Abstract
Background:
Both human health and the health systems we depend on are increasingly threatened by a range of environmental crises, including climate change. Paradoxically, health care provision is a significant driver of environmental pollution, with surgical and anesthetic services among the most resource-intensive components of the health system.
Objectives:
This analysis aimed to summarize the state of life cycle assessment (LCA) practice as applied to surgical and anesthetic care via review of extant literature assessing environmental impacts of related services, procedures, equipment, and pharmaceuticals.
Methods:
A state-of-the-science review was undertaken following a registered protocol and a standardized, LCA-specific reporting framework. Three bibliographic databases (Scopus®, PubMed, and Embase®) and the gray literature were searched. Inclusion criteria were applied, eligible entries critically appraised, and key methodological data and results extracted.
Results:
From 1,316 identified records, 44 studies were eligible for inclusion. The annual climate impact of operating surgical suites ranged between 3,200,000 and . The climate impact of individual surgical procedures varied considerably, with estimates ranging from . Anesthetic gases; single-use equipment; and heating, ventilation, and air conditioning system operation were the main emissions hot spots identified among operating room- and procedure-specific analyses. Single-use equipment used in surgical settings was generally more harmful than equivalent reusable items across a range of environmental parameters. Life cycle inventories have been assembled and associated climate impacts calculated for three anesthetic gases () and 20 injectable anesthetic drugs ().
Discussion:
Despite the recent proliferation of surgical and anesthesiology-related LCAs, extant studies address a miniscule fraction of the numerous services, procedures, and products available today. Methodological heterogeneity, external validity, and a lack of background life cycle inventory data related to many essential surgical and anesthetic inputs are key limitations of the current evidence base. This review provides an indication of the spectrum of environmental impacts associated with surgical and anesthetic care at various scales. https://doi.org/10.1289/EHP8666
Introduction
It has been a decade since climate change was declared this century’s greatest public health threat (Costello et al. 2009), yet greenhouse gas (GHG) emissions continue largely unabated (Friedlingstein et al. 2019). The scale of change required to meet the goals of the Paris Agreement is now immense: Last year’s reduction in global carbon dioxide () emissions due to COVID-19–related societal upheaval (6.4%; Tollefson 2021) is still less than the average year-on-year reductions that must be achieved over the next decade to limit global warming to 1.5°C above preindustrial levels (7.6%; United Nations Environment Programme 2019).
In the absence of immediate, concerted, and deep change, the health of current and future populations is likely to be drastically affected by climate change–related thermal stress, air pollution, extreme weather events, undernutrition, vector-borne disease, mental illness, conflict, and migration, with those least responsible for historical emissions most afflicted (Carleton et al. 2020; Watts et al. 2019). Health systems are also at increased risk of supply-chain disruption, resource scarcity, and infrastructure damage due to climate change (Cimprich et al. 2019; World Health Organization 2020). Furthermore, the health-related impacts of other environmental crises, such as biodiversity loss, ocean acidification, chemical pollution, and habitat fragmentation and loss, are expected to compound those of the climate crisis (Bologna and Aquino 2020; Gibb et al. 2020; Steffen et al. 2015).
Though historically underappreciated, health care provision itself is a significant driver of environmental pollution, responsible for emissions of 2%–5% of global GHG, sulfur dioxide (v), nitrogen oxide (), and particulate matter [(PM) with aerodynamic diameter less than ], according to recent environmentally extended multiregional input–output (EE-MRIO) analyses (Karliner et al. 2019; Lenzen et al. 2020; Pichler et al. 2019; Watts et al. 2019, 2020). Contrary to the primum non nocere axiom, health care pollution is associated with a substantial health burden. Conservative estimates indicate that health sector pollution may result in an annual loss of 23,000 (4,500–610,000, range) and 388,000 disability-adjusted life years (244,000–531,000, range; DALYs) in Canada and the United States, respectively (Eckelman et al. 2018, 2020). Although this health burden remains largely unrecognized, the latter estimate is comparable to the annual number of deaths attributable to preventable medical errors in the United States (Eckelman and Sherman 2018).
As a consequence of this adverse feedback loop, where the health sector functions as both perpetrator and victim of environmental pollution, health care is uniquely positioned to benefit from health and environmental co-benefits resulting from mitigative action (Eckelman et al. 2018; Lenzen et al. 2020). Due to its highly resource-intensive nature, reducing the environmental impacts of surgical and anesthetic care is expected to be among the highest yielding mitigation opportunities in the health sector (MacNeill et al. 2017; Selvy et al. 2020).
Although top-down, expenditure-based EE-MRIO analyses provide a useful indication of sector-level environmental impacts, process-based life cycle assessment (LCA) is the most established approach for both quantifying impacts of specific health care activities and identifying effective mitigation strategies (Weisz et al. 2020). LCA is designed to facilitate the quantification of material and energy inputs and outputs of a defined system over its life cycle, as well as resulting contributions to regional- and global-scale resource depletion and environmental degradation (Hellweg and Milà i Canals 2014). LCA is an internationally standardized methodology that typically consists of four main phases (Finkbeiner et al. 2006). The first phase, which involves outlining study objectives and scope, requires selection of study system boundaries, life cycle stages to be analyzed (e.g., raw material extraction, production, packaging, transportation, use, and disposal, or a defensible subset of these based on study objectives), an appropriate metric for comparing and reporting impacts known as the functional unit, and the impact categories (the suite of resource depletion and environmental concerns of interest) for which contributions per functional unit are assessed. This phase is followed by life cycle inventory (LCI) analysis, which involves compilation and quantification of inputs (e.g., energy and raw materials) and outputs (e.g., emissions and waste streams) for each process within the defined system. Due to the complexity of this phase, LCA practitioners typically employ established LCI data sets (e.g., EcoInvent) that contain granular and region-specific data on hundreds of background processes. The third phase, known as life cycle impact assessment (LCIA), characterizes potential contributions to impact categories that stem from energy and material flows detailed in the inventory. The final phase of LCA is the interpretation stage, which involves evaluation of the LCI and LCIA in the context of the study’s goal and scope (Hellweg and Milà i Canals 2014).
Although the application of LCA to health care has lagged behind other sectors (Campion et al. 2015), its use has expanded rapidly in recent years, including in the surgical discipline (Cimprich et al. 2019). To date, three systematic reviews have surveyed the application of LCA to health care generally, the most recent of which is already 4 y old in its temporal coverage (Alshqaqeeq et al. 2020; Brown et al. 2012; McGain and Naylor 2014). An important aspect is that none of these reviews has assessed the relative quality of their primary studies, with efforts instead focused on study identification, disciplinary coverage, and impact reporting. This lack of critical evaluation remains a key limitation of existing evidence summaries. Only one systematic review, which was published during the conduct of this research, has explored the application of LCA to the surgical discipline specifically: Rizan et al. (2020) evaluated existing studies reporting specifically on the climate impacts of surgical procedures. To the best of the authors’ knowledge, no review to date has assessed and critically evaluated the application of LCA across surgical and anesthetic services as a whole, encompassing not only surgical procedures but also operation of surgical suites and the provision and use of related equipment and pharmaceuticals as well.
To address this research gap, we conducted a state-of-the-science review to assess the state of LCA practice in surgical and anesthetic care using a standardized, LCA-specific reporting framework (Zumsteg et al. 2012). Via systematic identification, appraisal, and synthesis of available research, this review aimed to a) highlight LCA’s critical role in guiding sustainability interventions in surgical settings; b) examine methodological challenges and limitations of the current evidence base; c) identify priorities for future research; and d) help operationalize LCA in this important field.
Methods
Unlike the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) framework for reporting systematic reviews in health sciences (Moher et al. 2009), currently no established best practice exists for designing, conducting, and reporting systematic reviews of LCA studies (Zumsteg et al. 2012). Nor is there a readily accessible database (e.g., PROSPERO) where review protocols can be prospectively logged and tracked in the discipline of environmental sciences (Costa et al. 2019). This state-of-the-science review was instead guided by the Standardized Technique for Assessing and Reporting Reviews of Life Cycle Assessment Data (STARR-LCA), which is a PRISMA-based framework designed specifically to help address this research gap (Zumsteg et al. 2012). The completed STARR-LCA systematic review checklist, which was used to inform review design and manuscript preparation, is available in the Supplemental Material (Table S1). Furthermore, the review protocol, which conforms to the RepOrting standards for Systematic Evidence Syntheses (ROSES; Haddaway et al. 2018), was prospectively registered on the Open Science Framework platform to allow readers the opportunity to assess the degree to which this review adhered to its initial plan (Drew 2020). The accompanying ROSES for Systematic Review Protocols standardized reporting form (Haddaway et al. 2017) is available within the protocol’s supplemental material online.
Search Strategy
Input on database selection and search terms was sought from the Evidence Synthesis & Information Services Librarian based at the authors’ institution. Selected bibliographic databases included Scopus®, PubMed, and Embase®. The temporal scope of the search spanned from database inception to 15 May 2020 and the query string used within each database combined search terms relating to LCA with those relating to surgery and anesthesiology (see Boxes S1–S3 in the Supplemental Material). MeSH and Emtree terms were incorporated within query strings for PubMed and Embase® databases, respectively. No search limits were applied, and alerts were set up to identify relevant articles published during the review process and until provisional manuscript acceptance on 14 May 2021.
A supplemental gray literature search was also undertaken on 21 May 2020 by reviewing publications listed on the websites of the Center for Sustainable Health care (CSH), the CSH Sustainable Operating Theatres Network, and the National Health Service (NHS) Sustainable Development Unit. A further search, which aimed to identify relevant reports and theses not otherwise registered in bibliographic databases, was conducted on 10 June 2020 using the Advanced Search feature in Google and combining key search terms used in our Scopus® query string. For each search undertaken, results were limited to portable document format (e.g., “life cycle assessment AND surgery, filetype:pdf”) and the first 50 records were screened.
The sensitivity of our search strategy was crosschecked with a list of benchmark articles compiled by manually reviewing reference lists of extant systematic reviews of health care–related life cycle assessments (Alshqaqeeq et al. 2020; Brown et al. 2012; McGain and Naylor 2014; see Box S4 in the Supplemental Material). All benchmark articles were captured by the search strategy.
Article Screening and Study Inclusion Criteria
Identified records were screened by two independent reviewers (J.D. and J.S.F.), with a third reviewer independently tasked with conflict resolution (S.D.C.). Entries were assigned to one of seven categories based on predetermined exclusion and inclusion criteria (Table S2 in the Supplemental Material). In summary, studies were excluded based on title and abstract if they could not be accessed, were not written in English, or did not report on original research assessing environmental impact(s) in relation to health care. Potentially eligible entries were excluded based on full text if they did not assess environmental impact(s) in relation to surgery or anesthesiology or did not use an LCA-based methodology to do so. Entries reporting preliminary results, such as conference abstracts or papers that were later updated and revised in a peer-reviewed journal article, were excluded from the analysis to avoid double counting. Eligible entries were then categorized according to their scope of assessment: operating room, surgical procedure, or related equipment and pharmaceuticals.
Data Coding and Extraction
Data from eligible entries were coded and extracted according to predetermined forms. A methodological pro forma based on the four phases of LCA, as described in the International Organization for Standardization (ISO) reporting standards (Finkbeiner et al. 2006; Hellweg and Milà i Canals 2014), was used to organize important study attributes and methodological choices relating to scope, inventory compilation, impact assessment, and interpretation. Similarly, a results pro forma was used to organize reported study end points and harmonize relative contribution reporting via matching of reported life cycle stages to a list of predetermined stages (e.g., operating room energy use) and substages (e.g., heating ventilation and air conditioning) specific to this review (see Table S3 in the Supplemental Material).
Critical Appraisal
Eligible entries were critically appraised according to a predetermined appraisal pro forma. The pro forma uses a point-based scoring system based on Weidema’s (1997) guidelines for critical review of LCA to assess each eligible entry. The scoring system consists of 16 appraisal criteria divided between the four phases of LCA and addresses a range of study quality indicators, including internal validity, external validity, consistency, transparency, and bias. Important potential effect modifiers are also listed within the pro forma alongside the relevant appraisal criterion. For each eligible entry, assigned points were tallied and a percentage score was calculated to provide an indication of overall study quality (see Excel Table S1 in the Supplemental Material).
Data Synthesis and Presentation
Due to expected methodological heterogeneity among studies (i.e., variation in system scope, functional unit, data acquisition, and assessment methods), results were not intended to be combined through meta-analysis. Instead, quantitative data were summarized graphically, with results and hot spots from individual case studies presented separately and potential effect modifiers (e.g., LCA method) and critical appraisal scores clearly annotated to aid interpretation of results and highlight potential reasons for discrepancies among study results other than underlying differences in physical flow realities. Qualitative data, as well as data from the critical appraisal, were brought together in a narrative synthesis to contextualize study findings, discuss methodological decision-making, highlight strengths and limitations of the current evidence base, and ultimately draw conclusions about the state of LCA practice in surgical and anesthetic services, including key challenges moving forward.
