Abstract
Objective
To evaluate the clinical outcomes of oblique lumbar interbody fusion (OLIF) in conjunction with unilateral pedicle screw fixation (UPSF) via the Wiltse approach in treating degenerative lumbar scoliosis (DLS).
Methods
The article is a retrospective analysis. Twelve patients with DLS who underwent combined OLIF and UPSF between July 2017 and December 2018 were included. The study included 2 male and 10 female patients, with a mean age at the time of the operation of 67.2 ± 9.1 years. The surgical characteristics and complications were evaluated. The clinical and radiological data such as the correction of deformity, coronal and sagittal profile were analyzed.
Results
The mean follow‐up time of the study was 26.8 ± 1.8 months. At the final follow‐up, all patients who underwent combined OLIF and UPSF achieved statistically significant improvements in coronal Cobb angle (from 19.6° ± 4.8° to 6.9° ± 3.8°, P < 0.01), distance between the C7 plumb line and central sacral vertebral line (from 2.5 ± 1.7 cm to 0.9 ± 0.6 cm, P < 0.01), sagittal vertebral axis (from 4.3 ± 4.3 cm to 1.5 ± 1.0 cm, P = 0.03), lumbar lordosis (from 29.4° ± 8.6° to 40.8° ± 5.8°, P < 0.01), pelvic tilt (from 27.6° ± 10.8° to 18.3° ± 7.0°, P < 0.01), pelvic incidence‐lumbar lordosis mismatch (from 23.3° ± 10.5° to 11.9° ± 8.4°, P < 0.01), and cross‐sectional area of the dural sac (from 87.33 ± 39.41 mm2 to 124.70 ± 39.26 mm2, P < 0.01). The visual analogue score for back and leg pain and Oswestry Disability Index of all patients significantly improved postoperatively (P < 0.01). One case of lumbar plexus injury was found after surgery. During the follow‐up period, one patient had cage subsidence. A fusion rate of 100% and good positioning of the pedicle screws were achieved in all patients at the final follow‐up.
Conclusion
OLIF in conjunction with UPSF is a safe and effective minimally invasive procedure for correcting both coronal and sagittal deformities, as it results in an improved quality of life in patients with DLS.
Keywords: Degenerative lumbar scoliosis, Oblique lumbar interbody fusion, Unilateral pedicle screw fixation
OLIF in conjunction with UPSF seems to be a valuable surgical tool for the minimally invasive correction of coronal and sagittal plane deformities in patients with moderate degenerative lumbar scoliosis. It is a minimally invasive procedure that yields good radiographic and clinical results without any major complications.
Introduction
Degenerative lumbar scoliosis (DLS) mainly causes back pain, neurological symptoms of the lower extremities and radicular pain, which cause serious problems in terms of function and quality of life in patients. After conservative treatment, the symptoms of some patients are not relieved or recur and affect their quality of life, so they usually require surgical treatment. Posterior decompression, fusion fixation and correction are the classic methods of treating DLS. Although the resulting correction is good, the posterior approach involves extensive muscle stripping and invasive direct decompression, which are not only considered severe trauma but also considered interferences to the spinal cord and nerve structure; therefore, it is easy for complications such as nerve injury, extradural hematoma, fusion fixation failure, refractory low back pain, and adjacent segment disease to occur 1 , 2 . Degenerative lumbar scoliosis often occurs in adults over 50 years of age 3 , and most of these individuals have additional medical complications. The tolerance of these individuals to major surgery is relatively poor, and the postoperative rehabilitation period is relatively long.
In the past decade, minimally invasive spinal fusion techniques such as direct lateral lumbar interbody fusion (DLIF) and extreme lateral lumbar interbody fusion (XLIF) have been widely used in the treatment of DLS, and they have yielded satisfactory results regarding spinal canal decompression and correction and have the advantages of less trauma and less blood loss compared with traditional open approaches. However, in the lateral lumbar interbody fusion (LLIF) approach, the psoas needs to be split to expose the disc, which easily damages the lumbar plexus nerve running through it, resulting in serious complications, such as pain, numbness, paresthesias, or weakness 4 . Oblique lumbar interbody fusion (OLIF) is a minimally invasive spinal fusion technique that was reported by Silvestre et al. 5 in 2012. Its approach is through the space between the psoas and abdominal major vessels, which can overcome the limitation of the lateral approach. This technique has the advantage of relatively low complications of nerve injury in the treatment of lumbar degenerative diseases.
In recent years, most of the literature has reported that OLIF combined with bilateral pedicle screw fixation (BPSF) has yielded good results in the treatment of lumbar spinal stenosis, degenerated spondylolisthesis and DLS. However, BPSF increases damage to the posterior soft tissue structure of the lumbar spine and the economic burden on patients. In 2008, Yücesoy et al. 6 reported that multi‐level unilateral continuous pedicle screw fixation can provide enough biomechanical stability. Zhang et al. 7 conducted a prospective randomized study of unilateral versus bilateral instrumented TLIF in patients with two‐level degenerative lumbar disorders and concluded that two‐level unilateral instrumented TLIF is an effective and safe method. To the best of our knowledge, there have been no reports on the treatment of lumbar degenerative scoliosis with a combination of OLIF and unilateral pedicle screw fixation (UPSF). The purpose of the study was to: (i) explore the feasibility of (OLIF) in conjunction with UPSF in the treatment of DLS; and (ii) evaluate the clinical and radiographic efficacy of indirect decompression and correction using OLIF with UPSF via the Wiltse approach in treating DLS.
Materials and Methods
General Data
This study was approved by the ethical committee of General Hospital of Ningxia Medical University, and written informed consent was obtained from all participants. As agreed with the ethical committee, all methods were performed in accordance with the relevant guidelines and regulations. Twelve patients with DLS who were admitted to the Department of Orthopaedics at the General Hospital of Ningxia Medical University between July 2017 and December 2018 were retrospectively included in the study. All surgeries were performed by a single surgeon (Ge).
