Abstract
Purpose:
To assess adherence to the 2015-2020 Dietary Guidelines for Americans and 2018 Physical Activity Guidelines, and identify sociodemographic predictors of adherence among children.
Design:
Cross sectional.
Setting:
Colorado, United States.
Participants:
Children aged 5 (n = 482).
Measures:
Sex, race/ethnicity, maternal education, maternal employment, maternal subjective social status and household income were assessed via questionnaires. Diet was assessed via 2 interviewer-administered 24-hour dietary recalls. Physical activity was objectively-measured with accelerometry for 7 days. Adherence was defined as a Healthy Eating Index-2015 score of ≥70 and/or ≥6 hours/day of light, moderate and vigorous activity.
Analysis:
For each predictor, logistic regression was used to estimate odds ratios for adherence to the diet guidelines only, the activity guidelines only or both guidelines.
Results:
In the full sample, 29% of children were non-adherent to both guidelines, 6% adhered to the dietary guidelines only, 50% adhered to the activity guidelines only and 14% adhered to both. Girls had a 41% lower odds of adhering to the physical activity guidelines than boys (p = 0.01), after adjustment for race/ethnicity, household income and maternal education level, perceived social status and employment status.
Conclusion:
Efforts to improve the health of young children should promote adherence to the Dietary Guidelines for Americans among all children. Targeted interventions that increase physical activity among girls may help to mitigate health disparities.
Keywords: Dietary Guidelines for Americans, Physical Activity Guidelines, young children, health disparities, Healthy Eating Index, sex differences
Purpose
Early childhood is a critical time to develop healthy lifestyle behaviors.1 Dietary intake, physical activity and sedentary behaviors in early childhood have been linked to adiposity, bone and skeletal health, cognitive development, cardiometabolic outcomes and psychological well-being.2–6 Lifestyle behaviors developed in early childhood also provide a foundation for lifestyle behaviors in later life. The types and quantities of foods and nutrients consumed in early childhood show strong tracking into later childhood, adolescence and adulthood,7,8 even after adjustment for age-appropriate increases in energy intake.8 Similarly, physical activity and sedentary behaviors in early childhood track into adolescence.9 Thus, establishing healthy lifestyle behaviors in early childhood has important health implications across the life course.
One indicator of healthy lifestyle behaviors in early childhood is the degree of adherence to age-specific diet and physical activity guidelines.10,11 The 2015-2020 Dietary Guidelines for Americans provide evidence-based recommendations for daily energy, nutrient and food intake to support overall health and reduce the risk of chronic disease.11 Previous studies indicate that adherence to federal dietary guidance is low among young children,12,13 although most of these studies focus on older versions of the guidelines.14,15 The 2018 Physical Activity Guidelines provide recommendations for the type and intensity of physical activity to promote optimal health.10 The 2018 Guidelines are the first to include physical activity recommendations for children under age 6 years10; thus few studies have assessed adherence to federal physical activity guidance in early childhood. Further, no studies have assessed adherence to both the most recent Dietary Guidelines for Americans and Physical Activity Guidelines in a single cohort of children; therefore, the proportion of children who adhere to both guidelines or neither guideline is unknown.
Identifying sociodemographic predictors of adherence to diet and physical activity guidelines among young children is important for preventing health disparities in early life. The recent release of federal physical activity guidance among children under age 6 years10 provides a novel opportunity to investigate sociodemographic factors associated with adherence among children aged 5 and under. For diet, previous studies that evaluated sociodemographic predictors of adherence to the guidelines among young children used older versions of the guidelines, considered only a limited number of sociodemographic predictors, or included children ages 2 to 18 years, but did not disaggregate findings by age.12,16
The objectives of this study among children 5 years of age were to (1) assess adherence to the 2015-2020 Dietary Guidelines for Americans and 2018 Physical Activity Guidelines and (2) identify sociodemographic predictors of adherence. Using data from the Colorado Healthy Start study, we assessed the association between adherence and 6 individual, maternal and household sociodemographic characteristics that have been previously linked to children’s growth and development.17–21 Children were categorized as adherent or not adherent based on their Healthy Eating Index-2015 (HEI-2015) score and time spent in objectively-measured light, moderate and vigorous physical activity. This study is one of the first to examine adherence to federal physical activity guidance in early childhood, and which groups of children are most vulnerable to low adherence. We build on previous studies that described adherence to the dietary guidelines only by investigating the proportion of children who are non-adherent to either guideline or adhere to both guidelines. Our findings will inform the development of health promotion strategies to increase adherence to federal guidance on diet and physical activity among young children, and help policy makers prioritize the most critical areas of concern.
Methods
Design and Sample
We used data from the Healthy Start study, a Colorado prospective pre-birth cohort study that recruited 1410 socioeconomically and ethnically diverse pregnant women from 2009 to 2014 and is currently following offspring postnatally. Healthy Start collected measures of child, maternal and household sociodemographic characteristics, children’s dietary intake and objectively measured physical activity. Women participating in Healthy Start completed research visits during pregnancy and at delivery. Mother-child dyads were invited to participate in a research visit at age 5 years (mean 4.6 years, SD 0.4 years). Children age 5 years were selected as the focus of the study because early intervention is critical in supporting healthy diet and physical activity across the life course, and because there is a gap in the literature related to adherence to the Physical Activity Guidelines and related disparities among children younger than age 6. The Healthy Start study was approved by the Colorado Multiple Institutional Review Board (Protocol #09-0563), and women provided written informed consent for themselves and their offspring.
Measures
Sociodemographic variables.
Sociodemographic data were collected at enrollment, delivery and the 5-year visit. Mothers reported child sex, child race/ethnicity, maternal highest level of education, maternal employment status and annual household income. Maternal perceived social status at the 5-year visit was assessed with the MacArthur Scale of Subjective Social Status.19 The MacArthur Scale includes an image of a 10-rung ladder and respondents are queried about their position on the ladder relative to others in the US.
Diet and physical activity assessments.
