Abstract
Purpose:
We examine pilot results for the culturally adapted Weaving Healthy Families (WHF) program to promote resilience and wellness while preventing substance abuse and violence among Native American (NA) families.
Methods:
Results were drawn from paired sample t tests and analyses of variance (ANOVA) with a convenience sample of 24 adults and adolescents from eight NA families (pretest, posttest, and, where available, 6-month postintervention).
Results:
Along with substance abuse reduction and prevention, t test results indicated reductions in (a) adult depressive symptoms and improvements in adult conflict resolution and health behaviors; (b) adolescent wellness; and (c) adult and adolescent resilience, communal mastery, social support, and sugar-sweetened beverage consumption. ANOVA tests revealed reductions in adult psychological and physical violence and improvements in adult and adolescent family resilience, family environment, and emotional regulation.
Conclusions:
Results reveal promising preliminary results for the WHF program to promote resilience and thriving while reducing risk for substance abuse and violence in NA families.
Keywords: Native American, substance abuse, intimate partner violence, resilience, families
Intimate partner violence (IPV) and with alcohol and other drug (AOD) abuse are co-occurring and, often, familial risk factors (American Psychological Association, 2010; Breiding et al., 2014; U.S. Department of Health and Human Services, 2013) that drive Native American (NA) mortality and health inequities (Hawkins et al., 2004; Klostermann et al., 2010; Moran & Bussey, 2007; Sharps et al., 2003). AOD abuse and violence interventions among NAs (Thomas et al., 2009) tend to be approached from a culturally incongruent, non-NA perspective, which can be less effective and harmful to NAs (Gone & Trimble, 2012; Urban Indian Health Institute [UIHI], 2014).
Despite their co-occurrence, AOD abuse and violence are addressed in interventions separately and are not culturally specific (LutraGroup, 2007; Whitesell et al., 2018). Over 80% of women and men (84.3% and 81.6%, respectively) experience violent incidents in their lifetime, the majority of which are alcohol related (Rosay, 2016). On average, approximately 40% of NA women and 35% of NA men report experiencing violence in the past year (Rosay, 2016). Incidents of IPV among NA women approach twice that of non-NA women (1.7 times higher; Rosay, 2016), and child maltreatment rates for NAs are 1.5 times higher than non-NAs (U.S. Department of Health and Human Services, 2013).
NAs experience elevated rates of early mortality compared to other races due to accidents, including alcohol poisoning, cirrhosis, chronic liver disease, diabetes, and suicide (Shiels et al., 2017); however, treatments tend to address problems in isolation (Klostermann et al., 2010; Kraanen et al., 2013; Kumpfer et al., 2002; Satyanarayana et al., 2016; Tutty, 2013; Wallerstein & Belone, 2015; Whitbeck, 2015) and do not include the context of historical oppression (Burnette, 2015, 2016), family (Klostermann et al., 2010; Kraanen et al., 2013; Satyanarayana et al., 2016; Tutty, 2013), or culture (UIHI, 2014). Moreover, alcohol abuse is associated with poor nutrition, health, and primary causes of NA mortality, such as diabetes and obesity (Butler et al., 2018).
Family- and culturally based prevention programs that enhance resilience (i.e., the positive adaption of systems in response to adversity; Kirmayer et al., 2009; Ungar & Liebenberg, 2011) and reduce the co-occurring risks of AOD abuse and violence are absent (Gone & Trimble, 2012; UIHI, 2014). Programs that fail to integrate these culturally specific, co-occurring factors negate the drivers of healthy inequities among NAs (Dixon et al., 2007; Gone & Trimble, 2012; UIHI, 2014). With community-based participatory research (CBPR) methodology (Thomas et al., 2009; Wallerstein & Duran, 2006) and a longitudinal pretest, posttest, and 6-month postintervention design, we examine preliminary results from a pilot study.
The Weaving Healthy Families (WHF) Program
The WHF program is an empirically based intervention that integrates over 10 years of research (Burnette, Sanders, Butcher, & Rand, 2014; Burnette & Figley 2017; McKinley et al., 2019) and the Celebrating Families! evidenced-based program (EBP; National Association for Children of Alcoholics [NACA], 2011). White Bison’s (2015) cultural overlay of the original EBP informed the development of the WHF program. This intervention targets key community and social (community and social support), behavioral (AOD), psychological/emotional (emotional regulation, depressive symptoms, and resilience), familial (family environment, family resilience, and holistic resilience), relational (IPV), and physical (AOD abuse and nutrition) factors.
The WHF program was empirically built upon rigorous mixed methodology research with over 1,000 tribal members (McKinley et al., 2019). It integrates key culturally relevant risk (those that worsen negative outcomes), promotive (those that are strengths regardless of adversity), and protective factors (those that buffer against risks and enhance positive outcomes) across ecological levels identified in this research (see Figure 1). Prior research led to the development of culturally validated key measures such as the Family Resilience Inventory (FRI; Burnette et al., 2020; McKinley et al., 2020). Figure 1 displays key risk and protective factors identified in preliminary research, those addressed by the WHF program, and those not addressed by the WHF program. The WHF program was developed through rigorous CBPR (Burnette et al., 2020; McKinley et al., 2020) with an 11-person NA community advisory board (CAB).
Figure 1.
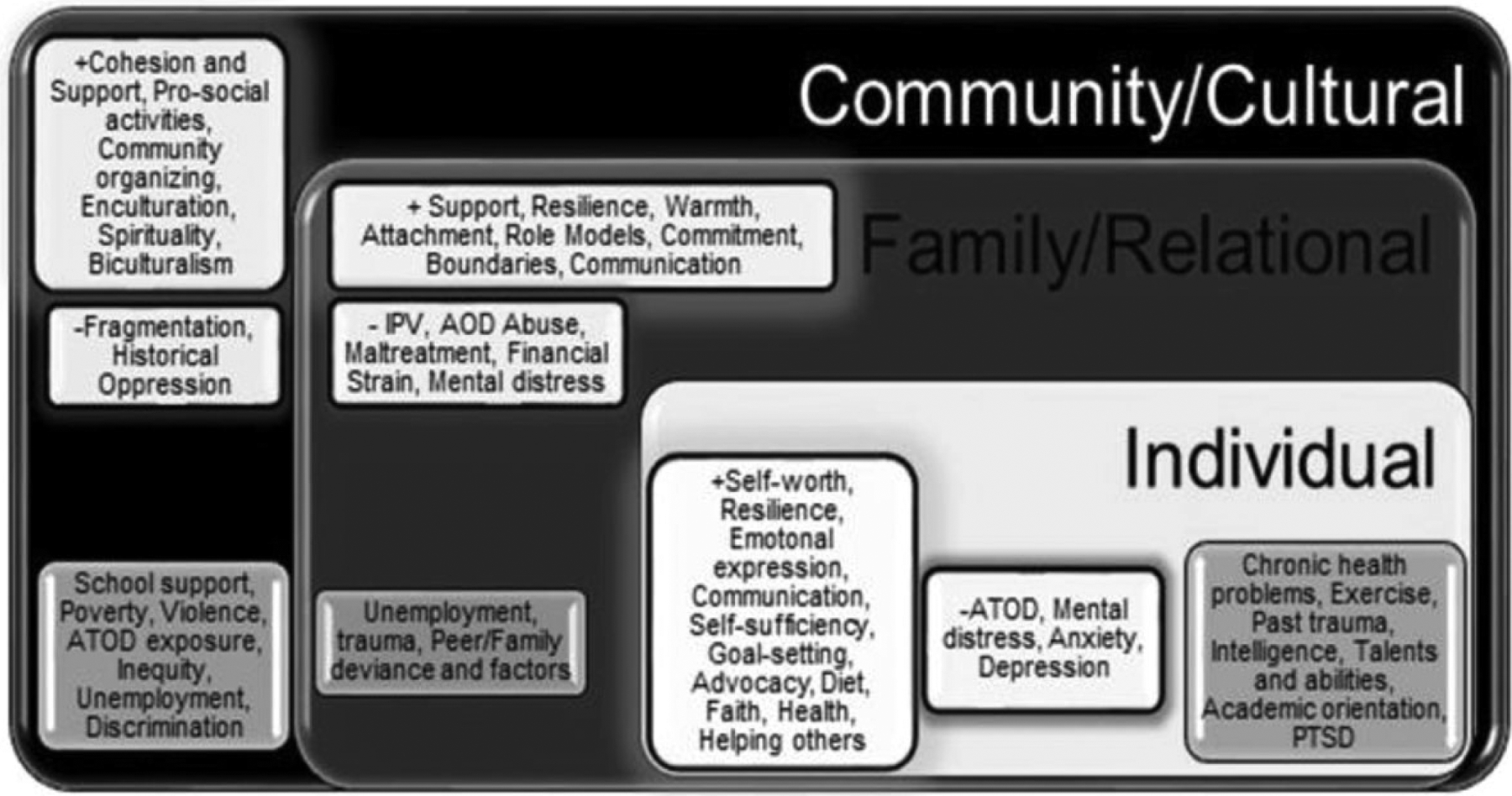
Conceptual model: Factors addressed and not addressed by intervention.
Note. Conceptual model: + indicates protective factors; − indicates risk factors; dark gray: factors not addressed in intervention.
We used the NA-grounded framework of historical oppression, resilience, and transcendence (FHORT; Burnette & Figley, 2017). Other research has found the original program to have very large effect sizes (d > 1.0) in the majority (15/18) of key family outcomes (LutraGroup, 2007). This is larger than the culturally adapted Strengthening Families Program, which focuses solely on AOD abuse and not IPV (LutraGroup, 2007; Whitesell et al., 2018); prior to this pilot study, neither the original nor the adapted WHF program had been tested with NAs. Figure 2 displays the focal outcomes for this pilot as they relate to the FHORT.
Figure 2.