All patients met the following inclusion criteria: (i) refractory back pain and radiating pain to the lower extremities that could not be effectively treated conservatively; (ii) a diagnosis of DLS (coronal Cobb angle of >10° or sagittal vertebral axis of >5 cm, Silva and Lenke 8 types 2–4, and computed tomography (CT) and magnetic resonance imaging (MRI) scans showed facet joint hyperplasia but not fusion); (iii) treatment of DLS with OLIF and UPSF via the Wiltse approach in one stage; and (iv) available preoperative and postoperative 36‐inch films of the scoliotic spine.
The bone mineral density (BMD) of the lumbar spine was assessed by dual‐energy X‐ray absorptiometry (DEXA). Standing anteroposterior and lateral 36‐inch films, and lumbar spine MRI scans were obtained in 12 patients preoperatively and at the final follow‐up. CT scans obtained during the follow‐up period were reviewed to assess the bridging bone to determine whether bony fusion had occurred.
Surgical Method
One patient in our case series underwent L2–L5 OLIF with L2–L5 UPSF via the Wiltse approach for the treatment of DLS. Step 1: the patient was placed under general anesthesia with endotracheal intubation, in the lateral decubitus position, an OlympicVac‐Pac® mattress with the ipsilateral hipflexed to allow relaxation of the ipsilateral psoas muscle, and the ipsilateral arm placed on an arm rest. Step 2: under C‐arm fluoroscopic guidance, the surgeon marked the anterior border of the L2–L3 and L4–L5 intervertebral spaces and made an oblique incision of 8 to 10 cm from the anterior border of the L2–L3 intervertebral space to approximately 4 cm in front of the anterior border of the L4–L5 intervertebral space (Fig. 1A). The retroperitoneal OLIF corridor was exposed. The OLIF technique has been generally described elsewhere 4 . First, a guide pin was introduced into the L4–L5 intervertebral space through this corridor under fluoroscopic guidance. Under direct vision, the psoas was retracted posteriorly, the L4–L5 intervertebral disc was exposed, a square window was made in the annulus fibrosis of the disc, and the intervertebral space was treated with nucleus pulposus forceps, reamers and curettes after the opposite annulus fibrosis was penetrated. Then, the cartilage endplates were resected to expose the bony endplates. An appropriately sized polyethere‐therketone (PEEK) interbody cage (Medtronic Sofamor Danek USA) filled with allogeneic bone graft was selected for insertion into the intervertebral space. Sufficiently wide cages were selected to prevent subsidence. If the restoration of sagittal lumbar lordosis was required, angled cages were selected. During cage implantation, it should be noted that the cage was first placed into the surgical pathway in an oblique direction, then rotated to a direction parallel to the posterior edge of the vertebral body, and placed into the intervertebral space. Then, a C‐arm was used to confirm that the cage spanned the entire ring apophysis with a larger footprint, and the interface support fixation and fusion procedures were completed. Afterwards, the L3–L4 intervertebral space was located in the same muscle window by moving up and adjusting the tubular retractor, and then the OLIF procedure was completed. For L2–L3 OLIF, a muscle window was made in the upper part of the incision, blunt separation was performed in the retroperitoneal space to reach the L2–L3 intervertebral space, and then the OLIF operation was completed. Step 3: after the OLIF procedure, the patient was moved to the prone position, and the left pedicle from L2 to L5 was marked. Then, the Wiltse approach was performed (Fig. 1B). Step 4: unilateral long‐tail multiaxial pedicle screw fixation was performed under direct vision at the left pedicle of L2–L5. The rod was prebent according to the curvature of the lumbar vertebra after the OLIF procedure. The rods were then placed and fixed without any force, such as compression, cantilever or rotation. These procedures were performed step by step under C‐arm fluoroscopic guidance. (Fig. 2 shows the operation schematic diagram).
Fig. 1.
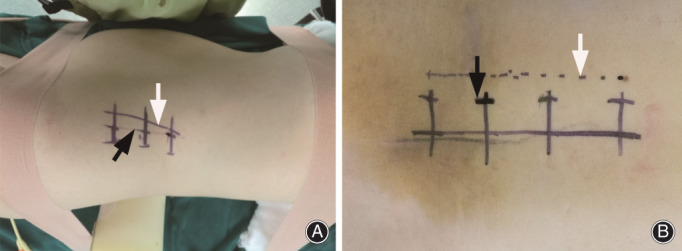
Three‐level OLIF from L2–L5 is taken as an example. (A) The anterior border of the L2–L3 and L4–L5 disc space (black arrow) was located using the C‐arm and then marked for the skin incision of OLIF (white arrow). (B) The C‐arm was used to locate the left pedicle of L2–L5 (black arrow), and then the skin at 2 cm away from the outer edge of the pedicle was marked for the incision of the Wiltse approach (white arrow).
Fig. 2.
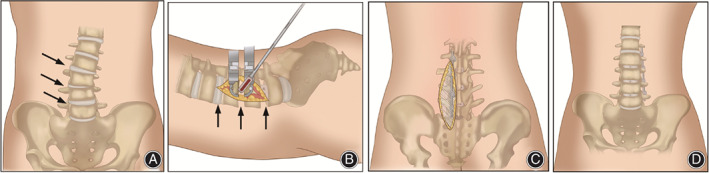
(A, D) Schematic diagram of preoperative and postoperative lumbar anterior view. (B) Schematic diagram of L2–L5 OLIF. (C) Schematic diagram of L2–L5 UPSF via Wiltse approach.
All patients were allowed to ambulate with the Boston brace on the second postoperative day. Removal of the Boston brace was recommended after 12 weeks.