At age 5 years, energy intake, nutrient intake and the types of foods and beverages consumed were assessed via 2 interviewer-administered 24-hour dietary recalls (1 weekday, 1 weekend) with mothers as proxy-reporters for children’s intake. Trained staff at the University of North Carolina administered the dietary recalls by phone in English or Spanish. The 24-hour dietary recall, with parents as proxy-reporters for their children, has been validated against doubly labeled water among children age 4-14 years and their parents.22 Doubly labeled water is an objective measure of total daily energy expenditure and is considered to be the gold standard for energy intake estimates in stable weight individuals.23 Dietary data were processed by the University of North Carolina using Nutrition Data System for Research (NDSR) software. At age 5 years, free-living physical activity was objectively measured with a waist-worn Acti-Graph accelerometers (model wGT3X-BT, Pensacola, FL). Accelerometers are a reliable and accurate measure of physical activity among children under free-living conditions.24 Mothers or fathers were trained to use the accelerometers on their child prior to use. Participants were instructed to wear the monitors during waking hours (except swimming/bathing) for the 7 consecutive days following the research visit. Data were collected in 1 second increments at a rate of 30 hertz and converted to vector magnitude-based accelerometer counts expressed as counts per minute using Actilife software. Output files were uploaded into SAS version 9.4 and processed using a modified version of the code developed by the National Cancer Institute.25 Monitor non-wear was identified as 60 consecutive minutes of non-movement with an allowance of up to 2 minutes with movement. Records with at least one day of valid wear were included in the analyses. Valid days were defined as those with ≥8 hours of wear time.26 Accelerometer count-based cut points validated for triaxial actigraph monitor use in preschool children were used (Light: 820 to <3908; Moderate: 3908 to <6112; Vigorous ≥6112).27 Examples of the types of activities for each intensity level include walking slowly or playing catch (light activity), roller skating or riding a bike with light effort (moderate activity) and running or playing in a family soccer game (vigorous activity).
Adherence to the 2015-2020 Dietary Guidelines for Americans.
The Healthy Eating Index-2015 (HEI-2015) was used to estimate children’s degree of adherence to the 2015-2020 Dietary Guidelines for Americans.28 Dietary recall data were used to calculate individual scores on the HEI-2015 per established protocols.28 In the most recent version of the index (HEI-2015), individual diets were scored based on intake of 11 food categories (e.g., total fruit, whole fruits, total vegetables, greens and beans, whole grains, refined grains, dairy, total protein foods, seafood and plant proteins, added sugars, saturated fats); 1 nutrient (sodium) and 1 nutrient ratio (fatty acid ratio). Children received scores between 0 and 100, with higher scores representing better adherence to the 2015-2020 Dietary Guidelines for Americans.28 A density approach (cup or ounce equivalents per 1,000 kcal) was used to compute scores for each HEI-2015 component. The exceptions were fatty acid ratio, which was a unitless measure, and added sugars and saturated fats, which were reported as a percent of total daily energy intake. The HEI-2015 is based on energy-adjusted intake, which accounted for any sex-based differences in energy requirements between boys and girls.
Guided by the approach of Krebs-Smith and colleagues, children with an HEI-2015 score of 70 or greater were categorized as adherent to the Dietary Guidelines for Americans.28 Scores equal to or greater than 70 were considered as adherent, even though they fell short of the maximum score of 100, because HEI-2015 scoring was designed to allow for improvement, even among those with higher adherence to the Guidelines.28
Adherence to the 2018 Physical Activity Guidelines.
The 2018 Physical Activity Guidelines recommended that children aged 3 to 5 years “be physically active throughout the day.”10 In the present study, adherence was defined as greater than or equal to 6 hours per day of activity of any intensity (light, moderate, vigorous).10 This cut-off was based on recommendations in the Scientific Report of the 2018 Physical Activity Guidelines Committee.29 For children aged 5, the Committee concluded that “important public health benefits would result if children, who fall below the median level for device-based measured total physical activity, increased their activity to at least the median” (Part F, Chapter 7, p. 6).29 Median total daily physical activity in Healthy Start at age 5 was just above 6 hours.
Analysis
The eligible cohort for the proposed analysis included mothers and children with complete data on sociodemographic characteristics, dietary intake at the 5-year visit and at least one complete day of accelerometry data at the 5-year visit. Of the 1410 pregnant who were enrolled in Healthy Start prior to 2015, 778 mother-child dyads had returned for the 5-year follow-up visit at the time the current analysis was conducted. Of the 778 dyads, 23% (n = 179) were excluded for missing physical activity data, 8% (n = 66) were excluded for missing dietary data, and 4% (n = 31) were excluded for missing sociodemographic data. Of the 502 dyads with complete data at the 5-year visit, 3% (n = 20) were excluded because the child was age 6 years or older at the time of the visit, and the Physical Activity Guidelines are different for children age 6 years.
Participants were categorized into 4 groups: (1) non-adherent to both guidelines, (2) adherent to 2015-2020 Dietary Guidelines for Americans only, (3) adherent to the 2018 Physical Activity Guidelines only, or (4) adherent to both guidelines. The Cochran-Mantel-Haenszel test30 was used to determine whether group membership was associated with sociodemographic factors. The Cochran-Mantel-Haenszel test30 with modified ridit scores was used to determine whether group membership was associated with income because income is an ordered predictor. Sociodemographic factors included categorized child sex (male or female); child race/ethnicity (Non-Hispanic white [NHW], Hispanic, Black/African American or other); mother’s highest level of education (college degree or no college degree); mother’s employment status (employed or not employed) and annual household income (less than $75,000 or greater than or equal to $75,000). The $75,000 income cut-off was selected based on the income distribution of the study population, and because $75,000 approximates the median household income for the metropolitan area where the study was conducted.31 Mothers who rated their social status as 6 or higher on a scale of 1 to 10 were categorized as higher perceived social status; mothers who rated their social status as 5 or lower were classified as lower perceived social status. For each sociodemographic predictor variable, univariable logistic regression was used to estimate odds ratios and 95% confidence intervals for 3 adherence outcomes: adherence to the dietary guidelines only, adherence to the physical activity guidelines only, or adherence to both guidelines. Multivariable logistic regression was then used to estimate odds ratios for adherence, after adjustment for all other sociodemographic variables. A sensitivity analysis was conducted for those with the standard criteria of at least 3 days of valid accelerometer wear.26 Descriptive statistics were used to describe the distribution of light, moderate and vigorous physical activity and HEI-2015 component scores in the full sample. We fit general linear multivariate models with minutes of light, moderate and vigorous activity as the outcomes. Predictors were limited to the sociodemographic characteristics associated with adherence to the physical activity guidelines (child sex and household income). We used a Hotelling Lawley Trace statistic to assess the association between each sociodemographic characteristic and the pattern of time spent in light, moderate and vigorous physical activity.32
Results
The analytic sample (n = 482) included children with complete data on dietary intake and physical activity at the 5-year visit, and all 6 sociodemographic characteristics. Compared to children in the full Healthy Start sample (n = 1410), a higher proportion of children in the analytic sample had an employed mother, were Non-Hispanic white and were from households with a higher socioeconomic position. Children in the study (mean age 4.6 years) were 46% female and 55% NHW. Forty-nine percent of children were from a household with an income below $75,000/year. Mean BMI z-score at age 5 years was 0.1 (SD 1.0). Among mothers, 74% were employed, 68% did not have a college degree and 36% had a low perceived social status compared to others in the US. Mean days of accelerometer wear was 6 (SD 2). Ninety-two percent of participants had ≥3 valid wear days. Mean hours per day of accelerometer wear was 12.7 (SD 2). Ninety-four percent of participants completed both 24-hour dietary recalls.
