Abstract
Introduction:
Although evidence indicates Black gay, bisexual, and other sexual minority men experience vast psychological and behavioral health inequities, most research has focused on individual rather than structural drivers of these inequities. This study examines associations between structural racism and anti–lesbian, gay, bisexual, transgender, and queer (LGBTQ) policies and the psychological and behavioral health of Black and White sexual minority men.
Methods:
Participants were an Internet-based U.S. national sample of 1,379 Black and 5,537 White sexual minority men during 2017–2018. Analysis occurred in 2019–2020. Structural equation modeling tested associations from indicators of structural racism, anti-LGBTQ policies, and their interaction to anxiety symptoms, depressive symptoms, perceived burdensomeness, heavy drinking, and HIV testing frequency. Separate models for Black and White sexual minority men adjusted for contextual and individual covariates.
Results:
For Black participants, structural racism was positively associated with anxiety symptoms (β=0.20, SE=0.10, p=0.04), perceived burdensomeness (β=0.42, SE=0.09, p<0.001), and heavy drinking (β=0.23, SE=0.10, p=0.01). Anti-LGBTQ policies were positively associated with anxiety symptoms (β=0.08, SE=0.04, p=0.03), perceived burdensomeness (β=0.20, SE=0.04, p<0.001), heavy drinking (β=0.10, SE=0.04, p=0.01), and negatively associated with HIV testing frequency (β= −0.14, SE=0.07, p=0.04). Results demonstrated significant interaction effects, such that the positive associations between structural racism and both perceived burdensomeness (β=0.38, SE=0.08, p≤0.001) and heavy drinking (β=0.22, SE=0.07, p=0.003) were stronger for individuals living in states with high levels of anti-LGBTQ policies. Neither of the oppression variables nor their interaction were significantly associated with outcomes for White sexual minority men.
Conclusions:
Results highlight the intersectional nature of structural oppression and suggest racist and anti-LGBTQ policies must be repealed to rectify health inequities facing Black sexual minority men.
INTRODUCTION
Over the past decade, major U.S. health organizations like the American Psychological Association1 and Centers for Disease Control and Prevention2 and have documented vast psychological and behavioral health inequities facing Black gay, bisexual, and other sexual minority men (SMM). Despite these reports, there is a dearth of research highlighting the structural causes of inequities like those in chronic psychological conditions1 and HIV.3 Indeed, most studies with Black SMM focus on individual-level explanatory variables4 despite evidence suggesting that health inequities cannot be accounted for by differences in individual-level factors (e.g., health behavior) alone.5–8 Research investigating the health effects of structural oppression has highlighted critical associations between structural racism and anti–lesbian, gay, bisexual, transgender, and queer (LGBTQ) policies with psychological and behavioral health outcomes.9,10 However, these studies have not examined the synergistic effects of these 2 forms of structural oppression that both target Black SMM. To address this gap, the present study examines independent and conjoint associations between U.S. state-level structural racism and anti-LGBTQ policies and psychological and behavioral health outcomes among a national sample of Black and White SMM.
Structural racist and anti-LGBTQ oppression have their foundation in historically rooted cultural ideologies and interconnected institutions (e.g., law enforcement, local governments) that systematically label and marginalize Black sexual minority communities.11–16 Structural oppression is unique from individual oppression because it is enacted through systems rather than just individuals with power and prejudice.17 The intersectionality framework provides a theoretical lens through which to examine how systems of oppression (e.g., racism, heterosexism) intersect at the social–structural level to produce inequalities that drive persistent health inequities.18–20 An example of how the intersection of structural racism and anti-LGBTQ policies operates in the U.S. is its carceral system, including law enforcement practices and HIV criminalization laws that vastly disproportionately affect Black SMM.21 These policies, in turn, affect individual health by increasing community-level stress.9,14,22 Recent recommendations for best practices in population research assert these sources of structural oppression are consequential, yet understudied, drivers of health inequities among individuals with multiple interlocking stigmatized social positions like Black SMM.18,23,24 Accordingly, there is a need for intersectionality research that investigates how structural racism and anti-LGBTQ policies jointly drive psychological and behavioral health inequities among Black SMM.
Although an accumulating body of empirical research provides evidence that structural oppression related to single axes of identity (e.g., race alone) is associated with negative health outcomes,9,10 there is limited research documenting the mutually reinforcing effects of structural racism and anti-LGBTQ policies on Black SMM’s health. This dearth of evidence reflects a substantial limitation in science studying the effects of oppression for Black SMM, who are a prime example of a community that is subjected to multiple, intersecting forms of oppression (e.g., racism, heterosexism).12 For structural racism, available, albeit relatively limited,10 research indicates that state- and county-level structural racism (e.g., White–Black inequities in housing, education, and incarceration) is associated with racial inequities in fatal police shootings,33 access to health care,34 myocardial infarction,35 adverse birth outcomes,36 BMI,37 and circulatory disease–related deaths34 among Black U.S. Americans.
In addition to structural racism research, studies that have examined the effects of anti-LGBTQ policies (e.g., laws restricting public services to sexual and gender minorities) have demonstrated associations between state-level oppression and negative health outcomes among predominantly White sexual minority communities in the U.S. These include links to psychological distress,25 generalized anxiety disorder,26 post-traumatic stress disorder,26 illicit substance use,27 drinking,28 lower awareness and engagement in biomedical HIV prevention,29 and higher odds of sexual HIV risk.29 Critically, studies have even found associations between structural anti-LGBTQ policies and severe psychological distress indicators like suicide attempts.30,31 In addition, a recent study found that anti-LGBTQ and antiimmigrant policies interacted to predict HIV risk and prevention among SMM in European countries.32 This important research notwithstanding, the authors are unaware of any studies that have investigated U.S. state-level structural racism and anti-LGBTQ policies as independent and conjoint drivers of psychological and behavioral health inequities for Black SMM.9
To promote the explanation and rectification of persistent health inequities facing Black SMM in the U.S., this study tests associations between state-level indicators of structural racism and anti-LGBTQ policies and anxiety symptoms, depressive symptoms, perceived burdensomeness (a psychological precursor to suicidality),38 heavy drinking, and HIV testing among Black and White SMM. Given evidence that structural racism is associated with negative health outcomes within Black communities, but has null or beneficial effects for White communities,35 researchers hypothesize that there are negative associations between structural racism and HIV testing, and positive associations with anxiety symptoms, depressive symptoms, perceived burdensomeness, and heavy drinking only among Black SMM. Given evidence illustrating the harmful psychological and behavioral effects of anti-LGBTQ laws for SMM,26–31 researchers hypothesize that there are associations between anti-LGBTQ policies and worse health outcomes for both White and Black SMM. Finally, in alignment with intersectionality frameworks18–20 and empirical findings,39,40 researchers hypothesize that structural racism and anti-LGBTQ policies are synergistic for Black SMM, such that living in states with higher levels of both forms of oppression is associated with exponentially higher levels of the aforementioned psychological and behavioral health outcomes.
