Key Points
Question
Among pregnant women, what is the association between receipt of BNT162b2 messenger RNA vaccine and risk of SARS-CoV-2 infection?
Findings
In a retrospective cohort study that included 15 060 pregnant women in Israel, vaccination with BNT162b2 vs nonvaccination was associated with an adjusted hazard ratio for incident SARS-CoV-2 infection of 0.22; this was statistically significant.
Meaning
Among pregnant women, receipt of the BNT162b2 vaccine was associated with a lower risk of incident SARS-CoV-2 infection.
Abstract
Importance
Data on BNT162b2 messenger RNA (mRNA) vaccine (Pfizer-BioNTech) effectiveness and safety in pregnancy are currently lacking because pregnant women were excluded from the phase 3 trial.
Objective
To assess the association between receipt of BNT162b2 mRNA vaccine and risk of SARS-CoV-2 infection among pregnant women.
Design, Setting, and Participants
This was a retrospective cohort study within the pregnancy registry of a large state-mandated health care organization in Israel. Pregnant women vaccinated with a first dose from December 19, 2020, through February 28, 2021, were 1:1 matched to unvaccinated women by age, gestational age, residential area, population subgroup, parity, and influenza immunization status. Follow-up ended on April 11, 2021.
Exposures
Exposure was defined by receipt of the BNT162b2 mRNA vaccine. To maintain comparability, nonexposed women who were subsequently vaccinated were censored 10 days after their exposure, along with their matched pair.
Main Outcomes and Measures
The primary outcome was polymerase chain reaction–validated SARS-CoV-2 infection at 28 days or more after the first vaccine dose.
Results
The cohort included 7530 vaccinated and 7530 matched unvaccinated women, 46% and 33% in the second and third trimester, respectively, with a mean age of 31.1 years (SD, 4.9 years). The median follow-up for the primary outcome was 37 days (interquartile range, 21-54 days; range, 0-70). There were 118 SARS-CoV-2 infections in the vaccinated group and 202 in the unvaccinated group. Among infected women, 88 of 105 (83.8%) were symptomatic in the vaccinated group vs 149 of 179 (83.2%) in the unvaccinated group (P ≥ .99). During 28 to 70 days of follow-up, there were 10 infections in the vaccinated group and 46 in the unvaccinated group. The hazards of infection were 0.33% vs 1.64% in the vaccinated and unvaccinated groups, respectively, representing an absolute difference of 1.31% (95% CI, 0.89%-1.74%), with an adjusted hazard ratio of 0.22 (95% CI, 0.11-0.43). Vaccine-related adverse events were reported by 68 patients; none was severe. The most commonly reported symptoms were headache (n = 10, 0.1%), general weakness (n = 8, 0.1%), nonspecified pain (n = 6, <0.1%), and stomachache (n = 5, <0.1%).
Conclusions and Relevance
In this retrospective cohort study of pregnant women, BNT162b2 mRNA vaccination compared with no vaccination was associated with a significantly lower risk of SARS-CoV-2 infection. Interpretation of study findings is limited by the observational design.
This cohort study explores the risk of SARS-CoV-2 infection in pregnant women vaccinated with BNT162b2 vaccine (Pfizer-BioNTech) vs those unvaccinated.
Introduction
During pregnancy, alterations in hormonal levels and immune system function may increase women's vulnerability to viral infections.1 Although SARS-CoV-2 infection in pregnant women is mostly asymptomatic or mild,2,3 it may result in severe complications, including admission to the intensive care unit and mechanical ventilation,4,5 particularly during the third trimester.6 Symptomatic SARS-CoV-2 infections in women also have been linked to a greater likelihood of preterm delivery7,8 and fetal intrapartum distress.9
A phase 3 trial of the Pfizer-BioNTech BNT162b2 messenger RNA (mRNA) vaccine demonstrated 95% efficacy in preventing SARS-CoV-2 infection 7 days from the second dose10; however, pregnant women were excluded from the trial. Association with SARS-CoV-2 infection also has been examined by several observational studies,11,12 but like the clinical trials, none included pregnant women. Although the manufacturer recently announced a phase 2/3 trial among pregnant women,13 there is currently no empirical evidence on the efficacy of the vaccine in this population. Therefore, assessment of vaccine safety and effectiveness in pregnancy can currently be made only by using observational epidemiologic data.
On December 19, 2020, Israel launched its BNT162b2 vaccination campaign. Although pregnant women were not excluded from receiving the vaccine, they were initially advised to discuss the possibility of vaccination with their treating physician. A month into the campaign, the Israel Ministry of Health released updated recommendations encouraging pregnant women to receive the vaccine.14
The purpose of this study was to assess the association between receipt of a BNT162b2 mRNA vaccine and incidence of SARS-CoV-2 infection among pregnant women.
Methods
This retrospective cohort study was approved by the Maccabi Healthcare Services institutional review board and informed consent was waived because only deidentified routinely collected data were used.
Study Population
We used the comprehensive database of the Maccabi Healthcare Services, a 2.5-million-member state-mandated health fund in Israel. Citizens can choose 1 of the 4 nationwide health funds in Israel. The Maccabi health fund members represent 26.7% of the population and share similar sociodemographic characteristics with the overall Israeli population. The fund has maintained a computerized database of electronic health records since 1993, containing extensive longitudinal data on a stable population (≈1% annual turnover).
