Synopsis
Electronic cigarettes (EC) are battery-operated devices that heat and aerosolize a liquid solution that typically contains nicotine. Since the products came into widespread use around 2007, ECs have polarized public health experts, governments, and the general public. On one hand, ECs have become commonly used among youth and may pose substantial risks of future addiction and health problems in this population. On the other hand, ECs are far less toxic per puff compared with combustible cigarettes, and as a result, might present an important harm reduction opportunity for cigarette smokers who cannot stop smoking by traditional means. The long-term health effects of ECs on individuals and the net effect on public health will remain unknown for many years. Late in 2019, an outbreak of e-cigarette, or vaping, product-use associated lung injury (EVALI) was identified in the United States. Though the definitive cause(s) of EVALI are not known as of the publication date, the epidemic has been strongly associated with the use of tetrahydrocannabinol (THC) vaping products containing vitamin E acetate (a cutting agent). These cases have increased awareness that some people use ECs to consume substances other than nicotine. The health risks of these behaviors remain poorly understood and require further investigation.
Keywords: Electronic cigarette, tobacco, smoking, nicotine, addiction
Introduction: What Are Electronic Cigarettes and Vaping?
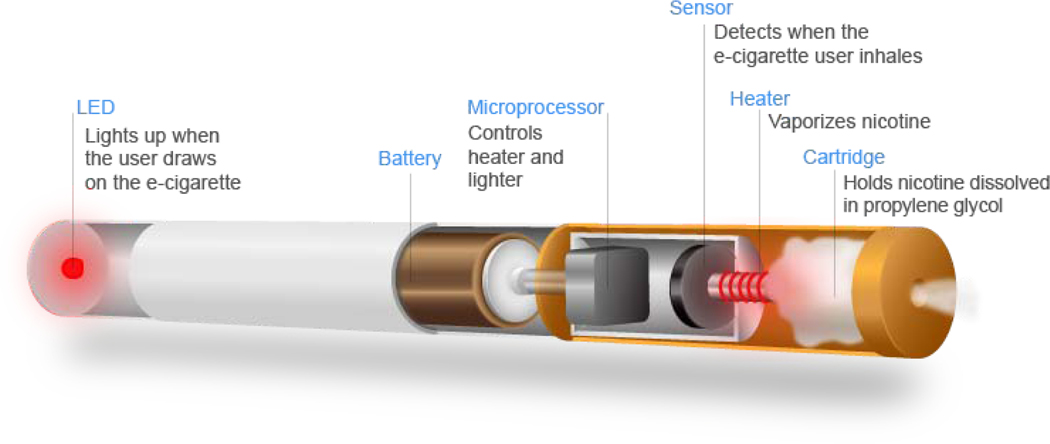
Electronic cigarettes (EC) are battery-operated devices that heat and aerosolize a liquid solution that typically contains nicotine. ECs do not refer to a single device or product, but rather a heterogeneous class of products. Despite their heterogeneity, ECs all contain the same basic features: (1) a battery to provide heat; (2) a metal heating element; and (3) a liquid solution (Figure 1).1
Figure 1:
E-Cig schematic. From US Department of Transportation. Electronic Cigarettes Safety. Available at: https://www.transportation.gov/fastlane/electroniccigarettes-safety-issue-aircraft; with permission.
Vaping is the act of inhaling a heated, aerosolized substance. It is critical to distinguish vaping from smoking. Smoking is the inhalation of a burned substance. The main difference between the two processes is that smoking occurs at much higher temperatures (i.e. > 1000 degrees Fahrenheit) compared with vaping (250–500 degrees Fahrenheit). This difference in temperature has significant implications for the relative toxicities of the two activities and for the chemical mixtures that are produced in the process.2 Smoking leads to a much more complex mixture of chemicals as compared with vaping.3
“E-liquids” are the liquid solutions contained in ECs that users vape. E-liquids usually contain the same basic elements: alcohol-based solvents (propylene glycol and vegetable glycerin), flavorings, and (typically, though not excluslvely) nicotine.4 Though e-liquids are relatively simple mixtures, the aerosol that forms following heating becomes much more complex.5 Many chemicals of concern in combustible cigarettes have been found in ECs, though at much lower levels.3
Why Are Electronic Cigarettes Controversial? The Dilemma of Youth Use and Adult Harm Reduction
The emergence of ECs has polarized physicians, public health experts, and governments.6 In the United States, ECs evoke memories of “Big Tobacco” (tobacco industry firms): its betrayal of public trust, and contribution to an epidemic of smoking-related diseases despite knowledge of the consequences.7 The tobacco industry’s explicit targeting of young people strikes a particularly noxious chord in the US.8 ECs indeed represent both an opportunity and a threat. The opportunity is harm reduction, which is the less harmful form of drug use or less harmful route of drug administration. If ECs are substantially less harmful than combustible cigarettes and an acceptable alternative to current smokers, the public health benefits to the adult population could be large. In the best-case scenario, ECs might lead to a reduction in combustible cigarette use and lower levels of heart, lung, and oncologic diseases.9,10 Whether harm reduction will occur, however, remains unknown. On the other hand, ECs pose a threat of reversing progress in tobacco control efforts that have occurred over the past 70 years.11 The products may pose a risk of engendering a new epidemic of nicotine addiction, with unknown long-term health harms among young people.12,13 In the worst-case scenario, ECs could lead to millions of new people using a harmful, addictive product that not only causes disease but does not reduce (and perhaps even increases) combustible cigarette smoking.
Economically, the EC industry has grown rapidly and poses an existential threat to combustible tobacco products. Though the EC market still pales in comparison to the combustible cigarette market (11.5 billion vs. 125 billion in 2018) [https://www.marketwatch.com/press-release/e-cigarette-market-size-worth-242-billion-by-2024-cagr-13-2019-07-31; [Euromonitor. (July 1, 2019). Market value of tobacco in the United States from 2015 to 2020 (in million U.S. dollars) [Graph]. In Statista. Retrieved February 04, 2020, from https://www.statista.com/statistics/491709/tobacco-united-states-market-value/], Big Tobacco has taken notice and is adapting accordingly [https://www.wsj.com/articles/altria-takes-4-1-billion-writedown-on-juul-investment-11580386578]. With so much at stake, it is not surprising that the EC debate has been spotlighted in the media and has received significant attention in the political sphere. Without a doubt, the EC question has proven to be as much a political issue as a scientific one. To more clearly understand the present issues surrounding ECs, we must first take a look at the past.
