Abstract
Objectives
The psychological impact of the COVID-19 pandemic on doctors is a significant concern. Due to the emergence of multiple pandemic waves, longitudinal data on the impact of COVID-19 are vital to ensure an adequate psychological care response. The primary aim was to assess the prevalence and degree of psychological distress and trauma in frontline doctors during the acceleration, peak and deceleration of the COVID-19 first wave. Personal and professional factors associated with psychological distress are also reported.
Design
A prospective online three-part longitudinal survey.
Setting
Acute hospitals in the UK and Ireland.
Participants
Frontline doctors working in emergency medicine, anaesthetics and intensive care medicine during the first wave of the COVID-19 pandemic in March 2020.
Primary outcome measures
Psychological distress and trauma measured using the General Health Questionnaire-12 and the Impact of Events-Revised.
Results
The initial acceleration survey distributed across networks generated a sample of 5440 doctors. Peak and deceleration response rates from the original sample were 71.6% (n=3896) and 56.6% (n=3079), respectively. Prevalence of psychological distress was 44.7% (n=1334) during the acceleration, 36.9% (n=1098) at peak and 31.5% (n=918) at the deceleration phase. The prevalence of trauma was 23.7% (n=647) at peak and 17.7% (n=484) at deceleration. The prevalence of probable post-traumatic stress disorder was 12.6% (n=343) at peak and 10.1% (n=276) at deceleration. Worry of family infection due to clinical work was the factor most strongly associated with both distress (R2=0.06) and trauma (R2=0.10).
Conclusion
Findings reflect a pattern of elevated distress at acceleration and peak, with some natural recovery. It is essential that policymakers seek to prevent future adverse effects through (a) provision of vital equipment to mitigate physical and psychological harm, (b) increased awareness and recognition of signs of psychological distress and (c) the development of clear pathways to effective psychological care.
Trial registration number
Keywords: Accident & emergency medicine, adult anaesthesia, adult intensive & critical care, COVID-19, mental health
Strengths and limitations of this study.
This paper presents key findings from a large cross-sectional longitudinal survey of practising emergency, anaesthetic and intensive care doctors in the UK and Ireland during the acceleration, peak and deceleration of the first wave of the COVID-19 pandemic.
This study provides an insight into the personal and professional factors associated with trauma and distress and could be used to identify those doctors who will most benefit from psychological interventions.
Variation in regional peaks may have influenced accurate capturing of psychological distress and trauma rates and have not been accounted for.
The findings cannot be extrapolated to long-term psychological impact, and future work is planned to capture this.
Introduction
Clinicians providing frontline care have become central to the primary reception, assessment and ongoing hospital treatment of patients with suspected COVID-19. These include doctors working in emergency medicine (EM), anaesthetics and intensive care medicine (ICM). While this healthcare workforce is highly resilient and accustomed to facing traumatic situations, the COVID-19 pandemic has imposed unprecedented demands in workload intensity and personal health risk.1–4 High infection rates have been reported in frontline clinicians, with over 150 fatalities in the UK by May 2020.5 These factors are likely to affect psychological well-being, increasing the risk of traumatic stress both in the acute phase of the pandemic and at long-term follow-up.6–9 Exposure to infectious disease outbreaks and elevated psychological distress have previously been associated with increased sickness rates, absenteeism, impaired performance at work and the development of physical health problems.10–12 There is also an emerging evidence base from around the world of the psychological impact on healthcare workers.13–16 During the current COVID-19 pandemic, there has been a global media focus on health and care workers with widespread public support.17 However, there is increasing recognition among key opinion leaders and psychological societies that this pandemic will lead to an unparalleled, although as yet unquantified, impact on the psychological well-being of healthcare workers.18 19
Studies evaluating psychological well-being in frontline clinicians during infectious disease outbreaks (including COVID-19) have demonstrated negative impacts that may be significant.10 20 21 Systematic reviews and meta-analyses converge around common predictors of psychological distress following traumatic events, many of which are relevant to frontline clinicians. Key factors include preparedness, training, social and occupational support, exposure and threat to life, media use and history of mental health problems.1 7 21–23 However, these data have largely been collected as a snapshot either during or following outbreaks or as cross-sectional surveys in highly selected or self-selecting cohorts. Longitudinal data which describe evolving and cumulative effects on the psychological well-being of frontline working during the COVID-19 pandemic are therefore urgently required. Such studies are essential to understand and mitigate psychological impacts of future events on this vital workforce and inform the development of policy and interventions.
The primary aim of this study was to assess the prevalence and degree of psychological distress and trauma in doctors providing frontline care during the acceleration, peak and deceleration phases of the COVID-19 pandemic. We also sought to establish which personal and professional factors were significantly associated with psychological distress at these time points.
Methods
Study design and participants
The ‘COVID-19 Emergency Response Assessment (CERA) Study’ was a prospective online longitudinal survey of frontline doctors across the UK and Ireland undertaken during the acceleration, peak and deceleration phases of the first COVID-19 pandemic wave.24 Doctors of all grades working in EM, anaesthetics or ICM during the acceleration phase were invited to participate.
Procedures
This survey study is reported in line with Checklist for Reporting Results of Internet E-surveys guidelines.25 Full details of survey distribution, design, administration and time points are available in the published protocol.24 In brief, the survey was initially distributed during the acceleration phase of the first pandemic wave through research networks, training faculties or Royal College Networks via email or instant messaging groups, coordinated by identified site/region leads. The participation link was not shared on wider social media platforms, to avoid international contamination. At completion of the acceleration phase survey, participants entered personal email addresses for direct approach at peak and deceleration phases with a unique survey link to avoid duplication.
The acceleration, peak and deceleration surveys were developed iteratively by the study team and underpinned by evidence, or by consensus where necessary. Psychometric tools were selected by consensus of the study team, considering validity and utility of a range of standardised measures, balanced against the feasibility of delivery and completion by individuals likely to be working at maximum capacity.
Study data were collected and managed using Research Electronic Data Capture hosted at University Hospitals Bristol and Weston NHS Foundation Trust.26 27 Acceleration, peak and deceleration phases were defined a priori and adapted from the United States Centers for Disease Control ‘Preparedness and Response Frameworks for Influenza Pandemics’.28 For each survey, exact survey distribution dates were decided per protocol by team consensus according to available public health data on number of confirmed cases (acceleration phase; UK: 18 March 2020–26 March 2020, Ireland: 25 March 2020–02 April 2020), nationally available COVID-19 daily death rates (peak phase; UK: 21 April 2020–05 May 2020, Ireland: 28 April 2020–12 May 2020) and at 30 days after distribution of the peak phase survey (deceleration phase; UK: 03 June 2020–17 June 2020, Ireland: 10 June 2020–24 June 2020). Participants provided electronic informed consent for each survey.
Survey questions
Survey questions collected data for both the primary and secondary outcomes. Items included the General Health Questionnaire-12 (GHQ-12; provided with licence fee waived by GL Assessments, London, UK) for distress, and the Impact of Events Scale-Revised (IES-R; off licence) for trauma.
Personal and professional characteristics relating to participants’ current role, and their preparedness and experiences during the pandemic were collected. These were used as secondary outcome measures and are provided in full in the protocol and online supplemental file 1.24
bmjopen-2021-049680supp001.pdf (683.2KB, pdf)
Outcomes
There were two co-primary outcomes in this survey: psychological distress, and trauma, as defined by the GHQ-12 and the IES-R respectively.
Distress—GHQ-12
The GHQ-12 is a 12-item self-report measure devised to screen for psychological distress in the general population.29 The measure has high specificity and sensitivity, with reliability demonstrated across a range of populations.30 31 The GHQ-12 has been used in similar clinician-based studies measuring the psychological impact of infectious outbreaks and was chosen due to the brevity of the measure and its suitability for time-pressured medical staff.21 The GHQ-12 assesses current state and asks the participants to compare with usual state. GHQ-12 was asked at all three survey phases. Case-level distress is defined as a score of >3.30
Trauma—IES-R
The IES-R is a 22-item measure commonly used to measure post-traumatic stress following a prespecified traumatic incident and has been used to evaluate the impact of infectious disease outbreaks on hospital staff.21 32 It contains eight items that focus on ‘intrusion’, eight items on ‘avoidance’ and six items on ‘hyperarousal’. The IES-R was used at the peak and deceleration survey phases. A score of 24 or above indicates a clinically significant traumatic stress response, a score above 33 indicates best cut-off for a diagnosis of ‘probable post-traumatic stress disorder’ (PTSD).33 34
The secondary outcomes captured included personal and professional characteristics and their association with psychological distress and trauma. These personal and professional factors were identified through rapid literature review of high-quality systematic reviews and meta-analysis by experts in pandemic research.1 21–23 All factors identified as predictors of outcome were retained. This was supplemented by factors deemed of specific or emerging interest by the expert study steering committee. These were defined a priori in the study protocol, with the exception of ethnicity which was added during the peak survey due to the specific emergence of ethnicity as a potential marker of poor physical health outcomes.24
Statistical analysis
The statistical analysis is described in detail in the published protocol.24 GHQ-12 items were reported using two methods. In the first method, item responses are assigned to the values 0, 0, 1, 1 (from the most positive to the most negative sentiment) and summed to form an aggregate score from zero (least distressed) to 12 (most distressed). Using this method, a score of >3 is indicative of case-level distress.30 The second method assigns responses to 0, 1, 2, 3 (positive to negative sentiment) producing a score in the range 0–36, with zero representing the most healthy response (no psychological distress) and 36 the most unhealthy (maximal psychological distress). By presenting the two different scoring methods, we can both report the prevalence of case-level distress across the sample (0-0-1-1 scoring method) and more sensitively detect changes within the sample over the three phases of the pandemic (0-1-2-3 scoring method).
