Abstract.
We evaluated the performance of a commercial rapid diagnostic test (RDT) in a field setting for the diagnosis of abdominal cystic echinococcosis (CE) using sera collected during an ultrasound population screening in a highly endemic region of the Peruvian Andes. Abdominal CE was investigated by ultrasonography. Sera collected from individuals with abdominal CE (cases) and age- and gender-matched volunteers with no abdominal CE (controls) were tested independently in two laboratories (Peru and Italy) using the VIRapid® HYDATIDOSIS RDT and RIDASCREEN® Echinococcus IgG enzyme-linked immunosorbent assay. Performance indexes of single and serially combined tests were calculated and applied to hypothetical screening and clinical scenarios. Test concordance was also evaluated. Prevalence of abdominal CE was 6.00% (33 of 546) by ultrasound. Serum was obtained from 33 cases and 81 controls. The VIRapid test showed similar sensitivity (76% versus 74%) and lower specificity (79% versus 96%) than results obtained in a hospital setting. RDTs showed better performance when excluding subjects reporting surgery for CE and if weak bands were considered negative. Concordance between tests was moderate to very good. In hypothetical screening scenarios, ultrasound alone or confirmed by RDTs provided more reliable prevalence figures than serology alone, which overestimated it by 5 to 20 times. In a simulation of case diagnosis with pre-test probability of CE of 50%, positive and negative post-test probabilities of the VIRapid test were 78% and 22%, respectively. The application of the VIRapid test alone would not be reliable for the assessment of population prevalence of CE, but could help clinical decision making in resource-limited settings.
INTRODUCTION
Cystic echinococcosis (CE) is a parasitic zoonosis caused by the larval stage of the cestode Echinococcus granulosus sensu lato, naturally transmitted between dogs and ungulates.1 Humans acquire the infection by ingestion of E. granulosus eggs shed through infected dog feces and contaminating the environment.2 In humans, the parasite larvae develop as fluid-filled cysts mainly in the liver and lungs.3 People can remain asymptomatic, or growing cysts may induce variable, sometimes life-threatening, clinical manifestations.4 CE is prevalent in rural livestock-raising areas worldwide.1 Its global burden has been estimated in more than 1 million disability-adjusted life years and more than USD2,000 million lost yearly in animal production, when accounting for underreporting of the condition.5 Latin America is among the regions where CE is most prevalent.6,7 In Peru, human prevalence reaches 5.5% to 9.3%.7–9
CE diagnosis is based on imaging. The WHO Informal Working Group on Echinococcosis (IWGE) ultrasound-based classification of CE cysts guides diagnosis and clinical management.4,10 Serology may complement CE diagnosis, but assays are non-standardized and often require infrastructures and training. Their results are influenced by several factors relating to the patient (cyst characteristics, previous treatment), the test (antigenic preparation, test format), and the underlying disease epidemiology.11–14 Therefore, serology alone is unreliable when estimating CE prevalence in population studies.13 In endemic, resource-limited settings, where ultrasound expertise is scant and the WHO-IWGE classification is scarcely known, a rapid diagnostic test (RDT) might be an appealing confirmatory test for cases suspected of CE on the basis of imaging. Several reports described the performance of commercial and experimental RDTs for the diagnosis of CE.14–18 However, all previously published studies were hospital based, and several of them14–16,18 did not include control patients from an endemic area. This is relevant, because part of the false-positive results shown by serological assays may derive from a transient immunity after environmental exposure without cyst development or from cross-reactions with other parasitic diseases co-endemic in the area.19 We present the first performance evaluation of a commercial RDT in a field setting for the diagnosis of abdominal CE using sera collected during an ultrasound screening campaign in a highly endemic region of Peru.
MATERIALS AND METHODS
Study area and population.
