Abstract
Introduction
Students desire instruction in skill development to address both their own implicit biases and bias perceived in the learning environment. Curricula to date achieve strategy identification through reflection and discussion but do not provide opportunity for personally relevant skill development and practice in implicit bias recognition and management. To address this gap, we developed and evaluated a skills-based elective in implicit bias recognition and management focused on learners' own interpersonal interactions, including patient encounters, and perceived bias in the learning environment.
Method
Fifteen first-year medical students completed the nine-session elective over three annual offerings. Each session lasted 1.5 hours. Curriculum development was informed by published frameworks and transformative learning theory. Direct observation of student performances in role-plays and other active learning exercises constituted the formative assessment. Program evaluation focused on the impact of instruction through pre- and posttests, along with analysis of notes taken by the investigative team, including notes on formative assessments.
Results
Students engaged with all aspects of instruction, including role-plays. Pretest/posttest results demonstrated increased self-reported knowledge and comfort in addressing perceived bias. Formative assessment demonstrated students' skill development in safely and respectfully addressing perceived bias in the learning environment without endangering their relationships with supervisors.
Discussion
Skills developed—addressing bias in interpersonal encounters and perceived bias in clinical and teaching encounters—are relevant to learners throughout their careers. This course is relevant to medical students and trainees at various experience levels and could serve as a template for novel, skills-based curricula across health professions.
Keywords: Self-Assessment, Implicit Bias, Unconscious Bias, Health Disparities, Hidden Curriculum, Learning Environment, Anti-racism
Educational Objectives
By the end of this course, learners will be able to:
-
1.
Identify when implicit bias may be influencing their own communication with a patient or peer.
-
2.
Advocate on behalf of patients when perceiving bias in a witnessed encounter.
-
3.
Address biased comments made within the learning environment.
Introduction
Evidence demonstrates an association between racial implicit bias and disparate outcomes regarding provider communication with patients of different races; these disparate communication behaviors are perceived by patients as well.1,2 Moreover, learners report perceiving bias both in patient encounters during their clinical training and in teaching encounters throughout their education.3–5 Implicit bias is therefore present in the learning environment. Students clamor for skill development to address bias within their own encounters with patients, as well as to advocate for patients, themselves, and others in the learning environment.3,4 Unfortunately, in the current state of implicit bias instruction, learners are too often left with increased awareness of implicit bias in themselves and in clinical encounters, without actual skill development to mitigate the influence of implicit bias in their clinical and nonclinical interpersonal encounters or the learning environment.6–9 Awareness of bias without skills to address it may lead to discomfort for learners,4 as well as avoidant behaviors to minimize the chances of acting in a biased fashion.10 Instruction in implicit bias recognition and management (IBRM) is a skills-based approach with two central components. IBRM instruction first facilitates students recognizing when implicit bias may be influencing an encounter and then empowers them with skills to mitigate the negative influence of implicit bias on their own encounters and to address perceived bias in witnessed encounters.11,12 It additionally alleviates the unintended consequences of increased awareness as a sole strategy.10,13
We recently published a blueprint of our skills-based elective for preclinical students in IBRM and its comprehensive qualitative program evaluation.14 Here, we provide all course materials and accompanying facilitator guides to enable the delivery of our curriculum at other institutions. We have built on previous curricula that achieved reflection and strategy identification,6–9 lessons learned from our own delivery of implicit bias instruction,7,15 and existing frameworks and learning theories related to implicit bias.11,12,16–18 Our work adds to the existing publications in MedEdPORTAL on addressing implicit bias by providing opportunities for skill development and practice. Sandoval and colleagues incorporated skill development.5 Our curriculum advances their work by having learners perform the unscripted role within the role-play as themselves (instead of as a hypothetical learner) in order to develop and practice personally relevant skills to address bias in themselves and in the learning environment. By providing opportunities for personally relevant skill development and practice, we expand upon other MedEdPORTAL publications focused on addressing implicit bias in the learning environment but culminating in strategy identification, rather than actual skill development.8,9,19