Imaging Evaluation
All the parameters were measured twice, and the averages were adopted. The coronal Cobb angle, distance between the C7 plumb line and central sacral vertebral line (CSVL‐C7), sagittal vertebral axis (SVA), lumbar lordosis (LL), pelvic tilt (PT), and pelvic incidence‐lumbar lordosis mismatch (LL‐PI) were determined and compared. The fusion criteria for the CT studies included the presence of bony trabeculation across the fusion level and a lack of bony lucency at the graft/vertebral body junction 9 . A picture archiving and communication system was used to measure the cross‐sectional area of the dural sac (CSA) in the axial T2‐weighted MRI scans.
Clinical Evaluation
Lower back pain and leg pain were evaluated according to the Visual Analog Scale (VAS). The Oswestry Disability Index (ODI) before surgery and at the final follow‐up were compared. Surgical characteristics and complications were also recorded. The complications were evaluated during the follow‐up period and retrospectively reviewed in this study.
Visual Analog Scale
The VAS is the most commonly used questionnaire for quantifification of pain. It is a continuous scale comprised of a horizontal or vertical line, usually 10 cm in length. For pain intensity, the scale is most commonly anchored by “no pain” (score of 0) and “pain as bad as it could be” (score of 10). A score of 0 is considered no pain, 1–3 mild pain, 4–6 moderate pain, and 7–10 severe pain.
Oswestry Disability Index
The ODI is one of the principal condition‐specific outcome measures used in the management of spinal disorders, and to assess patient progress in routine clinical practice. The ODI score system includes 10 sections: pain intensity, personal care, lifting, walking, sitting, standing, sleeping, sex life, social life, and traveling. For each section of six statements, the total score is 5. Intervening statements are scored according to rank. If more than one box is marked in each section, the highest score is taken. If all 10 sections are completed, the score is calculated as follows: total scored out of total possible score × 100. If one section is missed (or not applicable), the score is calculated as: total score/(5× number of questions answered) × 100%. A score of 0%–20% is considered mild dysfunction, 21%–40% is moderate dysfunction, 41%–60% is severe dysfunction, and 61%–80% is considered a disability. For cases with a score of 81%–100%, patients are either long‐term bedridden, or exaggerating the impact of pain on their life.
Statistical Analysis
SPSS 23.0 software was used for statistical processing and analysis (SPSS Inc., Chicago, Illinois). The data that followed a normal distribution are expressed as the mean ± SD. The paired t‐test was used to perform pairwise comparisons. A P value of <0.05 was considered significant.
Results
Patients
A total of 12 patients were diagnosed with DLS and were successfully treated with OLIF in conjunction with UPSF. Of the patients, 2 were male and 10 others were female. The mean age at the time of the operation was 67.2 ± 9.1 years (range, 49–85 years). Mean body mass index (BMI) was 27.6 ± 2.1 kg/m2 (range, 24.4–31.2), and mean BMD was −1.9 ± 0.5 SD (range, −2.7 to −1.2). In addition, all patients were followed up by clinic review. The mean follow‐up period was 26.8 ± 1.8 months after the surgery (range, 24–30 months) (Table 1).
TABLE 1.
Summary of the patient demographic and operative characteristics
| Parameter | Value |
|---|---|
| Total no.of patients | 12 |
| Sex ratio (M:F) | 2:10 |
| Age, mean (range), years | 67.2 ± 9.1 (49–85) |
| Body mass index, mean (range), Kg/m2 | 27.6 ± 2.1 (24.4–31.2) |
| Bone mineral density. T‐score, mean (range) | −1.9 ± 0.5 (−2.7– −1.2) |
| Level of fusion | |
| L2‐L5 | 10 |
| L3‐L5 | 2 |
| Operation time, mean (range), mins | 156.5 ± 39.5 (85–210) |
| Intraoperative blood loss, mean (range), ml | 101.5 ± 47.8 (65–195) |
| Bed rest time, mean (range), days | 2 |
| Hospital stay, mean (range), days | 4.8 ± 1.4 (3–7) |
| Mean follow‐up, mean (range), months | 26.8 ± 1.8 (24–30) |
| Fusion rate (CT confirmation) | 100% |
Operation Results
All patients underwent a primary OLIF of ≥2 contiguous levels of fusion for DLS, 2‐level fusions were performed in two patients, and 3‐level fusions were performed in 10 patients. During surgery, time and blood loss were recorded. The mean blood loss was 101.5 ± 47.8 mL (range, 65–195 mL). The mean operation duration was 156.5 ± 39.5 min (range, 85–210 min). The mean bed rest time was 2 days. The mean length of postoperative hospital stay was 4.8 ± 1.4 days (range, 3–7 days) (Table 1).
Imaging Results
Imaging measurements preoperatively and at final follow‐up were showed in Tables 2 and 3.
TABLE 2.
Changes of CSA in surgical levels
| Time point | Cross‐sectional area of the dural sac (mm2) | |||
|---|---|---|---|---|
| L2–L3 | L3–L4 | L4–L5 | Average value | |
| Preoperative | 130.60 ± 50.53 | 79.06 ± 30.50 | 84.39 ± 38.58 | 87.33 ± 39.41 |
| Final follow‐up | 155.10 ± 50.63 | 111.60 ± 33.66 | 126.10 ± 38.55 | 124.70 ± 39.26 |
| P | 0.0007 | 0.0001 | 0.0001 | 0.0001 |
TABLE 3.