Results
Search Results
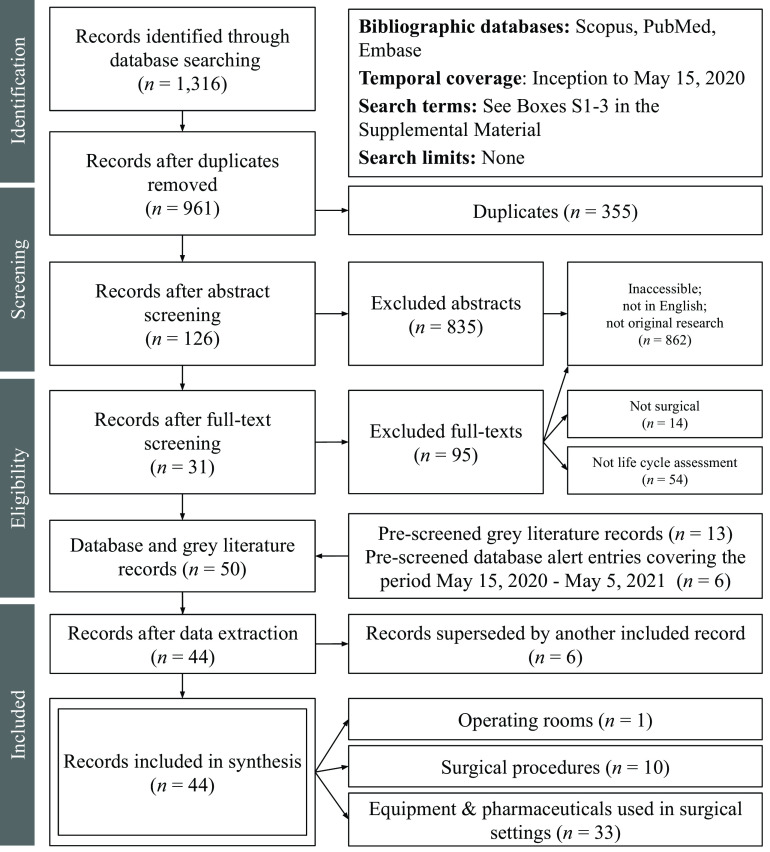
A total of 1,316 entries were identified via bibliographic searching, including 355 duplicates; 961 entries were independently screened based on title and abstract and, following resolution of conflicting decisions for 107 entries, 126 were selected for independent full-text review. Of these, 31 studies were determined to be eligible, and a further 13 relevant studies were identified through gray literature searching. During the data extraction process, six studies were excluded because they reported results that were covered in another included article (e.g., conference papers that were superseded by journal articles). Six additional eligible studies were identified via search strategy email alerts during the conduct and peer review of our analysis resulting in a final total of 44 studies. Figure 1 summarizes search results using a PRISMA-based flow diagram.
Figure 1.
Flow diagram summarizing search results.
Study Characteristics
Among the 44 eligible studies, one study examined impact contributions from operating rooms generally, 10 studies characterized contributions from specific surgical procedures, and 33 assessed the environmental impact contributions from the provision and use of surgical or anesthetic equipment or pharmaceuticals. Eligible studies were primarily peer-reviewed journal articles (), with other publication types including reports (2), theses (2), correspondence pieces (1), preprint commentaries (1), reviews (1), and online articles (1). Regarding geographical distribution, most studies were specific to the United States (), followed by Australia (7), the United Kingdom (6), Sweden (3), Germany (2), Austria (1), Chile (1), India (1), Netherlands (1), Singapore (1), and Switzerland (1), whereas two studies were multinational in scope. Anesthesiology was the most studied discipline among included studies (), followed by obstetrics and gynecology (7), ophthalmology (3), urology and nephrology (2), dermatology and plastic surgery (2), gastroenterology (1), neurology (1), orthopedics (1), and oncology (1), whereas one study was multidisciplinary (gastroenterology, obstetrics and gynecology, urology and nephrology), and 15 studies were not specific to any particular discipline(s).
Methodological Design
Regarding LCA method, the most common approach was attributional (), followed by hybrid (4), economic input–output (EIO; 3), and consequential (1). Most studies reported being guided by ISO LCA standards (ISO 14040 and 14044; ), whereas other studies followed the Publicly Available Specification (PAS) 2050 standard for reporting of GHG emissions in the United Kingdom (3), the GHG Protocol standard (3), or a combination of the preceding (1). Ten studies did not specify which, if any, standard was followed.
Among studies that reported using inventory databases for background systems (), the majority (88%, ) drew from EcoInvent, followed by both the U.S. Life Cycle Inventory Database (USLCI; 15%, ) and the European reference Life Cycle Database (ELCD; 12%, ). In terms of environmental impact categories assessed, all studies included global warming potential (GWP) and nearly two-thirds included at least one other impact category (64%, ), with eutrophication potential (EP, ), acidification potential (AP, ), photochemical oxidant creation potential (POCP, ), and ozone depletion potential (ODP; ) among the most assessed. The Tool for the Reduction and Assessment of Chemical and Other Environmental Impacts (TRACI) was the most used characterization method (), along with ReCiPe (RIVM and Radboud University, CML and PRé Consultants; ), Intergovernmental Panel on Climate Change (IPCC; ), Centrum voor Milieuwetenschappen (CML; ), EcoIndicator (), and the Cumulative Energy Demand (CED) method (); 13 studies did not describe how impacts were characterized.
Approximately one-half of included studies reported using a dedicated impact assessment software package (55%, ) and, among those, 15 studies used SimaPro, and a single study used each of: Chain Management by Life Cycle Assessment (CMLCA), Ganzheitliche Bilanz (GaBi), LCOPT, OpenLCA, Packaging Industry Research Association Environmental Management System Software (PEMS), The Activity Browser, TRACI, Umberto NXT, and the EIO-LCA tool from Carnegie Mellon University in Pittsburgh, Pennsylvania. Tables 1–2 summarize the characteristics and methodological design of each included study. Further information can be found in the completed methodological pro forma (see Excel Table S2 in the Supplemental Material).
Table 1.
Characteristics and methodological overview of studies employing life cycle assessment to quantify environmental impact contributions from operating rooms and surgical procedures.
| Reference (type) | Discipline: Case studies (Country) | Life cycle assessment method (Standard) | Functional unit | System boundaries | Productiona | Transporta | OR energy usea | Pharmaceuticalsa | Use/Reusea | Disposala | Inventory database(s) [Characterization method] (Software) | Impact categories assessed | Impacts reportedb | Contributionsc |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Life cycle assessments of operating rooms | ||||||||||||||
| MacNeill et al. 2017 (Article) | Nonspecific: surgical suite operation at 1) VGH 2) UMMC 3) JRH (Canada, UK, USA) | Attributional (GHG Protocol) | 1 y of surgical suite operation | OR door-to-door | Y | N | Y | Y | Y | Y | [Andersen et al. 2012] | 1 | Y | Y |
| Life cycle assessments of surgical procedures | ||||||||||||||
| Berner et al. 2017 (Correspondence) | Plastic surgery: 1) rhinoplasty 2) abdominoplasty 3) bilateral breast augmentations (Chile) | Attributional (GHG Protocol)d | One procedure | OR door to recovery room discharge | N | Y | Y | N | N | Y | – | 1 | Y | Y |
| Campion et al. 2012 (Article) | O&G: 1) cesarian delivery 2) vaginal delivery (USA) | Attributional (ISO) | One procedure | OR door-to-door | Y | N | Y | N | Y | Y | USLCI, EcoInvent, IDEMAT, Franklin US [TRACI] | 8 | Ne,f | Y |
| Gatenby 2011 (Article)g | Gastroenterology: 1) fundoplication surgery 2) ongoing medical management (UK) | EIO (Unspecified) | Management of one patient with GERD (0–20 years) | Preop work-up to post-op out-patient appointment | – | – | – | – | – | – | – | 1 | Y | Y |
| Morris et al. 2013 (Article) | Ophthalmology: 1) cataract surgery (UK) | Hybrid (PAS 2050) | One procedure | Referral to discharge at out-patient appointment | Y | Y | Y | Y | Y | Y | – | 1 | Y | Y |
| Power et al. 2012 (Article) | Gastroenterology, O&G, urology and nephrology: 1) minimally invasive surgery (USA) | EIO (GHG Protocol) | One year of procedures performed in the United States (2009; ,520,223) | OR door-to-door | N | N | N | Y | N | Y | – | 1 | Y | Y |
| Tan and Lim 2021 | Dermatology: 1) 30-min skin cancer excision in clinic 2) 30-min skin cancer excision in hospital (Australia) | Attributional (Unspecified) | One procedure | OR door-to-door | Y | Y | Y | N | Y | Y | Evah OzLCI2019 [IMPACT ] (OpenLCA) | 1 | Yf | Y |
| Thiel et al. 2015 (Article) | O&G: hysterectomy: 1) vaginal 2) abdominal 3) laparoscopic 4) robotic (USA) | Hybrid (ISO) | One procedure | OR door-to-door | Y | Y | Y | Y | Y | Y | USLCI, EcoInvent [TRACI] | 10 | Ne | Y |
| Thiel et al. 2017 (Article) | Ophthalmology: 1) cataract surgery (India) | Hybrid (ISO) | One procedure | Preop cleaning to OR exit | Y | N | Y | Y | Y | Y | EcoInvent [TRACI] | 10 | Y | Y |
| Thiel et al. 2018 (Article) | O&G: laparoscopic hysterectomy: 1-16) various mitigation scenarios (USA) | Hybrid (ISO) | One procedure | OR door-to-door | Y | Y | Y | Y | Y | Y | USLCI, EcoInvent [TRACI] | 1 | Y | Y |
| Woods et al. 2015 (Article) | O&G, oncology: endometrial staging: 1) laparotomy 2) laparoscopy 3) robotic (USA) | Attributional (PAS2050, GHG Protocol) | One procedure | OR door-to-door | N | N | Y | N | N | Y | – | 1 | Y | Y |
Note: –, Unspecified; EIO, Economic Input-Output Life Cycle Assessment; GERD, gastroesophageal reflux disease; GHG, greenhouse gas; ISO, International Organization for Standardization standards 14040 and 14044; JRH, John Radcliffe Hospital; min, minute; O&G, obstetrics and gynecology; OR, operating room; PAS, Publicly Available Specification; TRACI, Tool for Reduction and Assessment of Chemicals and Other Environmental Impacts; UK, United Kingdom; UMMC, University of Minnesota Medical Center; USA, United States of America; USLCI, United States Life Cycle Inventory Database; VGH, Vancouver General Hospital.
“Y” indicates that the specified life cycle stage was included in the analysis (“N” indicates exclusion).
Impacts reported refers to whether or not numerical impact values were reported in the relevant reference.
Contributions refers to whether or not results of a contribution analysis were reported in the relevant reference.
Life cycle assessment method inferred from text.
Relative impacts reported graphically.
Absolute impact values were provided by the article’s corresponding author.
Life cycle stage categorization was not applicable to the system used in this article.
Table 2.
Characteristics and methodological overview of studies employing life cycle assessment to quantify environmental impact contributions from provision and use of equipment and pharmaceuticals used in surgical settings.
