Abstract
Background
The novel Oblique lumbar interbody fusion [OLIF] technique has been proposed as a solution to approach related complications of anterior lumbar interbody fusion [ALIF] and lateral lumbar interbody fusion [LLIF]. There exists no study concerning morphological evaluation of retroperitoneal oblique corridor for the Oblique lumbar interbody fusion (OLIF) technique in the Indian population. The aim of our study was (a) to measure magnetic resonance imaging (MRI) based anatomic parameters concerning OLIF operative windows from L2–L3 to L4–L5 level (b) to determine the feasibility of this technique following MRI-based morphometric evaluation in the Indian population.
Material and methods
We did retrospective MRI analysis of 307 consecutive patients following our exclusion criteria. Bare window, psoas major window and psoas major width were measured from axial T2 MRI image taken at mid disc level from L2–L3 to L4–L5 levels.
Results
The mean bare window size was largest at L2–L3 (1.39 cm) level followed by L3–L4 and L4–L5 level (1.28 and 0.62 cm respectively), and differences between them were statistically significant (P < 0.001). Females had statistically significant larger bare windows at L2–L3 and L3–L4 level than males (P < 0.001). With increasing age, there was a significant increase in bare window size at each level (P < 0.001). The mean psoas major window (PMO) and mean psoas major width (PMI) were largest at L4–L5 level (PMO = 1.27 cm, PMI = 3.61 cm) followed by L3–L4 and L2–L3 level (L3–L4: PMO = 1.19 cm, PMI = 2.36 cm; L2–L3: PMO = 0.88 cm, PMI = 1.39 cm), and differences among each level concerning both parameters were statistically significant (P < 0.001). Both parameters (PMO, PMI) were significantly larger in males than females at each level (P < 0.001).
Conclusion
The OLIF technique is well suited for lumbar interbody fusion at L2 -L3 and L3–L4 level in the Indian population irrespective of age and sex. At L4–L5 level, overall 17.9 percent of the study population were unsuitable for this technique due to inaccessible bare window. In our opinion, this level may be better suited for OLIF approach in the elderly Indian population, especially for surgeons who are beginning to attempt this technique in their surgical practice. Preoperative MRI evaluation for the OLIF is important to assess its feasibility, as there exists significant age and gender differences in the Indian population for anatomic parameters concerning OLIF operative windows from L2–L3 to L4–L5 levels.
Supplementary Information
The online version contains supplementary material available at 10.1007/s43465-021-00393-7.
Keywords: Interbody fusion, OLIF, Indian population, Magnetic resonance imaging
Introduction
Lumbar interbody fusion is a proven treatment strategy for diverse spinal disorders which includes unstable degenerative conditions, trauma, infection and neoplasia [1]. Broadly fusion can be achieved via posterior approaches which include posterior lumbar interbody fusion [PLIF] and transforaminal interbody fusion [TLIF], and the anterolateral approaches: anterior lumbar interbody fusion [ALIF], transpsoas lateral lumbar interbody fusion [LLIF] and oblique lumbar interbody fusion [OLIF]. Posterior approaches have proven acceptable fusion rates but result in disruption of posterior tension band, iatrogenic injury to paraspinal musculature and limited endplate exposure restricted by thecal sac and nerve roots which may cause difficulty in the correction of coronal imbalance and lordosis restoration [1]. The ALIF approach provides excellent exposure of L4–L5 and L5-S1 disc levels allowing better endplate preparation and larger size cage implantation resulting to adequate deformity correction with the restoration of lumbar lordosis. Avoidance of posterior vertebral segments results in lesser postoperative axial pain and reduced possibility of adjacent segment disease. The associated complications include visceral injury, vascular injury, retrograde ejaculation, intestinal adhesions, and abdominal hernia [2]. The LLIF approach aims to overcome these ALIF-related complications by utilizing access to disc via transmuscular interval through psoas. However, this approach results in a potential risk of injury involving lumbar plexus or femoral nerve as they course through psoas muscle and this mandates the procedure to be done under intraoperative neuromonitoring [3]. The “pre-psoas” approach involving oblique corridor between psoas major laterally and aorta or common iliac vessels medially, was first described by Mayer and referred to as OLIF by Silvestre et al. [4, 5]. It is among the latest techniques being proposed as a solution to approach related complications of ALIF and LLIF, which has been demonstrated by promising preliminary results by various studies [6]. Further anatomical research regarding OLIF will guide the surgeons to enhance their skills and help in achieving widespread acceptance of this approach among them [7]. In the present literature there exist few cadaveric and radiological studies involving computed tomography & magnetic resonance imaging, which have described the oblique corridor concerning the OLIF technique in white and Asian population [7–12]. To the best of our knowledge, the present study is the first to evaluate retroperitoneal oblique corridor for OLIF technique in the Indian population. The aim of our study was (a) to measure magnetic resonance imaging (MRI) based anatomic parameters concerning OLIF operative windows from L2–L3 to L4–L5 level and (b) to determine the feasibility of this technique following MRI based morphometric evaluation in the Indian population. This will provide a robust anatomical database to guide future studies about this emerging technique from the Indian subcontinent.