The health fund has developed several computerized registries of major clinical conditions. These registries are continuously updated and can detect relevant patients by automated criteria (relying on coded diagnoses, extensive laboratory data, treatments, administrative billing codes, etc) rather than depending on active reporting by physicians. Pregnancy data routinely coded by the patient's gynecologist on a designated pregnancy-tracking form within the electronic health record were used to construct a pregnancy registry. In 2020, the fund's pregnancy registry included data on approximately 55 000 new pregnancies, including 40 000 live births, accounting for 24% of all live births in Israel.15
Conception date was calculated according to the last menstrual period. Pregnancy end date was defined by expected delivery date (based on conception date) for ongoing pregnancies and actual delivery date for completed ones. Gestational age was categorized into trimesters defined as less than 14 weeks, 14 to 26 weeks, and 27 weeks or longer.
The eligible study population included all of the health fund's female members who were pregnant at any time from December 19, 2020 (initiation of the national vaccination campaign), through February 28, 2021. Excluded a priori were members who joined the fund less than 1 year preconception, with any preconception records indicating SARS-CoV-2 infection (defined as a positive polymerase chain reaction test result or a hospital diagnosis of SARS-CoV-2 infection), and members who were vaccinated prepregnancy with the BNT162b2 mRNA vaccine.
For each calendar day during the study period, we matched newly vaccinated pregnant women in a 1:1 ratio with eligible women who were unvaccinated on that day and had no prior records indicating a SARS-CoV-2 infection. The index date for the vaccinated woman and her paired control was the calendar date of the vaccinated woman’s first dose. Matching was done (without replacement) by age (up to 5 years), gestational age (up to 5 weeks), exact matching by residential area, population subgroup (nonultra-Orthodox Jewish, ultra-Orthodox Jewish, and Israeli Arab), parity (categorized into nulliparous, para 1, para 2, and more), and having a seasonal influenza vaccine in the current pregnancy (as a proxy for health-seeking behavior). Extreme age was truncated in 4% of the pregnancies eligible for matching to increase eligible matches (<20 to 20; >40 to 40 years).
For each pregnant woman, follow-up lasted from the index date to the earliest occurrence of 1 of the following: an outcome of interest, leaving the fund, or the end of the study period. Matched unvaccinated women who were subsequently vaccinated were censored 10 days after their own first dose date because studies published to date have indicated that no immunity develops during this period16; symmetric censoring occurred on the same date as that of their pair (to maintain balance on matched covariates).
To compare groups, chronic comorbidities were obtained from validated automated registries, including diabetes,17 cardiovascular disease,18 chronic kidney disease,19 hypertension,20 cancer,21 and prediabetes. The latter was defined by at least 1 diagnosis of prediabetes or by abnormal fasting glucose level or hemoglobin A1c level 5.7% or greater, oral glucose tolerance test result 140 mg/dL or greater, at least 2 fasting glucose test results greater than 100 mg/dL, or purchases of diabetic medications during pregnancy. Obesity and infertility were used as adjustment factors. Infertility was defined by infertility diagnoses or medications, ovarian stimulation procedures, or receipt of a donated egg.
Study Outcomes
The primary outcome was documented SARS-CoV-2 infection 28 days or more after the first vaccine dose. This period was chosen because previous analyses10,11 have suggested that immunity develops gradually, reaching full immunity approximately 7 days after the second dose. The number of events between day 28 and the end of follow-up included those occurring on day 28. SARS-CoV-2 infection was defined as a positive real-time polymerase chain reaction test result obtained from nasopharyngeal swabs. The tests are offered free to all Israeli citizens and without a need for referral. Both asymptomatic and symptomatic patients were included.
In addition, the following pregnancy- and birth-related complications were examined as exploratory outcomes: abortions (both spontaneous and induced) defined by diagnoses (International Classification of Diseases, Ninth Revision codes 632-637, 768, and 779) and procedures, intrauterine growth restriction (764), preeclampsia (642.4), stillbirth (V27 and V35), maternal death, obstetric pulmonary embolism (673), birth weight, and gestational age at birth.
In accordance with the Israeli Ministry of Health guidelines, the health fund developed a dedicated short form within its electronic medical record to report adverse events occurring soon after vaccination. The form was open to entry by all physicians and nurses in the health fund and was also pushed as a pop-up window during any visit with a documented diagnosis code of “adverse event SARS-CoV-2 vaccination.”
Forms related to the current study population were manually reviewed by a gynecology specialist to assess the severity and duration of reported events, and to classify them according to timing as related to infection or vaccination, in women who were both infected and vaccinated.
Follow-up for all outcomes continued after pregnancy ended until April 11, 2021.
Statistical Analysis
Descriptive statistics were generated with mean and SD or percentage for continuous and categorical covariates, respectively. Comparisons between vaccinated and nonvaccinated patients were analyzed with analysis of variance or Kruskal-Wallis and χ2 tests for continuous and categorical variables, respectively. Considering the large population size, P values were accompanied by standardized mean differences (the difference between the 2 groups' means divided by the pooled SD), in which a standardized mean difference greater than 0.1 was considered meaningful.
