Abstract
Objective
To investigate whether the modified K‐line can be used to predict the clinical outcome and to determine the surgical approach for K‐line (−) patients with cervical ossification of the posterior longitudinal ligament (OPLL).
Methods
A new modified K‐line was defined as the line connecting the midpoints of the spinal cord at C4 and C6 on the lateral cervical radiographs. A total of four consecutive patients (three men and one woman) with cervical myelopathy due to OPLL were included in this research. The patients were diagnosed with OPLL with K‐line (−) while they were also classified as modified K‐line (+). Preoperative modified K‐line was used to predict the surgical outcome in K‐line (−) patients with OPLL according to the original K‐line. And a modified laminoplasty with C3 laminectomy and C4‐6 bilateral open‐door laminoplasty was adopted to perform on all the patients. The Japanese Orthopaedic Association scores before surgery and at 1‐year follow‐up after surgery were evaluated and the recovery rate was calculated. The visual analogue scale (VAS) scores were also evaluated before surgery and after surgery. Furthermore, cervical plain radiographs in neutral position before surgery and after surgery were obtained to measure C2–C7 angles for assessing the cervical sagittal alignment.
Results
The results showed that good neurological improvement could be achieved in all K‐line (−) patients who underwent C3 laminectomy with C4–C6 bilateral open‐door laminoplasty. The Postoperative JOA scores improved from 13.5 to 16.5, from 11 to 16.5, from 13 to 16, and from 12.5 to 13, respectively. The mean recovery rate was 65.4% in the K‐line (−) patients. And the VAS scores dropped from 3 to 1, 5 to 2, 5 to 3, and 4 to 2, respectively. The JOA and VAS scores showed satisfaction in all patients at the 1‐year follow‐up. Relatively satisfactory and stable cervical sagittal alignment was observed on postoperative lateral radiography in all patients at the 3‐month follow‐up period. There were no postoperative complications associated with this technique found in all the patients.
Conclusions
Modified K‐line may predict the clinical outcome of this modified laminoplasty and offer guidance regarding the choice of surgical method for K‐line (−) patients with OPLL. Additionally, C3 laminectomy with C4–C6 bilateral open‐door laminoplasty should be recommended for the use in patients with K‐line (−) OPLL, who were also classified as modified K‐line (+). However, further studies with more cases will be required to reveal its generalizability and availability.
Keywords: Cervical myelopathy, Laminectomy, Laminoplasty, Modified K‐line, Ossification of the posterior longitudinal ligament
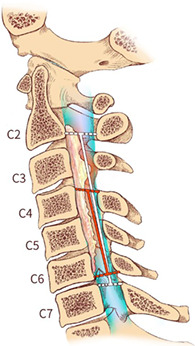
Illustration of the K‐line and modified K‐line on a plain lateral radiograph. K‐line was defined as a straight line connecting the midpoints of the spinal canal at C2 and C7 introduced by Fujiyoshi et al. (white line). A modifed straight line connecting the midpoints of the spinal canal from C4–C6 was first raised based on the K‐line (red line).
Introduction
Ossification of the posterior longitudinal ligament (OPLL) is a common disorder that often leads to neurological symptoms, ranging from discomfort to severe myelopathy, due to compression of the spinal cord and nerve roots by progressive ossification. One of the main surgical treatments is laminoplasty from posterior decompression 1 . The K‐line can predict clinical outcomes after laminoplasty, as reported in the previous research 2 . The K‐line is defined as a straight line connecting the midpoints of the spinal canal at C2 and C7 on lateral radiographs. OPLL not exceeding the K‐line is indicated by K‐line (+), and OPLL extending beyond the K‐line is considered K‐line (−) 2 . Previous research has demonstrated sufficient neurological improvement could be obtained from posterior decompression procedure in the K‐line (+) patients with cervical OPLL 2 . Thus, the selection of surgeries from the posterior approach is appropriate for such patients. Although laminoplasty has been recognized as a standard procedure to release the compression of the spinal cord due to cervical multilevel OPLL, it may be accompanied by persistent axial symptoms when damaging semispinalis cervicis muscles 3 , 4 . Recently, numerous papers have reported that C4–C7 laminoplasty with C3 laminectomy is an effective technique for preventing postoperative axial symptoms 5 . In contrast, C3–C6 laminoplasty has a significantly lower incidence of axial neck pain 6 , for which the spinal cord is rarely affected at the C6/7 level in patients with degenerative spinal diseases 7 .
In K‐line (−) cases, anterior decompression with fusion (ADF) or posterior decompression with fusion (PDF) is a commonly used surgical procedure that would be recommendable. However, some complications usually occur in these procedures, including upper airway obstruction, adjacent‐segment degeneration, C5 palsy, and a reduction in the ROM of the cervical spine 8 , 9 .