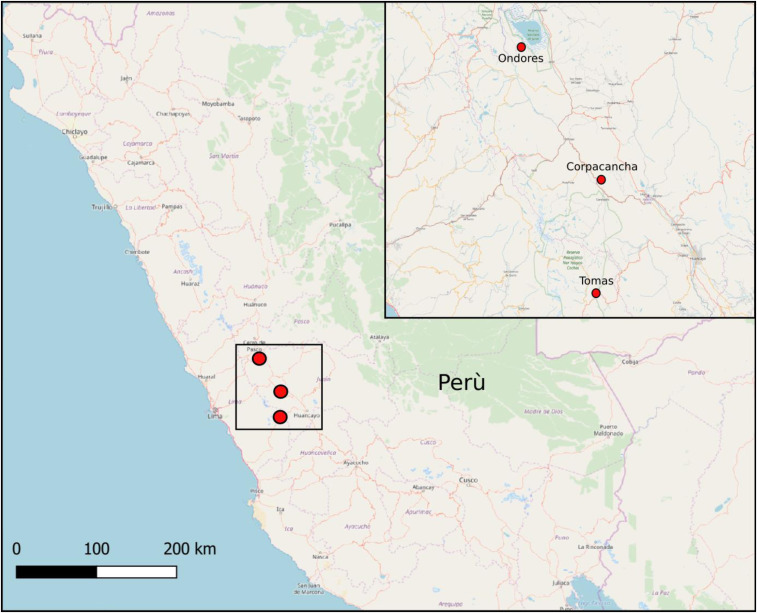
The study was approved by the ethics committee of the Universidad Peruana Cayetano Heredia (Lima, Peru), and consent was granted by community leaders of the Central Peruvian Highlands target communities: Ondores (Junin Region, Ondores District), Corpacancha (Junin Region, Marcapomacocha District), and Tomas (Yauyos Province, Tomas District) (Figure 1). Information about project activities and CE was provided to communities through primary care centers (PCCs) and radios in Quechua and Spanish. A census of the local population was carried out. The survey took place in October 2017. All people older than 5 years were invited to participate. Volunteers could pose questions about the study to a Spanish-speaking team member before signing the informed consent form (ICF). Parents or guardians signed the ICF for minor participants. All participants were asked about previous CE diagnosis and treatment.
Figure 1.
Map showing the study sites. This figure appears in color at www.ajtmh.org.
Ultrasonography.
Abdominal CE was investigated using portable ultrasound machines with convex probes: Mindray Z6 (Mindray, China), Samsung UGEO PT60A (Samsung, Seoul, South Korea) and Sonosite 180 (FUJIFILM Tokyo, Japan). Three expert physicians performed the examinations, and consensually identified and staged CE cysts according to the WHO-IWGE classification.4 Participants were informed about ultrasound results and were provided with a report in Spanish indicating whether they required further medical attention. In the case of abdominal CE, clinical management was suggested according to the WHO-IWGE expert consensus.4 Individuals requiring medical attention were addressed to the PCC’s officer for liaison with the national health system. Unfortunately, as a result of logistic constraints, it was impossible to perform chest radiography on the participants to rule out lung CE.
Serology.
Controls included volunteers matched for age and gender (±5 years) found to be negative for abdominal CE. The case to control ratio was around 1:3. Serum was aliquoted and frozen at –20°C until used. All samples were pseudonymized. One serum aliquot was tested using the VIRapid® HYDATIDOSIS (Vircell, Granada, Spain) test at the Instituto Peruano de Parasitologia Clinica y Experimental in Lima, Peru. The second aliquot was tested in San Matteo Hospital (Pavia, Italy) with the VIRapid test and the commercial enzyme-linked immunosorbent assay (ELISA) test RIDASCREEN® Echinococcus IgG (R-Biopharm AG, Darmstadt, Germany). All tests were performed according to the manufacturers’ instructions. For the VIRapid test, the reading of “weak band” results was noted for further analysis. The operators performing RDTs and ELISA tests were blind to sample classification and other test results.
Statistical analysis.
For the analysis, CE cysts were grouped into active (CE stage 1 [CE1], CE stage 2 [CE2], CE stage 3b [CE3b]), transitional (CE stage 3a [CE3a]), and inactive (CE stage 4 [CE4], CE stage 5 [CE5]).11 Furthermore, sera from patients carrying multiple cysts in different stages were classified according to the stage more likely associated with a positive serology. This decision was based on previous studies showing a correlation between cyst stage and serology results, with CE1, CE4, and CE5 showing lower seropositivity rates compared with CE2, CE3a, and CE3b.11,15,20 Thus, a person harboring two cysts—for example, one CE1 and one CE3b—would more probably have a positive serology associated with the CE3b stage, and as such was classified as CE3b.
For each test, sensitivity, specificity, negative predictive value, positive predictive value, positive likelihood ratio, and negative likelihood ratio were calculated. Individuals reporting a history of CE-related surgery but with no CE cyst on ultrasound were excluded from the analysis in a first scenario and included as controls in a second scenario. RDT weak-band positivity was also accounted for in two separate analyses, by considering the results either positive or negative. The performance of ultrasound and serology tests combined serially was also calculated.11 Sensitivity and specificity of different scenarios were compared using McNemar’s test. Diagnostic accuracy was assessed using a non-parametric approach for correlated receiver operating characteristic curves that allows one not to make assumptions on variable distributions.21 This method used the theory on generalized U statistics to generate an estimated covariance matrix, which allows not to make assumptions on distribution; concordance between tests was evaluated by Cohen’s kappa. Data were analyzed by STATA v. 15.0 (STATA Corp., College Station, TX).
