Abstract
Background
Intramedullary nailing is the most preferred fixation method for diaphyseal radius and ulna fractures in the young age group. The aim of this study was to compare the dorsal and lateral entry points in the context of entry site-related complications, fracture union and functional results.
Methods
This retrospective comparative study included pediatric patients who underwent surgery for isolated diaphyseal radius or both bone forearm fractures with intramedullary nailing using Kirschner wire between January 2013 and January 2019. K-wire was introduced from the distal radius through dorsal entry (Group A) in 19 patients and lateral entry (Group B) in 18 patients. The mean follow-up was 37 months. Complications were noted and functional outcomes were evaluated according to the CHOP criteria.
Results
All fractures were healed. The functional results were determined to be excellent for 30, fair for 4, and poor for 3 patients. The overall complication rate was 18.9%, including distal radius fracture, mild pain in the wrist, and minor loss in ROM. No statistically significant differences were determined between the groups in respect of functional results and complication rates.
Conclusion
Good functional results and similar complication rates can be obtained with both dorsal and lateral entry approaches. Stainless steel K-wire is an inexpensive intramedullary fixation implant option, which provides strong stabilization. Distal radius fracture is a newly reported complication for forearm intramedullary nailing. Leaving the implant out of the skin seems safe with the benefit of avoiding a further surgical intervention to extract the implant.
Keywords: Pediatric forearm fractures, Intramedullary nailing, Dorsal or lateral approach
Introduction
Diaphyseal radius and ulna fractures, which are common in childhood and adolescence, can usually be successfully treated with closed reduction and casting [1]. Open fractures, skeletally mature patients, inadequate reduction of fracture, associated ipsilateral humeral fracture, neurovascular injury and unacceptable displacement during follow-up after conservative treatment are commonly accepted surgical indications [2].
Intramedullary nailing (IMN) is the most preferred fixation method for diaphyseal radius and ulna fractures in the young age group, allowing minimally invasive treatment of these fractures with great success [2, 3]. However, complications are still reported for surgical treatment of pediatric forearm fractures with IMN [4–6].
The preferred entry points for radius IMN are dorsally near Lister tubercle and directly lateral of distal radius. Good results have been reported for both entry points separately, although there are not sufficient data to guide surgeons in the choice of which one of these entry points to use [5, 7–9].
To the best of our knowledge, there has been no previously published study which has compared the results of pediatric forearm fractures treated with IMN according to the entry points. The aim of this study was to compare the two entry points in respect of entry site-related complications, fracture union, and functional results.
Patients and Methods
This retrospective study was approved by the Local Ethics Committee. The orthopedic trauma registry of a level 1 trauma center was searched for pediatric and adolescent patients who underwent surgery for isolated diaphyseal radius or both bone forearm fractures between January 2013 and January 2019. The inclusion criteria were as follows:
Patients who
had sustained a traumatic isolated diaphyseal radius or both bone forearm fracture,
underwent surgery with IMN,
age < 14 years, and
were followed up for at least 12 months after surgery.
Exclusion criteria were pathological fractures, previous fracture and surgery of the involved bone and the use of extramedullary implants for internal fixation.
In the specified time period, a total of 52 patients were identified who had been treated surgically for a traumatic isolated diaphyseal radius or both bone forearm fracture. After exclusion of 15 patients, the study was completed with the remaining 37 patients (Fig. 1), comprising 30 males and 7 females with an average age at the time of surgery of 10.5 years. Patient files were examined in terms of age, injury mechanism, additional fractures, presence of any open fracture or neurovascular injury, fracture side and the surgical approaches. For patients who required a change of implant choice because of a complication, initial choice for entry point was taken into account.
Fig. 1.