Several sources informed the development of this curriculum. We conducted a comprehensive needs assessment of patient,20 student,4 and faculty21 perspectives on implicit bias, including challenges and opportunities to restore the encounter and participate in and facilitate instruction on implicit bias, respectively. Our approach to teaching students to manage real or perceived bias in their own encounters with patients was informed by the results of our patient focus group study.20 Specifically, we included instruction based on the following conclusions of that work:
1) Instruction focusing on the influence of the patient's lived experience will enhance students' ability to partner with their patients to acknowledge perceived bias; and 2) Skill development in recognizing both perceived and real implicit bias in an encounter will enable students to mitigate its effect on the clinical encounter leading to continued patient engagement in the present and future medical encounters.20
In response to our student focus group study, facilitators explicitly role-modeled their own experiences with IBRM, both successes and failures in addressing it in a timely manner, in order to decrease potential shame for students.4 Several other features included ground rules and small-group continuity, among other features found to enhance student engagement in instruction in IBRM.4 Role-plays and other active learning exercises were developed in response to students' concerns about being aware of bias but lacking the skills to address it in themselves or in witnessed encounters.3,4 Finally, the facilitator guides were replete with suggested scripts/talking points and various other facilitator tips in anticipation of the challenges and opportunities facilitators might face. These aspects of the facilitator guides were informed by our in-depth faculty interview study.21
We crafted the sessions to guide the students through the stages identified by Teal and colleagues from complete denial of implicit bias through acceptance of it in themselves and its influence on their interpersonal encounters to adaptation of behaviors through skill development and practice.16 Although we began our curriculum before the framework by Sukhera and Watling was published,17 we were pleased to see that our curriculum aligned with many of their suggestions: We followed a longitudinal, developmentally appropriate approach to instruction, assessment, and program evaluation. Transformative learning theory guided our design of the individual sessions and informed the overall sequence of sessions.11,18 Briefly, transformative learning theory has four main components: an experience, critical reflection, guided discourse, and action (skill development).18 All four components are achieved by the end of the curriculum. Our target audience was first-year medical students, who had 8 prior months of experience with lectures, small-group sessions, shadowing physicians, and learning to interview patients in clinical settings.
Methods
We developed this course in a collaborative manner among the members of the research team and revised it in an iterative fashion in response to ongoing learner feedback.14 We routinely adapted the findings of our patient focus group study for IBRM in nonclinical encounters, given our learners' early stage of training.20 Significant amounts of time were spent normalizing the concept of implicit bias and creating a safe learning environment.4,17 We additionally approached instruction as a professionalism issue relevant to all physicians and maintained a learning orientation to foster a growth mindset as our students progressed through the curriculum.22 We delivered the elective in the spring of the academic year, giving students time to experience the learning environment. No prerequisite knowledge or experience related to IBRM was required. Learners benefited most from this instruction if they had some experience interviewing patients and observing clinical encounters. The faculty facilitator (Cristina M. Gonzalez) conducted research on IBRM, and student facilitators (Sydney A. Walker, Natalia Rodriguez, and Yuliana S. Noah) were members of her research team in 2017, 2018, and 2019, respectively. The guides were written to ensure facilitators needed no prerequisite knowledge regarding IBRM.
We developed a nine-session elective for first-year medical students, delivered in the spring of 2017–2019. We were unable to offer the course in the spring of 2020. Here, we present the finalized materials that were successfully used in 2019. We created a syllabus (Appendix A) providing an overview of the sessions, session learning objectives, overview of session content, the three presession assignments, and assessment criteria. The course was pass/fail; learners were assessed by the listed criteria and formatively assessed during the active learning exercises through direct observation, self-assessment, and facilitator and peer feedback. Appendix A is the full syllabus should the course be used in its entirety. The entire course was conceptually divided into two sections; each individual session lasted 90 minutes.
Section 1: Direct Participation in Interpersonal Encounters With Patients and Peers
Session 1
We introduced the concept of IBRM using slides (Appendix B) and a facilitator guide (Appendix C). We required only the ability to project the slides.
Session 2
We designed the session to give students opportunities to begin observing behaviors. Using slides (Appendix D) as the backdrop to discussion, we introduced some relevant frameworks, including transformative learning theory. As detailed in the facilitator guide (Appendix E), we used widely available video clips to demonstrate the ubiquitous nature of implicit bias in society. We required the ability to project the slides and internet connectivity to play the videos.
