Abstract.
In French Guiana, a French overseas region partly located in the Amazon, “Africanized” bees, a hybrid species of Brazilian bees known as “killer bees,” have been observed since 1975. Since then, several cases requiring long hospitalization times have been described, allowing for a better understanding of the physiopathological mechanisms of this particular envenomation. Here, we report on a series of 10 cases of patients simultaneously attacked by hundreds of killer bees and immediately treated by a prehospital medical team already on site. Between 75 and 650 stingers were removed per victim. The reference treatment for anaphylaxis using intramuscular injection of epinephrine, vascular filling, and oxygen therapy was administered to all patients without delay. A clinical description was provided, and biological tests were performed immediately after the envenomation. We therefore observe the existence of a two-phase, medically well-controlled systemic toxic reaction. Thus, all our patients left the hospital after 44 hours of monitoring with no complications or sequelae, despite levels of intoxication described as potentially fatal elsewhere in the literature.
INTRODUCTION
“Killer bees,” observed since 1975 in French Guiana, a French overseas region partly located in the Amazon, are known to regularly provoke swarm attacks involving several hundred individuals in populations throughout the Americas.1–5 There is a risk of systemic toxic reaction from as few as 50 stings for an adult, and the median lethal dose is 19 stings/kg.6
Here, we describe the immediate clinical symptoms and early biological disorders following a swarm attack by hundreds of Africanized bees on a group of 10 healthy adult men. To our knowledge, no collective attack of this magnitude has been reported thus far.
The reference treatment using intramuscular epinephrine injection, vascular filling, and oxygen therapy was administered to all patients without delay. The objective of this article is to highlight the prompt recovery of our 10 patients and to clinically and biologically describe the biphasic reaction of massive envenomation by bee venom treated immediately according to the international recommendations for anaphylaxis.7–9
CASES DESCRIPTION
In Cayenne, French Guiana, at 3:00 pm, 10 male police officers were attacked by hundreds of killer bees during an intervention on the edge of the Amazon forest, less than 1 km from the nearest houses. The incidental presence of a Cayenne hospital mobile emergency unit on site made it possible to provide emergency care without any response times. Because of signs of anaphylaxis (Figure 1), each of them immediately received an intramuscular (IM) injection of epinephrine 1 mg, combined with oxygen therapy using high-concentration masks befitting their blood oxygen saturation levels, vascular filling with a NaCl 0.9% solution, and an intravenous injection of 2 mg/kg of methylprednisolone and 5 mg of polaramine (dexchlorpheniramine).
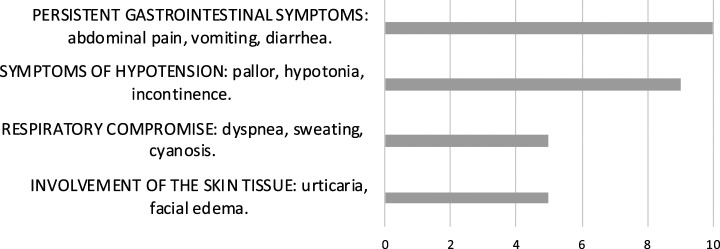
Figure 1.
Frequency of symptoms reported immediately after envenomation by the 10 patients and the on-site physicians.
During the first hour, five patients improved rapidly, whereas the other five required a second IM injection of epinephrine 1 mg. One patient required a third dose.
Once stabilized, all 10 patients were evacuated to the Cayenne hospital. In the emergency department, between 75 and 650 stingers were removed per victim. Most were located on their arms, head, neck, and abdomen. The victims were male, aged between 22 and 52 (median age = 27) years, weighing between 71 and 97 (median weight = 82) kg, with no medical history.
Two hours after envenomation, all the patients suffered from digestive symptoms (nausea, vomiting, and abdominal pain), which disappeared within 24 hours with intravenous symptomatic treatment: 120 mg of phloroglucinol, 4 g of paracetamol, and 30 mg of metoclopramide. Electrocardiograms were all normal. Breathing improved rapidly, and oxygen support was stopped within the first 24 hours.
