Abstract.
Leprosy is an infectious disease caused by Mycobacterium leprae. China was once one of the countries with severe leprosy epidemics, but its incidence has remained low in recent years. Despite this, there has been no decrease in its incidence more recently, and it is still a public health problem which needs to be controlled. In this study, we analyzed the epidemiological characteristics and trends in the detection rate of new cases of leprosy in China between 2004 and 2016. There were 4,519 cases of leprosy in 28 provinces, municipalities, and autonomous regions between 2004 and 2016, and the total incidence was 0.02815 (per 100,000 individuals) and 21 deaths. The overall incidence of leprosy showed an inverted “V” distribution (i.e., an increase followed by a decrease). Yunnan, Sichuan, Guangdong, Guizhou, and Guangxi were the top five regions with the highest incidence rates, and they accounted for 68.7% of the total cases. There were more male patients than female patients, and peasants accounted for 71.7% of the leprosy cases. The patients with leprosy in China were mainly concentrated in the age-group 15–44 years, as this group accounted for 57.2% of the total cases. The purpose of this study is to explore the epidemiology of leprosy in China. This analysis will be useful for future monitoring of leprosy and establishment of public health measures in China, in keeping with the “Programme for the Elimination of Leprosy in China 2011–2020.”
INTRODUCTION
Leprosy, a chronic infectious disease caused by Mycobacterium leprae infection, primarily invades the skin and peripheral nerves and causes irreversible neurological damage and chronic disability.1 This disease has been plaguing humans for at least 100,000 years and still affects millions of people all the world. At present, leprosy is mainly distributed in tropical and subtropical parts of the world such as Asia, Central America, Africa, and South America; its distribution may be related to poor sanitary conditions in these areas and has little association with warm climate.2
According to a WHO report published in 2018, there were 208,619 new cases of leprosy in the world, and these new cases are mainly concentrated in 23 global priority countries.3 China was once one of the countries with severe leprosy epidemics4: In 1975, more than 400,000 cases of leprosy were registered nationwide in China. After the combination chemotherapy program was adopted in 1986, the number of patients rapidly declined.5,6 By 1994, 80% of the provinces and cities in China had reached the basic elimination index (with a prevalence rate of 1/100,000 individuals.7 However, the number of new cases in China has not decreased in the past 15 years, and leprosy remains an important health problem in some regions of China.8 Moreover, China is adjacent to India, Myanmar, and Nepal, which belong to the 23 priority countries, and as a result, there is an increased risk of imported cases. In addition, drug-resistant cases have emerged since combination chemotherapy was started,9,10 and this has led to increased difficulty in treatment and control. Thus, it is important to monitor the incidence of leprosy in China and understand its patterns, to aid efficient prevention and management of this disease.
This study uncovers the epidemiological characteristics and trends of leprosy in China between 2004 and 2016. This analysis will be useful for future monitoring of the disease and public health measures in China.
MATERIALS AND METHODS
Data sources.
Although a national standardized reporting system for selected infectious diseases has been established since 1955 in China, leprosy was included in the system only in 1978.11 The paper-based method of reporting notifiable diseases in 1950 was replaced by the electronic version in 1985; following this, an Internet-based case reporting system was introduced in 2003. Therefore, patient data have been more accurate and detailed since 2004. In this study, the number, age, and geographic data of patients with leprosy from 2004 to 2016 were collected from the Public Health Data Center. In addition, the annual population data of the year 2004–2016 were collected from the data published on the website of the Chinese National Bureau of Statistics.
Statistical analysis.
We used joinpoint regression models12 to examine the incidence and mortality trends of leprosy from 2004 to 2016 and to identify changes in the trends at every stage. The software program Joinpoint Regression Program Version 4.7.0.0 (Statistical Research and Applications Branch, National Cancer Institute) was used to build the joinpoint regression models and calculate annual percentage change (APC) and average APC (AAPC) as indicators of trends. Annual percentage change is a measure used to characterize trends in rates over time. One advantage of characterizing trends this way is that it is comparable across scales. Average annual percentage change is a summary measure of the trend over a prespecified fixed interval. It is a single variable that represents the average APC over a period of multiple years. The Z test or t-test was used to assess whether an APC or AAPC was significantly different from zero. The terms “increase” and “decrease” were used when P < 0.05 for the Z test or t-test. A non-significant APC (P ≥ 0.05) was described as stable, and it indicated that the incidence was maintained at a perennially stable level or that the incidence was perennially unreported or only reported sporadically.