IES-R responses were analysed by assigning the responses to 0, 1, 2, 3, 4 (positive to negative) producing a score in the range 0 (no trauma) to 88 (maximal trauma). A score of 24 or above indicates a clinically significant traumatic stress response, a score above 33 indicates best cut-off for a diagnosis of ‘probable PTSD’.33 34
The change over time in the GHQ-12 (phases I, II and III) and IES-R scores (phases II and III) among participants who responded to all three surveys was examined with repeated measures linear mixed-effect models, with survey phase as the single fixed effect and a participant-level random effect. These model describe the association between pandemic phase and psychological distress (GHQ-12) and trauma (IES-R).
To identify potential modifiers of the change in GHQ-12-score or IES-R-score over time, further models were constructed for each of the measured personal and professional variables. Each model included the single variable of interest, survey phase, their interaction (to allow for a change in the association between the outcome and the variable over time) and a participant-level random effect as before. Responses where the variable value was missing were removed.35 Nagakawa’s marginal R2 was used to measure the proportion of outcome variance accounted for by the model (excluding random effects, ie, when there is no a priori knowledge of the expected outcome for each participant). Values vary from 0 to 1, with 1 occurring when the model perfectly predicts the outcome, and 0 occurring when the model only returns the population average.
Finally, a comparison analysis done to compare distress and trauma outcomes in those who completed all three surveys against those who dropped out.
Software
All analyses and statistical outputs were produced in the statistical programming language
R and the ‘tidyverse’, ‘lme4’ and ‘ggeffects’ packages were used for the mixed-effects models.36–38
Patient and public involvement
The study team contains frontline doctors from all represented specialties who undertook clinical work throughout the COVID-19 pandemic. This research is in line with recent RCEM research prioritisation and research recommendations.
Role of the funding source
The sponsor and funder had no role at any stage of this work.
Results
Distribution across networks in the UK and Ireland generated 5440 responses. Follow-up responses from the peak and deceleration surveys were 3896 (71.6%) and 3079 (56.6%), respectively (figure 1). The final analysis cohort was 3079 participants, consisting of 1686 (54.8%) from EM, 1114 (36.2%) from anaesthetics and 526 (17.1%) from ICM, with some participants working across multiple specialties.
Figure 1.
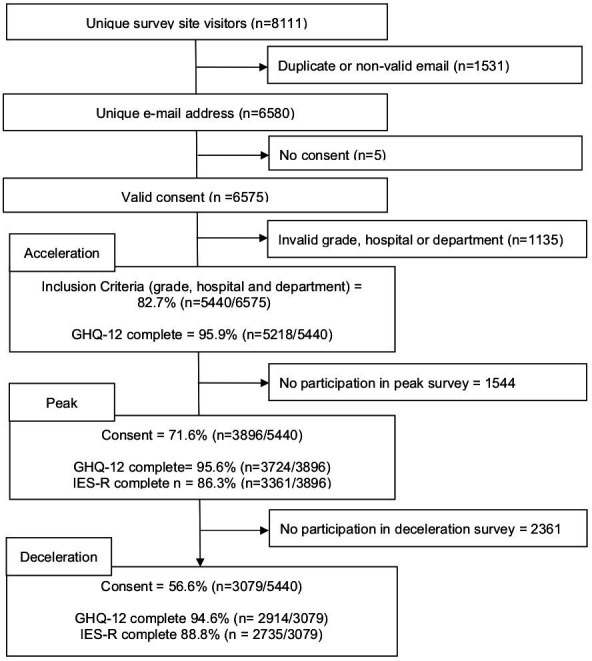
Participant flow chart. GHQ-12, General Health Questionnaire-12; IES-R, Impact of Events Scale-Revised.
The demographic and professional characteristics of the respondent population are summarised in table 1. The cohort was 51.0% female, with a median age group of 36–40 years, and was representative of all professional grades. Respondents were 63.7% ‘white British’, 6.2% ‘Irish’ and ‘30.1% ‘ethnic minority’; a full breakdown of ethnicity is provided in the online supplemental file 1 (https://github.com/wjchulme/TERN-CERA-study/tree/main/outputs).39 40
Table 1.
Demographic and occupational characteristics of responders who completed all three study phases
| All (n=3079) | Emergency medicine (n=1686) |
Anaesthetics (n=1114) |
Intensive care medicine (n=526) |
|
| Age (years) | ||||
| 20–25 | 111 (3.6%) | 99 (5.9%) | 3 (0.3%) | 9 (1.7%) |
| 26–30 | 737 (24.0%) | 471 (28.0%) | 184 (16.5%) | 130 (24.8%) |
| 31–35 | 682 (22.2%) | 366 (21.7%) | 242 (21.8%) | 141 (26.9%) |
| 36–40 | 497 (16.2%) | 279 (16.6%) | 177 (15.9%) | 81 (15.5%) |
| 41–45 | 406 (13.2%) | 220 (13.1%) | 156 (14.0%) | 55 (10.5%) |
| 46–50 | 282 (9.2%) | 128 (7.6%) | 133 (12.0%) | 55 (10.5%) |
| 51–55 | 203 (6.6%) | 72 (4.3%) | 121 (10.9%) | 27 (5.2%) |
| 56–60 | 107 (3.5%) | 34 (2.0%) | 63 (5.7%) | 19 (3.6%) |
| >60 | 49 (1.6%) | 14 (0.8%) | 33 (3.0%) | 7 (1.3%) |
| Missing | 5 | 3 | 2 | 2 |
| Gender | ||||
| Male | 1455 (48.8%) | 774 (47.4%) | 542 (50.1%) | 272 (53.8%) |
| Female | 1522 (51.0%) | 855 (52.4%) | 538 (49.7%) | 233 (46.0%) |
| Other | 7 (0.2%) | 4 (0.2%) | 2 (0.2%) | 1 (0.2%) |
| Missing | 95 | 53 | 32 | 20 |
| Seniority | ||||
| Junior doctor | 1089 (35.4%) | 692 (41.0%) | 276 (24.8%) | 187 (35.6%) |
| Middle grade doctor | 660 (21.4%) | 357 (21.2%) | 230 (20.6%) | 129 (24.5%) |
| Other senior doctor | 228 (7.4%) | 156 (9.3%) | 66 (5.9%) | 34 (6.5%) |
| Senior doctor (consultant grade) | 1102 (35.8%) | 481 (28.5%) | 542 (48.7%) | 176 (33.5%) |
| Geographical region | ||||
| East Midlands | 177 (5.7%) | 78 (4.6%) | 84 (7.5%) | 24 (4.6%) |
| East of England | 172 (5.6%) | 87 (5.2%) | 70 (6.3%) | 29 (5.5%) |
| London | 454 (14.7%) | 319 (18.9%) | 103 (9.2%) | 42 (8.0%) |
| North East | 132 (4.3%) | 68 (4.0%) | 47 (4.2%) | 30 (5.7%) |
| North West | 334 (10.8%) | 149 (8.8%) | 141 (12.7%) | 78 (14.8%) |
| South East | 355 (11.5%) | 229 (13.6%) | 105 (9.4%) | 48 (9.1%) |
| South West | 430 (14.0%) | 208 (12.3%) | 167 (15.0%) | 76 (14.4%) |
| West Midlands | 183 (5.9%) | 89 (5.3%) | 78 (7.0%) | 44 (8.4%) |
| Yorkshire and the Humber | 212 (6.9%) | 90 (5.3%) | 102 (9.2%) | 55 (10.5%) |
| Northern Ireland | 87 (2.8%) | 41 (2.4%) | 34 (3.1%) | 20 (3.8%) |
| Scotland | 253 (8.2%) | 159 (9.4%) | 80 (7.2%) | 32 (6.1%) |
| Wales | 92 (3.0%) | 21 (1.2%) | 62 (5.6%) | 21 (4.0%) |
| Dublin | 111 (3.6%) | 82 (4.9%) | 21 (1.9%) | 16 (3.0%) |
| Rest of Ireland | 87 (2.8%) | 66 (3.9%) | 20 (1.8%) | 11 (2.1%) |
| Nation | ||||
| England | 2449 (79.5%) | 1317 (78.1%) | 897 (80.5%) | 426 (81.0%) |
| Northern Ireland | 87 (2.8%) | 41 (2.4%) | 34 (3.1%) | 20 (3.8%) |
| Ireland | 198 (6.4%) | 148 (8.8%) | 41 (3.7%) | 27 (5.1%) |
| Scotland | 253 (8.2%) | 159 (9.4%) | 80 (7.2%) | 32 (6.1%) |
| Wales | 92 (3.0%) | 21 (1.2%) | 62 (5.6%) | 21 (4.0%) |
| Ethnicity | ||||
| White British | 1888 (63.7%) | 949 (58.4%) | 755 (70.3%) | 338 (67.1%) |
| Irish | 185 (6.2%) | 118 (7.3%) | 51 (4.7%) | 33 (6.5%) |
| Ethnic minority | 893 (30.1%) | 557 (34.3%) | 268 (25.0%) | 133 (26.4%) |
| Missing | 113 | 62 | 40 | 22 |
| Redeployed | ||||
| Yes | 249 (8.1%) | 47 (2.8%) | 196 (17.6%) | 20 (3.8%) |
| No | 2824 (91.9%) | 1636 (97.2%) | 916 (82.4%) | 504 (96.2%) |
| Missing | 6 | 3 | 2 | 2 |
Primary outcomes
General Health Questionnaire-12
The prevalence of psychological distress, as defined by scores >3 on the GHQ-12 0-0-1-1 scoring method, was 44.7% (n=1334) in the acceleration survey, 36.9% (n=1098) at peak and 31.5% (n=918) during the deceleration phase. Median GHQ-12 scores were 13.0 (Q1–Q3, 10.0–17.0), 13.0 (Q1–Q3, 9.0–16.0) and 12.0 (Q1–Q3, 9.0–16.0), respectively (figure 2), and mean scores were 13.7, 13.2 and 12.9 across the acceleration, peak and deceleration surveys. Median distress scores were higher in the anaesthetic and ICM cohorts at the acceleration phase when compared with EM, but these decreased in all three groups throughout the first pandemic wave.
Figure 2.