| Reference (type) | Discipline: Case studies (Country) | Life cycle assessment method (Standard) | Functional unit | System boundaries | Raw materialsa | Productiona | Packaginga | Transporta | Use/reusea | Disposala | Inventory database(s) [Characterization method] (Software) | # Impact categories | Impacts reportedb |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Equipment | |||||||||||||
| Allison et al. 2020 (Preprint commentary) | Nonspecific: surgical masks: 1) single-use surgical 2–5) reusable cloth and variable washing conditions (UK) | Attributional (Unspecified)d | 1 y of use by the UK population | Cradle to grave | Y | Y | Y | Y | Y | Y | GaBi, EcoInvent [Environmental Footprint] (GaBi) | 14 | Y |
| Campion et al. 2015 (Article) | O&G: 1–15) disposable custom packs for delivering infants (USA, Thailand) | Attributional (ISO) | One item | Cradle to grave | Y | Y | N | Y | Y | Y | EcoInvent, USLCI, Industry Data LCA database [TRACI] | 10 | Y |
| Carre 2008 (Report) | Nonspecific: surgical gown and huck towel: 1) disposable 2) reusable (Australia) | Attributional (ISO) | One use | Cradle to grave | Y | Y | Y | Y | Y | Y | EcoInvent [CML, EcoIndicator] | 8 | Y |
| Davis et al. 2018 (Article) | Urology and nephrology: flexible ureteroscopes: 1) single-use 2) reusable (Australia) | Attributional (Unspecified)d | One use | Cradle to grave | Y | Y | N | N | Y | Y | – | 1 | Y |
| Donahue et al. 2020 (Article) | O&G: vaginal specula: 1) single-use acrylic 2) reusable steel 3) reusable surgical steel (USA) | Attributional (ISO)d | 20 uses | Cradle to grave | Y | Y | N | Y | Y | Y | EcoInvent, IDEMAT, GREET, WARM [IPCC] (SimaPro) | 1 | Y |
| Eckelman et al. 2012 (Article) | Anesthesiology: laryngeal mask airways 1) single-use 2) reusable (USA) | Attributional (ISO) | 40 uses | Cradle to grave | Y | Y | Y | Y | Y | Y | EcoInvent [BEES] (SimaPro) | 10 | Ye |
| Grimmond and Reiner 2012 (Article) | Nonspecific: sharps container systems: 1) disposable 2) reusable (USA) | Attributional (PAS 2050) | Provision for 100 occupied hospital beds for 1 y | Cradle to grave | N | Y | Y | Y | Y | Y | GaBi [IPCC] | 1 | Y |
| Ibbotson et al. 2013 (Article) | Nonspecific: surgical scissors: 1) disposable plastic 2) disposable stainless steel 3) reusable stainless steel (Germany) | Attributional (ISO) | 4,500 uses | Cradle to grave | Y | Y | Y | Y | Y | Y | EcoInvent, Australian Data 2007 [ReCiPe, CED Method] (SimaPro) | 18 | Yf |
| Ison and Miller 2000 (Article) | Nonspecific: suction receptacles: 1) disposable 2–3) reusable (UK) | Attributional LCA (Unspecified) | One kilogram of collected body fluids | Cradle to grave | Y | Y | Y | Y | Y | Y | [CML] (PEMS) | 5 | Y |
| Lee et al. 2021 (Article) | Nonspecific: face masks: 1) single-use surgical 2) reusable with embedded filtration layer (Singapore) | Attributional (Unspecified) | 1 month of use for one individual | Cradle to grave | Y | Y | Y | Y | Y | Y | EcoInvent [ReCiPe] (The Activity Browser) | 10 | Y |
| Leiden et al. 2020 (Article) | Neurology: single-level lumbar fusion instrument sets: 1) disposable 2) reusable (Germany) | Attributional (ISO) | One use | Cradle to grave | Y | Y | Y | Y | Y | Y | EcoInvent [CML, ReCiPe] (Umberto NXT) | 5 | N |
| Liang, 2019 (Thesis) | Anesthesiology: laryngeal mask airways: 1) disposable 2) reusable (Sweden) | Attributional (ISO) | 40 uses | Cradle to grave | Y | Y | Y | Y | Y | Y | EcoInvent, ELCD [ReCiPe] (SimaPro) | 7 | N |
| Lyons et al. 2021 (Article) | Orthopedics: femoral component of knee implant: 1) conventional manufacturing 2) additive manufacturing (USA) | Attributional (ISO) | One item | Cradle to grave | Y | Y | N | N | N | Y | – | 2 | Y |
| McGain et al. 2010 (Article) | Anesthesiology: plastic anesthetic drug trays 1) single-use 2) single-use with gauze and paper towel 3) reusable (Australia) | Attributional (ISO) | One use | Cradle to grave | Y | Y | Y | Y | Y | Y | EcoInvent (SimaPro) | 2 | Y |
| McGain et al. 2012 (Article) | Anesthesiology: central venous catheter insertion kits 1) single-use 2) reusable (Australia) | Attributional (ISO) | One use | Cradle to grave | Y | Y | Y | Y | Y | Y | EcoInvent (SimaPro) | 6 | Ye |
| McGain et al. 2017 (Article) | Anesthesiology: anesthetic equipment (breathing circuits, face masks, LMAs, direct- and video-laryngoscopes: 1–5) variable proportions of single-use and reusable items (Australia) | Consequential (ISO) | 1 y of use at one hospital | Cradle to grave | Y | Y | Y | Y | Y | Y | EcoInvent (SimaPro) | 6 | Y |
| McPherson et al. 2019 (Article) | Nonspecific: sharps container systems: 1) disposable 2) reusable (USA) | Attributional (PAS 2050) | Provision for 10,000 adjusted patient days of care | Cradle to grave | Y | Y | Y | Y | Y | Y | GaBi [IPCC] | 1 | Y |
| Mikusinska, 2012 (Thesis) | Nonspecific: surgical scrubs 1) single-use 2) reusable (Sweden) | Attributional (ISO) | One use | Cradle to grave | Y | Y | Y | Y | Y | Y | EcoInvent, ELCD [ReCiPe] (SimaPro) | 8 | Y |
| Rizan et al. 2021 (Article) | Nonspecific: personal protective equipment (masks, gloves, aprons, gowns, and face shields) | Attributional (ISO) | 6 months of provision in the UK during COVID-19 | Cradle to grave | Y | Y | Y | Y | Y | Y | EcoInvent [ReCiPe] (SimaPro) | 21 | Y |
| Schmutz et al. 2020 (Article) | Nonspecific: face masks: 1) single-use surgical 2) reusable cotton (Switzerland) | Attributional (Unspecified) | 5 d of use for one individual | Cradle to grave | Y | Y | N | N | Y | Y | EcoInvent [IPCC, AWARE] | 3 | Yf |
| Sherman et al. 2018 (Article) | Anesthesiology: laryngoscope handles and blades: 1–2) single-use plastic 3–4) single-use metal 4–9) reusable stainless steel with different reprocessing conditions (USA) | Attributional (ISO) | One use | Cradle to grave | Y | Y | Y | Y | Y | Y | EcoInvent, US-EI [TRACI] (SimaPro) | 10 | Y |
| Stripple et al. 2008 (Article) | Urology and nephrology: urinary catheters: 1) PVC 2) TPU 3) polyolefin-based elastomer (Sweden) | Attributional (ISO) | Catheterization of one patient for 1 y | Cradle to grave | Y | Y | N | Y | N | Y | [CML, EcoIndicator, EPS] | 13 | N |
| Unger and Landis 2016 (Article) | Nonspecific: reusable medical devices: 1-6) different reprocessing conditions (USA) | Attributional (ISO) | Provision at one facility over 1 y | Cradle to grave | Y | Y | Y | Y | Y | Y | ELCD, EcoInvent, USLCI [USEtox, TRACI] (TRACI) | 4 | Yf |
| Unger et al. 2017 (Article) | O&G: single-use medical devices and equipment used for four different hysterectomy approaches: 1–4) plastic-based 5–8) bio-polymer-based scenarios (USA) | Attributional (ISO) | One procedure | Cradle to grave | Y | Y | N | Y | N | Y | EcoInvent [TRACI, CED method] (SimaPro) | 10 | N |
| Van den Berghe and Zimmer 2011 (Online article) | Nonspecific: surgical gown 1) single-use 2) reusable (USA) | Attributional (ISO) | 50 uses | Cradle to grave | Y | Y | N | Y | Y | Y | EcoInvent [TRACI] (CMLCA) | 9 | Y |
| Vozzola et al. 2018 (Report) | Nonspecific: surgical drapes and tapes: 1) disposable 2) reusable (Netherlands) | Attributional (ISO) | 1,000 uses | Cradle to grave | Y | Y | Y | Y | Y | Y | Environmental Clarity Inc., EcoInvent, ELCD [CML] (SimaPro) | 12 | Y |
| Vozzola et al. 2020 (Article) | Nonspecific: surgical gown 1) disposable 2) reusable (USA) | Attributional (ISO) | 1,000 uses | Cradle to grave | Y | Y | Y | Y | Y | Y | Environmental Clarity Inc. | 3 | Y |
| Weisz et al. 2020 (Article) | Nonspecific: surgical gloves: 1) latex 2) nitrile (Austria) | Attributional (Unspecified) | 1 kg | Cradle to gate | Y | Y | N | N | N | N | EcoInvent | 1 | Y |
| Pharmaceuticals | |||||||||||||
| Hu et al. 2021 (Article) | Anesthesiology: general anesthetic agents: 1) desflurane 2) isoflurane 3) sevoflurane 4) propofol (UK) | Attributional (ISO) | One MAC-h or MAC-equivalent | Cradle to use | Y | Y | Y | Y | Y | N | EcoInvent (LCOPT) | 1 | Yf |
| McAlister et al. 2016 (Article) | Anesthesiology: 1) morphine infusion bag (Australia) | Attributional (ISO) | One standard infusion bag | Cradle to factory gate | Y | Y | Y | Y | N | N | AusLCI, EcoInvent | 6 | Y |
| Parvatker et al. 2019 (Article) | Anesthesiology: 20 injectable anesthetic agents (USA) | Attributional (ISO) | 1 kg of API | Cradle to gate | Y | Y | N | N | N | N | EcoInvent | 1 | Y |
| Sherman et al. 2012 (Article) | Anesthesiology: general anesthetic agents: 1) desflurane 2) isoflurane 3) sevoflurane 4) propofol (USA) | Attributional (Unspecified)d | One MAC-h or MAC-equivalent | Cradle to grave | Y | Y | Y | Y | Y | Y | EcoInvent | 1 | Yf |
| Tauber et al. 2019 (Article) | Ophthalmology: 1–4) unused pharmaceuticals following phacoemulsification cataract surgery (USA) | EIO (Unspecified) | One procedure | Cradle to gate | Y | Y | N | N | N | N | – | 3 | Ye |
Note: –, Unspecified; API, active pharmaceutical ingredient; AWARE, Available Water Remaining method; CED, cumulative energy demand; CML, Centrum voor Milieuwetenschappen; CMLCA, Chain Management by Life Cycle Assessment; EIO, Economic Input–Output Life Cycle Assessment; ELCD, European reference Life Cycle Database; GaBi, Ganzheitliche Bilanz; IPCC, Intergovernmental Panel on Climate Change; ISO, International Organization for Standardization standards 14040 and 14044; MAC, mean alveolar concentration; O&G, obstetrics and gynecology; PAS, Publicly Available Specification; PEMS, Packaging Industry Research Association Environmental Management System Software; PVC, polyvinyl chloride; TPU, thermoplastic polyurethane; TRACI, Tool for Reduction and Assessment of Chemicals and Other Environmental Impacts; UK, United Kingdom; USA, United States of America; USLCI, United States Life Cycle Inventory Database.
“Y” indicates that the specified life cycle stage was included within the analysis (“N” indicates exclusion).
Impacts reported refers to whether or not numerical impact values were reported within the relevant reference.
Contributions refers to whether or not results of a contribution analysis were reported within the relevant reference.
Life cycle assessment method inferred from text.
Selected impact categories only.
Impacts reported graphically.
Critical Appraisal
Eligible studies varied considerably in terms of quality, completeness, and risk of bias, with critical appraisal scores ranging between 44% and 89% (see Excel Table S1 in the Supplemental Material for the completed critical appraisal pro forma). Most notably, 11% of studies () did not clearly state their selected LCA methodology, and 23% () did not report which, if any, LCA standard was followed. Furthermore, nearly one-third of studies (30%, ) did not report numerical impact values, opting instead to report results either graphically (Hu et al. 2021; Ibbotson et al. 2013; Ison and Miller 2000; Schmutz et al. 2020; Sherman et al. 2012; Tan and Lim 2021; Unger and Landis 2016) or relative to the most or least impactful case study (Campion et al. 2012; Leiden et al. 2020; Liang 2019; Stripple et al. 2008; Thiel et al. 2015; Unger et al. 2017).
This general lack of transparency regarding methodological design and outcome reporting poses challenges for both study reproducibility and comparability. Separately, results of LCA studies are also prone to considerable variability arising from a combination of both data collection- and processing-related decisions and assumptions, alongside methodological and background inventory data choices, that are made by researchers while operating within LCA standards of practice (Weisz et al. 2020). In addition, many activities that contribute to the provision or use of a good or service vary naturally, giving rise to ontological uncertainty related to a given model input parameter. Nevertheless, only six studies (14%) reported undertaking an uncertainty analysis (e.g., Monte Carlo simulations). Sensitivity analyses were conducted by approximately half of the included studies () to test the impact of various methodological assumptions on study outcomes. The most common assumptions tested were alternate reprocessing practices (e.g., autoclave loading, sterilization techniques, detergents; ), alternate lifespans for reusable products (), alternate energy supplies (), and alternate disposal processes ().
Regarding the potential for bias, more than one-quarter of studies did not include a competing-interests statement (27%, ) or funding declaration (30%, ). Among those that did, authors of three studies reported having potential competing interests due to industry ties (McAlister et al. 2016; McPherson et al. 2019; Vozzola et al. 2020) and nine studies received funding from industry groups (Carre 2008; Hu et al. 2021; Leiden et al. 2020; McAlister et al. 2016; McPherson et al. 2019; Stripple et al. 2008; Van den Berghe and Zimmer 2011; Vozzola et al. 2018, 2020). Although industry partnerships risk introducing bias into the analysis, in many cases they represent the only way researchers can obtain granular data that are otherwise inaccessible due to propriety interests (Weisz et al. 2020). Among eligible studies that were not peer-reviewed journal articles, four studies did not report having been subject to independent, external critical review (Berner et al. 2017; Liang 2019; Van den Berghe and Zimmer 2011; Vozzola et al. 2018).