To our knowledge, the K‐line is a reliable clinical indicator which plays a significant role in selecting the surgical approach of patients with cervical myelopathy caused by OPLL. However, it is not suitable in all kinds of conditions, especially for certain regional larger OPLL masses. On the one hand, it was designed for total en bloc laminoplasty of five segments from C3 to C7. Therefore, segmental larger OPLL masses may make a difference to the result of K‐line, decreasing its predictive value. On the other hand, the loss of cervical lordosis at segmental level could also change K‐line (+) into K‐line (−). Furthermore, Taniyama et al. 10 , 11 made a modification of the K‐line as the line that connecting the midpoints of the spinal cord at C2 and C7 on preoperative T1‐weighted sagittal MRI, which demonstrated that this modified K‐line could be used to predict insufficient decompression of cervical laminoplasty and clinical outcome in patients with non‐lordotic alignment. Another study indicated that the modified K‐line can provide a guide for predicting poor clinical outcome after laminoplasty and making decisions regarding the surgical approach in patients with cervical spondylotic myelopathy 12 .
Taking all these things into consideration, we introduced a new modified K‐line, which is defined as the line connecting the midpoints of the spinal cord at C4 and C6 on the lateral cervical radiographs, to assess whether this index predicted clinical outcome after laminoplasty in patients with K‐line (−) OPLL. Additionally, we adopted C3 laminectomy with C4–C6 bilateral open‐door laminoplasty as a surgical procedure for cervical OPLL patients in this study.
The purpose of this study was to: (i) investigate the influence of the modified K‐line on the selection of the surgical approach in patients with k‐line (‐) OPLL; (ii) investigate whether the modified K‐line should be applied to evaluate the surgical outcomes for patients with K‐line (−) OPLL; (iii) assess the efficiency and safety of C3 laminectomy with C4–C6 laminoplasty that performed on the patients with K‐line (−) OPLL.
Methods
Modified K‐line
To draw the modified K‐line, the same instructions were used as those for drawing the original K‐line. A lateral view of the cervical radiograph was used in the neutral position. We drew a straight line that connected the midpoints of the spinal canal from the C4–C6 segments on plain lateral radiographs in the neutral position, which defined as modified K‐line (Fig. 1). As the original K‐line, the modified K‐line (+) meant that the OPLL mass did not pass the modified K‐line, while the modified K‐line (−) meant that the OPLL extended beyond the modified K‐line. The patients were also divided into groups with modified K‐line (+) and modified K‐line (−) according to the original definition of the K‐line.
FIG 1.
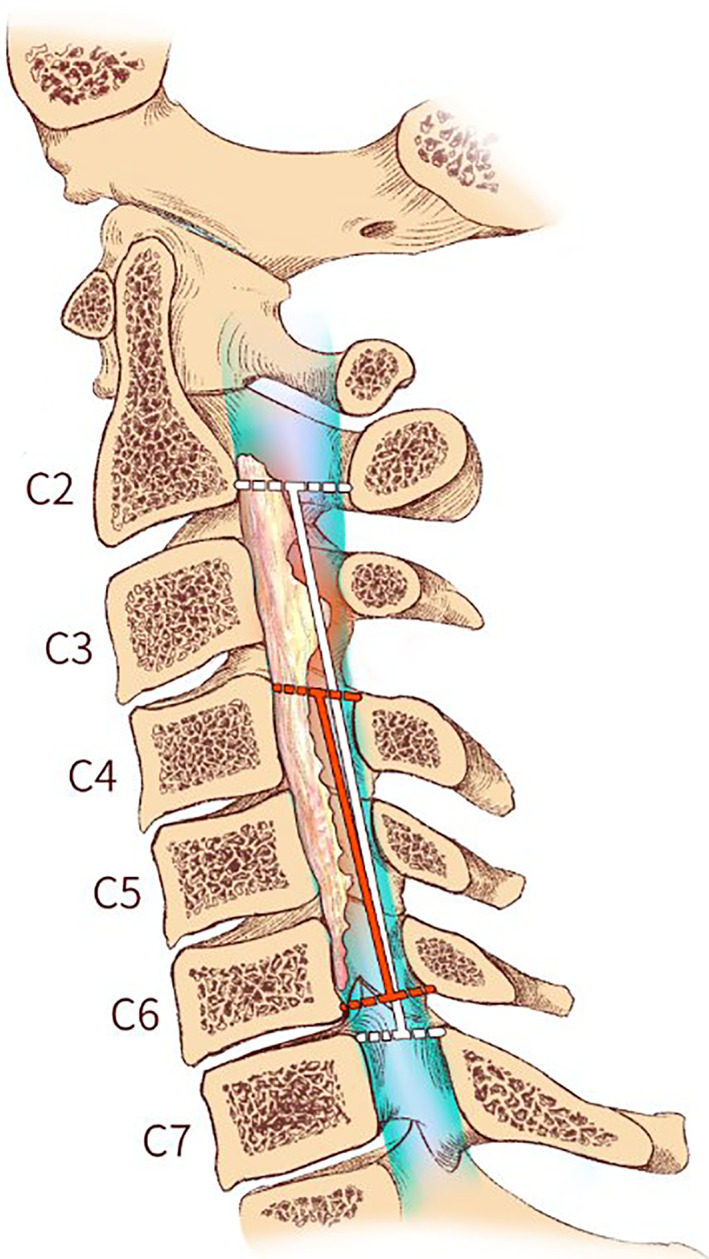
Illustration of the K‐line and modified K‐line on a plain lateral radiograph. K‐line was defined as a straight line connecting the midpoints of the spinal canal at C2 and C7 introduced by Fujiyoshi et al. (white line). A modifed straight line connecting the midpoints of the spinal canal from C4–C6 was first raised based on the K‐line (red line).
