Abstract
The world's practice has shown the importance of medical rehabilitation, which allows increasing the effectiveness of treatment of patients with COVID-19, and also significantly reduce the risks of developing complications after COVID-19. Moreover, timely medical rehabilitation reduces the frequency of disability retirement. We developed and investigated the effectiveness of the telemedicine platform “COVIDREHAB” in order to enhance the effectiveness of the recovery period during self-isolation, as well as to provide access to rehabilitation for patients residing in remote areas or unable to undergo in-person medical rehabilitation. This pilot open clinical study includes 178 patients (108 women and 70 men) aged 32 to 82 years [mean age 50 (33-56) years] who had a moderate disease of COVID-19. We used the specialised platform COVIDREHAB for remote monitoring of the rehabilitation efficiency of patients who suffered from COVID-19. During the study, the supervising doctor assigned the patient a set of specialised questionnaires, which were filled in online. The questionnaires distributed to the patient included questions specifically designed for the COVIDREHAB remote platform as well as the mMRC (Modified Medical Research Council) questionnaire. Patients who completed the remote rehabilitation programme were found to have positive dynamics of indicators of the respiratory system functional state, and complaints.Pulmonary rehabilitation is an important part of case management for patients with respiratory diseases and plays an active role in improving lung function and general well-being of patients. Patients who completed the comprehensive medical rehabilitation program using the information and analytical system COVIDREHAB, were found to have positive dynamics of indicators of the respiratory system functional state, and complaints. Hence, at the end of the course the shortness of breath severity decreased (from 34.8% to 12.4%, as well as the feeling of lack of oxygen from 32% to 17.4%, p <0.05). We anticipate the online approach to rehabilitation will improve the functioning of the respiratory and cardiovascular systems, restore physical function, reduce anxiety and depression, and restore quality of life. An essential benefit of this program is the prevention of secondary complications and reduction of serious adverse effects of COVID-19 treatment.".
Key Words: Rehabilitation, COVID-19, telemedicine technologies, physiotherapy exercises
Ethical Publication Statement
We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
In the Russian Federation, about 4.606.162 cases of COVID-19 were detected from 03/02/2020 to 04/07/2021. Of these, 4.239.038 people recovered. The published data indicate that symptoms such as coughing and shortness of breath may persist in patients with moderate to severe COVID-19 after Hospital discharge, as well as signs of muscle atrophy (including respiratory and torso muscles) and other disorders. Apart from cardiorespiratory system dysfunctions, some patients suffer from digestive system disorders: diarrhoea, abdominal pain, complete lack of appetite, nausea.1-4 Moreover, the tolerance of these patients to physical activity and quality of life in general decreases sharply.5 Again, the risk of long-term physical, cognitive, and emotional complications, the so-called PICS syndrome (Post Intensive Care Syndrome, Post-Reanimation Syndrome), increases in severe and critical patients who stay in intensive care units (ICU) for a long time.6 Major risk factors include cognitive impairment, acute brain dysfunction, hypoxia, and arterial hypotension.7 For example, cognitive impairment is observed in 30–80 % of patients after ICU. PICS annual results have been reported to include new symptoms such as shortness of breath, sexual dysfunction, impaired lung function and impaired exercise tolerance. At least 25 % of such patients become disabled and experience a dramatic drop in independence during the year following ICU, placing a huge burden on informal and formal caregivers.8-10 The world's practice has shown the importance of medical rehabilitation, which allows increasing the effectiveness of treatment of patients with COVID-19, as well as significantly reduce the recovery period and the return of the patient to normal daily life.11,12 Moreover, timely medical rehabilitation reduces the frequency of disability retirement. Therefore, rehabilitation of patients who have suffered from COVID-19 should include 4 components:10
Abatement of symptoms associated with pneumonia and pulmonary fibrosis developing in an injured area;
Correction of concomitant lung diseases [chronic obstructive pulmonary disease (COPD), bronchial asthma, chronic obstructive bronchitis], which have worsened as a result of the infection;
Recovery of breathing muscles reserves, and recovery of the best achievable functional independency;
Restoration of other systems and organs.10
Considering low availability of medical rehabilitation and the conditions of self-isolation as a whole, the use of telemedical technologies for rehabilitation activities is considered to only solutions to these problems.13-15 In order to enhance the effectiveness of the recovery period during self-isolation, as well as to provide access to rehabilitation for patients residing in remote areas or unable to undergo in-person medical rehabilitation, we developed the telemedicine platform COVIDREHAB.