Big Vapes? A Brief History of Electronic Cigarettes
Contrary to popular belief, ECs were initially launched into commercial markets independently of the tobacco companies. It was not until much later in the evolution of ECs that “Big Tobacco” decided to take a stake in an industry that threatened to make the combustible cigarette obsolete. The first EC available for commercial use is usually attributed to Hon Lik, a Chinese pharmacist.14 Hon sought to design a smoking-cessation product that could mimic the look, feel, and experience of smoking without the associated toxicities. Thus, the first EC later became known as a “cig-alike” (Figure 2). Cig-alikes could mimic the behavioral elements of smoking. They were roughly the same size as a cigarette and usually had a red light-emitting diode (LED) attached to the end of it. However, these products had problems. The battery life was short and unreliable. The e-liquid chamber was small (i.e. 1 mL or less), meaning that heavy users needed to change products frequently. And perhaps most importantly, for many users, cig-alikes simply did not deliver nicotine fast enough or in high enough quantity to provide an effective smoking substitute.15,16
Figure 2.
1st Generation Electronic Cigarette (“cig-alike”). From Dave Cross. The State of Vaping. Planet of the Vapes. Available at: https://www.planetofthevapes.co.uk/news/vaping-news/2018-06-05_the-state-of-vaping.html; with permission.
Thus, entrepreneurs designed second generation ECs to address many of these issues (Figure 3). Today, second generation ECs are commonly associated with the term “vape pens,” given their pen-like shape. Two innovations were key. First, the battery was significantly larger compared with cig-alikes. This allowed for longer, more frequent use, and a larger amount of aerosol and nicotine delivery to users.15 Second, refillable “tank systems” were introduced. Tank systems allowed users to fill and refill the EC with e-liquids of varying nicotine strengths and flavorings. This led to the explosion of the “e-liquid” industry and its thousands of available (and unregulated) flavors.17 From the user perspective, it provided an increased amount of flexibility and customizability to the vaping experience. Furthermore, it permitted the use of other substances such as tetrahydrocannabinol (THC; the psychoactive chemical in cannabis) oils,18,19 which came to prominence late in 2019 (described in more detail below).20
Figure 3.
2nd Generation Electronic Cigarette. From Simple and Practical Mental Health. What are electronic cigarettes (e-cigarettes)? Available at: https://simpleandpractical.com/what-are-electronic-cigarettes-e-cigarettes/ With permission.
Over time, it became clear that aerosol production was a significant factor in the user experience and increasing the efficiency of nicotine delivery. Thus, the third generation of ECs (Figure 4), commonly referred to as modifiable (“mods”) or personal vaporizers, pair a tank system with a significantly larger battery compared with the second-generation devices. Larger batteries could provide a greater amount of electrical power to the liquid, leading a bigger aerosol “hit” to users, more rapid nicotine delivery,21 and less frequent need for battery charging. One additional consequence of the proliferation of higher powered devices was a shift by consumers to lower strength nicotine e-liquids,21 which were less harsh on the throat.
Figure 4.
Third Generation E-Cig (“Mod”). From Simple and Practical Mental Health. What are electronic cigarettes (e-cigarettes)? Available at: https://simpleandpractical.com/what-are-electronic-cigarettes-e-cigarettes/ With permission.
Most recently (as of the year 2020), the EC market was disrupted once more with the development of fourth generation “pod-style” ECs22 (Figure 5). The most well-known product in this category is currently “JUUL,” a novel EC that captured a large portion of the US market as of 2020.23 There were some key differences between JUUL and prior EC products. First, the new device was small, rectangular, and resembled a computer thumb drive. It was portable and very easy to access and conceal.24 Second, the e-liquid mixture contained benzoic acid, an additive used to lower the chemical pH of nicotine.25 Since the high pH contained in many commercially available ECs could be harsh on the throat, a lower pH could make the product less harsh and more appealing. Over just a few years, JUUL came to dominate the US EC market. Their products have become very popular among youth,26,27 and the company has faced significant public and regulatory criticism as a result.28
Figure 5.
Pod-style E-Cig (i.e. Juul). From Simple and Practical Mental Health. What are electronic cigarettes (e-cigarettes)? Available at: https://simpleandpractical.com/what-are-electronic-cigarettes-e-cigarettes/ With permission.
Are E-Cigs Addictive?
As commonly used, ECs (particularly later generation products) are addictive through rapid delivery of nicotine to the brain.29 Though there are reports of the use of other psychoactive drugs such as THC via vaping devices,30 the discussion that follows focuses on the role of nicotine-containing ECs. Nicotine is a central nervous system stimulant that is highly reinforcing when delivered rapidly and at high dose.31 Its role in perpetuating combustible cigarette addiction has been well-established.32 When considering the addictive properties of psychoactive drugs, several factors are critical including: (1) pharmacologic effect; (2) route of administration; (3) speed of delivery; (4) development of tolerance (requiring more of the drug for pharmacologic effect); and (5) severity of withdrawal. Differences in these factors demonstrate why two nicotine-containing products may vary substantially with respect to addictive risk. On one hand, conventional cigarettes delivery nicotine via inhalation through the pulmonary circulation.33 This leads to rapid drug delivery to the brain within several seconds, resulting in a highly reinforcing effect. Furthermore, the ability of users to “titrate” the drug dose by varying puff volume and speed contributes significantly to abuse liability and reinforcement.34 On the other end of the spectrum, the nicotine patch delivers nicotine slowly via the transdermal route over a period of 24 hours.35 The onset is gradual and there is no ability to rapidly titrate the dose. As a result, the patch does not have significant reinforcing effects or abuse liability.