Patients
This study was approved by the ethics committee of the First affiliated Hospital of Sun Yat‐sen University. Patients with cervical myelopathy due to OPLL underwent posterior decompression surgery. A total of four consecutive patients with K‐line (−) OPLL between January 2017 and May 2018 were included and these patients with modified K‐line (+) OPLL were confirmed by two spine surgeons. All the patients with modified K‐line (+) OPLLAQ34 were diagnosed based on these patients with original K‐line (−). All the patients presented with severe symptoms caused by spinal cord compression and cervical lordosis. All the patients were followed up for at least 1 year. Our cervical enlargement laminoplasty consisted of C4 to C6 laminoplasty (Kurokawa's method) with C3 laminectomy 13 . The mean age at surgery was 56.8 years old. An example (case 1) is shown in Fig. 2.
FIG 2.
Case 1 Images obtained from a 51‐year‐old female who presented with hand numbness. (A) Preoperative plain lateral radiograph showing an OPLL mass surpassing the K‐line but not extending beyond the modified K‐line. (B) Flexion and extension lateral radiographs. (C) Preoperative sagittal CT showing a multilevel OPLL mass. (D) cervical sagittal MRI showing spinal cord compression due to OPLL. (E) postoperative plain lateral radiograph showing C3 laminectomy with C4‐6 bilateral open‐door laminoplasty.
Clinical Assessment
Japanese Orthopaedic Association Score and Recovery Rate
The Japanese Orthopaedic Association (JOA) score was introduced to assess the neurological outcomes for cervical myelopathy. The JOA scores were evaluated before surgery and 1 year after surgery according to the JOA scale. And the recovery rates of the JOA score were calculated as follows:
Recovery ratio (%) = 100 (postoperative score – preoperative score)/ (17 – preoperative score) 14 .
The JOA score and recovery rate was to evaluate spinal cord function. Recovery ratio of more than 75% is regarded as excellent effect, 50% to 75% is considered as favorable treatment, 25% to 50% means ordinary effect, 0% to 25% indicates invalid treatment, and less than 0% is considered as deteriorated treatment.
Visual Analogue Scale Score
The visual analog scale (VAS) was commonly used to assess neck pain after surgery. The VAS scores were evaluated according to VAS scale preoperatively and postoperatively. The VAS score can respond to the validity of treatment: VAS of 0 to 2 is considered as excellent effect, 3 to 5 indicates favorable treatment, 6 to 8 means accepatable effect, and more than 8 is regarded as poor treatment.
Radiological Assessment
C2–C7 Lordotic Angle
The C2–C7 lordotic angle was defined as the Cobb angle formed by the inferior endplate of C2 and C7 on a standing lateral radiograph. C2–C7 lordotic angle was measured on the lateral radiograph before and after surgery. Cervical lordosis was used to predicted the surgical prognosis assessed by the C2–C7 lordotic angle.
Ossification Thickness
The thickness of OPLL was measured as the thickest part of the OPLL by sagittal CT reconstruction images. The thickness of OPLL contributed to the assessment of OPLL.
Spinal Canal Occupation Ratio
The spinal canal occupation ratio was defined as the ratio of maximum anteroposterior thickness of ossified ligament to anteroposterior diameter of spinal canal. The occupying ratio of the spinal canal was measured on a CT sagittal image before operation. The spinal canal occupation ratio was helpful to assess the severity of cord compression and directing surgical treatment.
The OPLL Types
OPLL was classified into continuous, segmental, mixed, or localized type on the basis of the criteria previously reported. The OPLL type was observed on the CT reconstruction sagittal image. The type of OPLL contributed to the assessment of OPLL and selection of surgical method.
Areas of Ossified Vertebrae
Radiological features of OPLL showed it involved different areas of ossified vertebrae due to its different type. The areas of ossified vertebrae were observed on a sagittal view of CT of the cervical spine. The areas of ossified vertebrae contributed to the assessment of OPLL and the instruction to surgery.
Results
General Results
All patients exhibited improvement of both subjective symptoms and clinical scores. The preoperative and postoperative clinical data are summarized (Table 1). No systemic complications occurred in any of the patients at the final follow‐up period. The mean operative time was 90 min, and the mean amount of blood loss was 50 mL. The postoperative lateral radiographs revealed cervical lordosis with a modified K‐line (+) and sufficient enlargement of the spinal cord. Examples (cases 2 and 3) are shown in Figs 3 and 4. In addition, the postoperative lateral radiographs also revealed cervical lordosis with K‐line (+). An example (case 4) is shown in Fig. 5.