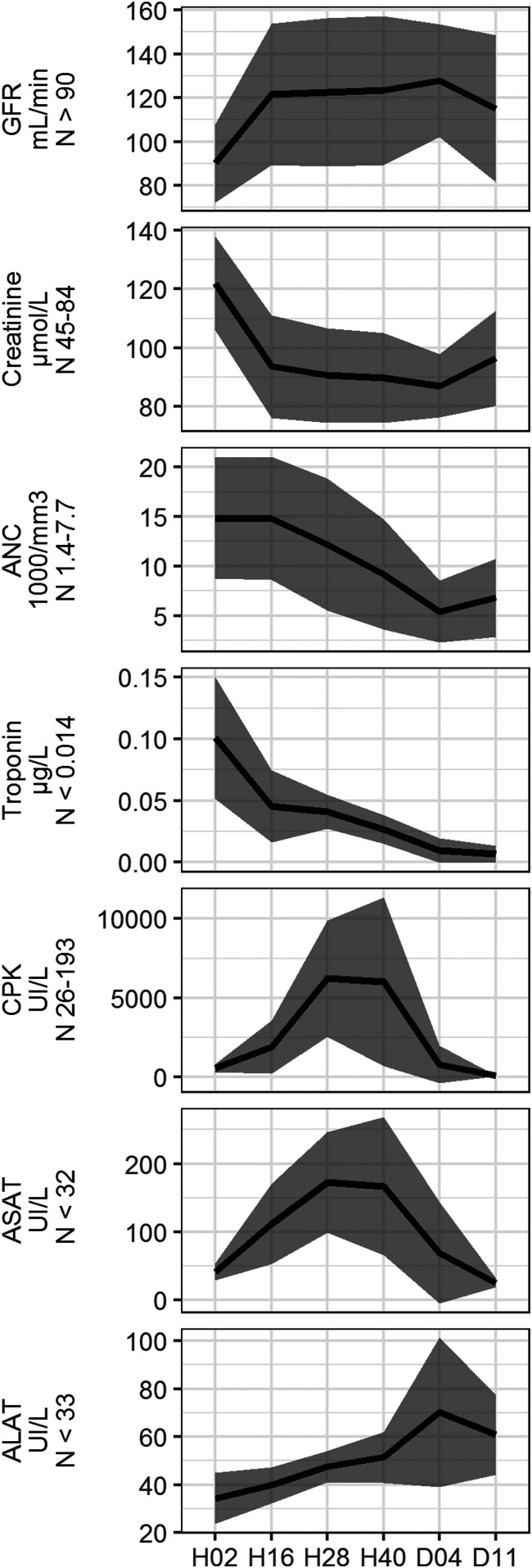
Four blood tests were performed per patient at 2 hours (H2), 10 hours (H10), 16 hours (H16), and 40 hours (H40) after envenomation. A first biological phase, characterized by moderate acute renal failure, an increase in troponins and an inflammatory syndrome peaked at H2 and gradually normalized after H16. From H16 onward, a second phase peaked at H28 and normalized after day 4, showing an increase in creatinine kinase (CK) associated with an increase in aspartate aminotransferase (AST) and alanine aminotransferase (ALT) (Figure 2).
Figure 2.
Mean kinetics of seven biological parameters, suggesting two phases before and after 16 hours (mean and SD for the 10 patients hospitalized). From top to bottom: glomerular filtration rate (GFR), creatinine, neutrophils (ANC), troponin, creatine phosphokinase (CPK), aspartate aminotransferase (AST), and alanine aminotransferase (ALT).
After 44 hours of hyperhydration with a NaCl 0.9% solution at 3 L/24 hours, all 10 patients were discharged with an oral prescription of 5 mg/day of dexchlorpheniramine, 1 mg/kg/day of prednisolone, 4 g/day of paracetamol, and antiseptic cleanser for local application. A medical, clinical, and biological checkup carried out on day 4 (D4) and day 11 (D11) did not reveal any complications.
DISCUSSION
In French Guiana, located within the Intertropical Convergence Zone, all local bees have been Africanized since the arrival of the “killer bees” in 1975.10 Killer bee venom, composed of 102 proteins and peptides, is no different from that of European bees.11,12 But the release of a pheromone (2-heptanone) onto the skin of their target, in addition to that injected via the venom, emits a powerful alarm signal and causes swarm attacks involving hundreds of individuals.13 It is therefore the high dose of venom injected that makes these attacks so dangerous.
