Abstract
Objective
This study aimed to investigate the clinical effects of surgically treating lumbosacral tuberculosis with a modified posterior unilateral limited laminectomy method for debridement.
Methods
This retrospective study enrolled a total of 26 patients who were administered in our institution from January 2010 to December 2016, diagnosed with lumbosacral tuberculosis at the L5/S1 level, and underwent one‐stage posterior unilateral limited laminectomy as surgical treatment for debridement, allograft of cortical bone grafting, and fixation. The erythrocyte sedimentation rate (ESR), C‐reactive protein (CRP) level, visual analog scale (VAS) score, Oswestry Disability Index (ODI), and lumbosacral angle (LA, Cobb's method) were statistically compared, and the American Spinal Injury Association Impairment (ASIA) Scale was compared between the preoperative and postoperative time points to evaluate the clinical outcomes.
Results
All 26 patients were observed during the follow‐up period, and the mean follow‐up time was 1.3 ± 0.42 years. The mean age was 56 ± 7.4 years old. The average operation time was 118.1 ± 17.5 min, and the mean bleeding volume was 513.0 ± 79.6 mL. There were no intraoperative complications or tuberculous sinus, and two cases experienced hypostatic pneumonia during hospitalization, which resolved with responsive antibiotics and symptomatic supportive treatment. At the final follow‐up, there was no recurrence of tuberculosis, and the ESR (11.8 ± 1.8 mm/h) and CRP (3.0 ± 1.0 mg/L) levels in all patients had returned to normal. The patients with neurologic deficits had improved, and the mean ODI was 79.9 ± 10.6 (87–62) preoperatively and significantly decreased to 20.5 ± 5.7 (11–29) at the final follow‐up (P < 0.01). ASIA scale scores were improved by 1~2 grades at the last follow‐up. The patients' pain levels were significantly alleviated; the mean VAS score declined to 1.2 ± 0.4 (0–2.5) at the final follow‐up compared to 7.5 ± 1.6 (6.5–8.5) preoperatively (P < 0.01). All patients achieved bony graft fusion at an average time of 6.8 ± 1.2 months. Physiological lumbar lordosis was significantly improved, and the mean LA before operation was 17.6° ± 2.1°, which was significantly different from the postoperative LA (29.3° ± 7.4°, P < 0.01) at the final follow up. The LA (27.1° ± 5.5°, P = 0.15) slightly rebounded but without significance compared to the postoperative level.
Conclusion
Only posterior approach by unilateral limited laminectomy for debridement could be served as an effective and safe method to treat short‐segment lumbosacral tuberculosis without extensive anterior sacral and gravitation abscesses.
Keywords: Clinical effects, Debridement, Spine, Tuberculosis, Unilateral limited laminectomy
One‐stage posterior unilateral limited laminectomy for debridement, internal fixation, and bone graft fusion could reserve the posterior appurtenances of the lumbosacral spine, and serve as an effective procedure to treat short‐segment lumbosacral tuberculosis without extensive anterior sacral abscesses and gravitation abscesses.
Introduction
The World Health Organization has reported that tuberculosis is still a major global public health problem worldwide 1 . Spinal tuberculosis accounts for almost 50% of all skeletal/joint tuberculosis cases, of which lumbosacral tuberculosis is uncommon and only accounts for approximately 2%–3% of all spinal tuberculosis cases 2 . The lumbosacral region, as the transitional area of the spine and pelvis that transmits over half of the body weight to the legs, is one of the key sites for maintaining biomechanical stability of the spine and the body. Tuberculosis in the lumbosacral region often involves the anterior columns and intervertebral discs and manifests as vertebral destruction and intervertebral space collapse; furthermore, paravertebral abscesses are usually observed on spinal computed tomography (CT) scans or magnetic resonance imaging (MRI), along with spinal instability, low back pain, alignment disorders, neurological deficiencies, and even death 3 . As a persistent barrier to ending the tuberculosis epidemic, the need to find an effective response to tuberculosis is increasing 4 . In general, treatment with consistent antituberculosis chemotherapy is indeed the most important strategy, which likely leads to spontaneous healing in some tubercular cases 5 . However, for those with failed conservative antituberculosis treatment or with other complications, surgical treatment is still required, especially for spinal tuberculosis. More importantly, surgery for spinal tuberculosis aims to correct segmental alignment for spinal stability, eliminate pain and deformities, and improve neurological deficits.
According to current research, the choice of surgical approach for lumbosacral spinal tuberculosis remains controversial due to the complexity of tuberculosis, complicated anatomy and special biomechanical stability 6 . Many surgeons have proposed various surgical techniques to improve the clinical outcomes via either anterior, combined anterior/posterior, or posterior approaches, most of which have been suggested are useful and efficient surgical strategies 7 . The anterior approaches can allow surgeons to directly remove tuberculosis lesions and to facilitate the reconstruction of the vertebrae, as most spinal tuberculosis involves the anterior column 8 . However, there are some deficiencies for anterior approaches. There are abundant large blood vessels and nerves distributed with anatomical variations in the anterior of the lumbosacral region 9 . According to previous reports, vascular‐related complications are more common 6 , 8 . In addition, the anterior approach is insufficient to correct lumbosacral kyphosis, and the corrected kyphosis deformity is easily lost during follow‐up8. The combination of anterior and posterior approaches could result in the debridement of tuberculosis lesions directly and simultaneously solve the problem of loss of correction. Along with the convenience, there is increased intraoperative risk, with a longer operation time, substantial intraoperative trauma, and concomitant longer hospital stay 10 . The posterior approach to address lumbosacral tuberculosis has been reported by a number of studies since the application of posterior instrumentation 8 , 11 , 12 , 13 . By removing the spinous process, lamina, facet joints, and posterior ligaments, tuberculosis lesions can be effectively exposed and removed. In the posterior approach, the goals of correction of kyphosis, spinal reconstruction, and fusion can be effectively achieved by a pedicle screw‐and‐rod system and bone graft.