Material and Methods
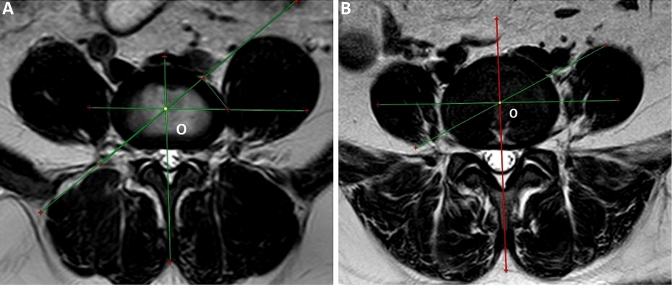
Approval of the ethical committee at our institute was obtained prior to the study. We collected data of 307 consecutive patients following our exclusion criteria after a retrospective review of MRI scans from September to December 2019, who had presented to our department for treatment regarding low back pain with or without radicular symptoms and required MRI of lumbar spine during their course of treatment. Exclusion criteria included age less than 18 years, traumatic, tumorous or spondylodiscitis cases, prior lumbar or retroperitoneal surgery, any lumbar anterior great vessel abnormality, vertebral abnormalities such as transitional lumbar anomalies, hemivertebrae, spina bifida, and spinal deformities such as scoliosis or kyphosis apart from lumbar degenerative disorders as their cause. MRI scans were taken with a 3 T Philips Achieva system (Philips healthcare, Netherlands) and data measurement was done using Radiant DICOM viewer software (version 72 5.0.0.219060). T2W MRI images in sagittal and axial plane were independently assessed by a senior spinal surgeon and a senior radiologist. First, mid-sagittal T2W view was used to identify disc level on the axial view. Subsequently axial T2W MRI image taken at mid disc level from L2–L3 to L4–L5 levels was used for performing measurements. As per prior published studies in the existing literature, the following operative windows of the OLIF were measured: bare window [bare unobstructed disc portion bounded by abdominal aorta or left iliac vessels medially and left psoas major laterally], psoas major window [left front portion of disc space which is covered by left psoas major from its anterior portion up to middle frontal plane], and psoas major width [width of left psoas major on the middle frontal plane of the intervertebral disc space] (Fig. 1) [7, 9]. The average of measurements obtained by the two reviewers for the operative windows of OLIF at each disc level were recorded.
Fig. 1.
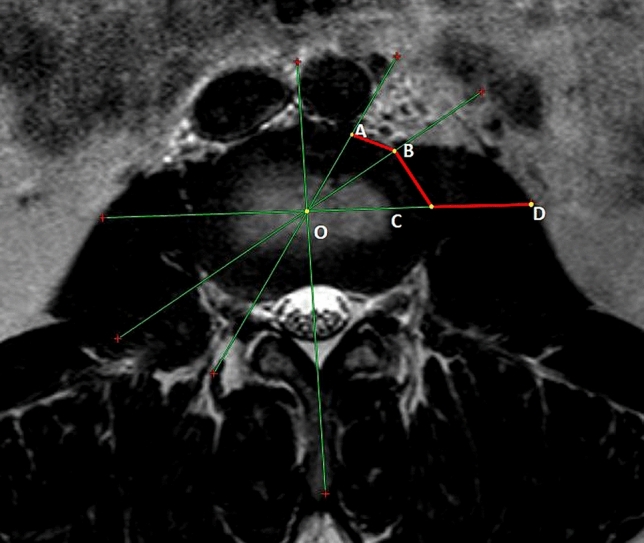
Axial T2 MR image at mid-disc level of L3–L4 level. O: approximate intervertebral disc centre; AB: Bare window; BC: Psoas major window; CD: Left psoas major width in the middle frontal plane.