Time to SARS-CoV-2 infection was described with Kaplan-Meier curves and compared with a log-rank test with robust variance estimator22 to account for matching. The cumulative incidence was calculated by 1 minus survival probability. Differences in cumulative incidence rates (risk differences) between the study groups were measured at points at which at least 10% of the matched cohort still remained under follow-up. For the primary outcome, the difference was a subtraction of the cumulative number of events at the end of follow-up minus the cumulative number of events on day 27. CIs for the differences in cumulative incidence rates were calculated with the bootstrap method, based on the 2.5% and 97.5% percentiles of 500 samples drawn from the matched pairs.
Cox regression model was used to estimate adjusted hazard ratios (aHRs) while controlling for parity, population subgroup, trimester, prior children, influenza vaccine, obesity, infertility, and age. Time-varying HRs were used as an estimate of vaccine effectiveness. To validate the time chosen for the primary outcome, nonproportionality over time was tested by exploring Schoenfeld residuals from a time-constant model. The intermediate point (knot) at 10 days was chosen after examination of the residuals plots. Model discrimination was assessed by the C statistic (concordance). The relationship between vaccination and infection was summarized by the aHR during 28 days or more of follow-up. A possible effect modification by trimester at index date was assessed through including in the model an interaction term reflecting HRs that differed by trimester in the post–day 28 period. Wald test of the interaction term within the Cox regression model was used to assess its statistical significance. The crude discrete time hazards were calculated for each period with Kaplan-Meier survival estimates as the survival at the beginning of the period minus survival at the end of it divided by the survival at the beginning of the period. The absolute difference of hazards between the study groups was calculated alongside percentile bootstrap 95% CIs.
Exploratory outcomes and adverse events were analyzed descriptively, without statistical comparisons, given the small numbers.
A sensitivity analysis was performed to exclude vaccinated women (and matched unvaccinated controls) who received their first vaccination dose before the Ministry of Health started recommending that pregnant women receive the vaccine (January 19, 2021) because women who received the vaccine before this date may have constituted a select subgroup who had elevated vulnerability to SARS-CoV-2 infection or complications due to either their occupation (medical or educational staff) or their underlying health status (eg, certain comorbidities).
To assess replicability of the findings, we conducted a sensitivity analysis on the matching process; 5 different matched subcohorts were generated, in which the eligible data set was randomly reordered before each matching iteration. The results were consistent in all iterations. The iteration with the median aHR for 28 days or more of follow-up is presented.
Among infected women, we described the proportion hospitalized in the vaccinated and unvaccinated groups.
Two-sided P < .05 was considered statistically significant.
Statistical analysis was performed with R version 4.0.2 (R Foundation for Statistical Computing).
Results
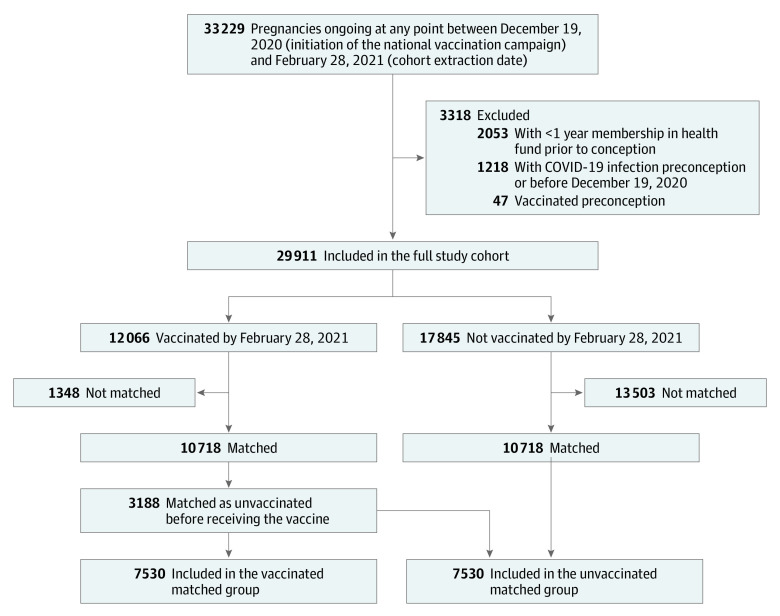
A total of 29 911 eligible pregnant women were identified. By February 28, 2021, 12 066 women had received the first vaccination dose during pregnancy (Figure 1). Among women with a follow-up of 21 days or longer, 5626 (99%) received the second dose by the end of follow-up, with a mean and median of 21 days between the first and second dose.
Figure 1. Flow of Eligible and Matched Vaccinated and Unvaccinated Pregnant Women.
Of the 12 066 vaccinated women, 10 718 were included in the matched cohort, in which 7530 were classified as vaccinated and the remaining 3188 were matched before their vaccination date and classified as unvaccinated (censored on vaccination date plus 10 days along with their matched pairs). Before matching, vaccinated women were slightly older, had a higher number of prior children, and were less likely to belong to a population minority subgroup compared with unmatched nonvaccinated women (Table 1).