Session 3
Using the facilitator guide (Appendix F), including a reflective writing prompt and debrief, we guided students toward introspection. They began reflecting on their own biases and explored the pervasiveness of assumptions.
Session 4
We assigned a presession assignment asking students to take the Race Implicit Association Test (IAT).23 Of note, we used the IAT as a tool for instruction in IBRM,11,24 not as an outcome measure or as an assessment of any individual. Using slides (Appendix G) as a backdrop, we highlighted the ubiquitous nature of implicit bias. We also examined two etiologies of implicit bias: personal lived experiences and stereotyping of minority groups by the media. We again used short, relevant, and timely video clips from the internet, as detailed in the facilitator guide (Appendix H). The prompt for the written reflection asked students to consider the effects of media representations of racial minority groups on both people who identify with a particular group and people who do not. Students were then asked to debrief on their experience taking the Race IAT. The IAT was intentionally assigned after a few sessions had occurred to enhance the probability that students would have increased knowledge and context about implicit bias, as well as an increased level of trust in each other, as compared to the first session. Finally, we guided students through a personal narrative exercise. In this exercise, students explored the influence of their lived experiences on the development of their biases; facilitators participated in this exercise as well. At the end of the session, we gave students the opportunity to reflect on previous learning objectives in order to reinforce learning. To run this session, we required the ability to project the slides, internet access to view the video clips, and printed copies of the writing prompt.
Session 5
We focused on the patient's perspective while facilitating an interactive discussion supported by slides (Appendix I) and the facilitator guide (Appendix J). We began this session with a brief discussion of empathy, then introduced perspective-taking exercises as a tool to teach empathy. We next reviewed the evidence suggesting patients' lived experience can influence their perception of bias in a clinical encounter.20 We guided students through the evidence and discussed the importance of acknowledgment of the perceived (or actual) bias. Following this discussion, students observed videos and practiced considering the perspective of each of the people portrayed in them. Using a reflection prompt, we encouraged the students to imagine the perspective of the person(s) portrayed and consider how these snippets of each person's lived experience could influence their behaviors as patients once in the clinical setting. The session closed with space for reflections on previous learning objectives. We required the ability to project the slides, internet access to view the video clips, and printed copies of the reflection prompt.
Session 6 (first portion)
Strategy identification began in earnest in session 6. Using the slides (Appendix K) and facilitator guide (Appendix L), we facilitated reflection on the influence of patients' lived experiences on their perceptions of bias, which built on the discussion started in session 5. Subsequently, students brainstormed to collectively identify strategies to connect with patients who may have a very different lived experience than the students. This brainstorm concluded section 1.
Section 2: Addressing Perceived Bias in the Learning Environment
In section 2, we delivered the remainder of the course—sessions 6–9. This section focused on perceived bias in the learning environment.
Session 6 (second portion)
During this session (Appendices K and L), students transitioned to skill development to address perceived bias in witnessed encounters. We delivered bystander training using the Confronting Prejudiced Responses (CPR) model.25 After we explained the CPR model, students practiced its steps. The facilitator read a prepared reflection. Subsequently, each student practiced their first skill, verbalizing out loud what they would say to the attending physician to advocate for the patient in the encounter while ensuring no damage was done to their relationship with the attending. We conducted a role-play in a fishbowl format for the final exercise in this session. The purpose of this role-play was to enable learners to practice observing behaviors (following an observation prompt) and the debrief of a role-play before they actually participated in a role-play in the unscripted role. We required the ability to project the slides, printed copies of the role-play roles, and printed copies of the handout (the latter two are included in Appendix L).
