Abstract
Background
chronic lymphocytic leukemia (CLL) patients have a high risk of occurrence of secondary cancers. This risk is three times higher for all cancers and eight times higher for skin cancer. The coexistence of CLL and adenocarcinoma of the prostate is rare.
Case presentation
We report a case of a66-year-old man who underwent radical prostatectomy for prostate carcinoma. The final histopathological diagnosis of Gleason 7 adenocarcinoma of the prostate with incidental Rai stage I chronic lymphocytic leukemia (CLL) was made. No further investigations or treatment was offered due to the age and low disease stage. At the last follow-up of 12 months, the patient is alive, without disease progression for both lymphoma and prostate, with a PSA value of 0.03 ng/ml.
Conclusion
Early detection of lymphoma after radical prostatectomy will allow optimal management. The analysis of this link requires, therefore, additional investigations.
Keywords: Radical prostatectomy, Chronic lymphocytic leukemia, Prostate carcinoma
Highlights
-
•
Chronic lymphocytic leukemia (CLL) patients have a high risk of occurrence of secondary cancers. This risk is three times higher for all cancers and eight times higher for skin cancer.
-
•
The coexistence of CLL and adenocarcinoma of the prostate is rare.
-
•
Early detection of lymphoma after radical prostatectomy will allow optimal management.
1. Introduction
Radical prostatectomy is the gold standard for the treatment of prostate cancer [1]. The detection of lymph nodes before surgery isproblematic because it is frequently microscopic and undetectable using existing imaging modalities [[1], [2], [3]]. Chronic lymphocytic leukemia (CLL) patients have a high risk of developing secondary cancers. However, the coexistence of CLL and prostate adenocarcinoma is rare [3,4]. We report a case of Incidental chronic lymphocytic leukemia (CLL) diagnosed following radical prostatectomy for prostate adenocarcinoma of the prostate with concomitant chronic lymphocytic leukemia in a 66-year-old man. The work has been reported in line with the SCARE criteria [5].
2. Case description
A 66-year-old man presented with history of lower urinary tract symptoms for 4 months. He raported nocturia, urgency and a weak urine stream. Abdominal examination was unremarkable, and digital rectal examination revealed an enlarged prostate with normal consistency without nodule or induration. Laboratory tests showed a high Prostate-specific antigen (PSA) level (5.06 ng/ml). Liver and renal function tests were normal. Blood test investigations revealed hyperleukocytosis (WBC: 32 × 109/l), hyperlymphocytosis (Lymph: 8 × 109/l), red blood cell, and platelet counts were in the normal range.Multi-parametric abdominal magnetic resonance imaging (MP-MRI) showed the presence of a posterior prostate lesion measuring 16 mm, located in the left peripheral zone, with associated left external iliac chain lymph node. The prostatic lesion was hypointense on T2-weighted (T2W) and apparent diffusion coefficient (ADC) images. However it was hyperintense on Diffusion-weighted imaging (DWI images) (Fig. 1). Based on these findings, the prostate lesion was classified as category five according to PI-RADS (Prostate Imaging–Reporting and Data System) assessment score. Endorectal ultrasound-guided prostate biopsy with cognitive fusion after MRI confirmed the presence of Gleason 4 + 3 = 7 adenocarcinoma of the prostate in 9 cores among 12 cores with a maximum core involvement of 90%. A bone scan did not reveal metastatic bone disease. Based on those findings, the diagnosis of prostatic adenocarcinoma with lymphatic metastasis was made. Radical prostatectomy with bilateral pelvic lymph node dissection was done.
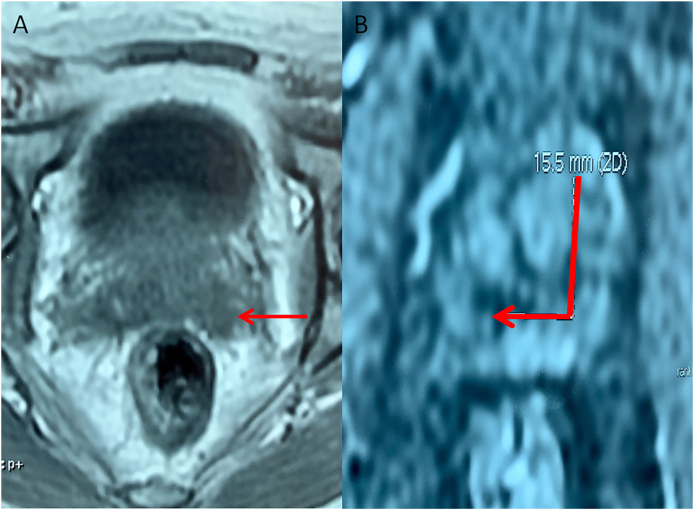
Fig. 1.