Clnical and radiographic outcomes
| Variable | Preoperative | Final follow‐up | P |
|---|---|---|---|
| Corona Cobb Angle (°) | 19.6 ± 4.8 | 6.9 ± 3.8 | 0.00 |
| Distance between the C7 plumb line and central sacral vertebral line (cm) | 2.5 ± 1.7 | 0.9 ± 0.6 | 0.00 |
| Sagittal vertebral axis (cm) | 4.3 ± 4.3 | 1.5 ± 1.0 | 0.03 |
| Lumbar lordosis (°) | 29.4 ± 8.6 | 40.8 ± 5.8 | 0.00 |
| Pelvic tilt (°) | 27.6 ± 10.8 | 18.3 ± 7.0 | 0.00 |
| Pelvic incidence‐lumbar lordosis mismatch (°) | 23.3 ± 10.5 | 11.9 ± 8.4 | 0.00 |
| Visual analog scale (back) | 7.3 ± 0.9 | 2.1 ± 0.8 | 0.00 |
| Visual analog scale (leg) | 7.8 ± 0.9 | 1.8 ± 0.8 | 0.00 |
| Oswestry disability index | 38.8 ± 2.3 | 21.9 ± 2.0 | 0.00 |
Cross‐Sectional Area of the Dural Sac
The mean CSA increased from 87.33 ± 39.41 mm2 before surgery to 124.70 ± 39.26 mm2 at the final follow‐up after surgery (P < 0.01).
Coronal Plane
The preoperative Coronal Cobb Angle and CSVL‐C7 were 19.6° ± 4.8° and 2.5 ± 1.7 cm, and the postoperative Coronal Cobb Angle and CSVL‐C7 at final follow up were 6.9° ± 3.8° and 0.9 ± 0.6 cm, respectively. Coronal Cobb Angle and CSVL‐C7 were significantly improved at the final follow‐up compared with the values before surgery (P < 0.01).
Sagittal Plane
All patients achieved statistically significant improvement in SVA (from preoperative 4.3 ± 4.3 cm to 1.5 ± 1.0 cm at final follow‐up, P = 0.03), LL (from preoperative 29.4° ± 8.6° to 40.8° ± 5.8° at final follow‐up, P < 0.01), PT (from preoperative 27.6° ± 10.8° to 18.3° ± 7.0° at final follow‐up, P < 0.01), and LL‐PI mismatch (from preoperative 23.3° ± 10.5° to 11.9° ± 8.4° at final follow‐up, P < 0.01).
Function Score
The VAS score and ODI score of 12 patients before surgery and at final follow‐up were available in Table 3.
Visual Analogue Scale Score
The VAS scores for back and leg pain of all patients at the final follow up (2.1 ± 0.8, 1.8 ± 0.8) were significantly lower than those before surgery (7.3 ± 0.9, 7.8 ± 0.9) (P < 0.01).
Oswestry Disability Index Score
The mean ODI score improved significantly from 38.8 ± 2.35 preoperatively to 21.9 ± 2.0 at the final follow up (P < 0.01).
Complications
One patient was found to have symptoms of lumbosacral plexus injury after surgery, such as thigh numbness, pain, and quadriceps weakness (grade 4 strength), which resolved on its own 1 week after surgery. During the follow‐up period, One patient had cage subsidence in L4–L5 intervertebral space 4 months after operation. Afterwards, the patients were treated with a spinal brace, were instructed not to perform weight‐bearing activity, and were treated with anti‐osteoporosis medication; she recovered well at the final follow‐up. The pedicle screws were not loose or pulled out in all patients at the final follow‐up. There were no other serious or minor complications during and after the operation (Table 4). The typical cases are shown in Figs 3, 4, 5.
TABLE 4.
Perioperative complications
| Complications | Number of patients | Percentage |
|---|---|---|
| Local hematoma | 0 | 0% |
| Ileus | 0 | 0% |
| Sympathetic chain symptom | 0 | 0% |
| Lumbar plexopathy (sensory) | 1 | 8.3% |
| Lumbar plexopathy (motor) | 1 | 8.3% |
| Cage subsidence | 1 | 8.3% |
| Screw malposition | 0 | 0% |
| Wound infection | 0 | 0% |
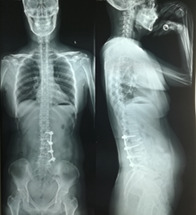
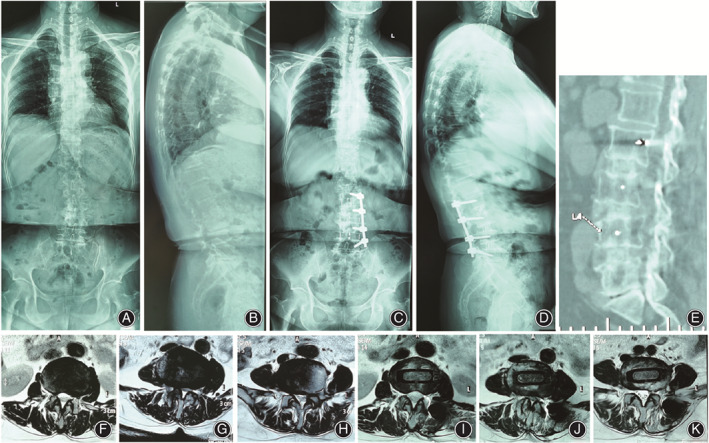
Fig. 3.
A typical case of a 58‐year‐old female who underwent a combined OLIF and UPSF for correction of DLS. (A) Anteroposterior (AP) view of preoperative standing full‐length spinal radiograph showed scoliosis. The Cobb angle was 30.8 degrees. (B) Lateral view of preoperative standing full‐length spinal radiograph showed sagittal alignment of the patient. (C) AP view of postoperative standing full‐length spinal radiograph showed correction of scoliosis. The Cobb angle was 0.3 degrees. (D) Lateral view of postoperative standing full‐length spinal radiograph showed realignment of sagittal plane. (E) 12‐month postoperative CT showing good alignment and fusion status. (F, G, H) The preoperative axial T2WI MRI scan showed narrowing of the spinal canal of L2–L3, L3–L4, and L4–L5. (I, J, K) The postoperative axial T2WI MRI scan showed indirect decompression of the spinal canal of L2–L3, L3–L4, and L4–L5.