Materials and Methods
The platform is an information and analytical system for remote monitoring of medical rehabilitation of patients who have suffered from COVID-19. According the urgency and importance of the issue of medical rehabilitation of patients after coronavirus infection, the platform was developed in May 2020 in record time and is currently being piloted at the National Medical Research Center of the Ministry of Health of Russia. The platform is technically located in the Rostelecom data center, in a cloud protected in accordance with the Federal Law "On Personal Data" dated July 27, 2006 N 152-FZ. The use of the platform is based on the "Temporary guidelines: prevention, diagnosis and treatment of a new coronavirus infection COVID-19", approved by the Ministry of Health of the Russian Federation. To work with the platform, the patient and physiotheraputist need: a device with a microphone and a camera: a mobile phone, tablet or computer, an Internet connection and an e-mail address on this device. The registration of a patient for classes is as follows: the patient opens www.covidrehab.online and clicks "Join group". Then he fills out the questionnaire and receives further instructions to his email address. The patient signs an informed consent to the processing of personal data, as well as consent to distant class of physiotherapy. The information and analytical system allows online group exercise therapy with an instructor or physiotherapist (breathing exercises, aerobic training, strength building of various intensity levels); training in drain breathwork in patients with increased mucus formation; neuropsychological support. And also to conduct Health Schools for patients on the following issues: nutrition, restoration of intestinal microflora, replenishment of deficits and non-drug methods of recovery after COVID-19. The study enrolled 178 patients (108 women and 70 men) aged 32 to 82 years (mean age 50 [33;56] years) who had moderate illness and severe illness.16 COVID-19 disease and were discharged from the hospital with negative tests for Severe acute respiratory syndrome-related coronavirus 2 (SARS-CoV2) with recommendations for a fortnight self-isolation. All patients signed an informed consent to the processing of personal data and to remote rehabilitation. During the study, the supervising doctor assigned patienst a set of specialised questionnaires, which were filled in online. The questionnaires distributed included questions specifically designed (Table 1) for the COVIDREHAB remote platform as well as the mMRC (Modified Medical Research Council) questionnaire.17
Table 1.
Breathing characteristics
| At the beginning of treatment, % | At the end of the treatment, % | Asymptotic significance | |
|---|---|---|---|
| Improving the condition of the respiratory system | 55,6 | 67,4* | 0,008 |
| Shortness of breath | 34,8 | 12,4* | 0,015 |
| Sense of oxygen deficiency | 32 | 17,4* | 0,018 |
Data are presented as frequencies. The analysis of differences was made according to the X2 criterion. *, significant improvement
The questionnaires of Figure 1 were primarily aimed at assessing the complaints rate and functional state of patients. The medical rehabilitation using the information and analytical system COVIDREHAB lasted 14 days: 10 days of online training with an instructor, 4 days of solo sessions with video.
Fig 1.