TABLE 1.
Characteristics of the four patients with cervical myelopathy and OPLL
| Case No. | Age (yrs), Sex | Major Symptoms | VAS | C‐JOA | C2‐7 Lordosis (degree) | Levels of OPLL | Follow‐up Period | Ossification thickness(mm) | Type of OPLL | Occupation ratio (%) | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Preop | Postop | Preop | Postop | Preop | Surgical intervention | Final FU | ||||||||
| 1 | 51, F | Hand numbness | 3 | 1 | 13.5 | 16.5 | 4.13 | 2.42 | 14 | C2‐6 | 1 | 8.7 | mix | 75.0 |
| 2 | 59, M | Hand clumsiness, Gait disturbance | 5 | 2 | 11 | 16.5 | 8.45 | 14.16 | 8.28 | C1‐5 | 1 | 6.89 | continuous | 48.3 |
| 3 | 53, M | Hand numbness | 5 | 3 | 13 | 16 | 8.19 | 18.43 | 5.91 | C2‐7 | 1 | 4.29 | mix | 31.3 |
| 4 | 54, M | Hand numbness | 4 | 2 | 12.5 | 13 | 8.26 | 4.7 | 12.3 | C3‐7 | 1 | 5.51 | mix | 34.5 |
Abbreviations: F, female; JOA, Japanese orthopedic association; M, male; VAS, Visual analog scale; OPLL, posterior longitudinal ligament.
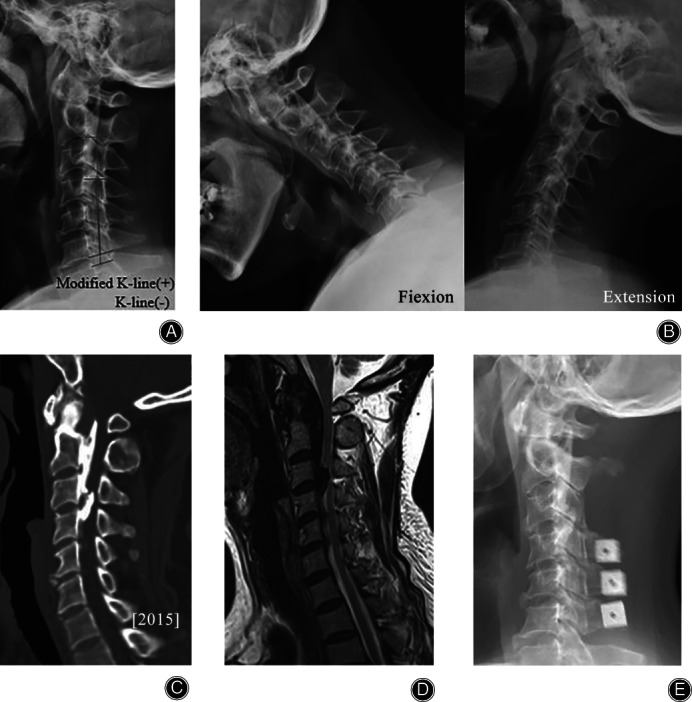
FIG 3.
Case 2 Images from a 59‐year‐old male who presented with hand clumsiness and slowly progressive gait disturbance. (A) Preoperative plain lateral radiograph showing K‐line (−) but modified K‐line (+). (B) Dynamic plain lateral radiographs. (C) Sagittal three‐dimensional reconstructed CT showing a continuous OPLL mass (arrows). (D) MR image showing multilevel spinal cord compression. (E) Postoperative plain lateral radiograph showing C3 laminectomy with C4–C6 laminoplasty after installing allograft bone (arrows) and modified K‐line (+).
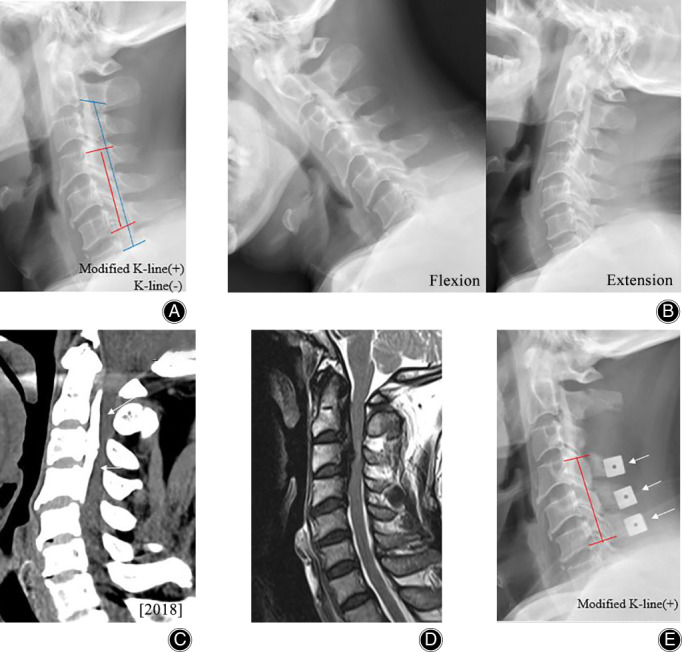
FIG 4.