Table 1. Baseline Characteristics of the Eligible Study Population.
| Characteristics | Full cohort | Matcheda cohort | ||||
|---|---|---|---|---|---|---|
| Vaccinated | Unvaccinated | SMDb | Vaccinated | Unvaccinated | SMDb | |
| No. | 12 066 | 17 845 | 7530 | 7530 | ||
| Patient age, mean (SD), y | 31.3 (5.15) | 30.4 (5.53) | 0.16 | 31.1 (5.01) | 31.0 (4.85) | 0.01 |
| Population subgroup,c No. (%) | ||||||
| Jewish, secular | 9867 (81.8) | 13 091 (73.4) | 0.28 | 6162 (81.8) | 6162 (81.8) | <0.001 |
| Ultra-Orthodox | 1891 (15.7) | 3244 (18.2) | 1174 (15.6) | 1174 (15.6) | ||
| Arab | 308 (2.6) | 1510 (8.5) | 194 (2.6) | 194 (2.6) | ||
| Prior children, No. (%) | ||||||
| 0 | 5175 (42.9) | 11 092 (62.2) | 0.39 | 3447 (45.8) | 3447 (45.8) | <0.001 |
| 1 | 3925 (32.5) | 3852 (21.6) | 2369 (31.5) | 2369 (31.5) | ||
| ≥2 | 2966 (24.6) | 2901 (16.3) | 1714 (22.8) | 1714 (22.8) | ||
| Vaccines during current pregnancy, No. (%) | ||||||
| Influenza | 5624 (46.7) | 5285 (29.6) | 0.36 | 3063 (40.7) | 3063 (40.7) | <0.001 |
| Pertussis | 2738 (22.7) | 6456 (36.2) | 0.30 | 3070 (40.8) | 2834 (37.6) | 0.06 |
| Preexisting condition,d No. (%) | ||||||
| Obesity (BMI ≥30) | 1342 (11.1) | 1934 (10.8) | 0.01 | 825 (11.0) | 793 (10.5) | 0.01 |
| Infertilitye | 903 (7.5) | 981 (5.5) | 0.08 | 556 (7.4) | 502 (6.7) | 0.03 |
| Cancer | 137 (1.1) | 145 (0.8) | 0.03 | 93 (1.2) | 58 (0.8) | 0.05 |
| Hypertension | 92 (0.8) | 133 (0.7) | 0.002 | 51 (0.7) | 58 (0.8) | 0.01 |
| Chronic kidney disease | 86 (0.7) | 113 (0.6) | 0.01 | 55 (0.7) | 48 (0.6) | 0.01 |
| Diabetes | 89 (0.7) | 87 (0.5) | 0.03 | 63 (0.8) | 30 (0.4) | 0.06 |
| Prediabetes | 38 (0.3) | 39 (0.2) | 0.02 | 28 (0.4) | 15 (0.2) | 0.03 |
| Cardiovascular disease | 5 (<0.1) | 5 (<0.1) | 0.007 | 2 (<0.1) | 2 (<0.1) | <0.001 |
| Chronic obstructive pulmonary disease | 4 (<0.1) | 4 (<0.1) | 0.006 | 2 (<0.1) | 2 (<0.1) | <0.001 |
Abbreviations: BMI, body mass index; SMD, standardized mean difference. Body mass index is calculated as weight in kilograms divided by height in meters squared.
Matching was done by age, residential area, population subgroup, number of prior children, and having an influenza vaccine in the current pregnancy. Matching design was by risk set (also known as exposure density or rolling cohort); for each calendar date, matched pairs were created among patients who received their first vaccine dose exactly on that date and those who were not yet vaccinated by that date. Matched unvaccinated patients who were subsequently vaccinated were censored 10 days after their own first dose date.
SMD is the difference between the groups' means divided by the pooled SD.
Population subgroup was assessed by enumeration areas (the Israeli census’s smallest unit of analysis), with a high proportion of Jewish Orthodox and Israeli Arab residents according to voting results, spatial presence of religious schools, religious centers such as synagogues or mosques, and other publicly available databases.
Preexisting comorbidities were defined by automated registries according to previously validated codes for inclusion and exclusion criteria (including diagnoses, treatments, and laboratory data).
Infertility was defined by diagnoses or medications, ovarian stimulation procedures, or receipt of donated egg.
Baseline characteristics of the matched 7530 vaccinated women and 7530 unvaccinated ones are depicted in Table 1. The groups were well balanced in terms of member age, gestational age, number of prior children, and population subgroup (which were used for matching). The absolute mean difference in gestational age was 9 days.
There were no missing data.