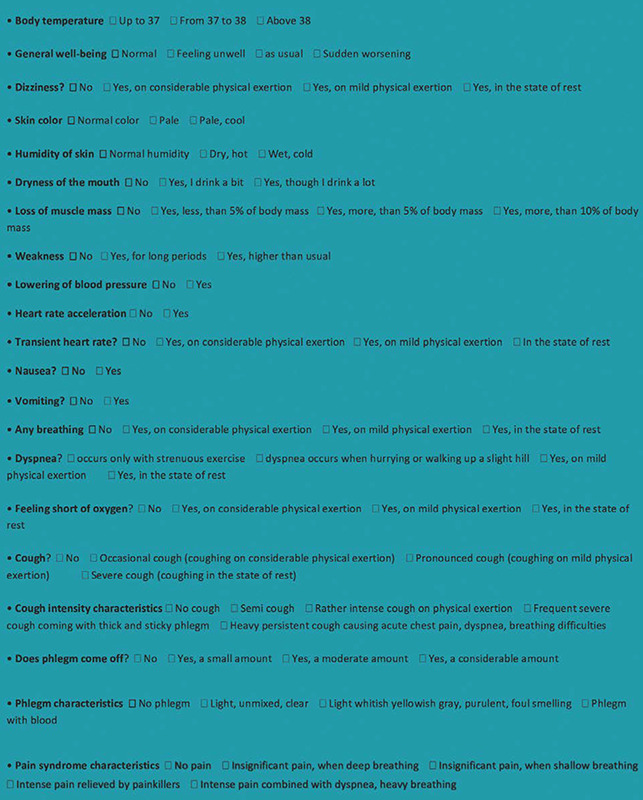
Questionnaire before the start and after the end of the telerehabilitation course
Table 2.
Cough characteristics
| At the beginning of treatment, % | At the end of the treatment, % | Asymptotic significance | |
|---|---|---|---|
| Cough | 35 | 20* | 0,011 |
| Having a cough | 26 | 15 | 0,125 |
Data are presented as frequencies. The analysis of differences was made according to the X2 criterion. *, significant improvement
Patients received a comprehensive medical rehabilitation program, consisting of breathing exercises and conditioning exercises in prone, seated and upright position, as well as abdominal breathing training. At the beginning of the remote course of remedial gymnastics, the total number of exercises varied from 10 to 12, the ratio of special breathing exercises to exercises for training limb muscles was 1:1. Subsequently, the load intensity increased, and the ratio of special breathing exercises and exercises for training limb muscles was changed to 1:2. After each session (45 min), the patient was advised to fill out a questionnaire on the toleration of remedial gymnastics. The patient receives all notifications about the beginning of classes by mail.
The condition of patients was assessed before and after the rehabilitation programme with the help of questionnaires.
The statistical data processing was carried out using the SPSS23 application package. Quantitative data were presented as median (Me) and quartiles [Q1; Q3]. The analysis of differences in dynamics (before and after medical rehabilitation) was performed by Wilcoxon signed-rank test and Verte.
Results and Discussion
Patients who completed the comprehensive medical rehabilitation program using the information and analytical system COVIDREHAB, were found to have positive dynamics of indicators of the respiratory system functional state, and complaints. Hence, at the end of the course the shortness of breath severity decreased (from 34.8% to 12.4%, as well as the feeling of lack of oxygen from 32% to 17.4%, p <0.05) (Table 1). Furthermore, coughing severity significantly reduced, as well as the amount of mucus. At the same time, it was noted that its consistency improved. Thus, in 85 % of patients sputum became easily discharged (p<0,05) (Table 2). Subsequent assessment of the complaints rate dynamics showed improvement in the overall well-being of patients in 83% of patients after medical rehabilitation compared with 75% of patients before the course, p <0.05). In addition, the percentage of complaints of weakness decreased (from 26 to 14, p <0.05), and positive changes were observed in the gastrointestinal tract [dry mouth (from 20 to 8, p <0.05)] (Table 3). The indicators for the cardiovascular system also improved (decrease of systolic and diastolic blood pressure and heart rate) (Table 4). During the online course of remedial gymnastics, 5 patients suffered from undesirable effects immediately after the session. Undesirable effects were observed during the first week of classes and were expressed in increased coughing immediately after the session (3 patients) and light vertigo (2 patient). No undesirable effects were observed in these patients during the next 2 weeks.
Table 3.