Operating Rooms
Only one study assessing the environmental impact contributions from operating rooms was identified. MacNeill et al. (2017) quantified the climate impact of 1 y (2011) of surgical suite operation at three case study hospitals: Vancouver General Hospital (VGH, Canada), University of Minnesota Medical Center (UMMC, United States), and John Radcliffe Hospital (JRH, United Kingdom). The study’s system boundary was defined as operating room door-to-door (i.e., exclusive to the intraoperative period and defining surgical suite as each hospital’s operating rooms, surrounding corridors, sterile core, and anesthetic and equipment rooms) and included the following life cycle activities: production of equipment, operating room energy use, pharmaceuticals, reuse of equipment, and disposal. The climate impact of the hospitals’ surgical suites ranged from 3,200,000 to per year and between 146 and per operation (when compared on a caseload basis), with provision and use of anesthetic gases and use of heating, ventilation, and air conditioning (HVAC) systems as the primary emissions hot spots (4%–63% and 16%–80% of the total impact, respectively; see Figure 2). Choice of anesthetic gas was the main determinant of variation in surgical suite GHG emissions found among the three case study hospitals, with avoidance of desflurane (a potent GHG) at JRH resulting in one-tenth of the anesthetic-related GHG emissions in comparison with the other two hospitals where desflurane represented 65%–76% of the anesthetic gas volume purchased.
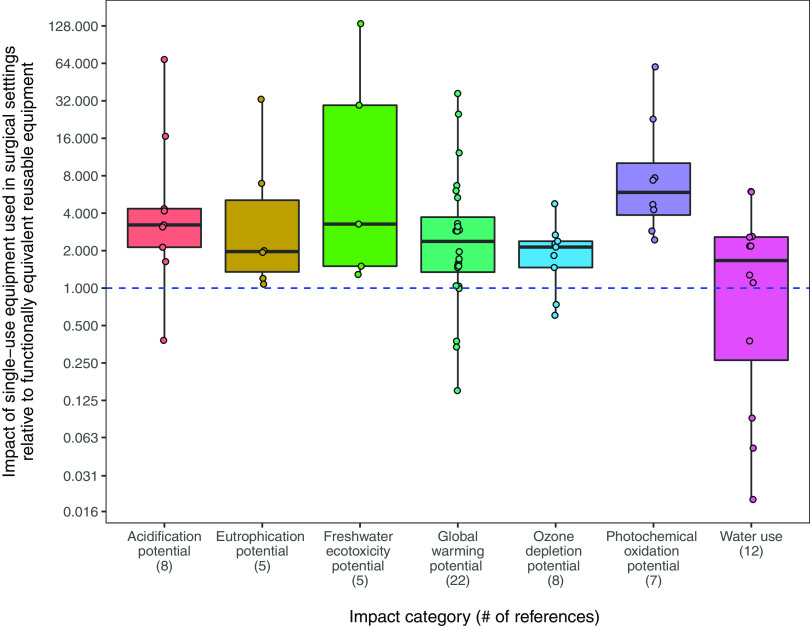
Figure 2.
Life cycle greenhouse gas emissions reported for 21 surgical procedures with impact contributions disaggregated by life cycle stage and considerable methodological variability among underlying references in terms of a) boundary of analysis, b) life cycle stages assessed, and c) overall completeness. Note: Direct comparison between case studies from different underlying sources is not advisable due to the heterogenous nature of the current evidence base. Substantial methodological differences exist among included references, especially with respect to system boundary, life cycle stages analyzed, and overall completeness (refer to Table 1 for details). This heterogeneity is evidenced by the highly variable per-procedure impact estimates () and inconsistent primary hot spot patterns depicted within Figure 2. Critical appraisal scores provide an indication of study quality. Each included reference was appraised using a predetermined point-based scoring system based on existing guidelines for critical review of life cycle assessment studies. Assigned points were tallied, and a percentage score was calculated to summarize results (see Excel Table S1 for details). Numerical data underlying Figure 2 are available in Excel Table S3. The disposal category in MacNeill et al. (2017) and the reuse category in both Campion et al. (2012) and Thiel et al. (2017) include production-related impacts due to disaggregated results not being reported. For case studies in Campion et al. (2012) and Tan and Lim (2021), absolute impact values and relative contributions were made available via the corresponding author. Absolute impact values for case studies in Thiel et al. (2015) were calculated based on information in the main text, whereas relative contributions for case studies in Thiel et al. (2015, 2018) were estimated from figures. With respect to MacNeill et al. (2017), impact estimates represent an average surgical procedure performed at each case study hospital (derived by dividing the global warming potential of annual surgical suite operation at the case study hospital by its annual surgical caseload). The dashed gray line partitions right and left axes. HVAC, heating, ventilation, and air conditioning; JRH, John Radcliffe Hospital; , kilograms of carbon dioxide equivalents; UK, United Kingdom; UMMC, University of Minnesota Medical Center; USA, United States of America; VGH, Vancouver General Hospital.
Surgical Procedures
Ten studies assessed the environmental impact contributions from at least one surgical procedure, including cesarian section (Campion et al. 2012); skin cancer excision (Tan and Lim 2021); rhinoplasty, bilateral breast augmentation and abdominoplasty (Berner et al. 2017); fundoplication (Gatenby 2011); cataract surgery (Morris et al. 2013; Thiel et al. 2017); vaginal, abdominal, laparoscopic, and robotic hysterectomy (Thiel et al. 2015, 2018); laparoscopy and robotic laparoscopy (Power et al. 2012); and endometrial staging via laparotomy, laparoscopy, and robotic laparoscopy (Woods et al. 2015). All studies used “one procedure” as the functional unit except Gatenby (2011) and Power et al. (2012), which both took an EIO-LCA approach and used management of gastroesophageal reflux disease for one patient over a defined period and 1 y of minimally invasive procedures in the United States as their respective functional units. The downstream boundary of analysis employed by most procedure-specific studies was all operating room services provided from patient entry to exit. Three studies, however, opted to include a slightly broader suite of related services, including preoperative eye cleaning to operating room exit (Thiel et al. 2017), preoperative workup to post-operative outpatient appointment (Gatenby 2011), and referral to discharge at outpatient appointment (Morris et al. 2013). Studies varied considerably in terms of the upstream or background system included in their assessment, with certain studies accounting for inputs and impact contributions from production of materials, transportation, operating room energy use, pharmaceuticals, and reuse and disposal of equipment and materials (Morris et al. 2013; Thiel et al. 2015, 2018), whereas others accounted for only one or two life cycle stages, such as operating room energy use and disposal of single-use materials and equipment (Woods et al. 2015) and carbon dioxide for abdominal insufflation and disposal of endoscopic trocars (Power et al. 2012). Not surprisingly, given the range of procedures characterized and upstream life cycle activities included, GHG emissions contributions from individual surgical procedures were found to vary considerably (). This heterogeneity in the current evidence base is clearly illustrated in Figure 2, which shows the range of procedures covered and their associated per-procedure global warming potentials disaggregated by life cycle stage.
Regarding GHG emissions hot spots, operating room energy use was responsible for 42% of total per-procedure emissions on average (, range 6%–76%), mainly from HVAC system demands. However, Thiel et al.’s (2015) study of impact contributions from four common approaches to hysterectomy, which was the only procedure-specific LCA to include the climate impact of anesthetic gases, estimated that the provision and use of anesthetic gases contributes 28%–69% toward hysterectomy’s total life cycle GHG emissions, depending on the approach taken, whereas operating room energy use constituted only 6%–16%. Based in a city where natural gas and nuclear energy are the main in-state sources of electricity, Thiel et al.’s (2015) study suggests that energy-related impacts may be relatively less important when anesthetic gases are also considered. Production of equipment and consumables was found to contribute 7%–65% () to total life cycle GHG emissions and was the main emissions hot spot among more technologically advanced procedures, including laparoscopic and robotic approaches to hysterectomy (60%–65%; Thiel et al. 2015). Transport of patients and staff, where considered alongside a broad range of life cycle activities, contributed minimally to the overall climate impact of surgical procedures (10%, ; Morris et al. 2013). Reprocessing of reusable equipment and materials contributed 0%–4% () of total procedure-related climate impact, except in Thiel et al.’s (2017) study of cataract surgery in India, where production and reprocessing of reusable surgical instruments constituted 61% of the total impact, with sterilization reported to compose the largest share of this. Disposal of waste materials and equipment contributed 0%–4% () to total per procedure GHG emissions, with the exception of Woods et al.’s (2015) study of different approaches to endometrial staging, where disposal was only one of two life cycle stages considered (the other being operating room energy use) and contributed 35%–40% of total GHG emissions. Excel Table S3 in the Supplemental Material contains the completed results pro forma, which details how life cycle stages were matched and provides the numerical data underlying Figure 2.
Equipment and Materials
Twenty-eight studies assessed environmental impact contributions from equipment used in surgical settings, including a) general surgical items, such as gowns (Carre 2008; Van den Berghe and Zimmer 2011; Vozzola et al. 2020), drapes (Vozzola et al. 2018), scrubs (Mikusinska 2012), scissors (Ibbotson et al. 2013), suction receptacles (Ison and Miller 2000), deep vein thrombosis (DVT) compression sleeves, pulse oximeters, LigaSure devices, harmonic scalpels, endoscopic trocars, arthroscopic shavers, scissor tips (Unger and Landis 2016); b) anesthetic equipment, such as anesthetic drug trays (McGain et al. 2010), laryngeal mask airways (LMA; Eckelman et al. 2012; Liang 2019), laryngoscope blades and handles (Sherman et al. 2018), central venous catheter insertion kits (McGain et al. 2012), and anesthetic equipment at two hospitals (McGain et al. 2017); c) items specific to particular procedures or specialties, such as titanium alloy knee implants (Lyons et al. 2021), custom packs used to deliver newborns (Campion et al. 2015), ureteroscopes (Davis et al. 2018), spinal fusion instrument sets (Leiden et al. 2020), and single-use medical devices and products used during hysterectomy (Unger et al. 2017); and d) items used in, but not specific to, surgery, such as personal protective equipment (masks, gloves, aprons, gowns, and face shields; Rizan et al. 2021), surgical face masks (Allison et al. 2020; Lee et al. 2021; Schmutz et al. 2020), medical gloves (Weisz et al. 2020), urinary catheters (Stripple et al. 2008), sharps containers (Grimmond and Reiner 2012; McPherson et al. 2019), and vaginal specula (Donahue et al. 2020).
In addition to issues arising from methodological decision-making, the comparison of LCA results between functionally equivalent items of surgical and anesthetic equipment is further complicated by the fact that many items are available in both single-use and reusable forms, meaning that their apparent impact contributions are highly dependent on the chosen functional unit used to express results. Seven studies selected “one use” as the functional unit and apportioned supply chain– (i.e., raw material extraction, production, packaging, transportation) and end-of-life–related impacts of reusable items over their expected lifetime number of uses. In contrast, eight other studies aligned their functional unit with the lifespan of the reusable item (e.g., maintenance of 40 airways using either 1 reusable LMA or 40 single-use LMAs in Eckelman et al. 2012). Other functional units employed included: per item (disposable custom packs, Campion et al. 2015; knee implants, Lyons et al. 2021), per kilogram (medical gloves, Weisz et al. 2020), per procedure (Unger et al. 2017), per kilogram of collected bodily fluid (suction receptacles, Ison and Miller 2000), use over a designated period (surgical masks, Allison et al. 2020; Schmutz et al. 2020; urinary catheters, Stripple et al. 2008), and service provision over a designated period (anesthetic equipment, McGain et al. 2017; personal protective equipment, Rizan et al. 2021; and reprocessed medical devices, Unger and Landis 2016) or to support a designated number of hospital beds or patient days of care (sharps containers, Grimmond and Reiner 2012; McPherson et al. 2019). Study system boundaries were set as cradle-to-grave in all studies, except in Weisz et al. (2020), where a cradle-to-manufacturer-gate analysis was undertaken.
