Abstract
Background
It has been widely reported that the prognostic nutritional index (PNI) played a pivotal role in nutritional assessment of surgical patients and tumor prognosis. In order to improve the accuracy of evaluation in Western China, we established reference intervals (RIs) of PNI in healthy controls.
Methods
A retrospective cohort study on healthy ethnic Han adults (18–79 years) was conducted to explore the influences of age, gender, study centers, and instruments on PNI and to establish RIs. The data came from a healthy routine examination center database and laboratory information system (LIS) of four centers in Western China, and there were 200 persons selected randomly for verification of RIs.
Results
Five thousand eight hundred and thirty‐nine healthy candidates were enrolled. PNI showed a marked gender dependence, and males had significantly higher PNI than females across all ages (p < 0.01). We found that PNI is significantly different between age groups (p < 0.01), the value of PNI tended to decrease with age increasing. There is also an obvious influence of centers and instruments on PNI (p < 0.01).
Conclusions
We established reference intervals of PNI in healthy Han Chinese population in Western China and validated successfully. Further established RIs will lead to better standardizations of PNI for clinical applications.
Keywords: cohort study, multi‐center study, observational study, prognostic nutritional index, reference interval
A retrospective cohort study on healthy ethnic Han adults (18–79 years) was conducted to explore the influences of age, gender, study centers, and instruments on prognostic nutritional index (PNI) and to establish reference intervals (RIs). We established reference intervals of PNI in healthy Han Chinese population in Western China, and validated successfully. Further established RIs will lead to better standardizations of PNI for clinical applications.

1. INTRODUCTION
Serum albumin is an objective nutritional indicator reflecting the body's protein reserve level, while total lymphocyte count is also an important indicator of patients’ nutrition and immunity. PNI based on serum ALB levels and total peripheral blood lymphocytes was originally used to assess the nutritional and immune status of surgical patients and predict surgical risks. 1 Patients with low PNI scores often have a poor prognosis after gastrointestinal surgery and undergo postoperative complications. 2 However, it was further applied to assess the nutritional status of different types of cancer patients 3 : esophageal carcinoma, 4 gastric cancer, 5 and lung cancer. 6 In addition, recent studies have shown that PNI is associated with the prognosis of specific lymphoma patients, such as diffuse large B‐cell lymphoma (DLBCL) 7 and Extranodal natural killer/T‐cell lymphoma (ENKTL). 8
However, there are few studies that have attempted to derive the normal reference intervals in healthy adults, and the roles of age, gender, and instrument on PNI have not been reported widely. Recently, the test results of blood indicators have also shown obvious regional differences; a previous study has reported that there is an obvious lower platelet count in Chengdu city compared with other regions in China. 9 It is absolutely urgent to establish RIs of PNI to apply it to clinical applications more standard and efficiently for healthy persons in Western China.
2. MATERIALS AND METHODS
2.1. Experimental arrangement
The Department of clinical laboratory of Sichuan Cancer Hospital & Institute leaded to establish reference intervals of prognostic major clinical laboratory items in the Han Chinese population in Western China. A total of four centers were selected to participate in this research study: Chengdu Fifth People's Hospital, the First people's Hospital of Yibin, People's Hospital of Jianyang city, and Zigong First people's Hospital. Each hospital was responsible for selecting healthy local candidates, performing tests and collecting samples, and the department of clinical laboratory of Sichuan Cancer Hospital & Institute was responsible for project quality assurance.
2.2. Inclusion and exclusion of subjects
Since the PNI was not completely distributed normally, and a two‐sided reference intervals need to be established, we calculated the minimum sample size required based on the formula: , proposed by Jennen‐Steinmetz. 10 In the formula, δ represents the allowable error, and η is a new statistic constructed when estimating the sample size, and there is no standard value range which generally taken as 0.9 and q represents the width of the reference value range. When r = 0.03, η = 0.9, and q = 0.95, the minimum sample size was calculated to be 74. The number of subjects recruited by four centers was supposed to exceed 74, respectively.
