Abstract
The major variant of concerns (VOCs) have shared mutations in severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) spike proteins, mostly on the S1 unit and resulted in higher transmissibility rate and affect viral virulence and clinical outcome. The spike protein mutations and other non-structural protein mutations in the VOCs may lead to escape approved vaccinations in certain extend. We will discuss these VOC mutations and discuss the need for combination therapeutic strategies targeting viral cycle and immune host responses.
Keywords: Transmissibility, Viral virulence, B.1.1.7, B.1.351, P.1. B.1617.1
Background
The surge of new severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) variants of concern (VOC) poses a major threat on international public health as the rapid change of the SARS-CoV-2 genome may alter viral phenotypes such as virulence, transmissibility, and ability to evade host response giving rise to greater challenge to diagnostic and clinical management [1, 2]. Yet, it is unclear whether the approved vaccines are effective against the VOCs. This article will summarize the main emerging VOCs and their potential epidemiological impact aiming at promoting development of drug therapy and effective vaccines and formulation of public health strategies.
SARS-CoV-2 genome and mutations
SARS-CoV-2 is a positive-sense single-stranded RNA virus whose genome is of a low stability thus is more prone for mutation accumulation, with approximately 9.8 × 10−4 substitutions/site yearly [3–7]. The architecture of SARS-CoV-2 is made of two groups of proteins: structural proteins (SP) and non-structural proteins (NSP). SPs are encoded by 4 genes, including E (envelop), M (membrane), S (spike) and N (nucleocapsid) genes [8]. NSPs are mostly enzymes or functional proteins that play a role in viral replication and methylation and may induce host responses to infection. These genes are encoded in several groups, namely ORF1a (NSP1-11), ORF1b (NSP12-16), ORF3a, ORF6, ORF7a, ORF7b, ORF8 and ORF10.
A variant can be as simply as a virus bearing a deviant mutation or complicated combinations of deviations leading to significant phenotypical alteration from original genome. Although by the beginning of May 2021, there has been reported more than 1.4 million sequences and among them 3913 major representative variants genomes that have been identified and included in the global SARS-CoV-2 sequence database operated by Global Initiative on Sharing Avian Influenza Data (GISAID) [9], not all genetic mutations lead to variation in major proteins and/or alter virus infectivity. The spike gene mutations account for most of the clinically influential VOCs while the ORF1a frame of the genome serves as a key region for NSP mutations.
We will focus our discussion here on the VOCs that have major global health impacts since the 4th quarter of the year 2020, including Alpha variant (B.1.1.7), Beta (B.1.351), Gamma (P.1) and Kappa and Delta (B.1.617.1 and B.1.617.2) (Table 1).
Table 1.
Molecular and clinical characteristics of SARS-CoV-2 variants of concern
| Variant of concern | Alpha B.1.1.7 |
Beta B.1.351 |
Gamma P.1 |
Delta and Kappa* B.1.617.2 B.1.617.1 |
|
|---|---|---|---|---|---|
| Epidemiology | First Identified |
September. 2020, UK |
October. 2020, South Africa |
December. 2020, Japan & Brazil |
December. 2020, India |
| Global frequency** | 48% | 7% | 7% | 14% | |
| Major geographic distribution | Worldwide | South Africa | South America | Asia | |
| Predominant mutations | Spike RBD mutations | N501Y | K417N, E484K, N501Y | K417T, E484K, N501Y |
L452R, E484Q, T478K (Delta) |
| Spike non- RBD mutations | D614G, P681H | D614G | D614G | D614G, P681R | |
| Clinical considerations *** | Transmissibility | ↑ **** | ↑? | ↑? | ↑? |
| Virulence | ↑? | ↑? | ↑? | ↑? | |
| Host Immune response | ↓ | ↓ | ↓? | ↓? | |
| Diagnostic tools | ↔ | ↔ | ↔ | ↔ | |
| Therapeutic considerations*** | Vaccinations’ effectivity | ||||
| mRNA- based | ↔ | ↓ | ↔ | ? | |
| Adenovirus-based | ↓ | ↓ | ↓ | ? | |
| Recombinant protein-based vaccines | ↓ | ↓↓ | ? | ? | |
| Inactivated virus-based | ↔ | ↓ | ↔ | ? | |
| Potential therapeutic strategies | |||||
|
S1 RBD targeted therapeutics: Soluble human recombinant ACE2, anti-RBD nanobodies Endosomal formation interruption: TMPRSS2 inhibitors (e.g., Camostat), ADAM17 inhibitors, Viral replication-oriented therapies: RdRp inhibitors (e.g. Remdesivir, GS-441524), Cas13d-based PAC-MAN |
|||||
*Delta and Kappa are derived from the emerging lineage B.1.617; **Last updated June 6th, 2021; ***All data is suggestive according to in vitro experiments unless mentioned otherwise; ****Clinical data showed higher transmissibility rate of 35–45% especially in younger group ages and children.
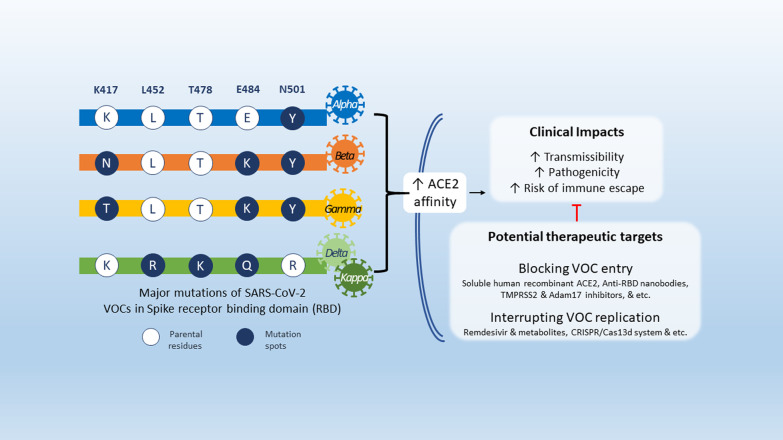
Spike mutations
Spike protein mediates the virus attachment to human cell surface angiotensin converting enzyme 2 (ACE2) receptor, thus facilitating viral entry during infection [10–12]. It is split into two subunits, S1 and S2. The S1 unit possess the receptor-binding domain (RBD) which can directly bind to ACE2 receptor and is also the dominant target of neutralizing antibodies (Ab) against SARS-CoV-2. S1 is thus considered a hotspot for mutations that may have high clinical relevance in terms of virulence, transmissibility, and host immune evasion [13–16] (Table 2).