The incidence (per 100,000 individuals) was calculated as the number of new cases of leprosy per year divided by the mid-year population size. This study included 28 provinces, municipalities, and autonomous regions, which were divided into two parts: the southern region (Shanghai city, Jiangsu Province, Zhejiang Province, Anhui Province, Fujian Province, Jiangxi Province, Hubei Province, Hunan Province, Guangdong Province, Guangxi Zhuang Autonomous Region, Chongqing city, Sichuan Province, Guizhou Province, Yunnan Province, and Hainan Province) and the northern region (Beijing city, Tianjin city, Hebei Province, Shanxi Province, Heilongjiang Province, Liaoning Province, Jilin Province, Shandong Province, Henan Province, Shannxi Province, Gansu Province, Qinghai Province, and Xinjiang Uygur Autonomous Region).
Gender-based differences were analyzed in this study. We divided the population into the following age-groups: < 0, 0–5, 5–10, 10–15, 15–20, 20–25, 25–30, 30–35, 35–40, 40–45, 45–50, 50–55, 55–60, 60–65, 65–70, 70–75, 75–80, 80–85, and > 85. The epidemiology of leprosy in 17 different groups according to occupation was analyzed: Peasant, Worker, Houseworker or Unemployed, Student, Migrant Worker, Others, Unknown, Retiree, Commercial Waiter, Scattered Children, Cadre Staff, Teacher, Fisherman, Caterer, Herdsman, and Medical Staff.
IBM SPSS Statistics v. 22.0 (IBM, New York, NY) and Excel 2010 (Microsoft Corp., Redmond, WA) were used to extract data and sort and clean it. IBM SPSS Statistics v. 22.0 and R ×64 3.5.2 were used for further data analysis. Maps were developed using the tmap package in R (source: Chinese CDC, http://www.chinacdc.cn/).
We received the approval of the Ethics Committee of the National Institute for Communicable Disease Control and Prevention at the Chinese CDC (http://www.chinacdc.cn/) to access the data and we anonymized it.
RESULTS
Incidence and mortality rate.
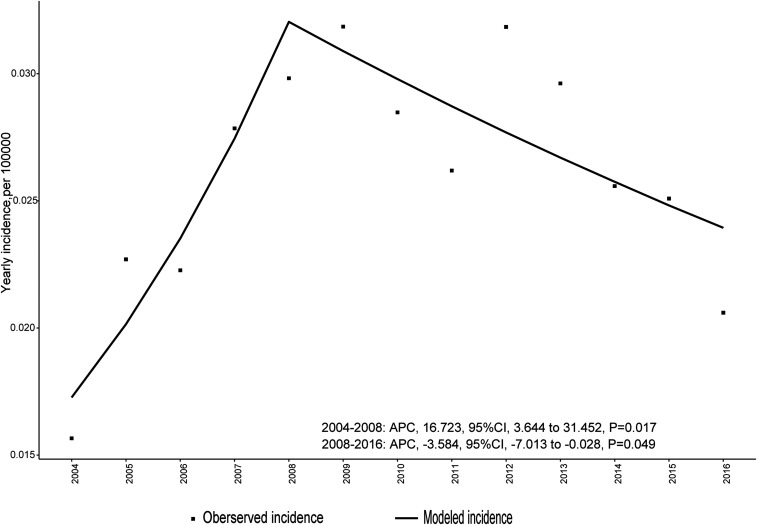
In the period 2004–2016, there were 4,519 cases of leprosy across the 28 provinces, municipalities, and autonomous regions, and the total incidence was 0.02815 (per 100,000 individuals), with 21 deaths reported. The average number of cases per year was 347.6. The overall incidence of leprosy showed an inverted “V” distribution (i.e., an increase followed by a decrease, Figure 1 and Table 1). From 2004 to 2008, the incidence showed a gradual upward trend, and it peaked in 2008. From 2008, the incidence slowly declined. However, the overall trend was relatively stable (AAPC = 2.8, 95% CI = −1.2 to 6.9, P = 0.200).
Figure 1.
Trends in the incidence of leprosy by year over the period 2004–2016 in China.
Table 1.