Infection Cumulative Incidence
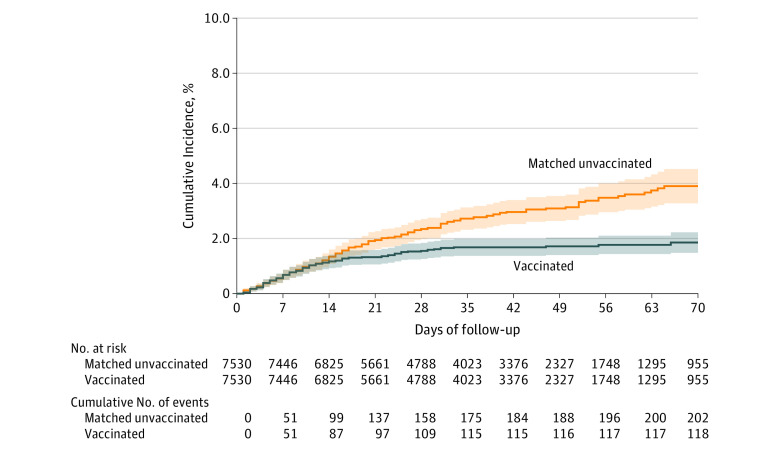
Overall, SARS-CoV-2 infections occurred in 118 vaccinated women and 202 unvaccinated ones during a median follow-up of 37 days (interquartile range, 21-54 days; range, 0-70). Cumulative incidence over time is shown in Figure 2, and the gradually increasing risk difference is depicted in Table 2. At 28 days, when 4788 women (63.6%) remained at follow-up in each group, the absolute cumulative number of events was 109 in the vaccinated group and 158 in the unvaccinated group, and the difference in cumulative incidence rates was 0.80% (95% CI, 0.47%-1.13%), with cumulative incidence rates of 1.55% (95% CI, 1.26%-1.84%) among vaccinated women and 2.34% (95% CI, 1.98%-2.71%) among unvaccinated women. At 10 weeks, when 955 women (12.7%) remained, the cumulative number of events was 118 in the vaccinated group and 202 in the unvaccinated group, and the difference in cumulative incidence rates was higher (2.05%; 95% CI, 1.53%-2.57%), with cumulative incidence rates of 1.85% (95% CI, 1.48%-2.22%) among vaccinated women and 3.90% (95% CI, 3.28%-4.52%) among unvaccinated women.
Figure 2. Cumulative Incidence of SARS-CoV-2 in Vaccinated vs Matched Unvaccinated Pregnant Women.
Kaplan-Meier curves were used for cumulative probability of SARS-CoV-2 infection. Follow-up for each matched pair was initiated simultaneously on the same calendar date for both the vaccinated woman and her control according to the date of the vaccinated woman’s first dose and was censored simultaneously 10 days after vaccination of the matched control to maintain groups' exchangeability over time and avoid selection bias.
Median follow-up time in both groups was 37 days (interquartile range, 21-54 days). P value for statistical comparison was estimated by log-rank test using robust variance estimator to account for matching: P < .001. Shading illustrates 95% CIs. There were no further events from day 70 to end of observation at 110 days.
Table 2. Time-Based Event Rates (%) of SARS-CoV-2 Infections in the Matched Cohort.
| Follow-up, d |
Vaccinated | Unvaccinated | |||||
|---|---|---|---|---|---|---|---|
| Uncensored raw rate a (events/women) | Hazard rate accounting for censoring b | Uncensored raw rate a (events/women) | Hazard rate accounting for censoring b | Absolute difference of hazard rate (95% CI) | Adjusted hazard ratio c (95% CI) | P value | |
| Primary analysis | |||||||
| ≤10 |
0.93 (70/7530) | 0.93 | 0.97 (73/7530) | 0.97 | 0.04 (–0.18 to 0.25) | 0.96 (0.69-1.33) | .79 |
| 11-27 |
0.51 (38/7387) | 0.60 | 1.12 (83/7387) | 1.34 | 0.74 (0.48 to 1.00) | 0.46 (0.31-0.67) | <.001 |
| ≥28d |
0.21 (10/4788) | 0.33 | 0.96 (46/4788) | 1.64 | 1.31 (0.89 to 1.74) | 0.22 (0.11-0.43) | <.001 |
| Post hoc analysis | Women, No. | Cumulative incidence c | Women, No. | Cumulative incidence e | Absolute difference of cumulative incidence (95% CI) | ||
| 10 | 7403 | 0.93 | 7403 | 0.97 | 0.04 (–0.18 to 0.25) | ||
| 27 | 4903 | 1.53 | 4903 | 2.30 | 0.77 (0.54 to 1.12) | ||
| 28 | 4788 | 1.55 | 4788 | 2.34 | 0.80 (0.47 to 1.13) | ||
| 35 | 4023 | 1.68 | 4023 | 2.72 | 1.04 (0.67 to 1.41) | ||
| 42 | 3376 | 1.68 | 3376 | 2.96 | 1.28 (0.87 to 1.65) | ||
| 49 | 2327 | 1.72 | 2327 | 3.09 | 1.37 (0.96 to 1.75) | ||
| 56 | 1748 | 1.77 | 1748 | 3.48 | 1.71 (1.26 to 2.17) | ||
| 63 | 1295 | 1.77 | 1295 | 3.75 | 1.97 (1.46 to 2.47) | ||
| 70 | 955 | 1.85 | 955 | 3.90 | 2.05 (1.53 to 2.57) | ||
Raw rate (not accounting for censoring) was calculated as the number of events during the period divided by the number of women at risk at the beginning of the period.
Hazard rate accounting for censoring for each period was calculated as the survival at the beginning of the period minus survival at the end of it divided by the survival at the beginning of the period. Survival (1 − cumulative incidence) was estimated with the Kaplan-Meier method to account for censoring. The absolute difference of hazards between vaccinated and unvaccinated is reported alongside CIs, which were calculated with the bootstrap percentile method with 500 samples of matched pairs.