All statistical data analysis was done using IBM SPSS Statistics for Windows, Version 20.0., IBM Corp., Chicago, IL. Descriptive statistics were reported as mean ± SD for continuous variables. The one-way analysis of variance (ANOVA) was used to assess any differences between the bare window of each age group. The unpaired T test was used to compare OLIF operative window parameters between sexes and differences between each level. P value < 0.05 indicated a significant difference for all the statistical data analysis done using ANOVA and unpaired t test.
Results
The study evaluated MRI records of 307 patients, 154 [50.2%] were males and 153 [49.8%] were females. Mean age was 41.07 years [SD 14.37, range 18–78 years].
Bare Window
The bare window represents the unobstructed oblique corridor and its size is critical to perform the OLIF technique safely. All MRI scans showed a clear bare window at L2–L3 and L3–L4 levels. In 55 [17.9%] MRI scans bare window at L4–L5 level was inaccessible because of absent interval seen in 25 (8.14%) patients and non-measurable interval either due to high rising psoas muscle (19 patients, 6.19%) or abnormal laterally positioned iliac vessels (11 patients, 3.58%) [Fig. 2a, b]. Among this group, 44 MRI scans [23 male, 21 females] were < 40 years age, seven [five male, two females] were between 40 and 60 years age and four [two male, two females] were > 60 years age. The value was taken as zero for both absent and non-measurable bare window at L4–L5 level while doing statistical data analysis. It was largest at L2–L3 (1.39 ± 0.39 cm) level followed by L3–L4 and L4–L5 level (1.28 ± 0.38 and 0.62 ± 0.49 cm, respectively) (Table 1). The unpaired T test was used to compare differences between sexes [Table 2]. The women had statistically significant larger size bare window than men at L2–L3 and L3–L4 levels (P < 0.001). At L4–L5 level bare window was larger in men than women, but the difference was not statistically significant (P = 0.122). On analysis of bare window size differences according to different age groups at each level using the ANOVA test, the size was found to increase with age and was statistically significant for each level (P < 0.05) (Table 3). On comparing bare window differences between each level using the unpaired t test, statistically significant differences were found between all levels (P < 0.001) [Table 4].
Fig. 2.
Axial T2 MR image at mid-disc level of L4–L5 level showing non-measurable bare window because of; a High rising psoas major muscle; b Abnormal laterally positioned iliac vessels; O: approximate intervertebral disc centre
Table 1.
OLIF operative window parameters of each level
| Disc Level | Mean [cm] | SD | Min. [cm] | Max. [cm] | |
|---|---|---|---|---|---|
| L2–L3 | Bare window | 1.39 | 0.39 | 0.44 | 2.89 |
| Psoas major window | 0.88 | 0.38 | 0.00 | 2.04 | |
| L3–L4 | Bare window | 1.28 | 0.38 | 0.38 | 2.67 |
| Psoas major window | 1.19 | 0.39 | 0.00 | 2.43 | |
| L4–L5 | Bare window | 0.62 | 0.49 | 0.00 | 2.12 |
| Psoas major window | 1.27 | 0.35 | 0.28 | 2.53 | |
Min, minimum; Max, maximum
Table 2.
Comparative analysis of OLIF operative window parameters between sexes
| Disc level | Mean ± SD [cm] | Min. [cm] | Max. [cm] | P value | ||||
|---|---|---|---|---|---|---|---|---|
| M | F | M | F | M | F | |||
| L2–L3 | BW | 1.31 ± 0.37 | 1.48 ± 0.39 | 0.44 | 0.63 | 2.20 | 2.89 | < 0.001 |
| PMW | 1.05 ± 0.36 | 0.70 ± 0.33 | 0.00 | 0.00 | 2.04 | 1.76 | < 0.001 | |
| L3–L4 | BW | 1.19 ± 0.37 | 1.36 ± 0.37 | 0.38 | 0.56 | 2.67 | 2.32 | < 0.001 |
| PMW | 1.41 ± 0.35 | 0.99 ± 0.32 | 0.48 | 0.00 | 2.43 | 2.08 | < 0.001 | |
| L4–L5 | BW | 0.66 ± 0.52 | 0.57 ± 0.47 | 0.00 | 0.00 | 2.12 | 1.91 | 0.122 |
| PMW | 1.45 ± 0.31 | 1.09 ± 0.30 | 0.62 | 0.28 | 2.53 | 2.12 | < 0.001 | |
Min minimum; Max maximum; BW Bare window; PMW Psoas major window; M male; F female
Table 3.