Performance simulation.
To assess the potential performance of the large-scale use of the RDT based on our field results, we envisaged a hypothetical cross-sectional prevalence study of 5,000 people in areas where the hypothetical but plausible true prevalence of abdominal CE was 1% or 5%.13
Performance of ultrasonography was set at 0.98 sensitivity and 0.96 specificity in accordance with previously reported values.22 The VIRapid test performance values applied (sensitivity, 0.76; specificity, 0.79) were those resulting from the Lima setting, with individuals reporting surgery for CE but without current abdominal CE considered non-infected. This was chosen because, ideally, a test should result as negative in the case of a residual cavity.
RESULTS
Ultrasound survey.
Of the 1,246 people contacted, 546 (43.8%) participated in the screening: 227 (35%) in Ondores, 213 (60%) in Corpacancha, and 106 (30%) in Tomas. The median age of participants was 35 years (range, 5–87 years); 347 (63.5%) were female. The 33 (6.00%) people infected had a total of 63 CE cysts. We observed the greatest prevalence (13.6%, 29 of 213) in Corpacancha. Table 1 shows the anatomic localizations and stage distribution of the cysts.
Table 1.
Distribution of cystic echinococcosis cysts across abdominal organs and relative stages
| Abdominal organ | CE1, N (%) | CE2, N (%) | CE3a, N (%) | CE3b, N (%) | CE4, N (%) | CE5, N (%) | Total, N (%) |
|---|---|---|---|---|---|---|---|
| Liver | 13 (20.8) | 4 (6.4) | 8 (12.8) | 6 (9.6) | 18 (28.8) | 10 (16) | 59 (94.2) |
| Spleen | 0 (0) | 0 (0) | 0 (0) | 1 (1.6) | 1 (1.6) | 0 (0) | 2 (3.1) |
| Kidney | 1 (1.6) | 1 (1.6) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 2 (3.1) |
| Total | 14 (22.4) | 5 (8) | 8 (12.8) | 7 (11.2) | 19 (30.4) | 10 (16) | 63 (100.4) |
CE = cystic echinococcosis; CE1 = CE stage 1; CE2 = CE stage 2; CE3a = CE stage 3a; CE3b = CE stage 3b; CE4 = CE stage 4; CE5 = CE stage 5.
Eighteen participants had non-CE focal liver lesions (12 simple cysts, two hemangiomas, one suspect fascioliasis/larva migrans, and one complex liver cyst). Unfortunately, none of these could be tested by serology. The serum from one participant who had an abdominal cyst classified as a cystic lesion (suspect CE with no pathognomonic ultrasound features4) was not analyzed because we had no information on the final etiology of the lesion.
Thirty-three participants (6%) had a history of CE-related surgery: 21 of 33 (63.7%) in the liver, 10 of 33 (30.3%) in the lungs, and 2 of 33 (6.06%) in both liver and lungs. Among these individuals, five who had undergone lung surgery had abdominal CE cysts on ultrasound: four had liver CE cysts (N = 3 CE3a and N = 1 CE4) and one had a splenic CE3b cyst. No participant with a history of liver surgery still presented CE cysts on ultrasound.
Serology results.
Serum was obtained from 33 participants with and 81 volunteers without abdominal CE. Supplemental Table 1 shows VIRapid test results in individuals with CE divided by cyst stage. Table 3 shows the results of the three tests excluding patients with a history of surgery for CE, whereas the results obtained including these patients as controls are provided in Table 2. Overall, the RDT diagnostic performance was better when subjects with a history of CE-related surgery were excluded from the analysis. This was expected because false-positive results in this group are likely due to the persistence of detectable antibody levels after treatment. The performance of the RDT was slightly better but not statistically different when applied in Lima, if weak bands in Pavia were considered negative. Specificity was significantly better in Lima compared with Pavia when weak bands in Pavia were considered positive (P < 0.001) (Supplemental Tables 3 and 4).
Table 3.
