Summary:
This article serves as a practical guide for plastic surgeons focusing on repair of primary cleft lip and nasal deformity. We discuss the key anatomic disruption present in cleft lip and nasal deformity and the goals of primary repair. In addition, our preferred surgical technique for unilateral and bilateral cleft lip and nasal deformity is summarized along with technical pearls and pitfalls.
INTRODUCTION
The cleft population as a whole is heterogeneous, and many treatment protocols have been developed worldwide to prioritize the needs of individual patient populations.1–5 Within different population groups, variations exist in the treatment of patients with cleft lip and nasal deformity. The variations include timing of repair, technique used, sequencing, scar burden, emphasis on facial growth and speech outcomes, socioeconomic restraints, resource availability, and cultural perception.2–12 An understanding of characteristics specific to the patient population being cared for is essential to achieving optimal outcomes.
The challenge in reconstruction of the cleft lip and nasal deformity is based on restoration of the normal anatomy of the individual orofacial cleft, which can present with varying degrees of severity, as well as correction that anticipates the fourth-dimensional changes that occur over time. Constant self-evaluation of surgical outcomes and course correction is necessary to continually improve and achieve consistent results.
In this article, we will focus on the analysis of patients with cleft lip and nasal deformities, describe the aberrant anatomy, and discuss preoperative adjuncts that can be used to optimize results. We will also underscore the importance of the nasal repair as the central component in repair of the cleft lip and nasal deformity. Finally, we aim to highlight technical pearls to optimize outcomes in patients with unilateral and bilateral cleft lip and nasal deformity.
ANALYSIS OF THE CLEFT LIP AND NASAL DEFORMITY
Following Sir Harold Gillies’ principle “diagnose before you treat,” accurate assessment of the heterogenous cleft lip and nasal anatomic deformities is crucial to surgical design.13 The anatomic variations are based on differences in rotation and projection of the premaxillary segment, width of the alveolar cleft, length of columella, displacement of the caudal septum, malposition of the lower lateral cartilage (LLC), fullness of the dry vermilion along the premaxillary segment and lateral lip, and the height of the lateral and medial lip segments. Each variable must be incorporated into the initial markings and surgical repair, while simultaneously considering ethnic differences in growth and scar quality to anticipate fourth-dimensional changes.
Although numerous techniques have been described to address each component in patients with cleft lip and nasal deformities, a critical analysis of the surgeon’s individual patient populations is necessary to decipher the optimal technique to achieve the desired outcome.14–23 Early methods of primary cleft lip repair differed in skin markings, which resulted in the unequal vertical heights seen in the straight-line repair technique. While Tennison and LeMesurier modified the initial markings and provided vertical height symmetry, their technique resulted in a disrupted philtral column and did not address the nasal deformity. In contrast, the Fisher anatomical subunit repair addressed the tissue deficiency, but did not address the primary nasal deformity.14–23
In our patient population of predominantly Hispanic ethnicity, our surgical design for the unilateral cleft lip and nasal deformity is a modification of the Millard rotation advancement technique.15,24,25 This modification evolved after analysis of our long-term results, where an unfavorable lip shortening and elevation of Cupid’s bow was noted on the cleft side, despite placement of a small Z plasty above Cupid’s bow. As a result, a triangular flap marked on the lateral lip segment was incorporated into the surgical design and has since augmented this lip length deficiency. In addition, we prioritize correction of the nasal deformity. A component of the repair that has evolved throughout practice is the recognition that the nose is the most visible and central component of the face, while the lip lies in its shadow.