Multi parametric abdominal magnetic resonance imaging (MP -MRI) showed the presence of a posterior prostate lesion measuring 16 mm, located in the left peripheral zone Magnetic hypointense on T2W (A) and markedly hyperintense on DWI (B).
On histopathology, bilateral, multifocal microacinar type of prostatic adenocarcinoma was identified. Surgical margins were negative. Lymph nodes and seminal gland examination showed diffuse infiltration of small B-cells lymphocytes. A final Gleason score was 4 + 3 = 7. On immunohistochemistry, the lymphoid infiltration was positively stained for the CD20, CD5, and CD23 and negatively staining for CD3, CD10, cyclin D1 and Bcl 6 (Fig. 2). Thus, the final histopathological diagnosis of Gleason 7 adenocarcinoma of the prostate, staged pT2c N0 MX, associated with an incidental chronic lymphocytic leukemia (CLL), was made. A body scan was performed and showed multiple enlarged mediastinal and bilateral axillary lymph nodes. The CLL was staged as low-risk lymphoma (Rai stage I). The patient was then referred for hematological evaluation. The standard treatment of patients with early disease LLC is a watch-and-wait strategy. Blood cell counts and clinical examinations were carried out every three months after the first year. At the last follow-up of 12 months, the patient is alive, without disease progression, the PSA value is 0.003 ng/ml and blood cell counts was stable.
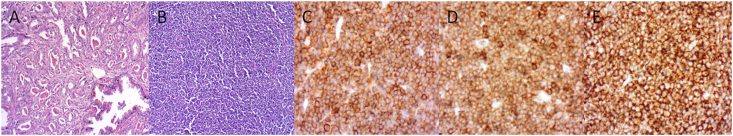
Fig. 2.
Microscopic examination of the prostate tissue showing crowded glands of adenocarcinoma with dense eosinophilic crystalloids [Gleason score 7 (4 + 3)] (A). The pelvic lymph node examination revealed small, round tumor cells with low grade of differentiation (H & E) (B) and positive staining for CD20 (C), CD5 (D) and CD23 (E).
3. Discussion
CLL is a lymphoproliferative syndrome characterized by a medullary proliferation of a clone B cell, which invades the blood and lymphoid organs [6]. CLL patients have a high risk of association with adenocarcinomas. It is more likely to coincide with adenocarcinoma of the gastrointestinal tract, skin, and breast. However its coexistence with prostatic cancer is rare [2,7,8]. This association rate was 0,8% in Terris et al. study, including 1092 patients who underwent radical prostatectomy. However this rate was 0% in Eisemberger et al. study, including 4319 patients [9,10]. Tsimberidou et al. reported a serie of 2028 patients diagnosed with CLL and small lymphocytic lymphoma, among which 551 patients had a history of other malignancies or developed other cancer during the follow-up period [11].
CLL patients have a high risk of secondary cancers, reaching 10–11 times higher than the average population [4,7]. Some authors attribute this risk to the chemotherapeutic treatment of the lymphoma, and others related it to a defect in the cellular immune mechanisms whereas some authors to chance alone [2].
Some authors reported independent factors predicting the development of other cancers such as older age, male sex, 2-microglobulin > 3 mg/L, Lactate dehydrogenase >618 U/L, Creatinine >1.6 mg/dL [9,11]. However, author studies showed that patients with 17p deletion, 6q deletion, 11q deletion or trisomy 12 had an increased risk of developing other cancers compared with other patients [12].
The literature review showed a good prognosis of CLL diagnosed after radical prostatectomy [1,8]. Due to the risk of developing prostate cancer in patients diagnosed with LLC, some authors reported the need for prostatic cancer screening using the PSA test [7].
The Rai classification divides the LLC into five stages [13].
According to this classification, our case was staged a low-risk Rai stage I: Lymphocytosis plus enlarged lymph nodes.,the spleen and liver are not enlarged, and the red blood cell and platelet counts are normal or only slightly low. According to the European society for medical oncology guidelines, the standard treatment of patients with early disease LLC(Rai I stage) is a watch-and-wait strategy, and no further treatment is needed.
After the first year, the patients should be seen at 3-monthly intervals, with physical examinations including palpation of all lymph node areas and a complete blood cell count [14].
4. Conclusion
Incidental chronic lymphocytic leukemia diagnosed following radical prostatectomy for prostate cancer is rare, with few cases reported in the literature.
However, the difficulties of their detection on imaging, the lymph node metastasis can be an indicator of LLC, influencing the therapeutic decision. Urologists should keep in mind such association due to the impact on therapeutic decision and patient follow-up.
Ethical approval
The study was approved by Ethics Committee of Sahloul Hospital approval references: U2350.
Sources of funding
This study has not received any funding.
Consent
Written informed consent was obtained from the patient.
Trial registry number
-
1.