ECs are capable of providing nicotine delivery rapidly and in a manner similar to combustible cigarettes, at least under some circumstances.36,37 The new generation of ECs are more efficient nicotine delivery systems as compared with older ECs.15 Nicotine exposure among adolescents who use pod-style ECs such as JUUL appears to be substantial, and similar in magnitude to prior studies of teen smokers.25,38 Furthermore, ease of use relating to the newer products may be another factor increasing addiction risk.
In addition to the drug effects of nicotine, a multitude of other environmental and social factors mediate addiction including product characteristics (i.e. design, flavor, image), social influences (i.e. behaviors of friends and family, advertising, health warnings/messaging), beliefs regarding harms and benefits, underlying host comorbidities and vulnerabilities (i.e. mental illness), and sensation-seeking.39 All of these factors, in combination with nicotine delivery, may affect the risk of addiction at the individual level.
In summary, ECs have addictive potential through their rapid delivery of nicotine to the brain, ease of use, and associated environmental influences.
Are E-Cigs Toxic and Do They Have Health Effects?
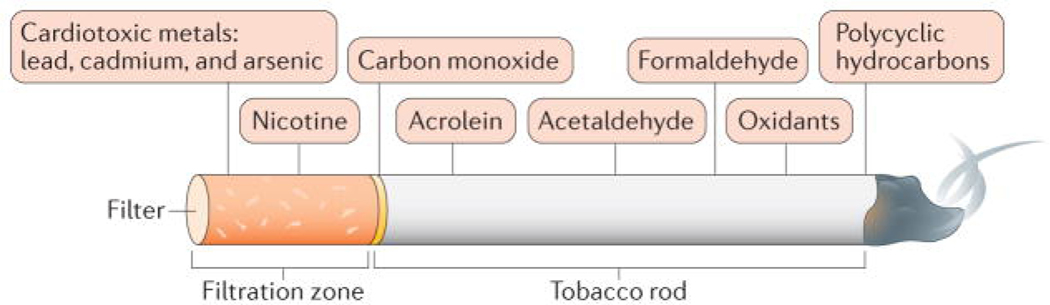
EC aerosol is inherently toxic, though exceedingly less so than combustible cigarettes when comparing the products puff-for-puff3 (Figure 6 & Figure 7). Unlike cigarettes, EC aerosol does not contain combustion products such as carbon monoxide and tar. Nonetheless, both clinical and preclinical data suggest that EC aerosol inhalation has adverse effects on the airways and lungs (Figure 8). In human epidemiologic studies, adolescents using ECs more frequently reported symptoms of chronic cough or sputum production compared with non-EC users.40,41 Studies of changes in spirometry following acute EC use have been mixed, with some studies showing obstructive effects and others not.42,43 These varying effects could depend on preexisting host co-morbidities. Bronchoscopies of healthy EC users have shown erythema of airway mucosa and altered airway epithelial cell gene expression patterns.44 In a three-way comparison of bronchoalveolar lavage inflammatory cell count and gene expression among EC users, smokers, and non-users, the EC users demonstrated gene expression patterns that were closer to never-smokers than to smokers.45 They also had inflammatory cell counts that were intermediate between smokers and never-smokers. Preclinical animal and cell culture studies have shown a variety of potentially adverse effects of ECs including increased airway reactivity, alterations in mucus production and clearance, and alteration of normal immune function.46–48 Our understanding of the adverse effects of ECs on the cardiovascular system are less well-characterized, but remain a significant concern. Particular EC emissions of concern include aldehydes, particulates, oxidizing chemicals, and nicotine itself.49
Figure 6.
Tobacco combustion products. From Benowitz NL, Fraiman JB. Cardiovascular effects of electronic cigarettes. Nature Reviews Cardiology. 2017;14(8):447; with permission.
Figure 7.
Components of an E-Cigarette. From Benowitz NL, Fraiman JB. Cardiovascular effects of electronic cigarettes. Nature Reviews Cardiology. 2017;14(8):447; with permission.
Figure 8.
Pulmonary effects of vaping. From Gotts JE, Jordt S-E, McConnell R, et al. What are the respiratory effects of e-cigarettes? BMJ (Clinical research ed.). 2019;366:l5275; with permission.
In summary, ECs are toxic and carry health risks for the development of pulmonary disease, and possibly cardiovascular and oncologic diseases. When compared with combustible cigarettes, ECs appear to be substantially less toxic when considered puff-for-puff (i.e. equal volumes of smoke vs. aerosol consumed). The long-term health effects of EC use are currently unknown.
E-Cigarette, or Vaping, Product-Use Associated Lung Injury (EVALI)
Beginning approximately June 2019, the US Centers for Disease Control (CDC) began receiving reports of severe acute lung injury occurring in the setting of e-cigarette use. As of April 2020, more than 2,800 cases of e-cigarette, or vaping, product-use associated lung injury (EVALI) had been reported.50 (Figure 9). Several EVALI case series were first described beginning around September 2019.51–53 The largest series, involving patients in Illinois and Wisconsin,51 reported that 84% of the cases involved the vaping of THC, the psychoactive chemical in marijuana. A wide variety of products and devices were reported, and a single etiologic agent could not be clearly identified. For the purpose of surveillance, case definitions were created. A “confirmed case” was defined as meeting 3 criteria: (1) use of an e-cigarette (vaping) within 90 days of symptom onset; (2) pulmonary infiltrate on chest imaging; (3) absence of pulmonary infection on initial workup; and (4) no evidence in the medical record of alternative plausible diagnoses (i.e. heart failure, rheumatic, or malignant processes). “Probable cases” were defined similarly except that there was evidence of pulmonary infection present and, despite this, the treating physicians believed infection was not the sole cause of the patient’s respiratory failure.
Figure 9.
E-cigarette associated lung injury (EVALI). From Layden JE, Ghinai I, Pray I, et al. Pulmonary Illness Related to E-Cigarette Use in Illinois and Wisconsin - Preliminary Report. N Engl J Med. 2019; with permission.