METHODS
Study Sample
The study’s sample drew from the baseline data of Understanding New Infections through Targeted Epidemiology study (UNITE), a national longitudinal cohort study with SMM to better understand risk factors for HIV infection.41 Recruitment and data collection occurred from 2017 to 2018. Analyses occurred from 2019 to 2020. The study team recruited a non-random purposive sample through advertisements on geosocial networking apps, social media sites, and e-mail blasts. Interested respondents completed a brief online screener that assessed eligibility criteria, including: being aged ≥16 years, identifying as male (including transmen), not reporting heterosexual identity, reporting HIV-negative or unknown status, reporting using any app to find sex partner(s), and sexual HIV risk in the past 6 months. Additional information on eligibility criteria can be found in the UNITE methods manuscript.41
Following the screener, participants provided informed consent online and completed an online survey assessing stress, psychosocial variables, and HIV risk. Participants received a $25 gift card for completing the baseline. The City University of New York IRB approved all study procedures.
In total, 3,982 Black SMM and 11,616 White SMM were eligible to participate and provided contact information. Of these, 1,439 (36.1%) Black and 5,656 (48.7%) White SMM completed the enrollment survey. The analytic sample consisted of the 1,379 Black and 5,537 White SMM participants who identified as non-Hispanic Black/African American only (i.e., not multiracial; n=1,439) or White only (i.e., not multiracial; n=5,656), were not living with HIV (Black: n=1,403; White: n=5,600), had a State Racism Index score because they did not live in Washington, District of Columbia or Puerto Rico (Black: n=1,386; White: n=5,564), and did not have missing data for any model covariates (Black: n=1,379; White: n=5,537). Models excluded cases missing on covariates because estimating them as endogenous in the models would have imposed a distributional assumption of normality,42 which was untenable for categorical (e.g., income) and positively skewed (e.g., age) covariates. Participants excluded for covariate missingness did not significantly differ on any primary study variables from those that were included.
Measures
Participants reported sociodemographic information, including: subjective social status,43 income, formal employment status, insurance status, recent housing instability, age, sexual identity, gender identity, relationship status, sexual identity outness, sexual positioning, and whether they were sexually active. A Rural–Urban Commuting Area44 measure of rural–urban classification and commuting was calculated using participant addresses.
The State Racism Index measured structural racism, a metric created to capture statewide racism on a scale from 0 to 100 on the following dimensions: residential segregation, incarceration rates, educational attainment, economic indicators, and employment status.33 Composite scores across these dimensions ranged from 25.9 to 74.9, with higher values indicating more racism. The State Racism Index is available for 50 states, excluding Washington, District of Columbia and Puerto Rico. Additional information on the calculation and validity of this variable is available in its original publication.33
The Human Rights Campaign’s 2018 State Equality Index45 measured anti-LGBTQ policies. The State Equality Index is based on statewide anti-LGBTQ policies (e.g., HIV/AIDS criminalization; permitting hate crimes, conversion therapy, and discrimination in housing, employment, and public accommodations). States are grouped into 4 categories where lower values indicate more anti-LGBTQ policies (1=high priority to receive basic equality to 4=working toward innovative equality). Because >94% of participants were in states that received the highest or lowest score, the scale was dichotomized. All estimates in the results are reversed for interpretability.
Participants completed the anxiety items of the Brief Symptom Inventory46 assessing past-week anxiety symptoms. Response options ranged from 0 (not at all) to 4 (extremely). Models included items as indicators of an anxiety symptoms latent variable. The scale showed good internal consistency (α=0.91).
Participants completed the 10-item Center for Epidemiological Studies Depression scale.47 Response options ranged from 0 (rarely or none of the time) to 3 (most or all of the time). Consistent with past research on the scale’s factor structure,48 models included subscale means across negative (depressed) affect and reverse-scored positive affect subscales. Models included subscale means as indicators of a depressive symptom latent variable. The scale showed good internal consistency (α=0.85).
The Interpersonal Needs Questionnaire assessed perceived burdensomeness, a proximal cause of suicidal desire.38 Response options ranged from 1 (not at all true for me) to 7 (very true for me). Models included the perceived burdensomeness subscore as a mean across 6 items. The scale demonstrated good internal consistency (α=0.94).
The 3-item Alcohol Use Disorders Identification Test-Consumption assessed heavy drinking.49 Each item has a unique 5-point scale with higher scores indicating higher levels of heavy drinking. Consistent with past research showing meaningful variation in drinking problems across the composite of the three scale items,50 models included a summed continuous outcome. The scale demonstrated acceptable internal consistency (α=0.78).
Participants responded to a single item: How often do you typically get tested for HIV? Response options were on a 7-point scale (0=never, 1=less than once a year, 2=about once a year, 3=once every six months, 4=once every three months, 5=once a month, 6=more than once a month).
Statistical Analysis
Structural equation modeling analyzed multiple associations simultaneously while accounting for measurement error.51 Confirmatory factor analyses assessed latent depressive and anxiety symptoms variables run within Mplus version 8.6. Accepted model fit indices including chi-square, comparative fit index (CFI), Tucker–Lewis index (TLI), and root mean square error of approximation (RMSEA) that assessed the appropriateness of models and together account for important model fit factors (e.g., sample size, number of freely estimated parameters).52 Independent but equivalent Black and White SMM structural equation models assessed hypothesized pathways. Models included main and interaction effects of the continuous structural racism and dichotomous anti-LGBTQ policies variables on latent anxiety and depressive symptoms variables and observed perceived burdensomeness, heavy drinking, and HIV testing variables. Models included interaction effects using an interaction term between the centered structural racism variable and the anti-LGBTQ policies variable. Models adjusted for theoretically meaningful contextual and individual covariates, including: rural–urban classification, SES, income, education, employment, insurance status, housing instability, age, sexual identity, gender identity, and relationship status. Given their relevance for HIV testing specifically, models adjusted for sexual activity, sexual identity outness, and sexual positioning. Models specified the manifest anxiety latent variable indicators as ordinal and used a variance-adjusted weighted least squares estimator. Observations were clustered by state to adjust for non-independence due to nesting within states. All data were complete other than income (99%), perceived burdensomeness (97%), HIV testing (95%), and depressive and anxiety symptoms (92%). Full information maximum likelihood estimation under the assumption that data were missing at random accounted for missing data,53 which was tenable given there was no reason to expect systematic differences in the dependent variables based on missingness patterns.54
RESULTS
Table 1 includes the sample’s sociodemographic characteristics. Most participants were gay-identified (81%), single (74%), and college-educated (42%). Overall, this sample was younger (Mean age=34 years) and more formally educated, albeit with lower income, than average U.S. SMM communities.55 Figure 1 depicts the national distribution of the sample and the structural racism and anti-LGBTQ policies scores by state. Correlations and descriptives among model variables are in Appendix Table 1.
Table 1.
