Key Points
Question
Is bariatric surgical weight loss intervention for obesity associated with microvascular and macrovascular outcomes, and are they differentially associated with sex, race, and metabolic status?
Findings
In 307 individuals with obesity who were followed up after bariatric surgery, the procedure was associated with significant weight loss and improvement in both macrovascular and microvascular function across subgroups of sex, race, and traditional metabolic syndrome. Biomarker assessment using high-sensitivity C-reactive protein plasma levels of greater than 2 mg/dL identified individuals with seemingly metabolically healthy obesity and low-grade inflammation who also derived microvascular benefit from weight loss surgery.
Meaning
These findings suggest that the beneficial effects of weight loss surgery extend broadly across sex, race, and certain metabolically healthy subgroups.
This cohort study identifies variables associated with vascular remodeling after bariatric surgery and examines how sex, race, and metabolic status are associated with microvascular and macrovascular outcomes.
Abstract
Importance
Bariatric surgical weight loss is associated with reduced cardiovascular mortality; however, the mechanisms underlying this association are incompletely understood.
Objectives
To identify variables associated with vascular remodeling after bariatric surgery and to examine how sex, race, and metabolic status are associated with microvascular and macrovascular outcomes.
Design, Setting, and Participants
This population-based longitudinal cohort included 307 individuals who underwent bariatric surgery. Participants were enrolled in the bariatric weight loss program at Boston Medical Center, a large, multi-ethnic urban hospital, with presurgical and postsurgical assessments. Data were collected from December 11, 2001 to August 27, 2019. Data were analyzed in September 2019.
Exposure
Bariatric surgery.
Main Outcomes and Measures
Flow-mediated dilation (FMD) and reactive hyperemia (RH) (as measures of macrovascular and microvascular function, respectively) and clinical variables were measured preoperatively at baseline and at least once postoperatively within 12 months of the bariatric intervention.
Results
A total of 307 participants with obesity (mean [SD] age, 42 [12] years; 246 [80%] women; 199 [65%] White; mean [SD] body mass index, 46 [8]) were enrolled in this study. Bariatric surgery was associated with significant weight loss and improved macrovascular and microvascular function across subgroups of sex, race, and traditional metabolic syndrome (mean [SD] pre- vs postsurgery weight: 126 [25] kg vs 104 [25] kg; P < .001; mean [SD] pre- vs postsurgery FMD: 9.1% [5.3] vs 10.2% [5.1]; P < .001; mean [SD] pre- vs postsurgery RH: 764% [400] vs 923% [412]; P < .001). Factors associated with change in vascular phenotype correlated most strongly with adiposity markers and several metabolic variables depending on vascular territory (eg, association of weight change with change in RH: estimate, −3.2; 95% CI, −4.7 to −1.8; association of hemoglobin A1c with change in FMD: estimate, −0.5; 95% CI, −0.95 to −0.05). While changes in macrovascular function among individuals with metabolically healthy obesity were not observed, the addition of biomarker assessment using high-sensitivity C-reactive protein plasma levels greater than 2 mg/dL identified participants with seemingly metabolically healthy obesity who had low-grade inflammation and achieved microvascular benefit from weight loss surgery.
Conclusions and Relevance
The findings of this study suggest that bariatric intervention is associated with weight loss and favorable remodeling of the vasculature among a wide range of individuals with cardiovascular risk. Moreover, differences in arterial responses to weight loss surgery by metabolic status were identified, underscoring heterogeneity in physiological responses to adiposity change and potential activation of distinct pathological pathways in clinical subgroups. As such, individuals with metabolically healthy obesity represent a mixed population that may benefit from more refined phenotypic classification.
Introduction
The obesity epidemic has become a major health care crisis, and its prevalence continues to surge worldwide in children and adults.1,2 Obesity-related deaths are largely driven by cardiovascular diseases,3,4,5 and bariatric surgery has emerged as the most effective and sustainable weight loss strategy as well as the sole weight loss intervention shown to reduce cardiovascular mortality.6,7,8,9,10,11 Data from our group and others have demonstrated that reduction in cardiovascular risk may occur as a function of reversing vascular endothelial dysfunction and insulin resistance.12,13,14,15,16 The objective of our present longitudinal study was to identify variables associated with vascular improvement after bariatric surgery and examine how sex, race, and metabolic status are associated with microvascular and macrovascular outcomes.
Methods
Participants and Study Design
We recruited men and women with obesity (body mass index [BMI; calculated as weight in kilograms divided by height in meters squared] ≥35 ) enrolled in the bariatric surgery program at Boston Medical Center from December 11, 2001, to August 27, 2019. Bariatric operations consisted of Roux-en-Y gastric bypass (RYGB) surgery, sleeve gastrectomy (SG), or laparoscopic adjustable gastric band (LAGB) surgery. Exclusion criteria for the study included patients with recent coronary syndromes, congestive heart failure, malignant neoplasm, systemic infection, acute illness, or pregnancy. The Boston University School of Medicine institutional review board approved study protocol, and all participants provided informed consent. This cohort study adhered to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline. Study participants were evaluated at a baseline visit before their surgical intervention and at least 1 follow-up evaluation no later than 12 months after their surgical intervention. During their baseline visit, participants were asked to self-identify sex and race, with race based on National Institutes of Health categories of Black or African American, American Indian or Alaska Native, Asian, Native Hawaiian or other Pacific Islander, and White. Participants who did not select any of these 5 categories checked other race. Categories were truncated into White and Black or other race for the analyses. Race data were collected because research has shown that individuals from minority racial/ethnic groups in the United States are disproportionately affected by obesity and its associated comorbidities compared with White individuals. One participant did not designate themselves as male or female and was not included in the sex-stratified analyses. Clinical characteristics, such as antihypertensive and lipid lowering medication use, blood pressure, height, weight, BMI, hip circumference (HC), and waist circumference (WC) were recorded during each study visit, and all biochemical analyses were quantified from fasting blood samples.
We stratified our cohort with obesity by traditional metabolic syndrome as previously described.17 Briefly, a metabolically unhealthy obese (MUHO) phenotype was defined by the presence of any 3 of the following traits: abdominal obesity, defined as a waist circumference in men of 102 cm or greater and in women of 88 cm or greater; triglyceride level of 150 mg/dL or greater (to convert to millimoles per liter, multiply by 0.0113); high-density lipoprotein (HDL) cholesterol level of less than 40 mg/dL in men and less than 50 mg/dL in women (to convert to millimoles per liter, multiply by 0.0259); systolic blood pressure of 130 mm Hg or greater, diastolic blood pressure of 85 mm Hg or greater, or use of any hypertension medication; and fasting plasma glucose level of 100 mg/dL or greater if fasting for at least 6 hours (to convert to millimoles per liter, multiply by 0.0555) or drug treatment for elevated blood glucose. Otherwise, participants were classified as having metabolically healthy obesity (MHO). Seven participants were missing 1 of the classifying data points and were removed from this analysis.