Cases typically involved young people, with a median age of 19 years, though a wide age range was reported (16–53). There was a male predominance (83%) of unknown significance. In addition to the near universal presence of respiratory and constitutional symptoms, over 80% of people reported prominent gastrointestinal symptoms such as nausea or vomiting. The typical course led to the development of the acute respiratory distress syndrome, and approximately one third of patients required mechanical ventilation. A range of pathologic findings were reported, complicating efforts to identify a clear precipitant and disease mechanism. Half of bronchoalveolar lavage (BAL) specimens noted lipid-laden macrophages with oil red O stain, raising the possibility of lipoid pneumonia. This pattern was subsequently seen commonly in cases from North Carolina and Utah.52,53 Other early reports noted a wide range of pathologic patterns that were more consistent with chemical pneumonitis.54 Improvement following the administration of steroids was noted in many cases.
The key takeaway from the EVALI outbreak was that it revealed people were using EC devices to vape substances other than nicotine, such as THC oils. The use of “street-bought” (i.e. illegal) or modified EC products were commonly reported, suggesting that low quality, unregulated products were the primary source of the problem. Indeed, vitamin E acetate, an oil-based cutting agent added to THC oils, was discovered by CDC in many of the BAL samples analyzed.55 Though this was one of likely several chemicals causing the illness, it illustrated the problems with an unregulated marketplace. To date, we still lack a comprehensive understanding of EVALI, though vitamin E acetate is heavily suspected as a culprit.55
The rise of EVALI reports turned out to be politically consequential. Under intense political pressure and with persistent media coverage, the FDA took action to ban flavorings in pod-style ECs. (https://www.fda.gov/news-events/press-announcements/trump-administration-combating-epidemic-youth-e-cigarette-use-planclear-market-unauthorized-non). Whether such action will reduce youth EC use, push adult EC users back toward combustible cigarette use, contribute to illegal EC markets, or have no effect on current trends remains to be seen. Nonetheless, bold policy taken in part because of EVALI reporting will likely be viewed as a significant event in the history of ECs when viewed retrospectively.
Do E-Cigs Promote Smoking Cessation?
The role of ECs for the purpose of smoking cessation has been controversial. After a few years following the introduction of ECs into commercial markets, physicians were solidly divided regarding whether ECs are helpful for smoking cessation and whether the products should be used for harm reduction in instances when patients fail to respond to conventional smoking cessation medications and behavioral support.56 The lack of understanding of the true risks of EC has made it difficult to provide adequate counsel for patients. Furthermore, balancing the values of promoting health, reducing harm, and echoing public health messages create communication challenges for clinicians.
Nonetheless, as noted above, ECs originated in large part as a means to treat smoking addiction and are commonly used for this purpose.57 Several lines of epidemiologic evidence suggest that intensive EC use is associated with greater odds of smoking cessation,58,59 and, importantly, smoking rates have continued to decline in the US since the introduction of ECs into commercial markets.60 It is now clear that ECs help some people with cessation of combustible tobacco.61 Earlier EC trials studied cig-alike ECs in both motivated and unmotivated smokers, finding quit rates equivalent or non-statistically higher than the nicotine patch, and reductions in cigarettes smoked per day.62,63 However, the overall smoking quit rates were low and the studies may have been underpowered. The most consequential study to date was a multicenter randomized controlled trial conducted in the United Kingdom from 2015–2018 comparing 2nd generation ECs to traditional combination nicotine replacement (i.e. nicotine patch, gum, lozenge, etc).64 886 study participants were smokers who were open to quitting smoking and had no strong preference regarding the use of NRT or ECs. The subjects were randomized to receive a 3-month supply of either an EC starter kit that included choice of different e-liquid strengths and flavors, or their preferred nicotine-replacement products. Behavioral support for smoking cessation (the standard of care) was provided to all study participants. The major study finding was that those randomized to the EC group were nearly twice as likely to achieve smoking abstinence at week 52 as compared with the NRT group (18.0% vs. 9.9%; RR 1.75 (1.24–2.46)). Adverse events were similar among groups. Importantly, around 80% of subjects in the EC group were still using their EC product at the end of the study, illustrating that long-term nicotine replacement is likely a necessary condition to maintain smoking abstinence.
E-Cigs in the Clinical Setting: How to Evaluate and Counsel Patients
For adult medicine clinicians, it is now nearly certain that EC use will be encountered in at least some patients who present in clinical settings. The vast majority of these patients are likely to be former combustible cigarette smokers, and many of them may suffer from medical and psychiatric comorbidities.65 Some of them will also be concurrent smokers of tobacco and other substances (i.e. marijuana/THC). In the near-future, however, providers are likely to see EC users who have never smoked combustible cigarettes. How should we evaluate and counsel these patients?
A strong history is the initial key step and will help identify the patient’s level of risk and other related comorbidities that require attention. A simple screening question can follow the smoking history typically taken as part of the patient’s social history: “Do you vape or use e-cigarettes?” Follow-up questions to a positive response help to clarify health risks and the level of nicotine dependence. It is important to understand which device(s) are being used, which e-liquids are vaped (i.e. nicotine content, flavorings, or other drugs, especially THC), where the products were obtained (i.e. authorized retailers or from informal sources such as friends), and the duration and frequency of use. We must seek to understand the patient’s reasons for use, including the patient’s perceived benefits and risks of use, as well as desire and willingness to stop. Concurrent use of combustible tobacco products is important, as studies have shown that any combustible product use significantly increases toxic exposure as compared with EC-only use.66 Similarly, understanding the role that ECs have played for the patient in maintaining abstinence from combustible cigarette smoking is crucial.
