Abstract
Background
Computer-assisted navigation system is well-known orthopaedic advancement which allow surgeon to obtain a real-time feedback during surgeries, thus helps to reduce intraoperative errors. Currently used navigation systems are tracker based, invasive and non-universal. Therefore this study was conducted to test novel tracker-less, image-based, non-invasive, universal, real-time navigation system to predict future position of the guide wire, K wire, screws and plates in orthopaedic trauma surgeries.
Methods
Firstly, the software was tested and validated on bone model. Then utilized for non-randomised comparative study conducted on 81 adult patients with stable intertrochanteric fracture treated by dynamic hip screw and barrel plate fixation. In one group, C-arm was used and in other, software navigation was used in addition to C-arm. Parameters such as time to insertion, number of C-arm shoots and number of attempts for guide wire insertion were documented and compared.
Results
Use of the navigation software for guide wire positioning in bone models and in the DHS barrel plate surgery proved to be significantly beneficial as compared to not using navigation.
Conclusion
Intraoperative use of this new navigation system eliminates trial and error improving accuracy and reducing the operative time and radiation exposure. Thus this novel trackerless, C-arm image-based navigation system have potential to replace existing tracker-based navigation systems because of its universal nature, noninvasive and more effective properties.
Keywords: Navigation, Novel, C-arm, Computer assisted, Tracker-less, Trauma
Introduction
Currently, orthopaedic is in the era of innovations and evolution. Advance researches in orthopaedic develops new effective techniques which improve the intraoperative precisions, ultimately yielding better results. One of these innovations in orthopaedic is the use of computer assisted navigation systems in planning and carrying out various orthopaedic procedure.
Computer-assisted navigation was first introduced in spine surgery for pedicle screw placement in the year 1998. Since then, it gained wide acceptance among orthopaedic surgeons for various procedures like reconstructive hip and knee surgery, sports injury, trauma, spine and tumour surgery. It allows the surgeons to obtain real-time feedback which can be used to modify the operating technique, thus decreasing the intraoperative errors and improving overall surgical result [1].
Computer-assisted navigation systems can be active or passive [2]. Active navigation prevents the surgeon from moving beyond predetermined safe zones. Passive navigation is used intra-operatively. It display images on a monitor, with the help of which the operating surgeon can modify their decisions in more precise manner.
Computer-assisted navigation systems are further classified on the basis of reference used such as computed tomography-based navigation systems, fluoroscopy-based navigation systems and imageless tracker-based navigation systems in which there is no radiation exposure [2].
In spite of many advances, the currently used navigation systems suffer from serious drawbacks. Many studies have shown improved accuracy and better postoperative image using navigation techniques, but clinically the results were almost same when compared with old conventional technique [3].
Excessive radiation in 3D-image intensifier, its invasive nature (due to the need to drill pins in bones) and its non-universal nature (not useful for all fractures, bones and implants) are additional drawbacks of the current computer navigation systems observed in day to day practice [4].
Also, instruments and systems are not cross compatible. For example Stryker (Stryker ADAPT, a computer-assisted navigation Adaptive Positioning Technology for Gamma 3) navigation system used for positioning of head screw in proximal femoral nailing is compatible only with the company’s own nail. Smith and Nephew system (TRIGEN SURESHOT Distal Targeting System) used for distal interlocking works only for the company’s nail (author’s disclosure at the end).
Keeping these drawbacks in mind and as per recommendations in the literature [4], a passive type fluoroscopy-based navigation system was developed called “System for accurate guide wire and implant positioning”. This system is based on intra-operative C-arm or X-ray images. It is a trackerless, non-invasive and universal system that can be used for all fracture and for all bones and also it is compatible with implants of various manufacturers.
Currently, navigation systems are used for the insertion of pedicle screws in the lumbar spine (its first use), distal locking of the intramedullary nail, femur neck fracture fixation with screws, iliac wing and sacroiliac joint screw fixation, acetabulum fracture fixation, proximal tibia or humerus fracture fixation [5].