Sessions 7, 8, and 9
We provided further opportunities for skill development and practice to address perceived bias in witnessed encounters within the learning environment using the facilitator guide (Appendix M). We addressed three types of bias in the role-plays—gender, religion, and race. Students participated in the role-plays in the unscripted role, in the scripted roles, or as observers of the role-play. Each role was described in the facilitator guide. All students participated in the debrief. Students reviewed their roles; the facilitator played the role of the faculty member. We encouraged the student in the unscripted role to do their best and reminded them they were in a safe and supportive learning environment. We conducted each role-play for 3 minutes, video-recorded them, and subsequently debriefed each one following the format developed at the Stanford Faculty Development Center for Medical Teachers.26 The debrief structure was the same regardless of the content of the role-play. After the debrief, the student in the unscripted role got a do-over. This enabled the student to practice implementing one of the skills identified during the debrief, thereby gaining a new skill. In order to conduct these final three sessions, we required the ability to video-record, the ability to project the recording, and a printed copy of each role for that session's role-play.
Student Assessment
Students completed a knowledge pretest/posttest, which was anonymous; we analyzed these in aggregate for the program evaluation. We formatively assessed students through multiple direct observations. These included (1) their contributions to discussions regarding their written reflections, (2) verbalized statements seeking to advocate on behalf patients, and (3) skills in addressing biased comments within the learning environment (i.e., performance in the unscripted role during the role-plays). This final assessment occurred during the debrief, always in a specified order. The student in the unscripted role self-assessed first, those in the role of participants in scripted roles discussed their reactions to the skills employed next, and then the observing students contributed their observations. Finally, as the facilitator participated in the role-play, she was able to assess the student's performance from her perspective in her scripted role and her experience in a general medical education context. Given that our direct observations were formative assessments, they were educational in nature as well.
Program Evaluation
We report the evaluation of the impact of our instruction following the classification of Kirkpatrick's educational outcomes as modified by Barr and colleagues.27 In this classification, learner reactions is level 1. Level 2 is divided into two: level 2a—modification of attitudes and perceptions—and level 2b—acquisition of knowledge and skills. We were striving to develop and pilot cutting-edge instructional strategies; thus, we utilized three approaches in our mixed-method program evaluation. First, students filled out a pretest and posttest during the first and last sessions of the elective, respectively. This survey was anonymous and therefore was not used to assess the students themselves. Pretests and posttests were linked by four-digit identifiers to enable matching while maintaining anonymity. These surveys included questions on demographic data plus eight questions related to knowledge and awareness of implicit bias as a concept and its potential to influence interpersonal encounters, as well as students' self-perceived comfort in addressing potential bias in four different types of interpersonal encounters (questions 1–4 and 5–8, respectively, in the Table). Responses were scored on a 6-point Likert-type scale (1 = strongly disagree, 6 = strongly agree). Results were analyzed in aggregate. Given the nonnormal distribution of our data and small sample size, statistical analyses were conducted using Wilcoxon signed rank tests to compare median values; for ease of interpretation, however, means and standard deviations are reported in the text and the Table. Second, members of the research team took notes to capture skills that emerged during each session and to identify aspects of each session needing improvement, as well as components that worked well. We debriefed after each session. Finally, we incorporated two additional mandatory feedback sessions within the course (2017–2018), one midway through the course and one upon completion of all instruction. This comprehensive qualitative component of the program evaluation has been reported elsewhere.14 All procedures were approved by the Institutional Review Board of the Albert Einstein College of Medicine, which deemed the research exempt.
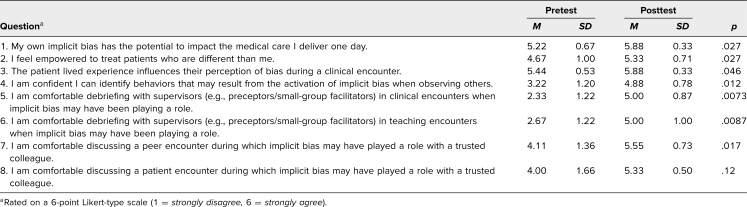
Table. Questions on Anonymous Pretest/Posttest.
Results
Out of 15 students who participated in all or some components of the elective, we obtained completed pretests and posttests from 12. Regarding student demographic data, two identified as Latino/a/x, five as Asian, and five as White; four identified as female, eight as male. Eight students had undergraduate degrees in physical sciences, two in social sciences, and two had double majors in both physical and social sciences. The median age was 23.5 years (range: 22–36 years).