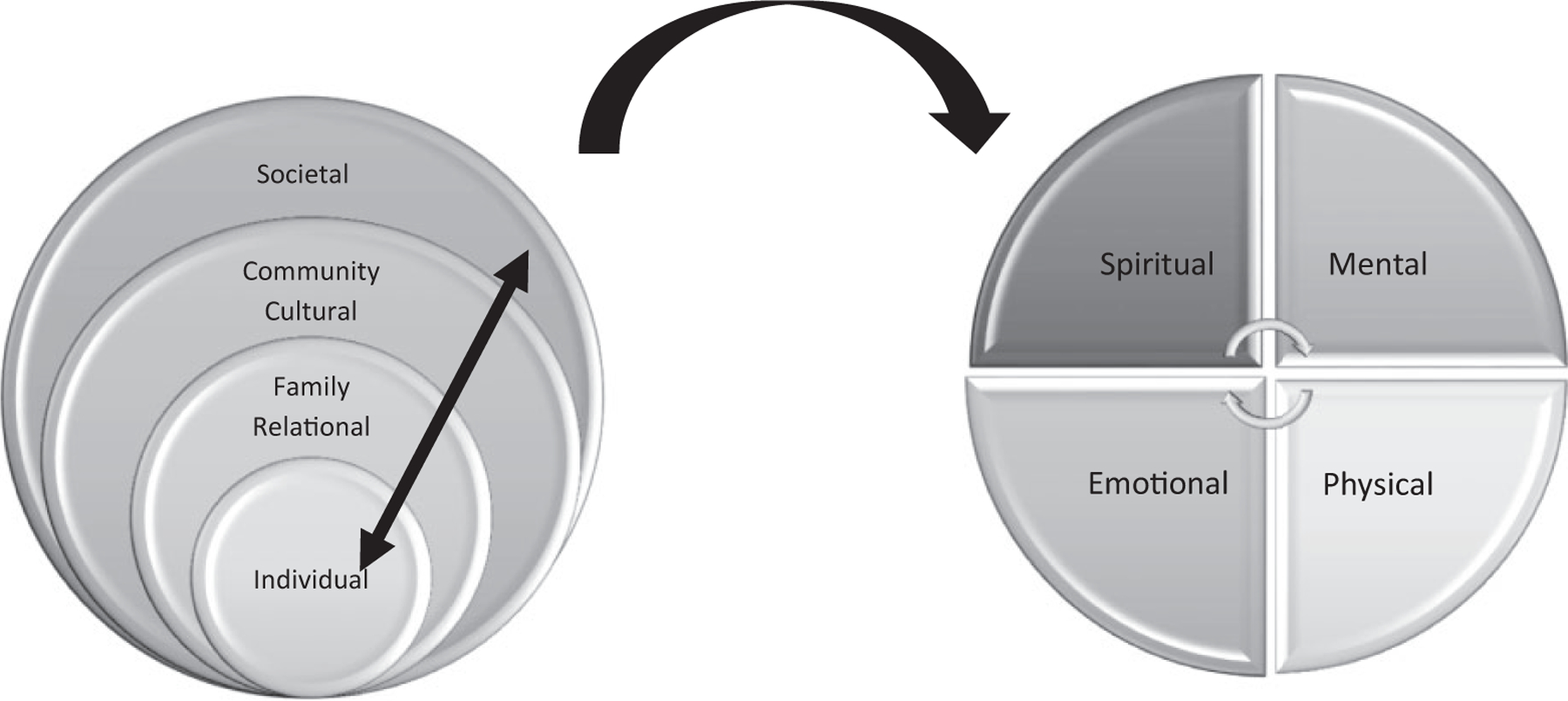
The framework of historical oppression, resilience, and transcendence (FHORT).
Note. Within the FHORT, ecological risk and protective factors across societal, cultural and community, family and relational, and individual levels predict key outcomes of wellness and resilience. We investigate community (communal master and social support) familial (family resilience, family environment, and holistic resilience) relational (intimate partner violence) as well as individual (emotional regulation, depressive symptoms, alcohol, tobacco, and other drug use, and health related quality of life/self-rated health practices) dimensions of wellness. In this way, we investigate key concepts of the FHORT (namely, aspects of ecological resilience).
Features of the WHF Program
First, unlike other programs, the WHF program includes a focus on violence and conflict in families along with AOD abuse (LutraGroup, 2007; Whitesell et al., 2018). Research continually documents that AOD abuse is associated with the majority (approximately two thirds) of homicides in IPV (Darke, 2010; Sharps et al., 2003). A recent international review indicated that, on average, over half of offenders are under the influence of AODs at the time of the homicide (Darke, 2010). This review indicated that 33%–66% of offenders and 40%–50% of victims were under the influence of alcohol at the time of the homicide (Darke, 2010). Parental AOD abuse is a risk factor for both IPV and child maltreatment (Bassuk et al., 2006; Few & Rosen, 2005; Masten & Monn, 2015; Tolan et al., 2006). Second, the WHF program is family focused. Most NA AOD programs focus exclusively on youth (Dickerson et al., 2015; Dixon et al., 2007; Hawkins et al., 2004; Miranda et al., 2005; Moran & Bussey, 2007), indicating a gap in family-focused interventions for NAs (Kumpfer et al., 2002). The absence of family members’ involvement is a barrier to AOD abuse and violence prevention (Kumpfer et al., 2002; Novins et al., 2012).
The effect sizes of family approaches to AOD abuse treatment and prevention are between two and nine times greater than conventional, child-only programs (Tutty, 2013). Given parental AOD abuse is among the strongest contributors to youth alcohol use (Dusenbury, 2000; Substance Abuse and Mental Health Services Association, 2004), disrupting the cycle of parental and youth alcohol use is critical for reducing AOD abuse among NAs. Research with NA tribes indicates the salience of families in treatment (Burnette, 2018), as families (nuclear, blended, extended, adopted, and nonkin family members; Red Horse, 1980; Robbins et al., 2013) are the essential social units organizing communities, providing support, and transmitting culture, which are protective factors for AOD abuse and violence prevention (Burnette & Figley, 2017).
Although interventions tend to be approached from a non-NA perspective, results from a nontargeted, multiethnic, AOD abuse prevention program with NA youth indicated an increase in drug use after the intervention (Dixon et al., 2007). Interventions targeted to cultural groups, however, are found to be four times more effective than nontargeted programs (Griner & Smith, 2006). Despite this, less than 20% of NA AOD programs offer culturally tailored services (UIHI, 2014). Cultural adaptation has been found to contribute to greater engagement, retention, sustainability, and more long-lasting improvements for key outcomes (Kumpfer et al., 2002; Lau, 2006; Marsiglia & Booth, 2015). Culturally tailored interventions have been found to minimize spontaneous changes made by practitioners to address cultural incongruity; these unplanned changes may undermine fidelity and effectiveness (Marsiglia & Booth, 2015).
Finally, using CBPR, the WHF program was developed, supported, vetted, and facilitated by the NA CAB members who were trained in and piloted the intervention. The WHF program is designed to prevent AOD abuse and violence in families by promoting positive parenting, emotional regulation, and resilience (NACA, 2011). The hallmarks of CBPR, including co-learning and sustainability, have been fostered through the training community health representatives (Terpstra et al., 2011), or CHRs, who have been working for NAs, beginning in 1969 when they were first funded by Indian Health Services (Uhrich, 1969). No known CHR research focuses on NA AOD abuse and violence prevention (Terpstra et al., 2011). CHRs are trusted (usually NA) community members who facilitate research (Spencer et al., 2010) and ensure culturally relevant and sustainable research methods (Terpstra et al., 2011).
Developing the WHF Program
Details of the cultural adaptation process are discussed elsewhere (see Burnette et al., 2019). Following CBPR methods, the CAB decided how to develop the intervention with the first author by (a) reviewing risk and protective factors for AOD abuse, violence, and resilience (see Figure 1) and (b) identifying potential NA-focused, effective, and acceptable interventions. The WHF program was developed from the Celebrating Families! curriculum, a cognitive behavioral EBP that follows a support group approach for high-risk families for violence and alcohol, tobacco, or other drugs (ATOD includes a tobacco component; Lum, 2008) and has improved family reunification rates following incidents of family violence (Quittan, 2004). The Celebrating Families! program has been found to lower AOD abuse, promote mental health, and strengthen families (NACA, 2011). Families meet together and with their peers with content tailored to age groups. This program has been found to demonstrate positive medium effect sizes (Cohen’s d = .52–.70) in family cohesion, resilience, communication, and organization, with a reduction (Cohen’s d = .15) in familial conflict (Kumpfer, 2006; LutraGroup, 2007). Moreover, parental involvement, efficacy, supervision, and improved parenting style were enhanced for medium effect sizes (Cohen’s d = .50–.60) and a small effect size (d = .22) in parental skills. AOD use among parents reduced as demonstrated by the effect size of 2.04 compared to Strengthening Families, which had an effect size of 1.15 (Kumpfer, 2006; LutraGroup, 2007). This program parallels the FHORT and has been used with NAs (NACA, 2011; White Bison, 2015).
Overview of Key Changes to the WHF Program
Figure 3 portrays the substantive changes made to the WHF program. The adapted WHF program addressed barriers identified by the CAB and other users who reported the curriculum was too dense, with little time for the conversations prioritized among many NA communities. Practitioners reported enacting spontaneous changes and excluding cultural tenets, which undermined the fidelity (Griner & Smith, 2006; Kumpfer et al., 2002; Lau, 2006; Marsiglia & Booth, 2015). As depicted in Figure 3, based on CAB feedback, sessions were reduced from 16 to 10, increasing feasibility. Second, we strategically removed overly burdensome content by retaining the main themes to maintain fidelity with the original program and simultaneously reduce participant burden. Third, a culturally relevant talking circle was integrated into the program, a method effective with NAs for AOD abuse (S. A. Becker et al., 2006; Morgan & Freeman, 2009). Fourth, we integrated NA nutritional aspects and tribal foodways, and we extended the time allocated for family dinners. Fifth, we integrated preadolescent and adolescent groups, which posed too many groups to facilitate separately, and we changed the ages of the youngest group to 5- to 7-year-olds, making this group in line with when children attend grade school. The WHF age groups include (a) parents/caregivers, (b) adolescents/youth aged 12–17, (c) children aged 8–11, and (d) young children aged 5–7 (see Figure 2). We enhanced the children and young children sessions to increase engagement, increasing their interactive and NA-focused aspects. We adapted the “connecting with my family” component to be more active, fun, and NA-focused, and less content heavy, as children and families were ready for this after the heavier content. We also integrated the FHORT and how gender relationships have been impaired through colonization. The WHF program was piloted with the CAB. The CAB members served as CHRs to facilitate WHF with the eight NAs fully completing the program. Initially, this pilot was aimed at assessing feasibility and acceptability before the full efficacy trial, but we got an unexpectedly large turnout, which enabled us to assess some preliminary changes in outcomes. Drawing from the ecological FHORT, we will use t test and analysis of variance (ANOVA) tests to examine pretest, posttest, and where available, 6-month postintervention scores, testing our hypotheses about whether the WHF intervention will improve the following outcomes across these ecological levels: (a) community: higher community mastery and social support; (b) familial: higher holistic resilience, family resilience, and a stronger family environment; (c) relational: lower IPV and improved conflict resolution; and (d) individual: higher emotional regulation, lower depressive symptoms, higher health-related quality of life, higher self-rated health practices, and lower sugar-sweetened beverage consumption.
Figure 3.