Demographic Characteristics of Study Sample
| Characteristic | Total (n=6,916) | Black men (n=1,379) | White men (n=5,537) |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Sexual identity | χ2(2)=41.15, p<0.001 | ||
| Gay | 5,608 (81.1) | 1,040 (75.4) | 4,568 (82.5) |
| Queer | 165 (2.4) | 32 (2.3) | 133 (2.4) |
| Bisexual | 1,143 (16.5) | 307 (22.3) | 836 (15.1) |
| Gender identity | χ2(1)=6.23, p<0.05 | ||
| Cisgender man | 6,858 (99.2) | 1,375 (99.7) | 5,483 (99.0) |
| Transgender man | 58 (0.8) | 4 (0.3) | 54 (1.0) |
| Formal educational attainment | χ2(3)=76.44, p<0.001 | ||
| High school diploma, GED, or less | 1,162 (16.8) | 274 (19.9) | 888 (16.0) |
| Some college or Associate’s degree | 2,889 (41.8) | 675 (48.9) | 2,214 (40.0) |
| 4-year college degree | 1,810 (26.2) | 286 (20.7) | 1,524 (27.5) |
| Graduate school | 1,055 (15.3) | 144 (10.4) | 911 (16.5) |
| Formal employment status | χ2(2)=20.36, p<0.001 | ||
| Unemployed, student, disability | 1,181 (17.1) | 255 (18.5) | 926 (16.7) |
| Part-time (<40 hours/week) | 1,298 (18.8) | 308 (22.3) | 990 (17.9) |
| Full-time (≥40 hours/week) | 4,437 (64.2) | 816 (59.2) | 3,621 (65.4) |
| Income | χ2(3)=119.86, p<0.001 | ||
| <$20,000 | 2,186 (31.6) | 544 (39.8) | 1,642 (29.9) |
| $20,000‒$49,999 | 2,763 (40.0) | 588 (43.0) | 2,175 (39.6) |
| $50,000‒$74,999 | 1,010 (14.6) | 156 (11.4) | 854 (15.6) |
| ≥$75,000 | 894 (12.9) | 78 (5.7) | 816 (14.9) |
| Subjective social status | χ2(4)=26.58, p<0.001 | ||
| 1‒2 | 180 (2.6) | 43 (3.1) | 137 (2.5) |
| 3‒4 | 1,198 (17.3) | 249 (18.1) | 949 (17.1) |
| 5‒6 | 2,738 (39.6) | 605 (43.9) | 2,133 (38.5) |
| 7‒8 | 2,473 (35.8) | 438 (31.8) | 2,035 (36.8) |
| 9‒10 | 327 (4.7) | 44 (3.2) | 283 (5.1) |
| Insured | χ2(2)=93.05, p<0.001 | ||
| No | 1,299 (18.8) | 352 (25.5) | 947 (17.1) |
| Yes | 5,510 (79.7) | 981 (71.1) | 4,529 (81.8) |
| Unknown | 107 (1.5) | 46 (3.3) | 61 (1.1) |
| Housing instability | χ2(1)=12.40, p<0.001 | ||
| No | 6,323 (91.4) | 1,228 (89.1) | 5,095 (92.0) |
| Yes | 593 (8.6) | 151 (10.9) | 442 (8.0) |
| Relationship status | χ2(1)=35.51, p<0.001 | ||
| Single | 5,089 (73.6) | 1,102 (79.9) | 3,987 (72.0) |
| Partnered | 1,827 (26.4) | 277 (20.1) | 1,550 (28.0) |
| Outness | χ2(3)=120.36, p<0.001 | ||
| Not at all | 441 (6.4) | 106 (7.7) | 335 (6.1) |
| Somewhat | 1,211 (17.5) | 355 (25.7) | 856 (15.5) |
| Mostly | 1,696 (24.5) | 368 (26.7) | 1,328 (24.0) |
| Completely | 3,568 (51.6) | 550 (39.9) | 3,018 (54.5) |
| Sexually active | χ2(1)=54.23, p<0.001 | ||
| No | 492 (7.1) | 161 (11.7) | 331 (6.0) |
| Yes | 6,424 (92.9) | 1,218 (88.3) | 5,206 (94.0) |
| Age, mean (SD) | t(6,914)= −13.54, p<0.001 | ||
| Range: 68, Median=31) | 34.03 (12.26) | 30.08 (9.24) | 35.01 (12.71) |
| Rural—urban classification, mead (SD) | t(6,914)= −6.10,p<0.001 | ||
| Range:9.4, Median=1) | 1.63 (1.61) | 1.39 (1.25) | 1.69 (1.69) |
Note: The total n for income does not equal 100% because participants under 18 were not asked.
Figure 1.
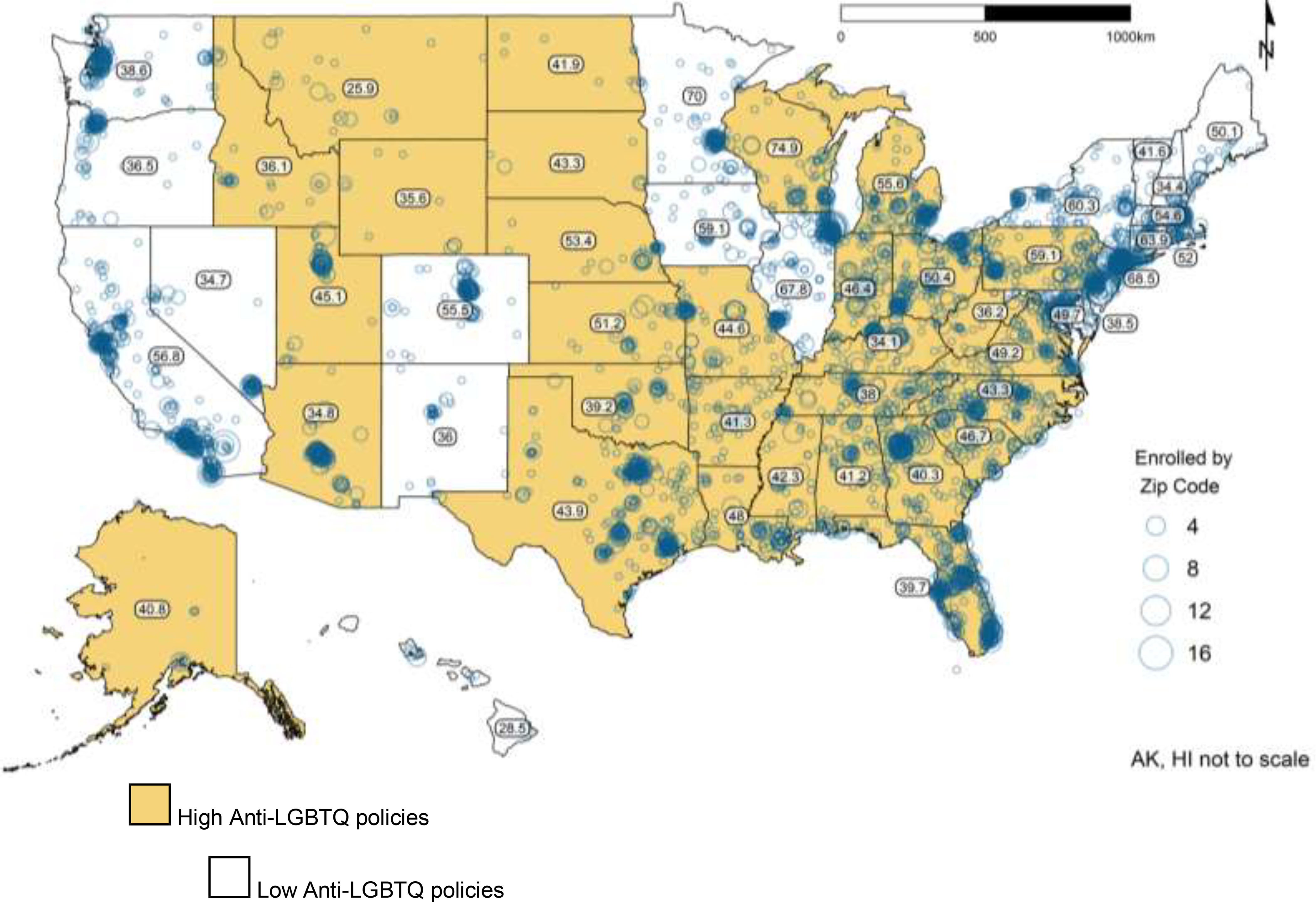
National distribution of participants in the analytic sample.
