Abstract
Introduction
Seborrheic keratoses are benign tumours that occur electively on the head, neck and trunk. It can be confused on its clinical appearance with other skin tumours and it is the histological examination that establishes the diagnosis. We report a case of seborrheic keratosis simulating squamous cell carcinoma.
Observation
A 62-year-old woman consulted for a budding right jugal lesion that had been evolving for 6 months. Clinical examination found a right jugal budding lesion with crusts on its surface, pedunculated, surrounded by a hyperpigmented halo at its base, firm to palpation, painless and non bleeding on contact. An initial biopsy of the lesion for histological examination confirmed the diagnosis, followed by complete surgical excision.
Discussion
Seborrheic keratoses are benign tumours that occur mainly in subjects over 50 years of age. They occur electively on the trunk, head and neck. Its clinical aspect is generally typical but sometimes misleading, as found in our case; only histology allows to make the diagnosis of certainty.
Keywords: Seborrheic keratosis, Squamous cell carcinoma, Diagnosis, Management
Highlights
-
•
Seborrheic keratoses are benign tumours that occur electively on the head, neck and trunk.
-
•
Its clinical aspect is generally typical but sometimes misleading, as found in our case simulating a squamous cell carcinoma.
-
•
Only histology allows a definite diagnosis.
-
•
Treatment is surgical for giant forms.
1. Introduction
Seborrhoeic keratoses are benign skin tumours that develop in people over 50 years of age [1]. They are usually initially papular, barely prominent, well-limited, single or multiple lesions, which later become thick, keratotic, pigmented, sometimes blackish, with a frankly verrucous appearance, which may be confused with other skin tumours. They are most often found on the head, neck and trunk. They usually range in size from a few millimetres to a few centimetres [2,3]. We report a case of a unique seborrheic keratosis of a size and clinical appearance that simulates squamous cell carcinoma, which was treated by surgical excision.
2. Case report
This article has been reported in line with the PROCESS criteria [4].
A 62 year old female patient, with no previous pathological history, presented to our maxillofacial surgery department with a lesion of the right sub-zygomatic region, which was small at first, then progressively increasing in size, and had been evolving for 6 months. Clinical examination found a right sub-zygomatic bulging lesion, rounded, measuring approximately 2.5 cm in greatest diameter, with crusts on its surface, pedunculated, surrounded by a hyperpigmented halo at its base, firm to palpation, painless and non-bleeding on contact (Fig. 1). There was an absence of cervical adenopathy. The patient first underwent a biopsy of the lesion, the anatomopathological result of which came back in favour of a seborrhoeic keratosis. Surgical removal of the lesion was then performed under local anaesthesia (Fig. 2) with reconstruction of the removal site by direct suture (Fig. 3).
Fig. 1.
Macroscopic appearance of the Seborrheic Keratosis lesion.
Fig. 2.
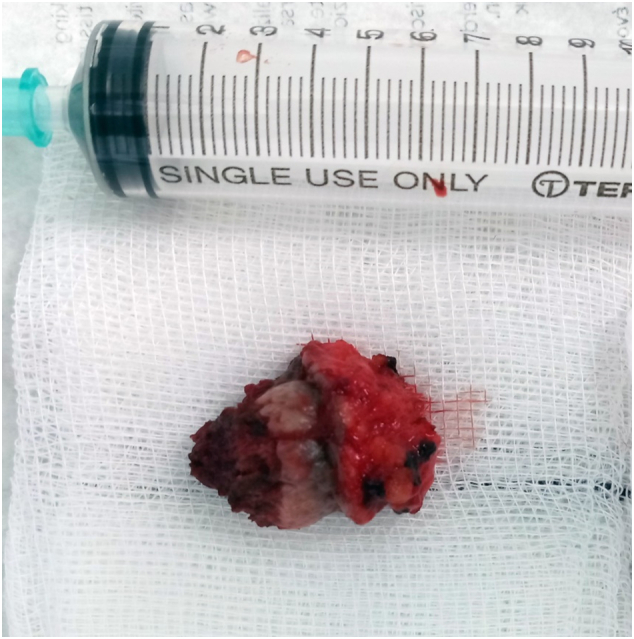
Surgical specimen after surgical removal of the lesion.
Fig. 3.

Condition of the excision site after reconstruction by direct suture.
The anatomopathological result of the surgical specimen confirmed the diagnosis of seborrheic keratosis and the patient was followed up at the consultation with good evolution and absence of local recurrence.