Area-under-the-curve values and concordance indexes excluding patients with a history of surgery for cystic echinococcosis and no abdominal cystic echinococcosis from analysis
| Tests | Weak bands positive | P value | Weak bands negative | P value |
|---|---|---|---|---|
| Lima RDT AUC | 0.79 | < 0.05 | 0.79 | 0.13 |
| Pavia RDT AUC | 0.63 | 0.71 | ||
| ELISA AUC | 0.71 | 0.71 | ||
| Test 1 | Test 2 | Cohen’s kappa (95% CI) | ||
| VIRapid®, Lima | VIRapid, Pavia (weak bands positive) | 0.557 (0.394–0.720) | ||
| VIRapid, Lima | VIRapid, Pavia (weak bands negative) | 0.689 (0.533–0.845) | ||
| ELISA | VIRapid, Lima | 0.598 (0.416–0.780) | ||
| ELISA | VIRapid, Pavia (weak bands positive) | 0.725 (0.578–0.872) | ||
| ELISA | VIRapid, Pavia (weak bands negative) | 0.920 (0.831–1.000) | ||
AUC = area under the curve; ELISA = enzyme-linked immunosorbent assay; RDT = rapid diagnostic test. Data obtained excludes post-surgical patients without abdominal cystic echinococcosis from analysis.
Table 2.
Serological results obtained, including post-surgical patients without abdominal cystic echinococcosis as controls
| VIRapid® test, Lima | VIRapid test, Pavia* (weak bands considered positive) | VIRapid test, Pavia* (weak bands considered negative) | ELISA RIDASCREEN test, Pavia‡ | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Performance (95% CI) | CE pos | CE neg | Total | Performance (95% CI) | CE pos | CE neg | Total | Performance (95% CI) | CE pos | CE neg | Total | Performance (95% CI) | CE pos | CE neg | Total |
| Test pos | 25 | 17 | 42 | Test pos | 24 | 37 | 61 | Test pos | 22 | 21 | 43 | Test pos | 18 | 23 | 41 |
| Test neg | 8 | 64 | 72 | Test neg | 9 | 43 | 52 | Test neg | 11 | 59 | 70 | Test neg | 9 | 51 | 60 |
| Total | 33 | 81 | 114 | Total | 33 | 80 | 113 | Total | 33 | 80 | 113 | Total | 27 | 74 | 101 |
| Sensitivity | 0.76 (0.67–0.83) | Sensitivity | 0.73 (0.63–0.81) | Sensitivity | 0.67 (0.57-0.75) | Sensitivity | 0.67 (0.57–0.76) | ||||||||
| Specificity | 0.79 (0.69–0.85) | Specificity | 0.54 (0.43–0.62) | Specificity | 0.74 (0.63–0.80) | Specificity | 0.69 (0.57–0.76) | ||||||||
| PPV | 0.59 (0.48–0.67) | PPV | 0.39 (0.30–0.48) | PPV | 0.51 (0.41–0.60) | PPV | 0.44 (0.33–0.53) | ||||||||
| NPV | 0.89 (0.81–0.94) | NPV | 0.83 (0.74–0.89) | NPV | 0.84 (0.76–0.90) | NPV | 0.85 (0.76–0.91) | ||||||||
| LR+ | 3.61 (2.72–4.27) | LR+ | 1.57 (0.14–2.06) | LR+ | 2.54 (1.84–3.20) | LR+ | 2.15 (1.51–2.80) | ||||||||
| LR– | 0.31 (0.25–0.39) | LR– | 0.51 (0.39–0.70) | LR– | 0.46 (0.35–0.61) | LR– | 0.48 (0.36–0.67) | ||||||||
CE = cystic echinococcosis; neg = negative; LR– = negative likelihood ratio; LR+ = positive likelihood ratio; NPV = negative predictive value; pos = positive; PPV = positive predictive value.
One serum from one post-surgical case with no abdominal cystic echinococcosis cyst at the time of screening was not available for analysis in Pavia.
Sera from three uninfected, four post-surgical, and six cystic echinococcosis (CE)-infected individuals (three CE stage 1, 1 one CE stage 3a, one CE stage 3b, and one CE stage 5) were not available for testing.
The ELISA test showed generally lower sensitivity and specificity than the RDT, but specificity was significantly greater compared with the RDT in Pavia when weak bands were considered positive (P = 0.001 and P = 0.003 if post-surgical cases without abdominal CE were analyzed as controls or excluded from the analysis, respectively) (Supplemental Tables 3 and 4).
Accuracy and concordance results are presented in Tables 3 and 4. Area-under-the-curve values improved slightly when post-surgical subjects were removed from the analysis, in accordance with results obtained for sensitivity and specificity. Areas under the curve in both cases differed significantly when weak bands were considered positive in Pavia. Concordance between tests as assessed using Cohen’s kappa coefficients was moderate to very good, and was greater if samples from post-surgical cases were excluded. Inter-laboratory results had the lowest concordance.
Table 4.