Vascular Function Studies
During each study visit, participants underwent an ultrasound of the forearm brachial artery while in a supine position during a fasting state in a quiet and temperature-controlled room under resting conditions by trained sonographers. Using a Powervision 6000 system (Toshiba Medical), brachial vasomotor responses were examined, as previously described.12 Flow-mediated dilation (FMD) is expressed as percentage change of the brachial artery and serves as a measure of endothelium-dependent dilation of the macrovasculature. Briefly, the brachial artery diameter (in millimeters) is recorded at rest and then again 1 minute after a 5-minute cuff occlusion in an upper arm position above the antecubital crease. Pulsed doppler flow velocity (in centimeters per second) at baseline and after cuff deflation served as the quantified measure of reactive hyperemia (RH). Defined as the percentage change in forearm blood flow, RH served as the measure of endothelium-dependent microvascular function. Specific soft tissue landmarks for each digitized frame were identified to ensure that the same arterial segment was imaged at baseline and during the follow-up visit(s). An investigator masked to clinical information performed all offline analyses of digitized end-diastolic images. Intra-observer and inter-observer correlation coefficients for diameter determination are 0.99 and 0.99, respectively, and 0.93 and 0.89 for FMD.18
Statistical Analysis
Analysis for this cohort study was performed in September 2019. Descriptive statistics of clinical characteristics at baseline and postsurgical assessment were examined; all tests were 2-tailed. Presurgical to postsurgical differences were assessed via paired t tests and McNemar test for continuous and categorical variables, respectively. Differences in baseline clinical characteristics by sex, race, and metabolic status were assessed via t tests and χ2 tests, respectively. To incorporate all information from participants with more than 1 follow-up assessment, we used generalized estimating equations (GEEs) with an autoregressive correlation structure to account for within-participant correlation between repeated measures. In an examination of the association between clinical characteristics and vascular measures, GEE was used, modeling change in the clinical characteristics associated with change in vascular measures. Analyses were stratified by sex, race, and metabolic status. All statistical analyses were performed using SAS version 9.4 (SAS Institute).
Results
A total of 307 participants with obesity (mean [SD] age, 42 [12] years; 246 [80%] women; 199 [65%] White; mean [SD] BMI, 46 [8]) were enrolled into this study. All participants underwent bariatric surgery for weight loss, with 259 (84%) having RYGB and remaining 48 (16%) undergoing an SG or LAGB surgery. Table 1 displays the clinical parameters measured at the pre- and postsurgical visits. Participants had a mean (SD) follow up period of 5.9 (4.1) months and lost 17.5% of their initial body weight at their postsurgical assessment (mean [SD] pre- vs postsurgery weight: 126 [25] kg vs 104 [25] kg; P < .001). As expected, improvements in metabolic parameters, such as glucose, insulin, and lipid levels, accompanied weight loss as well as a decrease in the need for medication use during the length of the study.
Table 1. Study Population Characteristics.
| Variable | Mean (SD) | P value | |
|---|---|---|---|
| Baseline visit (n = 307) | Postsurgical visit (n = 307) | ||
| BMI | 46 (8) | 38 (8) | <.001 |
| Waist circumference, cm | 125 (18) | 109 (19) | <.001 |
| Weight, kg | 126 (25) | 104 (25) | <.001 |
| Glucose, mg/dL | 111 (51) | 94 (25) | <.001 |
| Insulin, μIU/ml | 16 (8) | 8 (5) | <.001 |
| HOMA-IR | 5.4 (6.7) | 2.2 (2.9) | <.001 |
| Triglycerides, mg/dL | 121 (70) | 99 (38) | <.001 |
| Total cholesterol, mg/dL | 184 (41) | 167 (35) | <.001 |
| HDL cholesterol, mg/dL | 47 (11) | 43 (13) | <.001 |
| LDL cholesterol, mg/dL | 113 (33) | 104 (30) | <.001 |
| HbA1c, % | 6.2 (1.6) | 5.5 (0.9) | <.001 |
| hs-CRP, mg/dL | 9.9 (9.9) | 5.8 (7.8) | <.001 |
| Antihypertensive medication use, No. (%) | 161 (53) | 76 (25) | <.001 |
| Lipid-lowering medication use, No. (%) | 62 (20) | 20 (7) | <.001 |
| Flow-mediated dilation, % | 9.1 (5.3) | 10.2 (5.1) | <.001 |
| Reactive hyperemia, % change | 764 (400) | 923 (412) | <.001 |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); HbA1c, hemoglobin A1c\; HDL, high-density lipoprotein; HOMA-IR, Homeostatic Model Assessment for Insulin Resistance; hs-CRP, high-sensitivity C-reactive protein; LDL, low-density lipoprotein.
SI conversion factors: To convert insulin to picomoles per liter, multiply by 6.945; glucose to millimoles per liter, multiply by 0.0555; HbA1c to proportion of total hemoglobin, multiply by 0.01; HDL, LDL, and total cholesterol to millimoles per liter, multiply by 0.0259; hs-CRP to milligrams per liter, multiply by 10; and triglycerides to millimoles per liter, multiply by 0.0113.
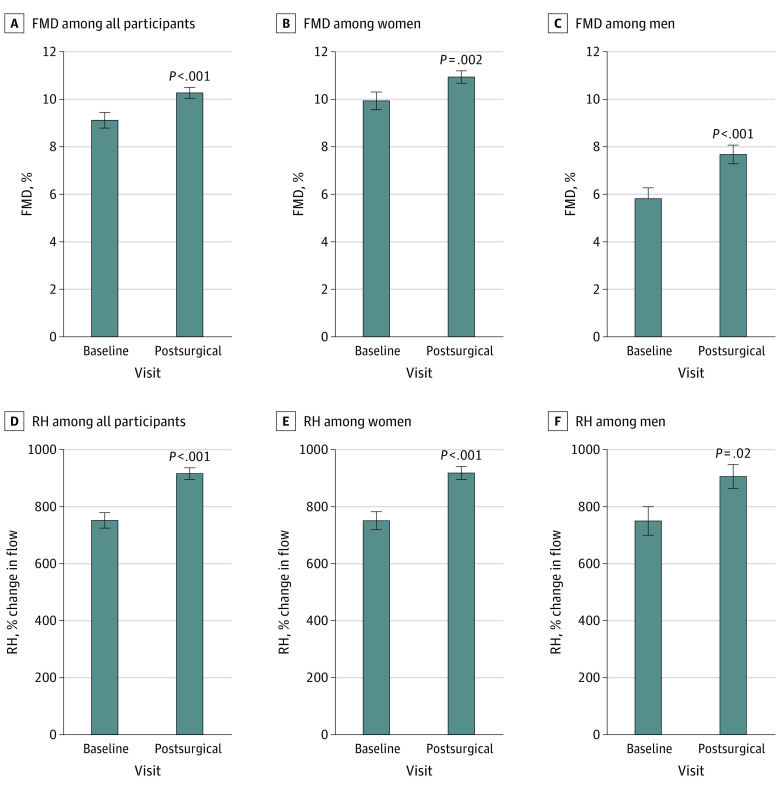
Both endothelium-dependent FMD and RH were improved after surgery, suggesting functional benefits to both the macrovasculature and microvasculature (mean [SD] pre- vs postsurgery FMD: 9.1% [5.3] vs 10.2% [5.1]; P = .001; mean [SD] RH change: 764% [400] vs 923% [412]; P < .001) (Figure 1A and Figure 1D). Clinical factors associated with improved RH were the change in weight, BMI, WC, HC and HDL (eg, association of weight change with change in RH: estimate, −3.2; 95% CI, −4.7 to −1.8), while improvement in hemoglobin A1c (HbA1c) was associated with change in FMD (estimate, −0.5; 95% CI, −0.95 to −0.05) (Table 2). In contrast, surgical procedure type was not associated with vascular end points. Of note, vascular function improved despite discontinuation of medications known to favorably affect endothelial function; thus, the overall cumulative effect of weight loss on vascular function may have been moderated by stoppage of vasculoprotective agents owing to clinical reasons, such as normotension.
Figure 1. Association of Bariatric Surgery With Vascular Function.
Data are presented as mean (SEM). FMD indicates flow-mediated dilation; RH, reactive hyperemia.