3. Discussion
Seborrheic Keratosis (formerly called seborrheic wart or hyperkeratotic papillary seborrheic wart) is a benign and frequent epithelial tumour of chronic evolution. It occurs mainly in elderly subjects over 50 years of age [1,5], as found in our cases. It occurs mainly on the face and trunk, but rarely in the genital area [6].
Seborrhoeic keratoses have a fairly typical clinical appearance, forming raised, well-limited, flat lesions, as if laid on the skin, with a squamo-keratotic appearance, brown-grey to black in colour (Fig. 4). They are easily removed with a curette. They are often multiple and can grow to several centimetres in size [6]. The main differential diagnoses are condyloma (genital warts), pigmented basal cell carcinoma and melanoma [7].
Fig. 4.
A and B are examples of the usual and typical mascroscopic appearance of seborrhoeic keratoses.
In our case, it was a single lesion with a rather budding, non-blackish, pedunculated appearance, with crusts on the surface, confusing with the budding character of squamous cell carcinoma [8].
The aetiology of seborrhoeic keratoses is unknown, although there may be some familial predisposition, which was not found in our patient [1]. It could also occur after an inflammatory dermatosis or at a site of repeated rubbing [2].
However, several authors claim that it is a pre-cancerous lesion and will be prone to malignant transformation into melanoma or basal cell carcinoma [[9], [10], [11], [12]]. Indeed, the malignant transformation of seborrhoeic keratoses is a source of controversy, hence the indisputable interest of anatomopathological examination to confirm or invalidate the diagnosis, especially when the latter present an atypical location or clinical manifestations. Indeed, pathological examination is the only reliable means of diagnosis and should be carried out systematically for a lesion whose benign or malignant nature is debated [5,12,13] and can thus guide the treatment of the lesion.
Therefore, pathological examination of any seborrhoeic keratosis should be considered when the lesion has an atypical location or clinical manifestations.
Histological examination of the excisional specimen confirmed the diagnosis by demonstrating a hyperacanthosic epidermis with focal parakeratosis, cornified pseudocystics and basal layer hyperplasia.
The treatment of seborrhoeic keratosis involves several therapeutic means. Sometimes it is not necessary to treat these lesions because they are only cosmetic and usually recur.
Cryotherapy, defined as the application of liquid nitrogen, is the first-line technique for the destruction of these lesions. Mechanical curettage or dermabrasion can completely remove small lesions. Electrocoagulation and the application of pure trichloroacetic acid are also used [3].
However, in some cases, surgery can be used for giant forms [14,15]. In addition, surgery has the advantage of performing a histopathological examination to confirm the diagnosis.
Therefore, in the case of a benign tumour known to be prone to recurrence, such as seborrhoeic keratosis, resection should be as complete as possible to avoid recurrence. In the case of histologically confirmed incomplete resection, the subsequent course of action would be to monitor the patient regularly for early detection of recurrence or malignant transformation of the tumour [3].
In this patient, after explaining the principles of the treatment and obtaining her consent, a complete surgical excision was performed under local anaesthesia with reconstruction of the skin substance loss by direct sutures. The margins of the excision were healthy, confirmed by anatomopathology, and no recurrence was observed at the one-year follow-up.
4. Conclusion
Seborrheic keratosis is a benign tumour with a preferential location in the cervico-facial region and on the trunk. Its clinical appearance is generally typical but sometimes misleading, as in our case, where it simulated a squamous cell carcinoma. Only the histological examination allows to make a diagnosis of certainty and to eliminate a malignant tumour or a malignant transformation. Several therapeutic means exist, but surgery is the most recommended for giant forms.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Sources of funding
The authors declared that this study has received no financial support.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Guarantor
Ulrich Opoko.
Registration of research studies
None.
CRediT authorship contribution statement
Ulrich Opoko: Corresponding author writing the paper.
Ayoub Sabr: writing the paper.
Mohamed Raiteb: writing the paper.
Amina Maadane: writing the paper.
Faiçal Slimani: Correction of the paper.
Declaration of competing interest
Authors of this article have no conflict or competing interests. All of the authors approved the final version of the manuscript.