A retrospective study retrieved the health examination center database and laboratory information system (LIS) of four centers which had been mentioned above, to enroll healthy ethnic Han individuals between 18 and 79 years of age, who took health examination between January 2017 and June 2017. Healthy candidates were finally selected based on the inclusion and exclusion criteria as Table 1.
TABLE 1.
Inclusion and exclusion criteria
| Inclusion criteria |
|
. Age >18 years and <79 years. |
|
. Availability of complete required data. |
|
. Ethnic Han population. |
|
. Matched individuals with age and gender (which mean that gender groups (male group and female group) and every subgroup (18–29, 30–39, 40–49, 50–64 and 65–79 years subgroups) to have an approximately equal number of the individuals.) |
| Exclusion criteria |
|
. Presence of any known medical condition (comorbidities). |
|
. Pregnancy. |
|
. History or continued use of alcohol, tobacco, or oral contraceptives. |
|
. Abnormal results of clinical laboratory, such as white blood cell count <3.0 × 109/L or >12.5 × 109/L, Abnormal urinalysis results, etc. |
|
. Any surgery within 6 months after enrollment. |
|
. Blood donation or transfusion within 4 months of enrollment. |
|
. Body mass index (BMI)>28 kg/m2. |
After applying the inclusion and exclusion criteria from LIS, 34,931 individuals were recruited, and 5,839 of them were enrolled in the final analysis (Figure 1). The included subjects were further divided into a training group (consisting of 5,639 subjects) and a validation group (consisting of 200 subjects), and each training group comprised the following: 18–29, 30–39, 40–49, 50–64, and 65–79 years (Table 2).
FIGURE 1.
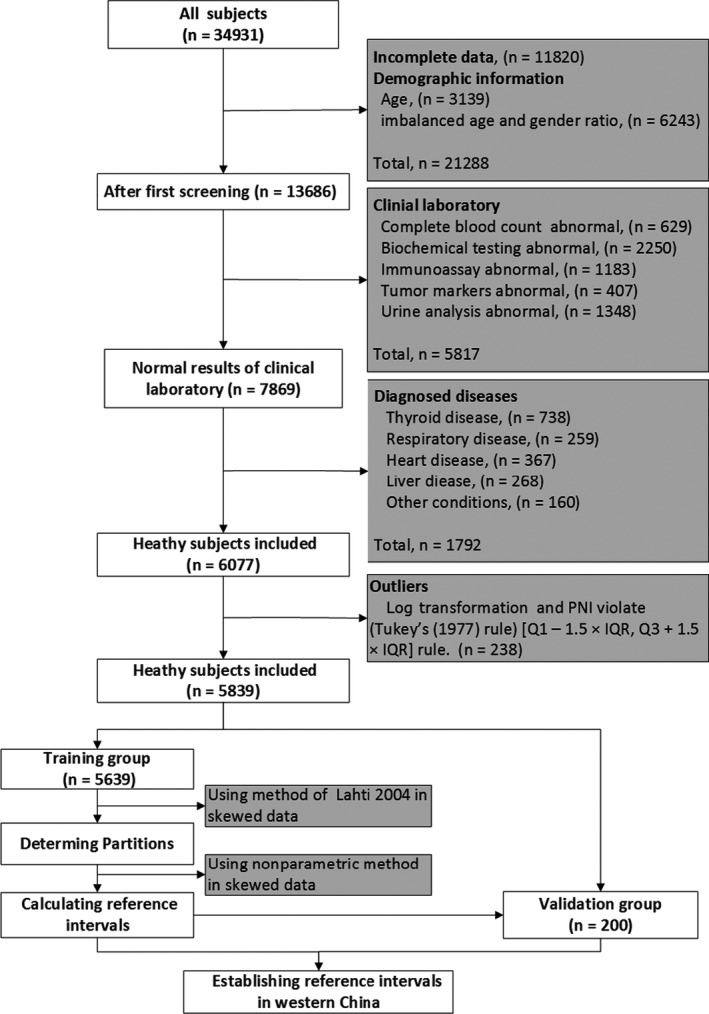
Flowchart of inclusion and exclusion of subjects to establish the reference intervals
TABLE 2.