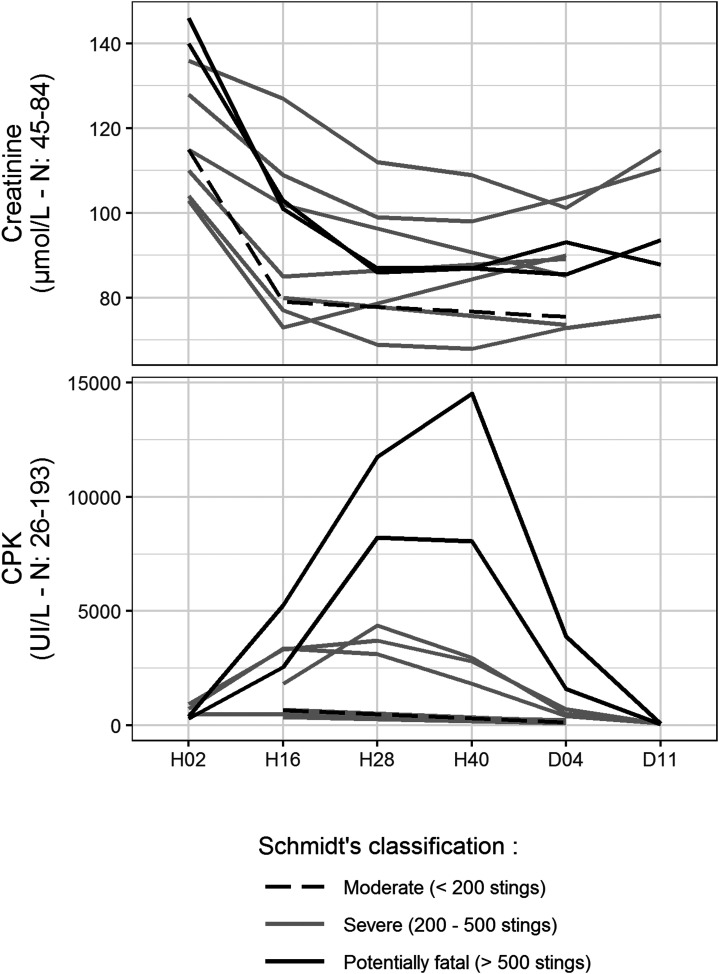
In 2018, Schmidt analyzed the cases reported in the Americas and defined three grades of severity of envenomation according to the number of stings: moderate from 50 to 200, severe from 200 to 500, and potentially fatal as of 500 stings.6 According to Schmidt’s classification, one of our patients with 75 stings fell within the category of moderate envenomation, seven patients with 200–500 stings fell within that of severe envenomation, and two patients with 600 and 650 stings fell within the clinical definition of potentially fatal envenomation.
In our cases, the immediate combination of clinical signs (Figure 1) allowed the on-site physician to diagnose anaphylaxis, according to the criteria put forward by Sampson et al.14 and based on American and European guidelines.7–9 The physician immediately administered epinephrine combined with isotonic saline vascular filling and oxygen therapy.
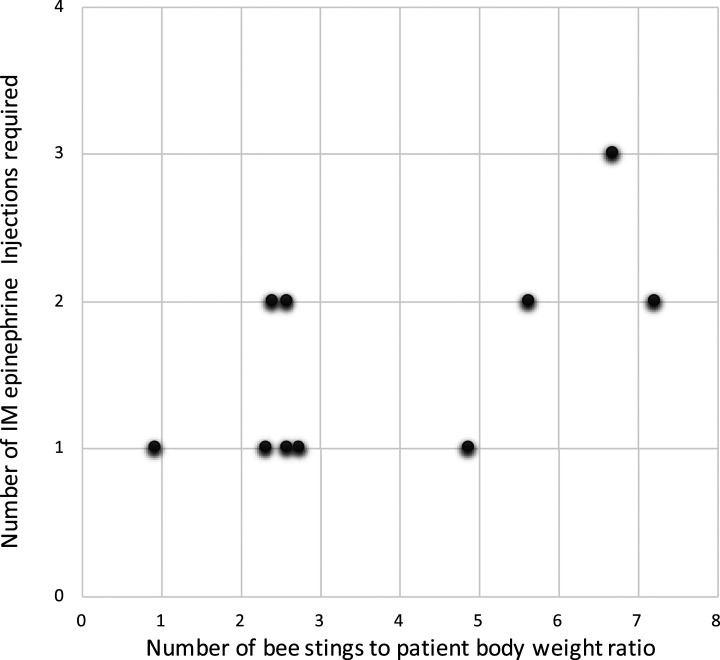
The clinically necessary epinephrine dose seemed to increase with the number of bee stings (Figure 3). This shows that the immediate systemic toxic reaction observed is caused by the high dose of venom injected. It was observed in our 10 patients with no known history of Hymenoptera allergy. It therefore does not require prior exposure and is not IgE-mediated. The early clinical signs are therefore caused by, on the one hand, mast cell degranulation due to the action of melittin and the “mast cell degranulation peptide” in the venom, and, on the other hand, the direct action of the biogenic amines in the venom.