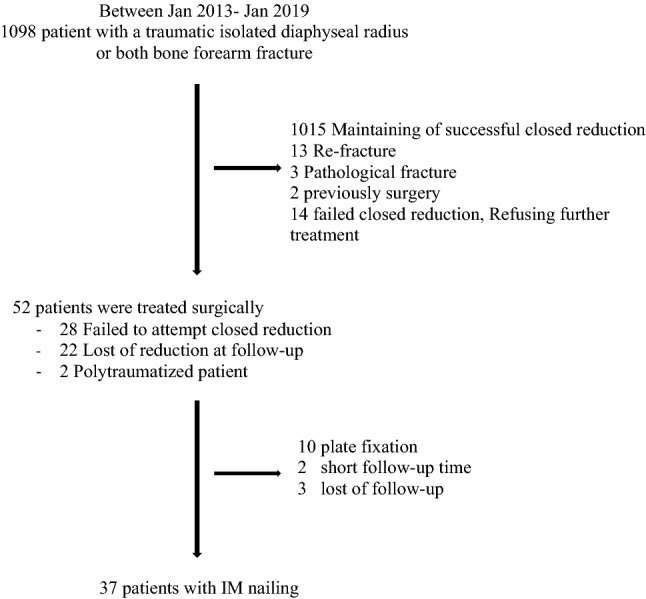
Flowchart showing the inclusion of patients
Preoperative Evaluation
All patients were evaluated initially in the Emergency Room. Physical examinations including neurovascular examination were performed. Appropriate conventional antero-posterior (AP) and lateral radiographs were obtained for all patients. Closed reduction and long-arm casting under sedation was attempted for all patients as initial treatment. The reduction was evaluated again with AP and lateral radiographs.
Failed closed reduction was accepted as > 15° angulation in any plane for girls ≤ 8 years and boys ≤ 10 years and > 10° angulation for girls > 8 years and boys > 10 years after closed reduction and casting. Bayonet apposition > 1 cm was also accepted as surgical criteria for all age groups [2, 3].
Surgical Procedure
All surgical procedures were performed under general anesthesia and a tourniquet was prepared for all patients for use if needed. Fluoroscopy was used in all steps throughout the surgery. Mini open fracture reduction was performed after three attempts of failed closed reduction and pin passage to the proximal fragment. Closed reduction and intramedullary fixation was achieved in 16 patients, whereas a mini open approach was used for 21 patients. Stainless steel Kirschner (K) wires of different sizes (1.2–2.5 mm) were used for all patients for IMN.
The implant was introduced from the distal radius through dorsal entry (Group A) in 19 patients and lateral entry (Group B) in 18 patients. The blunt end of the pin was slightly pre-contoured for easy medullary entry. For dorsal entry, a 2 cm of longitudinal incision was made over the Lister tubercle. After protecting the extensor pollicis longus and extensor carpi radialis brevis tendons with retractors, the bone was drilled with a 2.7 mm of drill proximal to the physeal line, under fluoroscopic guidance. For radial entry, a 2 cm longitudinal incision was made over radial styloid between the 1st and 2nd extensor compartments. After dissecting and protecting the dorsal branch of the radial nerve, bone was drilled proximal to the physeal line under fluoroscopic guidance. Pin was advanced manually with a help of a hammer if needed. Pin tips were left outside the skin.
Postoperative Period
Oral antibiotics for one week were prescribed to all patients to prevent pin site infection, and the pin site dressing was changed every second day.
The mean follow-up period was 37 months (range 12–64 months). All patients were evaluated with physical examination, and AP and lateral radiographs at every follow-up visit. The first two follow-up examinations were made at 2 and 4 weeks postoperatively, then at 4-week intervals until the 3rd month and every 3 months thereafter until the end of one year. After one year, all patients were examined once a year. Changes to follow-up visit dates were made if necessary, according to the availability of patients and families.
Radiographic examination was performed at all follow-up examinations. Callus formation in at least 3 of 4 cortices on AP and lateral radiographs was accepted as union. Delayed union and nonunion were defined as fracture healing beyond 3 months and 6 months, respectively [10]. Pins were removed under local anesthesia during the same clinic visit when fracture union was recorded.
Complications were noted and functional outcome was evaluated according to the Flynn Children’s Hospital of Philadelphia (CHOP) criteria at the final follow-up examination by an examiner independent of the surgical intervention. This outcome classification is based on range of motion (ROM) and perioperative complications [8]. Functional outcomes, entry site-related complications, and time to bone union (pin removal) were compared between the two groups. Complications which were not related to the entry site, such as re-fracture, were excluded from the statistical analysis.