In patients with a bilateral cleft lip and nasal deformity, our preferred surgical approach is a modification of Byrd’s technique.23 This modification abandons the incision around the alar base due to the hypertrophic scarring seen in our Hispanic patients. Although some authors advocate for a two-stage repair in patients with asymmetric bilateral cleft lip and nasal deformity, including lip adhesion on the contralateral side, we advise against the staged approach because scar burden can result in disruption of cutaneous landmarks, leading to suboptimal outcomes.26,27
ANATOMY OF THE CLEFT LIP NASAL DEFORMITY
Unilateral Cleft Lip Nasal Deformity
Precise repair of unilateral cleft lip and nasal deformity relies upon a three-dimensional understanding of the anatomic and functional relationship of the lip, nose, and adjacent expressive musculature; so an optimal result can be achieved with both repose and animation.28–31 The normal anatomy of the orbicularis oris muscle consists of a deep portion or profundus and a superficial portion or superficialis that behave with antagonist action during lip movement.30 The profundus is responsible for sphincteric function and is a constrictor muscle, whereas the superficialis is responsible for facial expression and functions as a retractor muscle.30,32,33 We find that accurate alignment of the profundus and superficialis is necessary to maintain dynamic function and prevent unfavorable distortion of the lip.34
In the complete unilateral cleft lip and nasal deformity, the superficialis muscle fibers proceed horizontally from the modiolus and insert in a discontinuous manner along the margins of the cleft.28,29 These muscular fibers terminate beneath the base of the columella along the noncleft side and beneath the base of the nasal ala along the cleft side. The profundus, while present, is hypoplastic and, rather than projecting anteriorly giving rise to a cutaneous-vermilion junction or white roll, terminates within the vermillion mucosa.14,28,29,31,35 In addition, the course of the cleft segment’s paranasal muscle fibers from the ala to the anterior nasal spine is interrupted, contributing to nasal deviation.36,37 These aberrant muscular insertions create facial imbalance further intensified by the degree of the retropositioned and hypoplastic maxillary cleft segment. Unopposed muscular forces result in an asymmetric nasal tip via displacement of the caudal septum, the cleft medial crural footplate, and columella toward the noncleft side and compensatory bowing of the septum, flaring of the cleft side LLC, and widening of the alar base towards the cleft side.28,29,31 The LLC’s change in position affects its attachment to the upper lateral cartilage (ULC) and weakens both the upper lateral cartilage and scroll region.
Bilateral Cleft Lip Nasal Deformity
Anatomic variants of the bilateral cleft lip nasal deformity resemble the unilateral deformity. They are characterized by dislocated bilateral medial crural footplates, leading to columellar shortening and lateral displacement of both alar bases. There is flattening of the lateral segment of both LLC due to aberrant muscular insertions, leading to alar flaring and poor delineation of the alar facial groove.18,23,28,29,31,35 Furthermore, the philtral columns and Cupid’s bow peaks are absent.
TIMING AND SEQUENCE OF REPAIR
Although numerous studies show no adverse effects on nasal and midfacial growth following primary cleft lip and nasal deformity repair with or without septoplasty, there is no consensus as to how timing of the lip repair may impact midfacial skeletal growth.12,38–44 Furthermore, timing and sequence may vary in different populations based on prioritization of speech and facial growth, socioeconomic factors, resource availability, and cultural variations.2–5,7,8,10,11,45
In a retrospective study performed by the senior author following a cohort of nonsyndromic patients until 23 years of age treated at our institution, a multivariate analysis showed that early age at primary lip procedure was the sole significant predictor of later orthognathic surgery.46 As such, the senior author’s protocol has transitioned to performing primary repair at 4 months of age and advocates that timing should not be standardized, but rather individualized based on population growth patterns.