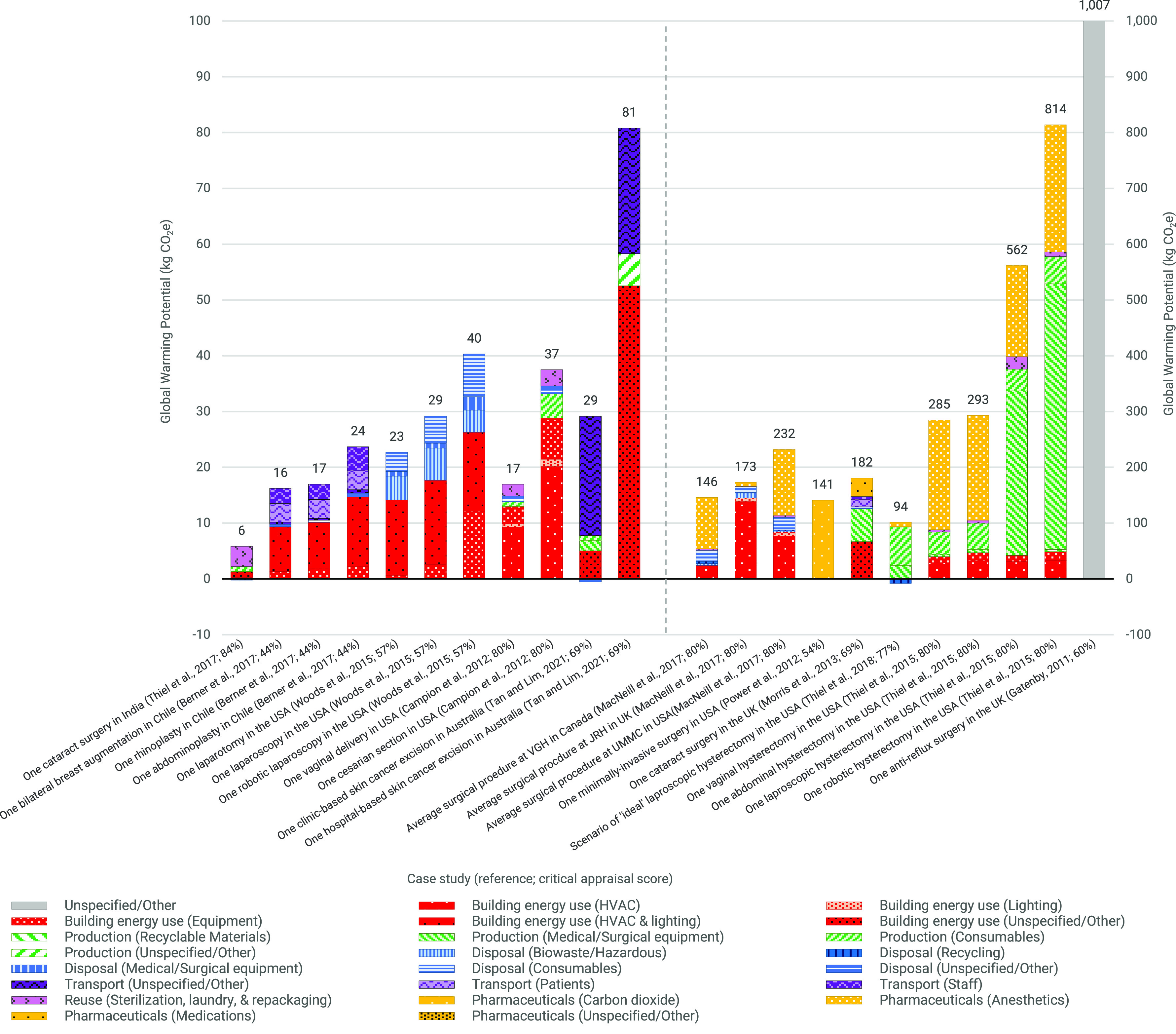
Most equipment-related studies (79%, ) compared life cycle contributions to environmental impacts of concern arising from single-use items with functionally equivalent reusable items. Figure 3 compares the relative climate impacts of reusable and disposable items with results reported relative to the most impactful case study within each reference. Reusable items were generally found to be more climate-friendly than their disposable equivalents, with only two studies concluding the opposite: Reusable central venous catheter insertion kits with coal-based energy used for reprocessing (McGain et al. 2012) and lumbar fusion instrument sets (Leiden et al. 2020) were found to be three (3.0) and nearly seven (6.7) times more climate polluting than their single-use equivalents, respectively (note that Leiden et al.’s 2020 study was funded by the manufacturer of the single-use set). One study comparing single-use and reusable face masks found that associated GHG emissions were similar between both types of mask (Schmutz et al. 2020), although the estimated lifespan of the reusable mask in this analysis was considerably shorter (5 washes) than in other similar studies (30–183 washes; Allison et al. 2020; Lee et al. 2021). Two further studies based in Melbourne, Australia, where electricity (the main energy source used in sterilization and reprocessing) is primarily sourced from coal, also concluded that disposable and reusable items have comparable climate impacts (flexible ureteroscopes, Davis et al. 2018; anesthetic equipment, McGain et al. 2017). In a sensitivity analysis designed to assess the effect of different primary energy carriers used to generate electricity on the climate impact of reusable anesthetic equipment, McGain et al. (2017) found that reprocessing equipment using renewable-based electricity (modeled on the UK/European mix) or natural gas–based electricity (modeled on the U.S. mix), as opposed to coal, could reduce the climate impact of reusable anesthetic equipment by 86% and 52%, respectively, thus highlighting the importance of energy sources when reusable products are used. Furthermore, one study found that relative impacts depended on the institutional context: Reusable suction receptacles at John Radcliffe Hospital (UK) had only 3% of the climate impact in comparison with that of disposable receptacles but were more than twice (2.7 times) as impactful as their disposable equivalents at Horton General NHS Trust (UK; Ison and Miller 2000). This variability was reportedly due to institutional differences in how reusable receptacles are reprocessed, namely the type of washing and drying machine used (e.g., combined vs. separate machines), their respective cycle lengths, and the associated energy requirements. Figure 3 also depicts the relative contributions of the various life cycle stages to overall climate impact and reveals that production processes and reuse processes are the main hot spots among disposable items (88%, median; 38%–97%, range) reusable items (68%, median; 0%–98%, range), respectively.
Figure 3.
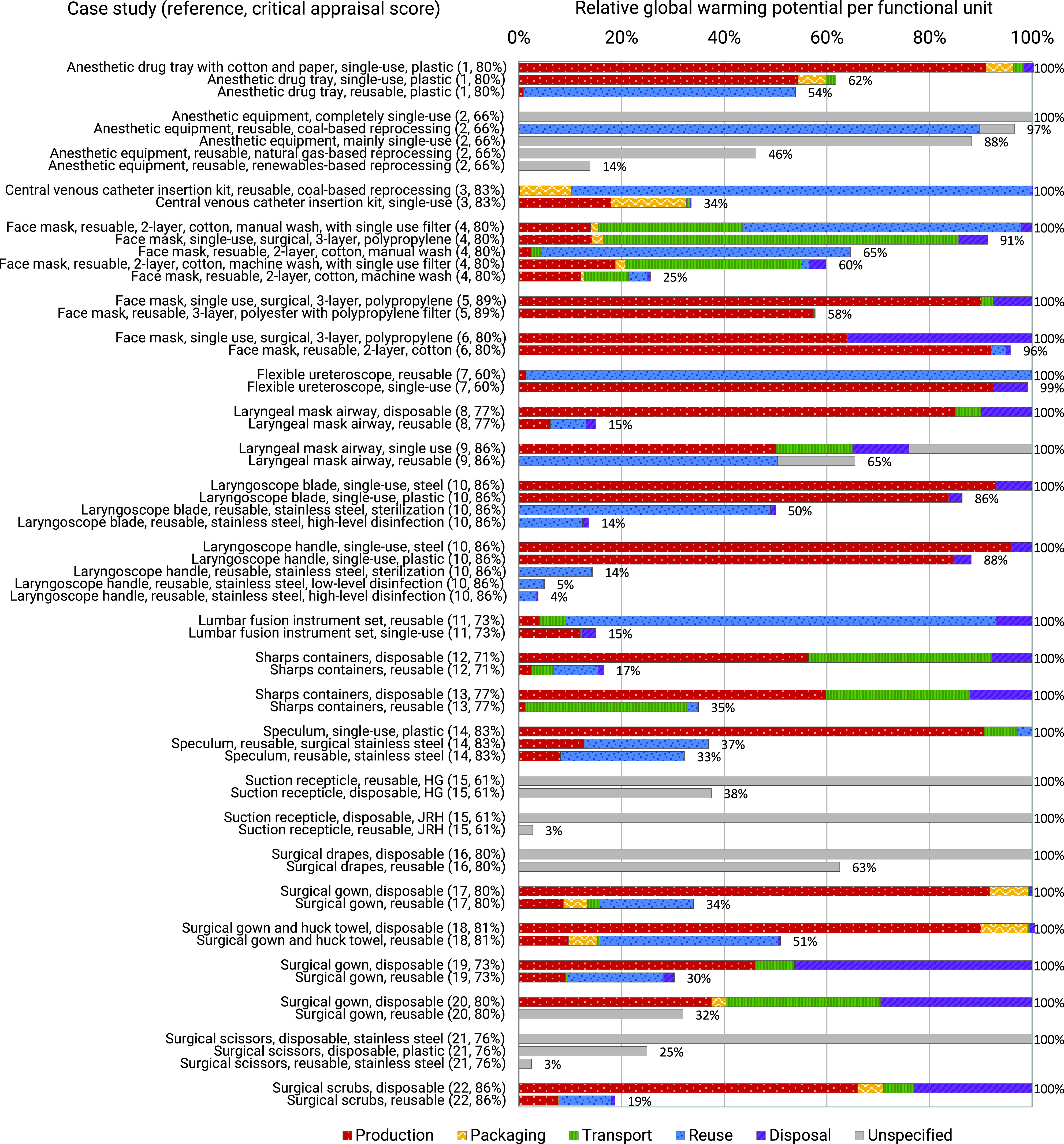
Comparing life cycle greenhouse gas emissions of single-use and functionally equivalent reusable equipment used in surgical settings with results reported relative to the most impactful case study within each reference and disaggregated by life cycle stage. Note: Underlying data sources vary in terms of the breadth of life cycle stages assessed (refer to Table 2 for details regarding which stages were considered within each reference). Critical appraisal scores provide an indication of study quality. Each included reference was appraised using a predetermined point-based scoring system based on existing guidelines for critical review of life cycle assessment studies. Assigned points were tallied and a percentage score was calculated to summarize results (see Excel Table S1 for further details). Numerical data underlying Figure 3 are available in Excel Table S4. “Production” includes raw material acquisition due to difficulty disaggregating these stages among included studies. For select studies, relative global warming potentials and life cycle stage contributions were estimated from figures (see Excel Table S4 for details). HG, Horton General NHS Trust, United Kingdom; JRH, John Radcliffe Hospital, United Kingdom. References: (1) McGain et al. 2010; (2) McGain et al. 2017; (3) McGain et al. 2012; (4) Allison et al. 2020; (5) Lee et al. 2021; (6) Schmutz et al. 2020; (7) Davis et al. 2018; (8) Liang 2019; (9) Eckelman et al. 2012; (10) Sherman et al. 2018; (11) Leiden et al. 2020; (12) Grimmond and Reiner 2012; (13) McPherson et al. 2019; (14) Donahue et al. 2020; (15) Ison and Miller 2000; (16) Vozzola et al. 2018; (17) Vozzola et al. 2020; (18) Carre 2008; (19) Van den Berghe and Zimmer 2011; (20) Rizan et al. 2021; (21) Ibbotson et al. 2013; (22) Mikusinska 2012.
In addition to global warming potential, most equipment-related studies (82%, ) also assessed life cycle impact contributions to at least one other resource depletion category (e.g., water use) or environmental concern (e.g., acidification potential). Figure 4 presents results from the seven most frequently assessed impact categories, with each data point representing an individual study’s estimate of the contributions arising from the provision and use of single-use equipment relative to equivalent reusable equipment. Although Figure 4 should be interpreted with caution due to the high degree of heterogeneity, both in terms of items studied and differences in methodological design, the available data suggest that single-use equipment used in surgical settings tends to result in higher contributions to a broad range of environmental concerns in comparison with functionally equivalent reusable items. A limited number of studies concluded the opposite: Acidification potential (lumbar fusion instrument sets, Leiden et al. 2020), ozone depletion potential (surgical drapes, Vozzola et al. 2018; surgical gowns, Van den Berghe and Zimmer 2011), water use (central venous catheter insertion kits, McGain et al. 2012; anesthetic equipment, McGain et al. 2017; face masks, Lee et al. 2021; Schmutz et al. 2020), and global warming potential (discussed earlier).
Figure 4.
Life cycle contributions to 7 impact categories arising from the provision and use of single-use equipment used in surgical settings relative to functionally equivalent reusable equipment with results from 22 studies covering a range of different items. Note: Each data point represents an individual study’s estimate of the impact of using an item of disposable surgical equipment relative to a functionally equivalent reusable item (multiplier). Environmental impact categories represent equivalent impact. Each box represents the interquartile range. The thick horizontal line within each box represents the median estimate; whiskers (vertical lines) represent the range of estimates. Horizontal deviation of data points along each whisker prevents them from overlapping and being obscured (i.e., it does not represent a hidden variable). Numerical data underlying Figure 4 are available in Excel Table S5.
Anesthetic Drugs and Related Pharmaceuticals
Five studies assessed life cycle contributions arising from the provision and use of pharmaceuticals used in surgical settings. Sherman et al. (2012) and Hu et al. (2021) assessed climate impacts of four general anesthetic agents using maintenance of minimum alveolar concentration for one hour (1 MAC-h), or MAC-equivalent (MAC-e) for propofol, as the functional unit to compare systems. Both studies concluded that life cycle GHG emissions contributions from the intravenous agent propofol were considerably lower () than commonly used inhalational agents (i.e., desflurane, isoflurane, and sevoflurane), whose impacts were found to vary according to synthesis method, carrier gas admixture, and flow rate utilization. For example, when the carrier gas admixture included nitrous oxide (60% :40% ), the life cycle GHG emissions associated with the provision and use of isoflurane and desflurane ranged 19–24 and , respectively (assuming a flow rate of ), whereas sevoflurane’s impact ranged with a flow rate of and between 38 and with a flow rate of (the regulated minimum gas flow rate for sevoflurane in the United States; Hu et al. 2021; Sherman et al. 2012). Conversely, when nitrous oxide was excluded from the carrier gas admixture, the per MAC-h climate impact associated with each of the inhaled agents ranged from 3 to 4, 3 to 11, 6 to 23, and for isoflurane (), sevoflurane (), sevoflurane (), and desflurane (), respectively (Hu et al. 2021).