How should we frame our advice? In the ideal world, the only thing we should inhale is clean air. This is certainly reasonable advice to give to patients, but it does not fully account for the complexities of a real world, in which addiction and other comorbidities interact to create behaviors that are very difficult to modify. Indeed, long-term abstinence rates from cigarette smoking are low, particularly among those who have difficulty achieving abstinence for at least 3 months.67 A nuanced message is important for patients who switched from combustible cigarettes to ECs for the purpose of harm reduction. Though the long-term effects of ECs are unknown, the devastating effects of continued combustible cigarette use are known.11 ECs are not without health risks, but these risks are likely substantially less when compared with combustible cigarettes.68–70 Permanent and complete cessation from combustible products should be highly prioritized. If the patient is using ECs successfully for this purpose, we should acknowledge and applaud their effort to stop smoking.
If the patient is solely using ECs (and not using combustible products), we should inquire whether they wish to discontinuing vaping as well. The optimal approach to nicotine vaping cessation is unknown. In the absence of clear evidence, the combination of behavioral and pharmacologic treatments, which is the standard of care for the treatment of cigarette smoking addiction, is a reasonable starting point despite a lack of evidence of effectiveness in people who vape. It is not clear whether gradually reducing the nicotine level in e-liquids is a beneficial strategy to promote cessation from vaping. There is some evidence that, like people who smoke, those who vape might engage in compensatory puffing behavior (i.e. bigger or longer puffs) to maintain similar nicotine intake from ECs that contain less nicotine.37 Studies examining effective interventions to promote cessation from nicotine vaping are needed to provide definitive guidance for clinicians.
What Else Do We Need to Learn About E-Cigs?
If the story of ECs is a book, we are currently at the beginning of the first chapter of a very long narrative. For context, tobacco smoking has been present in the Americas for centuries, if not milennia.71 The consumption of liquid nicotine via ECs is a distinctly 21st century phenomenon that will likely continue to grow. While the emotions surrounding the rise of EC use run high, facts and knowledge remain scarce.72 What are the key areas where we need more clarity?
First, and perhaps most importantly, we need to understand the long-term health effects of chronic EC use. Will it lead to chronic lung, heart, and oncologic diseases in the way cigarette smoking does? Does it cause a different disease phenotype such as chronic bronchitis, or increased susceptibility to pulmonary infection?44,73–75 We especially need to understand how these risks compare with chronic cigarette smoking, the current leading cause of preventable death in the United States. Longitudinal cohort studies exploring key health outcomes including heart, lung, and oncologic diseases will help us to understand both the absolute and relative risks of chronic EC use. Related to this point is figuring out which features of ECs contribute to the risks of both addiction and toxicity. As mentioned above, ECs are a heterogeneous group of products that likely carry differential risks depending on the device type, electrical power, and type of e-liquid used. Understanding the factors that influence these health risks will help us properly regulate the products and inform the public.
Second, we need to understand how to optimize use of ECs for smoking cessation64 and harm reduction9 in individuals who fail to stop smoking cigarettes through conventional methods. Which individuals or populations are most likely to respond to harm reduction strategies? What is the optimal timing for offering harm reduction strategies? How do we optimize complete product switching to remove all combustible cigarette consumption?
Third, developing an understanding of the environmental effects of EC emissions will be important for protecting the public. Again, comparing their polluting effects with combustible cigarettes is critical for proper regulation and protection of the public.
Fourth, do ECs create a gateway into cigarette smoking or provide an adequate substitute to reduce smoking at the population level? Some association studies have suggested an elevated risk of combustible cigarette use following initiation of ECs.76 Though not causal, the data raise concerns about what the increasing prevalence of ECs in youth means for long term tobacco control efforts to prevent combustible tobacco use. On the other hand, ECs might prevent combustible cigarette smoking simply by being a more satisfying alternative to would-be smokers and inhibiting smoking initiation. It will be critical to continue monitoring trends in cigarette smoking, which have continued to decline among adults and youth since the introduction of ECs.26
What is the Future of E-Cigs?
There is no doubt that the emergence of ECs marks a profound event in the history of human consumption of nicotine and tobacco products. On the one hand, ECs offer hope for harm reduction among people with smoking addiction who cannot or will not stop smoking using conventional methods. In the best-case scenario, ECs might help people reduce their chronic exposure to toxins, lower disease burden, and save lives. The products might eventually make combustible cigarettes obsolete. On the other hand, ECs threaten to reverse the significant advances made in tobacco control over the past half century. In the worst-case scenario, harm reduction gains fail to materialize and a new generation of young people develop chronic addiction to a potent nicotine delivery system with significant health consequences. What does the future hold?
ECs will likely continue to evolve in terms of design, drug delivery efficiency, and user experience. They will eventually be regulated by the Food and Drug Administration (FDA), which has begun to take steps to protect youth (https://www.fda.gov/news-events/press-announcements/fda-finalizes-enforcement-policy-unauthorized-flavored-cartridge-based-e-cigarettes-appeal-children) but has not yet finalized a regulatory paradigm. Research to inform optimal FDA strategies is ongoing.
From the perspective of industry, the endpoint is clear: to create products that are highly addictive, commonly used, and, most importantly, profitable. The industry playbook has been very well-characterized,77 and involves efforts to infiltrate every corner of society: aggressive advertising and marketing (particularly to youth, who are more likely to develop addiction than adults); public relations promotions; sponsored “friendly” research via universities and non-profit organizations; government lobbying; legal action against any proposed regulatory hurdles that curtail profit. These proven tactics were used by the tobacco industry in the past and are likely going to continue in the presence of aggressive corporate lobbying and absence of legislative counteraction.
Public health advocates will push back with equally clear endpoints: to prevent a health epidemic caused by vaping and to prevent a resurgence of cigarette smoking. Anti-vaping legislation has already been introduced in many countries and localities. Education efforts have been aimed at youth and other at-risk groups.78 Clean indoor air laws have been passed.79 Warning signals have been sounded.80,81 This push and pull of markets and social forces inherent to our society will ultimately determine the influence of ECs and their role in human history. This struggle has been playing out in the political arena in all branches of government, and will continue to do so for the years ahead.
Key Points:
Electronic cigarettes (EC) are battery-operated devices that heat and aerosolize a liquid solution that may contain nicotine.
Some ECs deliver nicotine rapidly and have addictive potential.
ECs have inherent toxicity and unknown long-term health effects.