PRESURGICAL ADJUNCTS
Nasoalveolar Molding
Early management of the cleft lip nasal deformity can be approached with Nasoalveolar molding (NAM) to passively mold the alveolar arch, expand the ala, and increase the columellar length, effectively remodeling the dentofacial skeleton.47–49 While advocates of NAM cite advantages including facilitation of the primary repair and sufficient alignment of the alveolar cleft segments enabling a gingivoperiosteoplasty (GPP) to be performed at the time of repair, opponents argue that there is a paucity of high-level evidence to support long-term benefits.49–54 In a retrospective study performed by Chang et al over an 11-year period assessing primary cleft rhinoplasty outcomes, patients who underwent NAM plus primary rhinoplasty and overcorrection demonstrated the best long-term outcomes. However, this cohort was treated with silicone sheets and nasal conformers for an additional 6 months postoperatively to maintain overcorrection.55
Lip Taping and Lip Adhesion
In geographic areas where presurgical NAM is unavailable, lip taping may be used in patients with wide clefts to approximate the alveolar segments by an indirect restraining force.56 Studies have previously shown that lip taping can reduce an alveolar gap by 53%.56,57 Although labial adhesion has been described as an alternative to facilitate definitive repair, the potential scar burden can compromise the surgical outcome and therefore is not recommended.12,39,58
OPTIMIZING RESULTS IN PRIMARY CLEFT LIP AND NASAL DEFORMITY
Goals of Surgical Repair
The goals of primary repair are to achieve nasal symmetry, functional symmetry of all lip elements with animation, and endure the fourth-dimensional changes of time. While numerous techniques have been described, the senior author has achieved consistent results using a modified Millard rotation advancement technique in patients with unilateral cleft lip and nasal deformities and a modification of the Byrd technique in patients with bilateral deformities.23,25
We found that utilization of NAM as early as 2 weeks of life can help align the alveolar segments and mold and shape the lateral crus on the cleft side in the short term (Fig. 1). In patients with an alveolar segment alignment less than 2 mm apart, we routinely perform GPP at the time of repair to reduce the need for subsequent alveolar bone grafting in up to 40% of patients.59
Fig. 1.

NAM can facilitate cleft lip and nasal deformity repair. A, Newborn with bilateral cleft lip and nasal deformity. B, Two months after application of NAM. C, After completion of NAM. D, Immediate postoperative view. Note the accentuated appearance of the nose due to overcorrection. E, Ten-year follow-up of the same patient (AP view). F, Nasal tip elevation is maintained (worm-eye view).
Preferred Surgical Approach in Primary Unilateral Cleft Lip and Nasal Deformity
Accurate assessment of the anatomic deformity is essential to achieving surgical success. Key to our surgical design is prioritization of the nasal repair and markings that account for fourth-dimensional changes. These include lip shortening, color mismatch, scar burden, nasal deviation, asymmetry of the alar base, and nasal tip depression.
Our cleft markings are a modification of Millard’s rotation advancement technique with the addition of an inferior triangular flap from the lateral lip element (Fig. 2). This modification accounts for the vertical height deficiency and lip shortening seen with overcorrection of the nasal deformity in our patient population over time. Additional landmarks include accurate identification of the wet-dry junction along the red line just above the transitional epithelium. This is important for color match, particularly when incorporating Noordhoff’s triangular flap to augment the noncleft side dry vermillion deficiency. Marking of the white roll are to be made above and below Cupid’s bow peak to preserve topography during realignment of this three-dimensional scroll region.
Fig. 2.
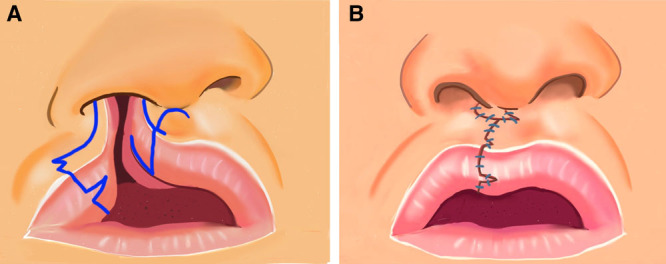
Cleft lip and nasal deformity markings. Unilateral cleft lip and nasal deformity with markings of the lateral segment triangular flap and Noordhoff’s dry vermilion flap (A) and (B) release of the nasalis muscle from its abnormal insertion to the orbicularis oris.
Releasing the rotation flap from its aberrant orbicularis attachments to the septum, nose, and maxilla corrects the medial lip segment. Adequate dissection must be performed so that the rotation flap has enough downward mobility to allow for an inferior positioning of Cupid’s bow peak on the cleft side and to visibly appear lower on the operating room table in comparison with the noncleft Cupid’s bow peak. We perform overcorrection of the lip length to avoid fourth-dimensional changes that result from scar contracture and cause shortening of the cleft side philtral column. The lateral segment is mobilized by releasing the nasalis muscle from its abnormal insertion to the orbicularis oris and advanced to align with medial lip segment. (See Video 1 [online], which displays unilateral lip markings and flap elevations.) In patients with wide clefts who did not undergo NAM, further dissection is performed to allow for proper alignment of the lip segments.