McAlister et al. (2016) estimated that the cradle-to-manufacturer-gate climate impact of a standard morphine infusion bag ( of morphine sulfate in a standard sterile infusion bag (0.9% saline) was . Parvatker et al. (2019) quantified, per gram of active pharmaceutical ingredient (API), the cradle-to-manufacturer-gate climate impacts of 20 commonly used injectable anesthetic drugs using a combination of stoichiometric and laboratory-to-industry scale-up calculations based on data available in patents, industry literature, and existing inventory databases. Emissions estimates covering local anesthetics (lidocaine, ropivacaine hydrochloride, bupivacaine hydrochloride), analgesics (morphine, fentanyl, remifentanil, hydromorphone), sedatives (midazolam, ketamine, dexmedetomidine), sympathomimetics (epinephrine, phenylephrine hydrochloride, ephedrine hydrochloride), anticholinergics (glycopyrrolate), antiemetics (ondansetron), and muscle relaxants and reversal agents (succinylcholine, rocuronium bromide, neostigmine methylsulfate, sugammedex), ranged between 0.01 and (Parvatker et al. 2019). Tauber et al. (2019) assessed the life cycle environmental impact contributions arising from unused pharmaceuticals (including eyedrops, injections, and systemics) per single phacoemulsification cataract removal procedure at four facilities using an EIO-LCA study design, and found that 21%–66% of pharmaceuticals (by volume) were wasted with associated impacts ranging between 6.3 and .
Discussion
Main Findings
Based on three case study hospitals in Canada, the United States, and the United Kingdom, life cycle GHG emissions contributions from the annual operation of surgical suites were found to range from 3,200,000 to (MacNeill et al. 2017). If these case studies were representative of all surgical suites in Canada, the United States, and the United Kingdom, the combined climate impact of operating rooms in these countries would be equivalent to the annual carbon footprint of 2 million passenger vehicles (; MacNeill et al. 2017). When compared on a caseload basis, the per-procedure climate impact of operating these surgical suites varied between 146 and , which is within the range of estimates reported among procedure-specific studies (; Figure 2). To further compare reported procedure- and surgical suite–based estimates, the annual climate impact of surgical procedures in the United States, Canada, and the United Kingdom can be crudely approximated by multiplying the total number of surgical procedures performed annually in these countries ( in 2012; Weiser et al. 2016) by the average per-procedure climate impact identified in this review (). This yields an estimate of , which aligns closely with MacNeill et al.’s (2017) operating room–based estimate of .
The degree to which the variability in climate impact between identified per-procedure studies () is due to differences in methodological design between studies (e.g., process-based vs. input–output method); differences in complexity, duration, and material demand between individual surgical procedures or approaches; and differences in geographical and institutional setting, is difficult to determine. Technologically advanced surgical procedures and approaches appear to be considerably more environmentally polluting than traditional approaches; according to Thiel et al. (2015), robotic laparoscopic hysterectomy was nearly three times more climate-intensive than abdominal (2.8 times) or vaginal hysterectomy (2.9 times). Moreover, Woods et al. (2015) found that robotic laparoscopy was 1.4 times and 1.8 times more climate-polluting than laparoscopy and laparotomy for endometrial staging, respectively. Only one study assessed the impact of geographical setting on procedure-related environmental burdens, finding cataract surgery in India to be 95% less impactful on the climate in comparison with such surgeries in the UK (Thiel et al. 2017).
Climate-related hot spots among surgical procedures depended in part on the comprehensiveness of the analysis: More inclusive studies concluded that primary hot spots were provision and use of anesthetic gases, HVAC-related energy use, and the production of single-use equipment (Campion et al. 2012; Morris et al. 2013; Thiel et al. 2015). Regarding equipment used in surgical settings, single-use items were found with few exceptions to be more impactful across a range of environmental parameters, including climate change, acidification potential, eutrophication potential, ozone depletion potential, photochemical oxidant creation potential, and water use, than functionally equivalent reusable items (Figure 4). Repeated manufacture constitutes the primary emissions hot spot for single-use equipment, whereas repeated reprocessing defines the impact burden of reusable items. Life cycle inventories have been assembled and associated climate impacts calculated for three anesthetic gases (desflurane, isoflurane, sevoflurane; ; Hu et al. 2021; Sherman et al. 2012) and 20 injectable anesthetic drugs, including general anesthetics (i.e., propofol), local anesthetics, analgesics, sedatives, sympathomimetics, anticholinergics, antiemetics, and muscle relaxants and reversal agents (; (McAlister et al. 2016; Parvatker et al. 2019).
Potential Interventions
Thiel et al. (2018), in an analysis of various interventions to reduce the climate impact of laparoscopic hysterectomy, found that anesthetic gas- and operating room energy-related emissions could be drastically reduced or eliminated via exclusive use of propofol or sevoflurane (without nitrous oxide) and energy mix decarbonization. These findings are consistent with MacNeill et al. (2017), who estimated that avoidance of desflurane in surgical suites could reduce anesthetic-related GHG emissions by as much as 90%. It should be noted that the substantial GHG mitigation potential of anesthetic gas substitution was originally described in Sherman et al. (2012) and that this early analysis underpins related estimates by both Thiel et al. (2018) and MacNeill et al. (2017). Research also suggests that operating room interventions targeting surgical equipment use may also yield substantial emissions savings: According to Thiel et al. (2018) using fewer surgical instruments and reprocessing single-use devices where possible could reduce the impact of laparoscopic hysterectomy by more than half (up to 55%).
Together, these findings indicate which mitigation strategies are likely to be effective at lowering the climate impact of surgical procedures and operating rooms, although the scale of any potential improvement will inevitably vary with context. Because surgical and anesthetic care are among the most resource-intensive components of the health system, we argue that every effort needs to be taken to lower the climate burden of these medical specialties if carbon neutrality is to be achieved by 2050 or earlier. Minor incremental improvements in the system, however, are likely to be counteracted by the projected increase in demand for surgical services associated with population growth, aging demographics, the growing burden of chronic disease, the apparent rise of unnecessary procedures, and worsening impacts of planetary disruption on human health (Brownlee et al. 2017; Cimprich et al. 2019; Lenzen et al. 2020; Malik et al. 2018). With more than half the global population () currently unable to access safe and affordable surgical care (Meara et al. 2015), service provision will also require dramatic scale-up if universal health coverage is to be achieved as outlined in the Sustainable Development Goals (United Nations General Assembly 2015). The role of public health and preventive medicine in reducing demand for surgical services in the first place should not be underestimated (MacNeill et al. 2021; Malik et al. 2018).
Limitations
The main limitation of this review is the relatively small number of studies identified, as well as the substantial methodological heterogeneity among extant studies, which ruled out any possibility of meta-analysis. The deployment of LCA methods in surgery and anesthesiology is still in its infancy, and current challenges in the field are carried through into this review. Most notably, there is a clear lack of peer-reviewed, accessible health care–specific life cycle inventory data that includes the material and energy flows for items and pharmaceuticals commonly used in surgical settings (Thiel et al. 2017, 2020). Consequently, researchers attempting to include the impacts of producing equipment and consumables in their analyses, for example, are required to estimate the material composition of each item, match each material to the most appropriate unit process in an inventory database, and make assumptions about production processes. Inventory compilation and subsequent impact assessment of individual items or pharmaceuticals, therefore, have great utility for improving the accuracy and completeness of higher-level analyses (Sherman et al. 2020).
Another challenge in the field is the selection and standardization of meaningful reference flows and functional units to allow effective comparison between treatment options. For instance, the various injectable anesthetic drugs assessed by Parvatker et al. (2019) on a per gram of active pharmaceutical ingredient (API) basis all have different clinical utilities and potencies. A mass-based functional unit, therefore, has little relevance to the actual function of such pharmaceutical agents. Future comparative analyses should strive to also report results in terms of a clinically equivalent metric (Parvatker et al. 2019), such as Sherman et al.’s (2012) assessment of anesthetic agents, which selected maintenance of minimum alveolar concentration for one hour as its functional unit.
Furthermore, the current evidence base lacks geographic and institutional diversity. Only two eligible studies assessed the environmental impacts in non-Organization for Economic Cooperation and Development (OECD) settings, with results suggesting that substantial differences may exist between health systems (Campion et al. 2015; Thiel et al. 2017). As a result, the generalizability of this review’s conclusions is likely to be limited.
Together, these limitations make it difficult to confidently compare the environmental impacts of different aspects of surgical and anesthesiology-related care. Any conclusions drawn should be interpreted with caution and reevaluated as new evidence becomes available.
Implications
Relatively few systematic reviews of health care-related environmental impacts have been undertaken (Alshqaqeeq et al. 2020; Brown et al. 2012; McGain and Naylor 2014). To the best of our knowledge, this review is the first to assess and critically evaluate the application of LCA across surgical and anesthetic services as a whole, including consideration of operating rooms, procedures, equipment, and related pharmaceuticals. We expand on Rizan et al.’s (2020) review, which was exclusive to surgical procedures (), to include an additional 36 studies from across both the peer-reviewed and gray literatures. We also broaden our analysis beyond global warming potential to include consideration of other environmental impact categories where possible. Furthermore, we are not aware of another analysis that has quantitatively synthesized equipment-related life cycle impact estimates (Figure 4). For the first time, the relative environmental effects of single-use and reusable equipment used in surgical settings can readily be compared. Our findings provide evidence in support of calls to reverse the three-decades-long trend toward reliance on single-use medical devices and transition to a more circular, reusable-based health care economy that prioritizes patient safety, affordability, supply chain resilience, and environmental sustainability (MacNeill et al. 2020).
In summarizing the state of LCA practice in surgical and anesthetic services, this review offers an indication of the spectrum of environmental impact contributions associated with surgery and anesthesiology at various scales. The results of this review are likely to be relevant to a broad range of stakeholders and may be used to: a) assist LCA practitioners in identifying existing inventory data and designing future assessments in this field; b) guide evidence-based decision-making that maximizes co-benefits and minimizes co-harms (e.g., to shift institutional preference toward less climate-polluting anesthetic agents, to decarbonize operating room energy provision, and to prioritize purchasing of reusable equipment and materials); c) inform regulators and policymakers about the role of LCA in the planning, implementation, and evaluation of pollution-related mitigative measures and advance efforts to make environmental impact reporting mandatory for all medical device and pharmaceutical suppliers; and d) educate surgical and anesthesia staff about the impacts of their practices and support a shift in organizational culture.
Future Research
This review highlights the recent proliferation of surgery- and anesthesiology-related LCAs, with more than half of the included studies having been published since 2017. Nevertheless, only a handful of the thousands of procedures, products, and pharmaceuticals that exist have been studied (Weisz et al. 2020). More LCAs are urgently needed to not only fill in the gaps, but to better elucidate the drivers of variation found to exist among available studies. Comparative assessments across different health care settings, particularly among low- and middle-income countries, should be a key priority for future LCA work in this field.
Assessments with wider system boundaries are also needed to better understand the true impacts of specific procedures and approaches: Accounting for downstream care pathways (e.g., post-anesthesia care and inpatient recovery) may, for example, reduce the relative impacts of minimally invasive approaches that shorten recovery time and lessen complication risk (Thiel et al. 2015). Furthermore, there is a need for further studies that compare the relative impacts of surgical and medical management for chronic conditions, such as that conducted by Gatenby (2011), which modeled the relative climate and financial impacts of managing gastroesophageal reflux disease with one-off fundoplication surgery vs. ongoing medical management.
Although sustainability interventions that are designed to mitigate the impacts of climate change (e.g., replacing single-use surgical equipment and consumables with reusable versions) tend also to reduce impacts on other environmental parameters (see Figure 4), trade-offs are inevitable. Incorporating a broader range of environmental impact categories within assessments, particularly among those focused on operating rooms and procedures, should be prioritized.
Progressive accumulation of surgical and anesthesiology-related life cycle assessments will allow researchers examining the health and environmental co-benefits of various policy measures (e.g., promotion of plant-based eating patterns and active transport) to incorporate the environmental advantage of avoided surgery within future modeling efforts. In turn, this information is likely to provide additional leverage for decision makers to institute bold policy on a scale that the climate crisis demands.