Table 2.
Major spike mutations
| Mutating residues | Mutation | Region | Pathophysiology | Clinical Impact expectations | Major variants | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| ACE2 affinity | Immune escape# | Transmissibility | Virulence | Alpha B.1.1.7 |
Beta B.1.351 |
Gamma P.1 |
Delta &Kappa B.1.617.2/1 |
|||
| K417 | K417N | RBD | ↑ | ↑ | ↑ | ↑ | √ | |||
| K417T | ↑ | ↑ | ↑ | ↑? | √ | |||||
| L452 | L452R | ↑ | ↑ | ↑ | ↑ | √ | ||||
| T478 | T478K | ↑ | ↑ | ↑ | ↑? | √ (Delta) | ||||
| E484 | E484K | ↑ | ↑ | ↑? | ↑? | √ (partially) | √ | √ | ||
| E484Q | ↑ | ↑ | ↑? | ↑? | √ | |||||
| N501 | N501Y | ↑ | ↑ | ↑ | ↑ | √ | √ | √ | ||
| D614 | D614G | non-RBD | ↑ | ↑ | ↑ | ↔ | √ | √ | √ | √ |
| P681 | P681H | S1/S2 Furin cleavage site | ↔ | ↑? | ↑ | ↑? | √ | |||
| P681R | ↔ | ↑? | ↑ | ↑? | √ | |||||
#Both host and vaccine-induced immunity. Abbreviations: RBD, receptor binding domain
The Alpha variant has an N501Y mutation: at the 501 residue, N asparagine has been replaced with Y tyrosine, as well as K417N—lysine K replaced with asparagine N [9]. An emerging variant derived from B.1.1.7 also carries E484K mutation—glutamic acid E replaced with lysine K [9]. Both Beta and Gamma variants have more substitutions other than N501Y [9]. The Beta variant has E484K, while the Gamma variant has the E484K and the K417T mutations [9]. The latest major variants, Delta and Kappa, sharing two mutations E484Q (glutamic acid E substituted by glutamine Q) and L452R (leucine L altered by arginine R) were identified in India’s second COVID-19 wave. Other than the two mutations above, Delta also harbours a unique mutation, T478K (threonine T replaced by lysine K) [9].
The S1 mutations significantly increases the binding affinity to ACE2 while showing lower affinity to neutralizing antibodies [17–21], suggesting a possible explanation for their occurring higher transmissibility and virulence [22, 23].
Another mutation at non-RBD sites, named D614G, is the most spreading mutation carried by over 99% of prevalent variants since early 2020 [23, 24]. Such mutation does not change the binding affinity to ACE2 or neutralizing Abs for the virion, yet it may increase spike density by preserving the integrity of spike and avoiding S1 shedding [25]. With more functional spikes available, D614G variants are armed with increased infectivity and hence increased replication in vitro while earlier transmission in vivo [23, 25, 26]. Recently, increasing deletions are observed in the neutralizing Ab-recognizing domain, namely recurrent deletion regions (RDRs), in the N-terminus of S1 subunit [27]. Deletions in RDRs wipe out the epitopes, and eventually aiding the virus evading host’s immune supervision and potentially defecting certain neutralizing Abs or vaccines. A majority of Alpha derived variants (ΔRDR1, S: ΔHV 69–70, & ΔRDR2, S: ΔY144), Beta derived variants (ΔRDR4, S: ΔLAL 242–244) and B.1.36 (ΔRDR3, S: ΔI210) carry this kind of mutation [27].
NSP mutations
Two mutation hot-spots, NSP1 of ORF1a/ORF1ab, and ORF8, have been found related to the virulence and transmissibility. NSP1 is a key protein to antagonize type I interferon induction in the host and benefit the replication of the virus itself [28, 29]. ORF8 is known as an immune-evasive protein that downregulates major histocompatibility complex class I (MHC-I) in host cells [30, 31]. Recently, the Alpha variant, identified from a single immunocompromised individual, was shown to contains a premature stop codon at position 27 of ORF8[32].
Variants with partial deletion of NSP1 and ORF8 have been identified (e.g., the NSP1: Δ500-532 variant in Sichuan, China, and the ORF8: Δ382 variant in Singapore) [29, 31]. Despite that truncated NSP1 and ORF8 both contribute to milder infections [29–31] and account for less than 5% of infections worldwide, they have become the major variants in Africa since late 2020[9].
Potential clinical impacts of SARS-CoV-2 VOCs
Increased transmissibility and viral virulence
It was shown that S-protein mutation D614G may impact SARS-CoV-2 transmissibility rate due to higher affinity for olfactory epithelium and it was shown to have higher transmissibility in animal models [33, 34]. It was also shown that it has a higher virion stability and was shown to be more resistant to proteolytic cleave as well as higher viral titer in upper airways [35, 36] suggesting that it may potentially affect virus transmissibility and virulence. Yet, it showed increased susceptibility for neutralizing antibodies and no difference in clinical severity nor hospitalization outcomes and mortality was observed [37, 38].
Evidence suggest that the VOCs Alpha and Beta increased transmissibility rate at ~ 50% especially in younger group ages and children [39, 40]. Alpha variant was shown to increase hospitalizations and mortality that may be attributed to their escape from neutralizing Abs due to their RBD mutations [41].
The Epsilon variant (B.1.427/B.1.429, California variants) increased transmissibility up to 24% with higher viral shedding, which is attributed to the of L452R spike mutation that was shown to stabilize spike-ACE2 receptor interaction [42, 43].
Although it is also suggested that other variants such as Gamma, Epsilon variants and recent Iota variants (B.1526, New York variant) may also have increased virulence due to spike mutations that increase affinity to ACE2, there is still no data available regarding viral virulence.