Video 1. Unilateral lip markings. Video 1 from “How to Get Consistently Good Results in Cleft Lip Repair”.
The remainder of our dissection prioritizes the nose with a focus on achieving nasal symmetry. Key technical maneuvers include release of tethering forces on the septum and the cleft LLC, reconstruction of a muscular ring across the nasal sill to provide a platform for the hypoplastic maxilla, and overcorrection of the nasal tip to combat fourth-dimensional changes that result in nasal tip depression.24 (See Video 2 [online], which displays unilateral nasal deformity and closure.)
Video 2. Unilateral nasal deformity. Video 2 from “How to Get Consistently Good Results in Cleft Lip Repair”.
To mobilize the retropositioned cleft nasal base into natural anatomic position, we release the accessory chain along the piriform aperture. The deviated caudal septum is exposed and released from its insertion to the anterior nasal spine. This allows for repositioning of the caudal septum toward the midline and represents a modification of our technique from prior outcome analysis. Patients who did not undergo septal repositioning had an increase in relapse of nasal tip deformity and need for intermediate rhinoplasty at school age.
To allow differential movements of the malpositioned nasal alae and LLC, we perform wide dissection of the nasal skin envelope, freeing the cartilaginous framework from the soft tissue. The middle crus of the cleft LLC is sutured to the upper lateral cartilage/septum junction of the noncleft side using a Tajima suture to recreate the nasal dome and provide projection and symmetry. The cleft nostril is intentionally overprojected to account for anticipated nasal tip depression due to inadequate boney foundation. An alar cinch stich is used to reduce the widened alar base width by suturing the nasalis on the cleft side to the nexus point—ie, the medial crural footplate on the noncleft side. The widened alar base in unilateral cleft lip nasal deformities is not overcorrected because it can result in a difficult external valve stenosis repair.
Muscle alignment with appropriate retraction is a critical component to maintaining consistent long-term outcomes. Overcorrection of the cleft nasal tip and cleft side lip length is maintained by retracting the cleft nose in a cephalad direction and the greater and lesser segments of the lip in a caudal direction. This aligns the cutaneous elements of Cupid’s bow during closure of the orbicularis. Lastly, the superficial portion of the orbicularis is separated from the deep orbicularis just above the white role to slightly overcorrection the rotation of the new cleft Cupid’s bow (Figs. 3, 4).
Fig. 3.

Left unilateral cleft lip and nasal deformity. A, C, Preoperative AP views of two patients with left unilateral cleft lip and nasal deformity. B, D, Six-year follow-up of the same patients (AP views).
Fig. 4.

Right unilateral cleft lip and nasal deformity. A, Preoperative AP view. B, Nine year follow up of the same patient (AP view). C, Worm-eye view.
Preferred Surgical Approach in Primary Bilateral Cleft Lip and Nasal Deformity
The markings of the bilateral cleft lip nasal deformity are based on a modification of Byrd’s technique (Fig. 5).23 This modification abandons the alar base incisions due to hypertrophic scarring seen in our ethnic population.
Fig. 5.
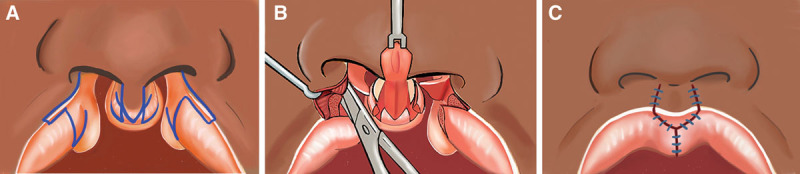
Cleft lip and nasal deformity markings. Bilateral cleft lip and nasal deformity with markings of the prolabium and lateral lip segment, including tubercle flaps (A, B) release of the nasalis muscle from its abnormal insertion to the orbicularis oris, and (C) skin and vermillion closure with inclusion of the prolabium white roll and dry vermillion.
The prolabium markings are designed to augment vermillion deficiency. The base of columella is used to determine the width of the prolabium flap and the midpoint at the redline marks the caudal extent of the prolabium flap. In patients with a rotated or projected prolabium, the frenulum can help identify the midpoint of Cupid’s bow. The prolabium flap markings include the dry vermillion within the tubercle, providing additional tissue to circumvent unfavorable fourth-dimensional changes that result in a tight lip. In patients with asymmetric complete/incomplete cleft lip and nasal deformity, the simonart band in the incomplete side is excised to maintain symmetry.