Incidence/rate of leprosy and number of leprosy-related deaths in 2004–2016 in China
| Year | No. of patients | Incidence (1/100,000) | No. of deaths |
|---|---|---|---|
| 2004 | 203 | 0.01566 | 2 |
| 2005 | 296 | 0.02270 | 3 |
| 2006 | 292 | 0.02227 | 3 |
| 2007 | 367 | 0.02785 | 2 |
| 2008 | 395 | 0.02982 | 1 |
| 2009 | 424 | 0.03185 | 0 |
| 2010 | 381 | 0.02848 | 4 |
| 2011 | 352 | 0.02619 | 0 |
| 2012 | 430 | 0.03184 | 3 |
| 2013 | 402 | 0.02962 | 2 |
| 2014 | 349 | 0.02558 | 0 |
| 2015 | 344 | 0.02509 | 1 |
| 2016 | 284 | 0.0206 | 0 |
| Total | 4,519 | 0.3378 | 21 |
Incidence (per 100,000) is calculated as the number of new cases of leprosy per year divided by the mid-year population size.
Regional distribution.
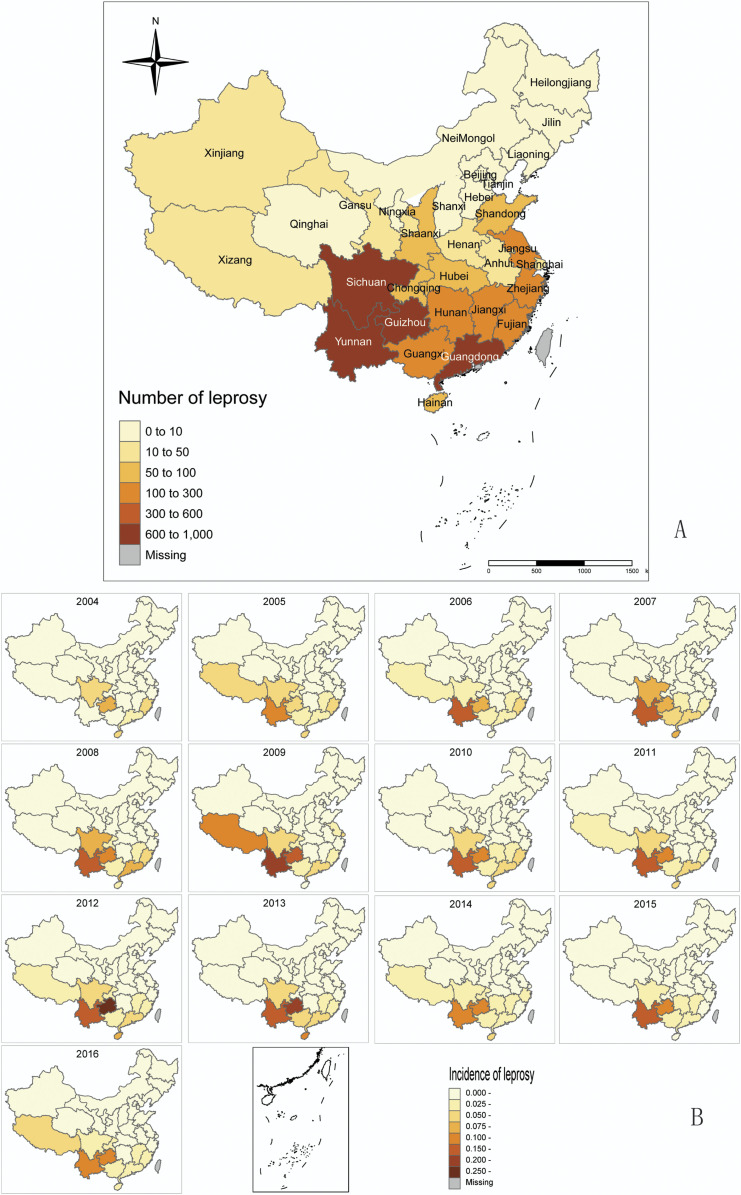
The incidence of leprosy in southern China is higher than that in northern China (P = 0.000). Yunnan (918 cases), Sichuan (661 cases), Guangdong (660 cases), Guizhou (616 cases), and Guangxi (250 cases) were the top five regions with the highest incidence rates. They were followed by some areas in the southeast, and the lowest incidence rates were found in the northeastern provinces. NingXia Hui Autonomous Region, Inner Mongolia Autonomous Region, and Heilongjiang Province did not report any cases during the study period (Figure 2). Yunnan and Guizhou had the highest incidence rates. The top five regions with the highest incidence rates accounted for 68.7% of the total cases. The southeastern coastal areas were also among the regions where the number of cases was relatively concentrated.