Although there are many effective surgical options, some existing problems remain as obstacles to the surgical treatment of lumbosacral tuberculosis. First, the intraoperative trauma must be minimized. As a chronic consumptive disease, tuberculosis patients suffer from the dangers of malnutrition and undernourishment 14 . It is a challenge to minimize the intraoperative trauma of tuberculosis surgery while effectively achieving the aims of the surgical treatment. For patients with poor general condition, some surgeons are trying to address the disease using two‐stage surgery or computed tomography‐guided percutaneous puncture preoperation and postural drainage with debridement 15 . All these methods can reduce the intraoperative trauma caused by debridement. However, resection of the posterior appurtenant structures is inevitable. Second, the degeneration of intervertebral discs of adjacent segments will be accelerated and may result in the loss of correction. The fixed motor unit loses mobility and does not share the pressure from the upper body; thus, the adjacent segments must compensate 16 . This will result in imbalance in the lumbosacral vertebra in the sagittal alignment, altering the lumbosacral stability. The posterior ligamentous complex includes interspinous and supraspinous ligamentum flavum and capsules of facet joints, together with other posterior appurtenant structures, which play important roles in maintaining the biomechanical stability of the spine. Sustaining such structures will benefit the adjacent segments over the long term. However, the choice of surgical approach for lumbosacral spinal tuberculosis remains controversial.
Herein, we present a group of lumbosacral spinal tuberculosis patients with localized lesions in the short L5/S1 segment. An individually tailored, simple one‐stage posterior approach was developed to modify the surgical procedure, during which a unilateral limited laminectomy is performed to provide a surgical window for debridement. Compared to the traditional posterior solution, which removes the whole vertebral plate and bilateral facet joints, our approach tended to retain more stable units of the posterior column rather than damage large structures of the posterior vertebral attachments. In this study, 26 patients with spinal tuberculosis localized at the L5/S1 segment underwent one‐stage posterior unilateral limited laminectomy, debridement, internal fixation, and bone graft fusion.
This retrospective study aims to: (i) introduce the benefits of a modified procedure to address spinal tuberculosis limited to the lumbosacral region; (ii) test the feasibility of one‐stage posterior unilateral limited laminectomy for the treatment of short‐segment lumbosacral spinal tuberculosis; and (iii) evaluate the clinical efficiency and safety of this modified surgical procedure.
Methods
This study project was approved by the Ethics Review Committee of the Xiangya Hospital.
Inclusion and Exclusion Criteria
Following the PICOS principle, the inclusion criteria are as follows:
Patients diagnosed with spinal tuberculosis identified by histology or bacteriological culture, with tubercular lesions located in the lumbosacral functional unit (L5/S1);
Patients underwent surgical procedures due to: (i) progressive neurological deficits; (ii) excruciating low back pain or local spinal instability/deformity caused by the development of bony destruction; or (iii) failed conservative antituberculosis treatment no less than 3 months previous to this study;
Patients underwent one‐stage posterior unilateral limited laminectomy as a surgical treatment for debridement, bone grafting, and fixation;
Complete medical records available related to the outcomes of the spinal tuberculosis;
A retrospective cohort study.
The exclusion criteria are defined as follows:
Patients complicated with extensive anterior sacral abscesses;
Gravitation abscesses.
General Clinical Data
A total of 26 patients (17 males, nine females; 56 ± 7.4 years, Table 1) were included in this retrospective study. All patients were identified as histology‐positive or bacteriological culture‐positive. All patients had L5/S1 lumbosacral tuberculosis with varying degrees of damage to the vertebral body and local paravertebral abscesses (January 2010–December 2016). All patients were treated by one‐stage posterior debridement with bone graft fusion and fixation. A total of nine patients also had pulmonary tuberculosis. Eleven patients had low fever, emaciation, sweating, poor appetite, and other symptoms of tuberculosis toxicity. All patients suffered from persistent low back pain when in a forced passive position in bed. Eleven patients presented with various severities of mobility disabilities of their lower extremities, among which two patients also had cauda equina syndrome with an American Spinal Injury Association (ASIA) score of grade A (Table 2). All patients received laboratory examinations (blood routine [BR], erythrocyte sedimentation rate [ESR], C‐reactive protein [CRP]) and radiological diagnoses (X‐ray, CT scan, and MR imaging) to differentiate spinal tuberculosis from other diseases.
TABLE 1.
Demographics, operative information, and inflammatory variables (mean ± SD, **P < 0.01)
| Case No. | TT | Operation Time (min) | hemorrhage Volume (mL) | Follow‐up (ys) | CRP (mg/L) | ESR (mm/h) | ||
|---|---|---|---|---|---|---|---|---|
| Pre‐ | Final | Pre‐ | Final | |||||
| 1 | Y | 125 | 450 | 0.9 | 96 | 3.1 | 64 | 13 |
| 2 | Y | 130 | 580 | 1.5 | 87 | 5.4 | 59 | 15 |
| 3 | Y | 130 | 410 | 0.9 | 47 | 2.3 | 32 | 11 |
| 4 | N | 90 | 430 | 0.6 | 79 | 4.5 | 56 | 10 |
| 5 | N | 120 | 630 | 1.5 | 65 | 2.0 | 51 | 9 |
| 6 | Y | 110 | 550 | 0.9 | 95 | 3.6 | 61 | 13 |
| 7 | N | 140 | 600 | 1.5 | 70 | 4.8 | 49 | 12 |
| 8 | N | 100 | 490 | 1.2 | 60 | 2.0 | 53 | 12 |
| 9 | N | 135 | 530 | 1.6 | 56 | 3.2 | 48 | 14 |
| 10 | N | 110 | 490 | 1 | 63 | 1.7 | 50 | 10 |
| 11 | N | 140 | 450 | 2 | 77 | 2.3 | 62 | 11 |
| 12 | Y | 130 | 600 | 1.5 | 88 | 2.4 | 54 | 12 |
| 13 | Y | 95 | 410 | 2 | 83 | 3.3 | 54 | 14 |
| 14 | N | 100 | 430 | 1.6 | 66 | 2.6 | 49 | 11 |
| 15 | N | 95 | 500 | 2 | 91 | 2.4 | 67 | 10 |
| 16 | Y | 136 | 530 | 1.8 | 79 | 1.0 | 53 | 13 |
| 17 | Y | 130 | 600 | 1 | 87 | 3.5 | 60 | 10 |
| 18 | N | 109 | 420 | 1.5 | 86 | 2.9 | 51 | 12 |
| 19 | N | 90 | 410 | 1.4 | 78 | 4.0 | 49 | 9 |
| 20 | N | 140 | 630 | 0.9 | 63 | 2.9 | 45 | 14 |
| 21 | Y | 130 | 500 | 1.5 | 87 | 3.5 | 59 | 13 |
| 22 | N | 100 | 440 | 0.9 | 65 | 3.0 | 45 | 15 |
| 23 | N | 135 | 630 | 0.6 | 65 | 3.4 | 39 | 12 |
| 24 | Y | 130 | 600 | 1 | 71 | 2.1 | 57 | 8 |
| 25 | N | 90 | 420 | 1.2 | 87 | 2.6 | 51 | 13 |
| 26 | Y | 130 | 610 | 1.3 | 81 | 2.7 | 49 | 11 |
| X ± s | ‐ | 118.1 ± 17.5 | 513.0 ± 79.6 | 1.3 ± 0.42 | 75.8 ± 12.7 | 3.0 ± 1.0** | 52.6 ± 7.5 | 11.8 ± 1.8** |
TABLE 2.