Hazard ratio during 28 days or more of follow-up was the primary outcome, calculated with a Cox time-varying hazard model adjusted for population subgroup, maternal age, gestational age, influenza vaccine, number of prior children, infertility, and obesity.
The maximum time of follow-up was 110 days and the median was 37 days (interquartile range, 21-54 days) for both groups.
Cumulative incidence was calculated as 1 minus survival probability at specific days during the follow-up until the maximal point at which at least 10% of the matched cohort remained under follow-up. The difference of cumulative incidence rates between vaccinated and unvaccinated is reported alongside CIs, which were calculated with the bootstrap percentile method with 500 samples of matched pairs.
Infection Hazard
A time-constant covariate was consistent with nonproportionality (Schoenfeld test P = .001), underestimated survival among the vaccinated group, and overestimated survival among the unvaccinated group (eFigure in the Supplement).
A time-varying covariate indicated a risk reduction increasing over time since vaccination (Table 2). There was no significant difference between the groups during the first 10 days postvaccination (aHR = 0.96; 95% CI, 0.69-1.33; P = .79; hazards, 0.93% vs 0.97% in the vaccinated and unvaccinated groups, respectively). A statistically significant hazard reduction was observed among the vaccinated group during 11 to 27 days postvaccination (aHR = 0.46; 95% CI, 0.31-0.67; robust P < .001; hazards, 0.60% vs 1.34% in the vaccinated and unvaccinated groups, respectively).
Primary End Point
During 28 days or more postvaccination, a statistically significant hazard reduction was observed among the vaccinated group compared with the unvaccinated group (aHR = 0.22; 95% CI, 0.11-0.43; robust P < .001) (Table 2). Beginning 28 days after vaccination, 10 and 46 infections were observed in the vaccinated and unvaccinated groups, respectively, including 1 event in the vaccinated group and 2 in the unvaccinated group on day 28, yielding hazards of 0.33% vs 1.64%, respectively, and an absolute difference of 1.31% (95% CI, 0.89%-1.74%).
The adjusted model C statistic was 0.72. The aHRs of the other 4 iterations of randomly matched cohorts were similar (eTable in the Supplement).
Sensitivity analysis excluding women who received their first-dose vaccination before the Ministry of Health recommendations (January 19, 2021) revealed similar results, with aHRs of 0.92 (95% CI, 0.65-1.30), 0.41 (95% CI, 0.27-0.63), and 0.23 (95% CI, 0.11-0.49) for the first 10 days, 11 to 27 days, and 28 days or more after vaccination, respectively. A higher risk of outcome was observed in the second and third trimesters but with no evidence of an interaction (P = .39) between vaccination and trimester at index.
Among infected patients, the presence of symptoms was documented for 105 (89%) and 179 (89%) of the vaccinated and unvaccinated patients, respectively. Among those documented, no significant difference was observed in the proportion of symptomatic patients, with 83.8% vs 83.2% in the vaccinated and nonvaccinated groups, respectively (P ≥ .99).
Exploratory Outcomes
The observed rate of SARS-CoV-2–related hospitalizations was 0.2% among the vaccinated group vs 0.3% among the unvaccinated group (Table 3).
Table 3. Exploratory Outcomesa Among the Matchedb Study Population.
| Outcomes | Vaccinated | Matched unvaccinated |
|---|---|---|
| No. | 7530 | 7530 |
| SARS-CoV-2 hospitalization, No. (%) | 13 (0.2) | 23 (0.3) |
| Abortion,c No. (%) | 128 (1.7) | 118 (1.6) |
| Intrauterine growth restriction, No. (%) | 36 (0.5) | 38 (0.5) |
| Preeclampsia, No. (%) | 20 (0.3) | 21 (0.3) |
| Stillbirth, No. (%) | 1 (<0.1) | 2 (<0.1) |
| Maternal death, No. (%) | 0 | 0 |
| Obstetric pulmonary embolism, No. (%) | 0 | 0 |
| Birth week, median (IQR) | 39 (38-40) | 39 (38-40) |
| Preterm birth (<37 wk), No. (%) | 77/1387 (5.6) | 85/1427 (6.0) |
| Infant weight, median (IQR), kg | 3.2 (2.9-3.6) | 3.2 (2.9-3.5) |
Abbreviation: IQR, interquartile range.
The median follow-up was 37 days (IQR, 21-54 days) for both groups. Among the unvaccinated group, a total of 60% were ultimately vaccinated, at a median of 16 days (IQR, 7-28 days) from index until receipt of first dose.
Matched by age, gestational age, residential area, population subgroup, number of prior children, and having a seasonal influenza vaccine in the last year.
Either spontaneous or induced abortion.
During the study follow-up period, 1387 (18.4%) of the vaccinated women and 1427 (18.9%) of the unvaccinated reached the end of pregnancy. There were no notable differences between the vaccinated and unvaccinated groups regarding preeclampsia, intrauterine growth restriction, infant birth weight, abortions, stillbirth, maternal death, or pulmonary embolism (Table 3).