Figure 2.
Distribution of leprosy cases in different regions of China. (A) Distribution of leprosy cases in different provinces of China from 2004 to 2016. (B) Annual distribution of leprosy cases in different provinces of China from 2004 to 2016. This figure appears in color at www.ajtmh.org.
In the study period (2004–2016), the number of cases in each region was between 0 and 103. Furthermore, the number of cases in most regions in China was less than 10, and the regions with less than 10 cases between 2004 and 2016 included Beijing, Gansu, Hebei, Henan, Hubei, Jilin, Liaoning, Qinghai, Shanxi, Shannxi, Tianjin, Xizang, and Xinjiang.
Gender, age, and occupational distribution.
Of the 4,519 patients with leprosy in China reported in the study period, 3,209 (71.1%) were male and 1,310 (28.9%) were female.
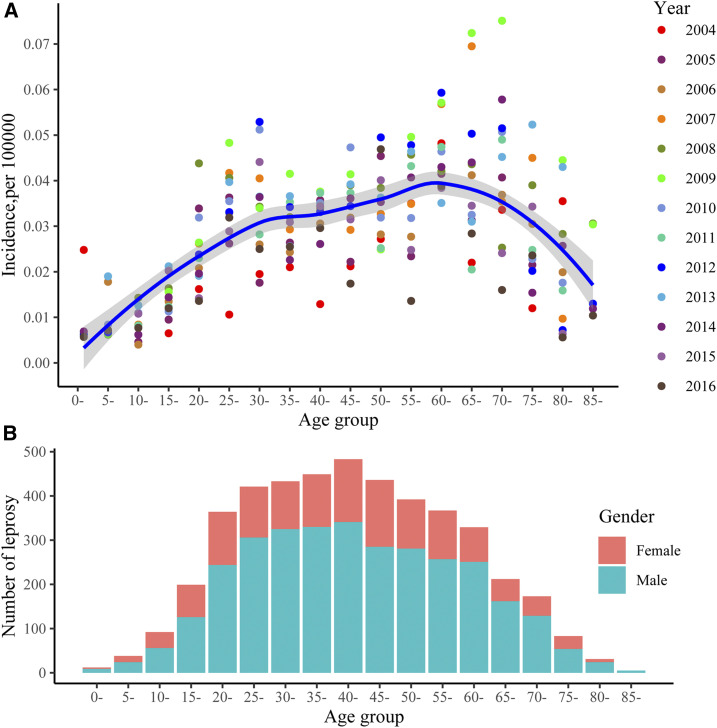
From 2004 to 2016, 341 new cases of leprosy in children who were < 15 years old were reported, and these accounted for 7.6% of the total cases. There were 2,586 cases among 15- to 44-year-olds, who accounted for 57.2% of the cases; 212 cases in 45- to 65-year olds, who accounted for 4.7% of the total cases; and 292 cases among those above 65 years, who accounted for 6.5% of the patients. Thus, the patients were mainly concentrated between the ages of 15 and 44 years (Figure 3).
Figure 3.
Distribution of leprosy cases among different age-groups in China from 2004 to 2016. This figure appears in color at www.ajtmh.org.
Table 2 shows the incidence of leprosy according to occupation. Peasants accounted for 71.7% of the leprosy cases, whereas kindergarten children accounted for 5%.
Table 2.