Dynamics of complaint rates in patients who have had COVID
| At the beginning of treatment, % | At the end of the treatment, % | Asymptotic significance | |
|---|---|---|---|
| Paleness of skin | 2 | 2 | 1 |
| Skin moisture content | 3 | 3 | 1 |
| Dry mouth | 20 | 8* | 0,063 |
| Reduced muscle mass | 2 | 2 | 0,48 |
| Weakness | 26 | 14* | 0,014 |
| Increased systolic pressure | 16 | 5* | 0,043 |
| Nausea | 1 | 1 | 1 |
| Vomiting | 0 | 0 | 1 |
Data are presented as frequencies. The analysis of differences was made according to the X2 criterion. *, significant improvement
Table 4.
Characteristics of the cardiovascular system
| At the beginning of treatment at rest | At the end of the treatment at rest | Asymptotic significance | |
|---|---|---|---|
| Heart rate | 89 [77;107] | 83[71;94]* | 0,027 |
| Saturation (using a pulse oximeter) | 91 [90;94] | 97 [95;98]* | 0,0445 |
The data are presented as median (Me) and quartiles [Q1; Q2]. The difference analysis was performed by the Wilcoxon signed-rank test. *, significant improvement
Rehabilitation lung therapy is an important part of management for patients with respiratory diseases and plays an active role in improving lung function and general well-being of patients.18-20 A need for a fortnight self-isolation of patients after discharge from the hospital, as well as a high occupancy of rehabilitation centres have contributed to the active development of digital technologies in the field of rehabilitation after COVID-19. We have made a confident and rapid start in this area in Russia due to the positive experience of our foreign colleagues.21-22 The data obtained indicate the high efficiency and significance of controlling online exercise therapy sessions for patients.23,24 This project for ex-COVID-19 patients has the following qualitative results: improvement of quality of patients’ life; timely dynamic monitoring and timely referral to relevant experts; speeding of restoration process after treatment; psychological support; prevention of secondary complications; reduction of severe adverse effects of treatment; lightening of burden on family members and guardians. The Russian Healthcare System might be interested in the following results of this project: reduction of disability periods; reduction of rehospitalization rates; decreased need in additional support; lower disability. The COVIDREHAB Project is designed for all COVID-19 patients, both in the present and in the future, as well as for optimising and reducing the burden on the medical officers involved in the treatment of COVID-19 patients in any respect. This clinical study to assess the effectiveness of distance rehabilitation is still ongoing. We anticipate the online approach to rehabilitation will improve the functioning of the respiratory and cardiovascular systems, restore physical function, reduce anxiety and depression, and restore quality of life. An essential benefit of this program is the prevention of secondary complications and reduction of serious adverse effects of COVID-19 treatment.
In conclusion, in modern realities, distance rehabilitation is a component that provides comprehensive recovery after COVID-19 offering improvement of the quality of life and well-being of the patient, psychological support, reduction of disability, timely dynamic observation and timely compliance with specialists, accelerating the recovery process after treatment, prevention of secondary complications, reduction of serious adverse effects of treatment end loads reduce the burden on family members and caregivers.
Acknowledgments
The Authors thank colleagues of the Department of Neurosciences, University of Padova, Italy and of the A&C M-C Foundation for Translational Myology, Padova, Italy for discussions and critical readings.
List of acronyms
- COPD
Chronic obstructive pulmonary disease
- COVID-19
Covid- 19 disease
- COVIDREHAB
telemedicine platform
- ICU
intensive care units
- mMRC
Modified Medical Research Council
- PICS syndrome
(Post Intensive Care Syndrome and Post-Reanimation Syndrome)
- SARS-CoV2
Severe acute respiratory syndrome-related coronavirus 2
Funding Statement
Funding None.
Contributor Information
Ilmira R. Gilmutdinova, Email: gilm.ilmira@mail.ru.
Vasiliy A. Kolyshenkov, Email: Vasiliy4kol@gmail.com.
Kristina A. Lapickaya, Email: Kri_kristy@mail.ru.