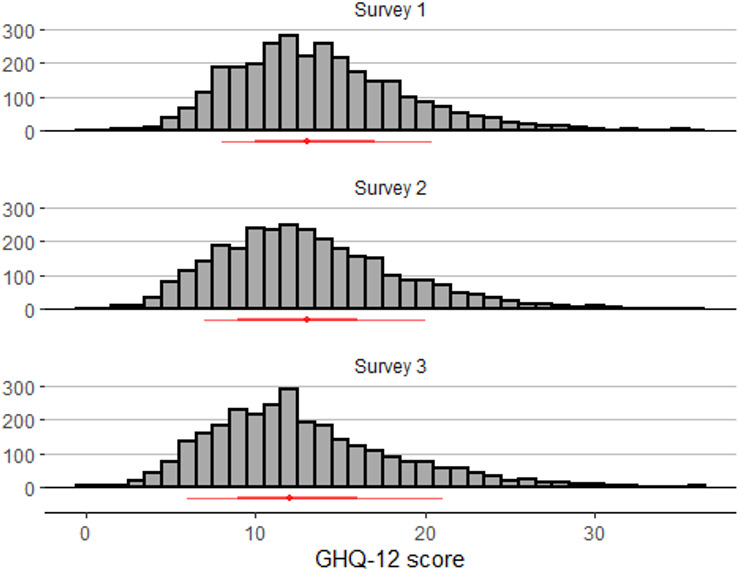
General Health Questionnaire-12 (GHQ-12) scores.
Impact of Events Scale-Revised
The prevalence of psychological trauma, as defined by a score of >24 on the IES-R, was 23.7% (n=647) at peak and 17.7% (n=484) at deceleration. The prevalence of ‘probable PTSD’, as defined by a score of >33 was 12.6% (n=343) at peak and 10.1% (n=276) at deceleration. During the peak phase, prevalence of trauma (>24) was 24.9% (n=378) in EM, 21.5% (n=204) in anaesthetics and 24.9% (n=117) in ICM. Prevalence of ‘probable PTSD’ (>33) was higher in EM (13.9%, n=211) and ICM (13.6%, n=64) when compared with anaesthetics (10.8%, n=103). During the deceleration phase, prevalence of trauma (>24) decreased to 19.7% (n=93) in ICM and 18.7% (n=285) in EM. ‘Probable PTSD’ (>33) decreased to 11.1% (n=169) in EM, compared with 10.8% (n=51) in ICM and 8.8% (n=85) in anaesthetics. The median IES-R was highest in the peak survey at 13 (Q1–Q3, 5–24), and 9 (Q1–Q3, 2–19) in the deceleration survey (see figure 3, table 2).
Figure 3.
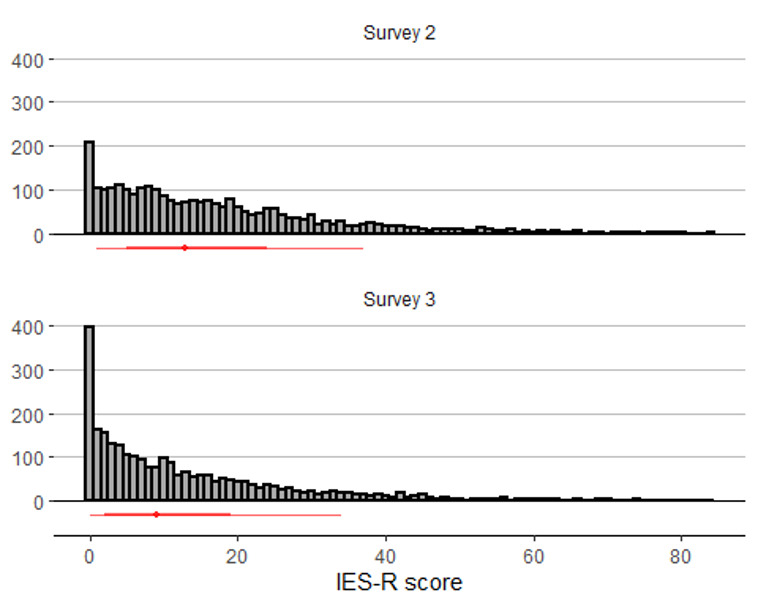
Impact of Events Scale-Revised (IES-R) scores.
Table 2.
GHQ-12 and IES-R scores for participants who responded to all three survey phases
| All (n=3079) | Emergency medicine (n=1686) |
Anaesthetics (n=1114) |
Intensive care medicine (n=526) |
|
| Acceleration | ||||
| GHQ-12 (0123 score) | ||||
| Mean | 13.7 | 13.3 | 14.4 | 14.0 |
| Median (Q1, Q3) | 13.0 (10.0, 17.0) | 13.0 (10.0, 16.0) | 14.0 (11.0, 18.0) | 14.0 (10.2, 17.0) |
| GHQ-12 (0011 >3) | ||||
| >3 | 1334 (44.7%) | 667 (40.7%) | 542 (50.2%) | 253 (49.6%) |
| N-Missing | 92 | 48 | 34 | 16 |
| Peak | ||||
| GHQ-12 (0123 score) | ||||
| Mean | 13.2 | 12.8 | 13.6 | 13.6 |
| Median (Q1, Q3) | 13.0 (9.0, 16.0) | 12.0 (9.0, 16.0) | 13.0 (10.0, 17.0) | 13.0 (10.0, 17.0) |
| GHQ-12 (0011 >3) | ||||
| >3 | 1098 (36.9%) | 543 (33.3%) | 454 (42.3%) | 211 (41.1%) |
| N-Missing | 105 | 56 | 40 | 13 |
| IES-R score | ||||
| Mean | 16.3 | 16.7 | 15.8 | 17.2 |
| Median (Q1, Q3) | 13.0 (5.0, 24.0) | 13.0 (5.0, 24.0) | 13.0 (6.0, 23.0) | 14.0 (6.0, 24.0) |
| IES-R >24 | ||||
| IES-R-0123 >24 | 647 (23.7%) | 378 (24.9%) | 204 (21.5%) | 117 (24.9%) |
| IES-R >33 | ||||
| IES-R-0123 >33 | 343 (12.6%) | 211 (13.9%) | 103 (10.8%) | 64 (13.6%) |
| N-Missing | 349 | 165 | 163 | 57 |
| Deceleration | ||||
| GHQ-12 (0123 score) | ||||
| Mean | 12.9 | 12.8 | 13.0 | 13.1 |
| Median (Q1, Q3) | 12.0 (9.0, 16.0) | 12.0 (9.0, 16.0) | 12.0 (9.0, 16.0) | 12.0 (9.0, 17.0) |
| GHQ-12 (0011 >3) | ||||
| >3 | 918 (31.5%) | 486 (30.2%) | 340 (32.6%) | 172 (34.6%) |
| N-Missing | 165 | 78 | 71 | 29 |
| IES-R score | ||||
| Mean | 13.2 | 13.6 | 12.6 | 14.2 |
| Median (Q1, Q3) | 9.0 (2.0, 19.0) | 9.0 (2.0, 20.0) | 8.0 (2.0, 18.0) | 9.0 (3.0, 20.0) |
| IES-R >24 | ||||
| IES-R-0123 >24 | 484 (17.7%) | 285 (18.7%) | 159 (16.5%) | 93 (19.7%) |
| IES-R >33 | ||||
| IES-R-0123 >33 | 276 (10.1%) | 169 (11.1%) | 85 (8.8%) | 51 (10.8%) |
| N-Missing | 344 | 164 | 153 | 53 |
GHQ-12, General Health Questionnaire-12; IES-R, Impact of Events Scale-Revised.