EC’s are substantially less toxic than combustible cigarettes.
ECs likely have a role in smoking cessation and harm reduction in a subset of people who smoke combustible cigarettes.
Some people use EC devices to consume tetrahydrocannabinol (THC) and other psychoactive substances.
Footnotes
Disclosure:
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.National Academies of Sciences E, Medicine. Public Health Consequences of E-Cigarettes. Washington, DC: The National Academies Press; 2018. [PubMed] [Google Scholar]
- 2.Kosmider L, Sobczak A, Fik M, et al. Carbonyl compounds in electronic cigarette vapors: effects of nicotine solvent and battery output voltage. Nicotine Tob Res. 2014;16(10):1319–1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goniewicz ML, Knysak J, Gawron M, et al. Levels of selected carcinogens and toxicants in vapour from electronic cigarettes. Tob control. 2014;23(2):133–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Callahan-Lyon P. Electronic cigarettes: human health effects. Tob Control. 2014;23(suppl 2):ii36–ii40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cheng T. Chemical evaluation of electronic cigarettes. Tob Control. 2014;23(suppl 2):ii11–ii17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Green SH, Bayer R, Fairchild AL. Evidence, policy, and e-cigarettes—will England reframe the debate? New England Journal of Medicine. 2016;374(14):1301–1303. [DOI] [PubMed] [Google Scholar]
- 7.Glantz SA, Barnes DE, Bero L, Hanauer P, Slade J. Looking through a keyhole at the tobacco industry: the Brown and Williamson documents. Jama. 1995;274(3):219–224. [PubMed] [Google Scholar]
- 8.Ling PM, Glantz SA. Why and how the tobacco industry sells cigarettes to young adults: evidence from industry documents. American journal of public health. 2002;92(6):908–916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cahn Z, Siegel M. Electronic cigarettes as a harm reduction strategy for tobacco control: a step forward or a repeat of past mistakes? Journal of public health policy. 2011;32(1):16–31. [DOI] [PubMed] [Google Scholar]
- 10.Polosa R, Rodu B, Caponnetto P, Maglia M, Raciti C. A fresh look at tobacco harm reduction: the case for the electronic cigarette. Harm reduction journal. 2013;10(1):19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Center for Chronic Disease P, Health Promotion Office on S, Health. Reports of the Surgeon General. The Health Consequences of Smoking-50 Years of Progress: A Report of the Surgeon General. Atlanta (GA): Centers for Disease Control and Prevention (US); 2014. [Google Scholar]
- 12.Kong G, Morean ME, Cavallo DA, Camenga DR, Krishnan-Sarin S. Reasons for electronic cigarette experimentation and discontinuation among adolescents and young adults. Nicotine Tob Res. 2015;17(7):847–854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Camenga DR, Delmerico J, Kong G, et al. Trends in use of electronic nicotine delivery systems by adolescents. Addict Behav. 2014;39(1):338–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hon L. Electronic cigarette. Google Patents; 2013. [Google Scholar]
- 15.Farsalinos KE, Spyrou A, Tsimopoulou K, Stefopoulos C, Romagna G, Voudris V. Nicotine absorption from electronic cigarette use: comparison between first and new-generation devices. Sci Rep. 2014;4:4133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eissenberg T. Electronic nicotine delivery devices: ineffective nicotine delivery and craving suppression after acute administration. Tob control. 2010;19(1):87–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Allen JG, Flanigan SS, LeBlanc M, et al. Flavoring chemicals in e-cigarettes: diacetyl, 2, 3-pentanedione, and acetoin in a sample of 51 products, including fruit-, candy-, and cocktail-flavored e-cigarettes. Environmental health perspectives. 2016;124(6):733–739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Borodovsky JT, Crosier BS, Lee DC, Sargent JD, Budney AJ. Smoking, vaping, eating: Is legalization impacting the way people use cannabis? International Journal of Drug Policy. 2016;36:141–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Spindle TR, Bonn-Miller MO, Vandrey R. Changing landscape of cannabis: novel products, formulations, and methods of administration. Current opinion in psychology. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kalininskiy A, Bach CT, Nacca NE, et al. E-cigarette, or vaping, product use associated lung injury (EVALI): case series and diagnostic approach. The Lancet Respiratory Medicine. 2019;7(12):1017–1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wagener TL, Floyd EL, Stepanov I, et al. Have combustible cigarettes met their match? The nicotine delivery profiles and harmful constituent exposures of second-generation and third-generation electronic cigarette users. Tob control. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fadus MC, Smith TT, Squeglia LM. The rise of e-cigarettes, pod mod devices, and JUUL among youth: Factors influencing use, health implications, and downstream effects. Drug and alcohol dependence. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Huang J, Duan Z, Kwok J, et al. Vaping versus JUULing: how the extraordinary growth and marketing of JUUL transformed the US retail e-cigarette market. Tob Control. 2019;28(2):146–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ramamurthi D, Chau C, Jackler RK. JUUL and other stealth vaporisers: hiding the habit from parents and teachers. Tob Control. 2019;28(6):610–616. [DOI] [PubMed] [Google Scholar]
- 25.Goniewicz ML, Boykan R, Messina CR, Eliscu A, Tolentino J. High exposure to nicotine among adolescents who use Juul and other vape pod systems (‘pods’). Tob Control. 2019;28(6):676–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Arrazola RA, Singh T, Corey CG, et al. Tobacco use among middle and high school students - United States, 2011–2014. MMWR. Morbidity and mortality weekly report. 2015;64(14):381–385. [PMC free article] [PubMed] [Google Scholar]