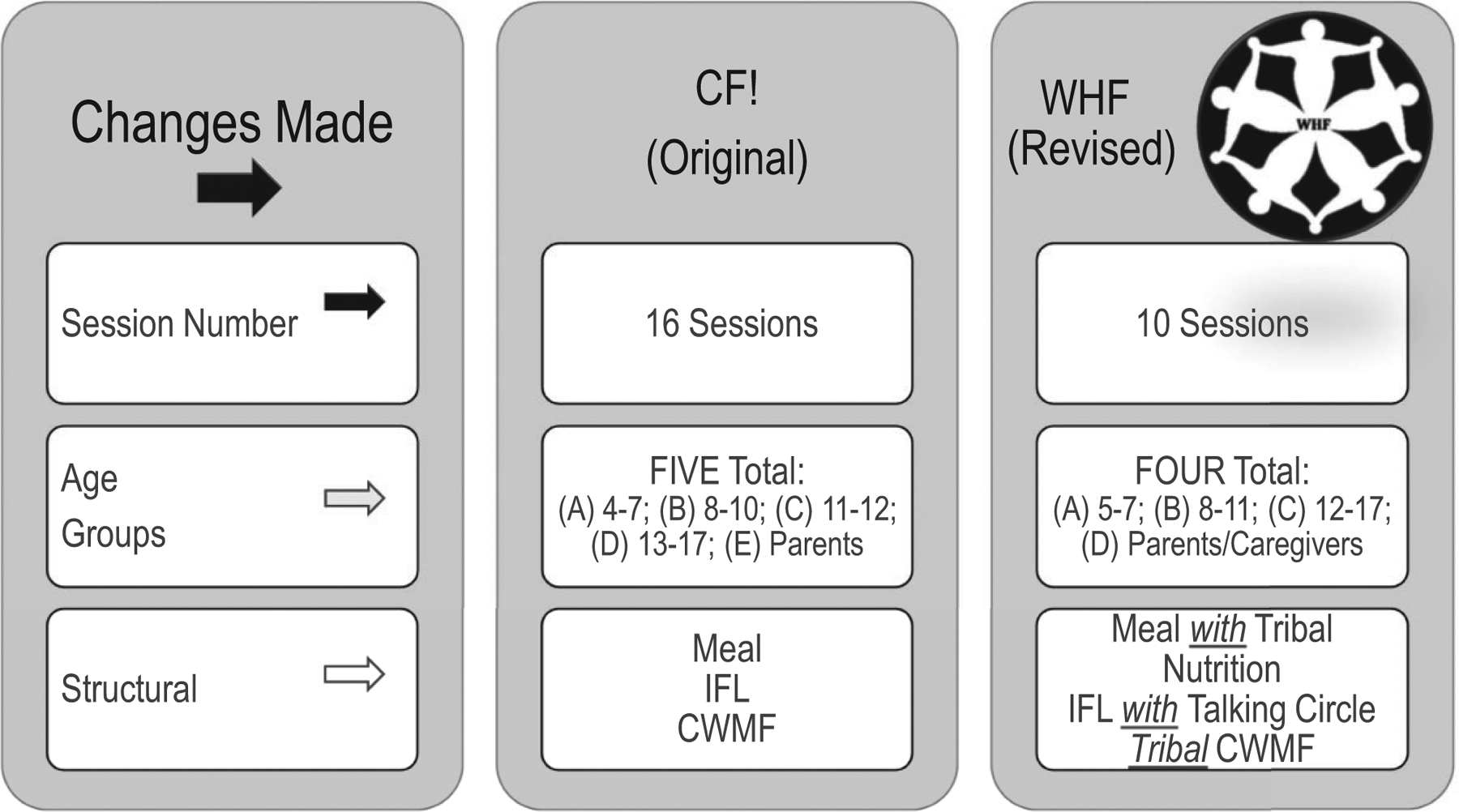
Summary of substantive changes to the WHF program.
Note. The first column displays the types of substantive changes made in the WHF program; the second column displays the original program (Celebrating Families! [CF!]) features, whereas the third displays the adapted WHF program. IFL = insights for living, the primary content; CWMF = connecting with my family, the family activities that facilitate connection. The WHF program was reduced from 16 sessions to 10, was reduced five age groups to four, and infused tribal content throughout the structure. The 10 finalized sessions include the following: (1) introduction and healthy living; (2) communication; (3) feelings and defenses; (4) alcohol, tobacco, and other drug use (ATOD); (5) ATOD and the family; (6) goal setting; (7) choices and problem-solving; (8) boundaries and healthy relationships; (9) resilience; and (10) celebration. Source: Figure adapted with permission from McKinley et al. (2020).
Method
Research Design
For the purpose of this pilot study, we used a nonrandomized intervention-only, convenience sample in a nonexperimental longitudinal pretest, posttest (immediately after the intervention), and 6-month follow-up data to analyze the change in key outcomes across time. Inclusion criteria included (a) tribal caregiver, (b) having at least one child aged 12 or above, (c) could attend all 10 sessions, and (d) were able to complete online surveys (with assistance if needed). All other participants were excluded. Because we were running the pilot initially for feasibility and acceptability of the intervention, we did not expect nor aim to enroll enough families to fully test intervention efficacy. If we were aiming to test efficacy, based on family studies with effect sizes of the Celebrating Families! program and comparable programs, sample sizes for families ranged from 60 to 75 with strong to moderate effect sizes (Kumpfer, 2006; Kumpfer et al., 2002).
We used word-of-mouth sampling, using CAB members to recruit families, and had an overwhelming response, doubling our expected family recruitment (we aimed for four families, and eight enrolled). Notably, all eight families completed the program. Although data were collected with youth and adults, the focus of the impact was on children 12 and older, and adults, as preliminary research indicates these periods are the ages of greatest risk for AOD abuse (Burnette, 2016; Burnette & Figley, 2017). The structure for each 2.5-hr session is as follows: Families meet together for a family meal and nutrition component; then, participants go to their developmental age groups (parents, adolescents aged 12–17, children aged 8–11, and young children aged 5–7) for the session content. Finally, they come back together for their time to connect with family. Two to three CHRs facilitate each session for each of the four age groups. CHRs, who were also CAB members, ran the intervention, with two NA CHR coordinators assisting with implementing the program. The CHR coordinators assisted with setup, meals, and materials and provided management and site oversight, including conducting weekly fidelity checks. The CHRs were trained in the WHF program, the FHORT, facilitation skills, and experiential activities. Two 3-day trainings prepared CAB/CHRs to run the program. The WHF training used role-plays and practice sessions. For the purpose of this study, we investigated only adult (over the age of 18) and adolescent outcomes (ages 12–17), as the key outcomes of AOD use and other health outcomes are only assessed at these levels. All families completed the 10-session intervention and follow-up measures.
Setting and Sample
The setting for the WHF progam was selected through consensus among the CAB. We settled on a church site large enough to house families in the local community. The intended samples size were three to four families to test for feasibility; however, we enrolled eight families. Based on evaluations of the original, Celebrating Famillies! program, a total of 60–75 families would be enrolled for adequate (Kumpfer, 2006; Kumpfer et al., 2002; LutraGroup, 2007); however, that was not the focus nor the intention of this pilot study. Although 33 participants enrolled, we focused on adults and adolescents for whom key outcomes are most germane. The sizes of families ranged from two to seven family members, with the average number of family members equal to 4.13 for the 33 total participants ages 5 and older. Table 1 (adolescents and adults) and Table 2 (adults only) provide the demographics in the forms of ages, gender, family size, household types, religion and spirituality, income and financial strain, educational attainment, and mental health and substance abuse services desired by adolescent and adult subsamples. The following results report findings from (a) baseline, or pretest, before the WHF intervention; (b) posttest, or after the WHF intervention; and (c) where available, at the 6-month follow-up after the WHF intervention. Table 1 displays participant demographics for both adults and adolescents (n = 24), and Table 2 displays demographics for questions asked only for adults (n = 14).
Table 1.
Participant Demographics: Adults and Adolescents.
| Demographic Factors | Adolescents (n = 10), n, % | Adults (n = 14), n, % |
|---|---|---|
| Age | 13.8 (M), range 12–17 | 34 (M), range 19–48 |
| Gender | ||
| Males | 6, 60 | 5, 36 |
| Females | 4, 40 | 9, 64 |
| Household size | 5.5 (M), range 2–8 | 6.1 (M), range 2–8 |
| Primary caregiver | ||
| Mother | 6, 60 | 3, 21 |
| Father | 0 | 1, 7 |
| Mother and father | 4, 40 | 5, 36 |
| Blended family (stepparents etc.) | 0 | 2, 14 |
| Grandparents | 0 | 6, 43 |
| Foster-parent or nonfamily | 0 | 1, 7 |
| Household type | ||
| Single | 6, 60 | 3, 21 |
| two-parent | 3, 30 | 8, 57 |
| Blended or extended | 1, 10 | 2, 14 |
| Religion | ||
| None | 5, 50 | 5, 36 |
| Tribal | 1, 10 | 2, 14 |
| Catholic | 1, 10 | 4, 29 |
| Spiritual, not religious | 1, 10% | 2, 14 |
| Other | 2, 20 | 4, 29 |
| How often participate in spiritual or religious practices | 2.6 (M), range 1–5 | 2.8 (M), range 1–5 |
| Speak tribal language | 4, 40 | 6, 43 |
| Financial strain | 2.5 (M), range 1–5 | 2.8 (M), range 1–5 |
Note. N = 24, caregiver indicates who raised the respondent growing up could check all that apply or more than one; thus, percentages exceed 100%. Extended families can include a stepparent, divorced, remarried, grandparents, aunts, uncles, and so on. Along with the religions displayed, other options included Protestant, Hinduism, Islam, Buddhism, Jewish; participants could check all that apply or more than one; thus, percentages exceed 100%. Response options for how often participate in spirituality included 1 = not at all, 2 = yearly, 3 = monthly, 4 = weekly/biweekly, and 5 = daily/almost daily. Response options for the financial strain question included 1 = not at all difficult, 2 = a little difficult, 3 = somewhat difficult, 4 = very difficult, and 5 = extremely difficult. M = mean; N or n = sample size.
Table 2.
Participant Demographics: Adults.
| Demographic Factor | Adults (n = 14), n, % | |
|---|---|---|
| Number of children | 3.5 (M), range 0–6 | |
| Relationship status | ||
| Married | 6, 43% | |
| Single | 4, 29% | |
| Cohabiting | 3, 21% | |
| Divorced | 1, 7% | |
| Annual income | ||
| US$15–25,000 | 1, 7% | |
| US$25–50,000 | 13, 93% | |
| Working full time | 11, 79% | |
| Education | ||
| Some high school | 3, 2l% | |
| GED/HS | 3, 2l% | |
| Some college | 6, 43% | |
| BA | 2, 14% | |
| How important traditional tribal spiritual practices | 1.6 (M), range 1–3 | |
| Participated in the following practices weekly/special occasions | Yes | No/unsure |
| Smudging | 6, 43% | 8, 64% |
| Talking circle | 7, 50% | 7, 50% |
| Sweat lodges | 2, 14% | 12, 86% |
| How important spirituality | 3.57 (M), range 0–5 | |
| Mental health/substance abuse services desired | ||
| None | 2, 14% | |
| Counseling | 4, 29% | |
| Traditional healing | 10, 7l% | |
| Family strengthening | 12, 86% | |
| Community/education programs | 8, 57% | |
| IPV/family violence | 9, 64% | |
| Parenting | 7, 50% | |
| Youth programs | 8, 57% | |
| Cultural enrichment | 8, 57% | |
| Programs for males | 5, 36% | |
| Programs for females | 4, 29% | |
| Programs for gender-fluid people | l, 7% | |
Note. Response options for how important traditional tribal practices included 1 = Don’t practice (n = 5), 2 = not very important (n = 2), and 3 = very important (n = 6). Smudging was defined as burning sage, cedar, sweetgrass, tobacco, or other herbs for ceremonial and cleansing purposes. Responses indicate when people did participate in tribal spiritual practices, they tended to do so often and they were very important to them; however, a significant number of participants (five to seven or half) had not been exposed or did not practice such traditions. Thus, participants may be fairly shielded from the opportunity to practice such traditions but desired them, as evidenced by responses and the desire for traditional healing programs (71%). Response options for important spirituality included 0 = not at all, 1 = very low, 2 = low, 3 = medium, 4 = high, and 5 = very high. Finally, participants indicated those services they would like to see more of in the community(s) in the rows displaying mental health/substance abuse services desired. GED/HS = general equivalency diploma/high school; BA = bachelor of arts; IPV = intimate partner violence.
Measures
We now describe the outcome measures organized by the ecological levels of the FHORT.