Name of the registry:
-
2.
Unique Identifying number or registration ID:
-
3.
Hyperlink to the registration (must be publicly accessible):
This is not applicable, because this is a case report.
Guarantor
Ghassen tlili.
Informed consent
The patient provided informed written consent prior to submission of this manuscript.
Author contributions
Wiem Majdoub– Editing of manuscript, data collection, Anatomopathology analysis.
Ghassen tlili – Editing of manuscript, supervision of the manuscript.
Houssem Ammar– Editing of manuscript, literature review, drafting the manuscript.
Emir akacha– Editing of manuscript, data collection.
Sonia Dziri– Data collection, Editing of the manuscript.
Waad Farhat-data collection, Editing of manuscript.
Mehdi jaidane- Editing of manuscript, data collection.
Rahul Gupta– Editing of manuscript, literature review, drafting the manuscript.
Khaled ben ahmed – manuscript correction, supervision of the manuscript.
Awatef Azzabi – Supervision of the manuscript, manuscript correction.
Declaration of competing interest
The authors declare that they have no conflict of interest.
Acknowledgment
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2021.102516.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.El-Taji O., Omer A., Al-Mitwalli A., Agarwal S. Incidental lymphoplasmacytic lymphoma diagnosed following robotic-assisted laparoscopic prostatectomy for prostate cancer. Curr. Urol. 2019;13:166–168. doi: 10.1159/000499275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gros R., Richter S., Bechar L. Prostatic carcinoma with concomitant non-Hodgkin lymphoma. Report of 2 cases. Urol. Int. 1984;39(2):121–122. doi: 10.1159/000280959. [DOI] [PubMed] [Google Scholar]
- 3.Fournier G., Valeri A., Mangin P., Cussenot O. Cancer de la prostate Épidémiologie. Facteurs de risques. Anatomopathologie. Ann Urol. 2004;38:187–206. doi: 10.1016/j.anuro.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 4.Ather M.H., Memon A. Acute urinary retention: a primary manifestation of chronic lymphocytic leukemia and organ confined prostate cancer. J. Pakistan Med. Assoc. 1999;49:124–125. [PubMed] [Google Scholar]
- 5.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A., Orgill D.P., For the SCARE Group The SCARE 2018 statement: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2018;60:132–136. doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]
- 6.Binet J.L., Caligaris-Cappio F., Catovsky D., Cheson B., Davis T., Dighiero G. Perspectives on the use of new diagnostic tools in the treatment of chronic lymphocytic leukemia. Blood. 2006;107:859–861. doi: 10.1182/blood-2005-04-1677. [DOI] [PubMed] [Google Scholar]
- 7.Hatim Nafil, Illias Tazi, L. Mahmal. Cancer de la prostate et leucémie lymphoïde chronique. Afr. J. Urol. 19(1):35–38.
- 8.Ballario R., Beltrami P., Cavalleri S., Ruggera L. An unusual pathological finding of chronic lymphocytic leukemia and adenocarcinoma of the prostate after transurethral resection for complete urinary retention: case report. BMC (Biomed. Chromatogr.) 2004;4:95. doi: 10.1186/1471-2407-4-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Terris M.K., Hausdorff J., Freiha F.S. Hematolymphoid malignancies diagnosed at the time of radical prostatectomy. J. Urol. 1997;158:1457–1459. [PubMed] [Google Scholar]
- 10.Eisenberger C.F., Walsh P.C., Eisenberger M.A., Chow N.H. Incidental non- Hodgkin's lymphoma in patients with localized prostate cancer. Urology. 1999;53:175–279. doi: 10.1016/s0090-4295(98)00422-1. [DOI] [PubMed] [Google Scholar]
- 11.Tsimberidou A.M., Wen S., McLaughlin P., O'Brien S. Other malignancies in chronic lymphocytic leukemia/small lymphocytic lymphoma. J. Clin. Oncol. 2009;27:904–910. doi: 10.1200/JCO.2008.17.5398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tsimberidou A.M., Wen S., O'Brien S., McLaughlin P. Assessment of chronic lymphocytic leukemia and small lymphocytic lymphoma by absolute lymphocyte counts in 2,126 patients: 20 years of experience at the University of Texas M.D. Anderson Cancer Center. J. Clin. Oncol. 2007;25(29):4648–5613. doi: 10.1200/JCO.2006.09.4508. [DOI] [PubMed] [Google Scholar]
- 13.Rai K.R., Sawitsky A., Cronkite E.P. Clinical staging of chronic lymphocytic leukemia. Blood. 1975;46:219–234. [PubMed] [Google Scholar]
- 14.Eichhorst B., Robak T., Montserrat E., Ghia P. Chronic lymphocytic leukaemia: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2021;32(1):23–33. doi: 10.1016/j.annonc.2020.09.019. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.