In the full sample, 29% of children were non-adherent to both guidelines, 6% adhered to the dietary guidelines only, 50% adhered to the physical activity guidelines only and 14% adhered to both guidelines. Patterns of adherence varied by child sex (p = 0.002) and household income (p = 0.009) (Table 1).
Table 1.
Proportion of Children Who Were Non-Adherent or Adhered to the 2015-2020 DGAs and 2018 Physical Activity Guidelines by Sociodemographic Characteristics Among Children Aged 5 Years in the Colorado Healthy Start Study.
| Proportions from the full sample | Analytic cohort (n = 482) | Non-adherence to both guidelines (29%) | Adherence to the 2015-2020 DGAs only (6%) | Adherence to 2018 Physical Activity Guidelines only (50%) | Adherence to both guidelines (14%) | ||
|---|---|---|---|---|---|---|---|
| Child Characteristics | X2 * | P | |||||
| Sex | |||||||
| Female | 224 | 33% | 8% | 48% | 10% | 9.6 | 0.002 |
| Male | 258 | 26% | 4% | 52% | 18% | ||
| Race/ethnicity | |||||||
| NHW | 263 | 27% | 5% | 54% | 14% | 1.0 | 0.32 |
| Hispanic | 115 | 32% | 9% | 43% | 16% | ||
| Black or African American | 44 | 32% | 2% | 57% | 9% | ||
| Other | 60 | 32% | 8% | 43% | 17% | ||
| Maternal Characteristics | |||||||
| Education level | |||||||
| No college degree | 329 | 32% | 6% | 48% | 14% | 1.6 | 0.2 |
| College degree | 153 | 24% | 7% | 55% | 14% | ||
| Perceived social status compared to others in US | |||||||
| Lower | 172 | 33% | 8% | 49% | 10% | 3.7 | 0.054 |
| Higher | 310 | 27% | 5% | 51% | 16% | ||
| Employment status | |||||||
| Employed | 358 | 29% | 6% | 51% | 14% | 0.003 | 0.95 |
| Not employed | 124 | 31% | 6% | 47% | 16% | ||
| Household characteristics Income ($) | |||||||
| <75,000 | 236 | 36% | 6% | 45% | 13% | 6.8 | 0.009 |
| ≥75,000 | 246 | 23% | 7% | 55% | 15% | ||
Cochran-Mantel-Haenszel test to determine if the pattern of adherence varied by sociodemographic factor. For each analysis, the degrees of freedom were equal to 1.
Compared to boys, girls had a 41% lower odds of adhering to the physical activity guidelines (p = 0.01) and a 51% lower odds of adhering to both guidelines (p = 0.01) after adjustment for child race/ethnicity, household income and maternal education level, perceived social status and employment status (Table 2). When the analytic sample was limited to children with at least 3 days of valid accelerometer wear (n = 446), these associations remained significant for adherence to the physical activity guidelines (p = 0.001) and adherence to both guidelines (p = 0.006). Compared to children from higher income households, children from lower income households had a 41% lower odds of adhering to the physical activity guidelines (p = 0.007), although this difference did not remain after adjustment for covariates (p = 0.1). There was no significant association between sociodemographic characteristics and adherence to the dietary guidelines.
Table 2.
Univariable Odds Ratios and 95% CIs for Sociodemographic Predictors of Adherence to the 2015-2020 DGAs and the 2018 Physical Activity Guidelines Among Children Aged 5 Years in the Colorado Healthy Start Study (n = 482).
| 2015-2020 DGAs |
2018 Physical Activity Guidelines |
Adherence to both guidelines |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Sociodemographic characteristics | OR | CI | OR | CI | OR | CI | |||
| Sex (ref: male) Female | 0.77 | 0.49 | 1.21 | 0.59** | 0.40 | 0.86 | 0.49** | 0.28 | 0.84 |
| Race/ethnicity (ref: NHW) Ethnic minority | 1.17 | 0.75 | 1.82 | 0.74 | 0.51 | 1.07 | 1.05 | 0.63 | 1.74 |
| Education level (ref: college degree) No college degree | 0.97 | 0.60 | 1.55 | 0.73 | 0.49 | 1.1 | 1.0 | 0.57 | 1.72 |
| Perceived social status (ref: higher perceived status) Lower | 0.78 | 0.49 | 1.26 | 0.73 | 0.50 | 1.08 | 0.59 | 0.34 | 1.05 |
| Employment status (ref: employed) Not employed | 1.18 | 0.72 | 1.93 | 0.91 | 0.60 | 1.39 | 1.21 | 0.69 | 2.14 |
| Household income (ref: > $75,000/year) < $75,000 | 0.84 | 0.54 | 1.31 | 0.59* | 0.41 | 0.87 | 0.83 | 0.5 | 1.38 |
Odds ratio statistically significant in the univariable model.
Odds ratios remained statistically significant after adjustment for all other sociodemographic variables.
