Abstract
Over 50% of young adults (defined as individuals aged 18–25 years) with substance use disorders (SUDs) have at least 1 co-occurring psychiatric disorder, and the presence of co-occurring disorders worsens SUD outcomes. Treatment of both co-occurring psychiatric disorders and SUDs in young adults is imperative for optimal treatment, yet many barriers exist to achieving this goal. We present a series of evidence-informed principles of care for young adults with co-occurring psychiatric disorders derived by a workgroup of experts convened by Boston Medical Center’s Grayken Center for Addiction. The 3 principles are as follows: (1) young adults should receive integrated mental health and addiction care across treatment settings; (2) care should be responsive to the needs of young adults exposed to trauma and other adverse childhood experiences; and (3) treatment programs should regularly assess and respond to the evolving mental health needs, motivations, and treatment goals of young adults with co-occurring disorders. Our guidance for each principle is followed by a review of the evidence supporting that principle, as well as practice considerations for implementation. More research among young adults is critical to identify effective treatments and service systems for those with co-occurring disorders.
Over 50% of young adults (defined as individuals aged 18–25 years) with substance use disorders (SUDs) have at least 1 co-occurring psychiatric disorder.1 When present together, psychiatric disorders and SUDs exacerbate one another, leading to more severe symptoms, lower treatment engagement and response, higher rates of relapse for both conditions, and worse prognoses, including a higher risk of suicide.2–4 Most psychiatric disorders begin by young adulthood5 and increase the risk of subsequent SUD development and persistence.6 Although successful treatment of childhood psychiatric disorders including attention-deficit/hyperactivity disorder, depression, and anxiety may mitigate some of this risk,7–10 most young adults with psychiatric conditions go untreated.4,11
The association between psychiatric disorders and SUD also works in reverse: substance use can precipitate development of psychiatric symptoms. Rapid neuroanatomical and neurochemical maturation occurs during young adulthood, with corresponding cognitive, social, and emotional changes.12 The transition to adulthood marks a time of biological vulnerability to the detrimental effects of substances. Substance use may impact critical developmental processes and predispose young adults to neuropsychiatric complications, including reduced cognitive function and episodes of psychotic and mood disorders.7,13,14
Adequate treatment of co-occurring psychiatric conditions in young adults is imperative for the optimal treatment of SUDs, and successful SUD treatment is necessary to achieve maximum benefit in treating certain psychiatric conditions. Many barriers, however, exist to delivering high-quality treatment of co-occurring disorders, including those related to system design, provider training and expertise, patient motivation, and lack of evidence-based treatments specific to young adults.
We communicate a series of evidence-informed principles of care for young adults with SUD and co-occurring psychiatric disorders, derived by a workgroup of experts in SUD among young adults, convened by Boston Medical Center’s Grayken Center for Addiction. The workgroup developed 3 principles of care on the topic of co-occurring mental health disorders: (1) young adults should receive integrated mental health and addiction care across treatment settings; (2) care should be responsive to the needs of young adults exposed to trauma and other adverse childhood experiences (ACEs); and (3) treatment programs should regularly assess and respond to the evolving mental health needs, motivations, and treatment goals of young adults with co-occurring disorders. The recommendations in this article are not American Academy of Pediatrics policy, and publication herein does not imply endorsement.
CARE PRINCIPLES
Principle 1: Young Adults Should Receive Integrated Mental Health and Addiction Care Across Treatment Settings
Guidance
The workgroup concluded that recognition of co-occurring psychiatric disorders and SUDs among young adults should inform clinical management. Treatment of co-occurring substance use and psychiatric disorders in young adults should ideally involve a triad of specialists working in conjunction: addiction specialists, mental health clinicians, and medical providers. These clinicians should collaborate both on the care of individual patients and at a systems level.