Secondary outcomes
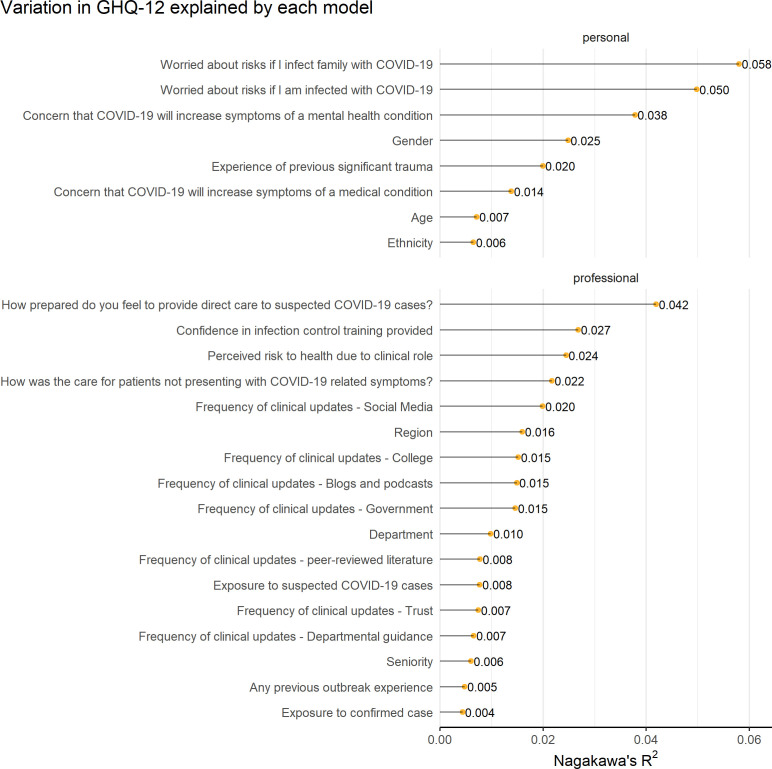
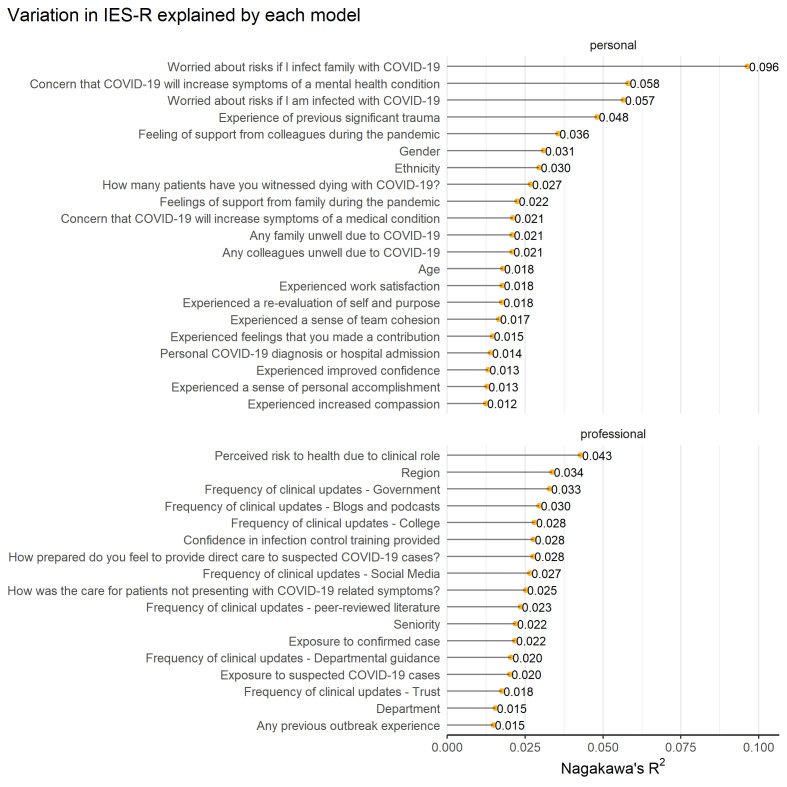
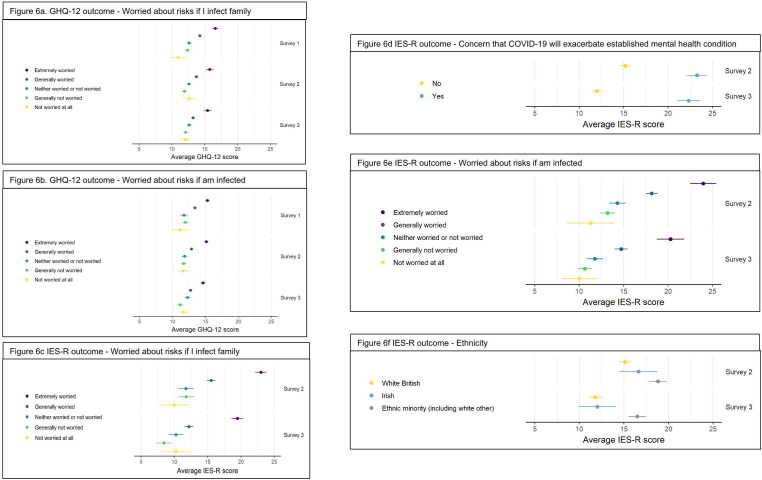
Risk factors for psychological distress (GHQ-12) and trauma (IES-R)
The overall strength of the relationship between participant factors and the two outcome measures, psychological distress and trauma, is summarised using Nagakawa’s marginal R2 (figures 4 and 5). The form of these univariable relationships is described graphically for the five variables with the highest R2 values in figure 6A. Graphs for the remaining variables are reported in https://github.com/wjchulme/TERN-CERA-study/tree/main/outputs.
Figure 4.
General Health Questionnaire-12 (GHQ-12) variance explained model.
Figure 5.
Impact of Events Scale-Revised (IES-R) variance explained model.
Figure 6.
(A)–(F) General Health Questionnaire-12 (GHQ-12) and Impact of Events Scale-Revised (IES-R) modelled outcomes.
Personal and professional variables predicting distress (GHQ-12)
Worry of infecting family members due to clinical work (R2=0.06) and worry of personal infection (R2=0.05) were the two variables most strongly associated with distress. Figure 6A, B report the mean GHQ-12-score for the levels within this variable. Those that were ‘extremely worried’ about infecting family had a mean GHQ-12-modelled score of 15.3 (95% CI 15.0 to 15.6), 15.1 (95% CI 14.8 to 15.5) and 14.6 (95% CI 14.3 to 15.0) during the acceleration, peak and deceleration, respectively, compared with mean scores of 13.7, 13.2 and 12.9, respectively for all participants. For those who were ‘extremely worried’ about personal infection, the mean GHQ-12 modelled score was 16.6 (95% CI 16.1 to 17.1) during the acceleration period, compared with 10.9 (95% CI 9.7 to 12.1) for those who were ‘not worried at all’ about being infected. For the mean GHQ-12 modelled score for each of the other variables, see the online link for the figures and values (https://github.com/wjchulme/TERN-CERA-study/tree/main/outputs).
Personal and professional variables predicting trauma (IES-R)
For trauma, worry of infection of family members due to clinical role had the highest R2 value (R2=0.10). Mean IES-R modelled score for those who were ‘extremely worried’ about infecting family was 23.0 (95% CI 22.2 to 23.8) during the peak compared with 10.0 (95% CI 7.8 to 12.2) for those who were ‘not worried at all’ during the peak (figure 6C). This is significantly higher than the reported mean IES-R overall of 16.3.
Concern that COVID-19 would exacerbate symptoms of an established mental health condition (R2=0.06) had the second highest R2 value. Peak IES-R mean modelled scores were 23.3 (95% CI 22.1 to 24.4) in those who agreed with this statement compared with 15.2 (95% CI 14.7 to 15.7) in those who disagreed. Deceleration mean IES-R modelled scores remained high for those who agreed, 22.3 (95% CI 21.1 to 23.6) (figure 6D).
Worry relating to personal infection due to clinical role (R2=0.06) was again strongly associated with trauma. Figure 6E displays the mean IES-R modelled scores and demonstrates the peak (24.0 (95% CI 22.5 to 25.4)) and deceleration (20.3 (95% CI 18.7 to 21.8)) outcomes in participants who were ‘extremely worried’ compared with those who were ‘not worried at all’ during the peak 11.3 (95% CI 8.6 to 14.0) and deceleration 10.0 (95% CI 8.0 to 12.0).
While ethnicity was not strongly associated with distress, it was a stronger predictor of trauma (R2=0.03). Mean modelled trauma scores for ‘ethnic minority’ participants at peak was 18.8 (95% CI 17.8 to 19.8), compared with ‘white British’ participants of 15.1 (95% CI 14.5 to 15.8) (Figure 6F). For the mean IES-R modelled scores for each of the other variables, see online link for the figures and values (https://github.com/wjchulme/TERN-CERA-study/tree/main/outputs).
Incidence of self-reported COVID-19 infection and isolation
By the deceleration phase of the pandemic, 6.9% (n=212) of respondents had received a positive diagnosis of COVID-19 and 0.4% (n=12) had been admitted to hospital. A positive diagnosis did not have a significant effect in prediction of trauma (R2=0.014).
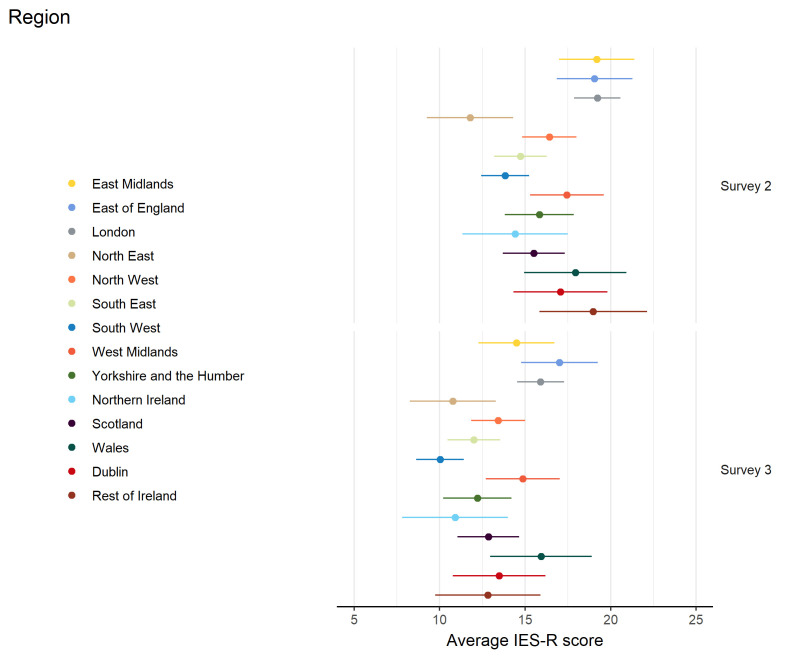
Regional and national variation of psychological distress and trauma
The region in which participants worked was more valuable for predicting trauma (R2=0.034), than for distress (R2=0.016). The mean modelled score of the different regions within the UK and Ireland on IES-R is demonstrated in figure 7.
Figure 7.
Impact of Events Scale-Revised (IES-R) outcome-region.
Drop-out by GHQ-12 and IES-R
Response rate for the peak and deceleration surveys was 71.6% and 56.6%, respectively. There was no significant difference in either the GHQ-12 or IES-R scores between those who dropped out and those who remained in the study (see online supplemental file 1).
Discussion
In this prospective longitudinal survey of 3079 frontline doctors, the prevalence of psychological distress reached 44.7% during the acceleration phase, and reached 23.7% for trauma during the peak phase—these figures were substantially higher than for the general population.41 For psychological distress, rates declined through peak and deceleration phases of the first wave to a level comparable to prepandemic levels.42 Prevalence of ‘probable PTSD’ was 12.6% at peak and 10.1% at deceleration, demonstrating a degree of natural recovery.43 44 However, just less than a quarter experienced subthreshold post-trauma symptoms 30 days following the pandemic peak.
Personal factors were the most powerful predictors of both psychological distress and trauma. The most significant predictors relate to familial safety, personal safety and established mental health conditions. These findings support aggregated data in recent reviews and meta-analyses on the key predictors of psychological distress in disaster or infectious outbreak settings.1 7 21–23 However, it cannot be ignored that the psychological harm associated with both familial and personal safety may potentially be explained by the perceived (and reported) inadequate provision of PPE to frontline workers.45 46 This is an area where improvements must be made in order to mitigate against future physical and psychological harms that novel pathogens present.