Clinical efficiency, radiography, and neurological comparison between pre‐ and post‐operation (mean ± SD, *P < 0.05; **P < 0.01)
| Characteristic | Pre‐ operation | 3 months post‐ operation | Final follow‐up | |
|---|---|---|---|---|
| VAS | 7.5 ± 1.6 | 3 ± 0.7* | 1.2 ± 0.4** | |
| ODI | 79.9 ± 10.6 | 34.1 ± 8.9** | 20.5 ± 5.7** | |
| LA | 17.6° ± 2.1° | 29.3° ± 7.4°* | 27.1° ± 5.5°* | |
| ASIS Scale | A | 2 | 0 | 0 |
| B | 1 | 1 | 0 | |
| C | 3 | 2 | 2 | |
| D | 13 | 4 | 3 | |
| E | 7 | 19 | 21 |
LA, lumbosacral angle.
Clinical Imaging
X‐ray, CT scan, and MRI examinations were performed for all patients. All patients had ostial and/or discogenic erosions at the L5/S1 segment. The diseased lumbosacral spine was sometimes accompanied by local cold abscesses, but no extensive anterior sacral abscesses were found.
Preoperative Preparation
All patients were required to lie on the bed for quiet rest. A high‐caloric and protein‐rich diet was encouraged to improve their nutritional status. Anemia and hypoalbuminemia were corrected preoperatively. The antituberculotic chemotherapy procedure was as follows: all patients received standard H/R/E/Z combined chemotherapy for 2–4 weeks (H, isoniazid: 300 mg/day, R, rifampicin: 450 mg/day, E, ethambutol: 750 mg/day and Z, pyrazinamide: 750 mg/day). Previous studies indicated a consensus that it would be reliable for significantly reducing the ESR level to no more than 40 mm/h, and the clinical symptoms were relieved 7 .
Surgical Strategy
Anesthesia and Position
The patients who underwent one‐stage posterior unilateral limited laminectomy were placed in a prone position after the administration of general anesthesia and tracheal intubation.
Approach, Exposure, Debridement, and Fixation
A midline lumbar spinal incision was made to expose the vertebral plate. Pedicle screws were inserted into the vertebra according to the preoperative plan. The Legacy Reconstruction System and Vertex Reconstruction System were used, respectively (Sofamor Danek, Medtronic, Winter Park, Florida, USA). A pre‐bent short titanium rod was temporarily installed to stabilize the diseased segment on one side. A unilateral limited laminectomy under protection of the zygapophyseal joint was performed to expose the vertebral canal on the other side. The dura and nerve roots were cautiously exposed and protected under direct vision (Fig. 1A). Various sizes of curettes were used to remove the necrotic tissue and inflammatory granuloma, as well as cold abscesses in the lesion epicenter via the intervertebral space, until the healthy bone interface was reached with blood oozing out (Figs 1B,2E). After tuberculosis focus elimination, the dural sac was carefully examined to make sure there was no damage. Then, the lesion was irrigated by a syringe and silicone tube with hydrogen peroxide and reduplicative physiological saline for intensive clearance (Figs 1C,3E). After cleaning the wound, the bone graft area was trimmed, and a suitable bulk cortical–cancellous bone allograft was inserted into the cavity and to support the space between the L5‐S1 vertebral bodies. In addition, the cartilage of the facet joint was removed and the vertebral plate was roughed up; then, the deficient laminectomy was coated by the tabular allograft coverage. Streptomycin (1.0 g) and isoniazid (0.2 g) were placed into the wound locally (Figs 1D,4E). Then, the titanium rod was installed on the laminectomy side and both sides were locked; following, a transverse connector was installed to fix the grafted allograft bone at the lamina defect and enhance the stability of the internal fixation system. A catheter was inserted into the paravertebral tissue to drain the remaining fluid and the wound was finally closed.
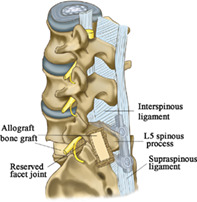
Fig 1.
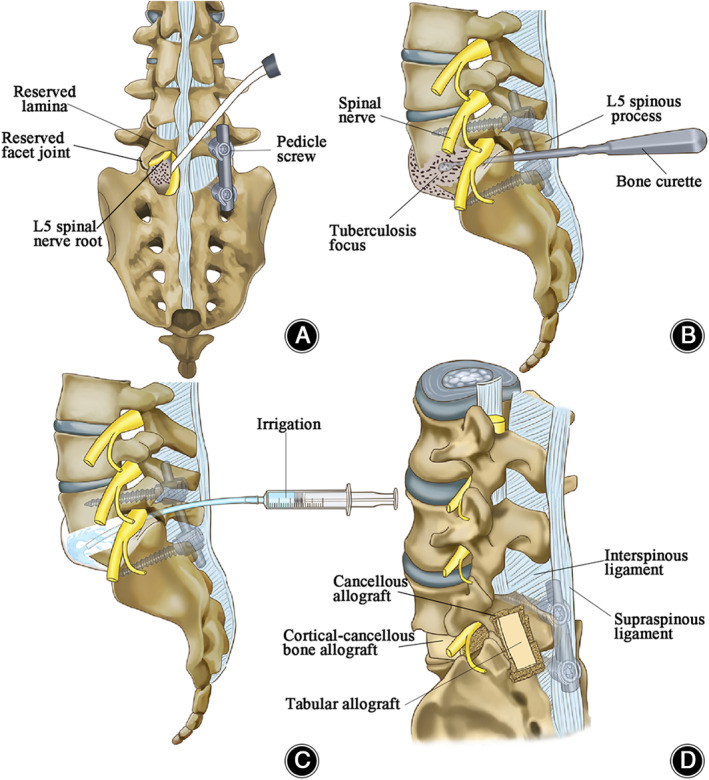
Schematic diagram indicating the dominating surgical process. (A) The access to the tuberculosis focus. After pedicle screws and titanium rod were inserted, limited unilateral vertebral plate was removed to establish an operational pathway that facilitated the access to spinal tuberculosis lesion and under direct vision protected the dura and nerve roots from injury. The zygapophyseal joint and part of the lamina were reserved. (B) The elimination of tuberculosis focus. Once the approach to the tuberculosis focus was established via the intervertebral space, the abnormal intervertebral disc and sclerosed dead bone, as well as necrotic tissue and inflammatory granuloma, were removed by bone curette during procedure of debridement, reaching healthy bone interface with blood oozing out. (C) Lesion irrigation. After examination of the dural sac, we confirmed there was no damage. The tubercular cavity is irrigated in sequence of physiological, saline‐hydrogen peroxide and reduplicative physiological saline for intensive clearance of the wound. (D) Posterolateral view of allogenic bone transplantation. Before bone transplantation, the reserved lamina is decorticated, trimmed bulk cortical–cancellous bone allograft was filled into the cavity and support the space between the L5‐S1 vertebral bodies. Also, the deficient laminectomy was coated by the tabular allograft coverage. After the procedure, the spinous process, the interspinous ligament, and the supraspinous ligament are preserved.