Conclusion
This state-of-the-science review details environmental impact contributions and emissions hot spots associated with surgical and anesthetic care provision at various scales. Although LCA research to date indicates that the environmental burden attributable to these services is substantial, it also suggests that effective mitigation strategies are readily available. Nonetheless, the decarbonization of surgical and anesthetic care is a monumental task whose success depends on the rapid operationalization of LCA across a wide range of related products and services. In summarizing the current state of LCA practice in surgery and anesthesiology, this review provides evidence in support of such a transition, along with impetus and direction for future assessments in the field.
Supplementary Material
Acknowledgments
J.D., J.S.F., and S.D.C. were involved in independently screening abstracts and analyzing full-text articles. J.D. analyzed the data, created the figures, and wrote the manuscript. S.D.C., D.R., and P.T. assisted with review design and manuscript preparation.
We would like to acknowledge Dalhousie University’s Healthy Populations Institute for project coordination; Robin Parker at Dalhousie University’s W. K. Kellogg Health Sciences Library for input on the literature search strategy; and Anna Graham-DeMello (Dalhousie University) for her assistance with manuscript editing and preparation.
References
- Allison AL, Ambrose-Dempster E, Domenech Aparsi T, Bawn M, Casas Arredondo M, Chau C, et al. 2020. The environmental dangers of employing single-use face masks as part of a COVID-19 exit strategy. UCL Open: Environment Preprint. 10.14324/111.444/000031.v1, [accessed 25 July 2020]. [DOI] [Google Scholar]
- Alshqaqeeq F, Esmaeili MA, Overcash M, Twomey J. 2020. Quantifying hospital services by carbon footprint: a systematic literature review of patient care alternatives. Resour Conserv Recycl 154:104560, 10.1016/j.resconrec.2019.104560. [DOI] [Google Scholar]
- Andersen MPS, Nielsen OJ, Wallington TJ, Karpichev B, Sander SP. 2012. Assessing the impact on global climate from general anesthetic gases. Anesth Analg 114(5):1081–1085, PMID: 22492189, 10.1213/ANE.0b013e31824d6150. [DOI] [PubMed] [Google Scholar]
- Berner JE, Gras MDP, Troisi L, Chapman T, Vidal P. 2017. Measuring the carbon footprint of plastic surgery: a preliminary experience in a Chilean teaching hospital. J Plast Reconstr Aesthet Surg 70(12):1777–1779, PMID: 28655513, 10.1016/j.bjps.2017.06.008. [DOI] [PubMed] [Google Scholar]
- Bologna M, Aquino G. 2020. Deforestation and world population sustainability: a quantitative analysis. Sci Rep 10(1):1–9, PMID: 31913322, 10.1038/s41598-020-63657-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown LH, Buettner PG, Canyon DV. 2012. The energy burden and environmental impact of health services. Am J Public Health 102(12):e76–e82, PMID: 23078475, 10.2105/AJPH.2012.300776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brownlee S, Chalkidou K, Doust J, Elshaug AG, Glasziou P, Heath I, et al. 2017. Evidence for overuse of medical services around the world. Lancet 390(10090):156–168, PMID: 28077234, 10.1016/S0140-6736(16)32585-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campion N, Thiel CL, DeBlois J, Woods NC, Landis AE, Bilec MM. 2012. Life cycle assessment perspectives on delivering an infant in the US. Sci Total Environ 425:191–198, PMID: 22482785, 10.1016/j.scitotenv.2012.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campion N, Thiel CL, Woods NC, Swanzy L, Landis AE, Bilec MM. 2015. Sustainable healthcare and environmental life-cycle impacts of disposable supplies: a focus on disposable custom packs. J Cleaner Production 94:46–55, 10.1016/j.jclepro.2015.01.076. [DOI] [Google Scholar]
- Carleton TA, Jina A, Delgado MT, Greenstone M, Houser T, Hsiang SM, et al. 2020. Valuing the Global Mortality Consequences of Climate Change Accounting for Adaptation Costs and Benefits (Working Paper 27599). Cambridge, MA: National Bureau of Economic Research, p. 57 https://www.nber.org/papers/w27599.pdf, [accessed 12 August 2020]. [Google Scholar]
- Carre A. 2008. Life Cycle Assessment Comparing Laundered Surgical Gowns with Polypropylene Based Disposable Gowns. Melbourne, Australia: RMIT University, p. 84. https://www.lac-mac.com/mediafiles/catalogue/RMIT_LifeCycleAssessmentDisposableVsReusableGowns.pdf, [accessed 25 July 2020]. [Google Scholar]
- Cimprich A, Santillán‐Saldivar J, Thiel CL, Sonnemann G, Young SB. 2019. Potential for industrial ecology to support healthcare sustainability: scoping review of a fragmented literature and conceptual framework for future research. J Ind Ecol 23(6):1344–1352, 10.1111/jiec.12921. [DOI] [Google Scholar]
- Costa D, Quinteiro P, Dias AC. 2019. A systematic review of life cycle sustainability assessment: current state, methodological challenges, and implementation issues. Sci Total Environ 686:774–787, PMID: 31195285, 10.1016/j.scitotenv.2019.05.435. [DOI] [PubMed] [Google Scholar]
- Costello A, Abbas M, Allen A, Ball S, Bell S, Bellamy R, et al. 2009. Managing the health effects of climate change: Lancet and University College London Institute for Global Health Commission. Lancet 373(9676):1693–1733, PMID: 19447250, 10.1016/S0140-6736(09)60935-1. [DOI] [PubMed] [Google Scholar]
- Davis NF, McGrath S, Quinlan M, Jack G, Lawrentschuk N, Bolton DM. 2018. Carbon footprint in flexible ureteroscopy: a comparative study on the environmental impact of reusable and single-use ureteroscopes. J Endourol 32(3):214–217, PMID: 29373918, 10.1089/end.2018.0001. [DOI] [PubMed] [Google Scholar]
- Donahue LM, Hilton S, Bell SG, Williams BC, Keoleian GA. 2020. A comparative carbon footprint analysis of disposable and reusable vaginal specula. Am J Obstet Gynecol 223(2):225.e1–225.e7, PMID: 32067971, 10.1016/j.ajog.2020.02.007. [DOI] [PubMed] [Google Scholar]
- Drew J. 2020. Operating in a Climate Crisis: A Systematic Review Protocol of Lifecycle Assessment within Surgical Services. Open Science Framework, 10.17605/OSF.IO/HDTXS, [accessed 30 July 2020]. [DOI]
- Eckelman MJ, Huang K, Lagasse R, Senay E, Dubrow R, Sherman JD. 2020. Health care pollution and public health damage in the United States: an update. Health Aff (Millwood) 39(12):2071–2079, PMID: 33284703, 10.1377/hlthaff.2020.01247. [DOI] [PubMed] [Google Scholar]
- Eckelman M, Mosher M, Gonzalez A, Sherman J. 2012. Comparative life cycle assessment of disposable and reusable laryngeal mask airways. Anesth Analg 114(5):1067–1072, PMID: 22492190, 10.1213/ANE.0b013e31824f6959. [DOI] [PubMed] [Google Scholar]
- Eckelman MJ, Sherman JD. 2018. Estimated global disease burden from US health care sector greenhouse gas emissions. Am J Public Health 108(S2):S120–S122, PMID: 29072942, 10.2105/AJPH.2017.303846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eckelman MJ, Sherman JD, MacNeill AJ. 2018. Life cycle environmental emissions and health damages from the Canadian healthcare system: an economic-environmental-epidemiological analysis. PLoS Med 15(7):e1002623, PMID: 30063712, 10.1371/journal.pmed.1002623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finkbeiner M, Inaba A, Tan R, Christiansen K, Klüppel H-J. 2006. The new international standards for life cycle assessment: ISO 14040 and ISO 14044. Int J Life Cycle Assess 11(2):80–85, 10.1065/lca2006.02.002. [DOI] [Google Scholar]
- Friedlingstein P, Jones MW, O’Sullivan M, Andrew RM, Hauck J, Peters GP, et al. 2019. Global carbon budget 2019. Earth Syst Sci Data 11(4):1783–1838, 10.5194/essd-11-1783-2019. [DOI] [Google Scholar]
- Gatenby PAC. 2011. Modelling the carbon footprint of reflux control. Int J Surg 9(1):72–74, PMID: 20932944, 10.1016/j.ijsu.2010.09.008. [DOI] [PubMed] [Google Scholar]
- Gibb R, Redding DW, Chin KQ, Donnelly CA, Blackburn TM, Newbold T, et al. 2020. Zoonotic host diversity increases in human-dominated ecosystems. Nature 584(7821):398–402, PMID: 32759999, 10.1038/s41586-020-2562-8. [DOI] [PubMed] [Google Scholar]
- Grimmond T, Reiner S. 2012. Impact on carbon footprint: a life cycle assessment of disposable versus reusable sharps containers in a large US hospital. Waste Manag Res 30(6):639–642, PMID: 22627643, 10.1177/0734242X12450602. [DOI] [PubMed] [Google Scholar]
- Haddaway N, Macura B, Whaley P, Pullin A. 2017. ROSES for Systematic Review Protocols Version 1.0. 10.6084/m9.figshare.5897269. [DOI] [Google Scholar]
- Haddaway NR, Macura B, Whaley P, Pullin AS. 2018. ROSES RepOrting standards for systematic evidence syntheses: pro forma, flow-diagram and descriptive summary of the plan and conduct of environmental systematic reviews and systematic maps. Environ Evid 7(1):7, 10.1186/s13750-018-0121-7. [DOI] [Google Scholar]
- Hellweg S, Milà i Canals L. 2014. Emerging approaches, challenges and opportunities in life cycle assessment. Science 344(6188):1109–1113, PMID: 24904154, 10.1126/science.1248361. [DOI] [PubMed] [Google Scholar]
- Hu X, Pierce JT, Taylor T, Morrissey K. 2021. The carbon footprint of general anaesthetics: a case study in the UK. Resour Conserv Recycl 167:105411, 10.1016/j.resconrec.2021.105411. [DOI] [Google Scholar]
- Ibbotson S, Dettmer T, Kara S, Herrmann C. 2013. Eco-efficiency of disposable and reusable surgical instruments—a scissors case. Int J Life Cycle Assess 18(5):1137–1148, 10.1007/s11367-013-0547-7. [DOI] [Google Scholar]
- Ison E, Miller A. 2000. The use of LCA to introduce life-cycle thinking into decision-making for the purchase of medical devices in the NHS. J Env Assmt Pol Mgmt 02(04):453–476, 10.1142/S1464333200000497. [DOI] [Google Scholar]
- Karliner J, Slotterback S, Boyd R, Ashby B, Steele K. 2019. Health Care’s Climate Footprint: How the Health Sector Contributes to the Global Climate Crisis and Opportunities for Action. Brussels, Belgium: Health Care Without Harm, p. 48. https://noharm-global.org/sites/default/files/documents-files/5961/HealthCaresClimateFootprint_092319.pdf, [accessed 23 June 2020]. [Google Scholar]
- Lee AWL, Neo ERK, Khoo Z-Y, Yeo Z, Tan YS, Chng S, et al. 2021. Life cycle assessment of single-use surgical and embedded filtration layer (EFL) reusable face mask. Resour Conserv Recycl 170:105580, PMID: 33814723, 10.1016/j.resconrec.2021.105580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leiden A, Cerdas F, Noriega D, Beyerlein J, Herrmann C. 2020. Life cycle assessment of a disposable and a reusable surgery instrument set for spinal fusion surgeries. Resour Conserv Recycl 156:104704, 10.1016/j.resconrec.2020.104704. [DOI] [Google Scholar]
- Lenzen M, Malik A, Li M, Fry J, Weisz H, Pichler P-P, et al. 2020. The environmental footprint of health care: a global assessment. Lancet Planet Health 4(7):e271–e279, PMID: 32681898, 10.1016/S2542-5196(20)30121-2. [DOI] [PubMed] [Google Scholar]
- Liang G. 2019. Life cycle assessment of disposable and reusable laryngeal mask airway in Skånevård Sund (Lund University). http://lup.lub.lu.se/student-papers/record/8986326, [accessed 24 July 2020].