References
- 1.Livaoglu M., Karakal N., Gucer H., Arvas L. Giant genital seborrheic keratosis. Dermatol. Surg. 2007;33:1357–1358. doi: 10.1111/j.1524-4725.2007.33289.x. [DOI] [PubMed] [Google Scholar]
- 2.El Amrani F. Kératoses séborrhéiques géantes de siège inhabituel. Ann. Dermatol. Venereol. 2012;139(11):723–726. doi: 10.1016/j.annder.2012.05.009. [DOI] [PubMed] [Google Scholar]
- 3.Kharrat W. Kératose séborrhéique palpébrale À propos d ' une observation. J. Fr. Ophtalmol. 2004;27(10):1146–1149. doi: 10.1016/s0181-5512(04)96284-5. [DOI] [PubMed] [Google Scholar]
- 4.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., Thoma A., Beamish A.J., Noureldin A., Rao A., Vasudevan B., Challacombe B., Perakath B., Kirshtein B., Ekser B., Pramesh C.S., Laskin D.M., Machado-Aranda D., Miguel D., Pagano D., Millham F.H., Roy G., Kadioglu H., Nixon I.J., Mukhejree I., McCaul J.A., Chi-Yong Ngu J., Albrecht J., Rivas J.G., Raveendran K., Derbyshire L., Ather M.H., Thorat M.A., Valmasoni M., Bashashati M., Chalkoo M., Teo N.Z., Raison N., Muensterer O.J., Bradley P.J., Goel P., Pai P.S., Afifi R.Y., Rosin R.D., Coppola R., Klappenbach R., Wynn R., De Wilde R.L., Surani S., Giordano S., Massarut S., Raja S.G., Basu S., Enam S.A., Manning T.G., Cross T., Karanth V.K., Kasivisvanathan V., Mei Z., The SCARE 2020 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020 doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 5.Salim S., Bouhelab J., Khalaayoune M., Hassam B. Kératose séborrhéique en transformation bowénoïde: quand la bénignité se mêle à l’atypie. Ann. Dermatol. Venereol. 2017;144(12):S166–S167. doi: 10.1016/j.annder.2017.09.242. Supplement. ISSN 0151-9638. [DOI] [Google Scholar]
- 6.Phiske M., Mamidwar S., Dhurat R., Jerajani H.R., Randive N., Joshi M. Giant lobulated seborrheic keratosis at an unusual site. Indian J. Pathol. Microbiol. 2003;46:96–97. [PubMed] [Google Scholar]
- 7.Thakur J., Thakur A., Chauhan C.G., Diwana V., Chauhan D.C. Giant pedunculated seborrheic keratosis of penis. Indian J. Dermatol. 2008;53:37–38. doi: 10.4103/0019-5154.39743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kouamé K. 2019. Dermatoses pré-néoplasiques et carcinome épidermoïde: 96 cas en Dermatologie/ pp. 253–257. [Google Scholar]
- 9.Akasaka T., Kon S. Two cases of basal cell carcinoma arising in seborrheic keratosis. J. Dermatol. 1997;24:322–327. doi: 10.1111/j.1346-8138.1997.tb02798.x. [DOI] [PubMed] [Google Scholar]
- 10.Yap W.M., Tan P.H., Ong B.H. Malignancy arising in seborrheic keratosis: a report of two cases. Ann. Acad. Med. Singap. 1997;26:235–237. [PubMed] [Google Scholar]
- 11.Cascajo C.D., Reichel M. Sanchez. Malignant neoplasms associated with seborrheic keratoses. Analysis of 54 cases. Am. J. Dermatopathol. 1996;18:278–282. doi: 10.1097/00000372-199606000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Rao B.K., Freeman R.G., Poulos E.G., Arbesfeld L., Rendon M. The relationship between basal epithelioma and seborrheic keratosis. A study of 60 cases. J. Dermatol. Surg. Oncol. 1994;20:761–764. doi: 10.1111/j.1524-4725.1994.tb03201.x. [DOI] [PubMed] [Google Scholar]
- 13.Zabel R.G., Vinson R.P., McCollough M.L. Malignant melanoma arising in a seborrheic keratosis. J. Am. Acad. Dermatol. 2000;42:831–833. doi: 10.1067/mjd.2000.103634. [DOI] [PubMed] [Google Scholar]
- 14.Di Benedetto G., Pierangeli M., Bertani A. A peculiar case of multiple gigantic seborrheic keratosis. Plast. Reconstr. Surg. 1997;99:1466–1467. [PubMed] [Google Scholar]
- 15.Sowden J.M., Lewis-Jones M.S., Williams R.B. The management of seborrheic keratoses by general practitioners, surgeons and dermatologists. Br. J. Dermatol. 1998;139:348–349. doi: 10.1046/j.1365-2133.1998.02384.x. [DOI] [PubMed] [Google Scholar]