Intertrochanteric femur fracture is one of the commonest fractures happening in young and geriatric population. During treatment of such stable intertrochanteric fractures using dynamic hip screw with barrel plate, optimum positioning of lag screw is of utmost important, which is considered as slightly superior in anterioposterior view and central in lateral view, which if not achieved properly increases the chances of screw cut out significantly [6].
Lots of research has happened over various aspects to improve the results of DHS for IT fracture fixation but none of the study describes use of navigation in it which can help to guide and modify the techniques intra-operatively and improve the results postoperatively.
Thus, this pilot study was carried out using new trackerless image-based universal navigation system in case of Dynamic hip screw with barrel plate fixation for stable IT fractures.
It was expected that intraoperative use of this new navigation tool can help to reduce radiation exposure to patient and surgeon, eliminate trial and error, improve accuracy, reduce surgical time and complication rates.
Functioning of Trackerless Navigation System
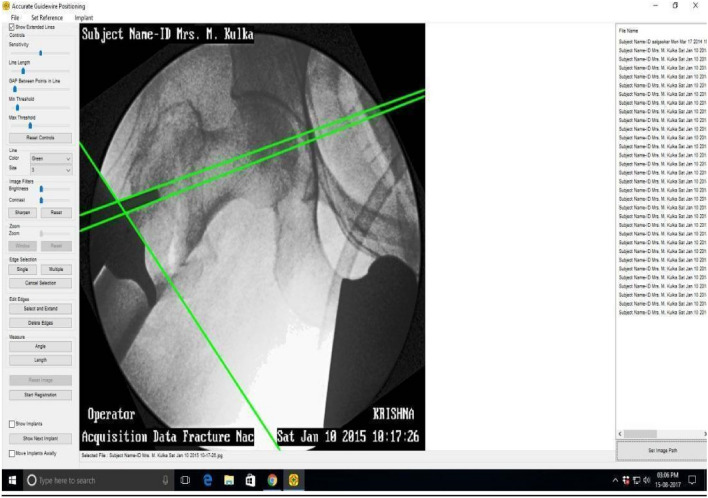
Software imaging and image manipulation is the heart of this system. For example, for an intertrochanteric femur fracture, the C-arm or X-ray image is captured. The software then performs the image processing. It then predicts and displays future position of the guide wire inside the bone on a separate monitor without driving the actual wire inside the bone. (Fig. 1).
Fig. 1.
Software displaying (predicting) future position of the guide wire
Based on this, the surgeon can adjust the position of the guide wire outside the bone itself, so that when the actual guide wire is driven in, it will assume the ideal position.
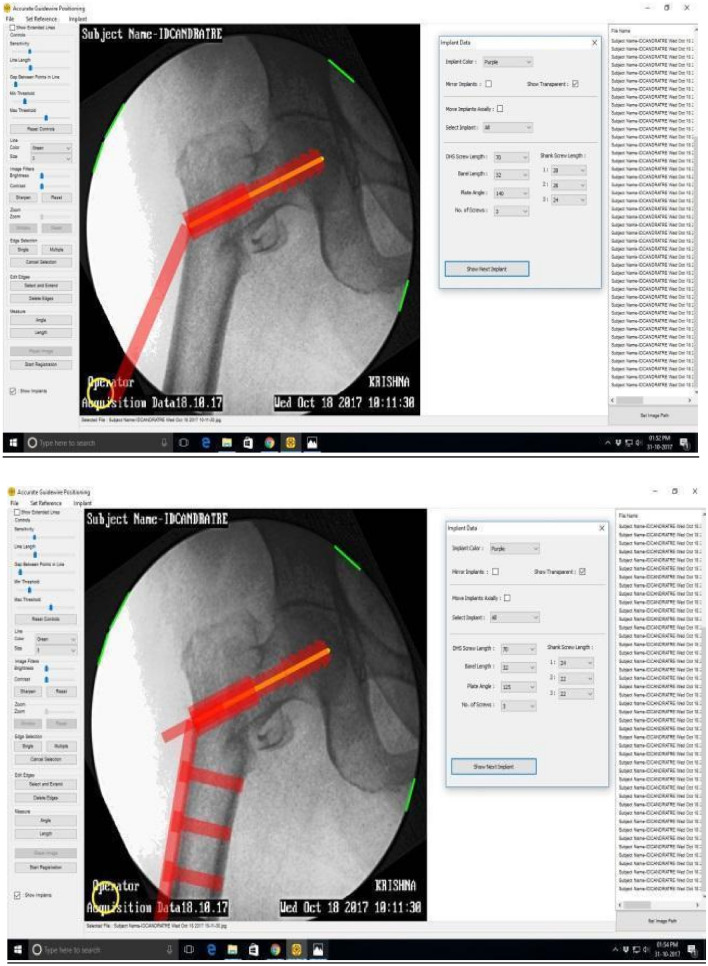
The software then superimposes virtual dynamic hip screw on the future guide wire position. Similarly, other implants like the barrel plate and cortex screws are suitably superimposed and displayed. (Fig. 2).