Decreased diagnostic sensitivity
The new VOCs can reduce the detection sensitivity of RT-PCR based diagnostic tools especially when mutations occur in locations where probes and primers may bind [44]. Reports suggest that 79% of the primer binding sites used in the RT-PCR assay are already mutated in at least one genome with the highest significance of the GGG → AAC substitution [45]. Recent analysis which mapped primers or probes binding sites showed a cumulative variants frequency of ≥ 1% in the global SARS-CoV-2 genomes [46]. The Alpha lineage was shown to have higher false-negative results when using specific commercial kits directed to the spike (S) gene but not when using standard protocols such as Berlin-Cherite protocol since it does not involve the S protein-encoding gene as target [47]. Another concern is a variant detected in France of a S deletion (ΔH69-V70) which has shown to be associated with S-gene target gene detection failure in three-target RT-PCR [48]. Several reports have targeted mutations in different open reading frames (ORFs) especially ORF8 position which was found in some isolates from Mexico, Belize and Guatemala as potentially leading to epitope loss and reduced sensitivity for serological testing [49–51].
On the other hand, other studies showed that although mismatches in the primer/probes binding regions of SARS-CoV-2 diagnostic assays can be detected in different SARS-CoV-2 variants, they were tolerated and did not result in reduced assay performance and false-negative results [52, 53]. Moreover, according to bioinformatic analysis performed, the known variability occurring in the SARS-CoV-2 population have minimal or no effect on the sensitivity existing diagnostic tools for viral detection [54, 55].
Still, the continuous emergence of SARS-CoV-2 variants and possible mismatches highlight the importance of global molecular surveillance and designing diagnostic strategies such as combining diagnostic methods during future outbreaks or perform assays that target two or more positions in highly conserved regions of the viral genome to promote higher specificity and sensitivity results as well as developing highly specific diagnostic tools using CRISPR [56, 57].
Potential influence on vaccination
Currently, all vaccines are based on introducing spike protein, which is the major superficial virulence of SARS-CoV-2, using the reference genome isolates early in the pandemic. As there is no sufficient evidence to support the effect of vaccines against Delta and Kappa variants, we’ll focus on the Alpha, Beta and Kappa variants.
mRNA Vaccines
Two major mRNA-based anti-SARS-CoV-2 vaccines have been approved: BNT162b2 (Pfizer-BioNTech) and mRNA-1273 (Moderna). Studies suggest that BNT162b2 vaccines were able to stimulate the recipients to generate capable antibodies to neutralize Alpha and Gamma variants yet being significantly less protective against Beta variant [41, 58, 59] mRNA-1273 was shown to enhance sufficient neutralizing ability against Alpha variant yet lower reciprocal titer against Beta variant [41, 60, 61].
Adenovirus-based vaccines
There are 4 adenovirus-based vaccines that have been authorized for general or emergency use. Among of which, Ad26.COV2.S is a recombinant, replication-incompetent adenovirus serotype 26 (Ad26) vector encoding a full-length and stabilized SARS-CoV-2 spike protein (Janssen) was shown to have reduced efficacies to Beta variant (64%) and Gamma dominant Latin America variant (61%), compared to the U.S. (72%) where Alpha is the dominant strain [62]. ChAdOx1 nCoV-19 (Oxford) is a chimpanzee adenovirus-vectored vaccine expressing the SARS-CoV-2 spike protein. Recent studies revealed that the efficacy of ChAdOx1 nCoV-19 was 74.6% against Alpha but as low as 10.4% against Beta [63, 64]. Gam-COVID-Vac (Ad26 and Ad5) is also claimed protective to the global VOCs, yet the clinical trial result has not yet been publicized [65]. An ongoing clinical trial on the combination of ChAdOx1 nCoV-19 and Gam-COVID-Vac (Russia), which is a heterologous COVID-19 vaccine consisting of two components, a recombinant adenovirus type 26 (rAd26) vector and a recombinant adenovirus type 5 (rAd5) vector, both carrying the gene for SARS-CoV-2 spike glycoprotein. There is no data regarding its efficacy on VOCs [66].
Subunit vaccines
NVX-CoV2373 (Novavax) contains a full-length, prefusion spike protein, and shows an 86.3% efficacy against Alpha, yet 48.6% against Beta [67]. However, none of the recombinant protein-based vaccines have yet to be approved for general use.
Inactivated virus-based vaccines
Three inactivated virus- based vaccines have been approved so far and have been widely used in China, India and Brazil. A recent in vitro study suggests that antisera elicited by BBIBP-CorV vaccine (Sinopharm) are able to neutralize the Beta variant in a differentially weaker level compared to the wildtype strain and the D614G variant [68]. A recent serological study has shown that BBV152 (Bharat Biotech International Limited) vaccinated human serum is able to neutralize the Alpha variant [69]. Preliminary data from a study conducted in Sao Paulo, Brazil indicate that the most widely vaccinated vaccine, CoronaVac (Sinovac Biotech), is effective against Gamma variant [70]. The same research facility claimed the vaccine also ‘works well’ against the Alpha and Gamma variants [71].
To conclude, it appears that Beta is most likely variant to affect the approved vaccines efficiency while Alpha and Gamma variants do not. These results suggest that a new vaccine might be required specifically to target Beta variant. Many strategies are currently under development to cope with Beta variant challenge such as booster vaccines [72].
Potential therapeutics for VOCs
S1 RBD targeted therapy
Whether specifically targeting spike proteins using small peptide-based therapies or using single-domains neutralizing antibodies against any of those targets, these therapeutic strategies efficiency may be compromised by the emergence of SARS-CoV-2 variants especially those possessing spike proteins and RBD mutations that increase affinity to ACE2 such as Alpha, and Iota variant, by potentially escaping neutralizing antibodies and competing with those agents for the same binding targets [73–75]. In order to avoid antibody escape, strategies to combine different neutralizing antibody cocktail have been suggested as a therapeutic approach against the emerging variants [76]. Other treatments such as anti-RBD nanobodies isolated from llamas were shown to neutralize RBD variants suggesting they might be a promising tool against new SARS-CoV-2 VOCs as well [77, 78].
Different engineered variants of human recombinant soluble ACE2 (hrACE2), were reported to significantly inhibit SARS-CoV-2 infection in vitro and causing sustained viral entry blockade upon engagement of hrACE2 with the RBD in SARS-CoV-2 S protein with high affinity [79–81]. This is a potentially powerful treatment against SARS-CoV-2 VOCs as it can exploit the increase S-protein host receptor-binding affinity caused by S-mutations, toward increasing S-protein affinity to hrACE2. Moreover, no mutations that limit receptor-binding affinity were discovered as this will decrease affinity to native ACE2 receptor and may likely to attenuate virulence [82], suggesting that viral escape from hrACE is very unlikely.