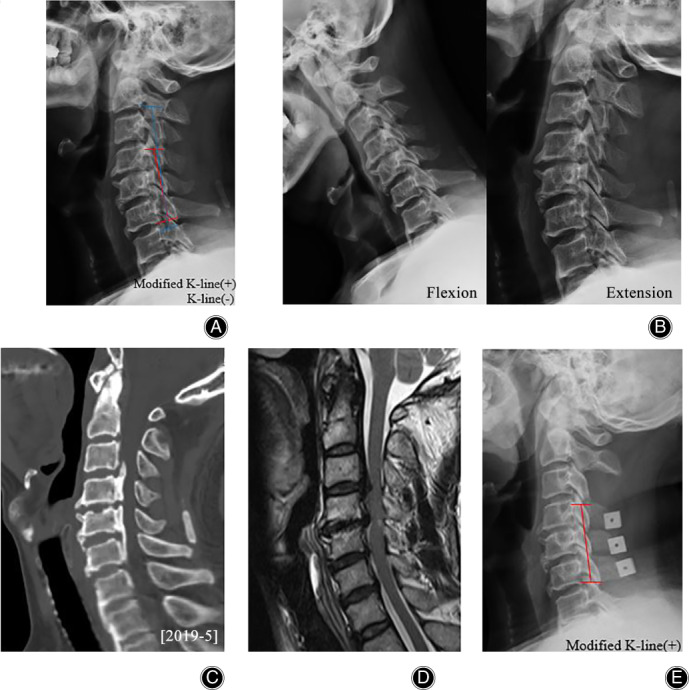
Case 3 Images obtained from a 53‐year‐old male who presented with hand numbness. (A) cervical plain lateral radiograph demonstrated K‐line (−) but modified K‐line (+). (B) Flexion and extension lateral radiographs. (C) Sagittal CT reconstruction image demonstrated a continuous and segmental OPLL mass. (D) T2‐weighted MR image demonstrated severe spinal cord compression caused by OPLL. (E) Postoperative plain lateral radiograph demonstrated modified K‐line (+).
FIG 5.
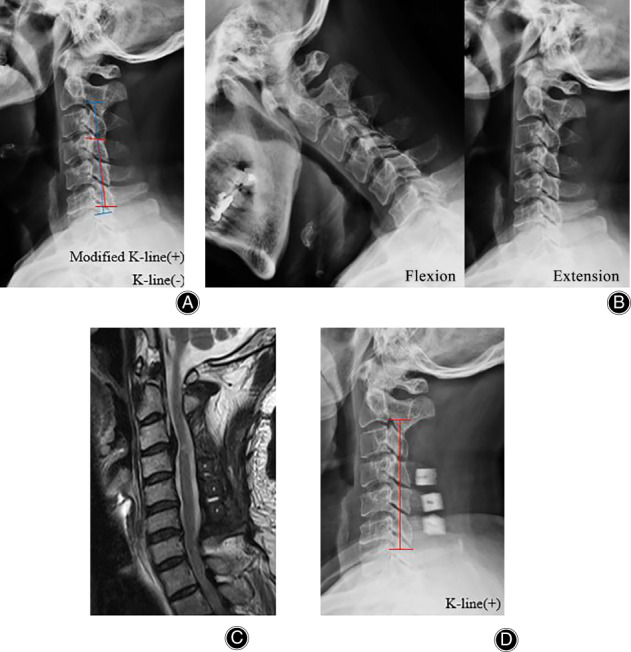
Case 4 Images obtained from a 54‐year‐old male who presented with hand numbness and underwent C3 laminectomy with C4–C6 laminoplasty. (A) Preoperative plain lateral radiograph showing K‐line (−) but modified K‐line (+). (B) Dynamic plain lateral radiographs. (C) MR image showing spinal cord compression. (D) Postoperative plain lateral radiograph showing K‐line (+).
Clinical Results
Japanese Orthopaedic Association Score and Recovery Rate
The JOA scores improved (from 13.5 to 16.5, from 11 to 16.5, from 13 to 16, and from 12.5 to 13) in all patients at the 1‐year follow‐up. The recovery rate in all patients with K‐line (−) was 85.7%, 91.7%, 75%, and 11.1%, respectively.
Visual Analogue Scale Score
The VAS scores in all patients decreased from 3 to 1, 5 to 2, 5 to 3, and 4 to 2, respectively.
Radiological Results
C2–C7 Lordotic Angle
The mean C2‐7 lordotic angles preoperatively and immediately after surgery were also shown in Table 1. The mean C2–C7 lordotic angles immediately changed in all patients after surgery from 4.13° to 2.42°, from 8.45° to 14.16°, from 8.19° to 18.43°, and from 8.26° to 4.7°. The radiological parameters regarding cervical sagittal alignment remained stable, and there were no changes in kyphosis at the 3‐month follow‐up.