At the individual level, the working group identified joint treatment planning, care coordination, and regular communication about diagnoses, symptoms, and functional impairment as vital aspects of high-quality SUD care for young adults. The group agreed that treatment planning should consider evolving symptoms and needs and address disruptions of important developmental milestones (eg, academic failure or employment difficulties) that are common sequelae of psychiatric disorders and substance use. The working group noted that care coordination should specifically include assistance with level of care transitions, provider referrals, securing community resources, and addressing other logistic barriers to care. Facilitation of joint treatment planning among providers, patients, caregivers, and nonhealthcare sector personnel is also critical.
At the systems level, the working group determined that collaboration among clinicians should include interdisciplinary case conferences and cross-training to enhance knowledge, build interpersonal and professional connections across settings, and bridge culture divides that can underlie potentially conflicting treatment recommendations. The working group emphasized that clinicians should make every effort to set up systems that do not inadvertently exclude patients with co-occurring disorders from care. Clinicians should establish care delivery workflows based on the setting where patients first present (inpatient, outpatient, or emergency department) to ensure that collaborative, multidisciplinary services and care planning can be established from each setting.
Evidence
McGovern and colleagues proposed the quadrant model (Fig 1) in 2002 as a framework for integrating care for patients whose symptom severity varies along the 2 axes of SUD and psychiatric disorder.15 The proposed integration strategy differs on the basis of the quadrant that best describes the severity of a patient’s psychiatric and addiction symptoms. Initial validity and feasibility studies in adults indicate that the model accurately characterizes patients and their needs.16,17
FIGURE 1.
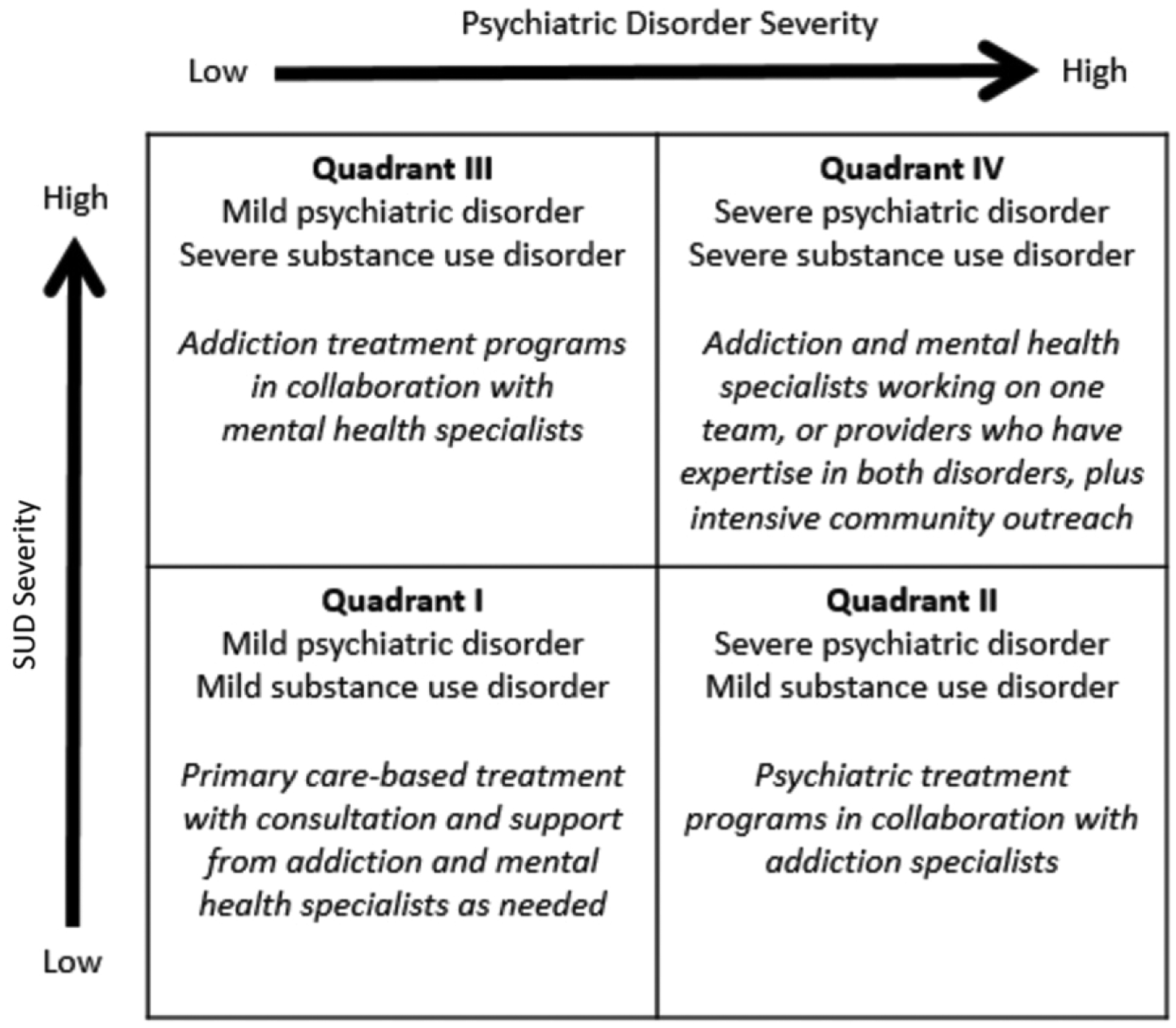
The 4-quadrant model of care for co-occurring substance use and psychiatric disorders adapted from Substance Abuse and Mental Health Services Administration and McGovern et al.15,16
The greatest evidence for integrated care exists for adults with severe mental illness (SMI; defined as chronic, long-term psychiatric disorders18) and SUDs, who fall into quadrants II (SMI plus mild SUD) and IV (SMI plus severe SUD) and receive services largely through mental health agencies. In their 2001 review, Drake et al18 described the evidence supporting dual diagnosis services (in which a single team, usually at a mental health agency, provides care for both disorders) for patients with SUD and SMI. They identified several critical components of these programs (Table 1) supported by results from 8 studies that demonstrated improved outcomes for patients receiving dual diagnosis treatment.18 They also suggested that mental health agencies caring for patients with SMI should designate a clinical leader to ensure availability of dual diagnosis services for patients within the agency. Otherwise, there may be cases in which acute psychiatric treatment may be needed first because of safety concerns, such as acute suicidality or psychosis.19
TABLE 1.
Critical Components of Dual Diagnosis Programs
| Component | Description |
|---|---|