Community and social
Communal mastery (CM).
Another component of resilience is feeling effective and masterful because of feeling connected at the community level. Within relationally focused or collectivist cultures, a sense of shared efficacy, or CM, may be central to resilience (Hobfoll, 2002; Hobfoll et al., 2002). CM is the belief one is capable of attaining goals through close connection with others (Hobfoll, 2002; Hobfoll et al., 2002). We used a 10-item CM Scale (Hobfoll, 2002; Hobfoll et al., 2002) with items such as, “By joining with friends and family, I have a great deal of control over the things that happen to me” and “Working together with friends and family I can solve many of the problems I have.” Responses ranged from 1 = strongly disagree to 4 = strongly agree. Items were summed to find total scores of CM. Internal reliability for pre- and posttests for the adults was .86, and the internal reliability for adolescents was .81.
Social support.
Social support has implications for all health and behavioral health challenges, including AOD abuse and violence. Social support and social undermining (SSSU; Oetzel et al., 2007) were measured with 20 total items that were validated and demonstrated to be internally consistent with a sample of American Indian women (Oetzel et al., 2007). A Likert-type scale ranging from 0 (never) to 2 (often) was used for emotional support (i.e., perceived love, affirmation, and appreciation), critical appraisal (i.e., perceived criticism from others), and isolation (i.e., feel disconnected from others) items. A scale with 0 = no and 1 = yes was used for instrumental support (i.e., perceived available support for assistance and to do things with) items. We focus on the six-item Emotional Support subscale (e.g., “How much do your friends or relatives really care about you?” “How much do they understand the way you feel about things?”) and the five-item Instrumental Support subscale (e.g., “Among the people you know, is there someone you can count on to check in on you regularly?” and “Would lend you money if you needed it in an emergency?”), which were found to be significant for participants. Internal reliability for pre- and posttests was .74 for adults and .85 for adolescents.
Familial
Family resilience.
The FRI (McKinley et al., 2020) was designed from a decade of preliminary research with this tribe to assess family resilience. The items include protective factors (those that buffer against adversity) and promotive factors (those that are supportive, regardless of whether there is a current challenge). Items from this 20-item scale are added for total scores. Higher scores indicate higher levels of family resilience. Internal reliability for pre- and posttests was .87 for adults and .84 for adolescents. Given assumptions of normality, independence, and homogeneity of variance1 to measure the change between FRI scores at pretest, posttest, and 6-month postintervention times, we conducted an ANOVA test.
Holistic resilience.
A key outcome of interest was whether the intervention had a significant effect on one’s resilience, particularly as it related to a holistic wellness approach across individual, relational, cultural, and community domains framed by the FHORT. Thus, we measured this holistic resilience using the Resilience Research Center–Child/Adult Resilience Measures (RRC-C/ARM; Ungar et al., 2011). This screening tool was designed to measure resources (individual, relational, communal, and cultural) available to individuals which may bolster their resilience and developed as part of the International Resilience Project at the RRC in 14 communities around the world (Ungar et al., 2011). We used the 12-item short form using the three-level response set: 0 = no, 1 = sometimes, and 2 = yes. Items assessed individual aspects of resilience (personal skills, peer support, and social support), relational resilience (physical and psychological caregiving), and holistic aspects of resilience (spiritual, educational, and cultural). Items were added for total mean and sum scores of overall levels of reported resilience. Higher levels indicated higher levels of resilience. Internal reliability for pre- and posttests was .80 for adults and .86 for adolescents. Because this was not a primary outcome measure, it was measured at pre- and posttests but not at the 6-month follow-up.
Family environment.
The Family Environment Scale (FES; Moos & Moos, 2009; Teufel-Shone et al., 2005) is a 90-item scale used to test the original, unadapted intervention to assess the health of the family environment. It includes the following 10 subscales: Cohesion (degree of commitment, help, and support from family members); Expressiveness (how much expressing feelings is encouraged), Conflict (amount of openly expressed anger and conflict), Independence (how assertive, self-sufficient, and autonomous people are), Achievement Orientation (how activities, such as school, are framed in an achievement or competitive framework), Intellectual–Cultural Orientation (level of interest in political, intellectual, and cultural activities), Active-Recreational Orientation (participation in social and recreational activities), Moral Religious Emphasis (emphasis on ethical and/or religious issues or values), Organization (importance of clear organization and structure in family activities and responsibilities), and Control (degree to which rules and procedures are used to run the family). Items for each subscale are added for individuals’ subscale totals. For family scores, which were the focus of this pilot, all family members’ raw scores were averaged, creating one family score. Internal reliability for pre- and posttests was .89 for adults and .88 for adolescents. To measure the change between FES scores at pretest, posttest, and where available, 6-month postintervention times, we conducted an ANOVA test.
Relational
IPV.
This intervention focused on developing healthy conflict resolution skills to lower violence. We measured violence using the Revised Conflict Tactics Scales (CTS2; Straus & Douglas, 2004). This widely used self-report measure assesses psychological and physical assaults as well as negotiation in domestic relationships, which is healthy verbal communication and conflict resolution (Straus & Douglas, 2004). The CTS2 has been used in a variety of settings with individuals from varying races, cultures, and ethnic backgrounds, including minority groups represented in this study (Straus & Douglas, 2004). The CTS2 consistently demonstrates sound psychometric properties, with internal consistency, reliability, and construct validity in several studies (Straus & Douglas, 2004). The CTS2 was designed to measure the range and frequency of tactics used in response to conflict with a family member. The CTS2 is a comprehensive 39-item (78-question) self-reported inventory designed to measure five scales: Negotiation (positive verbal conflict resolution skills), Psychological Aggression, Physical Assault, Sexual Coercion, and Injury. Negotiation includes actions taken to resolve conflict through discussion; psychological aggression measures nonverbal aggressive acts; physical assault includes physical violence; sexual coercion focuses on coercing a partner into unwanted sexual activity; and, finally, injury includes partner-induced physical injury (Straus & Douglas, 2004). Respondents rate each item of the aforementioned scales on a 7-point Likert-type frequency scale (0 = this has never happened before, 1 = once in the past year, 2 = twice in the past year, 3 = three to five times in the past year, 4 = six to 10 times in the past year, 5 = 11–20 times in the past year, 6 = more than 20 times in the past year, and 7 = not in the past year, but it did happen before). To create interpretable scores, Values 1 and 2 remained the same, and Values 3–6 were recoded as midpoints (3 = 4, 4 = 8, 5 = 15, 6 = 25; Straus & Douglas, 2004). We created frequency scores (how often) and prevalence (whether this had ever happened) for each subscale. Cronbach’s α was high for the adults who completed this scale (α = .98). The scale was not distributed to adolescents.
Individual
Emotional regulation.
Understanding emotional regulation and dysregulation, or how people identify, accept, and manage emotional experiences, is important for physical health and behavioral health outcomes (Victor & Klonsky, 2016). A common and widely cited measure of emotion dysregulation is the Difficulties With Emotion Regulation Scale (DERS; Gratz & Roemer, 2004), which has been extensively used to facilitate understanding of how emotion dysregulation is associated with psychiatric symptoms. Because emotional regulation is at the heart of mental and behavioral health problems, the DERS has been found to associate with a wide range of mental health issues such as anxiety, borderline personality disorder, depression, posttraumatic stress disorder, and substance/alcohol use and IPV (Gratz & Roemer, 2004; Victor & Klonsky, 2016). The 18-item scale assesses emotional regulation with items related to awareness (e.g., “I pay attention to how I feel”); clarity (e.g. “I have no idea how I am feeling”); goals (e.g., “When I’m upset, I have difficulty getting work done”), impulse control (e.g., “When I become upset, I have difficulty controlling my behaviors”), non-acceptance (e.g., “When I become upset, I am embarrassed for feeling that way”), and strategies (e.g., “When I’m upset, I believe I will remain that way for a long time”). Internal reliability for pre- and posttests was .93 for adults and .90 for adolescents. Responses include 1 = almost never, 2 = sometimes, 3 = about half of the time, 4 = most of the time, and 5 = almost always. First, items for each subscale are summed, and then, all subscales are summed for the total score. Higher scores are indicative of lower emotional regulation skills.
Depressive symptoms.
Depression has been found to be high among some tribal communities and is associated with a host of health and behavioral health problems, such as AOD abuse, violence, diabetes, and other health outcomes of interest. The frequency of an individual’s depressive symptoms was measured by the Patient Health Questionnaire-9 (PHQ-9; Kroenke et al., 2001), a tool used and recommended for use with Indigenous peoples (Urban Indian Health Institute, 2012) and has also been used with this tribe (Burnette et al., 2020). Participants indicated how often over the past 2 weeks they were bothered by “feeling down, depressed, or hopeless”; “feeling tired or having little energy”; and “trouble falling or staying asleep, or sleeping too much.” For each of the nine items, four response options were available: 0 = not at all, 1 = several days, 2 = more than half the days, and 3 = nearly every day. When summed, the nine scale items had a possible range of 0–27, and the total score corresponded to an individual’s level of depressive symptoms along a continuum scored as 0–4 = minimal, 5–9 = mild, 10–14 = moderate, 15–19 = moderately severe, and 20–27 = severe depression. PHQ-9 scores of 10 or higher indicate clinical depression, a cutoff point validated across numerous studies. Cronbach’s α for the study sample was .95. Because this was a tertiary measure, this was measured at pre- and posttests but not at the 6-month follow-up.
Youth health.
We also wanted to measure overall wellness among our youth. The SCREENing and Promotion for Health-Related Quality of Life in Children and Adolescents—A European Public Health Perspective (KIDSCREEN) (Power et al., 2019; Silva et al., 2018) is a generic health-related quality of life measure for children and adolescents was developed as part of a European project called and funded by the European Commission. The KIDSCREEN-27 was developed to construct a shorter version of the KIDSCREEN-52 with a minimum of information loss and with good psychometric properties. The KIDSCREEN-27 has five dimensions: physical well-being (five items), psychological well-being (seven items), autonomy and parents (seven items), peers and social support (four items), and school environment (four items). Responses range from 1 = never to 5 = always. Items are summed and/or means are calculated for a total health-related quality of life. Cronbach’s α was high for adolescents who completed this scale (α = .93). Because this was a tertiary measure, this was measured at pre- and posttests but not at the 6-month follow-up.
Self-rate health practices.
Similarly, we wanted to assess reported health practices among adults. Participants completed the 28-item Self-Rated Abilities for Health Practices Scale (H. Becker et al., 1993), which is a 5-point scale (0 = not at all to 4 = completely) to measure perceived ability to implement health-promoting behaviors. Health self-efficacy has been found to be associated with cardiovascular disease (Saquib et al., 2013), and preliminary research indicates self-efficacy may be helpful in preventing alcohol abuse (Gause et al., 2018), including with NAs (McKinley et al., 2020). Participants indicate the extent to which they perform health practices related to the four domains of exercise (“Do exercises that are good for me”), nutrition (“Eat a balanced diet”), responsible health practice (“Watch for negative changes in my body’s condition”), and psychological well-being (“Change things to reduce my stress”). Scores range from 0 to 112, with higher scores indicating greater feelings of self-efficacy related to health practices. Cronbach’s α for the study sample was .93.
Sugar-sweetened beverages.