Ossification Thickness
The ossification thickness in all patients was 8.7 mm, 6.89 mm, 4.29 mm, and 5.51 mm, respectively. And the mean ossification thickness was 6.35 mm.
Spinal Canal Occupation Ratio
The spinal canal occupation ratio in patients was 75%, 48.3%, 31.3%, 34.5%, respectively.
The OPLL Types
Among these K‐line (−) patients with cervical myelopathy due to multilevel OPLL, mixed‐type was the major cause and continuous‐type was the other cause.
Areas of Ossified Vertebrae
All patients with OPLL involved in multilevel cervical vertebrae, including C2–C6, C1–C5, C2‐7, and C3–C7.
Discussion
Cervical myelopathy resulting from OPLL is a common condition that can lead to cervical cord compression and usually requires surgical decompression. Although the selection of the anterior or posterior approach has been the subject of debate 15 , multilevel cord compression by OPLL and preoperative cervical lordotic sagittal alignment are conditions that favor a posterior approach 16 . Cervical laminoplasty has been a standard treatment for compressive myelopathy associated with OPLL with fewer complications than anterior or posterior fusion. The long‐term neurologic results of laminoplasty over 10 years have been satisfactory 17 , 18 , 19 . However, many studies have shown that poor clinical and radiological outcomes may occur if posterior laminoplasty is performed in OPLL patients with K‐line (−) 2 , 9 , 20 . The K‐line has been reported to be a reliable indicator that may predict surgical outcomes in patients with OPLL and cervical myelopathy 2 , and it has been suggested that sufficient posterior shifting of the spinal cord will not be obtained after posterior decompressive surgery in K‐line (−) patients.
For cervical lordosis in K‐line (−) patients with multilevel OPLL masses, ADF might be considered an appropriate way to rebuild cervical alignment and save neurological function. Previous studies showed that ADF was one of the suitable surgical options that could provide better improvement than laminoplasty or PDF for K‐line (−) patients with OPLL 9 , 21 , 22 . However, this approach requires high technical demands that accompanies by a high incidence of surgery‐related complications, including CSF leakage, dysphagia, C5 nerve palsy, and graft‐related problems 23 , 24 . By comparison, laminoplasty as an indirect method for relieving spinal cord compression may be more effective and safer to obtain better surgical outcomes in K‐line (−) patients with OPLL under certain circumstances. In addition, PDF could be a surgical option for K‐line (−) patients with OPLL 22 . Obviously, there is a lack of evidence to support posterior decompression for K‐line (−) patients with OPLL.
Several studies have shown that the K‐line in different cervical positions will lead to different treatments and will affect clinical outcomes 20 , 25 , 26 . Regarding the influence and efficiency of the K‐line, we introduced a new concept of the modified K‐line in different segments of the cervical spine, which may provide a basis for the posterior approach, especially for K‐line (−) patients with OPLL. In the current study, we proposed a new modified K‐line that changed from C2–C7 to C4–C6, and patients with K‐line (−) OPLL were classified as modified K‐line (+) confirmed by two independent spine surgeons. Regarding the surgical options, we believe it is highly advisable to choose a modified laminoplasty according to the results of previous reports 5 , 6 , 13 , 27 and personal experience. Thus, C4–C6 laminoplasty with C3 laminectomy was conducted, and almost all the patients attained good recovery of neurological function and maintained acceptable sagittal alignment of the cervical spine after this modified laminoplasty in accordance with the modified K‐line. By using the modified K‐line, we also evaluated cervical alignment and OPLL size specifically.
In the present study, three of the patients achieved a high recovery rate of the JOA score, and one of them had a low recovery rate. The average recovery rate of the JOA score was 65.4%, which is consistent with the clinical results described in a previous study 21 , 24 , 28 , 29 . Ha et al. reported that laminoplasty was much better at preserving preoperative cervical lordosis and cervical range of motion, and maximally reduced neck disability than laminectomy with fusion 30 . In our study, two patients lost preoperative cervical lordosis on immediate postoperative plain radiography and regained cervical lordosis at the final follow‐up. There were no kyphotic changes found in any of the patients, and high satisfaction was achieved by using this technique. These may be slightly different results from those showing that K‐line (−) patients obtained poor neurological improvement after double‐door C2–C7 or C3–C7 laminoplasty 31 . These possible explanations for this finding could be the function of modified K‐line (+) and this surgical technique. It was shown that almost the same neurologic recovery and radiological results were obtained in K‐line (+) patients, which is probably more applicable than the K‐line in OPLL.
Limitations
There are several limitations in this study. First, a large sample of randomized controlled studies was lacking to confirm the advantage of this parameter. We still need a multicenter trial to reveal the effectiveness and instruction of this modified K‐line. Second, this technique was not be applied to patients with continuous ossification of the upper cervical region. Third, the radiological follow‐up time was not satisfied due to patients' compliance. In this study, our work mainly focused on the guidance of the modified K‐line to determine the surgical approach, without a focus on the surgical procedure or surgical timing that may influence the results. Finally, multivariable analyses with more cases should be used to assess the surgical outcomes of this technique, and long‐term follow‐up is strongly needed in future studies.