Pretest and posttest results are listed in the Table. Overall, scores increased 10.1 points (from M = 32.8, SD = 1.92, to M = 42.9, SD = 1.45, out of a total possible 48; p = .0078). Scores demonstrated an increase in self-reported perceptions of knowledge, comfort, and confidence (level 2a). The largest and most significant increases involved perceptions of comfort with debriefing with supervisors (e.g., attending physicians) about perceived bias in clinical and teaching encounters (items 5 and 6, respectively). Debriefing about a patient encounter during which students' own bias may have played a role (item 8) was the only item that did not demonstrate a statistically significant increase. In 2019, the Office of Medical Education sent out course evaluations to the students. Of the three responses submitted, “More role-play!” was the only suggestion in response to the question “If you were the elective director, what changes, if any, would you make to this elective?”
We assessed knowledge and skill acquisition (level 2b) through direct observation during the active learning exercises, as described above. Analysis of notes taken by the investigative team during direct observation revealed the creativity of our students in their skill development. We found that a common denominator for skills was to address the bias but to do so in a way that was nonthreatening. Students learned to ask for clarification regarding rationales in decision-making and for the evidence when comments were stated as truths about the hypothetical patient. For example, during the role-play of a lecture in which the lecturer made an off-the-cuff statement that the students perceived as bias, one student raised his hand and asked, “I'm curious to learn more about that, may I have the references?” Students most commonly addressed perceived bias by framing statements as inquiries to enhance their own learning or clarify clinical concepts.
Discussion
We created a skills-based curriculum to address implicit bias in the learning environment. To our knowledge, we are the first to successfully implement role-plays to enable learners to develop and practice skills that are personally relevant to them to address bias. In addition, students are able to resolve the discomfort previously reported when they feel unable to advocate for patients.4 Role-plays address perceived bias not only with peers but also with supervisors (a special challenge for medical students given the inherent hierarchy of medical training). The learning objectives, detailed facilitator guides, and course materials can be used sequentially as a stand-alone course or can be integrated within existing compulsory instruction. Any active learning exercise can be offered on its own, thereby enabling the skills-based exercises to be delivered to learners with existing knowledge and experience concerning IBRM. Given the ubiquitous nature of bias, the impact of perceived or actual bias on communication with patients, and the hierarchical structure of medical education and training, course materials should be relevant to both undergraduate and graduate medical education. Although this curriculum was developed for preclinical medical students, it can be adapted to any level of learner, given its focus on three content areas relevant to health professionals at any stage of their career: “1) interpersonal interactions; 2) advocating for patients when bias is perceived in witnessed encounters with peers and supervisors; and 3) addressing comments within the learning environment.”14 A final key point is that the skills identified by our learners are relevant to perceived bias across multiple constructs (e.g., gender, religion, and race) and not unique to each particular construct. Therefore, the curriculum can serve as a framework that is broadly applicable across many constructs of interest; modifications of the active learning exercises could be made to include scenarios that address perceived bias against sexual or gender minorities, other religious minorities, and obese patients, among others.