Area-under-the-curve values and concordance indexes for patients with a history of cystic echinococcosis surgery and no abdominal cystic echinococcosis in the control group
| Tests | Weak bands positive | P value | Weak bands negative | P value |
|---|---|---|---|---|
| Lima RDT AUC | 0.76 | < 0.05 | 0.76 | 0.13 |
| Pavia RDT AUC | 0.6 | 0.69 | ||
| ELISA AUC | 0.68 | 0.68 | ||
| Test 1 | Test 2 | Cohen’s kappa (95% CI) | ||
| VIRapid®, Lima | VIRapid, Pavia (weak bands positive) | 0.532 (0.386–0.677) | ||
| VIRapid, Lima | VIRapid, Pavia (weak bands negative) | 0.717 (0.584–0.850) | ||
| ELISA | VIRapid, Lima | 0.602 (0.443–0.762) | ||
| ELISA | VIRapid, Pavia (weak bands positive) | 0.686 (0.549–0.823) | ||
| ELISA | VIRapid, Pavia (weak bands negative) | 0.853 (0.749–0.958) | ||
AUC = area under the curve; ELISA = enzyme-linked immunosorbent assay; RDT = rapid diagnostic test. Data obtained include post-surgical patients without abdominal cystic echinococcosis (controls).
Simulation of performance of ultrasound and serology tests for abdominal CE diagnosis.
The expected results of hypothetical screening campaigns using ultrasonography alone, the VIRapid test alone, and ultrasonography followed by the VIRapid test in individuals with suggestive ultrasound imaging are summarized in Table 5. The use of serology alone would substantially overestimate disease prevalence compared with ultrasound alone. The performance of the RDT in individuals with possibly evocative lesions would slightly underestimate or overestimate the prevalence of CE, depending on the prevalence scenario.
Table 5.
The expected results of a hypothetical screening study for abdominal cystic echinococcosis using the VIRapid® test alone (+/−), ultrasonography alone (+/−), or the sequential application of ultrasonography followed by the VIRapid test only in individuals with evocative ultrasound imaging.
| VIRapid test alone | Ultrasonography alone | Ultrasonography followed by VIRapid test only in individuals with evocative abdominal lesions | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivity | 0.76 | Sensitivity | 0.98 | Net sensitivity | 0.74 | ||||||
| Specificity | 0.79 | Specificity | 0.96 | Net specificity | 0.99 | ||||||
| True prevalence, 5% | |||||||||||
| RDT+ | RDT– | Total | US+ | US– | Total | Test+ | Test– | Total | |||
| CE pos | 190 | 60 | 250 | CE pos | 245 | 5 | 250 | CE pos | 186 | 64 | 2,500 |
| CE neg | 998 | 3,753 | 4,750 | CE neg | 190 | 4,560 | 4,750 | CE neg | 40 | 4,710 | 4,750 |
| Total | 1,188 | 3,813 | 5,000 | Total | 435 | 4,565 | 5,000 | Total | 226 | 4,774 | 5,000 |
| PPV | 0.16 (0.15–0.17) | PPV | 0.56 (0.55–0.58) | PPV on US+ | 0.82 (0.78–0.86) | ||||||
| NPV | 0.98 (0.98–0.99) | NPV | 0.99 (0.99–1.00) | NPV on US+ | 0.72 (0.67–0.76) | ||||||
| Estimated prevalence | 23.8% | Estimated prevalence | 8.7% | Estimated prevalence | 4.52% | ||||||
| True prevalence, 1% | |||||||||||
| RDT+ | RDT– | Total | US+ | US– | Total | Test + | Test - | Total | |||
| CE pos | 38 | 12 | 50 | CE pos | 49 | 1 | 50 | CE pos | 37 | 13 | 50 |
| CE neg | 1,040 | 3,911 | 4,950 | CE neg | 198 | 4,752 | 4,950 | CE neg | 42 | 4.908 | 4.950 |
| Total | 1,078 | 3,923 | 5,000 | Total | 247 | 4,753 | 5,000 | Total | 79 | 4.921 | 5.000 |
| PPV | 0.03 (0.03–0.04) | PPV | 0.20 (0.19–0.21) | PPV on US+ | 0.47 (0.41–0.53) | ||||||
| NPV | 1.00 (0.99–1.00) | NPV | 1.00 (0.99–1.00) | NPV on US+ | 0.93 (0.89–0.96) | ||||||
| Estimated prevalence | 21.6% | Estimated prevalence | 4.94% | Estimated prevalence | 1.58% | ||||||
CE = cystic echinococcosis; neg = negative; NPV = negative predictive value; pos = positive; PPV = positive predictive value; RDT–, negative VIRapid test; RDT+ = positive VIRapid test; US– = negative ultrasonography; Test– = negative evocative ultrasound imaging; Test+ = evocative ultrasound imaging; US+ = positive ultrasonography.