Interruption of endosomal formation
Targeting endosomal formation of SARS-CoV-2 to block entry to host cells such as antimalarial drugs and macrolides, and us of drugs targeting host cell transmembrane protease serine 2 (TMPRSS2) such as Camostat [83–85] or A disintegrin and metalloprotease 17 (ADAM17) inhibitors [86].
Interruption of SARS-CoV-2 VOC genome
Promising antiviral drugs such as the FDA-approved Remdesivir and its metabolites, Ribaverin and Galidesivir have been shown to inhibit viral replication in vitro and in vivo studies due to their effect on inhibiting RNA dependent RNA polymerase (RdRp) [87, 88]. The discovery of RdRp hotspot mutations in SARS-CoV-2, found mostly in European strains may lead to drug-resistance of to RdRp inhibitors in a similar mechanism found in Influenza and Hepatitis C [89–91]. However, it has been shown currently that those variants have minimal impact for pre-existing resistance to Remdesivir.
Another potential approach is Prophylactic Antiviral CRISPR in Human Cells (PAC-MAN), which is a Cas13d-based strategy that target reserved regions such as nucleocapsid protein and RdRp in SARS-CoV-2 viral genome and may serve as pan-coronavirus strategy for any future coronaviruses and variant that may emerge [92].
Conclusion
Emerging VOCs have the potential to effect clinical and global health outcomes, emphasizing the necessity for genomically tailored therapeutic approach in the future therefore we suggest that a combination strategy targeting different components in viral cycle and immune host response may be critical but overlooked in the combat against SARS-CoV-2 VOCs.
Acknowledgements
Not Applicable.
Abbreviations
- Ab
Antibodies
- ACE2
Angiotensin Converting Enzyme 2
- ADAM17
A disintegrin and metalloprotease 17
- E
Envelope
- GISAID
Global Initiative on Sharing Avian Influenza Data
- hrACE2
Human Recombinant Soluble Angiotensin Converting Enzyme 2
- M
Membrane
- MHC-I
Major Histocompatibility Complex Class I
- N
Nucleocapsid
- NSP
Non-Structural Proteins
- ORF
Open Reading Frames
- PAC-MAN
Prophylactic Antiviral CRISPR in Human Cells
- RBD
Receptor-Binding Domain
- RDR
Recurrent Deletion Regions
- RdRp
RNA dependent RNA polymerase
- S
Spike
- SARS-CoV-2
Severe Acute Respiratory Syndrome Coronavirus 2
- SP
Structural Proteins
- TMPRSS2
Transmembrane Protease Serine 2
- VOC
Variant Of Concern
Authors' contributions
JK and YL did the literature search and drafted the paper. JK, YL and HZ revised the paper, tables and graphic abstract. The authors read and approved the final manuscript.
Funding
Not applicable.
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.COVID-19 daily epidemiology update - Canada.ca [Internet]. [cited 2021 May 8]. https://health-infobase.canada.ca/covid-19/epidemiological-summary-covid-19-cases.html
- 2.Berry I, Soucy JPR, Tuite A, Fisman D. Open access epidemiologic data and an interactive dashboard to monitor the COVID-19 outbreak in Canada. CMAJ. Canadian Medical Association; 2020. p. E420. [DOI] [PMC free article] [PubMed]
- 3.Duchene S, Featherstone L, Haritopoulou-Sinanidou M, Rambaut A, Lemey P, Baele G. Temporal signal and the phylodynamic threshold of SARS-CoV-2. Virus Evol. 2020;6. [DOI] [PMC free article] [PubMed]
- 4.van Dorp L, Acman M, Richard D, Shaw LP, Ford CE, Ormond L, et al. Emergence of genomic diversity and recurrent mutations in SARS-CoV-2. Infect Genet Evol. 2020; 83. https://pubmed.ncbi.nlm.nih.gov/32387564/ [DOI] [PMC free article] [PubMed]
- 5.van Dorp L, Richard D, Tan CCS, Shaw LP, Acman M, Balloux F. No evidence for increased transmissibility from recurrent mutations in SARS-CoV-2. Nat Commun. 2020. https://pubmed.ncbi.nlm.nih.gov/33239633/ [DOI] [PMC free article] [PubMed]
- 6.Giovanetti M, Benvenuto D, Angeletti S, Ciccozzi M. The first two cases of 2019-nCoV in Italy: Where they come from? J Med Virol. 2020;92:518–521. doi: 10.1002/jmv.25699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li X, Wang W, Zhao X, Zai J, Zhao Q, Li Y, et al. Transmission dynamics and evolutionary history of 2019-nCoV. J Med Virol. 2020;92:501–511. doi: 10.1002/jmv.25701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wu F, Zhao S, Yu B, Chen YM, Wang W, Song ZG, et al. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579:265–269. doi: 10.1038/s41586-020-2008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.GISAID - hCov19 Variants [Internet]. [cited 2021 Jun 6]. https://www.gisaid.org/hcov19-variants/
- 10.Yan R, Zhang Y, Li Y, Xia L, Guo Y, Zhou Q. Structural basis for the recognition of SARS-CoV-2 by full-length human ACE2. Science. 2020; 367:1444–8. [DOI] [PMC free article] [PubMed]
- 11.Li W, Moore MJ, Vasilieva N, Sui J, Wong SK, Berne MA, et al. Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature. 2003;426:450–454. doi: 10.1038/nature02145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li F, Li W, Farzan M, Harrison SC. Structure of SARS coronavirus spike receptor-binding domain complexed with receptor. Science United States. 2005;309:1864–1868. doi: 10.1126/science.1116480. [DOI] [PubMed] [Google Scholar]
- 13.Huang Y, Yang C, Xu X, Feng, Xu W, Liu S wen. Structural and functional properties of SARS-CoV-2 spike protein: potential antivirus drug development for COVID-19. Acta Pharmacol Sin. 2020. 10.1038/s41401-020-0485-4 [DOI] [PMC free article] [PubMed]