We developed this course in an iterative process over 3 years. Initially, we began as a small team developing the initial content. Sessions were revised based on postsession debriefs conducted by the investigative team, as well as two formal feedback sessions incorporating focus groups in the first 2 years. While we recognize that level of feedback is unrealistic for general offerings of this content, there are opportunities to involve learners and solicit feedback. For example, as detailed in the facilitator guides, learners can be engaged in selection of video clips available on the internet, providing an excellent opportunity to co-construct instruction by asking students for their suggestions. In our qualitative program evaluation, students liked video clips from popular-cultures shows or authentic YouTube user experiences; they valued their relevance and timeliness.14 An open policy can be communicated to students soliciting both feedback on what is working well and suggestions for improvement. Faculty can role-model a growth mindset by accepting and implementing feedback. A growth mindset and a focus on implicit bias as a professionalism issue relevant to all physicians are beneficial for instruction in IBRM.22
Many learners are coming into medical school and postgraduate training with experience in issues of implicit bias and social justice. A central tenet of adult learning theory is to respect and build upon learners' lived experiences.28 In delivering this course, we learned a lot from our students, and we ensured they had space to express their views and ideas. This is in keeping with Freire's theory of problem-posing education, during which the teacher becomes the teacher-student and the student becomes the student-teacher, thus jointly becoming responsible for the instructional process.29 As we have previously reported, this approach could engage more faculty as facilitators, as it can alleviate the pressures perceived by faculty regarding implicit bias instruction.21 When possible, cofacilitation with a facilitator who is a near peer to the students can also help engage learners in the compulsory curriculum.4
We have identified several specific lessons learned that could inform implementation of this curriculum beyond a small elective. Learners at all stages of training and practice may have deep and emotional reactions to the IAT.4,30 We recommend that it be assigned only after at least some introductory instruction has been delivered, in order to engage learners in a meaningful discussion. The role-plays were initially intimidating for our students. The safe, respectful, and structured debrief, along with the do-over, enhanced students' attitudes toward participating in role-plays. This do-over was described as a “gift” during our student feedback sessions.14 Students' approach to addressing perceived bias during the role-pays by framing the question as an inquiry to enhance their own learning was a powerful way to draw attention to the biased statement without directly accusing the faculty member. This approach avoided the tacit complicity of silence after hearing a biased statement but did not risk damaging the relationship with the supervisor or peer. Finally, we learned that making ourselves vulnerable to discuss mistakes we make because of our biases did not result in any student backlash. On the contrary, it enhanced student engagement, consistent with previous research.4
Limitations
Our curriculum has several limitations. Because we developed and implemented the instruction with a small number of self-selected learners, we do not know how students in our compulsory curriculum will react to it, although we have provided suggestions for consideration. Very small groups might not be realistic in a full medical school class, hindering the possibility that every learner will get to participate in the unscripted role in a role-play. Fortunately, according to social learning theory, learners can have increased self-efficacy to address bias in the learning environment through the vicarious experience of being observers of the role-play and participating in the debriefs.31 Assessment of learners requires direct observation, which requires faculty presence. A potential method to alleviate this time constraint may be to utilize near-peer cofacilitators. Furthermore, no standardized checklists for skills in IBRM exist, as the skills at the time were not known. Thus, our assessments were based on general notes taken during the sessions themselves. We were only able to evaluate perceived knowledge gains in this program evaluation, as the outcomes were self-reported. Although we wrote the facilitator guides to provide enough guidance that faculty would not need prerequisite knowledge to facilitate the sessions, faculty may feel more comfortable practicing facilitation with peer groups, or a single faculty member could conduct faculty development programs in the same way we have previously outlined.32 In addition, we refer interested faculty to a recent publication on facilitating instruction in IBRM for further best practices.12
Future Directions
We developed skills-based instruction to empower learners to address perceived bias in their own encounters and within the learning environment. Future directions include evaluation of the course within the compulsory curriculum, as well as collaboration and adaptation for instruction across health professions throughout the spectrum of training and practice and while working in interprofessional teams. In addition, we envision creating role-plays and exercises with standardized patients for more advanced learners in order to offer opportunities for skill development and practice in restoring rapport with the patient during the encounter once bias is perceived.
Appendices
- Syllabus.docx
- Session 1 Slides.pptx
- Session 1 Facilitator Guide.docx
- Session 2 Slides.pptx
- Session 2 Facilitator Guide.docx
- Session 3 Facilitator Guide.docx
- Session 4 Slides.pptx
- Session 4 Facilitator Guide.docx
- Session 5 Slides.pptx
- Session 5 Facilitator Guide.docx
- Session 6 Slides.pptx
- Session 6 Facilitator Guide.docx
- Sessions 7-9 Facilitator Guide.docx
All appendices are peer reviewed as integral parts of the Original Publication.
Acknowledgments
We would like to thank Monica L. Lypson, MD, MHPE, for providing graphics for the Confronting Prejudiced Responses (CPR) model.
Since this research was done, Sydney A. Walker has graduated and earned an MD degree.
Disclosures
None to report.
Funding/Support
None to report.