Bare window width analysis according to age group
| Age group [n] | L2–L3 | L3–L4 | L4–L5 |
|---|---|---|---|
| < 40 years [n = 173] | 1.32 ± 0.35 | 1.20 ± 0.33 | 0.46 ± 0.41 |
| 40–60 years [n = 97] | 1.43 ± 0.39 | 1.33 ± 0.38 | 0.74 ± 0.47 |
| > 60 years [n = 37] | 1.63 ± 0.45 | 1.49 ± 0.50 | 1.04 ± 0.59 |
| P value | < 0.001 | < 0.001 | < 0.001 |
All values are mean ± SD [cm]; n, number of cases in each age group
Difference of Bare window width at L2–3: < 40 versus 40–60 (p = 0.03); 40–60 versus > 60 (p = 0.007); < 40 versus > 60 (p = < 0.001)
Difference of Bare window width at L3–4: < 40 versus 40–60 (p = 0.007); 40–60 versus > 60 (p = 0.032); < 40 versus > 60 (p = < 0.001)
Difference of Bare window width at L4-5: < 40 versus 40–60 (p = < 0.001); 40–60 versus > 60 (p = 0.001); < 40 versus > 60 (p = < 0.001)
Table 4.
OLIF operative window measurement differences between levels
| Operative window | Level | P value |
|---|---|---|
| Bare window | L2–L3 vs L3–L4 | < 0.001 |
| L3–L4 vs L4–L5 | < 0.001 | |
| L2–L3 vs L4–L5 | < 0.001 | |
| Psoas major window | L2–L3 vs L3–L4 | < 0.001 |
| L3–L4 vs L4–L5 | < 0.001 | |
| L2–L3 vs L4–L5 | < 0.001 |
Psoas Major Window
The psoas major window was largest at L4–L5 level (1.27 ± 0.35 cm) followed by L3–L4 and L2–L3 level (1.19 ± 0.39 and 0.88 ± 0.38 cm respectively) (Table 1). On comparison between sexes using unpaired T test, males had larger values than females at each level which were statistically significant (P < 0.001) (Table 2). Differences between each level were found to be statistically significant using unpaired t test (P < 0.001) (Table 4).
Psoas Major Width
The psoas major width was largest at L4–L5 level (3.61 ± 0.67 cm) followed by L3–L 4 and L2–L3 level (2.36 ± 0.77 and 1.39 ± 0.61 cm respectively), and statistically significant differences were found between each level using paired t test (P < 0.001). On comparing differences based on sex using unpaired T test, men had statistically significant larger values than women at each level (P < 0.001) (Table 5).
Table 5.
Psoas major width measurement analysis
| Parameters | L2–L3 | L3–L4 | L4–L5 |
|---|---|---|---|
| Male | 1.74 ± 0.52 | 2.79 ± 0.68 | 3.92 ± 0.61 |
| Female | 1.04 ± 0.48 | 1.93 ± 0.59 | 3.29 ± 0.57 |
| P value | < 0.001 | < 0.001 | < 0.001 |
| Male + Female | 1.39 ± 0.61 | 2.36 ± 0.77 | 3.61 ± 0.67 |
All values are mean ± SD [cm]; Psoas major width: L2–L3 versus L3–L4, P < 0.001; L3–L4 versus L4–L5, P < 0.001; L2–L3 versus L4–L5, P < 0.001
A further comparative depiction of present study results with those of prior published studies concerning MRI-based morphometric assessment of retroperitoneal OLIF corridor in the lumbar spine at different disc levels has been highlighted in Table 6.
Table 6.