Table 2. Change in Clinical and Anthropometric Measures Associated With the Change in Vascular Measures.
| Variable | GEE estimate (95% CI)a | |||||
|---|---|---|---|---|---|---|
| Entire cohort (n = 307) | Women (n = 246) | Men (n = 60) | ||||
| Change in FMD | Change in RH | Change in FMD | Change in RH | Change in FMD | Change in RH | |
| Change in weight | −0.01 (−0.028 to 0.009) | −3.2 (−4.7 to −1.8)b | −0.02 (−0.04 to 0.006) | −3.6 (−5.4 to −1.8)b | 0.005 (−0.01 to 0.02) | −2.4 (−4.9 to 0.09) |
| Change in body mass index | −0.05 (−0.16 to 0.07) | −19.6 (−28.7 to −10.6)b | −0.09 (−0.23 to 0.06) | −20.7 (−31.4 to −10.0)b | 0.03 (−0.10 to 0.16) | −15.4 (−32.9 to 2.2) |
| Change in waist circumference | −0.06 (−0.19 to 0.06) | −20.4 (−30.0 to −10.7)b | −0.07 (−0.2 to 0.08) | −19.7 (−31.2 to −8.2)b | −0.07 (−0.21 to 0.08) | −20.8 (−37.9 to −3.7)c |
| Change in hip circumference | −0.025 (−0.15 to 0.09) | −28.8 (−39.5 to −18.0)b | −0.08 (−0.2 to 0.05) | −27.5 (−40.3 to −14.6)b | −0.03 (−0.20 to 0.13) | −32.7 (−47.4 to −18.1)b |
| Change in total cholesterol | −0.003 (−0.018 to 0.01) | 0.35 (−0.9 to 1.7) | −0.005 (−0.02 to 0.01) | 0.60 (−0.81 to 2.0) | 0.007 (−0.02 to 0.03) | −0.73 (−3.9 to 2.5) |
| Change in HDL cholesterol | 0.005 (−0.04 to 0.05) | 5.4 (1.3 to 9.6)c | 0.006 (−0.04 to 0.06) | 5.8 (1.4 to 10.3)c | 0.08 (−0.02 to 0.17) | −0.75 (−17.0 to 15.5) |
| Change in LDL cholesterol | −0.002 (−0.02 to 0.02) | −0.9 (−2.5 to 0.6) | −0.006 (−0.03 to 0.02) | −0.74 (−2.4 to 0.9) | 0.008 (−0.02 to 0.03) | −1.7 (−5.4 to 2.0) |
| Change in triglycerides | −0.002 (−0.01 to 0.008) | −0.3 (−1.3 to 0.7) | −0.001 (−0.01 to 0.01) | −0.38 (−1.6 to 0.84) | −0.009 (−0.02 to 0.005) | 0.05 (−1.7 to 1.6) |
| Change in glucose | −0.01 (−0.02 to 0.003) | −0.5 (−1.6 to 0.7) | −0.01 (−0.02 to 0.005) | −0.3 (−1.6 to 1.0) | −0.005 (−0.03 to 0.02) | −1.5 (−3.3 to 0.43) |
| Change in insulin | −0.02 (−0.08 to 0.04) | −7.5 (−16 to 1.1) | −0.02 (−0.10 to 0.06) | −5.8 (−15.7 to 4.1) | 0.007 (−0.08 to 0.09) | −14.4 (−29.9 to 1.2) |
| Change in HOMA-IR | −0.04 (−0.1 to 0.05) | −4.1 (−12.8 to 4.5) | 0.008 (−0.12 to 0.10) | −7.3 (−18.0 to 3.4) | −0.06 (−0.12 to 0.005) | 0.08 (−9.4 to 9.6) |
| Change in HbA1c | −0.5 (−0.95 to −0.05)c | −19.6 (−90.8 to 51.6) | −0.67 (−1.2 to −0.17)d | −26.9 (−104.2 to 50.4) | 0.4 (−0.8 to 1.7) | 68.0 (−91.5 to 227.5) |
| Change in hs-CRP | 0.003 (−0.05 to 0.05) | −4.4 (−10.1 to 1.3) | 0.009 (−0.09 to 0.07) | −8.2 (−15.3 to −1.1)c | −0.004 (−0.04 to 0.03) | −1.5 (−10.3 to 7.3) |
Abbreviations: FMD, flow-mediated dilation; GEE, generalized estimating equations; HbA1c, hemoglobin A1c; HDL, high-density lipoprotein; HOMA-IR, Homeostatic Model Assessment for Insulin Resistance; hs-CRP, high-sensitivity C-reactive protein; LDL, low-density lipoprotein; RH, reactive hyperemia.
Data are presented as GEE estimates of association of the change in a clinical variable and vascular measures for 1-unit change in the variable measure.
P < .001.
P < .05.
P < .01.
Stratification by Sex
Next, we explored whether vascular outcomes over time differed when stratified by sex (eTable 1 in the Supplement). The mean (SD) follow-up period for men and women was 6.0 (4.0) and 5.9 (4.1) months, respectively. Both men and women had similar BMI at baseline and lost a comparable percentage of weight at their postoperative assessment. Women displayed an improvement in FMD and RH following bariatric surgery (mean [SD] FMD: presurgery, 9.9% [5.4] vs postsurgery, 10.9% [4.9]; P = .002) (Figure 1B and Figure 1E). Decreased measures of adiposity assessed by weight, BMI, WC, and HC, lower circulating high-sensitivity C-reactive protein (hs-CRP), and increased HDL cholesterol were all associated with improvement in RH, while change in HbA1c was associated with FMD (Table 2). Similarly, we observed a significant improvement in FMD and RH in men at their postoperative assessment (mean [SD] FMD: presurgery, 5.8% [3.3] vs postsurgery, 7.7% [3.9]; P < .001) (Figure 1C and Figure 1F), with increased RH associated with decreases in WC and HC (Table 2). As such, the improvement in FMD and RH in men and women was equivalent.
Stratification by Self-identified Race
In our cohort, 199 participants (65%) self-identified as White, 75 participants (24%) self-identified as Black, and 33 participants (11%) self-identified as other. Baseline clinical characteristics stratified by race are displayed in eTable 2 in the Supplement. White participants were older and had higher blood levels of triglycerides and cholesterol compared with the rest of the cohort, while BMI was similar across races prior to surgery. As displayed in Figure 2A and Figure 2E, White participants had a significant improvement in FMD (mean [SD] FMD: presurgery, 8.5% [4.9] vs postsurgery, 9.8% [4.7]; P < .001) and RH at their postoperative assessment (mean [SD] 6.0 [4.1] months follow-up time). Changes in adiposity measures and hs-CRP were negatively associated with RH, and improvements in circulating HDL was associated positively with microvascular function (Table 3). Black participants and those who identified as other also displayed favorable macrovascular and microvascular outcomes at their postoperative visit (mean [SD] FMD: presurgery, 10.3% [5.7] vs postsurgery, 11.5% [5.2]; P = .045; mean [SD] follow-up time, 5.7 [4.0] months) (Figure 2B and Figure 2F), and factors associated with microvascular change were similar across races. In contrast, amelioration in triglycerides, glucose control, and insulin resistance were associated with the improvement in FMD only in participants who identified as belonging to a minority racial group, highlighting that determinants of vascular remodeling following weight loss surgery may differ between races.
Figure 2. Microvascular and Macrovascular Function Improvement Following Bariatric Surgery by Race and Metabolic Status.