Anastasiya S. Trepova, Email: anastasiatrepova@yandex.ru.
Valeriia A. Vasileva, Email: Valeri08.00@bk.ru.
Andrei N. Prosvirnin, Email: Mister.prosvirnin2011@yandex.ru.
Larisa A. Marchenkova, Email: MarchenkovaLA@nmicrk.ru.
Maxim Y. Yakovlev, Email: masdat@mail.ru.
Andrey P. Rachin, Email: andrey_rachin@mail.ru.
Anatoliy D. Fesyun, Email: fad68@yandex.ru.
Igor V. Reverchuk, Email: bios@reverchuk.com.
References
- 1.Khan F, Amatya B. Medical Rehabilitation in Pandemics: Towards a New Perspective. J Rehabil Med. 2020. Apr 14;52(4):jrm00043. doi: 10.2340/16501977-2676. [DOI] [PubMed] [Google Scholar]
- 2.Kedor С, Freitag H, MeyerArndt L, Wittke K, Zoller T, Steinbeis F, Haffke M, Rudolf G, Heidecker B, Volk HD, Skurk C, Paul F, Bellmann-Strobl J, Scheibenbogen C. Chronic COVID-19 Syndrome and Chronic Fatigue Syndrome (ME/CFS) following the first pandemic wave in Germany – a first analysis of a prospective observational study. MedRxiv. 2021. Feb 06. 21249256; doi: 10.1101/2021.02.06.21249256. [Google Scholar]
- 3.Fesyun AD, Lobanov AA, Rachin AP, Yakovlev MYu, Andronov SV, Konchugova TV, Gilmutdinova IR, Barashkov GN, Mitroshkina EE, Bogdanova EN, Lebedev YaO, Nikitina AM. Challenges and Approaches to Medical Rehabilitation of Patients With COVID-19 Complications. Bulletin of Rehabilitation Medicine. 2020. June 97(3):3-13. doi:10.38025/2078-1962-2020-97-3-3-1 . [Google Scholar]
- 4.Chinese Thoracic Society; Chinese Association of Chest Physicians. [Guide for the prevention and treatment of coronavirus disease 2019]. Zhonghua Jie He He Hu Xi Za Zhi. 2020. Jun 12;43(6):473-489. Chinese. doi: 10.3760/cma.j.cn112147-112147-20200321-00392. [DOI] [PubMed] [Google Scholar]
- 5.Delorey TM, Ziegler CGK, Heimberg G, Normand R, Yang Y, Segerstolpe Å, Abbondanza D, Fleming SJ, Subramanian A, Montoro DT, Jagadeesh KA, Dey KK, Sen P, Slyper M, Pita-Juárez YH, Phillips D, Biermann J, Bloom-Ackermann Z, Barkas N, Ganna A, Gomez J, Melms JC, Katsyv I, Normandin E, Naderi P, Popov YV, Raju SS, Niezen S, Tsai LT-Y, Siddle KJ, Sud M, Tran VM, Vellarikkal SK, Wang Y, Amir-Zilberstein L, Atri DS, Beechem J, Brook OR, Chen J, Divakar P, Dorceus P, Engreitz JM, Essene A, Fitzgerald DM, Fropf R, Gazal S, Gould J, Grzyb J, Harvey T, Hecht J, Hether T, Jané-Valbuena J, Leney-Greene M, Ma H, McCabe C, McLoughlin DE, Miller EM, Muus C, Niemi M, Padera R, Pan L, Pant D, Pe'er C, Pfiffner-Borges J, Pinto CJ, Plaisted J, Reeves J, Ross M, Rudy M, Rueckert EH, Siciliano M, Sturm A, Todres E, Waghray A, Warren S, Zhang S, Zollinger DR, Cosimi L, Gupta RM, Hacohen N, Hibshoos H, Hide W, Price AL, Rajagopal J, Tata PR, Riedel S, Szabo G, Tickle TL, Ellinor PT, Hung D, Sabeti PC, Novak R, Rogers R, Ingber DE, Jiang ZG, Juric D, Babadi M, Farhi SL, Izar B, Stone JR, Vlachos IS, Solomon IH, Ashenberg O, Porter CBM, Li B, Shalek AK, Villani A-C, Rozenblatt-Rosen O, Regev A. COVID-19 tissue atlases reveal SARS-CoV-2 pathology and cellular targets. Nature. 2021. Apr 29. doi: 10.1038/s41586-021-03570-8. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grant CJ, Doig LF, Everson J, Foster N, Doig CJ. Impact of Patient and Family Involvement in Long-Term Outcomes. Crit Care Nurs Clin North Am. 2020. Jun;32(2):227-242. doi: 10.1016/j.cnc.2020. 02.005. Epub 2020 Apr 8. [DOI] [PubMed] [Google Scholar]