Comparison of present study results with previous published studies
| Molinares et al. [10] study (x ± S, cm) | Boghani et al. [12] study (x ± S, cm) | Li et al. [11] study (x ± S, cm) | Zhang et al. [17] study (x ± S, cm) | Chen et al. [7] study (x ± S, cm) | Present study (x ± S, cm) | |
|---|---|---|---|---|---|---|
| BW [Disc level] | ||||||
| L2–L3 | 1.60 ± 0.58 | 1.73 ± 0.64 | 1.55 ± 0.54 | 1.35 ± 0.35 | 1.43 ± 0.46 | 1.39 ± 0.39 |
| L3–L4 | 1.42 ± 0.57 | 1.62 ± 0.63 | 1.28 ± 0.53 | 1.31 ± 0.35 | 1.37 ± 0.46 | 1.28 ± 0.38 |
| L4–L5 | 1.03 ± 0.68 | 1.48 ± 0.78 | 0.89 ± 0.66 | 0.90 ± 0.43 | 1.01 ± 0.60 | 0.62 ± 0.49 |
| PMO [Disc level] | ||||||
| L2–L3 | 1.04 ± 0.42 | 0.88 ± 0.38 | ||||
| L3–L4 | 1.34 ± 0.42 | 1.19 ± 0.39 | ||||
| L4–L5 | 1.40 ± 0.39 | 1.27 ± 0.35 | ||||
| PMI [Disc level] | ||||||
| L2–L3 | 1.34 ± 0.54 | 1.39 ± 0.61 | ||||
| L3–L4 | 2.20 ± 0.74 | 2.36 ± 0.77 | ||||
| L4–L5 | 3.37 ± 0.69 | 3.61 ± 0.67 | ||||
All values (x ± S, cm) are mean ± SD [cm]: BW Bare window: PMO Psoas major window: PMI Psoas major width
Discussion
The novel OLIF technique has become increasingly popular in view of its several advantages like minimal blood loss and tissue damage with preservation of posterior tension band, allows larger size cage placement with the adequate restoration of disc height and provides indirect decompression, achieves better correction of sagittal and coronal alignment, and has minimal risk of lumbar plexus injury [13]. However, there exists a paucity of high-quality literature regarding OLIF, although promising early results have demonstrated its feasibility [6]. As this relatively new technique involves traversing through an unfamiliar anatomy, it has its own specific approach-related complications. The most common complication is postoperative numbness in the groin or anterior thigh and hip flexion weakness because of undue retraction of the psoas muscle and its associated sensory nerves. Other reported complications include ureter injury, vascular complications involving main vessels, segmental artery or iliolumbar vein, peritoneal injury, and abdominal ileus because of overzealous retroperitoneal space manipulation [14].
For widespread acceptance of any new technique, a thorough anatomical knowledge is required to assess its feasibility and facilitate improvement in surgical skills of the surgeons resulting in minimizing complications [7]. According to Liu et al., the anatomical measurements made in vivo have credibility and reliable resemblance to the human surgical state [9]. Prior morphometric studies have highlighted significant differences among the Indian and western population with regard to various spinal parameters [15, 16]. Therefore, we decided to evaluate morphometric data regarding the OLIF operative windows in the Indian population, as no prior study has documented it in the existing literature. We evaluated the OLIF parameters from L2–L3 to L4–L5 levels. The oblique access trajectory above L2 level may be affected by ribs or by blockage because of the left kidney and its accompanying vasculature. OLIF at L5-S1 level remains a challenge because of risks involved with mobilization of iliac vessels and the presence of iliac wing [11]. In view of these reasons, L1–L2 and L5-S1 levels were not included in the present study.
The bare window represents the unobstructed oblique corridor leading to the intervertebral disc between the aortoiliac vessels and left psoas major [7]. On assessing mean bare window interval size of different lumbar levels, our result patterns were similar to prior studies that showed a progressive decrease in corridor size as we proceed from upper to lower lumbar levels [7, 10–12, 17]. The differences in bare window size among different levels in our study were statistically significant, as was reported by Molinares et al. in their study [10].