Finally, sugar-sweetened beverages or nondiet soda, fruit drinks that are not 100% juice, sweet tea, sports drinks, and energy drinks are the largest sources of added sugars for people in the United States, and their frequent consumption is associated with obesity, type 2 diabetes, heart problems, hypertension, and other health problems (Lundeen et al., 2018). We infused a culturally adapted nutrition component into the WHF program. As such, we asked adults and adolescents two questions from the Behavioral Risk Factor Surveillance System (Bhan et al., 2015; Bowlin et al., 1996; Salvail & Smith, 2007): “About how often do you drink regular soda or pop that contains sugar? Do not include diet soda or diet pop” and “About how often do you drink sweetened fruit drinks, such as Kool-Aid, cranberry cocktail, and lemonade? Include fruit drinks you made at home and added sugar to.” With responses from 0 = never/rarely, 1 = less than monthly, 2 = monthly, 3 = 2 or more times per month, 4 = weekly, 5 = 2 or more times per week, 6 = daily, and 7 = two or more times per day. These items were added to create sum and mean scores for these items.
AOD abuse.
Youth alcohol use was measured by the Car, Relax, Alone, Forget, Friends, Trouble (CRAFFT; Center for Adolescent Substance Abuse Research, 2016; Cummins et al., 2003), a nine-item evidenced-based screening tool to assess for AOD misuse, includes components for assessing AOD use separately and holistically (Center for Adolescent Substance Abuse Research, 2016; Cummins et al., 2003). CRAFFT is a mnemonic acronym of the first letters of key words in the six screening questions. This behavioral health screening tool is recommended for use with children under the age of 21 by the American Academy of Pediatrics’ Committee on Substance Abuse (Center for Adolescent Substance Abuse Research, 2016; Cummins et al., 2003). We also used the Adolescent Alcohol and Drug Involvement Scale (Moberg, 1983; Moberg & Hahn, 1991). Adult alcohol use was measured by the 10-item Alcohol Use Disorder Identification Test (Saunders et al., 1993), which identifies alcohol consumption, drinking behaviors, and alcohol-related problems. Parental drug use was measured by the 10-item Drug Abuse Screening Test (Skinner, 1982), a reliable form to assess drug use with adults.
Data Analysis
After establishing normality of data, homogeneity in variance, and missing data (there were no missing data in this case), we examined descriptive statistics for the sample. Next, paired sample t tests were utilized to examine significant changes between the pre- and posttest on aforementioned measures, where appropriate. Where available, we then used ANOVA tests to examine the change between pre-, post-, and 6-month postintervention. We examined effect sizes for each test (Cohen’s d for t tests and η2 for ANOVA). Finally, we conducted Tukey’s post hoc analysis to examine significant differences between each of the means.
Results
Regarding participant flow, all eight families and participants began with completing the pretest survey. Next, all eight families completed the 10 WHF sessions weekly, each lasting 2½ hr. These sessions were held at a community church as determined by spacing and the CAB judgment about the optimum facilitates. Participants then completed the posttest survey and 6-month follow-up surveys. Regarding demographics, 12 of 14 (86%) participants indicated a desire for community family strengthening programs, and 10 of 14 (71%) expressed a desire for use of traditional healing methods to address behavioral health needs (see Table 2); however, over half have not been exposed to or able to practice traditional healing methods, such as talking circles, smudging, and/or sweat lodges. Thus, given that this intervention incorporates the family talking circle, the intervention fills a gap in desired services.
Regarding main outcomes, the intervention prevented AOD abuse, as reported by the adolescent sample (n = 10). Thus, adolescents reported no smoking, alcohol use, nor drug use across the pretest, posttest, nor 6-month follow-ups. We also saw a reduction in alcohol use among parents. With only 14 participants, the statistical significance of this reduction was lower than 0.05. Parents’ drug use was negligible, as participants in this sample did not report significant levels of drug use. Given that we found any significant finding in such a small sample, indicating that, with a larger sample, these findings would likely be even more robust. We now detail the pilot significant findings.
As Table 3 depicts, across both adults and adolescents, and as predicted by hypotheses, we found significant behavioral health improvements in emotional regulation, family resilience, and family functioning; resilience across individual, relational, communal, and cultural levels; CM (a measure of communal resilience); social support; and a reduction in the consumption of sugar-sweetened beverages. Several measures were only assessed for adults, as they were not designed nor appropriate for children. We found improvements and reductions in IPV and an increase in healthy conflict resolution skills. We found significant reductions in depressive symptoms; we also found significant improvements in self-rated ability for health practices across nutrition, exercise, and responsible health practices domains and as a whole (all domains holistically). Likewise, we found adolescent health related to quality of life improved significantly. The focus now turns to the details of these results (see Table 3 for a snapshot).
Table 3.
Summary of Key Outcomes.
| 95% Confidence Interval | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Level | Outcome | Measure | Sample | Time points and Subscale | Test Results (t/F) | p | Effect Size | Lower | Upper | Reliability |
| Community | Communal mastery | CM | Both | Pre/post | t(23) = −2.58 | .017 | −.53 | −.95 | −.09 | α = .86/.81 |
| Social support | SSSU | Both | Pre/post | α = .74/.85 | ||||||
| Emotional | t(22) = −3.05 | .006 | −.64 | −1.08 | −.18 | |||||
| Instrumental | t(22) = −2.33 | .029 | −.49 | −.92 | −.05 | |||||
| Both | t(23) = −3.84 | .001 | −.78 | −1.23 | −.32 | |||||
| Familial | Resilience | RRC-C/ARM | Both | Pre/post | t(9) = −2.54 | .018 | −.52 | −.94 | −.09 | α = .80/.86 |
| Family resilience | FRI | Both | Pre/post/6mf | F(2, 69) = 4.51 | .014 | .12 | .01 | .25 | α = .87/.84 | |
| Family environment | FES | Both | Pre/post/6mf | α = .89/.88 | ||||||
| Cohesion | F(2, 69) = 5.17 | .008 | .07 | .00 | .19 | |||||
| Independence | F(2, 69) = 4.90 | .010 | .04 | .00 | .15 | |||||
| Cultural/intellectual | F(2, 69) = 3.84 | .026 | .06 | .00 | .07 | |||||
| Moral | F(2, 69) = 3.05 | .054 | .04 | .00 | .15 | |||||
| Relational | Intimate partner violence | CTS2 | Adults | Pre/post/6mf | α = .98 | |||||
| Psychological aggression | F(2, 30) = 6.87 | .003 | .30 | .05 | .49 | |||||
| Physical aggression | F(2, 30) = 4.18 | .027 | .25 | .00 | .46 | |||||
| Negotiation (pre/post) | t(9) = −3.00 | .005 | −1.15 | −1.94 | −.32 | |||||
| Individual—mental/physical | Emotional regulation | DERS | Both | Pre/post/6mf | F(2, 66) = 5.61 | .006 | .15 | .02 | .29 | α = .93/.90 |
| Depressive symptoms | PHQ-9 | Adults | Pre/post | t(13) = 2.4 | .031 | .65 | .06 | 1.21 | α = .95 | |
| Health-related quality of life | KIDSCREEN | Adol. | Pre/post | t(9) = −2.22 | .054 | −.70 | −1.38 | .01 | α = .93 | |
| Self-rated health practices | SRAHPS | Adults | Pre/post (overall) | t(13) = −3.05 | .009 | −.82 | −1.41 | −.20 | α = .93 | |
| Nutrition | t(13) = −2.1 | .052 | −.57 | −1.13 | .00 | |||||
| Exercise | t(13) = −2.4 | .025 | −.68 | −1.22 | −.08 | |||||
| Responsible health practices | t(13) = −3.0 | .010 | −.80 | −1.40 | −.19 | |||||
| Sugar beverage consumption | SRAHPS | Both | Pre/post | t(22) = 2.15 | .043 | .45 | .01 | .86 | NA | |
Note. For pre/post/6 mf, we conducted analysis of variance tests, which produce the F statistic, indicating whether significant changes were found across the time periods as a whole. The paired sample t tests were conducted where appropriate indicating significant changes from pre- to posttests. Levels of significance (p values) are indicated below the .05 cutoff point. If both sum and means were calculated, effect sizes are calculated for means scores. Adol. = the adolescents subsample; α = Cronbach’s α of the reliability of each scale; CM = communal mastery; RRC-C/ARM = Resilience Research Center–Child/Adult Resilience Measures; SSSU = Social Support and Social Undermining; FRI = Family Resilience Inventory; FES = Family Environment Scale; CTS2 = Revised Conflict Tactics Scales; DERS = Difficulties With Emotion Regulation Scale; PHQ-9 = Patient Health Questionnaire-9; SRAHPS = Self-rated Health Practices.
Community
Paired sample t tests indicated average levels of perceived CM increased from pretest (sum = 29.7 ± 5.4; M = 2.97 ± .54) to the posttest (sum = 32.5 ± 5.0; M = 3.25 ± .50) at a significant level with a medium effect size. With effect sizes ranging from medium to high (see Table 3), we found significant improvements across the SSSU Scales: (a) emotional support: Average levels of perceived emotional support increased from pretest (sum = 9.8 ± 3.9; M = 1.63 ± .65) to posttest (sum = 11.09 ± 2.9; M = 1.87 ± .42) at a significant level; (b) instrumental support: Average levels of perceived instrumental support increased from pretest (sum = 5.13 ± 2.1; M = 1.07 ± .29) to posttest (sum = 5.87 ± 2.0; M = 1.18 ± .39) at a significant level; and (c) emotional and instrumental social support: Average levels of perceived emotional and instrumental social support increased from pretest (sum = 14.5 ± 5.7; M = 7.35 ± 2.7) to posttest (sum = 16.42 ± 5.0; M = 8.31 ± 2.3) at a significant level.
Familial
Regarding holistic resilience, according to the RRC-C/ARM, t tests indicated average levels of resilience increased from pretest (sum = 20.7 ± 3.7; M = 1.7 ± .31) to posttest (sum = 22.37 ± 2.4; M = 1.9 ± .20) at a significant level with a low effect size. These results indicate resilience levels significantly increased from pre- to posttest. A one-way ANOVA found significant differences between mean FRI scores. The Tukey’s post hoc test revealed a significant difference between pretest mean scores (16.8 ± 3.8) and 6-month follow-up mean scores (19.4 ± 1.0; p = .011) but not between posttest mean scores (18.3 ± 3.2) and pretest mean scores, nor posttest and 6-month follow-up mean scores. The overall effect size for the FRI was low, likely due to this variability in significance across time points.
A one-way ANOVA found significant differences between mean FES scores for the following subscales: cohesion, F(2, 69) = 5.17, p = .008; independence, F(2, 69) = 4.90, p = .010; intellectual–cultural orientation, F(2, 69) = 3.84, p = .026; and moral religious emphasis, F(2, 69) = 3.05, p = .054, but not expressiveness, achievement orientation, active-recreational orientation, organization, or control. For cohesion, the Tukey’s post hoc test revealed a significant difference between pretest mean scores (6.5 ± .93) and posttest mean scores (7.3 ± 1.1, p = .006) but not between 6-month follow-up mean scores (6.9 ± .80) and pretest mean scores or posttest and 6-month follow-up mean scores. For independence, the Tukey’s post hoc test revealed a significant difference between posttest mean scores (6.0 ± .95) and 6-month follow-up mean scores (5.2 ± 1.3, p = .009) but not 6-month follow-up and pretest mean scores (5.4 ± .68) or pre- and posttest mean scores (the latter of which had a p value of .084 but not at the statistically significant level). For intellectual–cultural, the Tukey’s post hoc test revealed a significant difference between posttest mean scores (5.7 ± .70) and 6-month follow-up mean scores (4.8 ± 1.3, p = .032) but not 6-month follow-up and pretest mean scores (4.9 ± 1.6) or pre- and posttest mean scores (the latter of which had a p value of .083 but not at a statistically significant level). For moral or religious orientation, the Tukey’s post hoc did not reveal a significant difference between pretest mean scores (5.1 ± 1.0), posttest mean scores (5.8 ± 1.2), and 6-month follow-up mean scores (5.2 ± 1.0, p = .011); the difference between pre- and posttest mean scores had a p value of .069 but did not reach the level of statistical significance. Like the FRI and given variability in significance across time points, the effect sizes for the FES subscales were low.