On average, time spent in each activity intensity level as a proportion of total daily physical activity was 87% (SD 6) light activity, 10% (SD 4) moderate activity and 3% (SD 3) vigorous activity. Mean percent time in each physical activity intensity level is shown in Figure 1 by child sex and household income. Light activity accounted for at least 85% of total daily physical activity among both sexes and both income groups. Mean total daily minutes of physical activity was 386 with an SD of 76. Mean wear time was 762 minutes. The balance of active to sedentary time was 51% versus 49%, respectively. This included 334 (SD 65) minutes of light activity, 41 (SD 18) minutes of moderate activity and 11 (SD 9) minutes of vigorous activity. Minutes per day of light, moderate and vigorous activity differed by sex (p < 0.0001) and income (p = 0.007) (Table 3).
Figure 1.
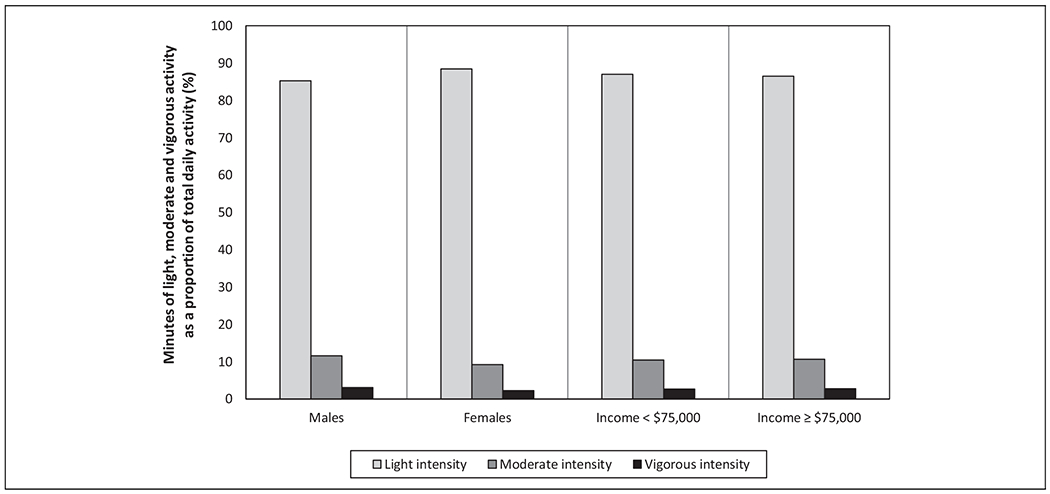
Proportion of total daily physical activity (in minutes/day) spent in different intensities of physical activity by sex and income among children aged 5 years in the Colorado Healthy Start study (n = 482).
Table 3.
Mean (SD) Minutes/Day of Light, Moderate and Vigorous Physical Activity by Sex and Household Income Among Children Aged 5 Years in the Colorado Healthy Start Study (n = 482).
| Sociodemographic characteristics | n | Total daily activity, minutes | Light activity, minutes | Moderate activity, minutes | Vigorous activity, minutes | P* |
|---|---|---|---|---|---|---|
| Sex | ||||||
| Male | 258 | 394.3 (76.9) | 336.2 (66.6) | 45.9 (18.9) | 12.2 (9.2) | <0.0001 |
| Female | 224 | 375.3 (73.3) | 332.1 (63.3) | 34.5 (15.8) | 8.7 (7.5) | |
| Income | ||||||
| <$75,000 | 236 | 373.3 (85.4) | 324.6 (73.1) | 38.7 (19.1) | 10.0 (8.8) | 0.007 |
| ≥$75,000 | 246 | 397.1 (63.3) | 343.6 (54.7) | 42.3 (17.6) | 11.2 (8.3) | |
Hotelling Lawley Trace statistics to evaluate differences in light, moderate and vigorous activity by sex and income.
Mean HEI-2015 score was 60 (SD 12), with a range of 30 to 96. For the 13 dietary components, children were most adherent to the dietary guidelines for whole fruit, total dairy, total protein, total fruit, and added sugar (Figure 2). Adherence was lowest for green and beans, fatty acid ratios and total vegetables.
Figure 2.
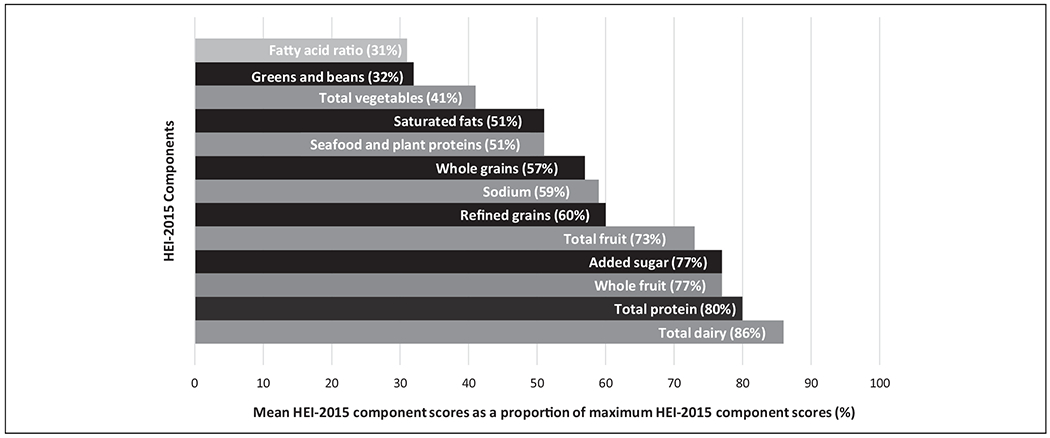
HEI-2015 component scores as a proportion of maximum component scores among children aged 5 years in the Colorado Healthy Start study (n = 482).
Discussion
Among a socioeconomically and ethnically diverse sample of young children in Colorado, we found low adherence to the 2015-2020 Dietary Guidelines for Americans. Only 14% of children adhered to both guidelines, suggesting that most children in this age group could benefit from interventions to improve diet and/or physical activity behaviors. Opportunities for intervention are greatest for saturated fat, vegetable and legume intake, and time spent in moderate and vigorous intensity activity. Adherence to the Physical Activity Guidelines was lowest for girls and children from households with a lower income.