While most findings are consistent with existing research, our study also identifies ethnicity as a novel, key predictor of trauma.47–49 This is unsurprising given higher rates of reported mortality in ethnic minority groups with this particular pandemic.50 However, the nature and direction of relationship between these risk factors and poorer outcomes is undoubtedly complex. Ongoing work continues to seek further understanding in this area.51
Rates of trauma were high across all three specialty groups. One in four doctors met the clinical threshold, with the highest rates seen in EM and ICM. This is likely explained by their clinical roles during the pandemic, in which they were exposed to a higher volume of COVID-19-positive patients compared with anaesthetic colleagues. However, it is important to note that the rate of trauma seen in anaesthetics was also of concern. At the deceleration phase, EM doctors had higher rates of ‘probable PTSD’ (IES-R >33), whereas ICM doctors had a higher prevalence of trauma (IES-R >24). This may reflect the later peak in intensive care units when compared with EM52 or the potential impact of downstream mortality. Further work should explore long-term outcomes in all cohorts.
It is evident from our longitudinal data that vulnerability to poorer psychological outcomes may be predicted by certain characteristics and therefore potentially mitigated through targeted intervention. Studies examining psychiatric outcomes in SARS reflect that psychological distress is likely to persist. Identification of those likely to experience adversity, and interventions to mitigate these, must begin now.8 10 53 54 Without appropriate support and intervention doctors are likely to experience long-term effects on mental health, resulting in increased sickness rates, absenteeism, impaired performance at work and the development of physical health problems.8 10 12 55 56 Therefore, the early identification of ongoing psychological distress will be pivotal in influencing the long-term mental health of frontline workers. Based on research from COVID-19 and other pandemics, we can be certain that rates and severity of distress will rise following this second wave of the pandemic. We now know that doctors are working on the frontline while carrying the heavy burden of fear of infecting themselves, or critically, family members, while some continue to battle high levels of psychological distress. This distress was evident in the lead up to the first peak, but sustained well beyond this time point. Doctors are continuing to work in very highly pressured, high-risk environments with a significant proportion doing so despite clinical levels of distress. Policymakers and professional bodies should urgently seek to develop an overarching ‘best practice’ pathway to support all healthcare staff in these environments.
While various interventions are recommended specifically for frontline workers there is common agreement in the necessity for basic psychosocial interventions (ie, sleep hygiene, exercise, health behaviour) to facilitate return to equilibrium,57–60 yet these measures are not always sufficient to ameliorate persistent distress. It is crucial that an overarching ‘best practice’ pathway and package of care is implemented to help support staff now and for the future. This must be evidence-based, multilevel, starting with the ‘individual’ level and moving though to ‘organisational’ level intervention, including (a) mobilisation of formal peer and organisational support structures, (b) mechanisms for recognising and monitoring distress and (c) offer clear referral pathways to evidence-based interventions. Access to appropriate psychological support is imperative; cognitive behavioural therapy is recommended by the National Institute for health and Care Excellence to ameliorate anxiety, depression and PTSD61 62; however further work is needed to ensure these interventions this are suitably tailored to the practicalities of shift work and the unique experiences faced by frontline clinicians. With this, there is a responsibility to ensure equality in the provision of care and pathways to access, for this is likely to be necessary for many.
Strengths and weaknesses
This is a large-scale longitudinal study examining prevalence of psychological distress in doctors in the UK and Ireland, offering a robust and reliable measure of the impact of COVID-19 on the mental health of frontline doctors, and allows comparison with other pandemic mental health trajectories. Due to the three-phase prospective design and extent of data collected, findings from this study can be reliably used to inform the development of preparations and interventions to mitigate the impact of COVID-19 and future infectious disease outbreaks on mental health in frontline doctors.
However, there are limitations that may influence our findings. The reported rates of distress and trauma do not take account of any pre-existing psychiatric morbidity or historical factors that may predispose doctors to developing mental health difficulties in these circumstances.63–66 Data were gathered with regard to historical trauma, one of the most significant predictors of mental health difficulties long-term. Furthermore, while the sample size is large, any self-reporting measure is open to selection bias. This may have resulted in a biased sample with particularly high or low levels of distress and trauma. However, in the follow-up surveys (peak and deceleration) there was no difference in acceleration distress or trauma scores between those who dropped out and those who continued; yet we are unable to comment on those who declined to participate. While the two primary outcome measures, GHQ-12 and IES-R, have good psychometric properties, there is a concern that survey data may overstate the prevalence of cases when compared with formal diagnostic interviews such as the Structured Clinical Interview for DSM-IV Axis I Disorders; this is difficult to implement in such large samples, thus we cautiously avoid inference of definite diagnosis.
While the protocol was closely adhered to, variation in regional peaks may have influenced accurate capturing of psychological distress and trauma rates. It is noted that while the acceleration phase is study ‘baseline’, as the pandemic was present and proliferating in the UK at the acceleration phase, it more accurately represents the initial stress associated with a rapidly spreading highly infectious virus of unknown pathogenic origins and no effective treatment; a reasonable response to the context. Future research should continue to follow frontline doctors through the pandemic and beyond, to assess whether the mental health trajectories are similar to other infectious disease pandemics.
Conclusion
Our findings reflect a pattern of elevated distress during the acceleration and peak phase of the current pandemic, some degree of natural recovery and a significant minority continuing to experience residual ongoing distress. It is essential that policymakers and professional bodies seek to prevent future adverse effects through provision of vital equipment to mitigate both physical and psychological harm and the development of clear pathways to effective psychological care. Moving forward, it is essential the COVID-19 pandemic serves as a foundation for significant development and growth in all of these areas and that there is ongoing assessment of the psychological health of healthcare workers both during the pandemic and beyond.
Supplementary Material
Acknowledgments
The authors would like to acknowledge Mai Baquedano, at the University of Bristol, for her support with REDCap, GL Assessments for providing the licence for the GHQ-12 free of charge and Simon O'Hare, Data and Insight Manager, General Medical Council.
Footnotes
Twitter: @hirstposition, @mdlyttle, @katie_samuel_, @PEMDublin, @eddcarlton
Collaborators: TERN: L Kane; L Mackenzie; S Sharma Hajela; J Phizacklea; K Malik; N Mathai; A Sattout; S Messahel; E Fadden; R McQuillan; B O'Hare; P Turton; S Lewis; D Bewick; R Taylor; I Hancock; D Manthalapo; Ramesh Babu; S Hartshorn; M Williams; A Charlton; L Somerset; C Munday; A Turner; R Sainsbury; E Williams; S Patil; R Stewart; M Winstanley; N Tambe; C Magee; D Raffo; D Mawhinney; B Taylor; T Hussan; G Pells; F Barham; F Wood; C Szekeres; R Greenhalgh; S Marimuthu; R Macfarlane; M Alex; B Shrestha; L Stanley; J Gumley; K Thomas; M Anderson; C Weegenaar; J Lockwood; T Mohamed; S Ramraj; M Mackenzie; A Robertson; W Niven; M Patel; S Subramaniam; C Holmes; S Bongale; U Bait; S Nagendran; S Rao; F Mendes; P Singh; S Subramaniam; T Baron; C Ponmani; M Depante; R Sneep; A Brookes; S Williams; A Rainey; J Brown; N Marriage; S Manou; S Hart; M Elsheikh; L Cocker; MH Elwan; K L Vincent; C Nunn; N Sarja; M Viegas; E Wooffinden; C Reynard; N Cherian; A Da-Costa; S Duckitt; J Bailey; L How; T Hine; F Ihsan; H Abdullah; K Bader; S Pradhan; M Manoharan; C Battle; L Kehler; R Muswell; M Bonsano; J Evans; E Christmas; K Knight; L O'Rourke; K Adeboye; K Iftikhar; R Evans; R Darke; R Freeman; E Grocholski; K Kaur; H Cooper; M Mohammad; L Harwood; K Lines; C Thomas; D Ranasinghe; S Hall; J Wright; S Hall; N Ali; J Hunt; H Ahmad; C Ward; M Khan; K Holzman; J Ritchie; A Hormis; R Hannah; A Corfield; J Maney; D Metcalfe; S Timmis; C Williams; R Newport; D Bawden; A Tabner; H Malik; C Roe; D McConnell; F Taylor; R Ellis; S Morgan; L Barnicott; S Foster; J Browning; L McCrae; E Godden; A Saunders; A Lawrence-Ball; R House; J Muller; I Skene; M Lim; H Millar; A Rai; K Challen; S Currie; M Elkanzi; T Perry; W Kan; L Brown; M Cheema; A Clarey; A Gulati; K Webster; A Howson; R Doonan; C Magee; A Trimble; C O’Connell; R Wright; E Colley; C Rimmer; S Pintus; H Jarman; V Worsnop; S Collins; M Colmar; N Masood; R McLatchie; A Peasley; S Rahman; N Mullen; L Armstrong; A Hay; R Mills; J Lowe; H Raybould; A Ali; P Cuthbert; S Taylor; V Talwar; Z Al-Janabi; C Leech; J Turner; L McKechnie; B Mallon; J McLaren; Y Moulds; L Dunlop; FM Burton; S Keers; L Robertson; D Craver; N Moultrie; O Williams; S Purvis; M Clark; C Davies; S Foreman; C Ngua; D George; J Morgan; D George; N Hoskins; J Fryer; R Wright; L Frost; P Ellis; A Mackay; K Gray; M Jacobs; I Musliam; Veettil Asif; P Amiri; S Shrivastava; F Raza; S Wilson; M Riyat; H Knott; M Ramazany; S Langston; N Abela; L Robinson; D Maasdorp; H Murphy; H Edmundson; R Das; C Orjioke; D Worley; W Collier; J Everson; N Maleki; A Stafford; S Gokani; M Charalambos; A Olajide; C Bi; J Ng; S Naeem; J Anandarajah; A Hill; C Boulind-TERNR O'Sullivan; S Gilmartin; S Uí Bhroin; P Fitzpatrick; A Patton; M JeePoh Hock; S Graham; S Kukaswadia; C Prendergast; A Ahmed; C Dalla Vecchia; J Lynch; M Grummell; I Grossi; B MacManus; RAFT/TRIC/SATURNA- K Samuel; A Boyle; A Waite; B Johnson; J Vinagre.