Note: Numbers within states correspond to the State Racism Index Score. Participants in Puerto Rico and Washington DC not included in the analytic sample.
LGBTQ, lesbian, gay, bisexual, transgender, queer.
Regarding latent variable specification, confirmatory factor analysis indicated that a 6-item 1-factor specification of anxiety symptoms fit the data adequately for Black participants (χ2[9]=74.06, p≤0.001; CFI=1.00, TLI=0.99, RMSEA=0.08) and White participants (χ2[9]=510.91, p≤0.001; CFI=0.99, TLI=0.99, RMSEA=0.10). Standardized factor loadings ranged from 0.62 to 0.84. For depressive symptoms, although it is not possible to consult fit statistics with an under-identified 2-indicator model, standardized factor loadings were 0.59–0.74.
Figure 2 depicts the primary model for Black and White participants. Indices suggested good fit for Black (χ2[192]=363.00, p≤0.001; CFI=0.98, TLI=0.97, RMSEA=0.03) and White participants (χ2[192]=985.31, p≤0.001; CFI=0.98, TLI=0.97, RMSEA=0.03). Among Black participants, structural racism was positively associated with anxiety (β=0.20, SE=0.10, p=0.04), perceived burdensomeness (β=0.42, SE=0.09, p≤0.001), and heavy drinking (β=0.23, SE=0.10, p=0.01). Anti-LGBTQ policies were positively associated with anxiety (β=0.08, SE=0.04, p=0.03), perceived burdensomeness (β=0.20, SE=0.04, p≤0.001), and heavy drinking (β=0.10, SE=0.04, p=0.01), and negatively associated with HIV testing (β= −0.14, SE=0.07, p=0.04). The