Adherence to the Dietary Guidelines
Mean HEI-2015 score was 60 out of 100 and adherence was highest for the fruit, dairy and total protein components. In contrast, adherence was lowest for greens and beans, total vegetables and saturated fat. These findings confirm what has been reported among nationally representative samples of children in this age group in the US.12,13,33 Thus, efforts to support adherence should focus on maintaining existing habits for fruit, dairy and protein foods, while increasing vegetable and legume intake and decreasing saturated fat intake. For vegetable and legume intake, interventions could target household factors that are barriers to intake, including permissive parent feeding practices, low household availability of vegetables and legumes, and infrequent family meals.34–36 For saturated fat intake, interventions could focus on substituting foods high in saturated fats that are commonly consumed by children, such as fried foods, red meat and cheese,37 with foods high in polyunsaturated and monounsaturated fats, such as fish, avocado and nut butters. Substituting healthier fats may be superior to reducing total fat intake because fat intake among US children generally falls within the Acceptable Macronutrient Distribution Range (20 to 35% of total daily energy)38 and is necessary for healthy growth and development.39 Interventions to improve adherence to the dietary guidelines among young children will likely require a focus on parents and childcare providers because they are primarily responsible for the types and quantities of foods offered to children, mealtime routines, role modeling and other factors associated with children’s eating.40 However, multi-level approaches will be needed to address children’s behaviors, such as “picky eating,” and more distal structural factors (e.g., neighborhood access to nutrient-dense and affordable foods, and regulations for the types of foods offered on “kids’ menus” in restaurants).
In the current study, adherence to the Dietary Guidelines for Americans did not vary by child sex. This lack of variation is consistent with the findings of Thomson et al. which indicated no variation in HEI-2015 score by sex among a nationally representative sample of young children.12 Nevertheless, adherence is a measure of the overall diet that may mask differences in intake of individual food categories. For example, girls tend to score higher on the fruit and vegetable HEI components,33 while boys score higher on total protein component.12 Sex-specific interventions may be needed to increase overall adherence among both boys and girls.
The lack of variation in adherence by income among children participating in Healthy Start is partially consistent with previous studies; some show lower HEI scores among lower income children,33 while others indicate no differences by income.12 Among adults, a positive association between socio-economic status and diet quality is well documented.41 One possible explanation for predictable socioeconomic differentials among adults, but not children, is that disadvantaged children may be buffered from nutritional stress by parents or other community resources that primarily benefit children, such as Head Start or School Breakfast and Lunch programs.42–44
Higher HEI scores have been documented among Hispanic compared to Black or African American children participating in the National Health and Nutrition Examination Survey (NHANES).12,33 Our finding that 9% of Hispanic children adhered to the Dietary Guidelines compared to 2% of Black or African American children is consistent with NHANES, although the differences reported here were not statistically significant. For maternal characteristics, we did not identify differences in diet by education level, perceived social status and employment. Yet, plausible pathways exist between maternal characteristics and children’s diet.45 Therefore, future research should continue to investigate a link between parent-level sociodemographic characteristics and children’s adherence to dietary guidelines.
Adherence to the Physical Activity Guidelines
The finding that children spend 6 to 7 hours per day, on average, in non-sedentary behaviors is higher than the median 3 hours of daily activity observed in other studies among children in preschool within and outside the United States.46 The substantially higher time spent in non-sedentary activities in the current study may be due to the study setting. Colorado has one of the lowest rates of obesity of any US state, and relatively higher rates of physical activity and access to natural amenities that support an active lifestyle.47,48 Differences may also be partially due to the age range of the study population; other studies included preschoolers up to 2 years younger than Healthy Start children. Among preschool-aged children (2-5 years) in the US, Canada, Europe and Australia, total daily physical activity is similarly dominated by light activity, with less than 1 hour per day spent in moderate and vigorous activity.46 The relatively high contribution of light activity is concerning because light activity among young children does not necessarily provide the same health benefits as moderate and vigorous activity.49 Our finding that the children in this cohort spent, on average, 52 minutes per day in moderate to vigorous activity suggests that the transition from age 5 to 6 may merit special consideration. Physical activity recommendations are “physically active throughout the day” at age 5, and at least 1 hour daily of moderate to vigorous activity beginning at age 6.10 The gap between 52 minutes and 60 minutes may appear minor, but there is evidence from European children that the transition from preschool to elementary school results in a decrease in physical activity due to increases in the amount of sedentary time during the school day.50 The change in physical activity guidelines between age 5 and 6 coincides with the age at which most children enter kindergarten. Longitudinal studies are needed to understand how and why physical activity patterns may change during the transition from preschool to elementary school, and how these changes affect adherence to the Physical Activity Guidelines.
Our finding that boys had a higher odds of adhering to the physical activity guidelines compared to girls is consistent with a recent systematic review which concluded that boys are more physically active than girls between birth and age 6.51 Sex differences in physical activity in early childhood are concerning for 2 reasons. First, lower total physical activity among girls may contribute to sex disparities in health outcomes related to physical activity, including obesity, motor skill development, psychosocial health and cardiometabolic health.2 Second, differences in physical activity at age 5 may set the stage for disparities in middle childhood and adolescence, when total daily activity and moderate to vigorous activity are also lower among girls.52,53 Known barriers to physical activity among girls include lower participation in organized sports, less socialization toward physical activity and sports by families, and girls’ concerns about appearing overly masculine.54–56 Additionally, girls may have lower perceived competence in physical education and be less active during school recess.56,57 These barriers may begin early in life via differential development of motor skills across sexes in preschool-aged children (e.g., boys perform better at throwing a ball).58 Many of these barriers are modifiable,59,60 and may therefore be promising intervention targets for reducing sex disparities in adherence to the physical activity guidelines among youth. Nevertheless, future studies should continue to identify barriers to physical activity in preschool-aged girls.