Distribution of leprosy patients according to occupation
| Occupation | Case no. | Percentage |
|---|---|---|
| Peasant | 3,241 | 71.72 |
| Worker | 210 | 4.65 |
| Houseworker or unemployed | 201 | 4.45 |
| Student | 186 | 4.12 |
| Migrant worker | 181 | 4.01 |
| Others | 124 | 2.74 |
| Unknown | 102 | 2.26 |
| Retiree | 72 | 1.59 |
| Commercial waiter | 70 | 1.55 |
| Scattered children | 32 | 0.71 |
| Cadre staff | 23 | 0.51 |
| Teacher | 18 | 0.40 |
| Fisherman | 15 | 0.33 |
| Caterer | 14 | 0.31 |
| Herdsman | 12 | 0.27 |
| Medical staff | 6 | 0.13 |
| Kindergarten children | 5 | 0.11 |
| Seafarers and long-distance drivers | 4 | 0.09 |
| Waiter in public place | 2 | 0.04 |
| Children’s nurse | 1 | 0.02 |
| Total | 4,519 | 100.00 |
DISCUSSION
Despite its worldwide prevalence, leprosy is still a poorly understood disease. Although the global incidence has significantly decreased over the years, in many areas where leprosy is endemic, the incidence of the disease has not decreased significantly over the past decade. Moreover, among the millions of people who have been cured with multidrug therapy, a large number of patients still suffer from long-term complications, including permanent and temporary deformity, disability, and social stigma.
The incidence of leprosy has remained low in China in recent years, but the morbidity rates throughout the tropical zone are still significant. In 2011, the “Programme for the Elimination of Leprosy in China 2011–2020” was launched to aid professional training, early detection, and supervision of treatment, and to integrate information-specific information, education, and communication.13 The program was built on two specific objectives: halving the total number of cases in 2010 by 2020 (i.e., 3,300) and reducing the prevalence to below 1/100,000 in 98% of the counties.13 The first goal (i.e., reducing the number of cases to 3,230) was achieved in 2015. To achieve the second goal, we need to know more about the trends and characteristics of leprosy in China and develop prevention and control measures for these characteristics. The present study sought to gather and analyze this information related to leprosy trends.
In the study period, that is, 2004–2016, the total incidence of leprosy in China was 0.02815 (per 100,000 individuals), which is below 1/100,000, and the overall trend was relatively stable. Since 2004, the incidence of leprosy showed a gradual upward trend. This trend is mainly attributable to the following two reasons. First, as the notifiable disease reporting method switched from paper-based reporting to internet-based reporting, the timeliness of reporting has improved. Second, the technological improvements in diagnosis through advances in laboratory detection and case identification methods might have led to an increase in detection and, thus, incidence. After 2008, the incidence of leprosy slightly decreased. Various strategies have been implemented to prevent the spread of infectious diseases after the SARS epidemic in China. These strategies include improvements in early surveillance and warning with enhanced screening. Moreover, major special national science and technology projects on prevention and control were launched at the end of 2008.
In general, the overall leprosy incidence in China is low, but it is widely distributed. In the past 13 years, only three regions have not reported new cases. In addition, its distribution is extremely unbalanced, as it is concentrated in the southwest and south-central regions, especially Yunnan, Sichuan, Guangdong, Guizhou, and Guangxi. This is in agreement with previous studies.4,14 The high incidence in these five regions may be related to the high population density to some extent. Yunnan, Sichuan, and Guangxi are ethnically diverse, mountainous, and underdeveloped areas. The high prevalence of leprosy in Yunnan may be related to the socioeconomic level to some extent.
Exposure to M. leprae alone is not enough to cause leprosy. The involvement of a genetic susceptibility factor is highly likely to be one of the reasons for clinical leprosy.15 Currently, a few common risk variants (genes/proteins) have been discovered in the Chinese Han population by genome-wide association studies.16–19 The HLA-DRB1*13 allele was found to be associated with leprosy in the Liangshan Yi Autonomous Region of Sichuan Province.20 To further understand genetic susceptibility to leprosy, more genome-wide association studies should be performed in ethnic minority areas that are highly endemic (such as Buyi and Miao Autonomous Prefecture in Guizhou Province21).
A factor that shapes the epidemiological portrait of leprosy is movement of peoples around the globe and within nations; in fact, migration22 presents unique challenges to leprosy control in the twenty-first century.22,23 Historical evidence shows that leprosy spread from India to China around 500 BC24 and that the disease has been endemic in China for more than 2000 years. As China is adjacent to India, Myanmar, and Nepal, which belong to the 23 priority countries, the import of leprosy cases is highly likely. In particular, the regions that border these five countries should be on alert to prevent cross-provincial importation.