Contributors: The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. TR conceived the idea for the study. TR, EC, JD, ML and BG were responsible for the initial study design, which was refined with the help of KS, CR, RH, MB, DH and WH. Expert advice on psychological assessment scores was provided by JD. WH provided the statistical plan. TR and DH lead the dissemination of the study in UK Adult Emergency Departments (ED), ML lead the dissemination of the study in UK and Ireland Paediatric EDs, KS lead the dissemination of the study in UK Anaesthetic and ICU Departments, MB lead the dissemination of the study in Ireland EDs, along with JC, JF and EU. JV lead the dissemination in Ireland ICUs and Anaesthetic Departments. TR coordinated study set-up, finalisation of the study surveys and finalisation of study protocols. All authors contributed to the final study design and protocol development, critically revised successive drafts of the manuscript and approved the final version. The study management group is responsible for the conduct of the study.
Funding: The Chief Investigator is directly funded as a research fellow by the Royal College of Emergency Medicine. The GHQ-12 is being used under licence from GL assessments; the fee for use of this instrument within all three surveys has been waived. EC is a National Institute for Health Research Advanced Fellow. The study has direct funding from RCEM. Grant code: G/2020/1.
Disclaimer: The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, the Department of Health or the Royal Colleges involved in survey distribution.
Competing interests: Many of the authors have been working as frontline clinicians during the COVID-19 pandemic. They have no competing interests to declare.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Contributor Information
on behalf of TheTrainee Emergency Research Network (TERN):
L Kane, L Mackenzie, S Sharma Hajela, J Phizacklea, K Malik, N Mathai, A Sattout, S Messahel, E Fadden, R McQuillan, B O'Hare, P Turton, S Lewis, D Bewick, R Taylor, I Hancock, L Kane, L Mackenzie, S Sharma Hajela, J Phizacklea, K Malik, N Mathai, A Sattout, S Messahel, E Fadden, R McQuillan, B O'Hare, P Turton, S Lewis, D Bewick, R Taylor, I Hancock, L Kane, L Mackenzie, S Sharma Hajela, J Phizacklea, K Malik, N Mathai, A Sattout, S Messahel, E Fadden, R McQuillan, B O'Hare, P Turton, S Lewis, D Bewick, R Taylor, I Hancock, L Kane, L Mackenzie, S Sharma Hajela, J Phizacklea, K Malik, N Mathai, A Sattout, S Messahel, E Fadden, R McQuillan, B O'Hare, P Turton, S Lewis, D Bewick, R Taylor, I Hancock, D Manthalapo, Ramesh Babu, S Hartshorn, M Williams, A Charlton, L Somerset, C Munday, A Turner, R Sainsbury, E Williams, S Patil, R Stewart, M Winstanley, N Tambe, C Magee, D Raffo, D Mawhinney, B Taylor, T Hussan, G Pells, F Barham, F Wood, C Szekeres, R Greenhalgh, S Marimuthu, R Macfarlane, M Alex, B Shrestha, L Stanley, J Gumley, K Thomas, M Anderson, C Weegenaar, J Lockwood, T Mohamed, S Ramraj, M Mackenzie, A Robertson, W Niven, M Patel, S Subramaniam, C Holmes, S Bongale, U Bait, S Nagendran, S Rao, F Mendes, P Singh, S Subramaniam, T Baron, C Ponmani, M Depante, R Sneep, A Brookes, S Williams, A Rainey, J Brown, N Marriage, S Manou, S Hart, M Elsheikh, L Cocker, MH Elwan, K L Vincent, C Nunn, N Sarja, M Viegas, E Wooffinden, C Reynard, N Cherian, A Da-Costa, S Duckitt, J Bailey, L How, T Hine, F Ihsan, H Abdullah, K Bader, S Pradhan, M Manoharan, C Battle, L Kehler, R Muswell, M Bonsano, J Evans, E Christmas, K Knight, L O'Rourke, K Adeboye, K Iftikhar, R Evans, R Darke, R Freeman, E Grocholski, K Kaur, H Cooper, M Mohammad, L Harwood, K Lines, C Thomas, D Ranasinghe, S Hall, J Wright, S Hall, N Ali, J Hunt, H Ahmad, C Ward, M Khan, K Holzman, J Ritchie, A Hormis, R Hannah, A Corfield, J Maney, D Metcalfe, S Timmis, C Williams, R Newport, D Bawden, A Tabner, H Malik, C Roe, D McConnell, F Taylor, R Ellis, S Morgan, L Barnicott, S Foster, J Browning, L McCrae, E Godden, A Saunders, A Lawrence-Ball, R House, J Muller, I Skene, M Lim, H Millar, A Rai, K Challen, S Currie, M Elkanzi, T Perry, W Kan, L Brown, M Cheema, A Clarey, A Gulati, K Webster, A Howson, R Doonan, C Magee, A Trimble, C O’Connell, R Wright, E Colley, C Rimmer, S Pintus, H Jarman, V Worsnop, S Collins, M Colmar, N Masood, R McLatchie, A Peasley, S Rahman, N Mullen, L Armstrong, A Hay, R Mills, J Lowe, H Raybould, A Ali, P Cuthbert, S Taylor, V Talwar, Z Al-Janabi, C Leech, J Turner, L McKechnie, B Mallon, J McLaren, Y Moulds, L Dunlop, FM Burton, S Keers, L Robertson, D Craver, N Moultrie, O Williams, S Purvis, M Clark, C Davies, S Foreman, C Ngua, D George, J Morgan, D George, N Hoskins, J Fryer, R Wright, L Frost, P Ellis, A Mackay, K Gray, M Jacobs, L Kane, L Mackenzie, S Sharma Hajela, J Phizacklea, K Malik, N Mathai, A Sattout, S Messahel, E Fadden, R McQuillan, B O'Hare, P Turton, S Lewis, D Bewick, R Taylor, I Hancock, D Manthalapo, Ramesh Babu, S Hartshorn, M Williams, A Charlton, L Somerset, C Munday, A Turner, R Sainsbury, E Williams, S Patil, R Stewart, M Winstanley, N Tambe, C Magee, D Raffo, D Mawhinney, B Taylor, T Hussan, G Pells, F Barham, F Wood, C Szekeres, R Greenhalgh, S Marimuthu, R Macfarlane, M Alex, B Shrestha, L Stanley, J Gumley, K Thomas, M Anderson, C Weegenaar, J Lockwood, T Mohamed, S Ramraj, M Mackenzie, A Robertson, W Niven, M Patel, S Subramaniam, C Holmes, S Bongale, U Bait, S Nagendran, S Rao, F Mendes, P Singh, S Subramaniam, T Baron, C Ponmani, M Depante, R Sneep, A Brookes, S Williams, A Rainey, J Brown, N Marriage, S Manou, S Hart, M Elsheikh, L Cocker, MH Elwan, K L Vincent, C Nunn, N Sarja, M Viegas, E Wooffinden, C Reynard, N Cherian, A Da-Costa, S Duckitt, J Bailey, L How, T Hine, F Ihsan, H Abdullah, K Bader, S Pradhan, M Manoharan, C Battle, L Kehler, R Muswell, M Bonsano, J Evans, E Christmas, K Knight, L O'Rourke, K Adeboye, K Iftikhar, R Evans, R Darke, R Freeman, E Grocholski, K Kaur, H Cooper, M Mohammad, L Harwood, K Lines, C Thomas, D Ranasinghe, S Hall, J Wright, S Hall, N Ali, J Hunt, H Ahmad, C Ward, M Khan, K Holzman, J Ritchie, A Hormis, R Hannah, A Corfield, J Maney, D Metcalfe, S Timmis, C Williams, R Newport, D Bawden, A Tabner, H Malik, C Roe, D McConnell, F Taylor, R Ellis, S Morgan, L Barnicott, S Foster, J Browning, L McCrae, E Godden, A Saunders, A Lawrence-Ball, R House, J Muller, I Skene, M Lim, H Millar, A Rai, K Challen, S Currie, M Elkanzi, T Perry, W Kan, L Brown, M Cheema, A Clarey, A Gulati, K Webster, A Howson, R Doonan, C Magee, A Trimble, C O’Connell, R Wright, E Colley, C Rimmer, S Pintus, H Jarman, V Worsnop, S Collins, M Colmar, N Masood, R McLatchie, A Peasley, S Rahman, N Mullen, L Armstrong, A Hay, R Mills, J Lowe, H Raybould, A Ali, P Cuthbert, S Taylor, V Talwar, Z Al-Janabi, C Leech, J Turner, L McKechnie, B Mallon, J McLaren, Y Moulds, L Dunlop, FM Burton, S Keers, L Robertson, D Craver, N Moultrie, O Williams, S Purvis, M Clark, C Davies, S Foreman, C Ngua, D George, J Morgan, D George, N Hoskins, J Fryer, R Wright, L Frost, P Ellis, A Mackay, K Gray, M Jacobs, I Musliam, Veettil Asif, P Amiri, S Shrivastava, F Raza, S Wilson, M Riyat, H Knott, M Ramazany, S Langston, N Abela, L Robinson, D Maasdorp, H Murphy, H Edmundson, R Das, C Orjioke, D Worley, W Collier, J Everson, N Maleki, A Stafford, S Gokani, M Charalambos, A Olajide, C Bi, J Ng, S Naeem, J Anandarajah, A Hill, C Boulind, L Kane, L Mackenzie, S Sharma Hajela, J Phizacklea, K Malik, N Mathai, A Sattout, S Messahel, E Fadden, R McQuillan, B O'Hare, P Turton, S Lewis, D Bewick, R Taylor, I Hancock, D Manthalapo, Ramesh Babu, S Hartshorn, M Williams, A Charlton, L Somerset, C Munday, A Turner, R Sainsbury, E Williams, S Patil, R Stewart, M Winstanley, N Tambe, C Magee, D Raffo, D Mawhinney, B Taylor, T Hussan, G Pells, F Barham, F Wood, C Szekeres, R Greenhalgh, S