Fig. 2.
Virtual implant superimposition and templating of DHS barrel plate
Thus, the surgeon is able to visualize the future position of implants inside the bone even before actual guide wire is inserted.
By use of an appropriate scaling method, the software also helps to predict various parameters of the implants like screw length, number of screws required, and appropriate plate angle.
Material and Methods
Part 1
As it was the new software system-based study and as per literature guidelines [4], it was mandatory to test and validate this system in laboratory before using it on the patients. Therefore, initially, the system was tested and validated on plastic femur heads, tibia and humerus bone models in the operation theatre environment. Guide wires were passed in bone models in the operation theatre under C-arm control with and without the use of navigation system.
First, Benchmark was established by inserting the guide wire without the use of navigation software and parameters were noted. For benchmarking, a total of three models were used, one each for the femur, tibia and humerus.
Then the guide wires were inserted using the navigation software and the results of it were compared to the benchmark parameters. For navigation-assisted guide wire insertion, a total of 26 models were used: 20 for the femur, 3 for the tibia and 3 for the humerus.
The percentage error between the predicted guide wire position and actual guide wire position was also calculated in bone models by superimposing two images of predicted guide wire position and actual guide wire position using the adobe Photoshop software version CC 2018 (19.1.7) which was freely available on internet. Measurements were taken in both AP and lateral view C-arm images. The maximum difference (in mm) between the predicted guide wire position and actual guide wire position were expressed as percentage of maximum bone width.
Part 2
After testing and validating the software system on bone models the software was utilized on adult patients with stable intertrochanteric fracture who were to be fixed with DHS and barrel plate.
This non-randomised comparative study was carried out on adult patients aged 20 years or above with stable intertrochanteric fracture (Boyd and Griffin type 1 or 2). High-risk individuals, patients with polytrauma, unstable intertrochanteric fractures, compound fracture and medically unfit patients were excluded.
Intraoperative C-arm monitoring was used in all patients. Navigation software was used in patients depending upon the availability of compatible C-arm in addition to C-arm monitoring.
Thus, there were two groups: one in which only C-arm was used and the other, in which navigation was used in addition to the C-arm.
The following data were collected for each surgery:
Number of attempts for guide wire positioning
Radiation exposure as measured by number of C-arm shoots for guide wire positioning
Time required in minutes for guide wire positioning
We included 81 patients and navigation was used in 24 patients. Use of the software or not was left over to surgeons preference.
Approval of Institutional Ethics Committee was obtained. Patient consent was waived by the Ethics Committee as the study was considered to carry minimal or no risk there being no intervention, but only image manipulation and visual feedback.
Results
In the bone models, the values obtained using navigation system with regards to number of C-arm shoots, time and number of attempts taken for ideal guide wire positioning are significantly better when compared with non-navigated benchmark values as represented in Table 1.
Table 1.