- 14.Yi C, Sun X, Ye J, Ding L, Liu M, Yang Z, et al. Key residues of the receptor binding motif in the spike protein of SARS-CoV-2 that interact with ACE2 and neutralizing antibodies. Cell Mol Immunol. 2020;17:621–630. doi: 10.1038/s41423-020-0458-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lan J, Ge J, Yu J, Shan S, Zhou H, Fan S, et al. Structure of the SARS-CoV-2 spike receptor-binding domain bound to the ACE2 receptor. Nature. 2020;581:215–220. doi: 10.1038/s41586-020-2180-5. [DOI] [PubMed] [Google Scholar]
- 16.Shang J, Ye G, Shi K, Wan Y, Luo C, Aihara H, et al. Structural basis of receptor recognition by SARS-CoV-2. Nature. 2020;581:221–224. doi: 10.1038/s41586-020-2179-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Piccoli L, Park YJ, Tortorici MA, Czudnochowski N, Walls AC, Beltramello M, et al. Mapping neutralizing and immunodominant sites on the SARS-CoV-2 spike receptor-binding domain by structure-guided high-resolution serology. Cell. 2020;183:1024–1042.e21. doi: 10.1016/j.cell.2020.09.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Investigation of novel SARS-COV-2 variant: Variant of Concern 202012/01 - GOV.UK [Internet]. gov.uk. 2020. https://www.gov.uk/government/publications/nervtag-paper-on-covid-19-variant-of-concern-
- 19.Fratev F. The SARS-CoV-2 S1 spike protein mutation N501Y alters the protein interactions with both hACE2 and human derived antibody: a Free energy of perturbation study [Internet]. bioRxiv. bioRxiv; 2020 [cited 2021 Feb 20]. p. 2020.12.23.424283. 10.1101/2020.12.23.424283
- 20.Edara VV, Norwood C, Floyd K, Lai L, Davis-Gardner ME, Hudson WH, et al. Reduced binding and neutralization of infection- and vaccine-induced antibodies to the B.1.351 (South African) SARS-CoV-2 variant. bioRxiv Prepr Serv Biol [Internet]. 2021. http://www.ncbi.nlm.nih.gov/pubmed/33655254%0Ahttp://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC7924283
- 21.Starr TN, Greaney AJ, Addetia A, Hannon WW, Choudhary MC, Dingens AS, et al. Prospective mapping of viral mutations that escape antibodies used to treat COVID-19. Science (80- ) [Internet]. 2021 [cited 2021 Feb 7];eabf9302. 10.1126/science.abf9302 [DOI] [PMC free article] [PubMed]
- 22.Nelson G, Buzko O, Patricia S, Niazi K, Rabizadeh S, Soon-Shiong P. Molecular dynamic simulation reveals E484K mutation enhances spike RBD-ACE2 affinity and the 1 combination of E484K, K417N and N501Y mutations (501Y.V2 variant) induces conformational 2 change greater than N501Y mutant alone, potentially resulting in an e. bioRxiv [Internet]. 2021 [cited 2021 Feb 7];2021.01.13.426558. 10.1101/2021.01.13.426558
- 23.Starr TN, Greaney AJ, Hilton SK, Ellis D, Crawford KHD, Dingens AS, et al. Deep mutational scanning of SARS-CoV-2 receptor binding domain reveals constraints on folding and ACE2 binding. Cell. 2020;182:1295–1310.e20. doi: 10.1016/j.cell.2020.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Plante JA, Liu Y, Liu J, Xia H, Johnson BA, Lokugamage KG, et al. Spike mutation D614G alters SARS-CoV-2 fitness. Nature. 2021;592:116–121. doi: 10.1038/s41586-020-2895-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang L, Jackson CB, Mou H, Ojha A, Peng H, Quinlan BD, et al. SARS-CoV-2 spike-protein D614G mutation increases virion spike density and infectivity. Nat Commun. 2020;11. [DOI] [PMC free article] [PubMed]
- 26.Hou YJ, Chiba S, Halfmann P, Ehre C, Kuroda M, Dinnon KH, et al. SARS-CoV-2 D614G variant exhibits efficient replication ex vivo and transmission in vivo. Science. 370:1464–8 [DOI] [PMC free article] [PubMed]
- 27.McCarthy KR, Rennick LJ, Nambulli S, Robinson-McCarthy LR, Bain WG, Haidar G, et al. Recurrent deletions in the SARS-CoV-2 spike glycoprotein drive antibody escape. Science. 2021;eabf6950. http://science.sciencemag.org/content/early/2021/02/02/science.abf6950.abstract [DOI] [PMC free article] [PubMed]
- 28.Xia H, Cao Z, Xie X, Zhang X, Chen JYC, Wang H, et al. Evasion of Type I Interferon by SARS-CoV-2. Cell Rep. 2020;33:108234. doi: 10.1016/j.celrep.2020.108234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lin J, Tang C, Wei H, Du B, Chen C, Wang M, et al. Genomic monitoring of SARS-CoV-2 uncovers an Nsp1 deletion variant that modulates type I interferon response. Cell Host Microbe; 2021. [DOI] [PMC free article] [PubMed]
- 30.Flower TG, Buffalo CZ, Hooy RM, Allaire M, Ren X, Hurley JH. Structure of SARS-cov-2 ORF8, a rapidly evolving immune evasion protein. Proc Natl Acad Sci U S A. 2021;118:1–6. doi: 10.1073/pnas.2021785118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Young BE, Fong SW, Chan YH, Mak TM, Ang LW, Anderson DE, et al. Effects of a major deletion in the SARS-CoV-2 genome on the severity of infection and the inflammatory response: an observational cohort study. Lancet. 2020;396:603–611. doi: 10.1016/S0140-6736(20)31757-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rambaut A, Loman N, Pybus O, Barclay W, Barrett J, Carabelli A, et al. Preliminary genomic characterisation of an emergent SARS-CoV-2 lineage in the UK defined by a novel set of spike mutations - SARS-CoV-2 coronavirus/nCoV-2019 Genomic Epidemiology - Virological. Virological.org [Internet]. 2020 [cited 2021 May 31];1–9. https://virological.org/t/preliminary-genomic-characterisation-of-an-emergent-sars-cov-2-lineage-in-the-uk-defined-by-a-novel-set-of-spike-mutations/563