Age‐partitioned reference intervals and 95% confidence intervals in training group
| Age (years) | All | Hit‐Sys | Sie‐Mir | Hit‐Mir | CRIs | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2.5th | 97.5th | 2.5th | 97.5th | 2.5th | 97.5th | 2.5th | 97.5th | 2.5th | 97.5th | |
| 18–29 | 51.4 (50.6–52.0) | 66.3 (65.8–66.8) | 50 (49.6–51.1) | 65.6 (63.8–66.3) | 53.3 (52.7–54.1) | 66.3 (64.9–67.7) | 53.3 (52.4–55.1) | 66.9 (66.0–67.8) | 48.7 (NA) | 70.6 (NA) |
| 30–39 | 50.2 (49.8–50.6) | 65.3 (64.3–66.2) | 49.7 (48.4–50.1) | 62.9 (62.3–63.7) | 51.1 (50.5–52.6) | 66.8 (65.4–67.7) | 52.1 (51.3–52.7) | 66.5 (65.1–67.6) | ||
| 40–65 | 49.4 (48.9–49.9) | 64.0 (63.6–64.3) | 48.7 (48.5–49.2) | 63.4 (62.8–64.1) | 50.5 (50.2–51.4) | 64.7 (64.2–65.8) | 50.4 (50.2–51.4) | 64.7 (64.2–65.8) | ||
| 65–79 | 48.1 (47.5–49.0) | 64.0 (63.3–64.2) | 47.9 (47.4–48.4) | 49.5 (47.8–50.6) | 49.5 (47.8–50.6) | 64.4 (63.5–65.5) | 51.7(51.7,54.0) | NA | ||
Abbreviations: CRIs, calculated RIs which were Calculated by data from published literature (PMID: 25769040 and PMID:24058449); Hit, Hitachi; Mir, Mindray; NA, not available; Sie, Siemens; Sys, Sysmex.
2.3. Instruments and measurement parameters
Lymphocyte count was analyzed by BC‐6600 (Mindray Medical Electronics Co.), and serum albumin value was measured by Sie‐2400 biomedical analyzer (Siemens AG) in Jianyang center. The BC‐6900 hematology analyzer (Mindray Medical Electronics Co.) was used to detect the lymphocyte count, and Hit‐008008 biomedical analyzer (Hitachi Construction Machinery) was applied to detect serum albumin in Chengdu center. While the lymphocyte count was detected by XN‐1000 hematology analyzers (Sysmex Corp.), and the serum albumin was measured by Hit‐7600 biomedical analyzer (Hitachi Construction Machinery) in Yibin and Zigong centers.
Each candidate fasted for solids and liquids for at least 12 h. Blood from each participant was drawn into appropriate blood collection tubes by using vacuum tube needles, and the K2‐EDTA tubes were used for lymphocyte count, while plain tubes were used for estimating albumin value. Samples collected in plain tubes were separated by centrifugation at 3,000 rpm for 5 min. After collection, all specimens were supposed to be tested within 1 h. The PNI was calculated according to the formula: PNI = serum albumin value (g/L) + 0.005 × peripheral lymphocyte count (MM3).
2.4. Identification and validation
For identification of RIs, the value of PNI of all subjects included was calculated based on the formula which was above‐mentioned, and we log transform the value of PNI after calculating the value. The Tukey's (1977) [Q1‐1.5 × IQR,Q3 + 1.5 × IQR] rule was used for insuring the reference values against outliers. 11 We made decisions on partitioning by following Ari Lahti et al’ proportion criteria: The subgroup‐specific reference intervals should be calculated, if at least one of the four proportions of the subgroup distributions cutoff by the reference limits of the combined distribution exceeds 4.1% or lies below 0.9%. 12 In the training group, the RIs (2.5th, 97.5th) of PNI by the nonparametric methods, while the validation group was utilized to verify the established RIs. Outsider rate of validation group<0.10 is considered successfully and efficient established.