Figure 3.
Scatterplot representing the number of intramuscular (IM) epinephrine injections required, as a function of the number of bee stings to patient body weight ratio.
Furthermore, according to Kounis, the degranulation of myocardial mast cells leads to coronary vasoconstriction and may explain the increase in troponin levels at H2.15 Twenty-eight hours later, we observe that aminotransferase (AST-ALT) and CK peak levels were significantly correlated with the number of stings (Table 1). This result suggests that a direct toxic mechanism causes rhabdomyolysis (Table 1). Among the components of venom, it is melittin and PLA2 that cause lysis of the muscle cell membranes.
Table 1.
Correlation between the number of stings and the peak value of biological parameters in the 10 patients hospitalized (lowest value for GFR).
| Parameter | Correlation coefficient | 95% CI | Correlation strength |
|---|---|---|---|
| Aspartate aminotransferase | 0.91 | (0.64–0.98) | High |
| Alanine aminotransferase | 0.89 | (0.58–0.97) | High |
| CPK | 0.87 | (0.54–0.97) | High |
| Troponin | 0.82 | (0.38–0.95) | Moderate |
| ANC | 0.69 | (0.10–0.92) | Low |
| Creatinine | 0.61 | (−0.03–0.90) | Low |
| GFR | −0.38 | (−0.81–0.33) | Low |
GFR = glomerular filtration rate.
In most cases described in the literature, acute renal failure ensues, requiring dialysis and hospitalization in the intensive care unit for several days.1,3,16–21 In accordance with American and European guidelines,7–9 the early administration of epinephrine via intramuscular injection at a dose of 10 µg/kg (repeated every 10–15 minutes until there is a response) to our 10 patients22 blocked mast cell activation, reduced the cascade of anaphylaxis mediators, and increased vascular resistance.
Thanks to this apt and immediate treatment, renal medullary ischemia due to anaphylaxis-induced hypovolemia was avoided. The initially impaired renal function rapidly returned to normal (H16) before the peak in rhabdomyolysis (H28) (Figure 4).
Figure 4.
Individual patient kinetics for creatinine (top) and creatine phosphokinase (CPK) (bottom) levels. Patients are grouped according to Schmidt’s classification of the severity of envenomation.
This allowed the renal system to progressively eliminate myoglobin, thus avoiding acute tubular necrosis due to its accumulation. Corticosteroids and antihistamines given in addition to epinephrine do not constitute emergency treatments to be used in cases of anaphylaxis. Their action is likely limited.23
CONCLUSION
In summary, our 10 patients suffered an anaphylactic-type reaction followed by a toxic reaction, which were treated early with prehospital medical care. Finally, our clinical and biological data suggest that an early injection of epinephrine combined with vascular filling prevented a chain reaction of acute functional renal failure, myoglobin accumulation, acute tubular necrosis, and acute organic renal failure. This observation is reinforced by the prompt recovery and absence of complications or death in our patient group, despite levels of envenomation described as potentially fatal elsewhere in the literature. This case demonstrates the importance of emergency treatment via IM epinephrine injection, available as a self-administered single-use autoinjector pen for use in the event of killer bee swarm attack.
REFERENCES
- 1.Pucca MB, Cerni FA, Oliveira IS, Jenkins TP, Argemí L, Sørensen CV, Ahmadi S, Barbosa JE, Laustsen AH, 2019. Bee updated: current knowledge on bee venom and bee envenoming therapy. Front Immunol 10: 2090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Costa AG, Chaves BA, Murta FLG, Sachett JAG, Sampaio VS, Silva VC, Monteiro WM, 2018. Hymenoptera stings in Brazil: a neglected health threat in Amazonas state. Revista da Sociedad e Brasileira de Medicina Trop 51: 80–84. [DOI] [PubMed] [Google Scholar]
- 3.Rahimian R, Shirazi FM, Schmidt JO, Klotz SA, 2020. Honeybee stings in the era of killer bees: anaphylaxis and toxic envenomation. Am J Med 133: 621–626. [DOI] [PubMed] [Google Scholar]