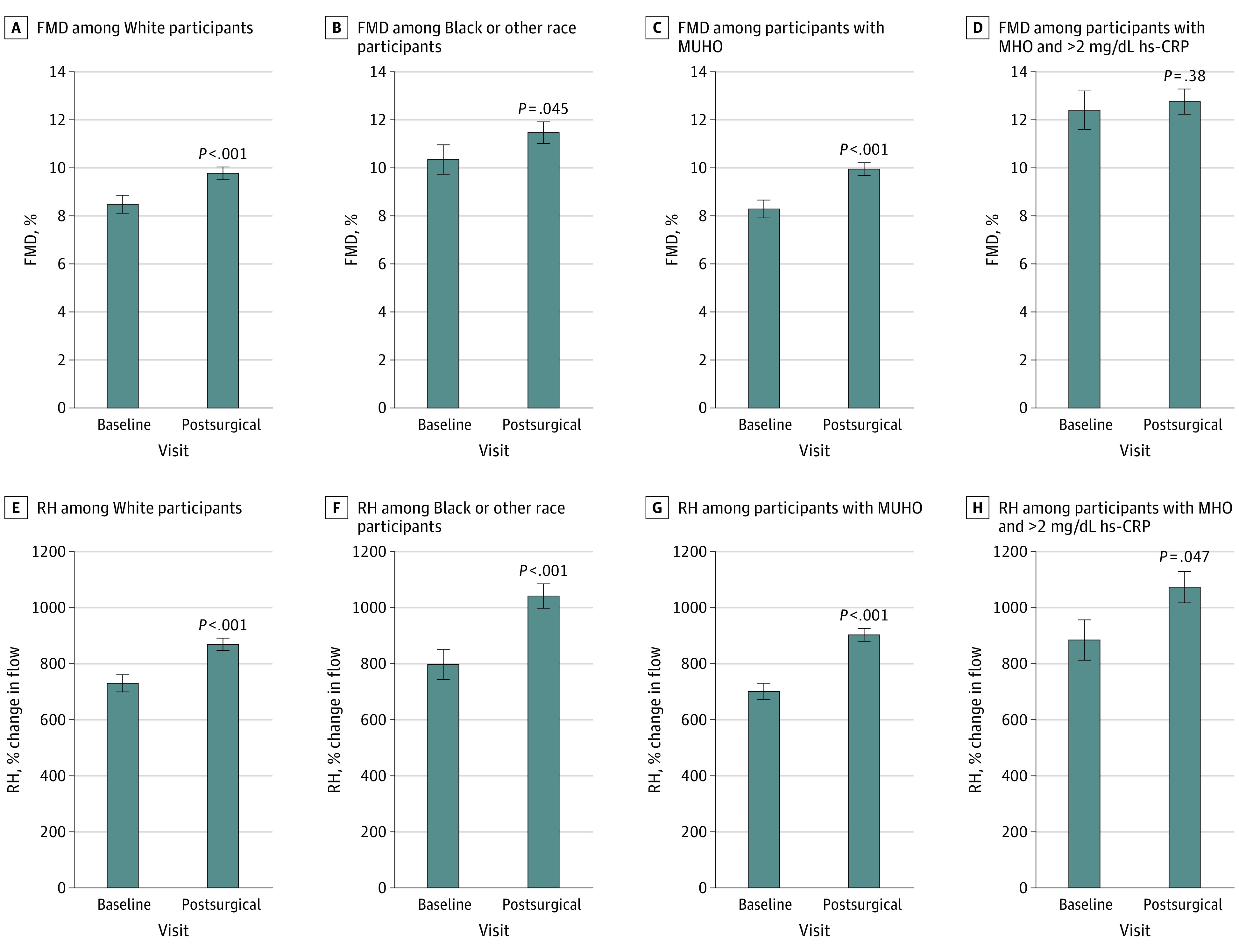
Data are presented as mean (SEM). FMD indicates flow-mediated dilation; hs-CRP, high sensitivity C-reactive protein (to convert to milligrams per liter, multiply by 10); MHO, metabolically healthy obesity; MUHO, metabolically unhealthy obesity; and RH, reactive hyperemia.
Table 3. Change in Clinical and Anthropometric Measures Associated With Change in Vascular Measures Stratified by Race and Metabolic Status.
| Variable | GEE estimate (95% CI)a | ||||||
|---|---|---|---|---|---|---|---|
| White (n = 199) | Black or other race (n = 108) | MUHO (n = 222) | MHO with hs-CRP level ≥2 mg/dL (n = 53) | ||||
| Change in FMD | Change in RH | Change in FMD | Change in RH | Change in FMD | Change in RH | Change in RH | |
| Change in weight | −0.01 (−0.03 to 0.01) | −3.1 (−4.6 to −1.6)b | −0.006 (−0.05 to 0.03) | −4.6 (−8.9 to −0.3)c | −0.01 (−0.04 to 0.01) | −2.6 (−4.0 to −1.1)b | −5.7 (−11 to −0.5)c |
| Change in body mass index | −0.07 (−0.20 to 0.06) | −19.2 (−28.6 to −9.9)b | 0.01 (−0.26 to 0.28) | −27.7 (−54.7 to −0.7)c | −0.08 (−0.2 to 0.06) | −15.1 (−24.0 to −6.2)b | −39.3 (−75.3 to −3.3)c |
| Change in waist circumference | −0.07 (−0.19 to 0.06) | −19.9 (−30.1 to −9.6)b | −0.06 (−0.3 to 0.2) | −25.3 (−47.3 to −3.3)c | −0.09 (−0.2 to 0.05) | −15.8 (−25.7 to −5.8)d | −40.9 (−76.3 to −5.7)c |
| Change in hip circumference | 0.04 (−0.11 to 0.19) | −27.5 (−39.4 to −15.5)b | −0.21 (−0.49 to 0.07) | −36.6 (−62.2 to −11.0)d | −0.06 (−0.2 to 0.08) | −22.2 (−32.8 to −11.6)b | −58.8 (−87.3 to −30.3)b |
| Change in total cholesterol | −0.0003 (−0.02 to 0.02) | 0.76 (−0.56 to 2.1) | −0.01 (−0.05 to 0.03) | −1.1 (−4.5 to 2.3) | −0.005 (−0.02 to 0.01) | −0.09 (−1.4 to 1.2) | 3.2 (−1.1 to 7.4) |
| Change in HDL cholesterol | −0.001 (−0.06 to 0.06) | 7.8 (3.6 to 12.1)b | 0.03 (−0.025 to 0.09) | 2.3 (−3.2 to 7.9) | 0.008 (−0.05 to 0.06) | 3.7 (−0.4 to 7.8) | 10.9 (1.8 to 19.9)c |
| Change in LDL cholesterol | −0.002 (−0.02 to 0.016) | −0.87 (−2.4 to 0.69) | −0.002 (−0.05 to 0.05) | −1.1 (−4.9 to 2.7) | −0.005 (−0.02 to 0.01) | −1.2 (−2.7 to 0.3) | 1.7 (−3.7 to 7.0) |
| Change in triglycerides | 0.005 (−0.007 to 0.02) | 0.23 (−0.82 to 1.3) | −0.01 (−0.03 to −0.002)c | −1.5 (−2.6 to −0.26)c | −0.002 (−0.01 to 0.01) | −0.05 (−1.1 to 1.0) | 1.9 (−2.6 to 6.3) |
| Change in glucose | 0.003 (−0.01 to 0.02) | 0.21 (−0.85 to 1.26) | −0.03 (−0.04 to −0.009)d | −0.94 (−2.8 to 0.9) | −0.01 (−0.02 to 0.003) | −0.35 (−1.5 to 0.8) | 13.9 (6.9 to 20.9)b |
| Change in insulin | 0.003 (−0.07 to 0.08) | −6.8 (−14.0 to 0.43) | −0.09 (−0.19 to 0.005) | −14.6 (−41.9 to 12.8) | −0.03 (−0.1 to 0.04) | −5.9 (−14.5 to 2.7) | 0.6 (−55.4 to 56.5) |
| Change in HOMA-IR | 0.03 (−0.07 to 0.13) | −5.2 (−16.1 to 5.7) | −0.17 (−0.3 to −0.04)c | −1.4 (−15.7 to 12.9) | −0.04 (−0.1 to 0.06) | −1.9 (−10.1 to 6.3) | 42.9 (−145.9 to 231.7) |
| Change in HbA1c | 0.27 (−0.54 to 1.1) | 35.2 (−43.9 to 114.2) | −0.82 (−1.4 to −0.2)d | −39.0 (−131.2 to 53.2) | −0.47 (−0.9 to 0.002) | −11.8 (−87.2 to 63.6) | 161.8 (−167.9 to 491.5) |
| Change in hs-CRP | 0.02 (−0.07 to 0.03) | −7.4 (−13.5 to −1.2)c | 0.07 (−0.07 to 0.2) | 5.4 (−6.2 to 17.1) | 0.001 (−0.05 to 0.05) | −4.6 (−10.5 to 1.2) | 31.2 (14.3 to 48.1)b |
Abbreviations: FMD, flow-mediated dilation; GEE, generalized estimating equations; HbA1c, hemoglobin A1c; HDL, high-density lipoprotein; HOMA-IR, Homeostatic Model Assessment for Insulin Resistance; hs-CRP, high-sensitivity C-reactive protein; LDL, low-density lipoprotein; MHO, metabolically healthy obesity; MUHO, metabolically unhealthy obesity; RH, reactive hyperemia.