interaction term was positively associated with perceived burdensomeness (β=0.38, SE=0.08, p≤0.001) and heavy drinking (β=0.22, SE=0.07, p=0.003). These interactions are depicted in Figure 3. The plots show that the positive associations from structural racism to perceived burdensomeness and heavy drinking were stronger at high levels of anti-LGBTQ policies. No other associations were significant for Black participants. Neither of the oppression variables was significantly associated with health outcomes for White SMM (Figure 2).
Figure 2.
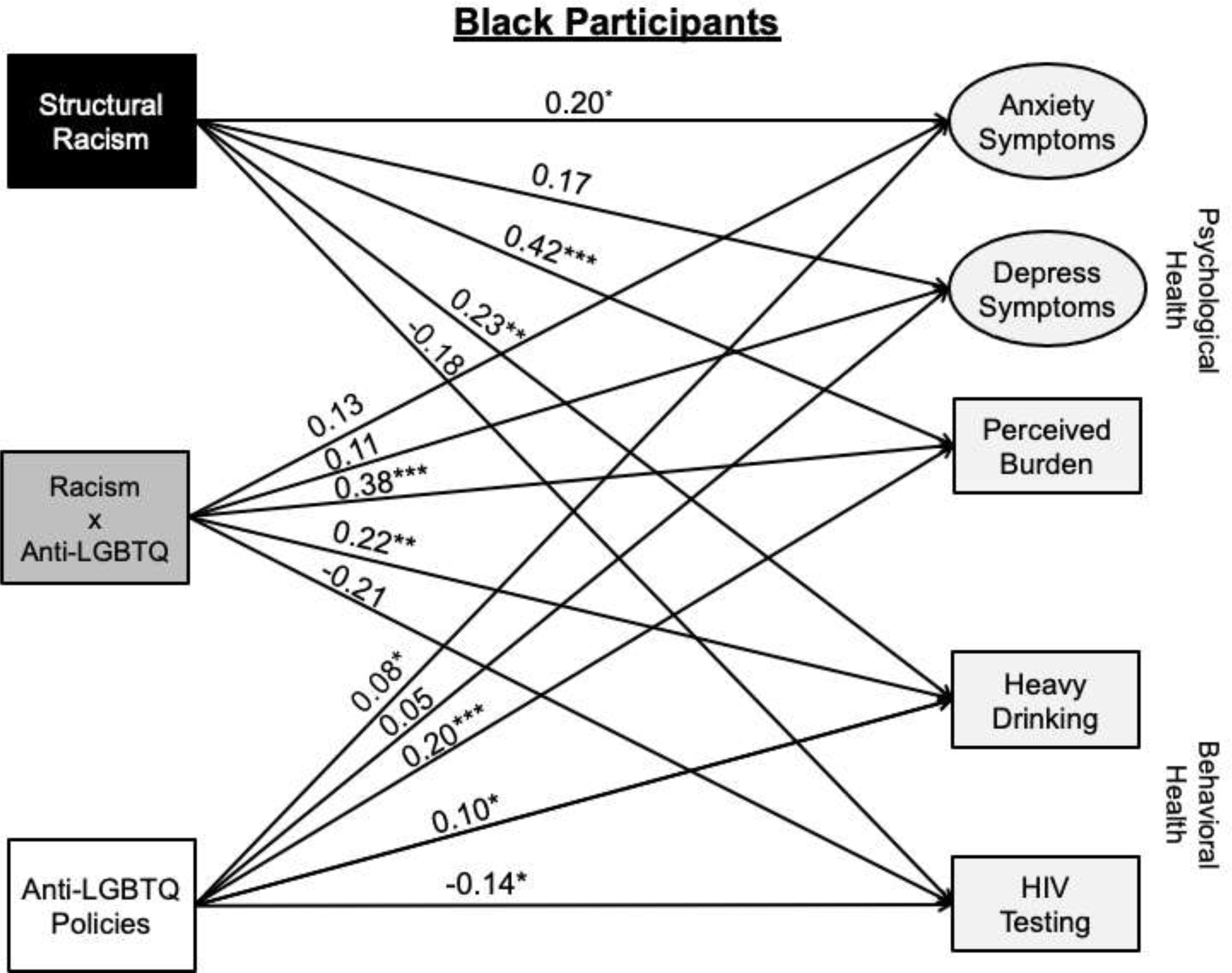
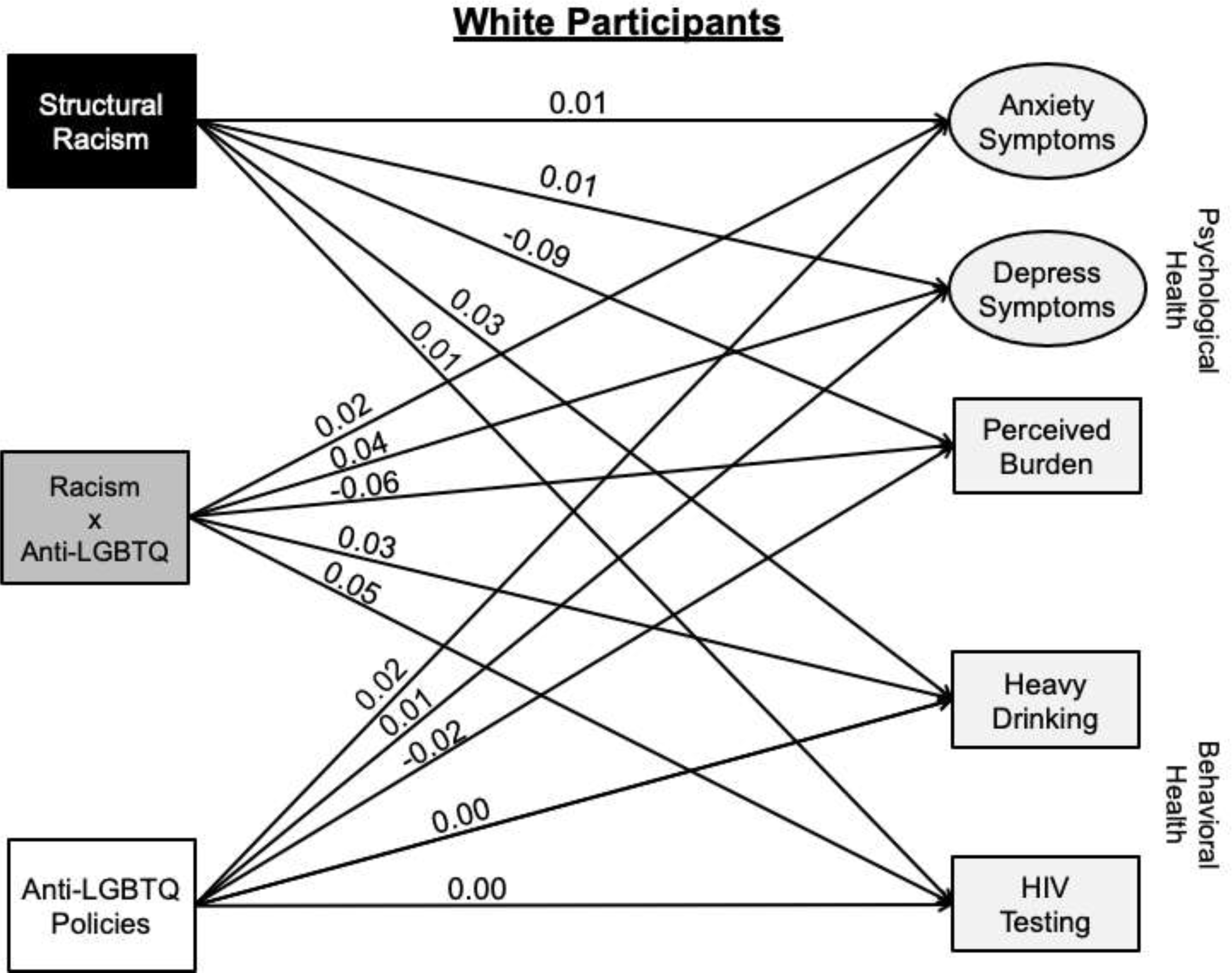
Structural equation models with structural racism and anti-LGBTQ policies predicting psychological and behavioral outcomes for Black and White SMM.
Note: ***p≤0.001; **p≤0.01; *p≤0.05; †p≤0.10. Standardized estimates. Depress symptom= Depressive symptoms. This model is adjusted for rural-urban classification, subjective SES, income, formal employment status, insurance status, housing instability, age, sexual identity, gender identity, relationship status, sexual activity (HIV testing), sexual identity outness (HIV testing), and sexual positioning (HIV testing).
LGBTQ, lesbian, gay, bisexual, transgender, queer; SMM, sexual minority men.
Figure 3.
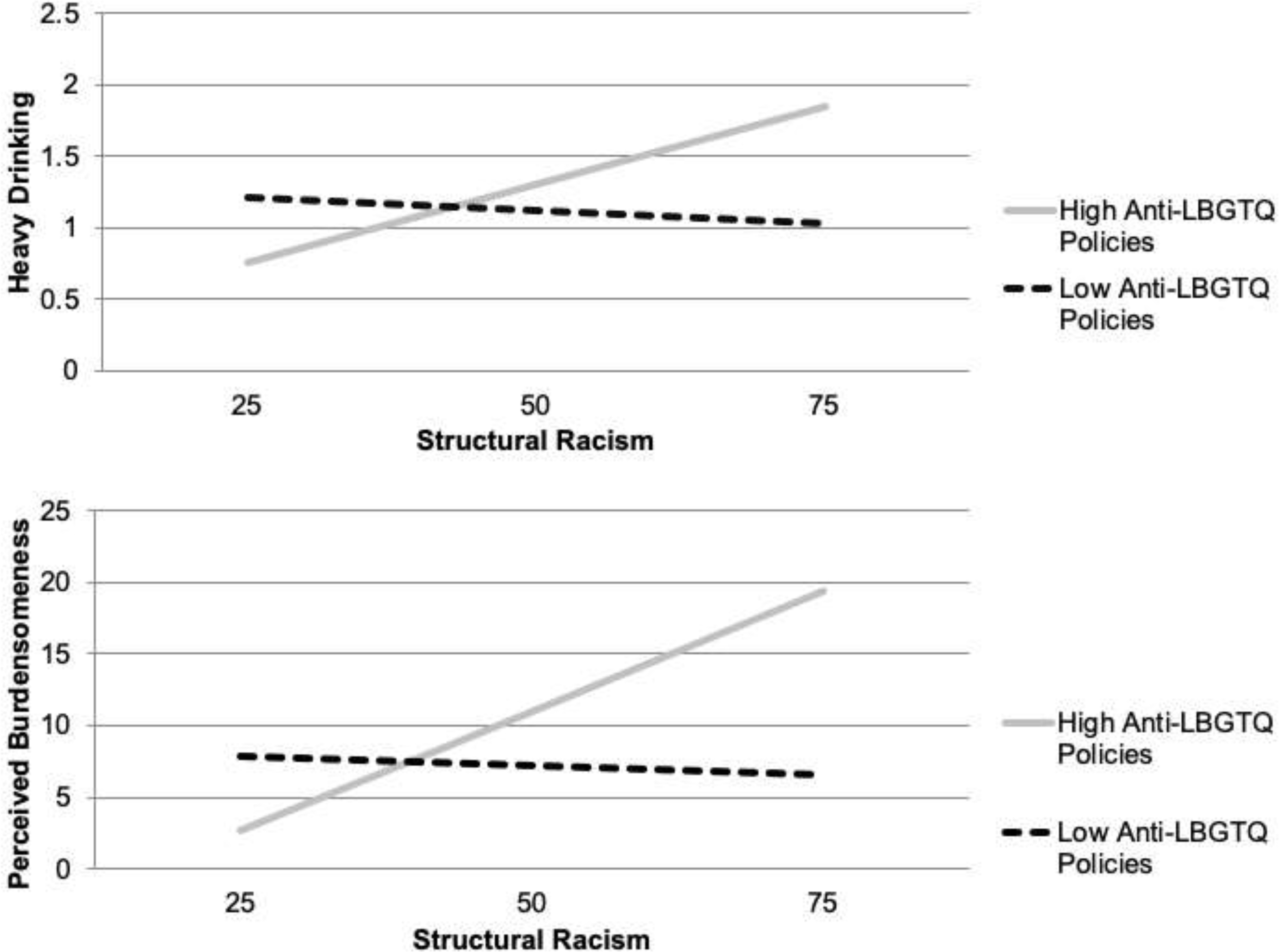
Interactions between structural racism and anti-LGBTQ policies on heavy drinking and perceived burdensomeness among Black SMM.