- 7.Ahmad I, Rathore FA. Neurological manifestations and complications of COVID-19: A literature review. J Clin Neurosci. 2020. Jul;77:8-12. doi: 10.1016/j.jocn.2020.05.017. Epub 2020 May 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stam HJ, Stucki G, Bickenbach J. Covid-19 and Post Intensive Care Syndrome: Call for Action. J Rehabil Med. 2020. Apr 15;52(4):jrm00044. doi: 10.2340/16501977-2677. [DOI] [PubMed] [Google Scholar]
- 9.Henk J. Stam, Gerold Stucki, Jerome Bickenbach. Covid-19 and Post Intensive Care Syndrome: A Call for Action. J Rehabil Med. 2020;52(4):jrm00046. Published 2020 Apr 15. doi:10.2340/16501977-2677. [DOI] [PubMed] [Google Scholar]
- 10.Brugliera L, Spina A, Castellazzi P, Cimino P, Tettamanti A, Houdayer E, Arcuri P, Alemanno F, Mortini P, Iannaccone S. Rehabilitation of COVID-19 patients. J Rehabil Med. 2020;52(4):jrm00046. Published 2020 Apr 15. doi:10.2340/16501977-2678. [DOI] [PubMed] [Google Scholar]
- 11.De Sire A, Andrenelli E, Negrini F, Negrini S, Ceravolo MG. Systematic rapid living review on rehabilitation needs due to COVID-19: update as of April 30th, 2020. Eur J Phys Rehabil Med. 2020. Jun;56(3):354-360. doi: 10.23736/S1973-9087.20.06378-9. Epub 2020 May 15. [DOI] [PubMed] [Google Scholar]
- 12.Barker-Davies RM, O'Sullivan O, Senaratne KPP, Baker P, Cranley M, Dharm-Datta S, Ellis H, Goodall D, Gough M, Lewis S, Norman J, Papadopoulou T, Roscoe D, Sherwood D, Turner P, Walker T, Mistlin A, Phillip R, Nicol AM, Bennett AN, Bahadur S. The Stanford Hall consensus statement for post-COVID-19 rehabilitation. Br J Sports Med. 2020. Aug;54(16):949-959. doi: 10.1136/bjsports-2020-102596. Epub 2020 May 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Venkatesan P. NICE guideline on long COVID. Lancet Respir Med. 2021. Feb;9(2):129. doi: 10.1016/S2213-2600(21)00031-X. Epub 2021 Jan 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Negrini S, Kiekens C, Bernetti A, Capecci M, Ceravolo MG, Lavezzi S, Zampolini M, Boldrini P. Telemedicine from research to practice during the pandemic. "Instant paper from the field" on rehabilitation answers to the COVID-19 emergency. Eur J Phys Rehabil Med. 2020. Jun;56(3):327-330. doi: 10.23736/S1973-9087.20.06331-5. Epub 2020 Apr 24. [DOI] [PubMed] [Google Scholar]