2.5. Statistics
The data were analyzed with the statistical programming language R and IBM SPSS Statistics version 20.0 software (IBM Corp.). 13 Data were finally reported as a median and interquartile range (IQR), 2.5 percentile and 97.5 percentile, appropriately. And the normal distribution was analyzed by using the Kolgomorov‐Smirnov test. Mann‐Whitney U test and Kruskal‐Wallis test were applied for comparisons of two or more than two groups, while the ggplot2 package was applied to data visualization. 14 We established age‐partitioned reference intervals for PNI based on significant correlation and visual identification of the relationship between age and PNI. We calculated 95% of reference intervals by bootstrap in IBM SPSS Statistics version 20. All p values <0.05 were considered statistically significant.
3. RESULTS
3.1. Study population summary
As showed in Figure 1, a total of 34,931 candidates were collected, and 5,839 subjects were selected for our study based on the inclusion and exclusion. The most common exclusions were incomplete data (n = 11,820), unmatched age and gender (n = 6,243), age (n = 3,139), clinical laboratory (n = 5,817), diagnose diseases (n = 1,792), and outliers (n = 238). A total of 2,728(46.72%) females and 3,111 (53.28%) males were finally collected; the average age was 44.7 years, with a standard deviation (SD) of 15.2 years, of whom were randomly divided into training group and validation group for the establishment and validation of the reference intervals.
The coefficient of variation (CV) of peripheral lymphocyte count, serum albumin value, and PNI were calculated in 5,839 subjects, according to the formula as follows: PNI = serum albumin value (g/L) + 0.005 × peripheral lymphocyte count (MM3). The results were 13.91%, 6.37%, and 6.89%, respectively.
There were 3,006(53.31%) males and 2,633(46.69%) females in the training group, and the average age of the subjects was 44.5, with a SD of 15.1 years in this group, while in the validation group, there were 105(52.5%) males and 95(47.5%) females, and the average age of the subjects was 50.6 years, with a SD of 17.3 years (Figure 2). We found that PNI was not completely distributed normally (data are not shown) following Kolmogorov‐Smirnov test. All p values<0.05 were considered statistically significant.
FIGURE 2.
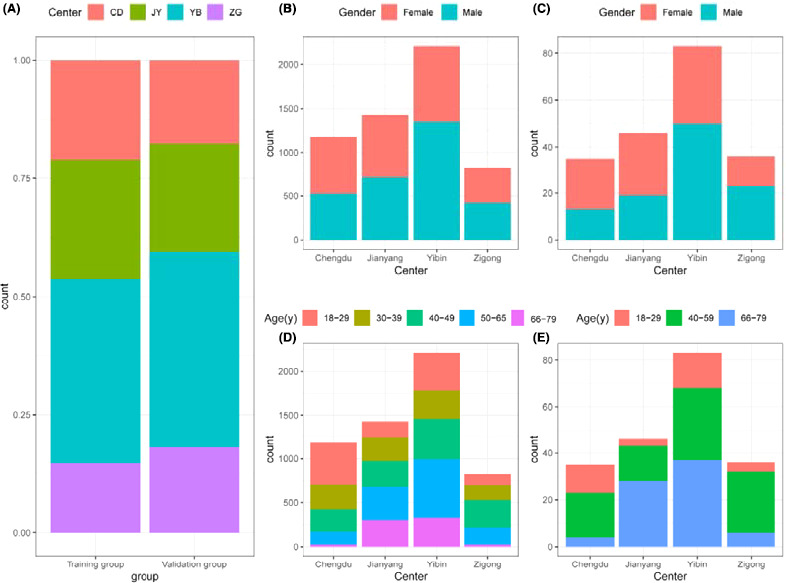
The distribution of candidates from each center, different genders, and age groups in the training group and validation group
3.2. Gender‐ and age‐related findings
We analyzed the influence of gender on PNI in the training group, and the significant difference was observed in PNI parameter between the males and females (p < 0.05; Figure 3A). While none of the four proportions of the subgroup distribution cutoff by the reference limits of the combined distribution exceeded 4.1% (Table S1), thus, we concluded that the PNI could be combined to calculate the consensus intervals, regardless of gender.