Postoperative Management
The drainage tube was removed when the drainage volume was less than 50 mL/24 h. All patients were closely inspected for mobility and sensation in the lower limbs. They were encouraged to perform straight leg raising exercises on the bed. On the basis of the recommendation from the World Health Organization, Standard H/R/E/Z combined antituberculosis chemotherapy was administered for 2 months followed by isoniazid and rifampicin for more than 7 months postoperatively. According to the clinical features, hepatic function, ESR, CRP response, and radiographic manifestation during the follow‐up, the antituberculosis regimen was appropriately adjusted and extended. A lumbar external fixation brace was required for at least 8 to 12 weeks after surgery without weight‐bearing daily activities. X‐ray, CT, and MRI were reviewed postoperatively at 6‐month intervals, and patients underwent a CT scan no more than twice a year. A successful bone fusion is firmly believed to show the formation of new trabeculae between the grafted block and vertebral body. BR, hepatic and renal function, CRP levels, and ESR were monitored regularly during the course of antituberculous chemotherapy therapy.
Follow‐up
All patients were followed up postoperatively at the scheduled times. The follow‐up visits were usually at every three months in the first year and every six months in the second year post‐operation. BR, ESR, and CRP were detected again to determine the activity level of tubercle bacillus. In addition, the Oswestry Disability Index (ODI), American Spinal Injury Association Impairment (ASIA) Scale, and visual analog scale (VAS) scores were applied to assess the severity of the clinical symptoms.
Oswestry Disability Index (ODI)
The ODI is a questionnaire designed to evaluate spinal disorders in routine clinical practice with condition‐specific outcomes. There are 10 sections included in the questionnaire: pain intensity, personal care, lifting, walking, sitting, standing, sleeping, sex life, social life, and traveling. Each section is scored from 0 to 5, and the percentage score is calculated based on the number of sections answered.
American Spinal Injury Association Impairment (ASIA) Scale
The ASIA Scale is widely used to define the impairment situation of neurological functions in patients with spinal cord injury. It reflects the sensory and motor functions below the injured segment, especially the sensory and motor functions in the sacral region.
Visual Analog Scale (VAS) Scores
The VAS score is a widely used method to evaluate pain grade in the clinic. A score of 0 indicates a painless condition, and unbearable intense pain is defined as a score of 10.
Lumbosacral Angle
LA is the angle between a horizontal line and the S1 vertebra superior endplate and ranges from 26° to 57° in normal people. It is used as one of the parameters to evaluate the lumbar lordosis. The LA was obtained on the lateral X‐ray before operation and during follow‐up.
The evaluations of the ODI, ASIA Scale, and VAS scores were performed preoperatively, in the third month post‐operation, and at the last follow‐up.
Bone Fusion
The X‐ray and CT scans were re‐evaluated for lumbar lordosis and lumbar intervertebral fusion efficiency. A solid bony fusion was confirmed by an obvious bone trabecula between the adjacent interosseous interfaces.
Statistical Analysis
Statistical analyses were performed with SPSS 18.0 software (SPSS Chicago, IL, USA). A paired t‐test was used to compare the ESR/CRP between different periods, and one‐way ANOVA with Tukey's multiple comparisons test was used to compare the ODI, VAS score, and LA among the preoperative, postoperative, and final follow‐up timepoints. The results are presented as the mean ± SD, and a P value < 0.05 indicates a significant difference.
Results
Participant Demographics and General Intraoperative Data
In this study, the male/female ratio of the lumbosacral tuberculosis patients was 17:9. The mean age was 56 ± 7.4 years old. The mean follow‐up time was 1.3 ± 0.42 years (Table 1). The average operation time was 118.1 ± 17.5 min (range from 90 to 140 min), and the mean hemorrhage volume was 513.0 ± 79.6 mL (range from 410 to 630 ml). At the final follow‐up, the ESR and CRP in all patients had decreased to the physiological range, which was significantly lower than the preoperative levels (**P < 0.01, Table 1).
Neurologic and VAS Score Outcomes
The patients with neurological deficits were improved at the final follow‐up. Three patients with ASIA scale scores of A and B improved by 1~2 grades at the last follow‐up. Before the spinal surgery, the mean ODI was 79.9 ± 10.6 (range from 87–62), which significantly declined at 3 months postoperatively (34.1 ± 8.9, range from 26 to 46; one‐way ANOVA with Tukey's multiple comparisons test, P > 0.05 compared to preoperative) and continued to decrease to 20.5 ± 5.7 (range from 11–29; one‐way ANOVA with Tukey's multiple comparisons test, P > 0.05 compared to preoperative) at the final follow‐up (P < 0.01). In addition, the VAS score significantly improved to 3.0 ± 0.7 (range from 1 to 4.5) at 3 months postoperatively compared to 7.5 ± 1.6 preoperatively (range from 6.5 to 8.5; one‐way ANOVA with Tukey's multiple comparisons test, P > 0.05). At the end of the follow‐up period, the mean score decreased markedly to 1.2 ± 0.4 (range from 0 to 2.5) (one‐way ANOVA with Tukey's multiple comparisons test, P > 0.05 compared to preoperative) (Table 2).