LGBTQ, lesbian, gay, bisexual, transgender, queer; SMM, sexual minority men.
DISCUSSION
This study examined associations between U.S. state-level structural racism and anti-LGBTQ policies and psychological and behavioral health outcomes among Black and White SMM. Results showed that among Black SMM, structural racism and anti-LGBTQ policies were both independently positively associated with higher anxiety symptoms, perceived burdensomeness, and heavy drinking. Additionally, anti-LGBTQ policies were negatively associated with HIV testing. Critically, among Black SMM, participants living in states with high levels of both structural racism and anti-LGBTQ policies showed exponentially higher levels of perceived burdensomeness and heavy drinking than participants in states with lower levels of structural oppression. Among White SMM, there were no associations between either form of structural oppression and health outcomes. Overall, these results highlight the intersectional nature of structural oppression and suggest that, to address health inequities facing Black SMM like those in chronic psychological conditions2 and HIV,3 racist and anti-LGBTQ policies must be redressed.
The finding that structural racism was associated with negative psychological outcomes and substance use among Black SMM, including precursors to suicidality (i.e., perceived burdensomeness, heavy drinking), is consistent with extant research with Black participants broadly.10,33–36 That structural racism was not significantly associated with any health outcomes for White SMM also conforms with evidence that state-level structural racism has a null or positive effect for White residents.35 This highlights how structural racism uplifts the health of White communities at the expense of Black communities in the U.S.17
The finding that anti-LGBTQ policies were associated with negative psychological and behavioral health outcomes among Black, but not White, SMM suggests this oppression may disproportionately affect Black SMM communities. This was contrary to the hypothesis that anti-LGBTQ policies would be associated with negative health outcomes for White SMM, as found in past studies with predominantly White samples.25–29 This result may reflect the reality that anti-LGBTQ laws, like HIV criminalization, are often disproportionately enforced against Black SMM relative to White SMM.56 As such, it appears that anti-LGBTQ policies are uniquely harmful for Black SMM and may underlie racial health inequities among SMM.2,3 This is critical given studies often highlight racial health inequities among SMM without also highlighting the structural oppression that causes them.57 Given these results, state-level policies like the prohibition of hate crimes and LGBTQ+ discrimination in employment, housing, and public accommodations, which dozens of states have not passed, may uniquely benefit Black SMM.21
The result showing that the interaction between structural racism and anti-LGBTQ policies was positively associated with perceived burdensomeness and heavy drinking supports intersectionality frameworks18–20 and recent evidence for the effects of intersectional oppression among Black SMM. 40,58,59 Specifically, the results suggest that to reduce inequities in individual-level psychological and behavioral distress among Black SMM, scientists, practitioners, and policymakers must uproot interlocking structural oppression from racist and anti-LGBTQ policies that drive inequities in housing, education, and incarceration. This stands in contrast to public health interventions with Black SMM that seek to reduce health inequities through individual-level psychological/behavioral intervention only.57 Findings suggest clinicians may effectively combat the negative health effects of structural oppression by screening for exposure among Black SMM,60,61 while also supporting community-led policy advocacy.62 This includes supporting policies that invest in reparations to promote Black LGBTQ health, wealth, and education63 and advocating for the repeal of stop-and-frisk policing and drug criminalization laws21 that mass incarcerate Black LGBTQ communities.
Research building on the present findings can look to replicate these results to ensure they are not driven by unique data patterns and examine mechanisms accounting for the associations between structural racism, anti-LGBTQ policies, and health outcomes. Researchers, policymakers, and clinicians should also consider the public health needs of Black SMM living in states where structural racism and anti-LGBTQ policies are most impactful (e.g., racially segregated Midwestern cities).18,23,24 Finally, given this study did not find associations between structural oppression and depressive symptoms, future studies can examine this further.
Limitations
This is one of few studies that has examined structural oppression and Black SMM’s health and the first, to the authors’ knowledge, to examine how different forms of structural oppression intersect to predict health among a national sample of Black SMM. These strengths notwithstanding, several limitations are worth noting. First, the study sample was connected to sexual networking apps and younger, with more formal education, and lower income than the average U.S. SMM community,55 which may limit generalizability. Second, the measure of anti-LGBTQ policies did not disentangle policies targeting different groups within LGBTQ communities, which may not have targeted some participants (e.g., anti-trans bathroom laws). Additionally, the structural racism and anti-LGBTQ policies indices were related, but not directly comparable, as the latter is based on specific policies (e.g., HIV criminalization), whereas the former is based on proximal indicators of policies (e.g., incarceration inequities). There also was a difference in the measurement years of the 2018 anti-LGBTQ index, and the structural racism index, which is based on Census and government data from 2010 to 2015. Although these indices are often highly consistent across time,10 future research may benefit from multiyear longitudinal models that examine changes in structural racism and anti-LGBTQ policies.25,31
CONCLUSIONS
These findings highlight the importance of policies as a sources of oppression for individuals at the intersections of stigmatized social positions and support eliminating racist and anti-LGBTQ policies as essential interventions to promote health equity among Black SMM.10,45
Supplementary Material
ACKNOWLEDGMENTS
We would like to thank the participants who volunteered their time, without whom this study would not have been possible. We would like to thank all the staff, students, and volunteers who made this study possible, particularly those who worked closely on the study: Trinae Adebayo, Juan Castiblanco, Jorge Cienfuegos Szalay, Ruben Jimenez, Scott Jones, Jonathan López Matos, Nico Tavella, and Brian Salfas. We would also like to thank our collaborators, Carlos Rodriguez-Díaz and Brian Mustanski. This study was supported by research grants from the National Institute of Allergy and Infectious Diseases, National Institute of Child Health and Human Development, and National Institute on Mental Health (UG3-AI133674, Principal Investigator: Rendina; K01-MH118091, Principal Investigator: English) and we are grateful for the work of the NIH staff who supported these grants, particularly Gerald Sharp, Sonia Lee, Michael Stirratt, and Gregory Greenwood. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
No financial disclosures were reported by the authors of this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.American Psychological Association, APA Working Group on Health Disparities in Boys and Men. Health disparities racial/ethnic and sexual minority boys and men. http://www.apa.org/pi/health-disparities/resources/race-sexuality-men.aspx. Published 2018. Accessed September 28, 2019.