DISCUSSION
We aimed to assess the performance of a commercial RDT (VIRapid HYDATIDOSIS), using samples collected in an endemic area, during an ultrasound screening for CE. Prevalence of abdominal CE was similar to that found in other areas of the Andes in Peru.8,9,23 In our hands, when tested using samples from selected patients in a controlled laboratory setting,14 the investigated RDT showed comparable sensitivity (74% versus 76%) and better specificity (96% versus 79%) than those obtained here. Similar sensitivities may depend on comparable distributions of CE cyst stages and localizations in both cohorts—two factors influencing the sensitivity of serodiagnostic tests.11,24 The lower specificity in this study is not surprising, considering the different control cohorts, hence the importance of evaluating test performance using control samples from endemic areas. False-positive serology results may derive from exposure to infection without development of cysts,19 from cross-reactions/non-specific reactions, from the use of control samples from people treated for CE still having detectable antibodies, and from patients with CE cysts only in extra-abdominal organs (e.g., lungs). This latter scenario may be particularly relevant in our study setting because a population study from the same area estimated that 20% of all CE infections were located in the lung.8 In our study, one third of patients reporting CE-related surgery had lung CE; however, this proportion cannot be used to infer the distribution of lung versus abdominal CE at population level. Lung CE is more commonly symptomatic than liver CE, making a larger proportion of lung CE patients seek medical attention, thus “overestimating” lung CE prevalence in comparison to abdominal CE.25 We could not assess the presence of lung CE by chest radiography; therefore, we could not identify how many individuals classified as false positive by serology were actually real positives. However, the sensitivity of serology in patients with lung CE is generally very low.8 Therefore, we can speculate that only a few results classified as false positive would correspond to people with isolated lung CE. This alone could not explain our results showing CE prevalence overestimation (5–20 times greater than the real one) in simulations in which the RDT was used alone.
Our study highlights the variable inter- and intra-laboratory concordance of test results, as already evidenced.24 Concerning RDTs, this may be the result of a subjective reading of weak bands, but also to batch-to-batch test variability. When the Pavia operator read the photos of the discordant RDTs performed in Lima (N = 29), only 60% (N = 17) of tests were interpreted by the Pavia operator in the same manner as the operator in Lima (data not shown). The introduction of tests based on recombinant antigens, and the application of training and standardized methods for the performance and reading of assays may improve this aspect. For the VIRapid HYDATIDOSIS test, excluding weak bands from positive readings, or at least their cautious interpretation, seems appropriate.
Point-of-care tools are particularly suitable in resource-poor settings. The use of serology alone for the assessment of CE prevalence is still diffuse, despite sound criticism.13 When applying the test performance values obtained in our field-based study to two hypothetical but plausible screening scenarios, serology alone overestimated prevalence figures dramatically compared with ultrasound alone or in combination with the RDT applied only to imaging-positive cases, as also shown previously.23,26,27 Unfortunately, it was not possible to perform a rigorous assessment of pre- and post-test probabilities of the RDT when applied in the differential diagnosis of hepatic lesions. However, when the RDT performance characteristics were applied on a simulation of diagnosis of cases with the pre-test probability of CE of 50%, positive and negative post-test probabilities of the VIRapid test would be 78% and 22%, respectively. If ELISA was applied as a further confirmation for subjects with ultrasound lesions with a positive VIRapid test with a pre-test probability of 70%, positive and negative post-test probabilities would be 83% and 53%, respectively.
Although removing individuals with previous CE-related surgery from the analysis improves the performance of serology tests, we included this subject category in the simulations, because the subjects’ real medical history and other factors influencing serology for CE (e.g., type of surgery and time elapsed from intervention) are not determined easily in real-life field settings.
Another issue in resource-poor endemic settings is the correct diagnosis and staging of CE cases. Ultrasonography is operator dependent, and its sensitivity and specificity depend considerably on individual expertise of CE. This factor, together with CE prevalence and the rate of CE cysts on the total abdominal lesions found with ultrasound in each population, influence pre-test and post-test probabilities. Our results show that the sequential application of one or more serology tests to cases with abdominal lesions on ultrasound may support the decision of a less-experienced clinician dealing with suspect abdominal CE cases. However, reason suggests not relying on serology to discriminate post-surgical CE recurrences from residual post-surgical cavities because of the known persistence of detectable antibody levels after surgery. Knowledge of the prevalence of CE in the population and of the proportion of other pathologies/conditions that are possible differential diagnoses of CE cysts in a particular area is imperative to define pre-test and post-test probabilities in different clinical settings. Worth mentioning is the scenario in which patients may have a non-CE lesion on ultrasound but tests positive on serology because they also have lung CE inducing seropositivity. The relevance of this scenario may be ascertained only by performing chest radiography to all individuals with any CE-compatible lesion on ultrasound, which could not be performed in our study.