FIGURE 3.
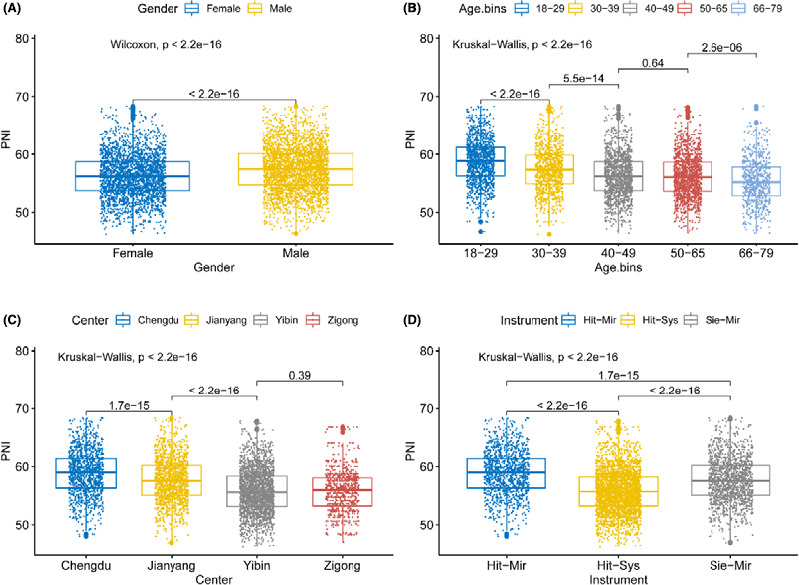
The boxplot of PNI stratified by gender, age, center, and instrument in training group. Our boxplot is not a standardized way and displays the distribution of data based on the three numbers summary: first quartile, median, third quartile
We analyzed the influence of age on PNI in the training group as well, and we found that the PNI was significantly influenced by age (Figure 4), while the difference was not observed between 40 and 49 subgroup and 50–65 subgroup (all p < 0.05; Figure 3B). Thus, we combined the two subgroups into a new group: 40–65 subgroup. In partitioning analysis, the largest one of the subgroup proportions outside a common reference limit is 6%, which exceeded 4.1% (Table S1). It shows that establishing the reference interval of PNI should consider the factor of age.
FIGURE 4.
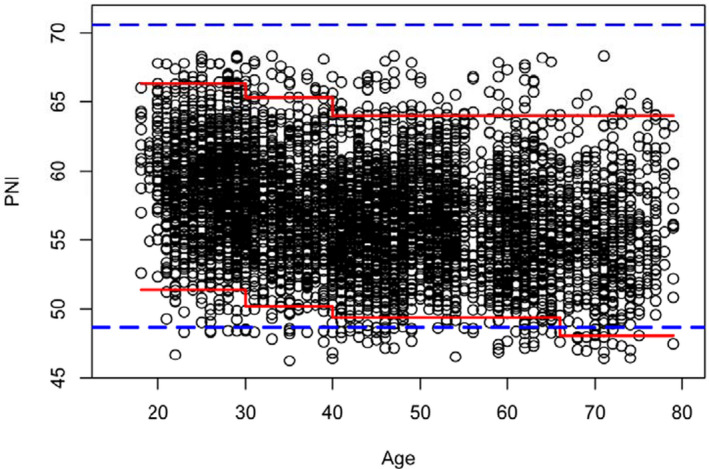
The scatter plot to show the association between PNI and age in training group. Partitioned intervals are shown with the red stepped line, and the existing unpartitioned interval is shown with the black dashed line. Individual points are shown as black circles
3.3. Center‐related and Instrument‐related findings
Except for Zigong and Yibin centers, there were significant differences among the other centers in PNI (all p < 0.05; Figure 3C). The main reason might be the same Instrument: Sysmex® instrument and Hitachi© instrument were used in Yibin and Zigong center. Moreover, it can be clearly observed that the median value of PNI produced by Sie‐Mir® instrument was significantly lower than the value produced with Hit‐Mir© instrument, while higher than the value produced with Hit‐Sys© instrument (all p < 0.05, Figure 3D). However, one of the Hit‐Mir subgroup distribution cutoffs by the reference limits of the combined distribution is 6%, which exceeded 4.1% (Table S1). Therefore, the factor of instrument should be considered when the reference intervals of PNI were calculated.