Radiographic Outcomes
The mean time to achieve bony fusion after allogeneic bone grafting was 6.8 ± 1.2 months. The LA (Cobb's method) was significantly improved from 17.6° ± 2.1° preoperatively to 27.1° ± 5.5° at the final follow‐up (one‐way ANOVA with Tukey's multiple comparisons test, P < 0.05 compared to preoperatively). There was no remarkable LA reduction at 3 months postoperatively and at the final follow‐up (Table 2, one‐way ANOVA with Tukey's multiple comparisons test, P > 0.05 compared to 3 months postoperatively). The imageology results of the representative case are show in Figs 2, 3, 4.
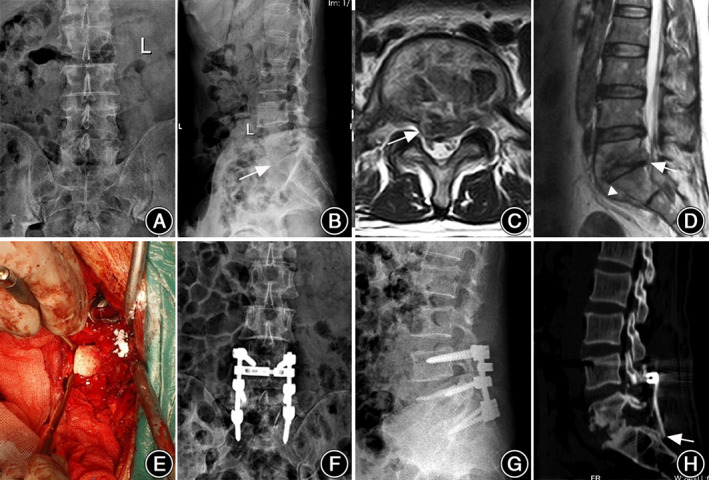
Fig 2.
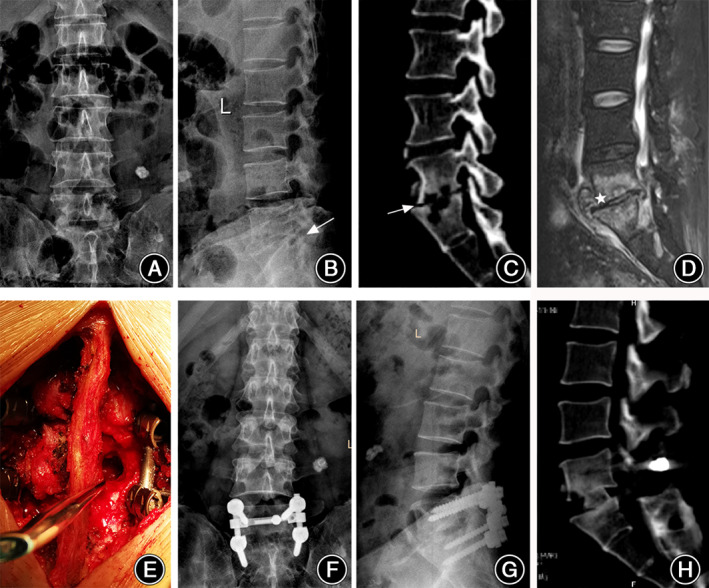
Representative case 1. A 51‐year‐old male, complaining of low back pain and sciatic pain, was finally diagnosed as L5/S1 lumbosacral tuberculosis by etiological examination in hospital. The patient underwent one‐stage modified only posterior debridement, internal fixation, and vertebral fusion. (A, B) Preoperative anteroposterior and lateral X‐ray showed the local kyphosis with a lower lumbosacral angle (arrow). (C) The sagittal CT slice indicated the loss of L5/S1 height in intervertebral space, accompanied by wormy eroded destruction of L5‐S1 vertebral bodies, around which was abnormal bony sclerosis (arrow). (D) The MRI sagittal images showed the lesion of L5/S1 disc with a few paravertebral cold abscesses and inflammatory long T2 signal involved in vertebral bodies (star). (E) Via a unilateral limited laminectomy, an intervertebral pathway was created for debridement to remove the lesions intraoperatively. (F, G) Review of the X‐ray at the 9‐month follow‐up checked the fixation stability and maintenance of lumbosacral lordosis. (H) The intervertebral bony grafting fusion was satisfactory at the 9‐month follow‐up.
Fig 3.
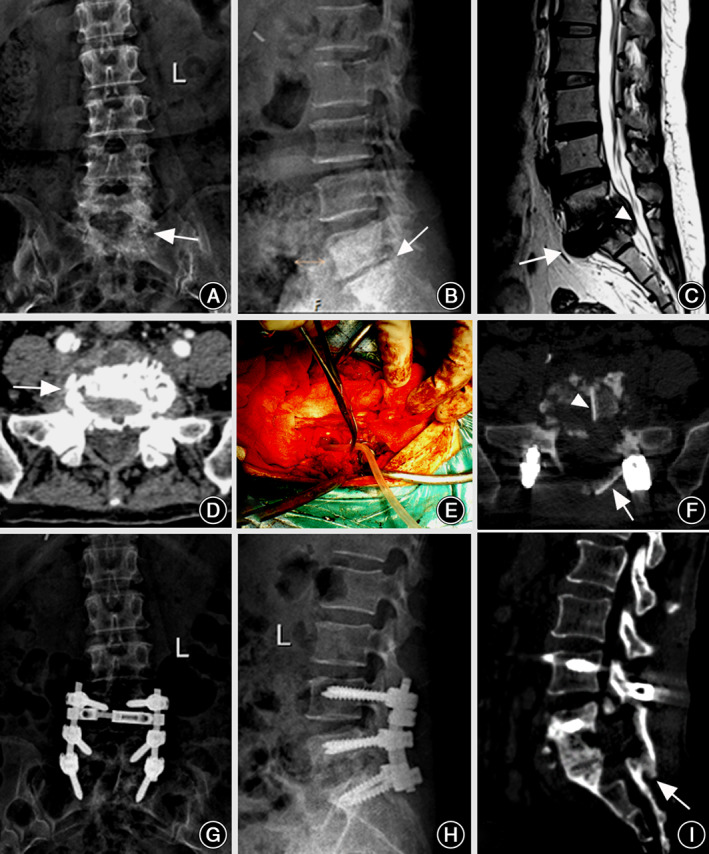
Representative case 2. A 56‐year‐old female patient with typical lumbosacral tuberculosis underwent only posterior approach for debridement, internal fixation and allogeneic bone grafting. (A) Preoperative anteroposterior X‐ray indicated the osseous sclerosis in L5 and S1 vertebral bodies (arrow). (B) Lateral X‐ray showed the collapse of L5/S1 intervertebral space, accompanied by the decrease of lumbosacral lordosis (arrow). (C) The MR sagittal imaging revealed the mild pre‐sacral cold abscess (arrow) and some necrotic disc herniates into the lumbosacral canal resulting in sciatica neuralgia (triangle). (D) The CT transverse slice showed the bony lesion on sacral sclerotic endplate (arrow). (E) A drainage tube was inserted into the wound to wash away the inflammatory mediator and puriform fluid after unilateral limited laminectomy. (F) One week later, a CT transverse slice showed the location of intervertebral bone graft (triangle) and vertebral plate bone graft (arrow). (G, H) The anteroposterior and lateral X‐rays confirmed the solidity of the internal instruments and the increase of lumbar lordosis 1 year postoperatively. (I) The intervertebral and vertebral plate bony fusions were observed in sagittal CT imaging 1 year postoperatively (arrows).
