Summary:
A narrow waist is considered one of the most attractive female body features. We have developed a minimally invasive surgical method of waist narrowing without rib removal. An access to XI and XII ribs is made through small incisions at the scapular line on both sides. The dorsal cortical plates are osteotomized using a sagittal oscillator saw with a 10 mm wide blade or a piezotome. The osteoclasy is performed, “green stick” type fracture is obtained, and wounds are closed. We put a tight chest corset on a patient for 2 months until the ribs’ fractures consolidate in new position. The number of our clinical cases is 93, and 14 of them were available for follow up at 6 months or more. The average waistline reduction is about 8.0 cm. We indicated period of time, number of cases, and selection criteria. This method is atraumatic, has a short rehabilitation period, and provides for obvious clinical effect.
INTRODUCTION
A narrow waist is an important part of feminine beauty, especially in combination with rounded hips.1 These features, along with full breasts, imply a good hormonal background to a potential partner. Recently, the thin waist has been sought by transgender individuals to feminize their bodies.2
The most common surgical method of body contouring, including the waist, nowadays, is liposuction.3 However, subcutaneous fat removal helps little in converting the “boxy” shape of the trunk into an “hourglass” in slim individuals. Some patients refer to plastic surgery for resection of XI and XII pairs of ribs, trying to get the desired thin waist.2 However, rib resection seems too aggressive in the context of body contouring. Lower pairs of ribs encompass internal organs, soften shocks, and protect kidneys, adrenal glands, the spleen, and the liver from damage. The removal of ribs may be complicated by hemothorax and pneumothorax. Moreover, a lower lateral rib cage defect may cause loss of respiratory function up to 42% of what is normal.4
We have developed a minimally invasive surgical method of waist shaping with rib preservation. This method is atraumatic, has a short rehabilitation period, and provides for marked clinical effect.
METHODS
The upper 10 pairs of ribs are attached in front either to the sternum, or to superior ribs with their cartilages. The lower two pairs of oscillating ribs do not have anterior attachments and end up in soft tissues.
Ninety-three women (age 19–43 years) were operated on. Obvious selection criteria were general health, strong motivation, and laboratory tests within the normal range. A history of pulmonary, renal, or alimentary disorders required a deeper examination in respective areas. Surgery was contraindicated in cases of elevated anesthesiologic risk, apparent emotional instability, and BMI more than 25.
The principles outlined in the Declaration of Helsinki have been followed. All patients gave the written informed consent in regard to anesthesia, surgery, and postoperative treatment. The first video is an animation of the procedure. (See Video 1 [online], which displays the animated schema of the operation process.)
Video 1. Video 1 from “Waist Narrowing without Ribs Removal”.
The rib osteotomy is performed under general, regional, or local anesthesia. The preferable osteotomy site is along the scapular line—that is, lateral to m. longissimus dorsi, between the attachments of m. serratus posterior inferior and m. abdominis obliquus externus. The surgeon makes access to Х1 and XII ribs through the incision about 2 cm long at the scapular line on both sides. Spreading the muscle fibers, the outer rib surface is reached, and the dorsal cortical layer is osteotomized using a sagittal oscillator saw with a blade of 10 mm width or a piezotome. A gentle, gradual increase in digital pressure at the end of a rib ends up with the “green stick” type fracture. (See Video 2 [online], which displays the surgeon cutting the dorsal surface of the XI rib by piezotome and performing the osteoclasy of the XI rib.)
Video 2. Video 2 from “Waist Narrowing without Ribs Removal”.
The pathological mobility of the distal rib fragment is verified both visually and by palpation. Then, the wound is sutured in layers. We put a tight chest corset on the patient immediately after wound dressing (Fig. 1).
Fig. 1.

Patient in a corset, immediately after surgery.
It is necessary to wear the corset no less than 2 months after surgery, until the rib fragments consolidate, changing their curvature, and the lower chest acquires aesthetic smooth narrowing. We control the consolidation by CT, performing it before surgery and 2 months after (Fig. 2). Then we allow the patient to discontinue wearing the corset. Postoperative period was quite comfortable in all patients. Pain was an issue with active movements for 10–14 days and gave in to common analgesics. We requested limiting physical activity and thermal procedures for 1.5–2 months.
Fig. 2.
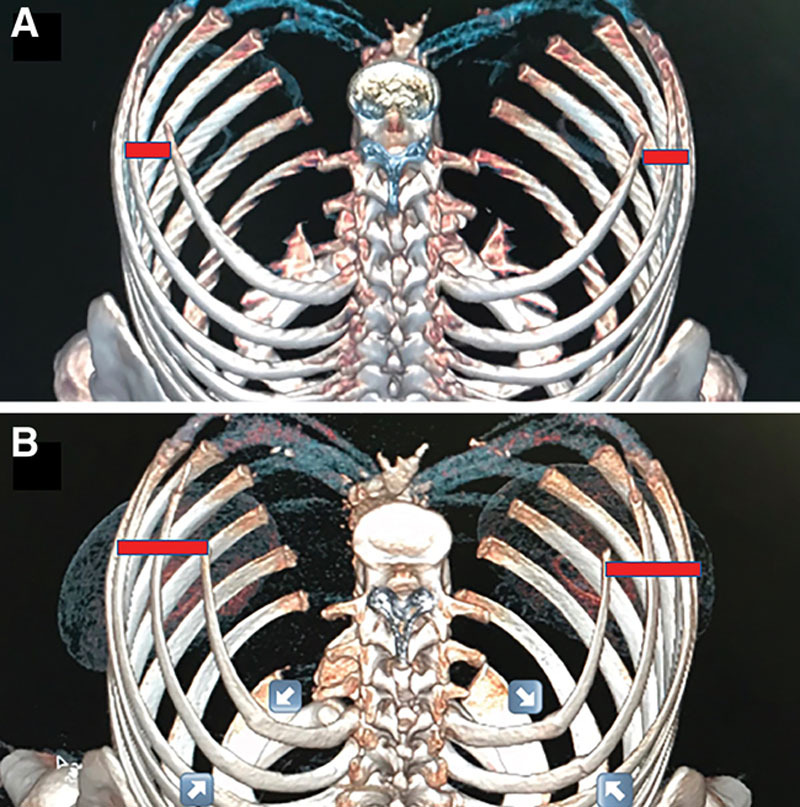
A, CT scan image of a 37-year-old patient before surgery. B, CT scan image of the same patient 2 months after surgery. White arrows point at the sites of rib fractures. Note full consolidation in all but one rib (left XI). Clinical effect is stable: decrease of the waist circumference from 71 cm (above) to 60 cm (below). Note the inward ribs’ displacement (red dots), which are symmetrical regardless of incomplete callus formation of the left XI rib fracture.