- 2.Half of Black gay men and a quarter of Latino gay men projected to be diagnosed within their lifetime. Centers for Disease Control and Prevention. https://www.cdc.gov/nchhstp/newsroom/2016/croi-press-release-risk.html. Published 2016. Accessed December 27, 2019. [Google Scholar]
- 3.HIV and African American Gay and Bisexual Men. Centers for Disease Control and Prevention. https://www.cdc.gov/hiv/group/msm/bmsm.html. Published 2018. Accessed December 4, 2018. [Google Scholar]
- 4.Wade RM, Harper GW. Young Black gay/bisexual and other men who have sex with men: a review and content analysis of health-focused research between 1988 and 2013. Am J Mens Health. 2015;11(5):1388–1405. 10.1177/1557988315606962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Millett GA, Flores SA, Peterson JL, Bakeman R. Explaining disparities in HIV infection among black and white men who have sex with men: a meta-analysis of HIV risk behaviors. AIDS. 2007;21(15):2083–2091. 10.1097/qad.0b013e3282e9a64b. [DOI] [PubMed] [Google Scholar]
- 6.Leyva B, Persoskie A, Ottenbacher A, et al. Do men receive information required for shared decision making about PSA testing? Results from a National Survey. J Cancer Educ. 2016;31(4):693–701. 10.1007/s13187-015-0870-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moses KA, Orom H, Brasel A, Gaddy J, Underwood W. Racial/ethnic disparity in treatment for prostate cancer: does cancer severity matter? Urology. 2017;99:76–83. 10.1016/j.urology.2016.07.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.American Psychological Association Working Group on Health Disparities in Boys and Men. Health disparities in racial/ethnic and sexual minority boys and men. http://www.apa.org/pi/health-disparities/resources/race-sexuality-men.aspx. Published 2018. Accessed February 26, 2019.
- 9.Hatzenbuehler ML. Structural stigma: research evidence and implications for psychological science. Am Psychol. 2016;71(8):742–751. 10.1037/amp0000068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hardeman RR, Murphy KA, Karbeah JM, Kozhimannil KB. Naming institutionalized racism in the public health literature: a systematic literature review. Public Health Rep. 2018;133(3):240–249. 10.1177/0033354918760574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Delgado R, Stefancic J. Critical Race Theory: An Introduction. New York, NY: NYU Press; 2017. [Google Scholar]
- 12.Bowleg L “Once you’ve blended the cake, you can’t take the parts back to the main ingredients”: Black gay and bisexual men’s descriptions and experiences of intersectionality. Sex Roles. 2013;68(11‒12):754–767. 10.1007/s11199-012-0152-4. [DOI] [Google Scholar]
- 13.Jagose A Queer Theory: An Introduction. New York, NY: NYU Press; 1996. [Google Scholar]
- 14.Link BG, Phelan JC. Conceptualizing stigma. Annu Rev Sociol. 2001;27(1):363–385. 10.1146/annurev.soc.27.1.363. [DOI] [Google Scholar]
- 15.Williams D R, Williams-Morris R Racism and mental health: the African American experience. Ethn Health. 2000;5(3‒4):243–268. 10.1080/713667453. [DOI] [PubMed] [Google Scholar]
- 16.Carmichael S, Ture K, Hamilton CV. Black power: the politics of liberation in America. New York, NY: Vintage; 1992. [Google Scholar]
- 17.Feagin J Systemic racism: A theory of oppression. Philadelphia, PA: Routledge; 2013. [Google Scholar]
- 18.Bowleg L The problem with the phrase women and minorities: intersectionality-an important theoretical framework for public health. Am J Public Health. 2012;102(7):1267–1273. 10.2105/ajph.2012.300750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Crenshaw K Demarginalizing the intersection of race and sex: A black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. University of Chicago Legal Forum; 1989:139. 10.4324/9780429500480-5. [DOI] [Google Scholar]
- 20.Collins PH. Black Feminist Thought: Knowledge, Consciousness, and the Politics of Empowerment. Philadelphia, PA: Routledge; 2002. [Google Scholar]
- 21.Unjust: How the broken criminal justice system fails LGBT people of color. Movement Advancement Project, Center for American Progress. http://www.lgbtmap.org/policy-and-issue-analysis/criminal-justice-poc. Published 2016. Accessed March 3, 2019. [Google Scholar]
- 22.Clark R, Anderson NB, Clark VR, Williams DR. Racism as a stressor for African Americans: a biopsychosocial model. Am Psychol. 1999;54(10):805–816. 10.1037/0003-066x.54.10.805. [DOI] [PubMed] [Google Scholar]
- 23.Kapilashrami A, Hankivsky O. Intersectionality and why it matters to global health. Lancet. 2018;391(10140):2589–2591. 10.1016/s0140-6736(18)31431-4. [DOI] [PubMed] [Google Scholar]
- 24.Evans CR. Modeling the intersectionality of processes in the social production of health inequalities. Soc Sci Med. 2019;226:249–253. 10.1016/j.socscimed.2019.01.017. [DOI] [PubMed] [Google Scholar]
- 25.Raifman J, Moscoe E, Austin SB, Hatzenbuehler ML, Galea S. Association of state laws permitting denial of services to same-sex couples with mental distress in sexual minority adults: a difference-in-difference-in-differences analysis. JAMA Psychiatry. 2018;75(7):671–677. 10.1001/jamapsychiatry.2018.0757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hatzenbuehler ML, Keyes KM, Hasin DS. State-level policies and psychiatric morbidity in lesbian, gay, and bisexual populations. Am J Public Health. 2009;99(12):2275–2281. 10.2105/ajph.2008.153510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hatzenbuehler ML, Jun H-J, Corliss HL, Bryn Austin S. Structural stigma and sexual orientation disparities in adolescent drug use. Addict Behav. 2015;46:14–18. 10.1016/j.addbeh.2015.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pachankis JE, Hatzenbuehler ML, Starks TJ. The influence of structural stigma and rejection sensitivity on young sexual minority men’s daily tobacco and alcohol use. Soc Sci Med. 2014;103:67–75. 10.1016/j.socscimed.2013.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Oldenburg CE, Perez-Brumer AG, Hatzenbuehler ML, et al. State-level structural sexual stigma and HIV prevention in a national online sample of HIV-uninfected MSM in the United States. AIDS. 2015;29(7):837–845. 10.1097/qad.0000000000000622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hatzenbuehler ML, Keyes KM. Inclusive anti-bullying policies and reduced risk of suicide attempts in lesbian and gay youth. J Adolesc Health. 2013;53(1 suppl):S21–S26. 10.1016/j.jadohealth.2012.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Raifman J, Moscoe E, Austin SB, McConnell M. Difference-in-differences analysis of the association between state same-sex marriage policies and adolescent suicide attempts. JAMA Pediatr. 2017;171(4):350–356. 10.1001/jamapediatrics.2016.4529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pachankis JE, Hatzenbuehler ML, Berg RC, et al. Anti-LGBT and anti-immigrant structural stigma: an intersectional analysis of sexual minority men’s HIV risk when migrating to or within Europe. J Acquir Immune Defic Syndr. 2017;76(4):356–366. 10.1097/qai.0000000000001519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mesic A, Franklin L, Cansever A, et al. The relationship between structural racism and Black-White disparities in fatal police shootings at the state level. J Natl Med Assoc. 2018;110(2):106–116. 10.1016/j.jnma.2017.12.002. [DOI] [PubMed] [Google Scholar]