Conclusion
Our results suggest that the modified K‐line may be an indicator for predicting clinical outcome and it could provide a basis for the determination of surgical approaches in such patients. C3 laminectomy with C4–C6 bilateral open‐door laminoplasty is a relatively safe and effective technique, which should be recommended for the use in patients with K‐line (−) OPLL when patients are classified as modified K‐line (+). However, further investigation is needed to clarify the efficiency and universality of these results.
Author Contribution
All authors contributed to this paper in terms of the conception and design of the study; the literature review and analysis; drafting, critical revision, and editing; and approval of the final version.
Grant Sources: No external financial support was received for this study.
References
- 1. Iwasaki M, Okuda S, Miyauchi A, et al. Surgical strategy for cervical myelopathy due to ossification of the posterior longitudinal ligament: part 1: clinical results and limitations of laminoplasty. Spine, 2007, 32: 647–653. [DOI] [PubMed] [Google Scholar]
- 2. Fujiyoshi T, Yamazaki M, Kawabe J, et al. A new concept for making decisions regarding the surgical approach for cervical ossification of the posterior longitudinal ligament: the K‐line. Spine, 2008, 33: E990–E993. [DOI] [PubMed] [Google Scholar]
- 3. Kang MS, Kim KH, Park JY, et al. Progression of cervical ossification of posterior longitudinal ligament after Laminoplasty or laminectomy with posterior fixation. Clin Spine Surg, 2019, 32: 363–368. [DOI] [PubMed] [Google Scholar]
- 4. Umeda M, Sasai K, Kushida T, et al. A less‐invasive cervical laminoplasty for spondylotic myelopathy that preserves the semispinalis cervicis muscles and nuchal ligament. J Neurosurg Spine, 2013, 18: 545–552. [DOI] [PubMed] [Google Scholar]
- 5. Takeuchi K, Yokoyama T, Aburakawa S, et al. Axial symptoms after cervical laminoplasty with C3 laminectomy compared with conventional C3‐C7 laminoplasty: a modified laminoplasty preserving the semispinalis cervicis inserted into axis. Spine, 2005, 30: 2544–2549. [DOI] [PubMed] [Google Scholar]
- 6. Hosono N, Sakaura H, Mukai Y, Fujii R, Yoshikawa H. C3‐6 laminoplasty takes over C3‐7 laminoplasty with significantly lower incidence of axial neck pain. Eur Spine J, 2006, 15: 1375–1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hayashi H, Okada K, Hashimoto J, Tada K, Ueno R. Cervical spondylotic myelopathy in the aged patient. A radiographic evaluation of the aging changes in the cervical spine and etiologic factors of myelopathy. Spine, 1988, 13: 618–625. [PubMed] [Google Scholar]
- 8. Nakashima H, Imagama S, Yukawa Y, et al. Multivariate analysis of C‐5 palsy incidence after cervical posterior fusion with instrumentation. J Neurosurg Spine, 2012, 17: 103–110. [DOI] [PubMed] [Google Scholar]
- 9. Yoshii T, Sakai K, Hirai T, et al. Anterior decompression with fusion versus posterior decompression with fusion for massive cervical ossification of the posterior longitudinal ligament with a >/=50% canal occupying ratio: a multicenter retrospective study. Spine J, 2016, 16: 1351–1357. [DOI] [PubMed] [Google Scholar]
- 10. Taniyama T, Hirai T, Yamada T, et al. Modified K‐line in magnetic resonance imaging predicts insufficient decompression of cervical laminoplasty. Spine, 2013, 38: 496–501. [DOI] [PubMed] [Google Scholar]
- 11. Taniyama T, Hirai T, Yoshii T, et al. Modified K‐line in magnetic resonance imaging predicts clinical outcome in patients with nonlordotic alignment after laminoplasty for cervical spondylotic myelopathy. Spine, 2014, 39: E1261–E1268. [DOI] [PubMed] [Google Scholar]
- 12. Sun LQ, Li M, Li YM. Prediction of incomplete decompression after cervical laminoplasty on magnetic resonance imaging: the modified K‐line. Clin Neurol Neurosurg, 2016, 146: 12–17. [DOI] [PubMed] [Google Scholar]
- 13. Takeuchi K, Yokoyama T, Wada KI, Kudo H. Relationship between enlargement of the cross‐sectional area of the Dural sac and neurological improvements after cervical Laminoplasty: differences between cervical Spondylotic myelopathy and ossification of the posterior longitudinal ligament. Spine Surg Relat Res, 2018, 3: 27–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kato S, Oshima Y, Oka H, et al. Comparison of the Japanese Orthopaedic association (JOA) score and modified JOA (mJOA) score for the assessment of cervical myelopathy: a multicenter observational study. PLoS One, 2015, 10: e0123022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wu JC, Chen YC, Huang WC. Ossification of the posterior longitudinal ligament in cervical spine: prevalence, management, and prognosis. Neurospine, 2018, 15: 33–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lawrence BD, Shamji MF, Traynelis VC, et al. Surgical management of degenerative cervical myelopathy: a consensus statement. Spine, 2013, 38: S171–S172. [DOI] [PubMed] [Google Scholar]