Statistical Analysis
Data were analyzed using NCSS (Number Cruncher Statistical System) 2007 (Kaysville, Utah, USA). For evaluation of study data descriptive statistical analysis (mean, standard deviation, median, first quartile, third quartile, frequency, percentage, minimum, maximum) were used. Relevance of qualitative data to normal distribution was tested via Shapiro–Wilk test and graphical examination. Comparison of quantitative data with normal distribution and without normal distribution between two groups was made with independent sample t-test and Mann–Whitney U test, respectively. Pearson chi-squared test, Fisher’s exact test and Fisher-Freeman-Halton test were used for comparing qualitative data. Level of significance was accepted as p < 0.05.
Results
Timing for Surgery and Postoperative Stay in Hospital
The mean time from trauma to surgery was 9.11 ± 8.33 days (range 0–31 days). There was no statistically significant difference between the groups (p = 0.55).
The mean postoperative stay in hospital was 2.81 days (range 1–8 days).
Fracture Union and Implant removal
The mean time to fracture union was 47.5 days.
Fracture union was achieved at mean 52.5 days for Group A, and at mean 42.2 days for Group B. The difference was statistically significant (p = 0.04). (Table 1).
Table 1.
Comparative statistical analyses for complications, fracture reduction, union, and functional score
| Approach | p | ||
|---|---|---|---|
| Dorsal | Lateral | ||
| Complication | |||
| (–) | 16 (84.2) | 14 (77.8) | b0.693 |
| ( +) | 3 (15.8) | 4 (22.2) | |
| Minor | 1 (5.3) | 3 (16.7) | c0.589 |
| Major | 2 (10.5) | 1 (5.6) | |
| Fracture reduction | |||
| Open | 9 (47.4) | 12 (66.7) | d0.236 |
| Close | 10 (52.6) | 6 (33.3) | |
| Fracture union (day) | 52.47 ± 16.31 | 42.17 ± 12.71 | a0.040* |
| Functional score | |||
| Poor | 2 (10.5) | 1 (5.6) | c0.589 |
| Fair | 1 (5.3) | 3 (16.7) | |
| Excellent | 16 (84.2) | 14 (77.8) | |
*p < 0.05
aIndependent sample t test
bFisher’s exact test
cFisher-Freeman-Halton exact test
dPearson χ2 test
The mean fracture union time was found 54.5, 50.2, 37.7, and 44.4 days for dorsal mini-open, dorsal closed, lateral closed, and lateral mini-open reduction subgroups, respectively.
There was no relationship between surgical delay and fracture (p = 0.694).
All implants were removed after fracture union.
Functional Assessment
According to the Forearm Fracture Fixation Outcome Classification of the Childrens Hospital of Philadelphia, 30 (81.1%) patients were classified as excellent, 4 (10.8%) patients as fair, and 3 (8.1%) patients as poor.
There was no statistically significant difference between groups (p > 0.05) (Table 1).
Complications and Unplanned Interventions
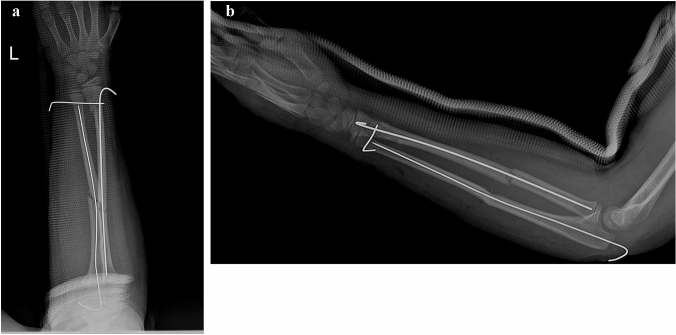
The overall complication rate was found to be 18.9% (n = 7), with minor complications at 10.8% (n = 4), and major complications of 8.1% (n = 3). Distal radius fracture occurred in two patients in Group A (Fig. 2a, b) and one patient in Group B during entry of the K-wire. There were 4 minor complications determined as mild pain in the wrist (n:3) and minor loss in range of motion (ROM) (n:1). All minor complications persisted at the final clinic visit. One patient had sustained both mild pain and minor loss in ROM during daily activities such as writing. Another patient with mild pain had also a weakness on thumb extension, during follow-up, which resolved following physiotherapy.