Taken together, our results indicate that, in accordance with previous literature13,28: 1) in the absence of a lesion compatible with CE on imaging, serology alone should not be used for prevalence or case-finding studies; and 2) a positive serology, if applied in a context of reasonably high pre-test probability, can be used to confirm a diagnosis of CE, but a negative serology should not be used to exclude it.
This study has several limitations, including the small number of subjects analyzed by serology and the impossibility of assessing the presence of lung CE. Also, most study participants (28 of 33, 84%) came from a single high-prevalence screening site, resulting in a very high positive predictive value of the diagnostic tests. Last, we could not test specifically the value of the RDT for the differential diagnosis of hepatic lesions.
In conclusion, the commercial VIRapid HYDATIDOSIS test applied in the field setting showed comparable sensitivity but lower specificity than those obtained in a controlled laboratory setting using a comparable cohort of CE cases. The application of VIRapid HYDATIDOSIS alone would not be reliable for the assessment of the population prevalence of CE, but could help clinical decision making in resource-limited settings.
Supplemental tables
Acknowledgments:
We acknowledge the study participants as well as the medical and nursing staff for taking part in the study.
Note: Supplemental tables appear at www.ajtmh.org.
REFERENCES
- 1.Deplazes P, et al. 2017. Global distribution of alveolar and cystic echinococcosis. Adv Parasitol 95: 315–493. [DOI] [PubMed] [Google Scholar]
- 2.Romig T, Deplazes P, Jenkins D, Giraudoux P, Massolo A, Craig PS, Wassermann M, Takahashi K, de la Rue M, 2017. Ecology and Life Cycle Patterns of Echinococcus Species. In Advances in Parasitology (Vol. 95). Elsevier Ltd. Available at: 10.1016/bs.apar.2016.11.002. [DOI] [PubMed] [Google Scholar]
- 3.Agudelo Higuita NI, Brunetti E, McCloskey C, 2016. Cystic echinococcosis. J Clin Microbiol 54: 518–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brunetti E, Kern P, Vuitton DA, 2010. Expert consensus for the diagnosis and treatment of cystic and alveolar echinococcosis in humans. Acta Trop 114: 1–16. [DOI] [PubMed] [Google Scholar]
- 5.Budke CM, Deplazes P, Torgerson PR, 2006. Global socioeconomic impact of cystic echinococcosis. Emerg Infect Dis 12: 296–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moro PL, Budke CM, Schantz PM, Vasquez J, Santivañez SJ, Villavicencio J, 2011. Economic impact of cystic echinococcosis in Peru. PLoS Negl Trop Dis 5: e1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moro P, Schantz PM, 2006. Cystic echinococcosis in the Americas. Parasitol Int 55 (Suppl): S181–S186. [DOI] [PubMed] [Google Scholar]
- 8.Gavidia CM, et al. 2008. Diagnosis of cystic echinococcosis, central Peruvian highlands. Emerg Infect Dis 14: 260–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tamarozzi F, et al. 2017. Prevalence and risk factors for human cystic echinococcosis in the Cusco region of the Peruvian highlands diagnosed using focused abdominal ultrasound. Am J Trop Med Hyg 96: 1472–1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hosch W, Junghanss T, Stojkovic M, Brunetti E, Heye T, Kauffmann GW, Hull WE, 2008. Metabolic viability assessment of cystic echinococcosis using high-field 1H MRS of cyst contents. NMR Biomed 21: 734–754. [DOI] [PubMed] [Google Scholar]
- 11.Lissandrin R, Tamarozzi F, Piccoli L, Tinelli C, De Silvestri A, Mariconti M, Meroni V, Genco F, Brunetti E, 2016. Factors influencing the serological response in hepatic Echinococcus granulosus infection. Am J Trop Med Hyg 94: 166–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schweiger A, Grimm F, Tanner I, Müllhaupt B, Bertogg K, Müller N, Deplazes P, 2012. Serological diagnosis of echinococcosis: the diagnostic potential of native antigens. Infection 40: 139–152. [DOI] [PubMed] [Google Scholar]