SI conversion factor: To convert hs-CRP to milligrams per liter, multiply by 10.
Data are presented as GEE estimates of association of the change in a clinical variable and vascular measures for 1-unit change in the variable measure.
P < .001.
P < .05.
P < .01.
Stratification by Traditional Metabolic Syndrome
When we stratified our cohort by traditional metabolic syndrome criteria, 222 participants (74%) had metabolic syndrome at the baseline visit and were classified as metabolically unhealthy with obesity (MUHO) vs 78 (26%) who were metabolically healthy with obesity (MHO). By definition, participants with MUHO had more cardiovascular risk factors, including greater WC and higher prevalence of diabetes, hypertension, and hyperlipidemia, compared with those with MHO. Additionally, participants with MUHO were older, and the group had fewer women than the group with MHO, but measures of adiposity were comparable at baseline (eTable 3 in the Supplement). Participants with MUHO had a mean (SD) follow-up time of 5.9 (4.1) months, and those with MHO had a mean (SD) follow up time of 5.9 (4.1) months. Following bariatric surgery, participants with MUHO and MHO had similar degrees of weight loss and significant improvements in clinical variables, such as HbA1c levels, Homeostatic Model Assessment for Insulin Resistance score, and lipid and hs-CRP levels, were observed, despite participants with MHO having a more favorable presurgical metabolic profile.
However, vascular outcomes after surgical intervention differed between the MUHO and MHO groups. In the MUHO group, both macrovascular and microvascular function improved (mean [SD] FMD: presurgery, 8.3% [5.1] vs postsurgery, 9.9% [5.0]; P < .001) (Figure 2C and Figure 2G) with change in weight, BMI, WC, and HC associated with microvascular function (Table 3). Among participants with MHO, there was no significant alteration in FMD or RH after surgery. Therefore, we excluded all participants with MHO with circulating hs-CRP levels of 2 mg/dL or lower, creating an MHO group that was further classified as exhibiting chronic inflammation (hs-CRP >2 mg/dL) as an additional cardiovascular disease risk factor.19 Comparable differences in clinical parameters between participants with MHO and hs-CRP levels greater than 2 mg/dL and participants with MUHO were observed (eTable 4 in the Supplement). In this subset of participants with MHO, RH improved significantly (mean [SD] RH: presurgery, 885% [413] vs postsurgery, 1074% [391]; P = .047), while FMD remained unaltered at the postoperative assessment (mean [SD] follow-up time, 5.9 [4.1] months) (Figure 2D and 2H). These findings suggest that even participants with seemingly metabolically healthy obesity, when stratified by elevated inflammatory biomarkers, such as hs-CRP, experienced vascular benefit after bariatric weight loss.
Discussion
To our knowledge, this study represents the largest longitudinal bariatric surgical cohort that examined both FMD and RH as measures of macrovascular and microvascular function, respectively. We found that both vascular outcomes, which have been clinically validated as independent predictors of cardiovascular risk,20,21,22 significantly improved following bariatric intervention and track changes in anthropometric measures and metabolic risk factors, depending on vascular territory. In smaller, previous studies, our group and others have observed improvement in subclinical atherosclerosis and vascular health following weight loss.12,13,23,24,25 Our subset analyses identified differences in arterial responses to weight loss surgery by metabolic status, underscoring heterogeneity in physiological response to adiposity change and potential activation of distinct pathological pathways in obesity subgroups. Moreover, by incorporating inflammatory biomarker assessment, we found that participants with seemingly MHO and signs of chronic low-grade inflammation experienced vascular benefit after weight loss, touching on a growing area of interest and controversy in the field that warrants further investigation.
Bariatric surgery has been shown to improve metabolism, reduce morbidity and mortality, and favorably remodel the vasculature.8,13,14,15,16,26,27,28,29,30,31,32 Clinical studies have observed improvement in FMD and carotid intima thickening (CIMT) after bariatric operations,13,16,26,31,33,34,35 and amelioration of metabolic syndrome, type 2 diabetes, and insulin resistance have been associated with enhanced microvascular function.14,30,36,37,38,39 Thus, our findings extend these previous reports that involved smaller cohorts and shorter follow-up periods.13,26,33,35 In our study, while we identified several traditional risk factors as associated with FMD and RH, these associations were modest or tracked weakly, particularly for macrovascular outcomes, consistent with some prior reports.13,16,33 In this regard, recent mortality data from the Swedish Obesity Study (SOS) showed that while most deaths were cardiovascular, treatment benefits and increased survival following bariatric surgery were actually even across subgroups of traditional risk factors, such as hypertension and cholesterol levels.40 These data, in conjunction with our present findings, highlight significant knowledge gaps in identifying mechanistic regulators of vascular physiology with weight change and underscore our need to search beyond the usual suspects, potentially considering the role of adipocytokines and genetic variability. Although bariatric surgery type may influence the extent of metabolic recovery,41,42,43,44 we did not identify a specific surgical approach that was differentially associated with vascular function.
While bariatric surgery is an effective strategy to combat obesity, there is considerable variability in comorbidity remission across individuals.45,46 This has generated clinical discussions regarding whether bariatric surgery can serve as a one size fits all approach in the treatment of obesity or whether tailored strategies are needed to improve outcomes in specific patient populations. For decades, clinical studies have consistently found that women are more likely to pursue bariatric surgery than men.47,48,49,50 Moreover, although men may have greater positive postoperative psychological outcomes,47 male sex is independently associated with major postoperative complications, mortality, and lower weight loss.47,50,51,52 Very limited data exist surrounding the association of bariatric surgery with vascular function with respect to sex, with small studies showing changes in CIMT after surgery.53,54 Our finding that both sexes had comparable percentage of weight loss and derived similar improvement in both macrovascular and microvascular function following weight loss surgery is of public health importance. Moreover, some inconsistent observations within the literature surrounding the differential outcomes of bariatric surgery among men and women underscores the need for sex-balanced studies.
Minority populations in the United States bear a disproportionate burden of the obesity epidemic and its associated comorbidities and tend to undergo fewer bariatric procedures compared with non-Hispanic White populations, which may be associated with socioeconomic factors, limited access to health care, and/or insurance options.55,56 In addition, recent studies have identified race as an important factor associated with weight fluctuations, remission of obesity-related comorbidities, lower weight loss, and higher rates of hospital resource utilization and mortality after bariatric surgery.57,58,59,60,61,62,63 In our current study, reversal of microvascular and macrovascular dysfunction was evident in both White participants and participants who identified as a minority racial/ethnic group, but the factors associated with vascular remodeling differed between races. Minority populations have been associated with lower hypertension remission and higher mortality rates,56,58,59,62,63 which may partly relate to abnormalities in vascular tone. Racial differences may exist in their anatomical and physiological properties, which warrant further investigation.