Relational
To measure the change between CTS2 scores at pretest, posttest, and where available, 6-month postintervention times, we conducted an ANOVA test. A one-way ANOVA found significant differences between mean CTS2 scores for the frequency of partner psychological aggression (being a victim of psychological violence) and prevalence of partner physical aggression (being a victim of physical violence). According to the frequency of partner psychological aggression scale, the Tukey’s post hoc test revealed a significant difference between pretest mean scores (8.0 ± 8.5) and posttest mean scores (4.1 ± 5.8, p = .007) and 6-month follow-up mean scores (2.1 ± 3.2, p = .010) but not posttest and 6-month follow-up mean scores. According to the prevalence of Partner Physical Aggression Scale, the Tukey’s post hoc test revealed a significant difference between pretest mean scores (.91 ± .94) and 6-month follow-up mean scores (.67 ± 1.0; p = .024) but not pre- and posttest mean scores (.50 ± .84) or posttest and 6-month follow-up mean scores. The effect sizes for these outcomes were low to medium. t tests for the negotiation subscales indicated the frequency of positive negotiation skills increased from pretest (13.9 ± 15.2) to posttest (24.0 ± 11.5) at a significant level, t(9) = −3.00, p = .005, indicating whereas partners’ psychological and physical aggression decreased with the introduction of the intervention, positive conflict resolution skills increased. The effect size of this difference was very high (over 1).
Individual
To measure the change between DERS scores at pretest, posttest, and where available, 6-month postintervention times, we conducted an ANOVA test. One outlier was removed before analysis. A one-way ANOVA found significant differences between mean DERS scores, F(2, 66) = 5.61, p = .006. The Tukey’s post hoc test revealed a significant difference between pretest mean scores (41.4 ± 12.5) and 6-month follow-up mean scores (31.4 ± 9.6, p = .003) but not between posttest mean scores (35.6 ± 8.1) and pretest mean scores, or posttest and 6-month follow-up mean scores. The effect size overall was low, likely due to variability in mean differences across time points. t tests indicated average levels of depressive symptoms decreased from pretest (6.9 ± 8.0) to posttest (2.7 ± 3.7) at a significant level. This reduced the average level of depressive symptoms from mild depressive levels to little or no depressive symptoms. The effect size of this difference was medium to high.
Among youth, t tests indicated average levels of health-related quality of life increased from pretest (sum = 86.0 ± 20.5; M = 3.2 ± .76) to posttest (sum = 101.3 ± 14.9; M = 3.8 ± .55) at a significant level. The effect size of this difference was medium to high. Among adults, self-related health practices improved for (a) nutrition: The t test indicated average levels of nutrition health practices increased from pretest (14.7 ± 6.6) to posttest (18.2 ± 5.4) at a significant level; (b) exercise: The t test indicated average levels of exercise health practices increased from pretest (12.4 ± 7.5) to posttest (16.6 ± 6.3) at a significant level; (c) responsible health practices: The t test indicated average levels of responsible health practices increased from pretest (16.9 ± 8.1) to posttest (22.2 ± 3.9) at a significant level; and (d) total self-rated health practices scores: The t test indicated average levels of total health practices increased from pretest (60.6 ± 24.5) to posttest (78.1 ± 15.3) at a significant level. These scales and subscales ranged from medium/high to high effect sizes. Finally, with a medium effect size, the average levels of reported consumption of sugar-sweetened beverages decreased from pretest (sum = 20.07 ± 7.5; M = 3.49 ± 1.7) to posttest (sum = 20.21 ± 10.3; M = 3.33 ± 1.7) at a significant level: sum and mean.
Discussion and Applications to Practice
Overall, we found positive outcomes spanning individual (resilience, health behaviors and quality of life, emotional regulation, and depressive symptoms), relational (social support, violence, and conflict resolution), familial (family resilience and family environment), and community (CM) levels from the pilot alone. AOD abuse was prevented among adolescents and lowered among adults, though, due to sample size limitations, this reduction did not reach statistical significance. At the community level, perceived community resilience, as measured by CM, increased with the introduction of the intervention. Results from the SSSU Scale indicate participants reported feeling more emotionally supported after the intervention and feeling they could turn to others for help. Both of these community-level improvements demonstrated medium-to-high effect sizes. These strong results likely bolster overall resilience, health, and well-being. The WHF program focuses on choosing safe people to trust, setting clear boundaries, and maintaining healthy relationships. These mechanisms may lead participants to choose healthier social support and enhance their ability to use their support networks through skill building. Moreover, the coming together of families for strength and resilience building may create community and positive social support networks.
At the family level, the WHF program specifically targets resilience, and results indicate holistic resilience levels significantly increased from pre- to posttest for adolescents and adults. Participants leveraged their individual, relational, communal, and cultural assets, which led to an increase in their resilience and well-being. Results also indicated both samples’ family resilience improved. Using the NA-specific FRI (McKinley et al., 2019) indicated levels of reported family resilience increased across all time points, but these results did not reach the level of statistical significance until the 6-month follow-up, contributing to a lower effect size. Because of the small sample, it may have taken a longer time after the intervention to develop new familial patterns, which are complex. These patterns may not have been well established immediately after the last session of the intervention. Results indicated aspects of the family environment improved with the intervention, such as family support, family independence, family involvement in cultural and community affairs, and families’ emphasis on living according to their morals and values. Similar to the FRI, some post hoc tests indicated levels of significance varying between individual pretests, posttests, and 6-month tests, likely due to the small sample having limited statistical power, lowering the overall effect size of these changes. Also, it likely would take time after the intervention to develop new familial patterns, and these patterns may not yet have been fully established at the time of the test.
At the relational level, participants reported experiencing psychological and physical abuse at lower levels and increased positive conflict resolution skills with the introduction of the intervention. The frequency of psychological aggression decreased significantly across all time points. Partners’ positive conflict resolution skills improved after the program. Despite small samples, the effect sizes of these improvements were low to medium for psychological and physical aggression, yet quite high for nonviolent conflict resolution. These robust results provide support that the WHF program may provide couples tools to negotiate in constructive ways.
At the individual level, results indicate, for emotional regulation, like family resilience and components of improvements in the family environment, the ability to regulate one’s emotions improved by the 6-month follow-up. Moreover, the robust results regarding depressive symptoms indicate participants’ overall feelings of depression decreased after the intervention, and the effect size of this was approached high. Youth results demonstrate the health-related quality of life that spanned across physical, psychological, social, and school well-being improved from pre- to posttest. Adult participants’ health practices related to nutrition, exercise, and health awareness improved as well as health practices overall. Finally, participants tended to drink less sugar-sweetened beverages after the intervention, which is positive for diabetes and obesity preventative perspectives. These health-related outcomes were quite robust, with medium-to-high effect sizes throughout. Given the co-occurrence of poor nutrition and AOD abuse, this holistic improvement in wellness is quite promising.
The greatest limitation of this research was its small sample sizes and preexperimental design; given the aim of the study was to test the WHF program for feasibility and acceptability, finding significant results is promising but preliminary. These results are not generalizable but may be relevant for other tribal contexts. This pilot study was initially planned to assess the feasibility and acceptability of the WHF program and lacked adequate power to detect true differences. Thus, weak or absent findings are not indicative of no significant relationship but rather a lack of power to detect these differences. Current efficacy trials with adequate power are currently underway. Given no adolescents reported AOD abuse, more high-functioning families and adolescents may have self-selected into this pilot. This study had several strengths, namely that all measures were either developed and validated with focal NA communities (McKinley et al., 2019, 2020) or had been piloted in past research. (McKinley et al., 2019). This research was a preexperimental design. Replication and scaling up this investigation in the full efficacy trial underway will provide a fuller understanding of WHF and its impacts.
Preliminary results of this research indicate the WHF program is a promising NA-specific way to enhance resilience and wellness while reducing and preventing AOD abuse and IPV and improving conflict resolution in NA families. Not only does the WHF program address key factors driving disparities, it also successfully promoted holistic resilience. Given preliminary positive results, WHF program is a promising intervention to address inequities in AOD abuse, violence, and well-being in a holistic and culturally grounded manner. This research used CBPR to include stakeholders’ perspectives to improve sustainability. The investment in NA infrastructure and nurturing NA leaders as CHRs enables the self-determination and continuation for many years. Many CAB members have furthered their professional and higher education credentials throughout this research, addressing a gap in highly skilled NA professionals to address community needs.
Thus, the WHF program provides a promising NA intervention that (a) focuses on trauma and AOD abuse, (b) is family-focused, (c) is culturally grounded, (d) uses the NA FHORT, and (e) martials CBPR for greater sustainability, engagement, and efficacy. The WHF program both contribute to immediate improvements in health and the intermediary building of family skills as well as IPV and AOD prevention and long-term development of infrastructure and leaders for greater equity (Burnette et al., 2014; McKinley et al., 2019). The importance of developing NA interventions with community members, incorporating NA-specific treatment modalities, and engaging NA members in facilitating, coordinating, and engaging participants is an essential way to provide not only acceptable and culturally congruent interventions but also interventions that are effective (Jumper-Reeves et al., 2014).
Given behavioral, psychological, physical, and social health are interrelated, social workers can seek culturally relevant interventions to address these factors holistically. The WHF program is one such holistic intervention that addresses community, social, familial, relational, and individual factors, bolstering protective factors and reducing risk factors in promising ways. It includes a primary determinant of youth AOD abuse, the family (Dusenbury, 2000; Substance Abuse and Mental Health Services Association, 2004), and seeks to promote the coping and resilience of all members in developmentally tailored and feasible ways. Although future research is necessary to establish true efficacy, the WHF program lends support to reducing and preventing AOD abuse and IPV with broad and inclusive strengths, improving not only individuals coping skills but also the family environment that provides the context and supports for individual members. We recommend additional work to provide culturally tailored, evidenced-based interventions that work within the worldview of NAs.