Fig. 2.
a, b Early postoperative AP (a) and lateral (b) view X-rays after initial operation for both bone diaphyseal forearm fracture. A distal radius fracture occurred during dorsal entry of K-wire, which was fixed through trans-ulnar K-wire
No statistically significant difference was determined between the groups according to complications (p > 0.05) (Table 2).
Table 2.
Complications for dorsal and lateral approaches
| Group A (n) | Group B (n) | |
|---|---|---|
| Major | ||
| Distal radius fracture | 2 | 1 |
| Minor | ||
| Mild pain | 1 | 2 |
| Loss at ROM | 1 | 0 |
| Pin tract infection | 0 | 0 |
| Growth disturbance | 0 | 0 |
| Delayed union/nonunion | 0 | 0 |
| EPL rupture | 0 | 0 |
There was no patient with pin tract infection even though the K-wire was left outside the skin. No growth disturbance was observed at the final follow-up examination. Re-fracture occurred in one patient due to a fall 8 months after implant removal, which was not considered to be related to the entry point.
Discussion
Diaphyseal radius fractures in the pediatric and adolescent age groups are seen as isolated or more commonly as part of a forearm fracture. Conservative treatment is preferred, while surgical interventions can be performed for open fractures, floating elbow injuries and unacceptable fracture reduction [2, 3]. At rates similar to those in literature, 1015 of 1098 (92.5%) patients admitted to our Emergency Department due to both bone or isolated radius diaphyseal fractures during the specified time period were successfully treated with conservative treatment (Fig. 1).
IMN using titanium elastic nails (TEN) through a closed or mini open approach is the most preferred fixation implant for these fractures in the pediatric age group. Similar functional results and complication rates have been reported with the use of K-wires [11]. The lower cost and higher strength could be reasons for choosing K-wire rather than TEN, especially for older children [12–14]. In the present study, K-wires were used for all patients as the internal fixation implant because of low cost and continuous availability in our public health system. While using K-wires, the biomechanical principle was not 3-point cortical contact like TEN but filling the intramedullary cavity with a relative stiff implant to prevent displacement.
In the lateral entry group, the fixation was achieved with closed maneuvers 33% of patients. We used a mini-open approach in 66% of these patients, while in the dorsal entry group, 47% of the patients needed an open reduction, which might suggest with the lateral entry point is more difficult to get a successful reduction or fixation with closed methods, even if the difference was statistically insignificant. We think that the difference for achieving closed reduction between two groups could due to different surgeons performing surgical interventions.
Dorsal and lateral entry points have been described for diaphyseal radius fractures, and overall good results have been reported for both approaches [5, 7–9]. In the current study, the functional outcome was evaluated with the CHOP classification, which is based on complications and range of motion. Similar to previous findings in literature, no statistically significant difference was determined between the two groups of the current study in respect of functional results. It has been reported that the incision made over the Lister tubercle for the dorsal approach or over the lateral cortex of the radial styloid for the lateral approach might put underlying structures at risk of iatrogenic injury [5].
IM nailing of pediatric diaphyseal radius fracture is not without problems, with reported complication rates ranging from 17 to 42% [2]. In a current systematic review of 22 published articles by Nørgaard et al. [5] minor and major complications were compared according to lateral and dorsal surgical approaches. The rates of major complications were reported as 5.6% and 8.9% and minor complications as 6.4% and 12.9% for the lateral and dorsal approach, respectively. Most common minor complication in this review was transient nerve palsy for lateral entry group and EPL compromise for dorsal entry group. The overall complication rate in the present study was 18.9%, which was similar to findings in previous studies. No statistically significant difference was determined between the surgical approaches in respect of complication rates.