- 33.Butowt R, Bilinska K, Von Bartheld CS. Chemosensory dysfunction in COVID-19: integration of genetic and epidemiological data points to D614G spike protein variant as a contributing factor. ACS Chem Neurosci. 2020;11:3180–3184. doi: 10.1021/acschemneuro.0c00596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhou B, Thao TTN, Hoffmann D, Taddeo A, Ebert N, Labroussaa F, et al. SARS-CoV-2 spike D614G change enhances replication and transmission. Nature; 2021. http://www.nature.com/articles/s41586-021-03361-1 [DOI] [PubMed]
- 35.Grubaugh ND, Hanage WP, Rasmussen AL. Making sense of mutation: what D614G means for the COVID-19 pandemic remains unclear. Cell. 2020;182:794–795. doi: 10.1016/j.cell.2020.06.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Korber B, Fischer WM, Gnanakaran S, Yoon H, Theiler J, Abfalterer W, et al. Tracking changes in SARS-CoV-2 spike: evidence that D614G increases infectivity of the COVID-19 virus. Cell. 2020;182:812–827.e19. doi: 10.1016/j.cell.2020.06.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Volz E, Hill V, McCrone JT, Price A, Jorgensen D, O’Toole Á, et al. Evaluating the effects of SARS-CoV-2 spike mutation D614G on transmissibility and pathogenicity. Cell Cell Press. 2021;184:64–75.e11. doi: 10.1016/j.cell.2020.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mlcochova P, Collier D, Ritchie A, Assennato SM, Hosmillo M, Goel N, et al. Combined Point-of-Care Nucleic Acid and Antibody Testing for SARS-CoV-2 following Emergence of D614G Spike Variant. Cell Reports Med; 2020. https://pubmed.ncbi.nlm.nih.gov/32905045/ [DOI] [PMC free article] [PubMed]
- 39.Washington NL, Gangavarapu K, Zeller M, Bolze A, Cirulli ET, Schiabor Barrett KM, et al. Genomic epidemiology identifies emergence and rapid transmission of SARS-CoV-2 B.1.1.7 in the United States. medRxiv [Internet]. medRxiv; 2021;2021.02.06.21251159. http://www.ncbi.nlm.nih.gov/pubmed/33564780 [DOI] [PMC free article] [PubMed]
- 40.Volz E, Mishra S, Chand M, Barrett JC, Johnson R, Geidelberg L, et al. Assessing transmissibility of SARS-CoV-2 lineage B.1.1.7 in England. Nature 2021. 10.1038/s41586-021-03470-x [DOI] [PubMed]
- 41.Wang P, Liu L, Iketani S, Luo Y, Guo Y, Wang M, et al. Increased Resistance of SARS-CoV-2 Variants B.1.351 and B.1.1.7 to Antibody Neutralization. bioRxiv Prepr Serv Biol [Internet]. Cold Spring Harbor Laboratory; 2021 [cited 2021 Mar 15];2021.01.25.428137. http://www.ncbi.nlm.nih.gov/pubmed/33532778
- 42.Deng X, Garcia-knight MA, Khalid MM, Servellita V, Morris MK, Sotomayor-gonzález A, et al. Transmission, infectivity, and neutralization of a spike L452R SARS-CoV-2 variant. Cell. 2021 doi: 10.1016/j.cell.2021.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhang W, Davis BD, Chen SS, Sincuir Martinez JM, Plummer JT, Vail E. Emergence of a novel SARS-CoV-2 variant in Southern California. JAMA J Am Med Assoc. 2021; 1324–6. https://pubmed.ncbi.nlm.nih.gov/33571356/ [DOI] [PMC free article] [PubMed]
- 44.Yang JR, Kuo CY, Huang HY, Wu FT, Huang YL, Cheng CY, et al. Newly emerging mutations in the matrix genes of the human influenza a(h1n1)pdm09 and a(h3n2) viruses reduce the detection sensitivity of real-time reverse transcription-pcr. J Clin Microbiol. 2014;52:76–82. doi: 10.1128/JCM.02467-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shu Y, McCauley J. GISAID: Global initiative on sharing all influenza data – from vision to reality [Internet]. Eurosurveillance. European Centre for Disease Prevention and Control (ECDC); 2017. https://pubmed.ncbi.nlm.nih.gov/28382917/ [DOI] [PMC free article] [PubMed]
- 46.Jain A, Rophina M, Mahajan S, Krishnan BB, Sharma M, Mandal S, et al. Analysis of the potential impact of genomic variants in global SARS-CoV-2 genomes on molecular diagnostic assays. Int J Infect Dis. 2021;102:460–462. doi: 10.1016/j.ijid.2020.10.086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ramírez JD, Muñoz M, Patiño LH, Ballesteros N, Paniz‐Mondolfi A. Will the emergent SARS‐CoV2 B.1.1.7 lineage affect molecular diagnosis of COVID‐19? J Med Virol; 2021. https://pubmed.ncbi.nlm.nih.gov/33506970/ [DOI] [PMC free article] [PubMed]
- 48.Bal A, Destras G, Gaymard A, Stefic K, Marlet J, Eymieux S, et al. Two-step strategy for the identification of SARS-CoV-2 variant of concern 202012/01 and other variants with spike deletion H69-V70, France, August to December 2020. Euro Surveill; 2021 [cited 2021 Feb 27];26. https://pubmed.ncbi.nlm.nih.gov/33478625/ [DOI] [PMC free article] [PubMed]
- 49.Pereira F. Evolutionary dynamics of the SARS-CoV-2 ORF8 accessory gene. Infect Genet Evol; 2020;85. https://pubmed.ncbi.nlm.nih.gov/32890763/ [DOI] [PMC free article] [PubMed]