3.4. Establishing final consensus intervals
Reference intervals (2.5th, 97.5th) and corresponding 95% confidence intervals of PNI were established in the training group (Table 2), with nonparametric methods. In addition, we further included a number of 200 healthy candidates to validate the reference intervals (Table 3). We finally found that proportions of outsiders which are validation values below or beyond established RIs are all <0.01 (Table 3), which means RIs of PNI are successfully and efficient established.
TABLE 3.
Validation results of reference intervals of PNI
| Groups | NO. | Range | <DL(n) | >UL(n) | NO. of outsider | OR |
|---|---|---|---|---|---|---|
| 18–29y & Hit‐Sys | 19 | 51.3–65.8 | 0 | 1 | 1 | 0.05 |
| 18–29y & Sie‐Mir | 3 | 59.8–61.7 | 0 | 0 | 0 | 0 |
| 18–29y & Hit‐Mir | 12 | 56.8–64.0 | 0 | 0 | 0 | 0 |
| 40–65y & Hit‐Sys | 57 | 47.2–66.8 | 2 | 3 | 5 | 0.088 |
| 40–65y & Sie‐Mir | 15 | 54.4–65.1 | 0 | 1 | 1 | 0.067 |
| 40–65y & Hit‐Mir | 19 | 53.5–61.5 | 0 | 0 | 0 | 0 |
| 65–79y & Hit‐Sys | 43 | 46.3–62.1 | 2 | 0 | 2 | 0.046 |
| 65–79y & Sie‐Mir | 28 | 49.1–68.2 | 1 | 1 | 2 | 0.071 |
| 65–79y & Hit‐Mir | 4 | 54.4–63.3 | 0 | NA | NA | NA |
Abbreviations: A, adults; DL, down‐limit; F, female; M, male; OA, old‐adults; OR, outsider –rate; UL, upper‐limit.
4. DISCUSSION
4.1. Main finding
In this research, we defined the values of PNI in four centers with a large population. It was found that the values of PNI decreased with age and varied in different instrument. So, RIs for PNI based on age and instrument were observed in the Han population of Western China.
4.2. Interpretation
The value of PNI reflects the nutritional status and immune status of the patient, which have profound effects on treatment options and quality of life. A low PNI value indicates that the patient is malnourished and has poor immune function. 15 Serum albumin related to PNI value is the important indicator reflecting the nutritional status of the body, the other related factor: Lymphocytes, which participate in the host's immune mechanism to prevent infection by mediating cellular immunity, are an important indicator of the body's immune function. Malnutrition is associated with postoperative complications, can lead to longer wound healing times, and may also be related to impaired immune function. 16 , 17 , 18 Therefore, monitoring the body's nutrition and immune status has guiding significance for the efficacy and prognosis judgment.
In this study, we defined the normal RIs of PNI in Western China by using a large population‐based multi‐center study in the training group, and validated the RIs in another small group included new candidates with the same conditions in. Meanwhile, we further studied the effect of study center, instruments, gender, and age for RIs of PNI in Western China. We found that the value of PNI changed significantly with gender and age; in addition, there is profound influence of study center and instruments. As all known, with advancing age, there is an increased risk of developing nutritional deficiencies, which could explain the decreasing PNI with increasing age. The bleeding during menstrual cycle might bring the nutritional deficiency, which indicates the lower value of PNI in female. Due to the laboratory conditions, including instrument, reagent, and operators, there might be different among the different center.