Results of guide wire insertion in bone models with and without navigation
| Bone model | Total time required (mins) | Reduction in time required (%) | Total number of shoots | Reduction in number of shoots (%) | Total number of attempts | Reduction in number of attempts (%) |
|---|---|---|---|---|---|---|
| Femur | ||||||
| Benchmark | 17 | 65 | 4 | |||
| Navigation | ||||||
| 1 | 6.42 | 62.23 | 18 | 72.3 | 3 | 25 |
| 2 | 7.5 | 55.88 | 17 | 73.84 | 4 | 0 |
| 3 | 2.45 | 85.58 | 16 | 75.38 | 1 | 75 |
| 4 | 6.1 | 64.11 | 16 | 75.38 | 2 | 50 |
| 5 | 5.5 | 67.64 | 12 | 81.53 | 2 | 50 |
| 6 | 6.09 | 64.17 | 15 | 76.92 | 3 | 25 |
| 7 | 5 | 70.59 | 15 | 76.92 | 1 | 75 |
| 8 | 7.2 | 57.65 | 21 | 67.69 | 1 | 75 |
| 9 | 4.83 | 71.59 | 13 | 80 | 1 | 75 |
| 10 | 6.83 | 59.82 | 21 | 67.69 | 2 | 50 |
| 11 | 5.22 | 69.29 | 23 | 64.62 | 3 | 25 |
| 12 | 4.86 | 71.41 | 18 | 72.31 | 3 | 25 |
| 13 | 3.02 | 82.24 | 5 | 92.31 | 1 | 75 |
| 14 | 4.46 | 73.76 | 15 | 76.92 | 3 | 25 |
| 15 | 3.4 | 80 | 8 | 87.69 | 1 | 75 |
| 16 | 7.39 | 56.53 | 14 | 78.46 | 2 | 50 |
| 17 | 5.2 | 69.41 | 17 | 73.85 | 2 | 50 |
| 18 | 7.6 | 55.29 | 19 | 70.77 | 2 | 50 |
| 19 | 5.2 | 69.41 | 15 | 76.92 | 1 | 75 |
| 20 | 7.2 | 57.65 | 20 | 69.23 | 1 | 75 |
| Tibia | ||||||
| Benchmark | 9 | 11 | 3 | |||
| Navigation | ||||||
| 1 | 5.2 | 42.22 | 3 | 72.72 | 3 | 0 |
| 2 | 1 | 72.88 | 3 | 72.73 | 1 | 66.67 |
| 3 | 0.5 | 85.47 | 2 | 81.82 | 1 | 66.67 |
| Humerus | ||||||
| Benchmark | 4.13 | 6 | 6 | |||
| Navigation | ||||||
| 1 | 1 | 75.78 | 2 | 66.66 | 1 | 83.33 |
| 2 | 1.12 | 72.88 | 2 | 66.67 | 2 | 66.67 |
| 3 | 0.6 | 85.47 | 1 | 83.33 | 1 | 83.33 |
When various parameters like percentage reduction in time, number of shoots, number of attempts, percentage errors in AP and Lateral view were studied in the bone models, the use of navigation demonstrated favourable reductions in all of them as represented in Table 2. Thus navigated system helped in getting more precision and accuracy in bone models.
Table 2.
Percentage comparison of navigated values with benchmark values in bone models
| Percentage reduction in time | Percentage reduction in number of shoots | Percentage reduction in number of attempts | Percentage error (antero-posterior view) | Percentage error (lateral view) |
|---|---|---|---|---|
| 68.42 | 75.17 | 53.52 | 2.53 | 2.49 |
After validating the software in bone models, it was used to compare the results between two study groups of patients, we found that the mean number of attempts required for guide-wire insertion was significantly less when navigation was used as compared to when navigation was not used (3 ± 1.7 Vs. 5.3 ± 2.1, respectively, p = 0.014). Similarly, when navigation was used, it was found that the mean duration (in minutes) required for guide-wire insertion was significantly less as compared to when navigation was not used (9.9 ± 6.5 min Vs. 19.63 ± 10 min respectively, p = 0.019). The number of shoots required was also lesser when navigation was used, but this difference was not statistically significant (20.9 ± 9.5 Vs. 37.8 ± 23.2, respectively, p = 0.059) (Table 3).
Table 3.