The focus of leprosy control should be the 15–44 year age-group, which accounts for 57.2% of the total cases. Therefore, individuals belonging to these age-groups are at high risk of leprosy. This is probably because those in this age-group have a wide range of social activities, greater mobility, and lesser knowledge about the disease. The monitoring of such populations should be strengthened in the future. In most Asian countries, male patients outnumber females, whereas in Africa, leprosy affects women more than men.25 For example, women in Bangladesh26 and Nigeria27 were less aware of causation and had fewer opportunities to access medical services than men. A research in Sichuan Province in China showed that more men were diagnosed with leprosy than women; this might be due to the fact that women mostly stayed at home and received less health-related information.28 This may also explain why there were more male patients than female patients in our study. Therefore, it is necessary to strengthen community health education to improve women’s awareness of leprosy. Moreover, women with suspected leprosy should be encouraged to actively detect the early symptoms of leprosy and then report to the doctor for treatment. In addition, the present findings indicate that peasants are the main occupational group affected by leprosy; therefore, monitoring should be strengthened in this group.
Delayed diagnosis and misdiagnosis of leprosy have always been the problems, as there is a lack of quick and accurate detection methods for diagnosis. Monitoring for early symptoms is an effective approach to eliminate and control leprosy in the future. The current strategy for leprosy control in China is based on multidrug therapy, as recommended by the WHO in 1982. Combination therapy with dapsone, rifampicin, and clofazimine is recommended for the treatment of multibacillary leprosy, whereas therapy with dapsone and rifampicin is recommended for paucibacillary leprosy. Moreover, ofloxacin is a key drug in the treatment of single-lesion leprosy cases and drug-resistant cases.29 However, drug-resistant cases emerged after combination chemotherapy was started, and this resulted in increased difficulty in treatment and control of the disease.
There are several limitations to the study. For one, the incidence of leprosy could have been underestimated because of under-diagnosis and under-reporting, as individuals with mild symptoms may not consult medical institutions and their data may not be entered into the system. In addition, as disability grades are not provided in the available data, it is difficult to analyze the data in more detail.
Financial support:
This work was supported by the Major Project of the Thirteenth Five Year Special for Infectious Diseases of China (grant no. 2018ZX10101002).
REFERENCES
- 1.Britton WJ, Lockwood DN, 2004. Leprosy. Lancet 363: 1209–1219. [DOI] [PubMed] [Google Scholar]
- 2.Pettit JH, Rees RJ, 1964. Sulphone resistance in leprosy. An experimental and clinical study. Lancet 2: 673–674. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization , 2019. Global leprosy update, 2018: moving towards a leprosy-free world. Weekly Epidemiol Rec 94: 389–421. [Google Scholar]
- 4.Long S, Yu M, Yan L, Zhang G, Sun P, 2017. Epidemiological features of leprosy in China from 2011 to 2015. Chin J Dermatol 50: 400–403. [Google Scholar]
- 5.Chen XS, Li WZ, Jiang C, Ye GY, 2001. Leprosy in China: epidemiological trends between 1949 and 1998. Bull World Health Organ 79: 306–312. [PMC free article] [PubMed] [Google Scholar]
- 6.Shen J, Zhang G, Chen X, Zhou M, Yu M, Yan L, 2008. A long-term evolution on the epidemiological characteristics of leprosy, towards the goal of its elimination in 1949–2007 in China. Zhonghua Liu Xing Bing Xue Za Zhi 29: 1095–1100. [PubMed] [Google Scholar]
- 7.Qian MB, Chen J, Bergquist R, Li ZJ, Li SZ, Xiao N, Utzinger J, Zhou XN, 2019. Neglected tropical diseases in the People’s Republic of China: progress towards elimination. Infect Dis Poverty 8: 86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen L, Shi W, Chen Q, 2018. Research progress on leprosy in domestic and foreign countries. J Public Health Prev Med 29: 79–81. [Google Scholar]