Normal healing of closed pediatric forearm shaft fractures occurs at an average of 5.5 weeks [15]. Delayed union has been defined as healing exceeding 12 weeks after injury and is accepted as a minor complication, which could be seen in both dorsal and lateral approach groups [3, 5]. In the current study, all the fractures were healed at mean 47.5 days, which was within the reported time interval. The mean time for fracture healing was found to be 52.5 days and 42.2 days for the dorsal and lateral approach groups, respectively. The time to fracture union was significantly shorter in the lateral entry group. Even though, we do not think the entry point as a reason for delayed bone healing. We did not find any relation between surgical delay and fracture union groups. A faster bone consolidation was determined with closed reduction for both group. This difference may also cause by variations of follow-up visit dates, as we accepted the date of the X-ray with bone union as bone healing time.
Complications could show differences according to the approach used. In literature, extensor pollicis longus (EPL) tendon rupture has been reported in the dorsal approach at rates of up to 18% [7, 8, 16–19]. Technical errors such as inadequate visualization during insertion, a sharp cut of the nail and leaving the nail in the extensor compartment have been blamed for this complication. Prolonged irritation of the tendon by the nail could be another reason, and the mean time for diagnosis of EPL tendon rupture has been reported to be 10.4 weeks (range 2–34 weeks) [4]. In the current study, all pins were left over the skin and were removed at mean 6.7 weeks (range 4–12 weeks), which could explain the lack of EPL tendon rupture in the current study. Weakness of thumb extension was detected in one patient, who was referred to the Hand Surgery Unit. It was reported as mild tendon adhesion without rupture and followed up with physiotherapy.
To the best of our knowledge, distal radius fracture during nail insertion has been never reported in previous studies, and this was seen in two patients with the dorsal approach and in one patient with the lateral approach in the current study. As the K-wire is stiffer than a titanium elastic nail [13], the combination of this stiffness and the introduction of the K-wire close to the meta-diaphyseal junction could be the reason for distal radius fracture. Fractures during dorsal pin entry occurred because of applying extreme force for wrist flexion to introduce the inadequate contoured K-wire to the medullary canal even though the K-wire was not oversized compared to medullary canal. One of these complications was treated by adding an extra K-wire across DRUJ because the iatrogenic instability and changing the entry point to lateral, whereas the other fracture did not require a change of entry point or extra fixation. To avoid this complication, we think, drilling the bone entry, pre-contouring the implant and gentle pushing during insertion are essential points of surgical technique. There is no need to flex the wrist to make insertion easier if we pay attention to these points. The patient in Group B with fracture was a distal 1/3 diaphyseal fracture, which intramedullary fixation was not the best treatment choice. During pin insertion, the short lateral cortex was not able to resist the force of the manipulation. This patient was treated by changing the K-wire for a low-profile plate applied through a lateral approach. All three patients were followed up for mean 46 (23, 52, and 63) months and healed without any ROM limitation or wrist pain. Preoperative X-rays of these patients were re-evaluated for an overlooked occult distal radial fracture. After this re-evaluation, fractures were confirmed to be iatrogenic.
There are concerns that leaving the pins outside the skin could cause potential complications such as infection, skin irritation. However, studies have reported no significant difference in complications whether the implant is left exposed or embedded beneath the skin [20, 21]. There are also secondary benefits such as avoiding any additional surgical intervention and thereby reducing costs [21]. In the current study, no entry site infection was observed that required additional debridement or antibiotics.
Four minor complications in three patients were determined comprising mild pain in the wrist [3] and minor loss of ROM [1] all these complications persisted at the final clinic visit. Transient or permanent nerve palsy of the sensory radial branch has been reported in many studies, at rates of 2.9% and 0.3%, respectively. This complication has been reported especially with the use of the lateral approach [5]]. No palsy in the dorsal sensorial branch of the radial nerve was determined in any of the current study patients where the intramedullary implant had been introduced through the lateral approach.
This study had some limitations, primarily the low number of patients. The follow-up clinic visit times showed some variability because of the retrospective nature of the study, and although the time to union showed a statistically significant difference between the groups, this variability weakens the result. There is need for further, prospectively designed studies of larger patient populations. Also, a prospective randomized study which compare the use of stainless-steel K-wire and titanium elastic nail could give valuable information.