Acknowledgments
The authors thank the dedicated work and participation of the tribes and collaborators who contributed to this work. We thank Jennifer Lilly, Jessica Liddell, Hannah Knipp, Jennifer Martin, Tamela Solomon, Nikki Comby, Harold Comby, Patricia Haynes, Kathleen Ferris, Juannina Mingo, Dan Isaac, Clarissa Stewart, Mariah Lewis, and Jeremy Chickaway for their incredible commitment, time, and energy devoted to the WHF program. We also thank Dana Kingfisher, Emily Matt Salois, d’Shane Barnett, and all the staff at the All Nations Health Center in Missoula, Montana, for their important contributions to the pilot program. We thank Charles R. Figley, Karina Walters, James Allen, and Tonette Krousel-Wood for their support and mentorship for this pilot program. We thank The National Association for Children of Addiction for the original program that the WHF program was developed from and White Bison for introducing cultural components.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Fahs-Beck Fund for Research and Experimentation Faculty Grant Program (grant number #552745), The Silberman Fund Faculty Grant Program (grant #552781), the Newcomb College Institute Faculty Grant at Tulane University, University Senate Committee on Research Grant Program at Tulane University, the Global South Research Grant through the New Orleans Center for the Gulf South at Tulane University, The Center for Public Service at Tulane University, Office of Research Bridge Funding Program support at Tulane University, and the Carol Lavin Bernick Research Grant at Tulane University. This work was also supported, in part, by Award K12HD043451 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health (Krousel-Wood-PI; Catherine McKinley [formerly Burnette]—Building Interdisciplinary Research Careers in Women’s Health [BIRCWH] scholar) and by U54 GM104940 from the National Institute of General Medical Sciences of the National Institutes of Health, which funds the Louisiana Clinical and Translational Science Center. Research reported in this publication was supported by the National Institute on Alcohol Abuse and Alcoholism of the National Institutes of Health under Award Number R01AA028201.
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Used Levene’s test.
References
- American Psychological Association. (2010). APA fact sheet, mental health disparities: American Indian and Alaska Natives. http://www.psych.org/Share/OMNA/Mental-Health-Disparities-Fact-Sheet-American-Indians.aspx
- Bassuk E, Dawson R, & Huntington N (2006). Intimate partner violence in extremely poor women: Longitudinal patterns and risk markers. Journal of Family Violence, 21(6), 387–399. 10.1007/s10896-006-9035-1 [DOI] [Google Scholar]
- Becker H, Stuifbergen A, Oh HS, & Hall S (1993). Self-rated abilities for health practices: A health self-efficacy measure. Health Values: The Journal of Health Behavior, Education & Promotion, 17(5), 42–50. [Google Scholar]
- Becker SA, Affonso DD, & Beard MBH (2006). Talking circles: Northern plains tribes American Indian women’s views of cancer as a health issue. Public Health Nursing, 23(1), 27–36. 10.1111/j.0737-1209.2006.230105.x [DOI] [PubMed] [Google Scholar]
- Bhan N, Kawachi I, Glymour MM, & Subramanian SV (2015). Time trends in racial and ethnic disparities in asthma prevalence in the United States from the Behavioral Risk Factor Surveillance System (BRFSS) Study (1999–2011). American Journal of Public Health, 105(6), 1269–1275. 10.2105/AJPH.2014.302172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowlin SJ, Morrill BD, Nafziger AN, Lewis C, & Pearson TA (1996). Reliability and changes in validity of self-reported cardiovascular disease risk factors using dual response: the behavioral risk factor survey. Journal of Clinical Epidemiology, 49(5), 511–517. 10.1016/0895-4356(96)00010-8 [DOI] [PubMed] [Google Scholar]
- Breiding MJ, Chen J, & Black MC (2014). Intimate partner violence in the United States—2010. National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. https://www.cdc.gov/violenceprevention/pdf/cdc_nisvs_ipv_report_2013_v17_single_a.pdf [Google Scholar]
- Burnette CE (2015). Historical oppression and intimate partner violence experienced by Indigenous women in the U.S.: Understanding connections. Social Services Review, 89(3), 531–563. http://www.jstor.org/stable/10.1086/683336 [Google Scholar]
- Burnette CE (2016). Historical oppression and Indigenous families: Uncovering potential risk factors for Indigenous families touched by violence. Family Relations, 65(2), 354–368. 10.1111/fare.12191 [DOI] [Google Scholar]
- Burnette CE (2018). Family and cultural protective factors as the bedrock of resilience for Indigenous women who have experienced violence. Journal of Family Social Work, 21(1), 45–62. 10.1080/10522158.2017.1402532 [DOI] [Google Scholar]
- Burnette CE, Boel-Studt S, Renner LM, Figley CR, Theall KP, Miller, Scarnato J, & Billiot S (2020). The family resilience inventory: A culturally grounded measure of intergenerational family protective factors. Family Process, 59(2), 695–708. 10.1111/famp.12423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burnette CE, & Figley CR (2017). Historical oppression, resilience, and transcendence: Can a holistic framework help explain violence experienced by Indigenous peoples? Social Work, 62(1), 37–44. 10.1093/sw/sww065 [DOI] [PubMed] [Google Scholar]
- Burnette CE, Ka’apu K, Scarnato JM, & Liddell J (2020). Cardiovascular health among U.S. Indigenous peoples: A holistic and sex-specific systematic review. Journal of Evidence-Based Social Work (2019), 17(1), 24–48. 10.1080/26408066.2019.1617817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burnette CE, Sanders S, Butcher HK, & Rand JT (2014). A toolkit for ethical and culturally sensitive research: An application with Indigenous communities. Ethics and Social Welfare, 8(4), 364–382. 10.1080/17496535.2014.885987 [DOI] [Google Scholar]
- Butler L, Popkin BM, & Poti JM (2018). Associations of alcoholic beverage consumption with dietary intake, waist circumference, and body mass index in US adults: National health and nutrition examination survey 2003–2012. Journal of the Academy of Nutrition and Dietetics, 118(3), 409–420. 10.1016/j.jand.2017.09.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Adolescent Substance Abuse Research. (2016). The CRAFFT screening tool. http://www.ceasar-boston.org/CRAFFT/index.php
- Cummins LH, Chan KK, Burns KM, Blume AW, Larimer M, & Marlatt GA (2003). Validity of the CRAFFT in American-Indian and Alaska-Native adolescents: Screening for drug and alcohol risk. Journal of Studies on Alcohol, 64(5), 727–732. 10.15288/jsa.2003.64.727 [DOI] [PubMed] [Google Scholar]
- Darke S (2010). The toxicology of homicide offenders and victims: A review. Drug and Alcohol Review, 29(2), 202–215. 10.1111/j.1465-3362.2009.00099.x [DOI] [PubMed] [Google Scholar]
- Dickerson D, Brown RA, Johnson CL, Schweigman K, & D’Amico EJ (2015). Integrating motivational interviewing and traditional practices to address alcohol and drug use among urban American Indian/Alaska Native youth. Journal of Substance Abuse Treatment, 65, 26–35. 10.1016/j.jsat.2015.06.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixon AL, Yabiku ST, Okamoto SK, Tann SS, Marsiglia FF, Kulis S, & Burke AM (2007). The efficacy of a multicultural prevention intervention among urban American Indian youth in the southwest US. The Journal of Primary Prevention, 28(6), 547–568. 10.1007/s10935-007-0114-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dusenbury L (2000). Family-based drug abuse prevention programs: A review. Journal of Primary Prevention, 20(4), 337–352. 10.1023/A:1021366721649 [DOI] [Google Scholar]
- Few AL, & Rosen KH (2005). Victims of chronic dating violence: How women’s vulnerabilities link to their decisions to stay. Family Relations, 54(2), 26–279. 10.1111/j.0197-6664.2005.00021.x [DOI] [Google Scholar]
- Gause NK, Elliott JC, Delker E, Stohl M, Hasin D, & Aharonovich E (2018). Association between change in self-efficacy to resist drinking and drinking behaviors among an HIV-infected sample: Results from a large randomized controlled trial. Journal of Health Psychology, 23(6), 829–839. 10.1177/1359105316664127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gone JP, & Trimble JE (2012). American Indian and Alaska Native mental health: Diverse perspectives on enduring disparities. Annual Review of Clinical Psychology, 8, 131–160. 10.1146/annurev-clinpsy-032511-143127 [DOI] [PubMed] [Google Scholar]
- Gratz KL, & Roemer L (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the Difficulties in Emotion Regulation Scale. Journal of Psychopathology and Behavioral Assessment, 26(1), 41–54. https://www.sispse.it/wp-content/uploads/2019/05/Gratz-Roemer-2004-DERS-DERS-DERS.pdf [Google Scholar]
- Griner D, & Smith TB (2006). Culturally adapted mental health intervention: A meta-analytic review. Psychotherapy: Theory, Research, Practice, Training, 43(4), 531–548. http://hdl.lib.byu.edu/1877/2796 [DOI] [PubMed] [Google Scholar]
- Hawkins EH, Cummins LH, & Marlatt GA (2004). Preventing substance abuse in American Indian and Alaska Native youth: Promising strategies for healthier communities. Psychological Bulletin, 130(2), 304–323. 10.1037/0033-2909.130.2.304 [DOI] [PubMed] [Google Scholar]
- Hobfoll SE (2002). Social and psychological resources and adaptation. Review of General Psychology, 6(4), 307–324. 10.1037/1089-2680.6.4.307 [DOI] [Google Scholar]
- Hobfoll SE, Jackson A, Hobfoll I, Pierce CA, & Young S (2002). The impact of communal-mastery versus self-mastery on emotional outcomes during stressful conditions: A prospective study of Native American women. American Journal of Community Psychology, 30(6), 853–871. 10.1023/A:1020209220214 [DOI] [PubMed] [Google Scholar]
- Jumper-Reeves L, Dustman PA, Harthun ML, Kulis S, & Brown EF (2014). American Indian cultures: How CBPR illuminated intertribal cultural elements fundamental to an adaptation effort. Prevention Science, 15(4), 547–556. 10.1007/s11121-012-0361-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirmayer LJ, Sehdev M, & Isaac C (2009). Community resilience: Models, metaphors, and measures. International Journal of Indigenous Health, 5(1), 62–117. 10.3138/ijih.v5i1.28978 [DOI] [Google Scholar]
- Klostermann K, Kelley ML, Mignone T, Pusateri L, & Fals-Stewart W (2010). Partner violence and substance abuse: Treatment interventions. Aggression and Violent Behavior, 15(3), 162–166. 10.1016/j.avb.2009.10.002 [DOI] [Google Scholar]
- Kraanen FL, Vedel E, Scholing A, & Emmelkamp PM (2013). The comparative effectiveness of integrated treatment for substance abuse and partner violence (I-StoP) and substance abuse treatment alone: A randomized controlled trial. BMC Psychiatry, 13(1), 1–14. 10.1186/1471-244X-13-189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JB (2001). The PHQ-9. Journal of General Internal Medicine, 16(9), 606–613. 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumpfer KL (2006). Year one (FY05–06) evaluation report for celebrating families. https://celebratingfamilies.net/PDF/YearOneEvaluationReport_new.pdf
- Kumpfer KL, Alvarado R, Smith P, & Bellamy N (2002). Cultural sensitivity and adaptation in family-based prevention interventions. Prevention Science, 3(3), 241–246. 10.1023/A:1019902902119 [DOI] [PubMed] [Google Scholar]
- Lau AS (2006). Making the case for selective and directed cultural adaptations of evidence-based treatments: Examples from parent training. Clinical Psychology: Science and Practice, 13(4), 295–310. 10.1111/j.1468-2850.2006.00042.x [DOI] [Google Scholar]