Fig 4.
Representative case 3. A 53‐year‐old male patient diagnosed with L5/S1 spinal tuberculosis and neurological deficit in the lower extremities. The patient underwent only modified one‐stage posterior debridement, internal fixation, and bony fusion. (A, B) Preoperative X‐ray showed the narrow height of L5/S1 intervertebral space, as well as the decrease of lumbosacral lordosis, and bony lesions on L5 intervertebral body and inferior endplate (arrow). (C) Transverse MRI indicated the typical inflammatory involvement of the L5/S1 intervertebral disc, the white arrow pointed out the intraspinal invasion of the cold abscess and necrotic tissue (arrow). (D) The sagittal MR panel indicated the moderate paravertebral and pre‐sacral cold abscess (triangle), as well as intraspinal invasion (arrow). (E) This panel performed the intraoperative procedure of allogeneic bone grafting after debridement to repair the deficient intervertebral structure. (F, G) The anteroposterior and lateral X‐rays confirmed the stability of internal instruments, and the lumbosacral lordosis was regained and retained at the 9‐month follow‐up. (H) The CT sagittal slice showed the solid intervertebral and vertebral plate bony grafting fusion at the 9‐month follow‐up.
Complications
Two patients experienced hypostatic pneumonia and were cured with susceptible antibiotics and symptomatic supportive treatment. There were no large blood vessel or nerve injuries, or other complications related to screw instrumentation, during the operative process. All patients experienced primary healing in the wound and no recurrence of spinal tuberculosis or sinus formation at the different follow‐up times.
Discussion
The spine is a common site of extrapulmonary tuberculosis. Spinal tuberculosis is more common in the thoracic and lumbar segments of the spine than the lumbosacral region (where it only accounts for 2%–3% of cases) 17 . Many studies have formed a consensus that anterior approaches are accompanied by higher vascular‐related complications and loss of corrected lumbosacral kyphosis 8 , and the combination of anterior and posterior approaches had a longer operation time and hospital stay 10 . In recent years, posterior approaches have been paid increasing amounts of attention in the surgical treatment of spinal tuberculosis, and spinal fixation is regarded as a high‐efficiency, safe, and reliable method 12 , 13 , 18 .
Benefit of Unilateral Limited Laminectomy in Lumbosacral Tuberculosis
One‐stage posterior unilateral limited laminectomy, annular bone grafting, and fixation for use with patients with limited lumbosacral tuberculosis is a modified procedure that can treat lumbosacral vertebra tuberculosis more accurately, reduce the intraoperative trauma, and meet the spinal goals of tuberculosis therapy. According to the current studies, the posterior approach routinely excises the posterior structure of the spine to expose and debride the lesion sufficiently 19 . In our study, the reliability of performing debridement via the intervertebral space through only a unilateral limited laminectomy is demonstrated. Biomechanical studies have shown that the posterior appurtenances of the spine play an important role in the stability of the spine, and each part of the vertebral column could serve as an anchor point for posterior muscles and ligaments, sharing the stress of the internal fixation 20 . Sparing the rest of the posterior appurtenances (e.g. the hemi‐lamina, facet joints, spinous process, interspinous and supraspinous ligaments) undoubtedly contributes to more areas of bone grafting (Figs 2, 3).
Reservation of posterior appurtenances also provided some additional stability for the lumbosacral region. A previous study pointed out that the spinal stability mainly came from the pedicle screw setting in the early postoperative period; later, it was mostly provided by bony grafting fusion 11 . In the long run, preserving the posterior appurtenances could be beneficial for maintaining spinal stability through multidimensional fusions of intervertebral and posterior column bony grafting. The three‐column structural bony reconstruction firmly contributed to lumbosacral biomechanical stability. Of course, it is necessary for us to collect more datasets with longer follow‐ups and to provide more valuable clinical evidence in the future.
The Feasibility of One‐stage Posterior Unilateral Limited Laminectomy
The aim of the lumbosacral tuberculosis surgery technique was to debride the focal infection, to recover the injured neurological function, and to restore alignment to regain spinal stability 21 . The surgical fixation approach we introduced is performed on a relatively short segment, and only limited laminectomy was performed. Therefore, to achieve the surgical goals, it is necessary to strictly understand the indications. First, this surgery applies only to patients without large presacral abscesses, paravertebral abscesses, and gravitation abscesses; for patients with such abscesses, anterior debridement could be applied to the tubercular lesion under direct vision 22 , or percutaneous drainage could be a better, less invasive method for treating spinal tuberculosis 15 . The surgical field is limited by the intervertebral space, and it is difficult to excise large abscesses in the front. Posterior debridement could avoid the variations in the vascular anatomy of the spine that impact surgical planning for the lumbosacral region 9 , 23 , 24 , which is significant for patients with localized abscesses. Second, this procedure is suitable for patients without pedicle involvement. The pedicle is one of the posterior spinal elements and is sometimes involved in spinal tuberculosis. For tuberculosis lesions involving the pedicle, it will be difficult to set pedicle screws and thus provide sufficient pullout strength 16 . Third, after tuberculosis debridement, endplate integrity is guaranteed. Without the integrity of the endplate, the implanted allogeneic bone may penetrate the endplate, resulting in bone graft fusion failure. Patients with severe osteoporosis, such as elderly patients, may need other, more appropriate bone grafting methods 12 .