- 27.Gentzke AS, Creamer M, Cullen KA, et al. Vital signs: tobacco product use among middle and high school students—United States, 2011–2018. Morbidity and Mortality Weekly Report. 2019;68(6):157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dyer O. FDA considers regulatory action as vaping among US teens jumps 78% in a year. British Medical Journal Publishing Group; 2019. [DOI] [PubMed] [Google Scholar]
- 29.Baldassarri SR, Bernstein SL, Chupp GL, Slade MD, Fucito LM, Toll BA. Electronic cigarettes for adults with tobacco dependence enrolled in a tobacco treatment program: A pilot study. Addict Behav. 2018;80:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Morean ME, Kong G, Camenga DR, Cavallo DA, Krishnan-Sarin S. High school students’ use of electronic cigarettes to vaporize cannabis. Pediatrics. 2015;136(4):611–616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Benowitz NL. Pharmacology of nicotine: addiction and therapeutics. Annual review of pharmacology and toxicology. 1996;36(1):597–613. [DOI] [PubMed] [Google Scholar]
- 32.Benowitz NL. Nicotine addiction. N Engl J Med. 2010;362(24):2295–2303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Henningfield JE, Stapleton JM, Benowitz NL, Grayson RF, London ED. Higher levels of nicotine in arterial than in venous blood after cigarette smoking. Drug Alcohol Depend. 1993;33(1):23–29. [DOI] [PubMed] [Google Scholar]
- 34.Gritz ER, Baer-Weiss V, Jarvik ME. Titration of nicotine intake with full-length and half-length cigarettes. Clinical Pharmacology & Therapeutics. 1976;20(5):552–556. [DOI] [PubMed] [Google Scholar]
- 35.Perkins KA, Lerman C, Keenan J, Fonte C, Coddington S. Rate of nicotine onset from nicotine replacement therapy and acute responses in smokers. Nicotine Tob Res. 2004;6(3):501–507. [DOI] [PubMed] [Google Scholar]
- 36.Ramôa CP, Hiler MM, Spindle TR, et al. Electronic cigarette nicotine delivery can exceed that of combustible cigarettes: a preliminary report. Tob Control. 2016;25(e1):e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Baldassarri SR, Hillmer AT, Anderson JM, et al. Use of electronic cigarettes leads to significant beta2-nicotinic acetylcholine receptor occupancy: evidence from a PET imaging study. Nicotine and Tobacco Research. 2017;20(4):425–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Benowitz NL, Nardone N, Jain S, et al. Comparison of urine 4-(methylnitrosamino)-1-(3) pyridyl-1-butanol and cotinine for assessment of active and passive smoke exposure in urban adolescents. Cancer Epidemiol Biomarkers Prev. 2018;27(3):254–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Carey FR, Rogers SM, Cohn EA, Harrell MB, Wilkinson AV, Perry CL. Understanding susceptibility to e-cigarettes: A comprehensive model of risk factors that influence the transition from non-susceptible to susceptible among e-cigarette naïve adolescents. Addict Behav. 2019;91:68–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wang MP, Ho SY, Leung LT, Lam TH. Electronic cigarette use and respiratory symptoms in Chinese adolescents in Hong Kong. JAMA pediatrics. 2016;170(1):89–91. [DOI] [PubMed] [Google Scholar]
- 41.McConnell R, Barrington-Trimis JL, Wang K, et al. Electronic cigarette use and respiratory symptoms in adolescents. American journal of respiratory and critical care medicine. 2017;195(8):1043–1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Vardavas CI, Anagnostopoulos N, Kougias M, Evangelopoulou V, Connolly GN, Behrakis PK. Short-term pulmonary effects of using an electronic cigarette: impact on respiratory flow resistance, impedance, and exhaled nitric oxide. Chest. 2012;141(6):1400–1406. [DOI] [PubMed] [Google Scholar]
- 43.Ferrari M, Zanasi A, Nardi E, et al. Short-term effects of a nicotine-free e-cigarette compared to a traditional cigarette in smokers and non-smokers. BMC pulmonary medicine. 2015;15(1):120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ghosh A, Coakley RC, Mascenik T, et al. Chronic e-cigarette exposure alters the human bronchial epithelial proteome. American journal of respiratory and critical care medicine. 2018;198(1):67–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Song M-A, Freudenheim JL, Brasky TM, et al. Biomarkers of Exposure and Effect in the Lungs of Smokers, Nonsmokers, and Electronic Cigarette Users. Cancer Epidemiol Biomarkers Prev. 2020;29(2):443–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lee H-W, Park S-H, Weng M-w, et al. E-cigarette smoke damages DNA and reduces repair activity in mouse lung, heart, and bladder as well as in human lung and bladder cells. Proceedings of the National Academy of Sciences. 2018;115(7):E1560–E1569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Khosravi M, Lin R-L, Lee LY. Inhalation of electronic cigarette aerosol induces reflex bronchoconstriction by activation of vagal bronchopulmonary C-fibers. American Journal of Physiology-Lung Cellular and Molecular Physiology. 2018;315(4):L467–L475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sussan TE, Gajghate S, Thimmulappa RK, et al. Exposure to electronic cigarettes impairs pulmonary anti-bacterial and anti-viral defenses in a mouse model. PloS one. 2015;10(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Benowitz NL, Fraiman JB. Cardiovascular effects of electronic cigarettes. Nature Reviews Cardiology. 2017;14(8):447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Outbreak of Lung Disease Associated with E-Cigarette Use, or Vaping. Centers for Disease Control and Prevention, https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html. 2019. [Google Scholar]
- 51.Layden JE, Ghinai I, Pray I, et al. Pulmonary Illness Related to E-Cigarette Use in Illinois and Wisconsin - Preliminary Report. N Engl J Med. 2019. [DOI] [PubMed] [Google Scholar]
- 52.Davidson K. Outbreak of Electronic-Cigarette–Associated Acute Lipoid Pneumonia—North Carolina, July–August 2019. MMWR. Morbidity and mortality weekly report. 2019;68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lewis N. E-cigarette Use, or Vaping, Practices and Characteristics Among Persons with Associated Lung Injury—Utah, April–October 2019. MMWR. Morbidity and mortality weekly report. 2019;68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Butt YM, Smith ML, Tazelaar HD, et al. Pathology of Vaping-Associated Lung Injury. New England Journal of Medicine. 2019. [DOI] [PubMed] [Google Scholar]