Marimuthu, R Macfarlane, M Alex, B Shrestha, L Stanley, J Gumley, K Thomas, M Anderson, C Weegenaar, J Lockwood, T Mohamed, S Ramraj, M Mackenzie, A Robertson, W Niven, M Patel, S Subramaniam, C Holmes, S Bongale, U Bait, S Nagendran, S Rao, F Mendes, P Singh, S Subramaniam, T Baron, C Ponmani, M Depante, R Sneep, A Brookes, S Williams, A Rainey, J Brown, N Marriage, S Manou, S Hart, M Elsheikh, L Cocker, MH Elwan, K L Vincent, C Nunn, N Sarja, M Viegas, E Wooffinden, C Reynard, N Cherian, A Da-Costa, S Duckitt, J Bailey, L How, T Hine, F Ihsan, H Abdullah, K Bader, S Pradhan, M Manoharan, C Battle, L Kehler, R Muswell, M Bonsano, J Evans, E Christmas, K Knight, L O'Rourke, K Adeboye, K Iftikhar, R Evans, R Darke, R Freeman, E Grocholski, K Kaur, H Cooper, M Mohammad, L Harwood, K Lines, C Thomas, D Ranasinghe, S Hall, J Wright, S Hall, N Ali, J Hunt, H Ahmad, C Ward, M Khan, K Holzman, J Ritchie, A Hormis, R Hannah, A Corfield, J Maney, D Metcalfe, S Timmis, C Williams, R Newport, D Bawden, A Tabner, H Malik, C Roe, D McConnell, F Taylor, R Ellis, S Morgan, L Barnicott, S Foster, J Browning, L McCrae, E Godden, A Saunders, A Lawrence-Ball, R House, J Muller, I Skene, M Lim, H Millar, A Rai, K Challen, S Currie, M Elkanzi, T Perry, W Kan, L Brown, M Cheema, A Clarey, A Gulati, K Webster, A Howson, R Doonan, C Magee, A Trimble, C O’Connell, R Wright, E Colley, C Rimmer, S Pintus, H Jarman, V Worsnop, S Collins, M Colmar, N Masood, R McLatchie, A Peasley, S Rahman, N Mullen, L Armstrong, A Hay, R Mills, J Lowe, H Raybould, A Ali, P Cuthbert, S Taylor, V Talwar, Z Al-Janabi, C Leech, J Turner, L McKechnie, B Mallon, J McLaren, Y Moulds, L Dunlop, FM Burton, S Keers, L Robertson, D Craver, N Moultrie, O Williams, S Purvis, M Clark, C Davies, S Foreman, C Ngua, D George, J Morgan, D George, N Hoskins, J Fryer, R Wright, L Frost, P Ellis, A Mackay, K Gray, M Jacobs, I Musliam, Veettil Asif, P Amiri, S Shrivastava, F Raza, S Wilson, M Riyat, H Knott, M Ramazany, S Langston, N Abela, L Robinson, D Maasdorp, H Murphy, H Edmundson, R Das, C Orjioke, D Worley, W Collier, J Everson, N Maleki, A Stafford, S Gokani, M Charalambos, A Olajide, C Bi, J Ng, S Naeem, J Anandarajah, A Hill, and C Boulind
Collaborators: Ireland Trainee Emergency Research Network (I-TERN) Collaborators, R O'Sullivan, S Gilmartin, S Uí Bhroin, P Fitzpatrick, A Patton, M Jee Poh Hock, S Graham, S Kukaswadia, C Prendergast, A Ahmed, C Dalla Vecchia, J Lynch, M Grummell, I Grossi, B MacManus, R O'Sullivan, S Gilmartin, S Uí Bhroin, P Fitzpatrick, A Patton, M JeePoh Hock, S Graham, S Kukaswadia, C Prendergast, A Ahmed, C Dalla Vecchia, J Lynch, M Grummell, I Grossi, B MacManus, Research and Audit Federation of Trainees (RAFT), Trainee Research in Intensive Care (TRIC) and Specialist Anaesthesia Trainee led Audit and Research Network (SATURN) Collaborators, K Samuel, A Boyle, A Waite, B Johnson, and J Vinagre
Data availability statement
Deidentified participant data will be made available for 2 years post publication. Requests for access will require HRA and ethical approval and decisions regarding data sharing will be made after discussion with the study senior authors. Statistical code and study figures are available directly from: https://github.com/wjchulme/TERN-CERA-study/tree/main/outputs
Ethics statements
Patient consent for publication
Obtained.
Ethics approval
Ethical approval was obtained from the University of Bath (UK) and Children’s Health Ethics Committee (Ireland). Regulatory approval was obtained from the Health Regulation Authority (UK), Health and Care Research Wales.
References
- 1. Brooks SK, Dunn R, Sage CAM, et al. Risk and resilience factors affecting the psychological wellbeing of individuals deployed in humanitarian relief roles after a disaster. J Ment Health 2015;24:385-413. 10.3109/09638237.2015.1057334 [DOI] [PubMed] [Google Scholar]
- 2. Liu Q, Luo D, Haase JE, et al. The experiences of health-care providers during the COVID-19 crisis in China: a qualitative study. Lancet Glob Health 2020;8:e790–8. 10.1016/S2214-109X(20)30204-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. McCabe R, Schmit N, Christen P, et al. Adapting Hospital capacity to meet changing demands during the COVID-19 pandemic. BMC Med 2020;18:329. 10.1186/s12916-020-01781-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Phua J, Weng L, Ling L, et al. Intensive care management of coronavirus disease 2019 (COVID-19): challenges and recommendations. Lancet Respir Med 2020;8:506-517. 10.1016/S2213-2600(20)30161-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kursumovic E, Lennane S, Cook TM. Deaths in healthcare workers due to COVID-19: the need for robust data and analysis. Anaesthesia 2020;75:989–92. 10.1111/anae.15116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Maunder RG, Lancee WJ, Rourke S, et al. Factors associated with the psychological impact of severe acute respiratory syndrome on nurses and other Hospital workers in Toronto. Psychosom Med 2004;66:938-42. 10.1097/01.psy.0000145673.84698.18 [DOI] [PubMed] [Google Scholar]
- 7. Kisely S, Warren N, McMahon L, et al. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ 2020;369:m1642. 10.1136/bmj.m1642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Allan SM, Bealey R, Birch J, et al. The prevalence of common and stress-related mental health disorders in healthcare workers based in pandemic-affected hospitals: a rapid systematic review and meta-analysis. Eur J Psychotraumatol 2020;11:1810903. 10.1080/20008198.2020.1810903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Roberts T, Daniels J, Hulme W. Psychological distress during the acceleration phase of the COVID-19 pandemic: a survey of doctors practising in emergency medicine, anaesthesia and intensive care medicine in the UK and ireland. Emerg Med J 2021;0:1–10. 10.1136/emermed-2020-210438 [DOI] [PubMed] [Google Scholar]
- 10. Maunder RG, Lancee WJ, Balderson KE, et al. Long-Term psychological and occupational effects of providing Hospital healthcare during SARS outbreak. Emerg Infect Dis 2006;12:1924-32. 10.3201/eid1212.060584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fiksenbaum L, Marjanovic Z, Greenglass ER. Emotional exhaustion and state anger in nurses who worked during the SARS outbreak: the role of perceived threat and organizational support. Can J Community Ment Heal 2006. 10.7870/cjcmh-2006-0015 [DOI] [Google Scholar]
- 12. Arora M, Asha S, Chinnappa J, et al. Review article: burnout in emergency medicine physicians. Emerg Med Australas 2013;25:491–5. 10.1111/1742-6723.12135 [DOI] [PubMed] [Google Scholar]
- 13. Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open 2020;3:e203976. 10.1001/jamanetworkopen.2020.3976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Di Tella M, Romeo A, Benfante A, et al. Mental health of healthcare workers during the COVID-19 pandemic in Italy. J Eval Clin Pract 2020;26:1583–7. 10.1111/jep.13444 [DOI] [PubMed] [Google Scholar]
- 15. Pappa S, Ntella V, Giannakas T. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun 2020. 10.1016/j.bbi.2020.05.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Benfante A, Di Tella M, Romeo A, et al. Traumatic stress in healthcare workers during COVID-19 pandemic: a review of the immediate impact. Front Psychol 2020;11:569935. 10.3389/fpsyg.2020.569935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Clap for Carers: UK in “emotional” tribute to NHS and care workers - BBC News. Available: https://www.bbc.co.uk/news/uk-52058013 [Accessed 20 Nov 2020].
- 18. COVID-19: protecting health-care workers. Lancet 2020. 10.1016/S0140-6736(20)30644-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Coronavirus: Mental health of NHS staff at long-term risk - BBC News. Available: https://www.bbc.co.uk/news/health-52528619 [Accessed 20 Nov 2020].