- 17. Seichi A, Takeshita K, Ohishi I, et al. Long‐term results of double‐door laminoplasty for cervical stenotic myelopathy. Spine, 2001, 26: 479–487. [DOI] [PubMed] [Google Scholar]
- 18. Matsumoto M, Chiba K, Toyama Y. Surgical treatment of ossification of the posterior longitudinal ligament and its outcomes: posterior surgery by laminoplasty. Spine, 2012, 37: E303–E308. [DOI] [PubMed] [Google Scholar]
- 19. Wang L, Wei F, Liu S, et al. Can modified Kurokawa's double‐door Laminoplasty reduce the incidence of axial symptoms at long‐term follow‐up?:a prospective study of 152 patients with cervical Spondylotic myelopathy. J Spinal Disord Tech, 2015, 28: E186–E193. [DOI] [PubMed] [Google Scholar]
- 20. Takeuchi K, Yokoyama T, Numasawa T, et al. K‐line (−) in the neck‐flexed position in patients with ossification of the posterior longitudinal ligament is a risk factor for poor clinical outcome after cervical Laminoplasty. Spine, 2016, 41: 1891–1895. [DOI] [PubMed] [Google Scholar]
- 21. Koda M, Mochizuki M, Konishi H, et al. Comparison of clinical outcomes between laminoplasty, posterior decompression with instrumented fusion, and anterior decompression with fusion for K‐line (−) cervical ossification of the posterior longitudinal ligament. Eur Spine J, 2016, 25: 2294–2301. [DOI] [PubMed] [Google Scholar]
- 22. Saito J, Maki S, Kamiya K, et al. Outcome of posterior decompression with instrumented fusion surgery for K‐line (−) cervical ossification of the longitudinal ligament. J Clin Neurosci, 2016, 32: 57–60. [DOI] [PubMed] [Google Scholar]
- 23. Kimura A, Seichi A, Hoshino Y, et al. Perioperative complications of anterior cervical decompression with fusion in patients with ossification of the posterior longitudinal ligament: a retrospective, multi‐institutional study. J Orthop Sci, 2012, 17: 667–672. [DOI] [PubMed] [Google Scholar]
- 24. Xu P, Zhuang JS, Huang YS, Tu C, Chen JT, Zhong ZM. Surgical outcomes of cervical myelopathy due to ossification of posterior longitudinal ligament: anterior decompression and fusion versus posterior laminoplasty. J Orthop Surg, 2019, 27: 2309499019837907. [DOI] [PubMed] [Google Scholar]
- 25. Nori S, Aoyama R, Ninomiya K, Suzuki S, Anazawa U, Shiraishi T. K‐line (−) in the neck‐flexed position affects surgical outcomes in patients with ossification of the posterior longitudinal ligament after muscle‐preserving selective laminectomy. J Orthop Sci, 2019, S0949‐2658: 30322–30327. [DOI] [PubMed] [Google Scholar]
- 26. Li J, Zhang Y, Zhang N, et al. Clinical outcome of Laminoplasty for cervical ossification of the posterior longitudinal ligament with K‐line (−) in the neck neutral position but K‐line (+) in the neck extension position: a retrospective observational study. Medicine, 2017, 96: e6964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hirabayashi S. Recent surgical methods of double‐door Laminoplasty of the cervical spine (Kurokawa's method). Spine Surg Relat Res, 2018, 2: 154–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Sakai K, Okawa A, Takahashi M, et al. Five‐year follow‐up evaluation of surgical treatment for cervical myelopathy caused by ossification of the posterior longitudinal ligament: a prospective comparative study of anterior decompression and fusion with floating method versus Laminoplasty. Spine, 2012, 37: 367–376. [DOI] [PubMed] [Google Scholar]
- 29. Masaki Y, Yamazaki M, Okawa A, et al. An analysis of factors causing poor surgical outcome in patients with cervical myelopathy due to ossification of the posterior longitudinal ligament: anterior decompression with spinal fusion versus laminoplasty. J Spinal Disord Tech, 2007, 20: 7–13. [DOI] [PubMed] [Google Scholar]
- 30. Ha Y, Shin JJ. Comparison of clinical and radiological outcomes in cervical laminoplasty versus laminectomy with fusion in patients with ossification of the posterior longitudinal ligament. Neurosurg Rev, 2019, 43: 1409–1421. [DOI] [PubMed] [Google Scholar]
- 31. Kanbara S, Imagama S, Ito K, Ito K, Ishiguro N, Kato F. A retrospective imaging study of surgical outcomes and range of motion in patients with cervical ossification of the posterior longitudinal ligament. Eur Spine J, 2018, 27: 1416–1422. [DOI] [PubMed] [Google Scholar]