Prior Presentations
Gonzalez CM, Walker SA, Karp E, Rodriguez N, Noah Y, Marantz PR. Implicit bias recognition and management: advancing from awareness to skills. Poster presented at: Society of General Internal Medicine Annual Meeting; April 11–14, 2018; Denver, CO.
Ethical Approval
The Albert Einstein College of Medicine Institutional Review Board approved this study.
References
- 1.Cooper LA, Roter DL, Carson KA, et al. The associations of clinicians' implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. Am J Public Health. 2012;102(5):979–987. 10.2105/AJPH.2011.300558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hagiwara N, Slatcher RB, Eggly S, Penner LA. Physician racial bias and word use during racially discordant medical interactions. Health Commun. 2017;32(4):401–408. 10.1080/10410236.2016.1138389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gonzalez CM, Bussey-Jones J. Disparities education: what do students want? J Gen Intern Med. 2010;25(suppl 2):102–107. 10.1007/s11606-010-1250-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gonzalez CM, Deno ML, Kintzer E, Marantz PR, Lypson ML, McKee MD. A qualitative study of New York medical student views on implicit bias instruction: implications for curriculum development. J Gen Intern Med. 2019;34(5):692–698. 10.1007/s11606-019-04891-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sandoval RS, Afolabi T, Said J, Dunleavy S, Chatterjee A, Ölveczky D. Building a tool kit for medical and dental students: addressing microaggressions and discrimination on the wards. MedEdPORTAL. 2020;16:10893. 10.15766/mep_2374-8265.10893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Teal CR, Shada RE, Gill AC, et al. When best intentions aren't enough: helping medical students develop strategies for managing bias about patients. J Gen Intern Med. 2010;25(suppl 2):115–118. 10.1007/s11606-009-1243-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gonzalez CM, Fox AD, Marantz PR. The evolution of an elective in health disparities and advocacy: description of instructional strategies and program evaluation. Acad Med. 2015;90(12):1636–1640. 10.1097/ACM.0000000000000850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brooks KC, Rougas S, George P. When race matters on the wards: talking about racial health disparities and racism in the clinical setting. MedEdPORTAL. 2016;12:10523. 10.15766/mep_2374-8265.10523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.DallaPiazza M, Padilla-Register M, Dwarakanath M, Obamedo E, Hill J, Soto-Greene ML. Exploring racism and health: an intensive interactive session for medical students. MedEdPORTAL. 2018;14:10783. 10.15766/mep_2374-8265.10783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Burgess D, van Ryn M, Dovidio J, Saha S. Reducing racial bias among health care providers: lessons from social-cognitive psychology. J Gen Intern Med. 2007;22(6):882–887. 10.1007/s11606-007-0160-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sukhera J, Watling CJ, Gonzalez CM. Implicit bias in health professions: from recognition to transformation. Acad Med. 2020;95(5):717–723. 10.1097/ACM.0000000000003173 [DOI] [PubMed] [Google Scholar]
- 12.Gonzalez CM, Lypson ML, Sukhera J. Twelve tips for teaching implicit bias recognition and management. Med Teach. Published online February 8, 2021. 10.1080/0142159X.2021.1879378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gonzalez CM, Noah YS, Correa N, Archer-Dyer H, Weingarten-Arams J, Sukhera J. Qualitative analysis of medical student reflections on the Implicit Association Test. Med Educ. 2021;55(6):741–748. 10.1111/medu.14468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gonzalez CM, Walker SA, Rodriguez N, Karp E, Marantz PR. It can be done! A skills-based elective in implicit bias recognition and management for preclinical medical students. Acad Med. 2020;95(12S):S150–S155. 10.1097/ACM.0000000000003697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gonzalez CM, Kim MY, Marantz PR. Implicit bias and its relation to health disparities: a teaching program and survey of medical students. Teach Learn Med. 2014;26(1):64–71. 10.1080/10401334.2013.857341 [DOI] [PubMed] [Google Scholar]