- Lum C (2008). The development of family resilience: Exploratory investigation of a resilience program for families impacted by chemical dependency. Celebrating Families! http://www.celebratingfamilies.net/PDF/EvalutionReport_ChrisLum.pdf [Google Scholar]
- Lundeen EA, Park S, Pan L, & Blanck HM (2018). Daily intake of sugar-sweetened beverages among US adults in 9 states, by state and sociodemographic and behavioral characteristics, 2016. Preventing Chronic Disease, 15, E154, 1–7. 10.5888/pcd15.180335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- LutraGroup. (2007). Final outcome evaluation May 2007 report for Lucile Packard Foundation for Children’s Health. Celebrating Families! http://www.celebratingfamilies.net/PDF/FinalOutcomeEvalution_LutraGroup.pdf [Google Scholar]
- Marsiglia FF, & Booth JM (2015). Cultural adaptation of interventions in real practice settings. Research on Social Work Practice, 25(4), 423–432. 10.1177/1049731514535989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masten AS, & Monn AR (2015). Child and family resilience: A call for integrated science, practice, and professional training. Family Relations, 64(1), 5–21. 10.1111/fare.12103 [DOI] [Google Scholar]
- McKinley CE, Boel-Studt S, Renner LM, Figley CR, Billiot S, & Theall K (2020). The historical oppression scale: preliminary conceptualization and measurement of historical oppression among Indigenous Peoples of the United States. Transcultural Psychiatry 57(2), 288–303. 10.1177/1363461520909605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKinley CE, Figley CR, Woodward S, Liddell J, Billiot S, Comby N, & Sanders S (2019). Community-engaged and culturally relevant research to develop mental and behavioral health interventions with American Indian and Alaska Natives. American Indian and Alaska Native Mental Health Research, 26(3), 79–103. 10.5820/aian.2603.2019.79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miranda J, Bernal G, Lau A, Kohn L, Hwang WC, & LaFrom-boise T (2005). State of the science on psychosocial interventions for ethnic minorities. Annual Review of Clinical Psychology, 1, 113–142. 10.1146/annurev.clinpsy.1.102803.143822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moberg DP (1983). Identifying adolescents with alcohol problems. A field test of the Adolescent Alcohol Involvement Scale. Journal of Studies on Alcohol, 44(4), 701–721. 10.15288/jsa.1983.44.701 [DOI] [PubMed] [Google Scholar]
- Moberg DP, & Hahn L (1991). The Adolescent Drug Involvement Scale. Journal of Child & Adolescent Substance Abuse, 2(1), 75–88. 10.1300/J272v02n01_05 [DOI] [Google Scholar]
- Moos RH, & Moos BS (2009). Family Environment Scale manual (4th ed.). Center for Health Care Evaluation, Stanford University of Medicine. [Google Scholar]
- Moran JR, & Bussey M (2007). Results of an alcohol prevention program with urban American Indian youth. Child and Adolescent Social Work Journal, 24(1), 1–21. 10.1007/s10560-006-0049-6 [DOI] [Google Scholar]
- Morgan R, & Freeman L (2009). The healing of our people: Substance abuse and historical trauma. Substance Use & Misuse, 44(1), 84–98. 10.1080/10826080802525678 [DOI] [PubMed] [Google Scholar]
- National Association for Children of Alcoholics. (2011). Celebrating Families! curriculum. http://www.celebratingfamilies.net/curriculum.htm
- Novins DK, Boyd ML, Brotherton DT, Fickenscher A, Moore L, & Spicer P (2012). Walking on: Celebrating the journeys of Native American adolescents with substance use problems on the winding road to healing. Journal of Psychoactive Drugs, 44(2), 153–159. 10.1080/02791072.2012.684628 [DOI] [PubMed] [Google Scholar]
- Oetzel J, Duran B, Jiang Y, & Lucero J (2007). Social support and social undermining as correlates for alcohol, drug, and mental disorders in American Indian women presenting for primary care at an Indian health service hospital. Journal of Health Communication, 12(2), 187–206. 10.1080/10810730601152771 [DOI] [PubMed] [Google Scholar]
- Power R, Akhter R, Muhit M, Wadud S, Heanoy E, Karim T, Badawi N, & Khandaker G (2019). Cross-cultural validation of the Bengali version KIDSCREEN-27 Quality of Life Questionnaire. BMC Pediatrics, 19(1), 1–10. 10.1186/s12887-018-1373-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quittan GA (2004). An evaluation of the impact of the Celebrating Families program and family drug treatment court (FDTC) on parents receiving family reunification services [Unpublished master’s thesis]. San Jose State University. [Google Scholar]
- Red Horse JG (1980). Family structure and value orientation in American Indians. Social Casework, 61(8), 462–467. 10.1177/104438948006100803 [DOI] [Google Scholar]
- Robbins R, Robbins S, & Stennerson B (2013). Native American family resilience. In Becvar DS (Ed.), Handbook of family resilience (pp. 197–227). Springer Publishing Company. [Google Scholar]
- Rosay AB (2016). Violence against American Indian and Alaska Native women and men: 2010 Findings from the National Intimate Partner and Sexual Violence Survey. National Institute of Justice. http://hdl.handle.net/11122/7025 [Google Scholar]
- Salvail FR, & Smith JM (2007, November). Survey shows … . The Hawaii behavioral risk factor surveillance system (Special report, year 5, issue 2) http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.174.3567&rep=rep1&type=pdf
- Saquib N, Brunner R, Kubo J, Tindle H, Kroenke C, Desai M, Daviglus ML, Allen N, Martin LW, Robinson J, & Stefa-nick ML (2013). Self-perceived physical health predicts cardiovascular disease incidence and death among postmenopausal women. BMC Public Health, 13(1), 468. 10.1186/1471-2458-13-468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satyanarayana VA, Nattala P, Selvam S, Pradeep J, Hebbani S, Hegde S, & Srinivasan K (2016). Integrated cognitive behavioral intervention reduces intimate partner violence among alcohol dependent men, and improves mental health outcomes in their spouses: A clinic based randomized controlled trial from South India. Journal of Substance Abuse Treatment, 64, 29–34. 10.1016/j.jsat.2016.02.005 [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, De la Fuente JR, & Grant M (1993). Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction, 88(6), 791–804. 10.1111/j.1360-0443.1993.tb02093.x [DOI] [PubMed] [Google Scholar]
- Sharps P, Campbell JC, Campbell D, Gary F, & Webster D (2003). Risky mix: Drinking, drug use, and homicide. NIJ Journal, 250, 8–13. https://www.ncjrs.gov/App/Publications/abstract.aspx?ID=196546 [Google Scholar]
- Shiels MS, Chernyavskiy P, Anderson WF, Best AF, Haozous EA, Hartge P, Rosenberg PS, Thomas D, Freedman ND, & de Gonzalez AB (2017). Trends in premature mortality in the USA by sex, race, and ethnicity from 1999 to 2014: An analysis of death certificate data. The Lancet, 389(10073), 1043–1054. 10.1016/S0140-6736(17)30187-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva N, Pereira M, Otto C, Ravens-Sieberer U, & Cristina M (2018). Do children/adolescents with chronic health conditions have worse HrQoL than their healthy peers? A meta-analysis of studies using the KIDSCREEN questionnaires [Paper presentation] Quality of Life Research, 27, S23–S24. 10.1007/s11136-019-02189-7 [DOI] [PubMed] [Google Scholar]
- Skinner HA (1982). The drug abuse screening test. Addictive Behaviors, 7(4), 363–371. 10.1016/0306-4603(82)90005-3 [DOI] [PubMed] [Google Scholar]
- Spencer MS, Gunter KE, & Palmisano G (2010). Community health workers and their value to social work. Social Work, 55(2), 169–180. 10.1093/sw/55.2.169 [DOI] [PubMed] [Google Scholar]
- Straus MA, & Douglas EM (2004). A short form of the Revised Conflict Tactics Scales, and typologies for severity and mutuality. Violence and Victims, 19(5), 507–520. 10.1891/vivi.19.5.507.63686 [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2004). Risk and protective factors for substance use among American Indian or Alaska Native youths: The NSDUH report. U.S. Department of Health and Human Services. [Google Scholar]
- Terpstra J, Coleman KJ, Simon G, & Nebeker C (2011). The role of community health workers (CHWs) in health promotion research: Ethical challenges and practical solutions. Health Promotion Practice, 12(1), 86–93. 10.1177/1524839908330809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teufel-Shone N, Staten LK, Irwin S, Rawiel U, Bravo AB, & Waykayuta S (2005). Family cohesion and conflict in an American Indian community. American Journal of Health Behavior, 29(5), 413–422. 10.5993/AJHB.29.5.4 [DOI] [PubMed] [Google Scholar]
- Thomas LR, Donovan DM, Sigo RL, Austin L, & Alan Marlatt G, & The Suquamish Tribe. (2009). The community pulling together: A tribal community–university partnership project to reduce substance abuse and promote good health in a reservation tribal community. Journal of Ethnicity in Substance Abuse, 8(3), 283–300. 10.1080/15332640903110476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolan P, Gorman-Smith D, & Henry D (2006). Family violence. Annual Review of Psychology, 57, 557–583. 10.1146/annurev.psych.57.102904.190110 [DOI] [PubMed] [Google Scholar]
- Tutty L (2013). An evaluation of strengthening families: The Calgary Counselling Centre’s program for couples dealing with intimate partner violence and substance use. Yarro Creek Enterprises. [Google Scholar]
- Uhrich RB (1969). Tribal community health representatives of the Indian health service. Public Health Reports, 84(11), 965–970. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2031694/pdf/pubhealthreporig01071-0037.pdf [PMC free article] [PubMed] [Google Scholar]
- Ungar M, & Liebenberg L (2011). Assessing resilience across cultures using mixed methods: Construction of the child and youth resilience measure. Journal of Mixed Methods Research, 5(2), 126–149. 10.1177/1558689811400607 [DOI] [Google Scholar]
- Urban Indian Health Institute. (2014). Supporting sobriety among American Indians and Alaska Natives: A literature review. http://www.uihi.org/wp-content/uploads/2014/02/Supporting-Sobriety_A-Literature-Review_WEB.pdf
- U.S. Department of Health and Human Services. (2013). Child maltreatment 2012. http://www.acf.hhs.gov/programs/cb/research-data-technology/statistics-research/child-maltreatment
- Victor SE, & Klonsky ED (2016). Validation of a brief version of the Difficulties in Emotion Regulation Scale (DERS-18) in five samples. Journal of Psychopathology and Behavioral Assessment, 38(4), 582–589. 10.1007/s10862-016-9547-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallerstein NB, & Belone L (2015). Family listening program: Multi-tribal implementation and evaluation. http://grantome.com/grant/NIH/R01-DA037174-01
- Wallerstein NB, & Duran B (2006). Using community-based participatory research to address health disparities. Health Promotion Practice, 7(3), 312–323. 10.1177/1524839906289376 [DOI] [PubMed] [Google Scholar]
- Whitbeck LB (2015). An RCT of a family-centered Ojibwe substance abuse prevention. http://grantome.com/grant/NIH/R01-DA037177-01A1
- Bison White. (2015). Celebrating Families! http://whitebison.org/Training/Families.aspx
- Whitesell NR, Sarche M, Keane E, Mousseau AC, & Kaufman CE (2018). Advancing scientific methods in community and cultural context to promote health equity: Lessons from intervention outcomes research with American Indian and Alaska Native communities. American Journal of Evaluation, 39(1), 42–57. 10.1177/1098214017726872 [DOI] [PMC free article] [PubMed] [Google Scholar]