Adverse Events
A total of 68 women vaccinated during pregnancy reported possibly vaccine-related adverse events. Three of these women were also infected with SARS-CoV-2 near vaccination; a manual review of their symptoms indicated that they were more likely associated with the infection rather than the vaccine. None of the reports indicated prolonged fever or severe adverse reactions. The commonly reported complaints were headache (n = 10, 0.1%), general weakness (n = 8, 0.1%), stomachache (n = 5, <0.1%), nonspecified pain (n = 6, <0.1%), dizziness (n = 4, <0.1%), and rash (n = 4, <0.1%). Three patients reported eye burning or blurred vision; all symptoms lasted less than 1 day.
Discussion
In this large population-based cohort of pregnant women, BNT162b2 vaccination compared with no vaccination was associated with a significantly lower risk of SARS-CoV-2 infection, although the absolute risk difference was small. As of April 11, 2021, approximately 69% of pregnant women in the health fund had received the first dose of the vaccine.
The aHR of 0.22 (95% CI, 0.11-0.43) at 28 days or more after vaccination corresponded to an estimate of vaccine effectiveness (1 − HR) of 78%. Although this finding suggests that the vaccine was associated with a substantially lower risk among pregnant patients, the magnitude of the risk reduction was slightly lower than reported previously among the general population.16 The benefit from the vaccine may be somewhat attenuated among this population compared with the general public because pregnant women were generally advised to take extra precautions during the pandemic and to maintain particular adherence to social distancing guidelines, regardless of vaccination status. Immunologic response may also be different among pregnant women compared with the general population. In Israel, the second half of February and March were characterized by lower infection rates in the overall population (regardless of pregnancy) related to a prolonged lockdown and a substantial increase in vaccine coverage among the general population. Increased herd immunity protects both vaccinated and nonvaccinated pregnant women and could attenuate the observed treatment effect over time, as previously reported with cholera vaccines.23 Moreover, during the same period there was increased media attention in Israel to SARS-CoV-2 complications, specifically among pregnant women (including reports of pregnant women hospitalized for severe SARS-CoV-2 complications, as well as the stillbirth of a fetus infected by SARS-CoV-2), which not only led to a rapid increase in vaccination among this population but also may have increased adherence to social distancing recommendations among unvaccinated pregnant women.
The strengths of this analysis include the use of a very large cohort with detailed demographic and clinical information on vaccination status, SARS-CoV-2 infection, and other comorbidities. The matching process and the lack of association with vaccination during the first 10 days after the first dose suggest that the results are minimally affected by bias.
Limitations
This study has several limitations. First, given the observational design, there is the potential for important unmeasured residual confounding. Given the small absolute risk differences, residual bias may account for significant findings. Second, the reported nominal level of P values from the time-varying model may be underestimated because the placement of knots was data driven, derived from examination of residuals from an initial model that assumed a constant HR. In light of the small P value for the results and that the observed change points are similar to those previously reported for the effect of the vaccine,10,11,16 the study findings are likely robust to this sequential inference. Third, the findings are susceptible to bias if women who were unvaccinated were more prone to present for testing than those who were vaccinated because of concerns about their ongoing vulnerability. Fourth, the study design did not provide adequate power to statistically assess differences in adverse events.
Conclusions
In this retrospective cohort study of pregnant women, BNT162b2 mRNA vaccination compared with no vaccination was associated with a significantly lower risk of SARS-CoV-2 infection. Interpretation of study findings is limited by the observational design.
eTable. Time varying hazard ratios (95% CI) of SARS-CoV-2 infections, at 5 different repeatedly matched datasets with random data re-ordering at each iteration
eFigure. Time till SARS-CoV-2 infection, vaccinated pregnant vs. matched unvaccinated, comparison of Kaplan Meier, Cox time-varying and Cox-time constant (proportional hazards) curves
References