One challenge in reconstruction of the bilateral cleft lip and nasal deformity is delayed development of a whistle deformity in patients with a protruded premaxilla. The lateral lip segment is designed to produce an overcorrection of the tubercle flaps by including all remaining dry vermillion and profundus of the orbicularis. (See Video 3 [online], which displays bilateral lip markings and nasal deformity.)
Video 3. Bilateral lip markings. Video 3 from “How to Get Consistently Good Results in Cleft Lip Repair”.
One critical element in elevation of the prolabium flap is dissection toward the caudal septum or nexus point. This critical maneuver provides additional length to the deficient columella and also serves as an anchor to secure the orbicular oris muscle at the time of closure. By anchoring the orbicularis oris to the nexus point, we can mitigate fourth-dimensional changes associated with lip lengthening that occurs with animation and muscle reunification.
Once the prolabium and lateral lip elements have been elevated, emphasis is placed on addressing the primary nasal deformity. Similar to the unilateral repair, the accessory chain along with the nasal side wall mucosa are released bilaterally to provide independent movement of the malpositioned LLC. The cartilaginous framework is freed from its soft tissue attachments. Tajima sutures elevate the depressed dome of the LLC, and inter-domal sutures narrow the widened nasal tip. Further columellar lengthening in the deficient bilateral deformity is achieved by sliding the medial crural footplates up the septum. Finally, an alar cinch stitch using the nasalis from both sides narrows and overcorrects the alar base to combat fourth-dimensional changes that lead to alar base widening (Fig. 6). The redundant nasal tip skin smooths out in the first 6 weeks postoperatively. (See Video 4 [online], which displays inset and closure.)
Fig. 6.

Bilateral cleft lip and nasal deformity. A, 3-month-old female child with rotated and projected premaxilla (AP view). B, Lateral view: patient did not receive nasoalveolar molding. C, Five-year follow-up (AP view). D, Ten-year follow-up (AP view). E, Right lateral oblique view.
Video 4. Inset and closure. Video 4 from “How to Get Consistently Good Results in Cleft Lip Repair”.
POSTOPERATIVE CARE
Postoperative results vary widely due to quality of scar formation, scar management compliance, and follow-up. Optimization of these components for each individual help yield more consistent results. We maintain silicone nasal retainers for a minimum of 6 weeks to combat scar contracture forces associated with wound healing. It is critical that nasal stents are not sewn in too tight and do not apply pressure to the columella. They are removed if there is any evidence that they may create pressure injury. We recommend application of sunscreen and minimal sun exposure for the first year postoperatively to minimize scar discoloration. Scar massage is started 2 weeks postoperatively and continued for an additional year. Application of adjunctions including silicone gel is encouraged. In patients who develop early scar contracture of the lip or element, Kenalog injections are performed.
PEARLS AND PITFALLS
An understanding of the surgeon’s patient population and ethnic variations is critical to achieving optimal outcomes in patients with cleft lip and nasal deformities. Accurate assessment of the anatomic deformity along with anticipated fourth-dimensional changes is critical to the surgical design. Prioritization of the nasal deformity is an essential component of repair and we emphasize overcorrection of the nasal tip to optimize outcomes. Finally, surgeons must be self-critical with constant reassessment of results and willingness to change course of action when necessary.
PATIENT CONSENT
Parents or guardians provided written consent for the use of the patients’ images.
Footnotes
Published online 12 July 2021.