On comparison of our results with those of prior published studies concerning the western population, we found that our mean bare window measurement at each lumbar level from L2–L3 to L4–L5 level was smaller on comparison to theirs, which might be because of anatomical variations based on racial differences [10–12]. Prior MRI-based morphometric studies among the Asian population concerning OLIF technique by Chen et al. and Zhang et al. have also illustrated smaller bare window size in Chinese in comparison to the western population based on racial differences [7, 17]. With regard to sex differences concerning bare window interval size, our results were similar to those reported by Chen et al. [7]. Female had statistically significant larger bare window at L2–L3 and L3–L4 levels, whereas difference at L4–L5 level was not statistically significant. On analysing bare window at each level with regard to different age groups, the results showed statistically significant larger corridor size with increasing age at each level. Our result patterns are similar to those documented by Li et al., and they proposed atrophy of psoas muscle with increasing age resulting in widening of bare window interval as the reason for it [11]. The results of a study by Chen et al. also illustrated that psoas major width decreased at each level with increasing age because of age-related muscle degeneration [7].
The safety and feasibility of the OLIF technique depend on the presence of an adequate bare window interval. As per Ng et al. an absent bare window corridor would be a contradiction for the OLIF procedure [18]. Based on methodology as per prior published studies, bare window interval was present in all our patients at L2–L3 and L3–L4 levels [7, 9]. Molinares et al. reported absent bare window in one case at L2–L3 level whereas Chen et al. reported absent bare window at both L2–L3 and L3–L4 levels in a single case [7, 10]. In our study at L4–L5 level which showed an overall narrowest bare window, twenty-five cases (8.14%) had an absent interval similar to results of prior studies. Molinares et al. reported absent bare window in nine cases (9%) at L4–L5 level, whereas Chen et al. reported it in twenty-nine cases (7.25%) of their study [7, 10]. In a recent MRI-based study by Ng et al. regarding bare window interval at L4–L5 level, the authors proposed that 25.2 percent or approximately one-fourth of the adult patients do not have accessible oblique corridor at this level. This group of patients in their study either had an absent bare window or high rising psoas major as the reason for inaccessible bare window interval at L4–L5 level [18]. Prior study by Louie et al. based on MRI evaluation of psoas muscle morphology at L4–L5 level raised concerns regarding the presence of tear drop morphology synonymous with high rising psoas which may increase the risk of neurovascular injury during direct and oblique lateral lumbar spine approaches, and proposed for considering alternate approach in such cases [19]. Another recent MRI-based study by Wang et al. analysed the anatomical relationship between left psoas major and the aorta or left common iliac artery concerning OLIF working corridor and proposed a classification system for their assessment. They proposed that cases in whom location of the left psoas major and left common iliac artery at L4–L5 level lie in zone AL, OLIF should be avoided in view of the high risk of vascular injury. The zone AL corresponded to the front tangential line for left psoas major lying in zone A as per Moro classification and left tangential line to left iliac artery lying lateral to left border of intervertebral disc [20, 21]. Based on our measurement method, we were unable to measure bare window interval in thirty cases (9.77%) at L4–L5 level in our study. The reasons responsible were similar to those proposed by prior studies: disturbed psoas anatomy (high rising psoas major) seen in nineteen cases (6.19%) or an abnormal laterally positioned iliac vessels present in eleven cases (3.58%). In total 17.9% of patients belonging to our study did not have accessible bare window interval at L4–L5 level.
On the basis of their study, Ng et al. have recently proposed a new grading system (grade 0–3) for the assessment of bare window interval size concerning OLIF approach. According to them, it will provide a better objective description of bare window size and help in assessing the feasibility of the OLIF approach. They suggested that grade 1 bare window size (≤ 1 cm) is not an absolute contraindication for OLIF technique but requires surgeon expertise in mobilizing psoas muscle for adequate disc space exposure and proper cage insertion [18]. We support their thought that surgeons who are beginning to attempt this technique should consider alternative approaches in such cases. In our study population the mean bare window size was > 1 cm at L2–L3 and L3–L4 levels, irrespective of age and sex. At L4–L5 level, the mean bare window was > 1 cm in > 60 year age group only, whereas < 1 cm in both 40–60 and < 40 year age groups.