Children from lower income households were less likely to adhere to 2018 Physical Activity Guidelines in the univariate models only. Previous studies among youth indicate that moderate, vigorous and total physical activity were either higher among wealthier children or did not differ by income, although most of these studies used subjective measures of physical activity, focused on children over the age of 5 or were conducted outside the US.61–63 Among families with children, lower household income has been linked to the affordability of organized sports64 and residence in a neighborhood where unsafe streets or playgrounds are a barrier to outdoor play.65 Our finding that adherence to the physical activity guidelines did not vary by maternal employment, education and perceived social status is consistent with previous studies conducted outside the US.66,67
Strengths and Limitations
One strength of this study is that we rigorously assessed adherence to the most recent versions of evidence-based guidance using 2 interviewer-administered dietary recalls and objectively-measured accelerometry collected for 7 days. Another strength of this study is the inclusion of outcomes for both diet and physical activity. This allowed us to identify the proportion of the participants who were non-adherent or adhered to both guidelines. The ethnically and socioeconomically diverse sample, and the finding that mean HEI-2015 score in the Healthy Start population was remarkably similar to what has been reported in nationally representative samples,33 supports the generalizability of findings. Children age 5 were selected as the focus of the study because age 5 may be a critical time in the development of lifestyle behaviors, and thus an important window of opportunity for behavior modification. At this age, children are in a transitional period, in which requirements for moderate and vigorous activity are about to increase, and opportunities for physical activity may decline during the transition from preschool to elementary school. Age 5 may also be a window of opportunity to intervene on diet because children this age are increasingly autonomous in their food selection, and selective, or “picky” eating, is prevalent.
This study has several limitations. First, the cross-sectional design prohibits conclusions about causality because socioeconomic conditions (e.g., household income), diet and physical activity were measured at a single time point. While we cannot establish a temporal relationship between socioeconomic conditions and lifestyle behaviors, there are limited plausible pathways by which children’s lifestyle behaviors could influence household income. Second, dietary recalls are prone to measurement error due to poor recall of past intake or under- or over-estimation of portion sizes. Social desirability bias could inflate diet quality if parents misreport some food types more than others, or misreporting occurs in different directions (e.g., intake of vegetables is over-reported and intake of energydense snack foods is under-reported).68 To minimize these limitations, dietary recalls were administered by trained interviewers who assisted participants in recalling commonly forgotten foods and accurately estimating portion size. Further, the finding that only 6% of children adhered to the dietary guidelines suggests that parents did, in fact, report low intake of recommended foods and high intake of less recommended foods. The scientific community should continue to improve the quality of dietary assessments because accurate estimates of children’s dietary intake are necessary to inform the development of effective nutritional interventions. Third, 3 days of valid accelerometer wear is the standard for estimating usual physical activity habits and 8% of our study population completed less than 3 days. However, we demonstrated that the association between female sex and lower physical activity remained significant among a sub-sample of participants with at least 3 valid days of accelerometer wear. Finally, while the 6-hour cutoff we selected for adherence to the physical activity guidelines is evidence-based,29 this cutoff is higher than the 3 hours of daily physical activity recommended for children aged 5 and under in Australia, the United Kingdom and Canada.10 This limits our ability to compare the adherence levels reported here with adherence levels of among children in other countries.
Conclusion
In a socioeconomically and ethnically diverse sample, only 14% of children aged 5 adhered to both the 2015-2020 Dietary Guidelines for Americans and 2018 Physical Activity Guidelines. Non-adherence to both guidelines appears to be primarily driven by low adherence to the dietary guidelines. This indicates that young children from all sociodemographic groups could benefit from lifestyle behavior interventions, especially for intake of vegetables, legumes and saturated fats. Girls and children from households with lower income in our sample were at greatest risk for low adherence to the 2018 Physical Activity Guidelines. To reduce disparities in adherence to recommended lifestyle behaviors among young children, future studies should develop and test lifestyle interventions, with a specific focus on increasing moderate and vigorous physical activity among girls and children from lower income households.
So What?
What is already known on this topic?
Among children, dietary intake and physical activity levels are associated with growth and development and numerous health outcomes. Sociodemographic variation in dietary intake and physical activity may contribute to preventable health disparities.
What does this article add?
In a socioeconomically and ethnically diverse sample, only 14% of children aged 5 adhered to both the 2015-2020 Dietary Guidelines for Americans and 2018 Physical Activity Guidelines. Girls and children from households with lower income had a higher risk of low adherence to the Physical Activity Guidelines.
What are the implications for health promotion practice or research?
To reduce health disparities among young children, future studies should develop and test lifestyle interventions, with a particular focus on increasing adherence to the Dietary Guidelines among all children in this age group, and increasing time spent in moderate and vigorous physical activity among girls and children from lower income households. Multi-level interventions will be needed that focus on parents and childcare providers, as well as more distal structural factors. Future research to reduce health disparities among children should identify the pathways by which female sex and lower income may influence time spent in moderate and vigorous activity.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Institutes of Health (R01DK076648 and R01GM121081)
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Mollborn S, James-Hawkins L, Lawrence E, Fomby P. Health lifestyles in early childhood. J Health Soc Behav. 2014;55(4):386–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Timmons BW, Leblanc AG, Carson V, et al. Systematic review of physical activity and health in the early years (aged 0-4 years). Appl Physiol Nutr Metab. 2012;37(4):773–792. [DOI] [PubMed] [Google Scholar]