- Lyons R, Newell A, Ghadimi P, Papakostas N. 2021. Environmental impacts of conventional and additive manufacturing for the production of Ti-6Al-4V knee implant: a life cycle approach. Int J Adv Manuf Technol 112(3–4):787–801, 10.1007/s00170-020-06367-7. [DOI] [Google Scholar]
- MacNeill AJ, Hopf H, Khanuja A, Alizamir S, Bilec M, Eckelman MJ, et al. 2020. Transforming the medical device industry: road map to a circular economy. Health Aff (Millwood) 39(12):2088–2097, PMID: 33284689, 10.1377/hlthaff.2020.01118. [DOI] [PubMed] [Google Scholar]
- MacNeill AJ, Lillywhite R, Brown CJ. 2017. The impact of surgery on global climate: a carbon footprinting study of operating theatres in three health systems. Lancet Planet Health 1(9):e381–e388, PMID: 29851650, 10.1016/S2542-5196(17)30162-6. [DOI] [PubMed] [Google Scholar]
- MacNeill AJ, McGain F, Sherman JD. 2021. Planetary health care: a framework for sustainable health systems. Lancet Planet Health 5(2):e66–e68, PMID: 33581064, 10.1016/S2542-5196(21)00005-X. [DOI] [PubMed] [Google Scholar]
- Malik A, Lenzen M, McAlister S, McGain F. 2018. The carbon footprint of Australian health care. Lancet Planet Health 2(1):e27–e35, PMID: 29615206, 10.1016/S2542-5196(17)30180-8. [DOI] [PubMed] [Google Scholar]
- McAlister S, Ou Y, Neff E, Hapgood K, Story D, Mealey P, et al. 2016. The environmental footprint of morphine: a life cycle assessment from opium poppy farming to the packaged drug. BMJ Open 6(10):e013302, PMID: 27798031, 10.1136/bmjopen-2016-013302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGain F, McAlister S, McGavin A, Story D. 2010. The financial and environmental costs of reusable and single-use plastic anaesthetic drug trays. Anaesth Intensive Care 38(3):538–544, PMID: 20514965, 10.1177/0310057X1003800320. [DOI] [PubMed] [Google Scholar]
- McGain F, McAlister S, McGavin A, Story D. 2012. A life cycle assessment of reusable and single-use Central venous catheter insertion kits. Anesth Analg 114(5):1073–1080, PMID: 22492185, 10.1213/ANE.0b013e31824e9b69. [DOI] [PubMed] [Google Scholar]
- McGain F, Naylor C. 2014. Environmental sustainability in hospitals–a systematic review and research agenda. J Health Serv Res Policy 19(4):245–252, PMID: 24813186, 10.1177/1355819614534836. [DOI] [PubMed] [Google Scholar]
- McGain F, Story D, Lim T, McAlister S. 2017. Financial and environmental costs of reusable and single-use anaesthetic equipment. Br J Anaesth 118(6):862–869, PMID: 28505289, 10.1093/bja/aex098. [DOI] [PubMed] [Google Scholar]
- McPherson B, Sharip M, Grimmond T. 2019. The impact on life cycle carbon footprint of converting from disposable to reusable sharps containers in a large US hospital geographically distant from manufacturing and processing facilities. PeerJ 7:e6204, PMID: 30809428, 10.7717/peerj.6204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meara JG, Leather AJM, Hagander L, Alkire BC, Alonso N, Ameh EA, et al. 2015. Global surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet 386(9993):569–624, PMID: 25924834, 10.1016/S0140-6736(15)60160-X. [DOI] [PubMed] [Google Scholar]
- Mikusinska M. 2012. Comparative Life Cycle Assessment of Surgical Scrub Suits: the Case of Reusable and Disposable Scrubs used in Swedish Healthcare. Stockholm, Sweden: KTH Royal Institute of Technology. https://www.diva-portal.org/smash/get/diva2:574013/FULLTEXT01.pdf, [accessed 25 July 2020]. [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. 2009. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151(4):264–269, PMID: 19622511, 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- Morris DS, Wright T, Somner JE, Connor A. 2013. The carbon footprint of cataract surgery. Eye (Lond) 27(4):495–501, PMID: 23429413, 10.1038/eye.2013.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parvatker AG, Tunceroglu H, Sherman JD, Coish P, Anastas P, Zimmerman JB, et al. 2019. Cradle-to-gate greenhouse gas emissions for twenty anesthetic active pharmaceutical ingredients based on process scale-up and process design calculations. ACS Sustainable Chem Eng 7(7):6580–6591, 10.1021/acssuschemeng.8b05473. [DOI] [Google Scholar]
- Pichler P-P, Jaccard IS, Weisz U, Weisz H. 2019. International comparison of health care carbon footprints. Environ Res Lett 14(6):064004, 10.1088/1748-9326/ab19e1. [DOI] [Google Scholar]
- Power NE, Silberstein JL, Ghoneim TP, Guillonneau B, Touijer KA. 2012. Environmental impact of minimally invasive surgery in the United States: an estimate of the carbon dioxide footprint. J Endourol 26(12):1639–1644, PMID: 22845049, 10.1089/end.2012.0298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rizan C, Reed M, Bhutta MF. 2021. Environmental impact of personal protective equipment distributed for use by health and social care services in England in the first six months of the COVID-19 pandemic. J R Soc Med 114(5):250–263, PMID: 33726611, 10.1177/01410768211001583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rizan C, Steinbach I, Nicholson R, Lillywhite R, Reed M, Bhutta MF. 2020. The carbon footprint of surgical operations: a systematic review. Ann Surg 272(6):986–995, PMID: 32516230, 10.1097/SLA.0000000000003951. [DOI] [PubMed] [Google Scholar]
- Schmutz M, Hischier R, Batt T, Wick P, Nowack B, Wäger P, et al. 2020. Cotton and surgical masks—what ecological factors are relevant for their sustainability? Sustainability 12(24):10245, 10.3390/su122410245. [DOI] [Google Scholar]
- Selvy M, Bellin M, Slim K, Muret J. 2020. Eco-responsibility in the operating theater: an urgent need for organizational transformation. J Visc Surg 157(4):301–307, PMID: 32747304, 10.1016/j.jviscsurg.2020.07.001. [DOI] [PubMed] [Google Scholar]
- Sherman J, Le C, Lamers V, Eckelman M. 2012. Life cycle greenhouse gas emissions of anesthetic drugs. Anesth Analg 114(5):1086–1090, PMID: 22492186, 10.1213/ANE.0b013e31824f6940. [DOI] [PubMed] [Google Scholar]
- Sherman J, Raibley LA, Eckelman MJ. 2018. Life cycle assessment and costing methods for device procurement: comparing reusable and single-use disposable laryngoscopes. Anesth Analg 127(2):434–443, PMID: 29324492, 10.1213/ANE.0000000000002683. [DOI] [PubMed] [Google Scholar]
- Sherman JD, Thiel C, MacNeill A, Eckelman MJ, Dubrow R, Hopf H, et al. 2020. The green print: advancement of environmental sustainability in healthcare. Resour Conserv Recycl 161:104882, 10.1016/j.resconrec.2020.104882. [DOI] [Google Scholar]
- Steffen W, Richardson K, Rockström J, Cornell SE, Fetzer I, Bennett EM, et al. 2015. Planetary boundaries: guiding human development on a changing planet. Science 347(6223):1259855, PMID: 25592418, 10.1126/science.1259855. [DOI] [PubMed] [Google Scholar]
- Stripple H, Westman R, Holm D. 2008. Development and environmental improvements of plastics for hydrophilic catheters in medical care: an environmental evaluation. J Clean Prod 16(16):1764–1776, 10.1016/j.jclepro.2007.12.006. [DOI] [Google Scholar]
- Tan E, Lim D. 2021. Carbon footprint of dermatologic surgery. Australas J Dermatol 62(2):, 10.1111/ajd.13522. [DOI] [PubMed] [Google Scholar]
- Tauber J, Chinwuba I, Kleyn D, Rothschild M, Kahn J, Thiel CL. 2019. Quantification of the cost and potential environmental effects of unused pharmaceutical products in cataract surgery. JAMA Ophthalmol 137(10):1156–1163, PMID: 31369052, 10.1001/jamaophthalmol.2019.2901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thiel CL, Cassels-Brown A, Goel H, Stancliffe R, Steinbach I, Thomas P, et al. 2020. Utilizing off-the-shelf LCA methods to develop a ‘triple bottom line’ auditing tool for global cataract surgical services. Resour Conserv Recycl 158:104805, 10.1016/j.resconrec.2020.104805. [DOI] [Google Scholar]
- Thiel CL, Eckelman M, Guido R, Huddleston M, Landis AE, Sherman J, et al. 2015. Environmental impacts of surgical procedures: life cycle assessment of hysterectomy in the United States. Environ Sci Technol 49(3):1779–1786, PMID: 25517602, 10.1021/es504719g. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thiel CL, Schehlein E, Ravilla T, Ravindran RD, Robin AL, Saeedi OJ, et al. 2017. Cataract surgery and environmental sustainability: waste and lifecycle assessment of phacoemulsification at a private healthcare facility. J Cataract Refract Surg 43(11):1391–1398, PMID: 29223227, 10.1016/j.jcrs.2017.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thiel CL, Woods NC, Bilec MM. 2018. Strategies to reduce greenhouse gas emissions from laparoscopic surgery. Am J Public Health 108(S2):S158–S164, PMID: 29698098, 10.2105/AJPH.2018.304397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tollefson J. 2021. COVID curbed carbon emissions in 2020-but not by much. Nature 589(7842):343, PMID: 30356183, 10.1038/d41586-021-00090-3. [DOI] [PubMed] [Google Scholar]
- Unger SR, Hottle TA, Hobbs SR, Thiel CL, Campion N, Bilec MM, et al. 2017. Do single-use medical devices containing biopolymers reduce the environmental impacts of surgical procedures compared with their plastic equivalents? J Health Serv Res Policy 22(4):218–225, PMID: 28530129, 10.1177/1355819617705683. [DOI] [PubMed] [Google Scholar]
- Unger SR, Landis AE. 2016. Assessing the environmental, human health, and economic impacts of reprocessed medical devices in a phoenix hospital’s supply chain. J Clean Prod 112:1995–2003, 10.1016/j.jclepro.2015.07.144. [DOI] [Google Scholar]
- United Nations Environment Programme. 2019. Emissions Gap Report 2019. New York, NY: United Nations Environment Programme, p. 108. https://wedocs.unep.org/bitstream/handle/20.500.11822/30797/EGR2019.pdf, [accessed 4 August 2020]. [Google Scholar]
- United Nations General Assembly. 2015. Transforming Our World: The 2030 Agenda for Sustainable Development. New York, NY: Division for Sustainable Development Goals, United Nations, p. 35. https://www.un.org/en/development/desa/population/migration/generalassembly/docs/globalcompact/A_RES_70_1_E.pdf, [accessed 5 November 2020]. [Google Scholar]
- Van den Berghe AJ, Zimmer C. 2011. Life Cycle Assessments Of Single- Versus Multiple-Use Surgical Gowns. Minneapolis, MN: Minnesota Technical Assistance Program, University of Minnesota. http://www.sustainabilityroadmap.org/pims/pdfs/pim247_lifecycle_assessment_disposable_versus_reusable.pdf, [accessed 10 June 2020]. [Google Scholar]
- Vozzola E, Overcash M, Griffing E. 2020. An environmental analysis of reusable and disposable surgical gowns. AORN J 111(3):315–325, PMID: 32128776, 10.1002/aorn.12885. [DOI] [PubMed] [Google Scholar]
- Vozzola E, Overcash M, Griffing E. 2018. Life Cycle Assessment of Surgical Drapes and Tapes: Reusable and Disposable. Environmental Clarity, p. 111. Environmental Clarity, Inc., Reston, VA. Contact mrovercash@earthlink.net, [accessed 25 July 2020].
- Watts N, Amann M, Arnell N, Ayeb-Karlsson S, Beagley J, Belesova K, et al. 2020. The 2020 report of The Lancet Countdown on health and climate change: responding to converging crises. Lancet 397(10269):129–170, PMID: 33278353, 10.1016/S0140-6736(20)32290-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watts N, Amann M, Arnell N, Ayeb-Karlsson S, Belesova K, Boykoff M, et al. 2019. The 2019 report of The Lancet Countdown on health and climate change: ensuring that the health of a child born today is not defined by a changing climate. Lancet 394(10211):1836–1878, 10.1016/S0140-6736(19)32596-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weidema BP. 1997. Guidelines for Critical Review of Product LCA. https://lca-net.com/files/critical_review.pdf, [accessed 23 June 2020].
- Weiser TG, Haynes AB, Molina G, Lipsitz SR, Esquivel MM, Uribe-Leitz T, et al. 2016. Size and distribution of the global volume of surgery in 2012. Bull World Health Organ 94(3):201–209F, PMID: 26966331, 10.2471/BLT.15.159293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisz U, Pichler P-P, Jaccard IS, Haas W, Matej S, Bachner F, et al. 2020. Carbon emission trends and sustainability options in Austrian health care. Resour Conserv Recycl 160:104862, 10.1016/j.resconrec.2020.104862. [DOI] [Google Scholar]
- Woods DL, McAndrew T, Nevadunsky N, Hou JY, Goldberg G, Yi-Shin Kuo D, et al. 2015. Carbon footprint of robotically-assisted laparoscopy, laparoscopy and laparotomy: a comparison. Int J Med Robot 11(4):406–412, PMID: 25708320, 10.1002/rcs.1640. [DOI] [PubMed] [Google Scholar]
- World Health Organization. 2020. WHO Guidance for Climate Resilient and Environmentally Sustainable Health Care Facilities. Geneva, Switzerland: World Health Organization, p. 79. https://apps.who.int/iris/handle/10665/335909, [accessed 27 October 2020]. [Google Scholar]
- Zumsteg JM, Cooper JS, Noon MS. 2012. Systematic review checklist: a standardized technique for assessing and reporting reviews of life cycle assessment data. J Ind Ecol 16(suppl 1):S12–S21, PMID: 26069437, 10.1111/j.1530-9290.2012.00476.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.