| Intervention staging | Responding to a patient’s needs and motivations as they change over time during a treatment relationship. |
| Assertive outreach | A strategy for engaging patients and their supports in care, typically with home-based outreach and intensive care management. |
| Motivational techniques | Use of motivational interventions to help patients identify their own goals, explore ambivalence, and ultimately recognize that management of their disorder is needed to attain those goals. |
| Therapeutic support | Counseling that includes cognitive and behavioral therapeutic strategies, which can be delivered in single or multiple formats including individual, group, and family. |
| Strengthening social supports | Activities to strengthen the social environment, including those incorporating family or social network interventions. |
| Chronic perspective | Incorporating long-term support for patients through multiple treatment phases including rehabilitation and relapse prevention. |
| Comprehensive services | Integrating services across specialties and domains, including addressing social determinants. |
| Cultural competence | Adapting to cultural and other local circumstances while keeping important evidence-based intervention components. |
Source: Drake et al.18
For patients in quadrant I (mild SUD and mild psychiatric disorder), in which there is likely to be a disproportionate number of adolescents and young adults, an increasing body of literature supports the integration of care for both disorders in the primary care setting, particularly as part of the patient-centered medical home (PCMH).20,21 In the PCMH, the primary care practice coordinates care for patients with chronic conditions across multiple providers and episodes of care.20,21 Evidence reveals that patients are more likely to access psychiatric care when integrated mental health providers conduct evidence-based interventions within primary care or collaborate with off-site mental health providers.21
The collaborative care model has the most evidence for integrating either mental health or SUD treatment within primary care.22 Collaborative care involves a multidisciplinary team of providers (typically a masters-level care manager, specialty mental health provider, and primary care provider) working together to systematically identify and evaluate patients; provide evidence-based treatment using stepped care algorithms; and use patient reported measures to monitor progress and guide next steps.23 Collaborative care improves engagement in care and outcomes for adolescents and young adults with psychiatric disorders,21 and a small body of literature has begun to support its use for individuals with SUDs.21,24,25 Evidence also supports screening young adults and adolescents in primary care for substance use with validated tools such as the CRAFFT (Car, Relax, Alone, Forget, Friends, Trouble),26,27 and for psychiatric symptoms with validated tools such as the 9-item Patient Health Questionnaire.28 The US Preventive Services Task Force recommends screening for substance use in adults when appropriate follow-up services could feasibly be provided (grade “B” recommendation) but found insufficient evidence to make a recommendation on screening adolescents.29,30