- 4.Marques MRV, Araújo KAM, Tavares AV, Vieira AA, Leite RS, 2020. Epidemiology of envenomation by Africanized honeybees in the state of Rio Grande do Norte, Northeastern Brazil. Rev Bras Epidemiol 23: e200005. [DOI] [PubMed] [Google Scholar]
- 5.Diniz AG, Belmino JF, Araújo KA, Vieira AT, Leite Rde S, 2016. Epidemiology of honeybee sting cases in the state of Ceara, Northeastern Brazil. Rev Inst Med Trop Sao Paulo 58: 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schmidt JO, 2018. Clinical consequences of toxic envenomations by Hymenoptera. Toxicon 150: 96–104. [DOI] [PubMed] [Google Scholar]
- 7.Campbell RL, Hagan JB, Manivannan V, Decker WW, Kanthala AR, Bellolio MF, Smith VD, Li JTC, 2012. Evaluation of National institute of allergy and infectious diseases/food allergy and anaphylaxis network criteria for the diagnosis of anaphylaxis in emergency department patients. J Allergy Clin Immunol 129: 748–752. [DOI] [PubMed] [Google Scholar]
- 8.Muraro A, Roberts G, Worm M, Bilò MB, 2014. Anaphylaxis: guidelines from the European academy of allergy and clinical immunology. Allergy 69: 1026–1045. [DOI] [PubMed] [Google Scholar]
- 9.Gloaguen A, Cesareo E, Vaux J, Valdenaire G, Ganansia O, Renolleau S, Pouessel G, Beaudouin E, Lefort H, Meininger C, 2016. Management of anaphylaxis in emergency medicine. French society of emergency medicine (SFMU) guidelines with the contribution of French allergology society (SFA) and the French speaking group in pediatric intensive care and emergency (GFRUP), and the support of the French pediatric pneumology and allergology society (SP2A). Ann françaises de médecine d’urgence 6: 342–364. [Google Scholar]
- 10.Winston ML, 1992. The biology and management of Africanized honey bees. Annu Rev Entomol 37: 173–193. [Google Scholar]
- 11.Schumacher MJ, Egen NB, 1995. Significance of Africanized bees for public health: a review. Arch Intern Med 155: 2038–2043. [PubMed] [Google Scholar]
- 12.Van Vaerenbergh M, Debyser G, Devreese B, de Graaf DC, 2014. Exploring the hidden honeybee (Apis mellifera) venom proteome by integrating a combinatorial peptide ligand library approach with FTMS. J Proteomics 99: 169–178. [DOI] [PubMed] [Google Scholar]
- 13.Faita MR, Colman Carvalho RMM, Alves-Junior VV, Chaud-Netto J, 2014. Defensive behavior of Africanized honeybees (Hymenoptera: Apidae) in Dourados-Mato Grosso do Sul, Brazil. Revista Colombiana de Entomología 40: 235–240. [Google Scholar]
- 14.Sampson HA, et al. 2006. Second symposium on the definition and management of anaphylaxis: summary report — second national institute of allergy and infectious disease/food allergy and anaphylaxis network symposium. J Allergy Clin Immunol 117: 391–397. [DOI] [PubMed] [Google Scholar]
- 15.Kounis NG, 2013. Coronary hypersensitivity disorder: the Kounis syndrome. Clin Ther 35: 563–572. [DOI] [PubMed] [Google Scholar]
- 16.Hommel D, Bollondard F, 1998. Multiple African honeybee stings and acute renal failure. Nephron 78: 235–236. [DOI] [PubMed] [Google Scholar]
- 17.Le Borgne A, 1998. Envenimations par piqûres multiples d’abeilles africanisées: revue à propos de cinq cas hospitalisés dans le service de réanimation du C. H. de Cayenne. Thèse de doctorat en médecine, Faculté de Brest, Brest, France. [Google Scholar]
- 18.Hughes RL, 2019. A fatal case of acute renal failure from envenoming syndrome after massive bee attack: a case report and literature review. Am J Forensic Med Pathol 40: 52–57. [DOI] [PubMed] [Google Scholar]
- 19.Worm M, et al. 2014. First European data from the network of severe allergic reactions (NORA). Allergy 69: 1397–1404. [DOI] [PubMed] [Google Scholar]
- 20.Grisotto LS, Mendes GE, Castro I, 2006. Mechanisms of bee venom-induced acute renal failure. Toxicon 48: 44–54. [DOI] [PubMed] [Google Scholar]
- 21.Malik GH, 1998. Rhabdomyolysis and myoglobin-induced acute renal failure. Saudi J Kidney Dis Transplant 9: 273–284. [PubMed] [Google Scholar]
- 22.Ring J, Klimek L, Worm M, 2018. Adrenaline in the Acute Treatment of Anaphylaxis. Dtsch Arztebl Int 115: 528–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Simons FE, et al. 2014. International consensus on (ICON) anaphylaxis. World Allergy Organ J 7: 9. [DOI] [PMC free article] [PubMed] [Google Scholar]