- 15.da Silva TD, de Oliveira PM, Dionizio JB, de Santana AP, Bahadori S, Dias ED, Ribeiro CM, Gomes RA, Ferreira M, Ferreira C, de Moraes ÍAP, Silva DMM, Barnabé V, de Araújo LV, Santana HBR, Monteiro CBM. Comparison Between Conventional Intervention and Non-immersive Virtual Reality in the Rehabilitation of Individuals in an Inpatient Unit for the Treatment of COVID-19: A Study Protocol for a Randomized Controlled Crossover Trial. Front Psychol. 2021. Feb 24;12:622618. doi: 10.3389/fpsyg.2021.622618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Akimkin VG, Kuzin SN, Semenenko TA, Shipulina OYu, Yatsyshina SB, Tivanova EV, Kalenskaya AV, Solovyova IV, Vershinina MA, Kvasova OA, Ploskireva AA, Mamoshina MV, Elkina MA, Klushkina VV, Andreeva EE, Ivanenko AV. Patterns of the SARS-CoV-2 epidemic spread in a megacity. Vopr Virusol. 2020. Sep 3;65(4):203-211. doi: 10.36233/0507-4088-2020-65-4-203-211. [DOI] [PubMed] [Google Scholar]
- 17.Richards JB. Calculated decisions: mMRC (Modified Medical Research Council) Dyspnea Scale. Emerg Med Pract. 2017. Oct 25;19(Suppl 10):1-2. [PubMed] [Google Scholar]
- 18.Liu W, Mu X, Wang X, Zhang P, Zhao L, Li Q. Effects of comprehensive pulmonary rehabilitation therapy on pulmonary functions and blood gas indexes of patients with severe pneumonia. Exp Ther Med. 2018. Sep; 16(3): 1953–1957. Published online 2018 Jul 3. doi: 10.3892/etm.2018.6396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sañudo B, Seixas A, Gloeckl R, Rittweger J, Rawer R, Taiar R, van der Zee EA, van Heuvelen MJG, Lacerda AC, Sartorio A, Bemben M, Cochrane D, Furness T, de Sá-Caputo D, Bernardo-Filho M. Potential Application of Whole Body Vibration Exercise For Improving The Clinical Conditions of COVID-19 Infected Individuals: A Narrative Review From the World Association of Vibration Exercise Experts (WAVex) Panel. Int J Environ Res Public Health. 2020. May 22;17(10):3650. doi: 10.3390/ijerph17103650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yang LL, Yang T. Pulmonary Rehabilitation for Patients with Coronavirus Disease 2019 (COVID-19). Version 2. Chronic Dis Transl Med. 2020. May 14;6(2):79-86. doi: 10.1016/j.cdtm.2020.05.002. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rassouli F, Boutellier D, Duss J, Huber S, Brutsche MH. Digitalizing multidisciplinary pulmonary rehabilitation in COPD with a smartphone application: an international observational pilot study. Int J Chron Obstruct Pulmon Dis. 2018. Nov 23;13:3831-3836. doi: 10.2147/COPD.S182880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bourne S, DeVos R, North M, Chauhan A, Green B, Brown T, Cornelius V, Wilkinson T. Online versus face-to-face pulmonary rehabilitation for patients with chronic obstructive pulmonary disease: randomised controlled trial. 2017 July. BMJ Open 7(7):e014580. doi:10.1136/bmjopen-2016-014580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shmonin AA, Maltseva MN, Melnikova EV, Mishina IE, Ivanova GE. Medical Rehabilitation For Coronavirus Infection: New tasks for physical and rehabilitation medicine in Russia. Bulletin of Rehabilitation Medicine. 2020. June; 97(3):14-21. doi:10.38025/2078-1962-2020-97-3-14-21. [Google Scholar]
- 24.Bodrova RA, Kiryanova VR, Tsykunov MB, Delyan AM, Sadykov IF, Savina AI, Khusainova ER. Abilities of physical rehabilitation in pneumonia. Bulletin of Rehabilitation Medicine. 2020. June; 97(3):31-39. doi:10.38025/2078-1962-2020-97-3-31-39. [Google Scholar]