- 3.LeBlanc AG, Spence JC, Carson V, et al. Systematic review of sedentary behaviour and health indicators in the early years (aged 0-4 years). Appl Physiol Nutr Metab. 2012;37(4):753–772. [DOI] [PubMed] [Google Scholar]
- 4.Saeedi P, Shavandi A, Skidmore PML. What do we know about diet and markers of cardiovascular health in children: a review. Int J Environ Res Public Health. 2019;16(4):548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smithers LG, Golley RK, Brazionis L, Lynch JW. Characterizing whole diets of young children from developed countries and the association between diet and health: a systematic review. Nutr Rev. 2011;69(8):449–467. [DOI] [PubMed] [Google Scholar]
- 6.Pate RR, Hillman CH, Janz KF, et al. Physical activity and health in children younger than 6 years: a systematic review. Med Sci Sports Exerc. 2019;51(6):1282–1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Northstone K, Emmett PM. Are dietary patterns stable throughout early and mid-childhood? A birth cohort study. Br J Nutr. 2008;100(5):1069–1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Singer MR, Moore LL, Garrahie EJ, Ellison RC. The tracking of nutrient intake in young children: the Framingham Children’s Study. Am J Public Health. 1995;85(12):1673–1677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Biddle SJ, Pearson N, Ross GM, Braithwaite R. Tracking of sedentary behaviours of young people: a systematic review. Prev Med. 2010;51(5):345–351. [DOI] [PubMed] [Google Scholar]
- 10.Piercy KL, Troiano RP, Ballard RM, et al. The physical activity guidelines for Americans. JAMA. 2018;320(19):2020–2028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.DeSalvo KB, Olson R, Casavale KO. Dietary Guidelines for Americans. JAMA. 2016;315(5):457–458. [DOI] [PubMed] [Google Scholar]
- 12.Thomson JL, Tussing-Humphreys LM, Goodman MH, Landry AS. Diet quality in a nationally representative sample of American children by sociodemographic characteristics. Am J Clin Nutr. 2019;109(1):127–138. [DOI] [PubMed] [Google Scholar]
- 13.Banfield EC, Liu Y, Davis JS, Chang S, Frazier-Wood AC. Poor adherence to US dietary guidelines for children and adolescents in the national health and nutrition examination survey population. J Acad Nutr Diet. 2016;116(1):21–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Haack SA, Byker CJ. Recent population adherence to and knowledge of United States federal nutrition guides, 1992-2013: a systematic review. Nutr Rev. 2014;72(10):613–626. [DOI] [PubMed] [Google Scholar]
- 15.Loth KA, Tate A, Trofholz A, Orlet Fisher J, Neumark-Sztainer D, Berge JM. The contribution of snacking to overall diet intake among an ethnically and racially diverse population of boys and girls. J Acad Nutr Diet. 2019;120(2):270–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kirkpatrick SI, Dodd KW, Reedy J, Krebs-Smith SM. Income and race/ethnicity are associated with adherence to food-based dietary guidance among US adults and children. J Acad Nutr Diet. 2012; 112(5):624–635. e626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sweeting HN. Gendered dimensions of obesity in childhood and adolescence. Nutr J. 2008;7:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Crosnoe R, Dunifon R. A developmental perspective on the link between parents’ employment and children’s obesity. Am Psychol. 2017;72(5):474–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goodman E, Adler NE, Daniels SR, Morrison JA, Slap GB, Dolan LM. Impact of objective and subjective social status on obesity in a biracial cohort of adolescents. Obes Res. 2003;11(8):1018–1026. [DOI] [PubMed] [Google Scholar]
- 20.Ogden CL, Fryar CD, Hales CM, Carroll MD, Aoki Y, Freedman DS. Differences in obesity prevalence by demographics and urbanization in US children and adolescents, 2013-2016. JAMA. 2018; 319(23):2410–2418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ogden CL, Carroll MD, Fakhouri TH, et al. Prevalence of obesity among youths by household income and education level of head of household—United States 2011-2014. MMWR Morb Mortal Wkly Rep. 2018;67(6):186–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Walker JL, Ardouin S, Burrows T. The validity of dietary assessment methods to accurately measure energy intake in children and adolescents who are overweight or obese: a systematic review. Eur J Clin Nutr. 2018;72(2):185–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Westerterp KR. Doubly labelled water assessment of energy expenditure: principle, practice, and promise. Eur J Appl Physiol. 2017;117(7):1277–1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cain KL, Sallis JF, Conway TL, Van Dyck D, Calhoon L. Using accelerometers in youth physical activity studies: a review of methods. J Phys Act Health. 2013;10(3):437–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–188. [DOI] [PubMed] [Google Scholar]
- 26.Hinkley T, O’Connell E, Okely AD, Crawford D, Hesketh K, Salmon J. Assessing volume of accelerometry data for reliability in preschool children. Med Sci Sports Exerc. 2012;44(12):2436–2441. [DOI] [PubMed] [Google Scholar]
- 27.Butte NF, Wong WW, Lee JS, Adolph AL, Puyau MR, Zakeri IF. Prediction of energy expenditure and physical activity in pre-schoolers. Med Sci Sports Exerc. 2014;46(6):1216–1226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Krebs-Smith SM, Pannucci TE, Subar AF, et al. Update of the healthy eating index: HEI-2015. J Acad Nutr Diet. 2018;118(9):1591–1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.2018 Physical Activity Guidelines Advisory Committee. 2018 Physical Activity Guidelines Advisory Committee Scientific Report. U.S. Department of Health and Human Services; 2018. [Google Scholar]
- 30.Mantel N Chi-square tests with one degree of freedom; extensions of the Mantel-Haenszel procedure. J Am Stat Assoc. 1963;58:690–700. [Google Scholar]
- 31.U.S. Census Bureau. American community survey 1-year estimates. Retrieved from Census Reporter Profile page for Denver-Aurora-Lakewood, CO Metro Area: March 1, 2020. https://censusreporter.org/profiles/31000US19740-denver-aurora-lakewood-co-metro-area/2019 [Google Scholar]
- 32.Muller KE, Steward PW. Linear Model Theory: Univariate, Multivariate, and Mixed Models. 1st ed. Wiley-Interscience; 2006. [Google Scholar]
- 33.Hiza HA, Casavale KO, Guenther PM, Davis CA. Diet quality of Americans differs by age, sex, race/ethnicity, income, and education level. J Acad Nutr Diet. 2013;113(2):297–306. [DOI] [PubMed] [Google Scholar]
- 34.Couch SC, Glanz K, Zhou C, Sallis JF, Saelens BE. Home food environment in relation to children’s diet quality and weight status. J Acad Nutr Diet. 2014;114(10):1569–1579. e1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hoerr SL, Hughes SO, Fisher JO, Nicklas TA, Liu Y, Shewchuk RM. Associations among parental feeding styles and children’s food intake in families with limited incomes. Int J Behav Nutr Phys Act. 2009;6:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Haines J, Haycraft E, Lytle L, et al. Nurturing children’s healthy eating: position statement. Appetite. 2019;137:124–133. [DOI] [PubMed] [Google Scholar]