Finally, the notion of whether patients with MHO should be approached differently remains a controversial clinical debate.64 Recent data suggest that these individuals may be in a transient physiological state along a progression to obesity-related diseases and should seek therapeutic lifestyle changes.65,66 Participants with obesity frequently display histological evidence of chronic low-grade inflammation in various organ systems, particularly hepatic and adipose tissues as well as plasma elevation in hs-CRP19 that may contribute to cardiometabolic diseases. In the present study, we used a more stringent definition of MHO, stratifying subjects by hs-CRP level as an inflammatory biomarker that is independently associated with vascular events and improves global classification in cardiovascular disease.19,67 In participants with MHO and elevated hs-CRP levels, we observed significant improvement in microvascular function following bariatric intervention, which was also associated with lower hs-CRP levels. These support the findings from the SOS study, suggesting that bariatric surgery is associated with reduced risk of microvascular complications across subsets of participants with obesity and varying degrees of metabolic disease.36 Thus, the notion of incorporating additional clinical markers to identify participants with MHO at higher risk may have clinical value.
Limitations
This study has limitations. First, most study participants were women, which reflects the general clinical practice and known sex differences in populations that seek bariatric treatments.37,49,50,68 Second, the study was observational and not randomized, and most surgeries were RYGB operations that were determined clinically. Third, racial categories were based on self-identification rather than ancestry informative markers. However, these are counterbalanced by the relatively large sample for this type of prospective clinical investigation involving validated vascular physiological outcomes. Fourth, we acknowledge that across the analyses conducted here, there were many hypothesis tests performed. We have not corrected the significance level to account for the multiple testing performed in the study; thus, there is the potential for some false-positive findings. Ideally, notwithstanding the challenges, these results should be validated in further studies.
Conclusions
In conclusion, the findings of this study suggest that bariatric surgery is associated with reductions in weight, amelioration of cardiovascular risk factors, and improvement in vascular endothelial phenotype. Improvements in microvascular function, in particular, were observed across all subgroups of sex, race, and metabolic syndrome, while variability in macrovascular changes were observed within subcategories of our cohort. Lastly, factors associated with vascular change were largely modest using known traditional clinical variables, exposing our limited knowledge of mechanisms that govern vascular physiology in obesity and underscoring the crucial need for further investigative studies in this field.
eTable 1. Clinical Characteristics Stratified by Sex
eTable 2. Clinical Characteristics Stratified by Race
eTable 3. Clinical Characteristics of Participants With Metabolically Unhealthy Obesity (MUHO) vs Metabolically Healthy Obesity (MHO)
eTable 4. Clinical Characteristics of Participants With Metabolically Unhealthy Obesity (MUHO) vs Metabolically Healthy Obesity (MHO) and High-Sensitivity C-Reactive Protein (hs-CRP) Levels Greater Than 2 mg/dL
References
- 1.Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL. Trends in obesity among adults in the United States, 2005 to 2014. JAMA. 2016;315(21):2284-2291. doi: 10.1001/jama.2016.6458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Lawman HG, et al. Trends in obesity prevalence among children and adolescents in the United States, 1988-1994 through 2013-2014. JAMA. 2016;315(21):2292-2299. doi: 10.1001/jama.2016.6361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Di Angelantonio E, Bhupathiraju ShN, Wormser D, et al. ; Global BMI Mortality Collaboration . Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet. 2016;388(10046):776-786. doi: 10.1016/S0140-6736(16)30175-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Whitlock G, Lewington S, Sherliker P, et al. ; Prospective Studies Collaboration . Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373(9669):1083-1096. doi: 10.1016/S0140-6736(09)60318-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Twig G, Yaniv G, Levine H, et al. Body-mass index in 2.3 million adolescents and cardiovascular death in adulthood. N Engl J Med. 2016;374(25):2430-2440. doi: 10.1056/NEJMoa1503840 [DOI] [PubMed] [Google Scholar]
- 6.Adams TD, Davidson LE, Litwin SE, et al. Weight and metabolic outcomes 12 years after gastric bypass. N Engl J Med. 2017;377(12):1143-1155. doi: 10.1056/NEJMoa1700459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aleassa EM, Khorgami Z, Kindel TL, et al. Impact of bariatric surgery on heart failure mortality. Surg Obes Relat Dis. 2019;15(7):1189-1196. doi: 10.1016/j.soard.2019.03.021 [DOI] [PubMed] [Google Scholar]
- 8.Aminian A, Aleassa EM, Bhatt DL, et al. Bariatric surgery is associated with a lower rate of death after myocardial infarction and stroke: a nationwide study. Diabetes Obes Metab. 2019;21(9):2058-2067. doi: 10.1111/dom.13765 [DOI] [PubMed] [Google Scholar]
- 9.Benotti PN, Wood GC, Carey DJ, et al. Gastric bypass surgery produces a durable reduction in cardiovascular disease risk factors and reduces the long-term risks of congestive heart failure. J Am Heart Assoc. 2017;6(5):e005126. doi: 10.1161/JAHA.116.005126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Johnson BL, Blackhurst DW, Latham BB, et al. Bariatric surgery is associated with a reduction in major macrovascular and microvascular complications in moderately to severely obese patients with type 2 diabetes mellitus. J Am Coll Surg. 2013;216(4):545-556. doi: 10.1016/j.jamcollsurg.2012.12.019 [DOI] [PubMed] [Google Scholar]
- 11.Lynch KT, Mehaffey JH, Hawkins RB, Hassinger TE, Hallowell PT, Kirby JL. Bariatric surgery reduces incidence of atrial fibrillation: a propensity score-matched analysis. Surg Obes Relat Dis. 2019;15(2):279-285. doi: 10.1016/j.soard.2018.11.021 [DOI] [PubMed] [Google Scholar]
- 12.Bigornia SJ, Farb MG, Tiwari S, et al. Insulin status and vascular responses to weight loss in obesity. J Am Coll Cardiol. 2013;62(24):2297-2305. doi: 10.1016/j.jacc.2013.07.078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lupoli R, Di Minno MN, Guidone C, et al. Effects of bariatric surgery on markers of subclinical atherosclerosis and endothelial function: a meta-analysis of literature studies. Int J Obes (Lond). 2016;40(3):395-402. doi: 10.1038/ijo.2015.187 [DOI] [PubMed] [Google Scholar]
- 14.Sjöström L, Peltonen M, Jacobson P, et al. Association of bariatric surgery with long-term remission of type 2 diabetes and with microvascular and macrovascular complications. JAMA. 2014;311(22):2297-2304. doi: 10.1001/jama.2014.5988 [DOI] [PubMed] [Google Scholar]
- 15.Sjöström L, Peltonen M, Jacobson P, et al. Bariatric surgery and long-term cardiovascular events. JAMA. 2012;307(1):56-65. doi: 10.1001/jama.2011.1914 [DOI] [PubMed] [Google Scholar]