Comparison of the various outcome measures between the two groups
| Outcome measure | Navigation used (n = 24) Mean ± SD | Navigation not used (n = 57) Mean ± SD | p value |
|---|---|---|---|
| No. of guide-wire insertion attempts | 3 ± 1.7 | 5.3 ± 2.1 | 0.014 |
| Time for guide-wire insertion (min) | 9.9 ± 6.5 | 19.63 ± 10 | 0.019 |
| Radiation exposure (no. of shoots) | 20.9 ± 9.5 | 37.8 ± 23.2 | 0.059 |
Discussion
Computer-assisted navigation system has been playing an important role in orthopaedics and traumatology since the last two decades. Although Navigation systems continue to evolve and improve, the currently used systems are not devoid of drawbacks.
In a review article by Mavrogenis et al. [1], they stated that currently used navigation systems are still in their infancy with the drawbacks of increase of operative time for arrangement of set up, high learning curve, risk of fractures (which is now minimized, but not eliminated, due to smaller pins), an inherent error of 0.1 to 1 mm in the tracking system of navigation markers, lack of improvement in clinical outcomes.
Zheng and Nolte [4] also concluded that even after about two decades since the introduction of the first robot and navigation systems for Computer-Assisted Orthopaedic Surgery (CAOS), it is still at the beginning of a rapid process of evolution. There is a need to eliminate the drawbacks of the currently available optical tracking systems and to stimulate the development of non-invasive registration methods and referencing tools. All the new techniques and devices will need to be carefully evaluated first in a laboratory setting and then clinically. More prospective and retrospective studies comparing the outcome of CAOS versus non-CAOS procedures with long follow-up time will have to be conducted.
In the study, conducted to fix the trochanteric fractures with gamma nail [7], significant improvement were found in parameters of surgical time, wound size, number of X-ray shoots and accuracy of implant placement using navigation system. Similarly, a study on navigated sub-capital fracture fixation allowed improved screw positioning and reduced radiation to both the surgeon and the patient [8].These results are more or less comparable to our study.
In our study, when percentage error between the predicted guide wire position and actual guide wire position was calculated, the error was found to be less than 4% in almost all cases of bone models. The tracking system of commercially available navigation markers has an inherent error of 0.1 to 1 mm for each of the three coordinates in space [2]. In our tests, the deviation in mm ranged from a minimum of 0 to a maximum of 2.8 mm in one plane (with an average of 1.31 mm).
In today’s practice, existing computer navigation systems also have drawbacks of morbidity such as fractures and infections due to the placement of bony reference arrays [10], or have excessive radiation exposure [9] and are non-universal [9]. The new navigation software which we used in our study is non-invasive, universal and its working is based as add-on to the C-arm images without actually replacing it.
Our study has demonstrated that the use of this new navigation software has significantly improved the parameters, namely, the time required for guide wire insertion, the number of C-arm shoots and the number of attempts ultimately reducing the radiation exposure to both patients and surgeons.
This same navigation system can be used for other surgeries as well, for example, distal end radius K-wire fixation/plate fixation, proximal femoral nailing, radius ulna shaft plate fixation and proximal humerus plate fixation. The software detects the position of guide wire (or sleeve) on C arm image while its end is touching the bone surface (not driven in) by edge detection and further image manipulation described earlier is effected. This universal nature, compatibility with various implants of different manufacturers and ability to be used in many trauma surgeries makes this new trackerless navigation system more handy and useful. The software is simple to use and does not require any specific learning curve, just understanding of the basic procedure, and basic knowledge of the computer is enough for its use even by young and experienced trauma surgeons.
Limitations
It is a non-randomized study conducted on small sample size.
Only two fracture types were considered (though, among the most common ones).
Conclusion
The use of trackerless navigation system proved to be beneficial when compared to the fixation done without navigation in various aspects. The universal nature of this new software makes it compatible to be used for various trauma surgeries with implant of different manufacturers. The non-invasive nature of this software also helps to prevent the complications of previously used systems.
Thus we conclude that, this tracker-less, image-based navigation system is a handy tool to improve precision and results both intra and postoperatively. Also it does have a potential to replace existing tracker-based navigation systems.
Further long-term multi-centric studies on a larger number of patients and in other fracture types are required to conclusively prove its benefit.