4.3. Strength and limitation
In the past studies on PNI, there is no unified algorithm for the critical value of PNI. Some studies 19 , 20 , 21 choose 45 ~ 49 as the critical value based on experience, while others 22 may draw the ROC curve to obtain the corresponding maximum Youden index to figure out the cutoff value. It is obvious that our research has developed a reasonable PNI reference value range through a comprehensive study of various factors, which is more clinically meaningful.
However, there are still some limitations in our research. On the one hand, our study is a retrospective study rather than a prospective study, all the data came from the health examination center database. It is difficult to prospectively collect more basic clinical characteristics of the subjects during the study. Individuals with different lifestyle, food habits, and socio‐economic status may have different serum albumin value and peripheral lymphocyte count, indicating that they may be in different nutrition and immune status, which may play an impact on the value of PNI to a certain extent. Therefore, in the further research, the influence of these covariates on the reference interval establishment is supposed to be taken into consideration. On the other hand, even though we validated the RIs in a validation group, a larger validation group need to be set in the future work.
5. CONCLUSION
In summary, there is an obvious influence of centers, instruments, age, and gender on the value of PNI, while the variations were not clinically significant for the subjects. We establish RIs of PNI in a big‐data‐based way in our multi‐center study for healthy Han Chinese populations in Western China. It will benefit experimental design of the related prognosis analyses a lot and lead to better standardizations of PNI for their clinical applications, which is supposed to be promoted into the routine CBC report.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest.
Supporting information
Table S1
Guishu Yang, Dongsheng Wang, Linbo He, Guangjie Zhang, Jianhong Yu, Yaping Chen, Tian Li, Ying Lin and Huaichao Luo contributed equally to this work.
Funding information
This study was supported by the Health and Family Planning Commission of Sichuan Province universal application project (No.20PJ115) and the Science and Technology Bureau of Chengdu technological innovation project (NO. 2019‐YF05‐01279‐SN)
Contributor Information
Tian Li, Email: tian@fmmu.edu.cn, Email: fmmult@foxmail.com.
Ying Lin, Email: liny042000@aliyun.com.
Huaichao Luo, Email: luo1987cc@163.com.
DATA AVAILABILITY STATEMENT
All data and materials are available upon reasonable request from the corresponding author.
REFERENCES
- 1. Buzby GP, Mullen JL, Matthews DC, Hobbs CL, Rosato EF. Prognostic nutritional index in gastrointestinal surgery. Am J Surg. 1980;139(1):160‐167. [DOI] [PubMed] [Google Scholar]
- 2. Murakami Y, Saito H, Kono Y, et al. Combined analysis of the preoperative and postoperative prognostic nutritional index offers a precise predictor of the prognosis of patients with gastric cancer. Surg Today. 2018;48(4):395‐403. [DOI] [PubMed] [Google Scholar]
- 3. Oh CA, Kim DH, Oh SJ, et al. Nutritional risk index as a predictor of postoperative wound complications after gastrectomy. World J Gastroenterol. 2012;18(7):673‐678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Nozoe T, Kimura Y, Ishida M, Saeki H, Korenaga D, Sugimachi K. Correlation of pre‐operative nutritional condition with post‐operative complications in surgical treatment for oesophageal carcinoma. Eur J Surg Oncol. 2002;28(4):396‐400. [DOI] [PubMed] [Google Scholar]
- 5. Watanabe M, Iwatsuki M, Iwagami S, Ishimoto T, Baba Y, Baba H. Prognostic nutritional index predicts outcomes of gastrectomy in the elderly. World J Surg. 2012;36(7):1632‐1639. [DOI] [PubMed] [Google Scholar]