At present, the posterior internal fixation of lumbosacral tuberculosis is divided into three ranges of long‐, short‐, and single‐segment fixations. Long‐segment fixation always sacrifices more than two normal motor units of the spine, even extending to ilium fixation 25 , 26 . Short‐segment fixation is limited to one‐level above/below the lesion body, aiming to retain physiological function during lumbosacral spinal tuberculosis surgery, and avoids the above shortcomings 27 . Biomechanical studies have confirmed that vertebral pedicles provide more than 60% of the pullout strength and 80% of the axial pullout strength, while only 15%–20% of the pullout strength was provided by vertebral cancellous bone 28 , 29 . A previous study reported that implanting single‐segment screws into a diseased body was an effective fixation for lumbosacral tuberculosis, and there was no significant Cobb angle loss in the follow‐up16. In the past, Ilium screws were commonly used for the purpose of long and stable fixation. For cases that concentrated on the single motor unit without large abscess, the preservation of lumbosacral junction will benefit a lot. The lumbosacral junction serves as a link between the spine and the pelvis, which is a particular anatomic region and stress‐concentrating site for bridging the spine and pelvis and plays an important role in maintaining the biomechanical balance of the overall sagittal spine–pelvis alignment 30 . However, in this study, all cases were caudally fixed to the S1 vertebrae at its base without any loss of spinal stability by screw fixation. Based on the feasibility, we believe that it makes sense to shorten the spino–pelvic fixation and decrease the incidence of other complications (e.g. blood loss) during the operation. As long as the pedicle pathway is reachable, pedicle screw implantation in the diseased sacral body fully satisfies the requirements of internal fixation biomechanics. In this study, the posterior surgical procedure was modified. The LA was effectively improved, and there was no significant change in the LA between the postoperative time point and the last follow‐up.
Considerable Clinical Efficiency and Safety of Unilateral Limited Laminectomy for Debridement
In our series, all patients achieved satisfactory results in neurological rehabilitation, functional reconstruction, and recovery from spinal tuberculosis following treatment with unilateral limited laminectomy for debridement, internal fixation, and bone graft fusion combined with antituberculotic chemotherapy. Thirteen patients with functional nerve impairment of ASIA D recovered to ASIA E; two ASIA A patients recovered to ASIA C at the final follow‐up. Furthermore, the ODI score also had significant improvements at the final follow‐up. Unilateral limited laminectomy for debridement could effectively relieve the nerve compression of lesions and create conditions for the recovery of nerve function. Although the procedure introduced by this study has limited field of vision for debridement, physiological saline and hydrogen peroxide were flushed into the wound intraoperatively to eliminate the lesions. By the debridement of tuberculosis lesions and the reconstruction of lumbosacral stability, the patient's pain could be effectively and rapidly relieved. The VAS score had significant improvements at the final follow‐up. Due to the minimally invasive removal of the vertebral plate and the limitation of the fixed segment, the operation time was shorter than that from previous reports employing multi‐segmental fusion 7 , 31 . Thus, unilateral limited laminectomy for debridement could completely debride the tuberculotic lesions in cases of limited lumbosacral tuberculosis.
Limitations of the Study
Finally, some limitations and technical notes should be considered. This study is only a retrospective study, and more clinical case data and long‐term follow‐up assessments should be carried out in the future. Extensive anterior sacral abscesses and gravitation abscesses would be unsuitable for this surgical approach because of the potential for recurrence. In addition, unilateral limited vertebral plate removal provides only a narrow field of view during surgery. Thus, extensive surgical procedures of the anterior disc and vertebral body are not feasible. Instead, the surgeon needs to patiently scrape the tuberculosis lesion, perform repetitive washing, and effectively perform bone graft fusion.
Conclusions
One‐stage posterior unilateral limited laminectomy for debridement, internal fixation, and bone graft fusion could serve as an effective and safe procedure to treat short‐segment lumbosacral tuberculosis without extensive anterior sacral abscesses and gravitation abscesses.
Authorship declaration
All authors listed meet the authorship criteria according to the latest guidelines of the International Committee of Medical Journal Editors and all authors are in agreement with the manuscript.
Acknowledgments
This study was funded by National Natural Science Foundation of China (grant number 81301542) Natural Science Foundation of Hunan Province China (grant number 2019JJ50959, 2020JJ5930) and Management and Research Fund of Xiangya Hospital, Central South University (grant number 2016GL14), covering the costs of the study design, data interpretation, and revising the manuscript.
Disclosure: No conflict of interest.
Contributor Information
Yong Cao, Email: caoyong1912@163.com.
Tianding Wu, Email: tiandingwu@hotmail.com.