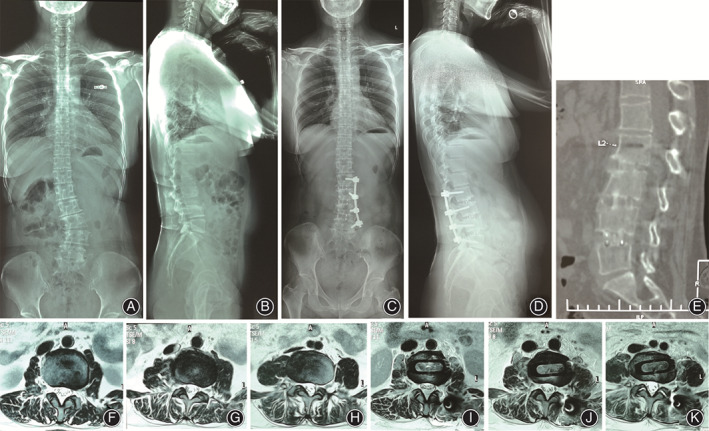
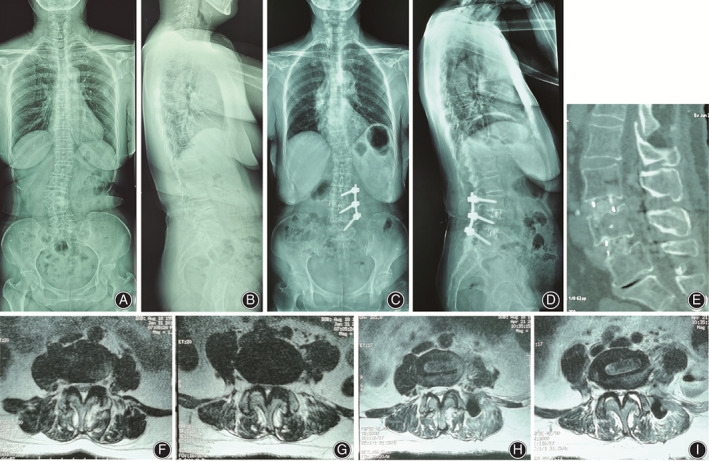
Fig. 4.
A typical case of a 64‐year‐old female of patient who underwent a combined OLIF and UPSF for correction of DLS. (A, B) Preoperative standing AP and lateral 36‐inch flms. (C, D) Postoperative standing AP and lateral 36‐inch flms. A satisfactory correction in coronal Cobb angle, LL, PT, LL‐PI mismatch, CSVL, and SVA was achieved. Parameters of coronal plane and sagittal plane were illustrated. (E) Interbody fusion had occurred. (F, G, H) Preoperative axial T2WI MRI showed narrowing of the spinal canal of L2–L3, L3–L4, and L4–L5. (I, J, K) Postoperative axial T2WI MRI showed indirect decompression of the spinal canal of L2–L3, L3–L4, and L4–L5.
Fig. 5.
(A–D) Pre‐ and postoperative standing full‐length spinal radiograph of patient who underwent a combined OLIF and UPSF for correction of DLS. OLIF procedure was performed at L3–L5 where degenerative change of intervertebral space happened. However, the coronal and sagittal spine alignment has been improved. (E) Interbody fusion had occurred. (F, G) Preoperative axial T2WI MRI showed narrowing of the spinal canal of L3–L4 and L4–L5. (H, I) Postoperative axial T2WI MRI showed indirect decompression of the spinal canal of L3–L4 and L4–L5.
Discussion
The main objectives of surgical treatment for DLS are to relieve lower back pain, improve lower extremity radiating pain and claudication, and correct the spinal deformity 10 , 11 . To achieve these goals, Silva and Lenke 8 classified DLS cases into six grades according to the patient's neurological symptoms, pain severity and spinal deformity severity and adopted different surgical methods for cases with different grades, including decompression, reduction, fusion fixation and deformity correction. To reduce perioperative complications, lumbar minimally invasive technology has attracted the attention of many scholars worldwide. The OLIF technique involves inserting a very large cage with the anterior approach, which can directly increase the height of the interbody, indirectly decompress the spinal canal, and improve coronal and sagittal spinal alignment 12 . The DLS cases included in this study were Lenke‐Silva type 2–4, and CT and MRI scans showed facet joint hyperplasia but not fusion; because these types of lumbar scoliosis angle are relatively small, the intervertebral space involved in the deformity is soft, and the balance of the coronal and sagittal planes are not obviously affected, satisfactory correction can be achieved through OLIF.
Radiographic and Clinical Outcomes
Degenerative lumbar scoliosis is often accompanied by lumbar stenosis. The OLIF technique can restore the disk height, stretch the ligamentum flavum, and indirectly decompress the spinal canal without removing the posterior lamina and ligaments by implanting a larger cage in the intervertebral space and removing the bulging disc. In our study, there was a significant improvement in the postoperative CSA compared with the preoperative values and good decompression effects in the central canal (P < 0.05), which are consistent with the results reported by Fujibayashi et al 13 . Fujibayashi et al. 13 performed indirect decompression with OLIF in 28 patients with lumbar spinal stenosis. The MRI scans showed that the CSA increased by 34.7 mm2, and all patients showed good clinical results. For patients with DLS, spinal canal decompression alone can significantly alleviate clinical symptoms in a short period of time, but it has no effect on the progression of scoliosis, lumbar instability or axial back pain. Even after decompression, because of damage to the lumbar structure, the above symptoms may be aggravated and require reoperation. Therefore, it is necessary to improve the sagittal and coronal alignment of the spine for these patients. In this group, the OLIF technique was used to implant the large cage through 2–3 intervertebral spaces and gradually adjust the curvature of the spine to achieve the correction. At the final follow‐up, the Cobb, LL, PT and LL‐PT angles were significantly improved compared with the values before surgery, and the correction result was similar to that reported in studies involving traditional open procedures 11 , 14 , 15 , 16 , 17 , 18 . Keorochana et al. 15 reported that 31 degenerative scoliosis patients with symptom of spinal stenosis were treated with traditional posterior decompression and fixation, the mean intraoperative blood loss was 667.39 mL, the mean follow‐up time was 32 months (range 24–60 months), and scoliosis was reduced from 14.38° to 7.85° at the latest follow‐up. Simmons and Simmons 16 reported 40 cases of lumbar scoliosis associated with spinal stenosis treated with posterior decompression and pedicular screw fixation, the average length of follow‐up was 44 months (range, 24–61), the average curve correction was better than 50% at the latest follow‐up.