- 34.Leitner JB, Hehman E, Ayduk O, Mendoza-Denton R. Blacks’ death rate due to circulatory diseases is positively related to whites’ explicit racial bias: a nationwide investigation using project implicit. Psychol Sci. 2016;27(10):1299–1311. 10.1177/0956797616658450. [DOI] [PubMed] [Google Scholar]
- 35.Lukachko A, Hatzenbuehler ML, Keyes KM. Structural racism and myocardial infarction in the United States. Soc Sci Med. 2014;103:42–50. 10.1016/j.socscimed.2013.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wallace ME, Mendola P, Liu D, Grantz KL. Joint effects of structural racism and income inequality on small-for-gestational-age birth. Am J Public Health. 2015;105(8):1681–1688. 10.2105/ajph.2015.302613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dougherty GB, Golden SH, Gross AL, Colantuoni E, Dean LT. Measuring structural racism and its association with BMI. Am J Prev Med. 2020;59(4):530–537. 10.1016/j.amepre.2020.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Van Orden KA, Cukrowicz KC, Witte TK, Joiner TE. Thwarted belongingness and perceived burdensomeness: construct validity and psychometric properties of the Interpersonal Needs Questionnaire. Psychol Assess. 2012;24(1):197–215. 10.1037/a0025358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jackson-Best F, Edwards N. Stigma and intersectionality: a systematic review of systematic reviews across HIV/AIDS, mental illness, and physical disability. BMC Public Health. 2018;18:919. 10.1186/s12889-018-5861-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Quinn K, Bowleg L, Dickson-Gomez J. “The fear of being Black plus the fear of being gay”: the effects of intersectional stigma on PrEP use among young Black gay, bisexual, and other men who have sex with men. Soc Sci Med. 2019;232:86–93. 10.1016/j.socscimed.2019.04.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rendina HJ, Talan AJ, Tavella NF, et al. Leveraging technology to blend large-scale epidemiologic surveillance with social and behavioral science methods: successes, challenges, and lessons learned implementing the UNITE longitudinal cohort study of sexual minority men at risk for HIV in the U.S. Am J Epidemiol. In Press. Online October 15, 2020. 10.1093/aje/kwaa226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Marcoulides GA, Schumacker RE. Advanced structural equation modeling: Issues and techniques. Hove, UK: Psychology Press; 1996. [Google Scholar]
- 43.Adler N, Stewart J. The MacArthur scale of subjective social status. https://macses.ucsf.edu/research/psychosocial/subjective.php. Published 2007. Accessed September 28, 2019.
- 44.Rural-Urban Commuting Area Codes U.S. Department of Agriculture, Economic Research Service. https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes. Accessed September 28, 2019. [Google Scholar]
- 45.Warbelow S, Oakley C, Kutney C. 2018 State Equality Index. Washington, DC: Human Rights Campaign Foundation; 2018. [Google Scholar]
- 46.Derogatis LR, Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychol Med. 1983;13(3):595–605. 10.1017/s0033291700048017. [DOI] [PubMed] [Google Scholar]
- 47.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D. Am J Prev Med. 1994;10(2):77–84. 10.1016/s0749-3797(18)30622-6. [DOI] [PubMed] [Google Scholar]
- 48.Zhang W, O’Brien N, Forrest JI, et al. Validating a shortened depression scale (10 item CES-D) among HIV-positive people in British Columbia, Canada. PloS One. 2012;7(7):e40793. 10.1371/journal.pone.0040793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Arch Intern Med. 1998;158(16):1789–1795. 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- 50.Rubinsky AD, Dawson DA, Williams EC, Kivlahan DR, Bradley KA. AUDIT-C scores as a scaled marker of mean daily drinking, alcohol use disorder severity, and probability of alcohol dependence in a U.S. general population sample of drinkers. Alcohol Clin Exp Res. 2013;37(8):1380–1390. 10.1111/acer.12092. [DOI] [PubMed] [Google Scholar]
- 51.Kaplan D Structural Equation Modeling. In: Smelser NJ, Baltes PB, eds. International Encyclopedia of the Social & Behavioral Sciences. Oxford, UK: Pergamon; 2001:15215–15222. 10.1016/b0-08-043076-7/00776-2. [DOI] [Google Scholar]
- 52.Lt Hu, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6(1):1–55. 10.1080/10705519909540118. [DOI] [Google Scholar]
- 53.Willett JB, Sayer AG, Schumacher R, Marcoulides G. Advanced structural equation modeling techniques. New York, NY: Taylor & Francis; 1996. [Google Scholar]
- 54.Bhaskaran K, Smeeth L. What is the difference between missing completely at random and missing at random? Int J Epidemiol. 2014;43(4):1336–1339. 10.1093/ije/dyu080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.The Williams Institute of the UCLA School of Law. LGBT Demographic Data Interactive. https://williamsinstitute.law.ucla.edu/visualization/lgbt-stats. Published 2019. Accessed September 28, 2019.
- 56.Movement Advancement Project, Center for American Progress, Youth First. Unjust: How the broken criminal justice system fails LGBT people of color. Published 2017. [Google Scholar]
- 57.Matthews DD, Smith JC, Brown AL, Malebranche DJ. Reconciling epidemiology and social justice in the public health discourse around the sexual networks of Black men who have sex with men. Am J Public Health. 2016;106(5):808–814. 10.2105/ajph.2015.303031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Taylor TN, DeHovitz J, Hirshfield S. Intersectional stigma and multi-level barriers to HIV testing among foreign-born Black men from the Caribbean. Front Public Health. 2020;7:373. 10.3389/fpubh.2019.00373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Earnshaw VA, Reed NM, Watson RJ, Maksut JL, Allen AM, Eaton LA. Intersectional internalized stigma among Black gay and bisexual men: a longitudinal analysis spanning HIV/sexually transmitted infection diagnosis. J Health Psychol. In press. Online Janury 1, 2019. 10.1177/1359105318820101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bowleg L, English D, del Rio-Gonzalez AM, Burkholder GJ, Teti M, Tschann JM. Measuring the pros and cons of what it means to be a Black man: development and validation of the Black Men’s Experiences Scale (BMES). Psychol Men Masc. 2016;17(2):177–188. 10.1037/men0000026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Follins LD, Lassiter JM. Black LGBT Health in the United States: The Intersection of Race, Gender, and Sexual Orientation. Lanham, MD: Lexington Books; 2016. [Google Scholar]
- 62.DecrimNY. https://www.decrimny.org/. Published 2020. Accessed July 24, 2020.
- 63.Bassett MT, Galea S. Reparations as a public health priority — a strategy for ending Black–White health disparities. N Engl J Med. 2020;383(22):2101–2103. 10.1056/nejmp2026170. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