Disclosure: All the authors have no financial interest to declare in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Salyer KE, Xu H, Genecov ER. Unilateral cleft lip and nose repair; closed approach Dallas protocol completed patients. J Craniofac Surg. 2009; 20(suppl 2):1939–1955. [DOI] [PubMed] [Google Scholar]
- 2.Agrawal K, Panda K. A modified surgical schedule for primary management of cleft lip and palate in developing countries. Cleft Palate-Craniofacial J. 2011; 48:1–8. [DOI] [PubMed] [Google Scholar]
- 3.De Mey A, Franck D, Cuylits N, et al. Early one-stage repair of complete unilateral cleft lip and palate. J Craniofac Surg. 2009; 20(suppl 2):1723–1728. [DOI] [PubMed] [Google Scholar]
- 4.Galárraga IMC. Use of botulinum toxin in cheiloplasty: a new method to decrease tension. Can J Plast Surg. 2009; 17:e1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shaw WC, Semb G, Nelson P, et al. The Eurocleft project 1996-2000: overview. J Cranio-Maxillofacial Surg. 2001; 29:131–140 [DOI] [PubMed] [Google Scholar]
- 6.Silva Filho OG, Calvano F, Assunção AG, et al. Craniofacial morphology in children with complete unilateral cleft lip and palate: a comparison of two surgical protocols. Angle Orthod. 2001; 71:274–284. [DOI] [PubMed] [Google Scholar]
- 7.Malek R, Psaume J: Nouvelle conception de la chronologie et de la technique chirurgicale du traitment des fentes labio-palatines. Results sur 220 cas. Ann Chir Plast Esthet. 1983; 28:237–244. [PubMed] [Google Scholar]
- 8.Manna F, Pensiero S, Clarich G, et al. Cleft lip and palate: current status from the literature and our experience. J Craniofac Surg. 2009; 20:1383–1387. [DOI] [PubMed] [Google Scholar]
- 9.Bardach J, Morris HL, Olin WH. Late results of primary veloplasty: the marburg project. Plast Reconstr Surg. 1984; 73:207– 2–18. [DOI] [PubMed] [Google Scholar]
- 10.Miachon MD, Leme PL. Surgical treatment of cleft lip. Rev Col Bras Cir. 2014; 41:208–214. [DOI] [PubMed] [Google Scholar]
- 11.Salyer KE. Excellence in cleft lip and palate treatment. J Craniofac Surg. 2001; 12:2–5. [DOI] [PubMed] [Google Scholar]
- 12.Salyer KE, Genecov ER, Genecov DG. Unilateral cleft lip-nose repair: a 33-year experience. J Craniofac Surg. 2003; 14:549–558. [DOI] [PubMed] [Google Scholar]
- 13.Davis AD. The Principles and Art of Plastic Surgery [Review]. Calif Med.1956; 87:67. [Google Scholar]
- 14.Gibson T. Cleft craft. The evolution of its surgery. II. Bilateral and rare deformities [Review]. Br. J. Plast. Surg. 1980; 33:307. [Google Scholar]
- 15.Millard DR. Rotation-advancement principle in cleft lip closure. Cleft Palate J. 1964; 12:246–252. [PubMed] [Google Scholar]
- 16.Millard DR. A radical rotation in single harelip. Am J Surg. 1958; 102:1331–1338. [DOI] [PubMed] [Google Scholar]
- 17.Mohler LR. Unilateral cleft lip repair. Plast Reconstr Surg. 1987; 80:511–517. [DOI] [PubMed] [Google Scholar]
- 18.Mulliken JB. Bilateral cleft lip. Clin Plast Surg. 2004; 31:209–220. [DOI] [PubMed] [Google Scholar]
- 19.Randall P. A triangular flap operation for the primary repair of unilateral clefts of the lip. Plast Reconstr Surg. 1959; 23:331- 347. [DOI] [PubMed] [Google Scholar]
- 20.Millard DR. Cleft Craft. The Evolution of Its Surgery. Volume I:The Unilateral Deformity. Philadelphia, PA: Lippincott Williams and Wilkins; 1976. [Google Scholar]
- 21.Lemesurier AB. The quadrilateral Mirault flap operation for hare-lip. Plast Reconstr Surg (1946). 1955; 16:422–433. [DOI] [PubMed] [Google Scholar]