RESULTS
Between April 2018 and November 2020, we operated on 93 patients. Three patients were reoperated within 5 months due to a lack of waist narrowing. They did not follow the strict regimen of corset wearing after initial surgery, but turned out to be fully compliant after revision and ended up with good outcomes. Thirty-one other patients never turned up after discharge. Reportedly, those reached by telephone or internet were “just fine.” Forty-eight patients were checked at the appointed time of 2–2.5 months after surgery and found to be quite satisfied. However, the results could not be considered permanent at that point, when the corset was taken off, because the waistline circumference could either increase (probably due to decompression), or continue to decrease due to dietary restrictions and/or voluntary prolonged corset wearing. Fourteen patients were checked at the interval of half a year or more. The average waistline reduction among them was 8.0 cm, ranging from minimal reduction of 4 cm through maximal reduction of 15 cm (See figure 1, Supplemental Digital Content 1, which displays (a) the 41-year-old patient. Waist circumference is 66 cm, BMI=22. Before surgery performed. (b) 2 months after surgery. The waist circumference is 60 cm. Decrease of the waist circumference is 6 cm. BMI is still 22. Patient satisfied. http://links.lww.com/PRSGO/B698.) (See figure 2, Supplemental Digital Content 2, which displays (a) the 39-year-old patient. Waist circumference is 78 cm, BMI=21. Before surgery performed. (b) 2.5 months after surgery. The waist circumference is 70 cm. Decrease of the waist circumference is 8 cm. BMI is still 21. Patient satisfied. http://links.lww.com/PRSGO/B699.)
Patient satisfaction with aesthetic results was generally high, though three of the 14 patients rated the outcome as “a bit lower than expected.” Rate of satisfaction did not correlate with numeric waistline reduction. There were no complications, and postoperative inconveniencies were perceived as moderate to low.
DISCUSSION
So far we have not come across any mention in the scientific literature of methods to reduce waist circumference by rib remodeling. Resection of ribs is commonly considered for treatment of various pathologies, such as cervical ribs5 and slipping rib syndrome.6 Davison et al2 removed the XI and XII rib pairs for aesthetic purposes in five transgender patients. The authors provided little description of the technique used and mentioned no complications. However, some researchers noted postoperative complications after rib resection such as neuralgia, pneumothorax, chest wall deformities, and respiratory functional loss.3
Our method allows waist narrowing, while obviating ribs’ resection, thereby maintaining their important role in protecting the internal organs and decreasing the potential risks of complications, like bleeding from the intercostal vessels. There is also hypothetical risk of pneumothorax due to the proximity of XI rib fracture to the attachment of parietal pleura. In fact, the very design of the osteotomy—on the dorsal rib aspect and only partial—makes pleura involvement very unlikely. Although we have not encountered these complications hitherto, for a beginner we would recommend to have a thoracic surgeon on the team.
CONCLUSIONS
We describe waist narrowing by means of controlled fracture of the XI and XII ribs without their removal. This method is atraumatic, has a short rehabilitation period, and provides for obvious clinical effect.
PATIENT CONSENT
The patient provided written consent for the use of her image.
Supplementary Material
Footnotes
Published online 12 July 2021.
Presented at the IXth National Congress of Plastic and Aesthetic Surgery (online), December 9, 2020, Moscow, Russia
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Pitanguy I. Evaluation of body contouring surgery today: a 30-year perspective. Plast Reconstr Surg. 2000; 105:1499–1514. [PubMed] [Google Scholar]
- 2.Davison SP, Clifton MS, Futrell W, et al. Aesthetic considerations in secondary procedures for gender reassignment. Aesthetic Surg J. 2000; 20:477–481. [Google Scholar]
- 3.Chamosa M. Lipectomy of the ilio-lumbosacral region. Plast Reconstr Surg. 2004; 113:419–424. [DOI] [PubMed] [Google Scholar]
- 4.Hatano A, Nagasao T, Cho Y, et al. Relationship between locations of rib defects and loss of respiratory function – a biomechanical study. Thorac Cardiovasc Surg. 2014; 62:357–362. [DOI] [PubMed] [Google Scholar]
- 5.Peek J, Vos CG, Ünlü Ç, et al. Outcome of surgical treatment for thoracic outlet syndrome: systematic review and meta-analysis. Ann Vasc Surg. 2017; 40:303–326. [DOI] [PubMed] [Google Scholar]
- 6.McMahon LE. Slipping rib syndrome: a review of evaluation, diagnosis and treatment. Semin Pediatr Surg. 2018; 27:183–188. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