- 16.Teal CR, Gill AC, Green AR, Crandall S. Helping medical learners recognise and manage unconscious bias toward certain patient groups. Med Educ. 2012;46(1):80–88. 10.1111/j.1365-2923.2011.04101.x [DOI] [PubMed] [Google Scholar]
- 17.Sukhera J, Watling C. A framework for integrating implicit bias recognition into health professions education. Acad Med. 2018;93(1):35–40. 10.1097/ACM.0000000000001819 [DOI] [PubMed] [Google Scholar]
- 18.Mezirow J. Transformative learning: theory to practice. In: Cranton P, ed. Transformative Learning in Action: Insights From Practice. Jossey-Bass; 1997:5–12. [Google Scholar]
- 19.Gill A, Thompson B, Teal C, et al. Best intentions: using the Implicit Associations Test to promote reflection about personal bias. MedEdPORTAL. 2010;6:7792. 10.15766/mep_2374-8265.7792 [DOI] [Google Scholar]
- 20.Gonzalez CM, Deno ML, Kintzer E, Marantz PR, Lypson ML, McKee MD. Patient perspectives on racial and ethnic implicit bias in clinical encounters: implications for curriculum development. Patient Educ Couns. 2018;101(9):1669–1675. 10.1016/j.pec.2018.05.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gonzalez CM, Garba RJ, Liguori A, Marantz PR, McKee MD, Lypson ML. How to make or break implicit bias instruction: implications for curriculum development. Acad Med. 2018;93(11S):S74–S81. 10.1097/ACM.0000000000002386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Williams RL, Vasquez CE, Getrich CM, et al. Racial/gender biases in student clinical decision-making: a mixed-method study of medical school attributes associated with lower incidence of biases. J Gen Intern Med. 2018;33(12):2056–2064. 10.1007/s11606-018-4543-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Project Implicit. Accessed January 29, 2021. https://implicit.harvard.edu/implicit/
- 24.Sukhera J, Wodzinski M, Rehman M, Gonzalez CM. The Implicit Association Test in health professions education: a meta-narrative review. Perspect Med Educ. 2019;8(5):267–275. 10.1007/s40037-019-00533-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ashburn-Nardo L, Morris KA, Goodwin SA. The Confronting Prejudiced Responses (CPR) model: applying CPR in organizations. Acad Manage Learn Educ. 2008;7(3):332–342. 10.5465/amle.2008.34251671 [DOI] [Google Scholar]
- 26.Objectives. Stanford Faculty Development Center for Medical Teachers. Accessed May 21, 2021. https://med.stanford.edu/sfdc.html
- 27.Barr H, Koppel I, Reeves S, Hammick M, Freeth D. Effective Interprofessional Education: Argument, Assumption and Evidence. Blackwell Publishing; 2005. [Google Scholar]
- 28.Merriam SB, Caffarella RS, Baumgartner LM. Learning in Adulthood: A Comprehensive Guide. 3rd ed. Wiley; 2007. [Google Scholar]
- 29.Freire P. Pedagogy of the Oppressed. Continuum; 1993. [Google Scholar]
- 30.Sukhera J, Wodzinski M, Milne A, Teunissen PW, Lingard L, Watling C. Implicit bias and the feedback paradox: exploring how health professionals engage with feedback while questioning its credibility. Acad Med. 2019;94(8):1204–1210. 10.1097/ACM.0000000000002782 [DOI] [PubMed] [Google Scholar]
- 31.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215. 10.1037/0033-295X.84.2.191 [DOI] [PubMed] [Google Scholar]
- 32.Gonzalez CM, Nava S, List J, Liguori A, Marantz PR. How assumptions and preferences can affect patient care: an introduction to implicit bias for first-year medical students. MedEdPORTAL. 2021;17:11162. 10.15766/mep_2374-8265.11162 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
- Syllabus.docx
- Session 1 Slides.pptx
- Session 1 Facilitator Guide.docx
- Session 2 Slides.pptx
- Session 2 Facilitator Guide.docx
- Session 3 Facilitator Guide.docx
- Session 4 Slides.pptx
- Session 4 Facilitator Guide.docx
- Session 5 Slides.pptx
- Session 5 Facilitator Guide.docx
- Session 6 Slides.pptx
- Session 6 Facilitator Guide.docx
- Sessions 7-9 Facilitator Guide.docx
All appendices are peer reviewed as integral parts of the Original Publication.