- 55.Blount BC, Karwowski MP, Morel-Espinosa M, et al. Evaluation of Bronchoalveolar Lavage Fluid from Patients in an Outbreak of E-cigarette, or Vaping, Product Use-Associated Lung Injury - 10 States, August-October 2019. MMWR. Morbidity and mortality weekly report. 2019;68(45):1040–1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Baldassarri SR, Chupp GL, Leone FT, Warren GW, Toll BA. Practise Patterns and Perceptions of Chest Health Care Providers on Electronic Cigarette Use: An In-Depth Discussion and Report of Survey Results. Journal of Smoking Cessation. 2017:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hartmann-Boyce J, Begh R, Aveyard P. Electronic cigarettes for smoking cessation. BMJ (Clinical research ed.). 2018;360. [DOI] [PubMed] [Google Scholar]
- 58.Zhu S-H, Zhuang Y-L, Wong S, Cummins SE, Tedeschi GJ. E-cigarette use and associated changes in population smoking cessation: evidence from US current population surveys. BMJ (Clinical research ed.). 2017;358:j3262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Biener L, Hargraves JL. A longitudinal study of electronic cigarette use among a population-based sample of adult smokers: association with smoking cessation and motivation to quit. Nicotine Tob Res. 2015;17(2):127–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Jamal A, Homa DM, O’Connor E, et al. Current cigarette smoking among adults - United States, 2005–2014. MMWR. Morbidity and mortality weekly report. 2015;64(44):1233–1240. [DOI] [PubMed] [Google Scholar]
- 61.Rahman MA, Hann N, Wilson A, Mnatzaganian G, Worrall-Carter L. E-cigarettes and smoking cessation: evidence from a systematic review and meta-analysis. PloS one. 2015;10(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Caponnetto P, Campagna D, Cibella F, et al. EffiCiency and Safety of an eLectronic cigAreTte (ECLAT) as tobacco cigarettes substitute: a prospective 12-month randomized control design study. PloS one. 2013;8(6):e66317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bullen C, Howe C, Laugesen M, et al. Electronic cigarettes for smoking cessation: a randomised controlled trial. Lancet. 2013;382(9905):1629–1637. [DOI] [PubMed] [Google Scholar]
- 64.Hajek P, Phillips-Waller A, Przulj D, et al. A Randomized Trial of E-Cigarettes versus Nicotine-Replacement Therapy. New England Journal of Medicine. 2019. [DOI] [PubMed] [Google Scholar]
- 65.Rojewski AM, Baldassarri S, Cooperman NA, et al. Exploring Issues of Comorbid Conditions in People Who Smoke. Nicotine Tob Res. 2016;18(8):1684–1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Shahab L, Goniewicz ML, Blount BC, et al. Nicotine, carcinogen, and toxin exposure in long-term e-cigarette and nicotine replacement therapy users: A cross-sectional study. Annals of internal medicine. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gilpin EA, Pierce JP, Farkas AJ, Farkas AJ. Duration of smoking abstinence and success in quitting. Journal of the National Cancer Institute. 1997;89(8):572. [DOI] [PubMed] [Google Scholar]
- 68.D’Ruiz CD, Graff DW, Yan XS. Nicotine delivery, tolerability and reduction of smoking urge in smokers following short-term use of one brand of electronic cigarettes. BMC public health. 2015;15:991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Goniewicz ML, Gawron M, Smith DM, Peng M, Jacob P, Benowitz NL. Exposure to Nicotine and Selected Toxicants in Cigarette Smokers Who Switched to Electronic Cigarettes: A Longitudinal Within-Subjects Observational Study. Nicotine Tob Res. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.McRobbie H, Phillips A, Goniewicz ML, et al. Effects of Switching to Electronic Cigarettes with and without Concurrent Smoking on Exposure to Nicotine, Carbon Monoxide, and Acrolein. Cancer prevention research (Philadelphia, Pa.). 2015;8(9):873–878. [DOI] [PubMed] [Google Scholar]
- 71.Mackay J, Eriksen M, Eriksen MP. The tobacco atlas. World Health Organization; 2002. [Google Scholar]
- 72.Bernstein SL. Electronic cigarettes: more light, less heat needed. The Lancet Respiratory Medicine. 2016;4(2):85–87. [DOI] [PubMed] [Google Scholar]
- 73.Ghosh A, Coakley RD, Ghio AJ, et al. Chronic E-Cigarette Use Increases Neutrophil Elastase and Matrix Metalloprotease Levels in the Lung. American journal of respiratory and critical care medicine. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Chun LF, Moazed F, Calfee CS, Matthay MA, Gotts JE. Pulmonary toxicity of e-cigarettes. American Journal of Physiology-Lung Cellular and Molecular Physiology. 2017;313(2):L193–L206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Gotts JE, Jordt S-E, McConnell R, Tarran R. What are the respiratory effects of e-cigarettes? BMJ (Clinical research ed.). 2019;366:l5275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Leventhal AM, Strong DR, Kirkpatrick MG, et al. Association of electronic cigarette use with initiation of combustible tobacco product smoking in early adolescence. Jama. 2015;314(7):700–707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Proctor RN, Proctor R. Golden holocaust: origins of the cigarette catastrophe and the case for abolition. Univ of California Press; 2011. [Google Scholar]
- 78.Dobbs PD, Hammig B, Sudduth A. 2015 legislative update of e-cigarette youth access and exposure laws. Preventive medicine. 2016;88:90–94. [DOI] [PubMed] [Google Scholar]
- 79.Gourdet CK, Chriqui JF, Chaloupka FJ. A baseline understanding of state laws governing e-cigarettes. Tob Control. 2014;23(suppl 3):iii37–iii40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Murthy VH. E-cigarette use among youth and young adults: a major public health concern. JAMA pediatrics. 2017;171(3):209–210. [DOI] [PubMed] [Google Scholar]
- 81.Roditis M, Lee J, Halpern-Felsher BL. Adolescent (mis) perceptions about nicotine addiction: Results from a mixed-methods study. Health education & behavior. 2016;43(2):156–164. [DOI] [PubMed] [Google Scholar]