References
- 1. Sulis G, Adam P, Nafade V, et al. Antibiotic prescription practices in primary care in low‐ and middle‐income countries: a systematic review and meta‐analysis. PLoS Med, 2020, 17: e1003139. 10.1371/journal.pmed.1003139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Pun WK, Chow SP, Luk KD, Cheng CL, Hsu LC, Leong JC. Tuberculosis of the lumbosacral junction. Long‐term follow‐up of 26 cases. J Bone Joint Surg Br, 1990, 72: 675–678. [DOI] [PubMed] [Google Scholar]
- 3. Abou‐Raya S, Abou‐Raya A. Spinal tuberculosis: overlooked? J Intern Med, 2006, 260: 160–163. [DOI] [PubMed] [Google Scholar]
- 4. The Lancet . End the tuberculosis emergency: a promise is not enough. Lancet, 2019, 394: 1482. [DOI] [PubMed] [Google Scholar]
- 5. Hemanth Kumar AK, Kumar A, Kannan T, et al. Pharmacokinetics of second‐line antituberculosis drugs in children with multidrug‐resistant tuberculosis in India. Antimicrob Agents Chemother, 2018, 62: e02410–e02417. 10.1128/AAC.02410-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Oguz E, Sehirlioglu A, Altinmakas M, et al. A new classification and guide for surgical treatment of spinal tuberculosis. Int Orthop, 2008, 32: 127–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Liu JM, Zhou Y, Peng AF, et al. One‐stage posterior surgical management of lumbosacral spinal tuberculosis with nonstructural autograft. Clin Neurol Neurosurg, 2017, 153: 67–72. [DOI] [PubMed] [Google Scholar]
- 8. Zheng B, Hao D, Guo H, He B. Anterior versus posterior surgical approach for lumbosacral tuberculosis. J Int Med Res, 2018, 46: 2569–2577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Tezuka F, Sakai T, Nishisho T, et al. Variations in arterial supply to the lower lumbar spine. Eur Spine J, 2016, 25: 4181–4187. [DOI] [PubMed] [Google Scholar]
- 10. Sun D, Zhang ZH, Mei G, et al. Comparison of anterior only and combined anterior and posterior approach in treating lumbosacral tuberculosis. Sci Rep, 2019, 9: 18475. 10.1038/s41598-019-53800-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Patil SS, Rawall S, Nagad P, Shial B, Pawar U, Nene AM. Outcome of single level instrumented posterior lumbar interbody fusion using corticocancellous laminectomy bone chips. Indian J Orthop, 2011, 45: 500–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wang YX, Zhang HQ, Liao W, et al. One‐stage posterior focus debridement, interbody graft using titanium mesh cages, posterior instrumentation and fusion in the surgical treatment of lumbo‐sacral spinal tuberculosis in the aged. Int Orthop, 2016, 40: 1117–1124. [DOI] [PubMed] [Google Scholar]
- 13. Tang MX, Zhang HQ, Wang YX, Guo CF, Liu JY. Treatment of spinal tuberculosis by debridement, interbody fusion and internal fixation via posterior approach only. Orthop Surg, 2016, 8: 89–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Shah K, Kothari M, Nene A. Role of frailty scoring in the assessment of perioperative mortality in surgical management of tuberculous spondylodiscitis in the elderly. Global Spine J, 2018, 8: 698–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Yin XH, Zhang HQ, Hu XK, Li JS, Chen Y, Zeng KF. Treatment of pediatric spinal tuberculosis abscess with percutaneous drainage and low‐dose local antituberculous therapy: a preliminary report. Childs Nerv Syst, 2015, 31: 1149–1155. [DOI] [PubMed] [Google Scholar]
- 16. Jin W, Wang Z. Clinical evaluation of the stability of single‐segment short pedicle screw fixation for the reconstruction of lumbar and sacral tuberculosis lesions. Arch Orthop Trauma Surg, 2012, 132: 1429–1435. [DOI] [PubMed] [Google Scholar]
- 17. Tuli SM. Severe kyphotic deformity in tuberculosis of the spine. Int Orthop, 1995, 19: 327–331. [DOI] [PubMed] [Google Scholar]
- 18. Zeng H, Zhang P, Shen X, et al. One‐stage posterior‐only approach in surgical treatment of single‐segment thoracic spinal tuberculosis with neurological deficits in adults: a retrospective study of 34 cases. BMC Musculoskelet Disord, 2015, 16: 186. 10.1186/s12891-015-0640-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ukunda UNF, Lukhele MM. The posterior‐only surgical approach in the treatment of tuberculosis of the spine: outcomes using cortical bone allografts. Bone Joint J, 2018, 100‐B: 1208–1213. [DOI] [PubMed] [Google Scholar]
- 20. Li J, Huang S, Tang Y, Wang X, Pan T. Biomechanical analysis of the posterior bony column of the lumbar spine. J Orthop Surg Res, 2017, 12: 132. 10.1186/s13018-017-0631-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Li J, Li XL, Zhou XG, Zhou J, Dong J. Surgical treatment for spinal tuberculosis with bilateral paraspinal abscess or bilateral psoas abscess: one‐stage surgery. J Spinal Disord Tech, 2014, 27: E309–E314. [DOI] [PubMed] [Google Scholar]
- 22. Jin W, Wang Q, Wang Z, Geng G. Complete debridement for treatment of thoracolumbar spinal tuberculosis: a clinical curative effect observation. Spine J, 2014, 14: 964–970. [DOI] [PubMed] [Google Scholar]
- 23. Weiner BK, Walker M, Fraser RD. Vascular anatomy anterior to lumbosacral transitional vertebrae and implications for anterior lumbar interbody fusion. Spine J, 2001, 1: 442–444. [DOI] [PubMed] [Google Scholar]
- 24. Unruh KP, Camp CL, Zietlow SP, Huddleston PM. Anatomical variations of the iliolumbar vein with application to the anterior retroperitoneal approach to the lumbar spine: a cadaver study. Clin Anat, 2008, 21: 666–673. [DOI] [PubMed] [Google Scholar]
- 25. Shi JD, Wang ZL, Geng GQ, Niu NK. Intervertebral focal surgery for the treatment of non‐contiguous multifocal spinal tuberculosis. Int Orthop, 2012, 36: 1423–1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wu P, Luo C, Pang X, Xu Z, Zeng H, Wang X. Surgical treatment of thoracic spinal tuberculosis with adjacent segments lesion via one‐stage transpedicular debridement, posterior instrumentation and combined interbody and posterior fusion, a clinical study. Arch Orthop Trauma Surg, 2013, 133: 1341–1350. [DOI] [PubMed] [Google Scholar]
- 27. Liu Z, Zhang P, Zeng H, Xu Z, Wang X. A comparative study of single‐stage transpedicular debridement, fusion, and posterior long‐segment versus short‐segment fixation for the treatment of thoracolumbar spinal tuberculosis in adults: minimum five year follow‐up outcomes. Int Orthop, 2018, 42: 1883–1890. [DOI] [PubMed] [Google Scholar]
- 28. Weinstein JN, Rydevik BL, Rauschning W. Anatomic and technical considerations of pedicle screw fixation. Clin Orthop Relat Res, 1992, 284: 34–46. [PubMed] [Google Scholar]
- 29. Seller K, Wahl D, Wild A, Krauspe R, Schneider E, Linke B. Pullout strength of anterior spinal instrumentation: a product comparison of seven screws in calf vertebral bodies. Eur Spine J, 2007, 16: 1047–1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Chang KW, Leng X, Zhao W, et al. Quality control of reconstructed sagittal balance for sagittal imbalance. Spine, 2011, 36: E186–E197. [DOI] [PubMed] [Google Scholar]
- 31. Li W, Liu J, Gong L, Zhou Y, Duan D. Posterior intervertebral space debridement, annular bone grafting and instrumentation for treatment of lumbosacral tuberculosis. BMC Surg, 2017, 17: 124. 10.1186/s12893-017-0310-2. [DOI] [PMC free article] [PubMed] [Google Scholar]