- 9.Gootz TD, Barrett JF, Sutcliffe JA, 1990. Inhibitory effects of quinolone antibacterial agents on eucaryotic topoisomerases and related test systems. Antimicrob Agents Chemother 34: 8–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gonzalez AB, Maestre JL, Hernandez O, Columbie Y, Atrio N, Martin M, Fernández AM, Rodríguez J, 1993. Survey for secondary dapsone and rifampicin resistance in Cuba. Lepr Rev 64: 128–135. [DOI] [PubMed] [Google Scholar]
- 11.Wang L, Wang Y, Jin S, Wu Z, Chin DP, Koplan JP, Wilson ME, 2008. Emergence and control of infectious diseases in China. Lancet 372: 1598–1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim HJ, Fay MP, Feuer EJ, Midthune DN, 2000. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med 19: 335–351. [DOI] [PubMed] [Google Scholar]
- 13.National Health and Family Planning Commission of the People’s Republic of China , 2019. Implementation Plan on the Programme on the Elimination of Leprosy Damage in China (2012–2020). Available at: http://www.nhc.gov.cn/wjw/gfxwj/201304/d1dfccbb4007487da1897f625aae671a.shtml. Accessed October 16, 2020. [Google Scholar]
- 14.Yu MW, Yan LB, Shen JP, Sun YM, Zhang GC, 2010. Epidemiological analysis on leprosy in China, 2009. Zhonghua Liu Xing Bing Xue Za Zhi 31: 1155–1157. [PubMed] [Google Scholar]
- 15.Fava VM, Dallmann-Sauer M, Schurr E, 2020. Genetics of leprosy: today and beyond. Hum Genet 139: 835–846. [DOI] [PubMed] [Google Scholar]
- 16.Liu H, et al. 2017. Genome-wide analysis of protein-coding variants in leprosy. J Invest Dermatol 137: 2544–2551. [DOI] [PubMed] [Google Scholar]
- 17.Wang Z, et al. 2018. Discovery of 4 exonic and 1 intergenic novel susceptibility loci for leprosy. Clin Genet 94: 259–263. [DOI] [PubMed] [Google Scholar]
- 18.Wang D, et al. 2018. Mis-sense variants in HIF1A and LACC1 contribute to leprosy risk in Han Chinese. Am J Hum Genet 102: 794–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang X, et al. 2019. Meta-analysis identifies major histocompatiblity complex loci in or near HLA-DRB1, HLA-DQA1, HLA-C as associated with leprosy in Chinese Han population. J Investig Dermatol 139: 957–960. [DOI] [PubMed] [Google Scholar]
- 20.Chong M, et al. 2019. Study on the association between HLA- DRB1 and HLA-DQB1 loci, and leprosy susceptibility in Yi nationality, Sichuan province, China. China J Lepr Skin Dis 27: 83–86. [Google Scholar]
- 21.Zhao T, Yang C, Zhou C, Lai Y, Li J, 2018. Awareness and acquisition of knowledge on leprosy in Qianxinan, Guizhou. China J Lepr Skin Dis 34: 278–281. [Google Scholar]
- 22.Kerr-Pontes LR, Montenegro AC, Barreto ML, Werneck GL, Feldmeier H, 2004. Inequality and leprosy in Northeast Brazil: an ecological study. Int J Epidemiol 33: 262–269. [DOI] [PubMed] [Google Scholar]
- 23.White C, Franco-Paredes C, 2015. Leprosy in the 21st century. Clin Microbiol Rev 28: 80–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Browne SG, 1985. The history of leprosy. Hastings RC, ed. Leprosy. Edinburgh, Scotland: Longman Group Ltd., 1–14. [Google Scholar]
- 25.Varkevisser CM, Lever P, Alubo O, Burathoki K, Idawani C, Moreira TM, Patrobas P, Yulizar M, 2009. Gender and leprosy: case studies in Indonesia, Nigeria, Nepal and Brazil. Lepr Rev 80: 65–76. [PubMed] [Google Scholar]
- 26.Richardus JH, Meima A, Croft RP, Habbema JD, 1999. Case detection, gender and disability in leprosy in Bangladesh: a trend analysis. Lepr Rev 70: 160–173. [DOI] [PubMed] [Google Scholar]
- 27.Ebeigbe JA, Kio F, 2011. Ocular leprosy in institutionalized Nigerian patients. Ghana Med J 45: 50–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liu YY, Yu MW, Ning Y, Wang H, 2018. A study on gender differences in newly detected leprosy cases in Sichuan, China, 2000–2015. Int J Dermatol 57: 1492–1499. [DOI] [PubMed] [Google Scholar]
- 29.Yang WZ, 2019. Dramatic achievements in infectious disease prevention and treatment in China during the past 70 years. Zhonghua Liu Xing Bing Xue Za Zhi 40: 1493–1498. [DOI] [PubMed] [Google Scholar]