However, all the patients in this group underwent the anatomical natural space approach, namely, OLIF and the Wiltse approach. Compared with the traditional surgery, there were fewer injuries to the psoas, paravertebral muscles and vascular bundles during the surgery. The average amount of blood loss during surgery was 101.5 ± 47.8 mL. After the surgery, this procedure showed the advantages of minor surgical trauma, a faster recovery, less postoperative pain, a shorter hospital stay and a lower cost. All patients could walk over ground with a Boston brace on the second postoperative day, which can prevent complications related to long‐term bedrest. The mean preoperative ODI index was 38.8 ± 2.3, and the mean preoperative VAS scores for back pain and leg pain were 7.3 ± 0.9 and 7.8 ± 0.9, respectively. The mean follow‐up duration was 26.8 ± 1.8 months. The results showed that the ODI and VAS scores at the final follow‐up were significantly improved, which is consistent with the results reported in other studies 14 , 19 , 20 , 21 .
Application of UPSF
Degenerative lumbar scoliosis is often complicated by osteoporosis 22 , as well as the presence of asymmetric tilt of a disc space in a deformed segment, which may lead to end plate fracture during the treatment of the intervertebral space by OLIF, so the cage is prone to subside after surgery. At present, most OLIF surgeries need to be performed with BPSF to prevent the subsidence of cages and maintain the stability of the spine. According to a study of large sample data, compared with UPSF, the overall effect of this procedure was not improved, and the complications caused by rigid internal fixation are increasingly prominent, such as the stress shielding effect, bone loss in the fused segment, and stress concentration, resulting in accelerated degeneration of adjacent segments 23 . In a finite element study, a 3‐level lateral interbody fusion with various supplemental instruments was constructed 24 . BPSF provided the maximum reduction in range of motion in every plane of motion (66.7%–90.9% of that of an intact spine), and UPSF also provided a significant reduction in segmental range of motion (45%–88.3% of that of an intact spine). Since pedicle screws are not be placed on the other side, compared with bilateral fixation, unilateral fixation has the advantages of lesser blood loss, a shorter operative time, a shorter length of hospital stay, and a lower medical cost.
Based on the advantages of the larger size of the OLIF cage and the fact that the bone structure, such as the posterior facet joint, is not damaged during the surgery, the authors attempted to treat 12 cases of lumbar degenerative scoliosis with OLIF combined with UPSF. The main purpose of UPSF is to provide stability for the fusion segments, promote interbody fusion, and prevent the subsidence of fusion cage. Before the installation of the rod, according to the lumbar lordosis after the OLIF procedure, the rod was prebent, and no force such as compression, cantilever or rotation was given during the fixation process. Let the fusion cage and internal fixation share the load together in the early postoperative period, so as to avoid excessive concentration of force on pedicle screws, which leads to loosening of the pedicle screw and further subsidence of the fusion cage. From the imaging data collected during follow‐up, cage subsidence at one level was observed in 1 of the patients at 4 months after the operation. Afterwards, the patients were treated with a spinal brace, were instructed not to perform weight‐bearing activity, and were treated with anti‐osteoporosis medication; 14 months after surgery, there was no looseness or breakage of the pedicle screw, and interbody fusion was complete. Ohtori et al. 25 reported 35 cases of lumbar degenerative diseases, including spondylolisthesis (20 patients), kyphoscoliosis (11 patients), and discogenic pain (four patients); After the treatment of OLIF combined with posterior fixation (open pedicle screws, percutaneous pedicle screws, or cortical bone trajectory screws); one patient was found to have subsidence of the cage. The incidence of cage subsidence in our group was comparable with that reported in the literature 25 , 26 . The results suggested that the stability of the spine can be maintained after UPSF.