- 1.Alberca RW, Pereira NZ, Oliveira LMDS, Gozzi-Silva SC, Sato MN. Pregnancy, viral infection, and COVID-19. Front Immunol. 2020;11:1672. doi: 10.3389/fimmu.2020.01672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Crovetto F, Crispi F, Llurba E, Figueras F, Gómez-Roig MD, Gratacós E. Seroprevalence and presentation of SARS-CoV-2 in pregnancy. Lancet. 2020;396(10250):530-531. doi: 10.1016/S0140-6736(20)31714-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Allotey J, Stallings E, Bonet M, et al. ; PregCOV-19 Living Systematic Review Consortium . Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: living systematic review and meta-analysis. BMJ. 2020;370:m3320. doi: 10.1136/bmj.m3320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ellington S, Strid P, Tong VT, et al. Characteristics of women of reproductive age with laboratory-confirmed SARS-CoV-2 infection by pregnancy status—United States, January 22–June 7, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(25):769-775. doi: 10.15585/mmwr.mm6925a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Collin J, Byström E, Carnahan A, Ahrne M. Public Health Agency of Sweden’s brief report: pregnant and postpartum women with severe acute respiratory syndrome coronavirus 2 infection in intensive care in Sweden. Acta Obstet Gynecol Scand. 2020;99(7):819-822. doi: 10.1111/aogs.13901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pierce-Williams RAM, Burd J, Felder L, et al. Clinical course of severe and critical coronavirus disease 2019 in hospitalized pregnancies: a United States cohort study. Am J Obstet Gynecol MFM. 2020;2(3):100134. doi: 10.1016/j.ajogmf.2020.100134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Savasi VM, Parisi F, Patanè L, et al. Clinical findings and disease severity in hospitalized pregnant women with coronavirus disease 2019 (COVID-19). Obstet Gynecol. 2020;136(2):252-258. doi: 10.1097/AOG.0000000000003979 [DOI] [PubMed] [Google Scholar]
- 8.Knight M, Bunch K, Vousden N, et al. ; UK Obstetric Surveillance System SARS-CoV-2 Infection in Pregnancy Collaborative Group . Characteristics and outcomes of pregnant women admitted to hospital with confirmed SARS-CoV-2 infection in UK: national population based cohort study. BMJ. 2020;369:m2107. doi: 10.1136/bmj.m2107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liang H, Acharya G. Novel corona virus disease (COVID-19) in pregnancy: what clinical recommendations to follow? Acta Obstet Gynecol Scand. 2020;99(4):439-442. doi: 10.1111/aogs.13836 [DOI] [PubMed] [Google Scholar]
- 10.Polack FP, Thomas SJ, Kitchin N, et al. ; C4591001 Clinical Trial Group . Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med. 2020;383(27):2603-2615. doi: 10.1056/NEJMoa2034577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chodick G, Tene L, Patalon T, et al. Assessment of effectiveness of 1 dose of BNT162b2 vaccine for SARS-CoV-2 infection 13 to 24 days after immunization. JAMA Netw Open. 2021;4(6):e2115985-e2115985. doi: 10.1001/jamanetworkopen.2021.15985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rossman H, Shilo S, Meir T, Gorfine M, Shalit U, Segal E. COVID-19 dynamics after a national immunization program in Israel. Nat Med. 2021;27(6):1055-1061. doi: 10.1038/s41591-021-01337-2 [DOI] [PubMed] [Google Scholar]
- 13.GlobeNewswire. Pfizer and BioNTech commence global clinical trial to evaluate COVID-19 vaccine in pregnant women. Accessed February 19, 2021. https://www.globenewswire.com/news-release/2021/02/18/2178392/0/en/Pfizer-and-BioNTech-Commence-Global-Clinical-Trial-to-Evaluate-COVID-19-Vaccine-in-Pregnant-Women.html
- 14.Israeli Ministry of Health . Vaccination recommendation for high-risk pregnant women. Article in Hebrew. Accessed February 19, 2021. https://www.gov.il/he/departments/news/19012021-05
- 15.National Insurance Institute of Israel . Capitation tables. Article in Hebrew. Accessed March 1, 2021. https://www.btl.gov.il/Mediniyut/Situation/haveruth1/2021/Pages/capitatia_022021.aspx
- 16.Dagan N, Barda N, Kepten E, et al. BNT162b2 mRNA Covid-19 vaccine in a nationwide mass vaccination setting. N Engl J Med. 2021;384(15):1412-1423. doi: 10.1056/NEJMoa2101765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chodick G, Heymann AD, Shalev V, Kookia E. The epidemiology of diabetes in a large Israeli HMO. Eur J Epidemiol. 2003;18(12):1143-1146. doi: 10.1023/B:EJEP.0000006635.36802.c8 [DOI] [PubMed] [Google Scholar]
- 18.Shalev V, Chodick G, Goren I, Silber H, Kokia E, Heymann AD. The use of an automated patient registry to manage and monitor cardiovascular conditions and related outcomes in a large health organization. Int J Cardiol. 2011;152(3):345-349. doi: 10.1016/j.ijcard.2010.08.002 [DOI] [PubMed] [Google Scholar]
- 19.Coresh J, Turin TC, Matsushita K, et al. Decline in estimated glomerular filtration rate and subsequent risk of end-stage renal disease and mortality. JAMA. 2014;311(24):2518-2531. doi: 10.1001/jama.2014.6634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Weitzman D, Chodick G, Shalev V, Grossman C, Grossman E. Prevalence and factors associated with resistant hypertension in a large health maintenance organization in Israel. Hypertension. 2014;64(3):501-507. doi: 10.1161/HYPERTENSIONAHA.114.03718 [DOI] [PubMed] [Google Scholar]
- 21.Israel Center for Disease Control . Israel national cancer registry. State of Israel Ministry of Health. Accessed February 19, 2021. https://www.health.gov.il/English/MinistryUnits/HealthDivision/Icdc/Icr/Pages/default.aspx
- 22.Borgan Ø. Multiple events per subject. In: Therneau TM, Grambsch PM, eds. Modeling Survival Data: Extending the Cox Model. Springer-Verlag; 2000:169-229. [Google Scholar]
- 23.Ali M, Emch M, von Seidlein L, et al. Herd immunity conferred by killed oral cholera vaccines in Bangladesh: a reanalysis. Lancet. 2005;366(9479):44-49. doi: 10.1016/S0140-6736(05)66550-6 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Time varying hazard ratios (95% CI) of SARS-CoV-2 infections, at 5 different repeatedly matched datasets with random data re-ordering at each iteration
eFigure. Time till SARS-CoV-2 infection, vaccinated pregnant vs. matched unvaccinated, comparison of Kaplan Meier, Cox time-varying and Cox-time constant (proportional hazards) curves