 pandemic and pre-pandemic periods: a systematic review and meta-analysis. World J Orthop. 2021;12(1):35–50. doi:10.5312/WJO.V12.I1.35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Wang W, Xu Y, Gao R, et al. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA. 2020;323(18):1843–1844. doi:10.1001/jama.2020.3786 [DOI] [PMC free article] [PubMed] [Google Scholar]