Acknowledgements
Author has received grant from Government of India for development of the navigation software. The validity of software has been confirmed first in laboratory setting on bone models before testing it on patients.
Abbreviations
- AP
Anterioposterior
- CAOS
Computer-Assisted Orthopaedic Surgery
- IT
Inter-trochanteric
- DHS
Dynamic Hip Screw
- 3D
3 Dimension
Author Contribution
Conception of work, NG and VP, acquisition of data NG and VP, data analysis and interpretation NG. Drafting of manuscript NG and VP. Critical revision of articles NG and VP, final approval of the versions to be published NG and VP.
Declarations
Conflict of interest
Author has received grant from Government of India for development of the navigation software.
Ethical approval
Studies have been approved by the appropriate ethical committee and have been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki. Patient consent was waived by the Ethics Committee as the study was considered to carry minimal or no risk there being no intervention, but only image manipulation and visual feedback. Manuscript has been read and approved by all the authors and represent our original work which has not been published anywhere or under consideration.
Contributor Information
Nishant D. Goyal, Email: nishantdgoyal@gmail.com
Vijay M. Panchnadikar, Email: vmpsanjeevan@gmail.com
References
- 1.Mavrogenis AF, Mimidis G, Koulalis D, Papagelopoulos PJ. Computer-assisted navigation in orthopaedics. OA Orthopaedics. 2014;2(1):8. doi: 10.3928/01477447-20130724-10. [DOI] [PubMed] [Google Scholar]
- 2.Bae DK, Song SJ. Computer assisted navigation in knee arthroplasty. Clinics in Orthopedic Surgery. 2011;3(4):259–267. doi: 10.4055/cios.2011.3.4.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Desai AS, Dramis A, Kendoff D, Board TN. Critical review of the current practice for computer assisted navigation in total knee replacement surgery: cost effectiveness and clinical outcome. Current Reviews in Musculoskeletal Medicine. 2011;4(1):11–15. doi: 10.1007/s12178-011-9071-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zheng G, Nolte L. Computer-assisted orthopedic surgery: current state and future perspective. Frontiers in Surgery. 2015 doi: 10.3389/fsurg.2015.00066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leung KS, Tang N, Cheung LW, Ng E. Image guided navigation in orthopaedic trauma. Journal of Bone and Joint Surgery. British Volume. 2010;2:1332–1337. doi: 10.1302/0301-620X.92B10.24594. [DOI] [PubMed] [Google Scholar]
- 6.Caruso G, Bonomo M, Valpiani G, Salvatori G, Gildone A, Lorusso V, Massari L. A six-year retrospective analysis of cut-out risk predictors in cephalomedullary nailing for pertrochanteric fractures. Bone and Joint Research. 2017;6(8):481–488. doi: 10.1302/2046-3758.68.BJR-2016-0299.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leung KS, Yung SH, Tang N, Kwok KO, Yue W. Clinical experience of Gamma nail-ing with fluoro-navigation. In: Langlotz F, Davis BL, Bauer A, editors. Procs 3rd Annual Meeting CAOS - International Proceedings. Darmstaft: Steinkopff; 2003. pp. 206–207. [Google Scholar]
- 8.Ilsar, I., Weil, Y., Mosheiff, R., Peyser, A., & Liebergall, M. Navigation-assisted cannulated hip screw insertion – the Hadassah experience Orthopaedic Proceedings 2006 88-B:SUPP_II, 338–338
- 9.Dabaghi Richerand A, Christodoulou E, Li Y, et al. Comparison of effective dose of radiation during pedicle screw placement using intraoperative computed tomography navigation versus fluoroscopy in children with spinal deformities. Journal of Pediatric Orthopedics. 2016;36:530–533. doi: 10.1097/BPO.0000000000000493. [DOI] [PubMed] [Google Scholar]
- 10.Koenen P, Schneider MM, Pfeiffer TR, Bouillon B, Bäthis H. “The impact of pinless navigation in conventionally aligned total knee arthroplasty. Advances in Orthopedics. 2018;2018:1–6. doi: 10.1155/2018/5042536. [DOI] [PMC free article] [PubMed] [Google Scholar]