Complications
In this group, the patients underwent interbody fusion and posterior fixation with OLIF and the Wiltse approach. Although the position of the patients needed to be changed during the operation, posterior fixation was performed under direct vision through the Wiltse approach, and long‐tailed multiaxial pedicle screws were used to reduce the difficulty of fixation to shorten the operating time and reduce the occurrence of hemorrhage. The actual operation time of this group of patients was 156.5 ± 39.5 min (85–210 min), which was almost the same as that of the patients who underwent OLIF combined with lateral fixation 27 . The treatment of lumbar degenerative diseases with OLIF combined with lateral fixation is performed with one incision, and the body position of the patient is not changed during surgery. Operations in the retroperitoneal space that take a long time and do not involve changing the position of the patient during the surgery which can lead to complications such as pressure sores, brachial plexus and common peroneal nerve injury and increase the possibility of injury to the retroperitoneal organs. However, the above situation can be avoided by using OLIF combined with pedicle screw fixation via the Wiltse approach, during which the position of the patient needs to be changed and internal fixation is not performed in the retroperitoneal space; the incision is smaller, the damage to the surrounding tissues and organs is smaller, and the risk of complications relating to incision such as hematoma and infection is reduced. Abe et al. 26 reported that 155 patients with lumbar degenerative diseases were treated with OLIF combined with posterior open or percutaneous pedicle screw fixation, and a postoperative surgical site infection occurred in three patients. Marchesi and Aebi 11 performed OLIF combined with percutaneous pedicle screw fixation in 28 patients with degenerative spinal diseases. During the early postoperative period, there were four cases of surgical site infection and three cases of retroperitoneal hematoma. In our study, the two surgical approaches had less damage to patients; no complications, such as incision hematoma and infection, were found; and the incidence was lower than that reported previous studies 11 , 26 . This discrepancy may be related to the choice of operative approach, the skill and experience of the surgeons and advancements in surgical instruments. The decompression and correction principle of LLIF in the treatment of DLS is similar to that of OLIF, but the LLIF approach passes through the psoas, and the approach is more posterior than that of OLIF, so damage to the lumbosacral nerves and psoas is more likely to occur. Moller et al. 28 retrospectively analyzed the data of 53 patients who underwent XLIF. The mean follow‐up duration was 21.2 months. The incidence of hip flexion weakness was 36%, the incidence of numbness in the front of the thigh was 25%, and the incidence of pain in the front of the thigh was 23%. Bergey et al. 29 reported that 30% of patients had paresthesia in the lower extremity and 27% had pain in the thigh after DLIF. In our study, we found that only one patient had a transient nerve injury, which resolved on its own 1 week after surgery, proving that the incidence of complications related to nerve injury after OLIF is significantly lower than that after LLIF 28 , 29 . In our group, all patients had undergone fusion of 2–3 levels. As the operation moves towards the caudal level, especially at the L4–5 level, the distribution of the psoas major and lumbar plexus nerve tends to be more anterior 30 ,which led to the reduction of OLIF operation space. Therefore, we considered that the symptoms of nerve injury may be related to the long‐time or excessive retraction of the psoas.
Limitations of the Study
There are some limitations in the present study. First, it is a retrospective and observational study. Second, it is a small sized study and the duration of follow‐up was also short. A large‐sample study needs to be conducted to prove the efficacy of OLIF combined with UPSF. Its long‐term efficacy and complications need to be further observed and studied. Based on the results of this study, it is our goal to conduct randomized control studies in the future. Third, further biomechanical studies are required to evaluate the stability of fusion constructs with UPSF with 3‐level OLIF, and comparative features against OLIF combined with BPSF. Fourth, our study did not include cases with severe sagittal imbalance and severe spinal stenosis, such as lumbar kyphosis or flat back.
Conclusion
This study is a retrospective study. OLIF in conjunction with UPSF seems to be a valuable surgical tool for the minimally invasive correction of coronal and sagittal plane deformities in patients with moderate degenerative lumbar scoliosis. It is a minimally invasive procedure that yields good radiographic and clinical results without any major complications.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The research project was approved by the ethics department of General Hospital of Ningxia Medical University, Ningxia. We have consensus with all participants. All the procedures were done under the Declaration of Helsinki and relevant policies in China. The Manuscript submitted does not contain information about medical device(s)/drug(s).
Funding
This work was financially supported by the Ningxia Provincial Key Research and Development Planed Projects (No. 2020BEG03034).
Open Access
This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Acknowledgements
This work was financially supported by the Ningxia Hui Autonomous Region Key Research and Development Planned Projects (No. 2020BEG03034).
References
- 1. Rihn JA, Patel R, Makda J, et al. Complications associated with single‐level transforaminal lumbar interbody fusion. Spine J, 2009, 9: 623–629. [DOI] [PubMed] [Google Scholar]
- 2. Rajaraman V, Vingan R, Roth P, Heary RF, Conklin L, Jacobs GB. Visceral and vascular complications resulting from anterior lumbar interbody fusion. J. Neurosurgery, 1999, 91: 60–64. [DOI] [PubMed] [Google Scholar]
- 3. Buchowski JM. Adult scoliosis:etiology and classification. Semin Spine Surg, 2009, 21: 2–6. [Google Scholar]
- 4. Ozgur BM, Aryan HE, Pimenta L, Taylor WR. Extreme lateral interbody fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. Spine J, 2006, 6: 435–443. [DOI] [PubMed] [Google Scholar]