- 22.Fisher DM. Unilateral cleft lip repair: an anatomical subunit approximation technique. Plast Reconstr Surg. 2005; 116:61–71. [DOI] [PubMed] [Google Scholar]
- 23.Byrd HS, Ha RY, Khosla RK, et al. Bilateral cleft lip and nasal repair. Plast Reconstr Surg. 2008; 122:1181–1190. [DOI] [PubMed] [Google Scholar]
- 24.Byrd HS, Salomon J. Primary correction of the unilateral cleft nasal deformity. Plast Reconstr Surg. 2000; 106:1276–1286. [DOI] [PubMed] [Google Scholar]
- 25.Lance S, Tsai C, Gosman A, et al. Cleft lip repair. In: Evans G, ed. Operative Plastic Surgery. 2nd ed. Oxford: Oxford University Press; 2019:503–518. [Google Scholar]
- 26.Wolfe SA, Ghurani R, Mejia M. Use of staged rotation-advancement procedures for the treatment of incomplete bilateral clefts of the lip. Ann Plast Surg. 2004; 52:263–268; discussion 269. [DOI] [PubMed] [Google Scholar]
- 27.Sumiya N, Ito Y, Otani K, et al. Correction of the bilateral complete cleft lip: transformation to a unilateral incomplete cleft lip closure. Ann Plast Surg. 2001; 46:369–374. [DOI] [PubMed] [Google Scholar]
- 28.Fara M. The anatomy of cleft lip. Clin Plast Surg. 1975; 2:205–214. [PubMed] [Google Scholar]
- 29.Fára M. Anatomy and arteriography of cleft lips in stillborn children. Plast Reconstr Surg. 1968; 42:29–36. [PubMed] [Google Scholar]
- 30.Nicolau PJ. The orbicularis oris muscle: a functional approach to its repair in the cleft lip. Br J Plast Surg. 1983; 36:141–153. [DOI] [PubMed] [Google Scholar]
- 31.Kaufman Y, Buchanan EP, Wolfswinkel EM, et al. Cleft nasal deformity and rhinoplasty. Semin Plast Surg. 2012; 26:184–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Latham RA, Deaton TG. The structural basis of the philtrum and the contour of the vermilion border: a study of the musculature of the upper lip. J Anat. 1976; 121(Pt 1):151–160. [PMC free article] [PubMed] [Google Scholar]
- 33.Nairn RI. The circumoral musculature: structure and function. Br Dent J. 1975; 138:49–56. [DOI] [PubMed] [Google Scholar]
- 34.Park CG, Ha B. The importance of accurate repair of the orbicularis oris muscle in the correction of unilateral cleft lip. Plast Reconstr Surg. 1995; 96:780–788. [DOI] [PubMed] [Google Scholar]
- 35.Mulliken JB, Pensler JM, Kozakewich HP. The anatomy of Cupid’s bow in normal and cleft lip. Plast Reconstr Surg. 1993; 92:395–403; discussion 404. [PubMed] [Google Scholar]
- 36.Delaire J. Theoretical principles and technique of functional closure of the lip and nasal aperture. J Maxillofac Surg. 1978; 6:109–116. [DOI] [PubMed] [Google Scholar]
- 37.Joos U. Muscle reconstruction in primary cleft lip surgery. J Cranio-Maxillofacial Surg. 1989; 17(suppl 1):8–10. [DOI] [PubMed] [Google Scholar]
- 38.Gawrych E, Janiszewska-Olszowska J. Primary correction of nasal septal deformity in unilateral clefts during lip repair – A long-term study. Cleft Palate-Craniofacial J. 2011; 48:293–300. [DOI] [PubMed] [Google Scholar]
- 39.Anderl H, Hussl H, Ninkovic M. Primary simultaneous lip and nose repair in the unilateral cleft lip and palate. Plast Reconstr Surg. 2008; 121:959–970. [DOI] [PubMed] [Google Scholar]
- 40.Xu H, Salyer KE, Genecov ER. Primary bilateral one-stage cleft lip/nose repair: 40-year Dallas experience: part I. J Craniofac Surg. 2009; 20(suppl 2):1913–1926. [DOI] [PubMed] [Google Scholar]
- 41.Xu H, Salyer KE, Genecov ER. Primary bilateral two-stage cleft lip/nose repair: part II. J Craniofac Surg. 2009; 20(suppl 2):1927–1933. [DOI] [PubMed] [Google Scholar]