- 13.Torgerson PR, Deplazes P, 2009. Echinococcosis: diagnosis and diagnostic interpretation in population studies. Trends Parasitol 25: 164–170. [DOI] [PubMed] [Google Scholar]
- 14.Tamarozzi F, et al. 2016. Comparison of the diagnostic accuracy of three rapid tests for the serodiagnosis of hepatic cystic echinococcosis in humans. PLoS Negl Trop Dis 10: 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vola A, Tamarozzi F, Noordin R, Yunus MH, Khanbabaie S, De Silvestri A, Brunetti E, Mariconti M, 2018. Preliminary assessment of the diagnostic performances of a new rapid diagnostic test for the serodiagnosis of human cystic echinococcosis. Diagn Microbiol Infect Dis 92: 31–33. [DOI] [PubMed] [Google Scholar]
- 16.Baraquin A, Zait H, Grenouillet FE, Moreau E, Hamrioui B, Grenouillet F, 2017. Large-scale evaluation of a rapid diagnostic test for human cystic echinococcosis. Diagn Microbiol Infect Dis 89: 20–25. [DOI] [PubMed] [Google Scholar]
- 17.Gao C-H, Wang J-Y, Shi F, Steverding D, Wang X, Yang Y-T, Zhou X-N, 2018. Field evaluation of an immunochromatographic test for diagnosis of cystic and alveolar echinococcosis. Parasit Vectors 11: 311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tamarozzi F, Mariconti M, Covini I, Brunetti E, 2017. Rapid diagnostic tests for the serodiagnosis of human cystic echinococcosis. Bull Soc Pathol Exot 110: 20–30. [DOI] [PubMed] [Google Scholar]
- 19.Hernández A, et al. 2005. Cystic echinococcosis: analysis of the serological profile related to the risk factors in individuals without ultrasound liver changes living in an endemic area of Tacuarembó, Uruguay. Parasitology 130: 455–460. [DOI] [PubMed] [Google Scholar]
- 20.Hernández-González A, Santivañez S, García HH, Rodríguez S, Muñoz S, Ramos G, Orduña A, Siles-Lucas M, 2012. Improved serodiagnosis of cystic echinococcosis using the new recombinant 2B2t antigen. PLoS Neglected Tropical Diseases 6: e1714. Available at: 10.1371/journal.pntd.0001714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.DeLong ER, DeLong DM, Clarke-Pearson DL, 1988. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44: 837–845. Available at: http://www.ncbi.nlm.nih.gov/pubmed/3203132. [PubMed] [Google Scholar]
- 22.Macpherson CNL, Milner R, 2003. Performance characteristics and quality control of community based ultrasound surveys for cystic and alveolar echinococcosis. Acta Trop 85: 203–209. [DOI] [PubMed] [Google Scholar]
- 23.Moro PL, Bonifacio N, Gilman RH, Lopera L, Silva B, Takumoto R, Verastegui M, Cabrera L, 1999. Field diagnosis of Echinococcus granulosus infection among intermediate and definitive hosts in an endemic focus of human cystic echinococcosis. Trans R Soc Trop Med Hyg 93: 611–615. [DOI] [PubMed] [Google Scholar]
- 24.Lorenzo C, et al. 2005. Comparative analysis of the diagnostic performance of six major Echinococcus granulosus antigens assessed in a double-blind, randomized multicenter study. J Clin Microbiol 43: 2764–2770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Larrieu EJ, Frider B, 2001. Human cystic echinococcosis: contributions to the natural history of the disease. Ann Trop Med Parasitol 95: 679–687. [DOI] [PubMed] [Google Scholar]
- 26.MacPherson CN, Romig T, Zeyhle E, Rees PH, Were JB, 1987. Portable ultrasound scanner versus serology in screening for hydatid cysts in a nomadic population. Lancet 2: 259–261. [DOI] [PubMed] [Google Scholar]
- 27.Shambesh MA, Craig PS, Macpherson CNL, Rogan MT, Gusbi AM, Echtuish EF, 1999. An extensive ultrasound and serologic study to investigate the prevalence of human cystic echinococcosis in northern Libya. Am J Trop Med Hyg 60: 462–468. [DOI] [PubMed] [Google Scholar]
- 28.Vola A, Manciulli T, De Silvestri A, Lissandrin R, Mariconti M, Siles-Lucas M, Brunetti E, Tamarozzi F, 2019. Diagnostic performances of commercial ELISA, indirect hemagglutination, and Western blot in differentiation of hepatic echinococcal and non-echinococcal lesions: a retrospective analysis of data from a single referral centre. Am J Trop Med Hyg 101: 1345–1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.