- 37.Keast DR, Fulgoni VL III, Nicklas TA, O’Neil CE. Food sources of energy and nutrients among children in the United States: national health and nutrition examination survey 2003-2006. Nutrients. 2013;5(1):283–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ervin RB, Ogden CL. Trends in intake of energy and macronutrients in children and adolescents from 1999-2000 through 2009-2010. NCHS Data Brief. 2013;(113):1–8. [PubMed] [Google Scholar]
- 39.Lifshitz F, Tarim O. Considerations about dietary fat restrictions for children. J Nutr. 1996;126(4 Suppl):1031S–1041S. [DOI] [PubMed] [Google Scholar]
- 40.Bekelman TA, Bellows LL, Johnson SL. Are family routines modifiable determinants of preschool children’s eating, dietary intake, and growth? A review of intervention studies. Current Nutrition Reports. 2017;2(6):171–189. [Google Scholar]
- 41.Rehm CD, Penalvo JL, Afshin A, Mozaffarian D. Dietary intake among US adults, 1999-2012. JAMA. 2016;315(23):2542–2553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Piperata BA, Schmeer KK, Hadley C, Ritchie-Ewing G. Dietary inequalities of mother-child pairs in the rural Amazon: evidence of maternal-child buffering? Soc Sci Med. 2013;96:183–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ritchie LD, Boyle M, Chandran K, et al. Participation in the child and adult care food program is associated with more nutritious foods and beverages in child care. Child Obes. 2012;8(3):224–229. [DOI] [PubMed] [Google Scholar]
- 44.Vernarelli JA, O’Brien B. A vote for school lunches: school lunches provide superior nutrient quality than lunches obtained from other sources in a nationally representative sample of US children. Nutrients. 2017;9(9):924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.D’Hooge L, Achterberg P, Reeskens T. Mind over matter. The impact of subjective social status on health outcomes and health behaviors. PLoS One. 2018;13(9):e0202489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hnatiuk JA, Salmon J, Hinkley T, Okely AD, Trost S. A review of preschool children’s physical activity and sedentary time using objective measures. Am J Prev Med. 2014;47(4):487–497. [DOI] [PubMed] [Google Scholar]
- 47.Myers CA, Slack T, Martin CK, Broyles ST, Heymsfield SB. Regional disparities in obesity prevalence in the United States: a spatial regime analysis. Obesity (Silver Spring). 2015;23(2):481–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Centers for Disease Control and Prevention. State Indicator Report on Physical Activity. U.S. Department of Health and Human Services; 2014. [Google Scholar]
- 49.Kwon S, Janz KF, Burns TL, Levy SM. Association between light-intensity physical activity and adiposity in childhood. Pediatr Exerc Sci. 2011;23(2):218–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sigmund E, Sigmundova D, El Ansari W. Changes in physical activity in pre-schoolers and first-grade children: longitudinal study in the Czech Republic. Child Care Health Dev. 2009; 35(3):376–382. [DOI] [PubMed] [Google Scholar]
- 51.Bingham DD, Costa S, Hinkley T, Shire KA, Clemes SA, Barber SE. Physical activity during the early years: a systematic review of correlates and determinants. Am J Prev Med. 2016;51(3):384–402. [DOI] [PubMed] [Google Scholar]
- 52.Wolff-Hughes DL, Bassett DR, Fitzhugh EC. Population-referenced percentiles for waist-worn accelerometer-derived total activity counts in U.S. youth: 2003-2006 NHANES. PLoS One. 2014;9(12):e115915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Corder K, Sharp SJ, Atkin AJ, et al. Age-related patterns of vigorous-intensity physical activity in youth: the international children’s accelerometry database. Prev Med Rep. December 2016;4:17–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Allender S, Cowburn G, Foster C. Understanding participation in sport and physical activity among children and adults: a review of qualitative studies. Health Educ Res. 2006;21(6):826–835. [DOI] [PubMed] [Google Scholar]
- 55.Kohl HW III, Hobbs KE. Development of physical activity behaviors among children and adolescents. Pediatrics. March 1998;101(3 Pt 2):549–554. [PubMed] [Google Scholar]
- 56.Telford RM, Telford RD, Olive LS, Cochrane T, Davey R. Why are girls less physically active than boys? Findings from the look longitudinal study. PLoS One. 2016;11(3): e0150041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Shervey SW, DiPerna JC. Engagement in physical activity during recess: gender and grade level differences in the elementary grades. J Phys Act Health. September 2017;14(9):677–683. [DOI] [PubMed] [Google Scholar]
- 58.Saraiva L, Rodrigues LP, Cordovil R, Barreiros J. Influence of age, sex and somatic variables on the motor performance of pre-school children. Ann Hum Biol. 2013;40(5):444–450. [DOI] [PubMed] [Google Scholar]
- 59.Van Capelle A, Broderick CR, van Doorn N, R EW, Parmenter BJ. Interventions to improve fundamental motor skills in pre-school aged children: a systematic review and meta-analysis. J Sci Med Sport. 2017;20(7):658–666. [DOI] [PubMed] [Google Scholar]
- 60.Frost MC, Kuo ES, Harner LT, Landau KR, Baldassar K. Increase in physical activity sustained 1 year after playground intervention. Am J Prev Med. 2018;54(5 Suppl 2): S124–S129. [DOI] [PubMed] [Google Scholar]
- 61.Ferreira I, van der Horst K, Wendel-Vos W, Kremers S, van Lenthe FJ, Brug J. Environmental correlates of physical activity in youth—a review and update. Obes Rev. 2007;8(2):129–154. [DOI] [PubMed] [Google Scholar]
- 62.Love R, Adams J, Atkin A, van Sluijs E. Socioeconomic and ethnic differences in children’s vigorous intensity physical activity: a cross-sectional analysis of the UK Millennium Cohort Study. BMJ Open. 2019;9(5):e027627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.O’Donoghue G, Kennedy A, Puggina A, et al. Socio-economic determinants of physical activity across the life course: a “DEterminants of Diet and Physical ACtivity” (DEDIPAC) umbrella literature review. PLoS One. 2018;13(1):e0190737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Somerset S, Hoare DJ. Barriers to voluntary participation in sport for children: a systematic review. BMC Pediatr. 2018;18(1):47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Chang SH, Kim K. A review of factors limiting physical activity among young children from low-income families. J Exerc Rehabil. 2017;13(4):375–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gwozdz W, Sousa-Poza A, Reisch LA, et al. Maternal employment and childhood obesity—a European perspective. J Health Econ. 2013;32(4):728–742. [DOI] [PubMed] [Google Scholar]
- 67.Sherar LB, Griffin TP, Ekelund U, et al. Association between maternal education and objectively measured physical activity and sedentary time in adolescents. J Epidemiol Community Health. 2016;70(6):541–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Foster E, Bradley J. Methodological considerations and future insights for 24-hour dietary recall assessment in children. Nutr Res. 2018;51:1–11. [DOI] [PubMed] [Google Scholar]