- 16.Tarzia P, Lanza GA, Sestito A, et al. Long-term effects of bariatric surgery on peripheral endothelial function and coronary microvascular function. Obes Res Clin Pract. 2017;11(1):114-117. doi: 10.1016/j.orcp.2016.12.005 [DOI] [PubMed] [Google Scholar]
- 17.Brant LC, Wang N, Ojeda FM, et al. Relations of metabolically healthy and unhealthy obesity to digital vascular function in three community-based cohorts: a meta-analysis. J Am Heart Assoc. 2017;6(3):e004199. doi: 10.1161/JAHA.116.004199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Duffy SJ, Keaney JF Jr, Holbrook M, et al. Short- and long-term black tea consumption reverses endothelial dysfunction in patients with coronary artery disease. Circulation. 2001;104(2):151-156. doi: 10.1161/01.CIR.104.2.151 [DOI] [PubMed] [Google Scholar]
- 19.Virani SS, Alonso A, Benjamin EJ, et al. ; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics—2020 update: a report from the American Heart Association. Circulation. 2020;141(9):e139-e596. doi: 10.1161/CIR.0000000000000757 [DOI] [PubMed] [Google Scholar]
- 20.Anderson TJ, Charbonneau F, Title LM, et al. Microvascular function predicts cardiovascular events in primary prevention: long-term results from the Firefighters and Their Endothelium (FATE) study. Circulation. 2011;123(2):163-169. doi: 10.1161/CIRCULATIONAHA.110.953653 [DOI] [PubMed] [Google Scholar]
- 21.Inaba Y, Chen JA, Bergmann SR. Prediction of future cardiovascular outcomes by flow-mediated vasodilatation of brachial artery: a meta-analysis. Int J Cardiovasc Imaging. 2010;26(6):631-640. doi: 10.1007/s10554-010-9616-1 [DOI] [PubMed] [Google Scholar]
- 22.Huang AL, Silver AE, Shvenke E, et al. Predictive value of reactive hyperemia for cardiovascular events in patients with peripheral arterial disease undergoing vascular surgery. Arterioscler Thromb Vasc Biol. 2007;27(10):2113-2119. doi: 10.1161/ATVBAHA.107.147322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bigornia SJ, Mott MM, Hess DT, et al. Long-term successful weight loss improves vascular endothelial function in severely obese individuals. Obesity (Silver Spring). 2010;18(4):754-759. doi: 10.1038/oby.2009.482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hamburg NM, Mott MM, Bigornia SJ, et al. Maladaptive enlargement of the brachial artery in severe obesity is reversed with weight loss. Vasc Med. 2010;15(3):215-222. doi: 10.1177/1358863X10362831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sturm W, Tschoner A, Engl J, et al. Effect of bariatric surgery on both functional and structural measures of premature atherosclerosis. Eur Heart J. 2009;30(16):2038-2043. doi: 10.1093/eurheartj/ehp211 [DOI] [PubMed] [Google Scholar]
- 26.Brethauer SA, Heneghan HM, Eldar S, et al. Early effects of gastric bypass on endothelial function, inflammation, and cardiovascular risk in obese patients. Surg Endosc. 2011;25(8):2650-2659. doi: 10.1007/s00464-011-1620-6 [DOI] [PubMed] [Google Scholar]
- 27.Coleman KJ, Huang YC, Hendee F, Watson HL, Casillas RA, Brookey J. Three-year weight outcomes from a bariatric surgery registry in a large integrated healthcare system. Surg Obes Relat Dis. 2014;10(3):396-403. doi: 10.1016/j.soard.2014.02.044 [DOI] [PubMed] [Google Scholar]
- 28.Jakobsen GS, Småstuen MC, Sandbu R, et al. Association of bariatric surgery vs medical obesity treatment with long-term medical complications and obesity-related comorbidities. JAMA. 2018;319(3):291-301. doi: 10.1001/jama.2017.21055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Reges O, Greenland P, Dicker D, et al. Association of bariatric surgery using laparoscopic banding, Roux-en-Y gastric bypass, or laparoscopic sleeve gastrectomy vs usual care obesity management with all-cause mortality. JAMA. 2018;319(3):279-290. doi: 10.1001/jama.2017.20513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sjöström L, Lindroos AK, Peltonen M, et al. ; Swedish Obese Subjects Study Scientific Group . Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351(26):2683-2693. doi: 10.1056/NEJMoa035622 [DOI] [PubMed] [Google Scholar]
- 31.Tschoner A, Sturm W, Gelsinger C, et al. Long-term effects of weight loss after bariatric surgery on functional and structural markers of atherosclerosis. Obesity (Silver Spring). 2013;21(10):1960-1965. doi: 10.1002/oby.20357 [DOI] [PubMed] [Google Scholar]
- 32.Piché ME, Clavel MA, Auclair A, et al. Early benefits of bariatric surgery on subclinical cardiac function: contribution of visceral fat mobilization. Metabolism. 2021;119:154773. doi: 10.1016/j.metabol.2021.154773 [DOI] [PubMed] [Google Scholar]
- 33.de Assunção Machado AC, da Silva AMV, Signori LU, da Costa Alvarez G, Mottin CC. Endothelial function of patients with morbid obesity submitted to Roux-en-Y gastric bypass with and without obstructive sleep apnea-hypopnea syndrome. Obes Surg. 2018;28(11):3595-3603. doi: 10.1007/s11695-018-3403-9 [DOI] [PubMed] [Google Scholar]
- 34.Ricci MA, Ministrini S, De Vuono S, et al. Sleeve gastrectomy efficacy on metabolic and cardiovascular dysfunction with a focus on the role of comorbidities. Angiology. 2018;69(6):475-482. doi: 10.1177/0003319717718707 [DOI] [PubMed] [Google Scholar]
- 35.Gluszewska A, Gryglewska B, Rewiuk K, et al. Arterial structure and function and its short- and long-term changes after bariatric surgery. J Physiol Pharmacol. 2019;70(6). [DOI] [PubMed] [Google Scholar]
- 36.Carlsson LMS, Sjöholm K, Karlsson C, et al. Long-term incidence of microvascular disease after bariatric surgery or usual care in patients with obesity, stratified by baseline glycaemic status: a post-hoc analysis of participants from the Swedish Obese Subjects study. Lancet Diabetes Endocrinol. 2017;5(4):271-279. doi: 10.1016/S2213-8587(17)30061-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Martín-Rodríguez JF, Cervera-Barajas A, Madrazo-Atutxa A, et al. Effect of bariatric surgery on microvascular dysfunction associated to metabolic syndrome: a 12-month prospective study. Int J Obes (Lond). 2014;38(11):1410-1415. doi: 10.1038/ijo.2014.15 [DOI] [PubMed] [Google Scholar]
- 38.Ministrini S, Fattori C, Ricci MA, et al. Microcirculatory improvement induced by laparoscopic sleeve gastrectomy is related to insulin sensitivity retrieval. Obes Surg. 2018;28(10):3151-3158. doi: 10.1007/s11695-018-3290-0 [DOI] [PubMed] [Google Scholar]
- 39.Streese L, Königstein K, Goricki L, et al. Short- and long-term effects of bariatric surgery on vascular phenotype. Obes Surg. 2019;29(4):1301-1308. doi: 10.1007/s11695-018-03679-2 [DOI] [PubMed] [Google Scholar]
- 40.Carlsson LMS, Sjöholm K, Jacobson P, et al. Life expectancy after bariatric surgery in the Swedish Obese Subjects Study. N Engl J Med. 2020;383(16):1535-1543. doi: 10.1056/NEJMoa2002449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wei JH, Chou RH, Huang PH, Lee WJ, Chen SC, Lin SJ. Metabolic surgery ameliorates cardiovascular risk in obese diabetic patients: influence of different surgical procedures. Surg Obes Relat Dis. 2018;14(12):1832-1840. doi: 10.1016/j.soard.2018.08.026 [DOI] [PubMed] [Google Scholar]
- 42.Chen JC, Hsu NY, Lee WJ, Chen SC, Ser KH, Lee YC. Prediction of type 2 diabetes remission after metabolic surgery: a comparison of the individualized metabolic surgery score and the ABCD score. Surg Obes Relat Dis. 2018;14(5):640-645. doi: 10.1016/j.soard.2018.01.027 [DOI] [PubMed] [Google Scholar]