In conclusion, good functional results and similar complication rates can be obtained with both the dorsal and lateral entry approaches. Stainless steel K-wire is an inexpensive intramedullary fixation implant option for pediatric diaphyseal forearm fractures, which provides strong stabilization until the fracture heals. Fracture of the distal radius is a newly reported complication of the application of intramedullary nailing for pediatric forearm fractures. It is remarkable that this complication is reported with K-wire as an implant, while TEN with higher elasticity might be a better choice, especially when precise surgical tips of forearm IMN application is overlooked. Leaving the implant outside the skin seems to be safe with the benefit of avoiding further surgical intervention to extract the implant.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Compliance with Ethical Standards
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical standard statement
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed consent
For this type of study informed consent is not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Ahmet Hamdi Akgülle, Email: ahmethamdiakglle@yahoo.com.
Tolga Onay, Email: onaytolga@yahoo.com.
Servet İğrek, Email: servetigrek@gmail.com.
Mehmet Deniz Kesimer, Email: m.denizkesimer@gmail.com.
Osman Mert Topkar, Email: drmerttopkar@gmail.com.
Evrim Şirin, Email: evrimsirin@yahoo.com.
References
- 1.Zionts LE, Zalavras CG, Gerhardt MB. Closed treatment of displaced both-bone forearm fractures in older children and adolescents. Journal of Pediatric Orthopedics. 2005;25:507–512. doi: 10.1097/01.bpo.0000158005.53671.c4. [DOI] [PubMed] [Google Scholar]
- 2.Pace JL. Pediatric and adolescent forearm fractures: current controversies and treatment recommendations. Journal of American Academy of Orthopaedic Surgeons. 2016;24(11):780–788. doi: 10.5435/JAAOS-D-15-00151. [DOI] [PubMed] [Google Scholar]
- 3.Mehlman CT, Wall EJ. Diaphyseal radius and ulna fractures. In: Flynn JM, Skaggs DL, Waters PM, editors. Rockwood and Wilkins’ fractures in children. 8. Philadelphia: Wolters Kluwer; 2015. pp. 413–472. [Google Scholar]
- 4.Murphy HA, Jain VV, Parikh SN, Wall EJ, Cornwall R, Mehlman CT. Extensor tendon injury associated with dorsal entry flexible nailing of radial shaft fractures in children: a report of 5 new cases and review of the literature. Journal of Pediatric Orthopedics. 2019;39(4):163–168. doi: 10.1097/BPO.0000000000000897. [DOI] [PubMed] [Google Scholar]
- 5.Nørgaard SL, Riber SS, Danielsson FB, Pedersen NW, Viberg B. Surgical approach for elastic stable intramedullary nail in pediatric radius shaft fracture: a systematic review. Journal of Pediatric Orthopedics. Part B. 2018;27(4):309–314. doi: 10.1097/BPB.0000000000000458.Review. [DOI] [PubMed] [Google Scholar]
- 6.Fernandez FF, Langendörfer M, Wirth T, Eberhardt O. Failures and complications in intramedullary nailing of children's forearm fractures. Journal of Children's Orthopaedics. 2010;4(2):159–167. doi: 10.1007/s11832-010-0245-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smith VA, Goodman HJ, Strongwater A, Smith B. Treatment of pediatric both-bone forearm fractures: a comparison of operative techniques. Journal of Pediatric Orthopedics. 2005;25(3):309–313. doi: 10.1097/01.bpo.0000153943.45396.22. [DOI] [PubMed] [Google Scholar]
- 8.Flynn JM, Jones KJ, Garner MR, Goebel J. Eleven years experience in the operative management of pediatric forearm fractures. Journal of Pediatric Orthopedics. 2010;30(4):313–319. doi: 10.1097/BPO.0b013e3181d98f2c. [DOI] [PubMed] [Google Scholar]