The evaluation of psoas major window and psoas major width size have a role in assessing the ease or difficulty which a surgeon can face while retracting it during the OLIF procedure. The results of our study showed significant differences in psoas major width between each level, largest at L4–L5 level followed by L3–4 and L2–L3 level. On comparing sex differences, men had significantly wider psoas than women at each level. The existing studies by Chen et al. and Liu et al. also highlighted similar results pattern regarding psoas window and psoas major width size at each lumbar level [7, 9]. Following an overall comparative assessment of our study results with prior published studies in the existing literature, we thus propose regarding the feasibility of OLIF approach at L2–L3 and L3–L4 levels in the Indian population irrespective of age and gender. At L4–L5 level this technique may be better suited for the elderly Indian population. The results of present MRI-based morphometric study can be combined with future clinical based studies in the Indian population to further verify our results, which will be our further research goal.
The present study has its own limitations. There may be some element of error in measuring the anatomic parameters concerning the OLIF technique. Although we selected an overall large sample size for the present study, subcategory analysis regarding different age groups may be underpowered because of the smaller sample size concerning certain age groups within the study population. In our study, we did not evaluate parameters like height, weight or body mass index which may have an influence on the size of operative windows concerning the OLIF technique. The present study data was mainly of patients from northern India, which may not represent full spectrum of India’s ethnic diversity. However, despite these limitations, this is the first morphometric study concerning this novel technique in the Indian population.
Conclusion
To the best of our knowledge, this is the first known anatomical study concerning novel OLIF technique in the Indian population. The OLIF technique is well suited for lumbar interbody fusion at L2–L3 and L3–L4 level in the Indian population irrespective of age and sex. At L4–L5 level, overall 17.9 percent of the study population were unsuitable for this technique due to inaccessible bare window. In our opinion, this level may be better suited for OLIF approach in the elderly Indian population, especially for surgeons who are beginning to attempt this technique in their surgical practice. Preoperative MRI assessment for the OLIF is important to assess its feasibility, as there exists significant age and gender differences in the Indian population for anatomic parameters concerning OLIF operative windows from L2–L3 to L4–L5 levels.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We thank Dr Preethi Selvaraj, MD, for her assistance with the statistical analysis of our data.
Funding
Nil.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Approval of ethical committee at our institute was obtained prior to the study [Approval number: SU/SMS&R/76-A/2020/16].
Informed consent
As it was a retrospective study, it was not possible to obtain informed consent. Image data which was used for the publication was anonymized. Hence the waiver for informed consent concerning the present retrospective study was taken from our institute ethical committee.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP LLIF and ALIF. Journal of Spine Surgery. 2015;1(1):2–18. doi: 10.3978/j.issn.2414-469X.2015.10.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Xu DS, Walker CT, Godzik J, Turner JD, Smith W, Uribe JS. Minimally invasive anterior, lateral, and oblique lumbar interbody fusion: a literature review. Annals of Translational Medicine. 2018;6(6):104. doi: 10.21037/atm.2018.03.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hah R, Kang P. Lateral and oblique lumbar interbody fusion—current concepts and a review of recent literature. Current Reviews in Musculoskeletal Medicine. 2019;12:305–310. doi: 10.1007/s12178-019-09562-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mayer HM. A new microsurgical technique for minimally invasive anterior lumbar interbody fusion. Spine (Phila Pa 1976) 1997;22:691–699. doi: 10.1097/00007632-199703150-00023. [DOI] [PubMed] [Google Scholar]