- 20. Halpern J, Maunder RG, Schwartz B, et al. Identifying risk of emotional sequelae after critical incidents. Emerg Med J 2011;28:51-6. 10.1136/emj.2009.082982 [DOI] [PubMed] [Google Scholar]
- 21. Brooks SK, Dunn R, Amlôt R, et al. A systematic, thematic review of social and occupational factors associated with psychological outcomes in healthcare employees during an infectious disease outbreak. J Occup Environ Med 2018;60:248-257. 10.1097/JOM.0000000000001235 [DOI] [PubMed] [Google Scholar]
- 22. Lancee WJ, Maunder RG, Goldbloom DS, et al. Prevalence of psychiatric disorders among Toronto Hospital workers one to two years after the SARS outbreak. Psychiatr Serv 2008;59:91-5. 10.1176/ps.2008.59.1.91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ozer EJ, Best SR, Lipsey TL, et al. Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychol Bull 2003;129:52–73. 10.1037/0033-2909.129.1.52 [DOI] [PubMed] [Google Scholar]
- 24. Roberts T, Daniels J, Hulme W, et al. COVID-19 emergency response assessment study: a prospective longitudinal survey of frontline doctors in the UK and ireland: study protocol. BMJ Open 2020;10:e039851. 10.1136/bmjopen-2020-039851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Eysenbach G. Improving the quality of web surveys: the checklist for reporting results of Internet E-Surveys (cherries). J Med Internet Res 2004;6:e34. 10.2196/jmir.6.3.e34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Harris PA, Taylor R, Minor BL, et al. The REDCap Consortium: building an international community of software platform partners. J Biomed Inform 2019;95:103208. 10.1016/j.jbi.2019.103208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Holloway R, Rasmussen SA, Zaza S. Updated preparedness and response framework for influenza pandemics, 2014. Available: https://www.cdc.gov/mmwr/preview/mmwrhtml/rr6306a1.htm [Accessed 08 Apr 2020]. [PubMed]
- 29. Goldberg D. Williams P. A user’s guide to the General Health Questionnaire. London: GL Assessment, 1988. [Google Scholar]
- 30. Goldberg DP, Gater R, Sartorius N, et al. The validity of two versions of the GHQ in the who study of mental illness in general health care. Psychol Med 1997;27:191-7. 10.1017/s0033291796004242 [DOI] [PubMed] [Google Scholar]
- 31. Goldberg DP, Oldehinkel T, Ormel J. Why GHQ threshold varies from one place to another. Psychol Med 1998;28:915–21. 10.1017/S0033291798006874 [DOI] [PubMed] [Google Scholar]
- 32. Christianson S, Marren J. The Impact of Event Scale - Revised (IES-R). Medsurg Nurs 2012;21:321–2. [PubMed] [Google Scholar]
- 33. Asukai N, Kato H, Kawamura N, et al. Reliability and validity of the Japanese-language version of the impact of event scale-revised (IES-R-J): four studies of different traumatic events. J Nerv Ment Dis 2002;190:175-82. 10.1097/00005053-200203000-00006 [DOI] [PubMed] [Google Scholar]
- 34. Creamer M, Bell R, Failla S. Psychometric properties of the Impact of Event Scale - Revised. Behav Res Ther 2003;41:1489-96. 10.1016/j.brat.2003.07.010 [DOI] [PubMed] [Google Scholar]
- 35. Nakagawa S, Johnson PCD, Schielzeth H. The coefficient of determination R2 and intra-class correlation coefficient from generalized linear mixed-effects models revisited and expanded. J R Soc Interface 2017;14. 10.1098/rsif.2017.0213. [Epub ahead of print: 13 09 2017]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Wickham H, Averick M, Bryan J, et al. Welcome to the Tidyverse. J Open Source Softw 2019;4:1686. 10.21105/joss.01686 [DOI] [Google Scholar]
- 37. Bates D, Mächler M, Bolker B, et al. Fitting Linear Mixed-Effects Models Using lme4. J Stat Softw 2015;67. 10.18637/jss.v067.i01 [DOI] [Google Scholar]
- 38. Lüdecke D. ggeffects: Tidy data frames of marginal effects from regression models. J Open Source Softw 2018;3:772. 10.21105/joss.00772 [DOI] [Google Scholar]
- 39. Khunti K, Routen A, Pareek M, et al. The language of ethnicity. BMJ 2020;371:m4493. 10.1136/bmj.m4493 [DOI] [PubMed] [Google Scholar]
- 40. Bunglawala Z. Please, don’t call me BAME or BME! 2019. Available: https://civilservice.blog.gov.uk/2019/07/08/please-dont-call-me-bame-or-bme/ [Accessed 12 Oct 2020].
- 41. Rettie H, Daniels J. Coping and tolerance of uncertainty: predictors and mediators of mental health during the COVID-19 pandemic. Am Psychol 2021;76:427-437. 10.1037/amp0000710 [DOI] [PubMed] [Google Scholar]
- 42. Kinman G, Teoh K. What could make a difference to the mental health of UK doctors?A review of the research evidence, 2018. https://uobrep.openrepository.com/handle/10547/622963 [Google Scholar]
- 43. Morina N, Wicherts JM, Lobbrecht J, et al. Remission from post-traumatic stress disorder in adults: a systematic review and meta-analysis of long term outcome studies. Clin Psychol Rev 2014;34:249-55. 10.1016/j.cpr.2014.03.002 [DOI] [PubMed] [Google Scholar]
- 44. Kessler RC, Sonnega A, Bromet E, et al. Posttraumatic stress disorder in the National comorbidity survey. Arch Gen Psychiatry 1995;52:1048-60. 10.1001/archpsyc.1995.03950240066012 [DOI] [PubMed] [Google Scholar]
- 45. McKee M. England's PPE procurement failures must never happen again. BMJ 2020;370:m2858. 10.1136/bmj.m2858 [DOI] [PubMed] [Google Scholar]
- 46. Godlee F. Covid-19: weathering the storm. BMJ 2020;368:m1199. 10.1136/bmj.m1199 [DOI] [Google Scholar]
- 47. Chew NWS, Lee GKH, Tan BYQ, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun 2020;88:559–65. 10.1016/j.bbi.2020.04.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Berger W, Coutinho ESF, Figueira I, et al. Rescuers at risk: a systematic review and meta-regression analysis of the worldwide current prevalence and correlates of PTSD in rescue workers. Soc Psychiatry Psychiatr Epidemiol 2012;47:1001–11. 10.1007/s00127-011-0408-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Perrin MA, DiGrande L, Wheeler K, et al. Differences in PTSD prevalence and associated risk factors among world Trade center disaster rescue and recovery workers. Am J Psychiatry 2007;164:1385-94. 10.1176/appi.ajp.2007.06101645 [DOI] [PubMed] [Google Scholar]
- 50. Coronavirus. (COVID-19) related deaths by ethnic group, England and Wales - Office for National Statistics. Available: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/articles/coronavirusrelateddeathsbyethnicgroupenglandandwales/2march2020to10april2020 [Accessed 20 Nov 2020].
- 51. Iacobucci G. Covid-19: increased risk among ethnic minorities is largely due to poverty and social disparities, review finds. BMJ 2020;371:m4099. 10.1136/bmj.m4099 [DOI] [PubMed] [Google Scholar]
- 52. Doidge JC, Mouncey PR, Thomas K. Trends in intensive care for patients with COVID-19 in England, Wales and Northern Ireland. 11, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Mak IWC, Chu CM, Pan PC, et al. Long-Term psychiatric morbidities among SARS survivors. Gen Hosp Psychiatry 2009;31:318-26. 10.1016/j.genhosppsych.2009.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Lee AM, Wong JGWS, McAlonan GM, et al. Stress and psychological distress among SARS survivors 1 year after the outbreak. Can J Psychiatry 2007;52:233-40. 10.1177/070674370705200405 [DOI] [PubMed] [Google Scholar]
- 55. McAlonan GM, Lee AM, Cheung V, et al. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Can J Psychiatry 2007;52:241-7. 10.1177/070674370705200406 [DOI] [PubMed] [Google Scholar]
- 56. Stuijfzand S, Deforges C, Sandoz V, et al. Psychological impact of an epidemic/pandemic on the mental health of healthcare professionals: a rapid review. BMC Public Health 2020;20:1230. 10.1186/s12889-020-09322-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Greenberg N, Docherty M, Gnanapragasam S, et al. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ 2020;368:m1211. 10.1136/bmj.m1211 [DOI] [PubMed] [Google Scholar]
- 58. Que J, Shi L, Deng J, et al. Psychological impact of the COVID-19 pandemic on healthcare workers: a cross-sectional study in China. Gen Psychiatr 2020;33:e100259. 10.1136/gpsych-2020-100259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Maben J, Bridges J. Covid-19: supporting nurses' psychological and mental health. J Clin Nurs 2020;29:2742–50. 10.1111/jocn.15307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Heath C, Sommerfield A, von Ungern‐Sternberg BS. Resilience strategies to manage psychological distress among healthcare workers during the COVID‐19 pandemic: a narrative review. Anaesthesia 2020;75:1364–71. 10.1111/anae.15180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Post-Traumatic stress disorder NICE guideline, 2018. Available: www.nice.org.uk/guidance/ng116 [Accessed 23 Nov 2020].
- 62. Kendrick T, Pilling S. Common mental health disorders--identification and pathways to care: NICE clinical guideline. Br J Gen Pract 2012;62:47–9. 10.3399/bjgp12X616481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Cottey L, Roberts T, Graham B, et al. Need for recovery amongst emergency physicians in the UK and ireland: a cross-sectional survey. BMJ Open 2020;10:e041485. 10.1136/bmjopen-2020-041485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Graham B, Cottey L, Smith JE, et al. Measuring 'Need for Recovery' as an indicator of staff well-being in the emergency department: a survey study. Emerg Med J 2020;37:555-561. 10.1136/emermed-2019-208797 [DOI] [PubMed] [Google Scholar]
- 65. Basu S, Qayyum H, Mason S. Occupational stress in the ED: a systematic literature review. Emerg Med J 2017;34:441–7. 10.1136/emermed-2016-205827 [DOI] [PubMed] [Google Scholar]
- 66. Schneider A, Weigl M. Associations between psychosocial work factors and provider mental well-being in emergency departments: a systematic review. PLoS One 2018;13:e0197375. 10.1371/journal.pone.0197375 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-049680supp001.pdf (683.2KB, pdf)
Data Availability Statement
Deidentified participant data will be made available for 2 years post publication. Requests for access will require HRA and ethical approval and decisions regarding data sharing will be made after discussion with the study senior authors. Statistical code and study figures are available directly from: https://github.com/wjchulme/TERN-CERA-study/tree/main/outputs