- 5. Silvestre C, Mac‐Thiong JM, Hilmi R, Roussouly P. Complications and morbidities of mini‐open anterior retroperitoneal lumbar interbody fusion: oblique lumbarInterbody fusion in 179 patients. Asian Spine J, 2012, 6: 89–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Yücesoy K, Yüksel KZ, Baek S, Sonntag VK, Crawford NR. Biomechanics of unilateral compared with bilateral lumbar pedicle screw fixation for stabilization of unilateral vertebral disease. J Neurosurg Spine, 2008, 8: 44–51. [DOI] [PubMed] [Google Scholar]
- 7. Zhang K, Sun W, Zhao CQ, et al. Unilateral versus bilateral instrumented transforaminal lumbar interbody fusion in two‐level degenerative lumbar disorders: a prospective randomised study. Int Orthop, 2014, 38: 111–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Silva FE, Lenke LG. Adult degenerative scoliosis: evaluation and management. Neurosurg Focus, 2010, 28: E1. [DOI] [PubMed] [Google Scholar]
- 9. Ghiselli G, Wharton N, Hipp JA, Wong DA, Jatana S. Prospective analysis of imaging prediction of pseudarthrosis after anterior cervical discectomy and fusion: computed tomography versus flexion‐extension motion analysis with intraoperative correlation. Spine (Phila Pa 1976), 2011, 36: 463–468. [DOI] [PubMed] [Google Scholar]
- 10. Bradford DS, Tay BK, Hu SS. Adult scoliosis: surgical indications, operative management, complications, and outcomes. Spine (Phila Pa 1976), 1999, 24: 2617–2629. [DOI] [PubMed] [Google Scholar]
- 11. Marchesi DG, Aebi M. Pedicle fixation devices in the treatment of adult lumbar scoliosis. Spine (Phila Pa 1976), 1992, 17: S304–S309. [DOI] [PubMed] [Google Scholar]
- 12. Sato J, Ohtori S, Orita S, et al. Radiographic evaluation of indirect decompression of mini‐open anterior retroperitoneal lumbar interbody fusion: oblique lateral interbody fusion for degenerated lumbar spondylolisthesis. Eur Spine J, 2017, 26: 671–678. [DOI] [PubMed] [Google Scholar]
- 13. Fujibayashi S, Hynes RA, Otsuki B, Kimura H, Takemoto M, Matsuda S. Effect of indirect neural decompression through oblique lateral interbody fusion for degenerative lumbar disease. Spine(Phila Pa 1976), 2015, 40: E175–E182. [DOI] [PubMed] [Google Scholar]
- 14. Tsai TH, Huang TY, Lieu AS, et al. Functional outcome analysis: instrumented posterior lumbar interbody fusion for degenerative lumbar scoliosis. Acta Neuroehir (Wien), 2011, 153: 547–555. [DOI] [PubMed] [Google Scholar]
- 15. Keorochana G, Tawonsawatruk T, Wajanavisit W, Jaovisidha S. The results of decompression and instrutnented fusion with pedicular screw plate system in degenerative lumbar scoliosis patients with spinal stenosis: a prospective observational study. J Med Assoc Thai, 2010, 93: 457–461. [PubMed] [Google Scholar]
- 16. Simmons ED Jr, Simmons EH. Spinal stenosis with scoliosis. Spine, 1992, 17: S117–S120. [DOI] [PubMed] [Google Scholar]
- 17. Transfeldt EE, Topp R, Mehbod AA, Bandiera S, Simoes C, Boriani S. Surgical outcomes of decompression, decompression with limited fusion, and decompression with full curve fusion for degenerative scoliosis with radiculopathy. Spine, 2010, 35: 1872–1875. [DOI] [PubMed] [Google Scholar]
- 18. Barbanti Brodano G, Terzi S, Gasbarrini A, Bandiera S, Simoes C, Boriani S. Do benefits overcome the risks related to surgery for adult scoliosis? A detailed analysis of a consecutive case series. Eur Spine J, 2013, 22: S795–S802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Tempel ZJ, Gandhoke GS, Bonfield CM, Okonkwo DO, Kanter AS. Radiographic and clinical outcomes following combined lateral lumbar interbody fusion and posterior segmental stabilization in patients with adult degenerative scoliosis. Neurosurg Focus, 2014, 36: E11. [DOI] [PubMed] [Google Scholar]
- 20. Ohtori S, Orita S, Yamauchi K, et al. Mini‐open anterior retroperitoneal lumbar interbody fusion: oblique lateral interbody fusion for degenerated lumbar spinal kyphoscoliosis. Asian Spine J, 2015, 9: 565–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Acosta FL, Liu J, Slimack N, Moller D, Fessler R, Koski T. Changes in coronal and sagittal plane alignment following minimally invasive direct lateral interbody fusion for the treatment of degenerative lumbar disease in adults: a radiographic study. J Neurosurg Spine, 2011, 15: 92–96. [DOI] [PubMed] [Google Scholar]
- 22. Lonner BS, Auerbach JD, Sponseller P, Rajadhyaksha AD, Newton PO. Variations in pelvic and other sagittal spinal parameters as a function of race in adolescent idiopathic seoliosis. Spine(Phila Pa 1976), 2010, 35: 374–377. [DOI] [PubMed] [Google Scholar]
- 23. Lee CS, Hwang CJ, Lee S, et al. Risk factors for adjacent segment disease after lumbar fusion. Eur Spine J, 2009, 18: 1637–1643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Liu X, Ma J, Park P, Huang X, Xie N, Ye X. Biomechanical comparison of multilevel lateral interbody fusion with and without supplementary instrumentation: a three‐dimensional finite element study. BMC Musculoskelet Disord, 2017, 18: 63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ohtori S, Orita S, Yamauchi K, et al. Mini‐open anterior retroperitoneal lumbar interbody fusion: oblique lateral interbody fusion for lumbar spinal degeneration disease. Yonsei Med J, 2015, 56: 1051–1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Abe K, Orita S, Mannoji C, et al. Perioperative complications in 155 patients who underwent oblique lateral interbody fusion surgery:perspectives and indications from a retrospective, multicenter survey. Spine(Phila Pa 1976), 2017, 42: 55–62. [DOI] [PubMed] [Google Scholar]
- 27. Wang K, Zhang C, Cheng C, Jian F, Wu H. Radiographic and clinical outcomes following combined oblique lumbar interbody fusion and lateral instrumentation for the treatment of degenerative spine deformity: a preliminary retrospective study. Biomed Res Int, 2019, 2019: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Moller DJ, Slimack NP, Acosta FL Jr, Koski TR, Fessler RG, Liu JC. Minimally invasive lateral lumbar interbody fusion and transpsoas approach related morbidity. Neurosurg Focus, 2011, 3l: E4. [DOI] [PubMed] [Google Scholar]
- 29. Bergey DL, Villavicencio AT, Goldstein T, Regan JJ. Endoscopic lateral transpsoas approach to the lumbar spine. Spine (Phila Pa 1976), 2004, 29: 1681–1688. [DOI] [PubMed] [Google Scholar]
- 30. Davis TT, Bae HW, Mok JM, Rasouli A, Delamarter RB. Lumbar plexus anatomy within the psoas muscle: implications for the transpsoas lateral approach to the L4‐L5 disc. J Bone Joint Surg Am, 2011, 93: 1482–1487. [DOI] [PubMed] [Google Scholar]