- 43.Almalki OM, Lee WJ, Chong K, Ser KH, Lee YC, Chen SC. Laparoscopic gastric bypass for the treatment of type 2 diabetes: a comparison of Roux-en-Y versus single anastomosis gastric bypass. Surg Obes Relat Dis. 2018;14(4):509-515. doi: 10.1016/j.soard.2017.12.022 [DOI] [PubMed] [Google Scholar]
- 44.Puzziferri N, Roshek TB III, Mayo HG, Gallagher R, Belle SH, Livingston EH. Long-term follow-up after bariatric surgery: a systematic review. JAMA. 2014;312(9):934-942. doi: 10.1001/jama.2014.10706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Courcoulas AP, Christian NJ, Belle SH, et al. ; Longitudinal Assessment of Bariatric Surgery (LABS) Consortium . Weight change and health outcomes at 3 years after bariatric surgery among individuals with severe obesity. JAMA. 2013;310(22):2416-2425. doi: 10.1001/jama.2013.280928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Courcoulas AP, King WC, Belle SH, et al. Seven-year weight trajectories and health outcomes in the Longitudinal Assessment of Bariatric Surgery (LABS) Study. JAMA Surg. 2018;153(5):427-434. doi: 10.1001/jamasurg.2017.5025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kochkodan J, Telem DA, Ghaferi AA. Physiologic and psychological gender differences in bariatric surgery. Surg Endosc. 2018;32(3):1382-1388. doi: 10.1007/s00464-017-5819-z [DOI] [PubMed] [Google Scholar]
- 48.Young MT, Phelan MJ, Nguyen NT. A decade analysis of trends and outcomes of male vs female patients who underwent bariatric surgery. J Am Coll Surg. 2016;222(3):226-231. doi: 10.1016/j.jamcollsurg.2015.11.033 [DOI] [PubMed] [Google Scholar]
- 49.Zizza CA, Herring AH, Stevens J, Carey TS. Bariatric surgeries in North Carolina, 1990 to 2001: a gender comparison. Obes Res. 2003;11(12):1519-1525. doi: 10.1038/oby.2003.203 [DOI] [PubMed] [Google Scholar]
- 50.Dugan N, Thompson KJ, Barbat S, et al. Male gender is an independent risk factor for patients undergoing laparoscopic sleeve gastrectomy or Roux-en-Y gastric bypass: an MBSAQIP database analysis. Surg Endosc. 2020;34(8):3574-3583. doi: 10.1007/s00464-019-07106-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cottam S, Cottam D, Cottam A. Sleeve gastrectomy weight loss and the preoperative and postoperative predictors: a systematic review. Obes Surg. 2019;29(4):1388-1396. doi: 10.1007/s11695-018-03666-7 [DOI] [PubMed] [Google Scholar]
- 52.Bal J, Ilonzo N, Adediji T, Leitman IM. Gender as a deterministic factor in procedure selection and outcomes in bariatric surgery. JSLS. 2021;25(1):e2020.00077. doi: 10.4293/JSLS.2020.00077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cobeta P, Osorio A, Cuadrado-Ayuso M, et al. Sleeve gastrectomy and gastric bypass decrease the carotid intima-media thickness in obese men: association with weight loss, cardiovascular risk factors, and circulating testosterone. Obes Surg. 2020;30(3):851-859. doi: 10.1007/s11695-020-04405-7 [DOI] [PubMed] [Google Scholar]
- 54.Gómez-Martin JM, Balsa JA, Aracil E, et al. Circulating adiponectin increases in obese women after sleeve gastrectomy or gastric bypass driving beneficial metabolic changes but with no relationship with carotid intima-media thickness. Clin Nutr. 2018;37(6 Pt A):2102-2106. doi: 10.1016/j.clnu.2017.10.003 [DOI] [PubMed] [Google Scholar]
- 55.Hecht LM, Pester B, Braciszewski JM, et al. Socioeconomic and racial disparities in bariatric surgery. Obes Surg. 2020;30(6):2445-2449. doi: 10.1007/s11695-020-04394-7 [DOI] [PubMed] [Google Scholar]
- 56.Hui BY, Roberts A, Thompson KJ, et al. Outcomes of bariatric surgery in African Americans: an analysis of the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) data registry. Obes Surg. 2020;30(11):4275-4285. doi: 10.1007/s11695-020-04820-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Istfan N, Anderson WA, Apovian C, Ruth M, Carmine B, Hess D. Racial differences in weight loss, hemoglobin A1c, and blood lipid profiles after Roux-en-Y gastric bypass surgery. Surg Obes Relat Dis. 2016;12(7):1329-1336. doi: 10.1016/j.soard.2015.12.028 [DOI] [PubMed] [Google Scholar]
- 58.Mocanu V, Dang JT, Switzer N, Madsen K, Birch DW, Karmali S. Sex and race predict adverse outcomes following bariatric surgery: an MBSAQIP analysis. Obes Surg. 2020;30(3):1093-1101. doi: 10.1007/s11695-020-04395-6 [DOI] [PubMed] [Google Scholar]
- 59.Nguyen GC, Patel AM. Racial disparities in mortality in patients undergoing bariatric surgery in the U.S.A. Obes Surg. 2013;23(10):1508-1514. doi: 10.1007/s11695-013-0957-4 [DOI] [PubMed] [Google Scholar]
- 60.Speed JS, Pruett WA, Lirette ST, Cook JJ, Phillips CL, Grayson BE. Cardiovascular risk factors following vertical sleeve gastrectomy in Black Americans compared with White Americans. Obes Surg. 2021;31(3):1004-10122020. doi: 10.1007/s11695-020-04938-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Thomas DD, Anderson WA, Apovian CM, et al. Weight recidivism after Roux-en-Y gastric bypass surgery: an 11-year experience in a multiethnic medical center. Obesity (Silver Spring). 2019;27(2):217-225. doi: 10.1002/oby.22360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Welsh LK, Luhrs AR, Davalos G, et al. Racial disparities in bariatric surgery complications and mortality using the MBSAQIP data registry. Obes Surg. 2020;30(8):3099-3110. doi: 10.1007/s11695-020-04657-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wood MH, Carlin AM, Ghaferi AA, et al. Association of race with bariatric surgery outcomes. JAMA Surg. 2019;154(5):e190029. doi: 10.1001/jamasurg.2019.0029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kramer CK, Zinman B, Retnakaran R. Are metabolically healthy overweight and obesity benign conditions? a systematic review and meta-analysis. Ann Intern Med. 2013;159(11):758-769. doi: 10.7326/0003-4819-159-11-201312030-00008 [DOI] [PubMed] [Google Scholar]
- 65.Bell JA, Hamer M, Sabia S, Singh-Manoux A, Batty GD, Kivimaki M. The natural course of healthy obesity over 20 years. J Am Coll Cardiol. 2015;65(1):101-102. doi: 10.1016/j.jacc.2014.09.077 [DOI] [PubMed] [Google Scholar]
- 66.Mongraw-Chaffin M, Foster MC, Anderson CAM, et al. Metabolically healthy obesity, transition to metabolic syndrome, and cardiovascular risk. J Am Coll Cardiol. 2018;71(17):1857-1865. doi: 10.1016/j.jacc.2018.02.055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Blaha MJ, Budoff MJ, DeFilippis AP, et al. Associations between C-reactive protein, coronary artery calcium, and cardiovascular events: implications for the JUPITER population from MESA, a population-based cohort study. Lancet. 2011;378(9792):684-692. doi: 10.1016/S0140-6736(11)60784-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Samuel I, Mason EE, Renquist KE, Huang YH, Zimmerman MB, Jamal M. Bariatric surgery trends: an 18-year report from the International Bariatric Surgery Registry. Am J Surg. 2006;192(5):657-662. doi: 10.1016/j.amjsurg.2006.07.006 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Clinical Characteristics Stratified by Sex
eTable 2. Clinical Characteristics Stratified by Race
eTable 3. Clinical Characteristics of Participants With Metabolically Unhealthy Obesity (MUHO) vs Metabolically Healthy Obesity (MHO)
eTable 4. Clinical Characteristics of Participants With Metabolically Unhealthy Obesity (MUHO) vs Metabolically Healthy Obesity (MHO) and High-Sensitivity C-Reactive Protein (hs-CRP) Levels Greater Than 2 mg/dL