- 50.Gong YN, Tsao KC, Hsiao MJ, Huang CG, Huang PN, Huang PW, et al. SARS-CoV-2 genomic surveillance in Taiwan revealed novel ORF8-deletion mutant and clade possibly associated with infections in Middle East. Emerg Microbes Infect. 2020;9:1457–1466. doi: 10.1080/22221751.2020.1782271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hernández-Huerta MT, Pérez-Campos Mayoral L, Romero Díaz C, Martínez Cruz M, Mayoral-Andrade G, Sánchez Navarro LM, et al. Analysis of SARS-CoV-2 mutations in Mexico, Belize, and isolated regions of Guatemala and its implication in the diagnosis. J Med Virol; 2020; 93. https://pubmed.ncbi.nlm.nih.gov/33049069/ [DOI] [PMC free article] [PubMed]
- 52.Khan KA, Cheung P. Presence of mismatches between diagnostic PCR assays and coronavirus SARS-CoV-2 genome. R Soc Open Sci;7:200636 [DOI] [PMC free article] [PubMed]
- 53.Gand M, Vanneste K, Thomas I, Van Gucht S, Capron A, Herman P, et al. Use of whole genome sequencing data for a first in silico specificity evaluation of the RT-QPCR assays used for SARS-CoV-2 detection. Int J Mol Sci. 2020;21:1–25. doi: 10.3390/ijms21155585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Arena F, Pollini S, Rossolini GM, Margaglione M. Summary of the available molecular methods for detection of SARS-CoV-2 during the ongoing pandemic. Int J. Mol. Sci. 2021. p. 1–14. https://pubmed.ncbi.nlm.nih.gov/33525651/ [DOI] [PMC free article] [PubMed]
- 55.Vogels CBF, Brito AF, Wyllie AL, Fauver JR, Ott IM, Kalinich CC, et al. Analytical sensitivity and efficiency comparisons of SARS-CoV-2 RT–qPCR primer–probe sets. Nat Microbiol. 2020;5:1299–1305. doi: 10.1038/s41564-020-0761-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kuchinski KS, Jassem AN, Prystajecky NA. Assessing oligonucleotide designs from early lab developed PCR diagnostic tests for SARS-CoV-2 using the PCR_strainer pipeline. J Clin Virol; 2020;131. https://pubmed.ncbi.nlm.nih.gov/32889496/ [DOI] [PMC free article] [PubMed]
- 57.Wang Y, Zhang Y, Chen J, Wang M, Zhang T, Luo W, et al. Detection of SARS-CoV-2 and its mutated variants via CRISPR-Cas13-based transcription amplification. Anal Chem; 2021. 10.1021/acs.analchem.0c04303 [DOI] [PubMed]
- 58.Liu Y, Liu J, Xia H, Zhang X, Fontes-Garfias CR, Swanson KA, et al. Neutralizing Activity of BNT162b2-Elicited Serum - Preliminary Report. N Engl J. 2021; NEJMc2102017. http://www.ncbi.nlm.nih.gov/pubmed/33596352 [DOI] [PMC free article] [PubMed]
- 59.Muik A, Wallisch A-K, Sänger B, Swanson KA, Mühl J, Chen W, et al. Neutralization of SARS-CoV-2 lineage B.1.1.7 pseudovirus by BNT162b2 vaccine–elicited human sera. Science (80- ) 2021;371:eabg6105. 10.1101/2020.12.30.20249034. [DOI] [PMC free article] [PubMed]
- 60.Wu K, Werner AP, Koch M, Choi A, Narayanan E, Stewart-Jones GBE, et al. Serum neutralizing activity elicited by mRNA-1273 vaccine—preliminary report. N Engl J Med 2021;NEJMc2102179. 10.1056/NEJMc2102179 [DOI] [PMC free article] [PubMed]
- 61.Wu K, Werner AP, Moliva JI, Koch M, Choi A, Steward-Jones GBE, et al. mRNA-1273 vaccine induces neutralizing antibodies against spike mutants from global SARS-CoV-2 variants. bioRxiv. 2021;
- 62.Vaccines and Related Biological Products Advisory Committee February 26, 2021 Meeting Announcement - 02/26/2021 - 02/26/2021 | FDA. https://www.fda.gov/advisory-committees/advisory-committee-calendar/vaccines-and-related-biological-products-advisory-committee-february-26-2021-meeting-announcement#event-materials
- 63.Emary KRW, Golubchik T, Aley PK, Ariani C V., Angus BJ, Bibi S, et al. Efficacy of ChAdOx1 nCoV-19 (AZD1222) Vaccine Against SARS-CoV-2 VOC 202012/01 (B.1.1.7). Lancet Prepr. 2021;
- 64.Madhi SA, Baillie V, Cutland CL, Voysey M, Koen AL, Fairlie L, et al. Efficacy of the ChAdOx1 nCoV-19 Covid-19 Vaccine against the B.1.351 Variant. N Engl J Med; 2021; 10.1056/NEJMoa2102214 [DOI] [PMC free article] [PubMed]
- 65.Russian scientists say Sputnik V performs well against COVID mutations | Reuters. https://www.reuters.com/article/us-health-coronavirus-sputnik-mutations-idUSKBN2AR0E7
- 66.AstraZeneca Vax - Sputnik V Combination Study - Full Text View - ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/NCT 04684446
- 67.Novavax Confirms High Levels of Efficacy Against Original and Variant COVID-19 Strains in United Kingdom and South Africa Trials [Internet]. 2021. https://www.novavax.com/resources#protocols
- 68.Huang B, Dai L, Wang H, Hu Z, Yang X, Tan W, et al. Neutralization of SARS-CoV-2 VOC 501Y.V2 by human antisera elicited by both 1 inactivated BBIBP-CorV and recombinant dimeric RBD ZF2001 vaccines 2 3 Authors. bioRxiv [Internet]. Cold Spring Harbor Laboratory; 2021 [cited 2021 Mar 17];2021.02.01.429069. 10.1101/2021.02.01.429069
- 69.Sapkal GN, Yadav PD, Ella R, Deshpande GR, Sahay RR, Gupta N, et al. Neutralization of UK-variant VUI-202012/01 with COVAXIN vaccinated human serum. bioRxiv [Internet]. 2021 [cited 2021 Mar 17]; 10.1101/2021.01.26.426986
- 70.Preliminary data indicates Sinovac COVID-19 vaccine effective against Brazilian P1 variant: official | Reuters [Internet]. [cited 2021 Mar 17]. https://www.reuters.com/article/us-health-coronavirus-brazil-variant-idUSKBN2B2274
- 71.Sinovac vaccine works on UK, South African variants - Brazil institute | Reuters [Internet]. [cited 2021 Mar 17]. https://www.reuters.com/article/us-health-coronavirus-brazil-idUSKBN2AH2H0
- 72.Moderna COVID-19 Vaccine Retains Neutralizing Activity Against Emerging Variants First Identified in the U.K. and the Republic of South Africa. 2021.