- 6. Jang HJ, Song JW, Cho S, Kim K, Jheon S. Prognostic implications of postoperative infectious complications in non‐small cell lung cancer. Korean J Thorac Cardiovasc Surg. 2018;51(1):41‐52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Periša V, Zibar L, Knezović A, Periša I, Sinčić‐Petričević J, Aurer I. Prognostic nutritional index as a predictor of prognosis in patients with diffuse large B cell lymphoma. Wien Klin Wochenschr. 2017;129(11–12):411‐419. [DOI] [PubMed] [Google Scholar]
- 8. Chen K‐L, Liu Y‐H, Li W‐Y, et al. The prognostic nutritional index predicts survival for patients with extranodal natural killer/T cell lymphoma, nasal type. Ann Hematol. 2015;94(8):1389‐1400. [DOI] [PubMed] [Google Scholar]
- 9. Wu X, Zhao M, Pan B, et al. Complete blood count reference intervals for healthy Han Chinese adults. PLoS One. 2015;10(3):e0119669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Jennen‐Steinmetz C, Wellek S. A new approach to sample size calculation for reference interval studies. Stat Med. 2005;24(20):3199‐3212. [DOI] [PubMed] [Google Scholar]
- 11. Hoaglin DC, Iglewicz B. Fine‐tuning some resistant rules for outlier labeling. J Am Stat Assoc. 1987;82(400):1147‐1149. [Google Scholar]
- 12. Lahti A, Petersen PH, Boyd JC, Rustad P, Laake P, Solberg HE. Partitioning of nongaussian‐distributed biochemical reference data into subgroups. Clin Chem. 2004;50(5):891‐900. [DOI] [PubMed] [Google Scholar]
- 13. Ginestet C. ggplot2: elegant graphics for data analysis. Journal of the Royal Statistical Society: Series A (Statistics in Society). 2011;174(1):245‐246. [Google Scholar]
- 14. McCudden CR, Brooks J, Figurado P, Bourque PR. Cerebrospinal fluid total protein reference intervals derived from 20 years of patient data. Clin Chem. 2017;63(12):1856‐1865. [DOI] [PubMed] [Google Scholar]
- 15. Okada S, Shimada J, Teramukai S, et al. Risk stratification according to the prognostic nutritional index for predicting postoperative complications after lung cancer surgery. Ann Surg Oncol. 2018;25(5):1254‐1261. [DOI] [PubMed] [Google Scholar]
- 16. Leedo E, Gade J, Granov S, et al. The effect of a home delivery meal service of energy‐ and protein‐rich meals on quality of life in malnourished outpatients suffering from lung cancer: a randomized controlled trial. Nutr Cancer. 2017;69(3):444‐453. [DOI] [PubMed] [Google Scholar]
- 17. Kiss N. Nutrition support and dietary interventions for patients with lung cancer: current insights. Lung Cancer (Auckl). 2016;7:1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mohan A, Poulose R, Kulshreshtha I, et al. High prevalence of malnutrition and deranged relationship between energy demands and food intake in advanced non‐small cell lung cancer. Eur J Cancer Care (Engl). 2017;26(4):e12503. [DOI] [PubMed] [Google Scholar]
- 19. Mohri Y, Inoue Y, Tanaka K, Hiro J, Uchida K, Kusunoki M. Prognostic nutritional index predicts postoperative outcome in colorectal cancer. World J Surg. 2013;37(11):2688‐2692. [DOI] [PubMed] [Google Scholar]
- 20. Inoue M, Okada S. Correspondence regarding "Is the prognostic nutritional index (PNI) a useful predictive marker for postoperative complications after lung surgery?" by Dr. X Li and J Chen. J Thorac Dis. 2019;11(Suppl 3):S472‐S473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Li X, Chen J. Is the prognostic nutritional index (PNI) a useful predictive marker for postoperative complications after lung surgery? J Thorac Dis. 2019;11(Suppl 3):S334‐S336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Gao J, Wang Y, Li F, et al. Prognostic nutritional index and neutrophil‐to‐lymphocyte ratio are respectively associated with prognosis of gastric cancer with liver metatasis undergoing and without hepatectomy. Biomed Res Int. 2019;2019:4213623. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1
Data Availability Statement
All data and materials are available upon reasonable request from the corresponding author.