- 9.Wall LB. Staying out of trouble performing intramedullary nailing of forearm fractures. Journal of Pediatric Orthopedics. 2016;36(Suppl 1):S71–S73. doi: 10.1097/BPO.0000000000000760.Review. [DOI] [PubMed] [Google Scholar]
- 10.Schmittenbecher PP, Fitze G, Gödeke J, Kraus R, Schneidmüller D. Delayed healing of forearm shaft fractures in children after intramedullary nailing. Journal of Pediatric Orthopaedics. 2008;28(3):303–306. doi: 10.1097/BPO.0b013e3181684cd6. [DOI] [PubMed] [Google Scholar]
- 11.Şahin N, Akalın Y, Türker O, Özkaya G. ESIN and K-wire fixation have similar results in pediatric both-bone diaphyseal forearm fractures. Ulus Travma Acil Cerrahi Derg. 2017;23(5):415–420. doi: 10.5505/tjtes.2017.85891. [DOI] [PubMed] [Google Scholar]
- 12.Heare A, Goral D, Belton M, Beebe C, Trizno A, Stoneback J. Intramedullary implant choice and cost in the treatment of pediatric diaphyseal forearm fractures. Journal of Orthopaedic Trauma. 2017;31(10):e334–e338. doi: 10.1097/BOT.0000000000000925. [DOI] [PubMed] [Google Scholar]
- 13.Battle J, Carmichael KD, Morris RP. Biomechanical comparison of flexible intramedullary nailing versus crossed Kirschner wire fixation in a canine model of pediatric forearm fractures. Journal of Pediatric Orthopedics. Part B. 2006;15(5):370–375. doi: 10.1097/01202412-200609000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Hunter JB. The principles of elastic stable intramedullary nailing in children. Injury. 2005;36:20–24. doi: 10.1016/j.injury.2004.12.009. [DOI] [PubMed] [Google Scholar]
- 15.Daruwalla JS. A study of radioulnar movements following fractures of the forearm in children. Clinical Orthopaedics and Related Research. 1979;139:114–120. [PubMed] [Google Scholar]
- 16.Lee AK, Beck JD, Mirenda WM, Klena JC. Incidence and risk factors for extensor pollicis longus rupture in elastic stable intramedullary nailing of pediatric forearm shaft fractures. Journal of Pediatric Orthopedics. 2016;36(8):810–815. doi: 10.1097/BPO.0000000000000568. [DOI] [PubMed] [Google Scholar]
- 17.Parikh SN, Jain VV, Denning J, Tamai J, Mehlman CT, McCarthy JJ, et al. Complications of elastic stable intramedullary nailing in pediatric fracture management: AAOS exhibit selection. Journal of Bone and Joint Surgery. American Volume. 2012;94(24):e184. doi: 10.2106/JBJS.L.00668. [DOI] [PubMed] [Google Scholar]
- 18.Cumming D, Mfula N, Jones JWM. Paediatric forearm fractures: The increasing use of elastic stable intra-medullary nails. International Orthopaedics. 2008;32:421–423. doi: 10.1007/s00264-007-0334-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Joulie S, Laville JM, Salmeron F. Posteromedial elastic stable intra-medullary nailing (ESIN) in volarly displaced metaphyso-diaphyseal distal radius fractures in child. Orthop Traumatol Surg Res. 2011;97:330–334. doi: 10.1016/j.otsr.2011.01.008. [DOI] [PubMed] [Google Scholar]
- 20.Dinçer R, Köse A, Topal M, Öztürk İA, Engin MÇ. Surgical treatment of pediatric forearm fractures with intramedullary nails: is it a disadvantage to leave the tip exposed? Journal of Pediatric Orthopedics. Part B. 2020;29(2):158–163. doi: 10.1097/BPB.0000000000000635. [DOI] [PubMed] [Google Scholar]
- 21.Kelly BA, Miller P, Shore BJ, Waters PM, Bae DS. Exposed versus buried intramedullary implants for pediatric forearm fractures: a comparison of complications. Journal of Pediatric Orthopedics. 2014;34(8):749–755. doi: 10.1097/BPO.0000000000000210. [DOI] [PubMed] [Google Scholar]