- 5.Silvestre C, Mac-Thiong JM, Hilmi R, Roussouly P. Complications and morbidities of mini-open anterior retroperitoneal lumbar interbody fusion: oblique lumbar interbody fusion in 179 patients. Asian Spine Journal. 2012;6(2):89–97. doi: 10.4184/asj.2012.6.2.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Phan K, Maharaj M, Aseem Y, Mobbs RJ. Review of early clinical results and complications associated with oblique lumbar interbody fusion (OLIF) Journal of Clinical Neuroscience. 2016;31:23–29. doi: 10.1016/j.jocn.2016.02.030. [DOI] [PubMed] [Google Scholar]
- 7.Chen X, Chen J, Zhang F. Imaging anatomic research of oblique lumbar interbody fusion in a Chinese population based on magnetic resonance. World Neurosurgery. 2019;128:e51–e58. doi: 10.1016/j.wneu.2019.03.244. [DOI] [PubMed] [Google Scholar]
- 8.Davis TT, Hynes RA, Fung DA, Spann SW, MacMillan M, Kwon B. Retroperitoneal oblique corridor to the L2–S1 intervertebral discs in the lateral position: an anatomic study. Journal of Neurosurgery: Spine. 2014;21:785–793. doi: 10.3171/2014.7.SPINE13564. [DOI] [PubMed] [Google Scholar]
- 9.Liu L, Liang Y, Zhang H, Wang H, Guo C, Pu X, et al. Imaging anatomical research on the operative windows of oblique lumbar interbody fusion. PLoS ONE. 2016;11(9):e0163452. doi: 10.1371/journal.pone.0163452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Molinares DM, Davis TT, Fung DA. Retroperitoneal oblique corridor to the L2–S1 intervertebral discs: an MRI study. Journal of Neurosurgery: Spine. 2016;24(2):248–255. doi: 10.3171/2015.3.SPINE13976. [DOI] [PubMed] [Google Scholar]
- 11.Li JXL, Mobbs RJ, Phan K. Morphometric MRI imaging study of the corridor for the oblique lumbar interbody fusion technique at L1–L5. World Neurosurgery. 2018;111:e678–e685. doi: 10.1016/j.wneu.2017.12.136. [DOI] [PubMed] [Google Scholar]
- 12.Boghani Z, Steele W, III, Barber SM, Lee JL, Sokunbi O, Blacklock JB, et al. Variability in the size of the retroperitoneal oblique corridor: a magnetic resonance imaging-based analysis. Surgical Neurology International. 2020;28(11):54. doi: 10.25259/SNI_438_2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li R, Li X, Zhou H, Jiang W. Development and application of oblique lumbar interbody fusion. Orthopaedic Surgery. 2020;12(2):355–365. doi: 10.1111/os.12625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Olvera JQ, Lin GX, Jo HJ, Kim JS. Complications on minimally invasive oblique lumbar interbody fusion at L2–L5 levels: a review of the literature and surgical strategies. Annals of Translational Medicine. 2018;6(6):101. doi: 10.21037/atm.2018.01.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Acharya S, Dorje T, Srivastava A. Lower dorsal and lumbar pedicle morphometry in indian population: a study of four hundred fifty vertebrae. Spine (Phila Pa 1976) 2010;35(10):E378–E384. doi: 10.1097/BRS.0b013e3181cb7f2b. [DOI] [PubMed] [Google Scholar]
- 16.Srivastava A, Nanda G, Mahajan R, Nanda A, Batra S, Mishra N, et al. Feasibility of sub-axial cervical laminar screws, including C7, in the Indian population: a study on 50 patients using computed tomography-based morphometry measurements. Asian Spine Journal. 2019;13(1):7–12. doi: 10.31616/asj.2018.0110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang F, Xu H, Yin B, Tao H, Yang S, Sun C, et al. Does right lateral decubitus position change retroperitoneal oblique corridor? A radiographic evaluation from L1 to L5. European Spine Journal. 2017;26(3):646–650. doi: 10.1007/s00586-016-4645-7. [DOI] [PubMed] [Google Scholar]
- 18.Ng JPH, Perumal AKK, Tandon AA, Oh JYL. The oblique corridor at L4–L5: a radiographic-anatomical study into the feasibility for lateral interbody fusion. Spine (Phila Pa 1976) 2020;45(10):E552–E559. doi: 10.1097/BRS.0000000000003346. [DOI] [PubMed] [Google Scholar]
- 19.Louie PK, Narain AS, Hijji FY, Yacob A, Yom KA, Phillips FM, et al. radiographic analysis of psoas morphology and its association with neurovascular structures at L4–5 with reference to lateral approaches. Spine (Phila Pa 1976) 2017;42(24):E1386–E1392. doi: 10.1097/BRS.0000000000002303. [DOI] [PubMed] [Google Scholar]
- 20.Wang Z, Liu L, Xu XH, Cao MD, Lu H, Zhang KB. The OLIF working corridor based on magnetic resonance imaging: a retrospective research. Journal of Orthopaedic Surgery and Research. 2020;15(1):141. doi: 10.1186/s13018-020-01654-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moro T, Kikuchi S, Konno S, Yaginuma H. An anatomic study of the lumbar plexus with respect to retroperitoneal endoscopic surgery. Spine (Phila Pa 1976) 2003;28(5):423–428. doi: 10.1097/01.BRS.0000049226.87064.3B. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.