- 73.Ye G, Gallant JP, Massey C, Shi K, Tai W, Zheng J, et al. The Development of a Novel Nanobody Therapeutic for SARS-CoV-2 [Internet]. bioRxiv. bioRxiv; 2020 [cited 2021 Mar 28]. p. 2020.11.17.386532. 10.1101/2020.11.17.386532
- 74.Grand R Le, Maisonnasse P, Aldon Y, Marc A, Marlin R, Dereuddre-Bosquet N, et al. COVA1–18 neutralizing antibody protects against SARS-CoV-2 in three preclinical models. Res Sq [Internet]. Res Sq; 2021 [cited 2021 Mar 28]; http://www.ncbi.nlm.nih.gov/pubmed/33619476 [DOI] [PMC free article] [PubMed]
- 75.Ramanathan M, Ferguson ID, Miao W, Khavari PA. SARS-CoV-2 B.1.1.7 and B.1.351 Spike variants bind human ACE2 with increased affinity. bioRxiv Prepr Serv Biol [Internet]. Cold Spring Harbor Laboratory; 2021 [cited 2021 Mar 28];2021.02.22.432359. http://www.ncbi.nlm.nih.gov/pubmed/33655251 [DOI] [PMC free article] [PubMed]
- 76.De Gasparo R, Pedotti M, Simonelli L, Nickl P, Muecksch F, Percivalle E, et al. Bispecific antibody neutralizes circulating SARS-CoV-2 variants, prevents escape and protects mice from disease 2 3. bioRxiv [Internet]. Cold Spring Harbor Laboratory; 2021 [cited 2021 Mar 28];2021.01.22.427567. 10.1101/2021.01.22.427567
- 77.Reuschl A-K, Thorne L, Zuliani Alvarez L, Bouhaddou M, Obernier K, Soucheray M, et al. Host-directed therapies against early-lineage SARS-CoV-2 retain efficacy against B.1.1.7 variant. bioRxiv Prepr Serv Biol 2021;10:9.
- 78.Bessalah S, Jebahi S, Mejri N, Salhi I, Khorchani T, Hammadi M. Perspective on therapeutic and diagnostic potential of camel nanobodies for coronavirus disease-19 (COVID-19). 3 Biotech; 2021. 10.1007/s13205-021-02647-5 [DOI] [PMC free article] [PubMed]
- 79.Wysocki J, Ye M, Hassler L, Gupta AK, Wang Y, Nicoleascu V, et al. A Novel Soluble ACE2 Variant with Prolonged Duration of Action Neutralizes SARS-CoV-2 Infection in Human Kidney Organoids. J Am Soc Nephrol. 2021;ASN.2020101537. www.jasn.org [DOI] [PMC free article] [PubMed]
- 80.Wysocki J, Ye M, Soler MJ, Gurley SB, Xiao HD, Bernstein KE, et al. ACE and ACE2 activity in diabetic mice. Diabetes. 2006;55:2132–2139. doi: 10.2337/db06-0033. [DOI] [PubMed] [Google Scholar]
- 81.Higuchi Y, Suzuki T, Arimori T, Ikemura N, Kirita Y, Ohgitani E, et al. High affinity modified ACE2 receptors prevent SARS-CoV-2 infection [Internet]. bioRxiv. bioRxiv; 2020 [cited 2021 Mar 28]. p. 2020.09.16.299891. 10.1101/2020.09.16.299891
- 82.Chan KK, Dorosky D, Sharma P, Abbasi SA, Dye JM, Kranz DM, et al. Engineering human ACE2 to optimize binding to the spike protein of SARS coronavirus 2. Science (80- ) 2020 ;369:1261–5 [DOI] [PMC free article] [PubMed]
- 83.Twomey JD, Luo S, Dean AQ, Bozza WP, Nalli A, Zhang B. COVID-19 update: The race to therapeutic development. Drug Resist. Updat. Churchill Livingstone; 2020. p. 100733. [DOI] [PMC free article] [PubMed]
- 84.Shang C, Zhuang X, Zhang H, Li Y, Zhu Y, Lu J, et al. Inhibitors of endosomal acidification suppress SARS-CoV-2 replication and relieve viral pneumonia in hACE2 transgenic mice. Virol J. 2021;18:46. doi: 10.1186/s12985-021-01515-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Deng Q, Rasool R ur, Russell RM, Natesan R, Asangani IA. Targeting androgen regulation of TMPRSS2 and ACE2 as a therapeutic strategy to combat COVID-19. iScience 2021;24:102254. [DOI] [PMC free article] [PubMed]
- 86.Haga S, Nagata N, Okamura T, Yamamoto N, Sata T, Yamamoto N, et al. TACE antagonists blocking ACE2 shedding caused by the spike protein of SARS-CoV are candidate antiviral compounds. Antiviral Res. 2010;85:551–555. doi: 10.1016/j.antiviral.2009.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Agostini ML, Andres EL, Sims AC, Graham RL, Sheahan TP, Lu X, et al. Coronavirus susceptibility to the antiviral remdesivir (GS-5734) is mediated by the viral polymerase and the proofreading exoribonuclease. MBio. 2018;9:221–239. doi: 10.1128/mBio.00221-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Heydari H, Golmohammadi R, Mirnejad R, Tebyanian H, Fasihi-Ramandi M, Moosazadeh-Moghadam M. Antiviral peptides against Coronaviridae family: A review. Peptides;139:170526 [DOI] [PMC free article] [PubMed]
- 89.Pachetti M, Marini B, Benedetti F, Giudici F, Mauro E, Storici P, et al. Emerging SARS-CoV-2 mutation hot spots include a novel RNA-dependent-RNA polymerase variant. J Transl Med. 18:179. 10.1186/s12967-020-02344-6 [DOI] [PMC free article] [PubMed]
- 90.Goldhill DH, Te Velthuis AJW, Fletcher RA, Langat P, Zambon M, Lackenby A, et al. The mechanism of resistance to favipiravir in influenza. Proc Natl Acad Sci U S A. 2018;115:11613–11618. doi: 10.1073/pnas.1811345115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Young KC, Lindsay KL, Lee KJ, Liu WC, He JW, Milstein SL, et al. Identification of a ribavirin-resistant NS5B mutation of hepatitis C virus during ribavirin monotherapy. Hepatology. 2003;38:869–878. doi: 10.1002/hep.1840380413. [DOI] [PubMed] [Google Scholar]
- 92.Abbott TR, Dhamdhere G, Liu Y, Lin X, Goudy L, Zeng L, et al. Development of CRISPR as an Antiviral Strategy to Combat SARS-CoV-2 and Influenza. Cell. 2020;181:865–876.e12. doi: 10.1016/j.cell.2020.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.