- 42.McComb HK, Coghlan BA. Primary repair of the unilateral cleft lip nose: completion of a longitudinal study. Cleft Palate Craniofac J. 1996; 33:23–30; discussion 30. [DOI] [PubMed] [Google Scholar]
- 43.McComb HK. Primary repair of the bilateral cleft lip nose: a long-term follow-up. Plast Reconstr Surg. 2009; 124:1610–1615. [DOI] [PubMed] [Google Scholar]
- 44.McComb H. Primary repair of the bilateral cleft lip nose: a 15-year review and a new treatment plan. Plast Reconstr Surg. 1990; 86:882–889; discussion 890. [PubMed] [Google Scholar]
- 45.Ysunza A, Pamplona MC, Quiroz J, et al. Maxillary growth in patients with complete cleft lip and palate, operated on around 4–6 months of age. Int J Pediatr Otorhinolaryngol. 2010; 74:482–485. [DOI] [PubMed] [Google Scholar]
- 46.Dalle Ore C, Schoenbrunner A, Brandel M, et al. Incidence of Le Fort surgery in a mature cohort of patients with cleft lip and palate. Ann Plast Surg. 2017; 78(5 suppl 4):S199–S203. [DOI] [PubMed] [Google Scholar]
- 47.Grayson BH, Cutting CB. Presurgical nasoalveolar orthopedic molding in primary correction of the nose, lip, and alveolus of infants born with unilateral and bilateral clefts. Cleft Palate Craniofac J. 2001; 38:193–198. [DOI] [PubMed] [Google Scholar]
- 48.Grayson BH, Maull D. Nasoalveolar molding for infants born with clefts of the lip, alveolus, and palate. Clin Plast Surg. 2004; 31:149–158, vii. [DOI] [PubMed] [Google Scholar]
- 49.Marcus JR, Allori AC, Santiago PE. Principles of cleft lip repair: conventions, commonalities, and controversies. Plast Reconstr Surg. 2017; 139:764e–780e. [DOI] [PubMed] [Google Scholar]
- 50.Mandell J, Unkart J, Gosman AA. Is NAM a scam? J Am Soc Maxillofac Surg. 2017; 1:17–20. [Google Scholar]
- 51.Hathaway RR, Long RE, Jr. Early cleft management: in search of evidence. Am J Orthod Dentofacial Orthop. 2014; 145:135–141. [DOI] [PubMed] [Google Scholar]
- 52.Grayson BH. Discussion: limited evidence for the effect of presurgical nasoalveolar molding in unilateral cleft on nasal symmetry: a call for unified research. Plast Reconstr Surg. 2013; 131:75e–76e. [DOI] [PubMed] [Google Scholar]
- 53.Grayson BH, Garfinkle JS. Early cleft management: the case for nasoalveolar molding. Am J Orthod Dentofacial Orthop. 2014; 145:134–142. [DOI] [PubMed] [Google Scholar]
- 54.van der Heijden P, Dijkstra PU, Stellingsma C, et al. Limited evidence for the effect of presurgical nasoalveolar molding in unilateral cleft on nasal symmetry: a call for unified research. Plast Reconstr Surg. 2013; 131:62e–71e. [DOI] [PubMed] [Google Scholar]
- 55.Chang CS, Por YC, Liou EJ, et al. Long-term comparison of four techniques for obtaining nasal symmetry in unilateral complete cleft lip patients: a single surgeon’s experience. Plast Reconstr Surg. 2010; 126:1276–1284. [DOI] [PubMed] [Google Scholar]
- 56.Pool R, Farnworth TK. Preoperative lip taping in the cleft lip. Ann Plast Surg. 1994; 32:243–249. [DOI] [PubMed] [Google Scholar]
- 57.Tse R. Unilateral cleft lip: principles and practice of surgical management. Semin Plast Surg. 2012; 26:145–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Scrimshaw GC. Lip adhesion—A passing fad? Ann Plast Surg. 1979; 2:183–188. [DOI] [PubMed] [Google Scholar]
- 59.Santiago PE, Grayson BH, Cutting CB, et al. Reduced need for alveolar bone grafting by presurgical orthopedics and primary gingivoperiosteoplasty. Cleft Palate Craniofac J. 1998; 3577–80. [DOI] [PubMed] [Google Scholar]