For young adults in quadrant III of the quadrant model, there is emerging support for specific strategies, most notably the Adolescent Community Reinforcement Approach (A-CRA).31 Numerous randomized trials among adolescents and young adults have demonstrated the efficacy of the A-CRA, adapted from its adult version, to reduce both SUD and psychiatric symptoms in youth with co-occurring conditions.31 A-CRA is a treatment based on positive reinforcement and operant conditioning principles for reducing substance use. The manualized intervention incorporates treatment strategies for individuals with co-occurring conditions, such as delivering evidence-based therapies for co-occurring conditions and facilitating adherence to psychotropic medication. Some psychopharmacological studies have supported concurrent medication management for co-occurring disorders in the outpatient setting, although the effect of such management varies by condition. For example, among 170 men and women aged 21 to 75 years with co-occurring depression and alcohol dependence, sertraline plus naltrexone led to significantly higher abstinence rates and longer time to relapse.32 However, this is not the case for all conditions and presentations, and some may necessitate sequential treatment. For example, it may be necessary to delay the prescription of controlled medications for a psychiatric condition until an SUD is stabilized (as in the treatment of attention-deficit/hyperactivity disorder among young adults, who are at risk for misuse and diversion of stimulant medication).33,34
Despite the evidence for integrated treatment of co-occurring disorders, mental health and addiction care is still rarely integrated within one system or provider team,20 which can lead to one disorder going undetected and untreated,35 or to conflicting treatment recommendations (eg, peer-support groups such as 12-step programs may discourage patients from taking psychotropic medications,36 and psychiatric treatment programs may require a commitment to abstinence37). When this happens, treatment in either scenario may be rendered less effective. More evidence is needed for specific interventions and systems-level strategies to provide optimally integrated care for adolescent and young adult patients.
Practice Considerations
The PCMH may be an important point of treatment entry for young adults with co-occurring disorders who are particularly difficult to engage in care.4 Many young adults, however, may cease pediatric care without establishing adult primary care and thus have no medical home. This age group is less likely to be insured, have a primary care provider, or receive preventive medical care than any other age group.38,39 In contrast, some young adults and their families who are engaged with pediatric care may resist transitioning to adult services, in part from concern that adult providers may not be as responsive to developmental needs.38,40 Therefore, a specialty addiction or mental health program may step in to coordinate care when a patient has no medical home or during acute episodes requiring higher level care.
PRINCIPLE 2: CARE SHOULD BE RESPONSIVE TO THE NEEDS OF YOUNG ADULTS EXPOSED TO TRAUMA AND OTHER ACES
Guidance
The working group agreed that settings and providers that treat young adults for SUDs should be equipped to provide both trauma-informed and trauma-specific services (Fig 2). Trauma-informed services represent approaches to care that are applied to all patients. These approaches assume that trauma exposure is common and thus an expectation rather than an exception.41 Trauma-specific services are directed at trauma-related distress, symptoms, and impairment42 and are reserved for individuals with trauma-related mental health diagnoses, such as posttraumatic stress disorder (PTSD).
FIGURE 2.
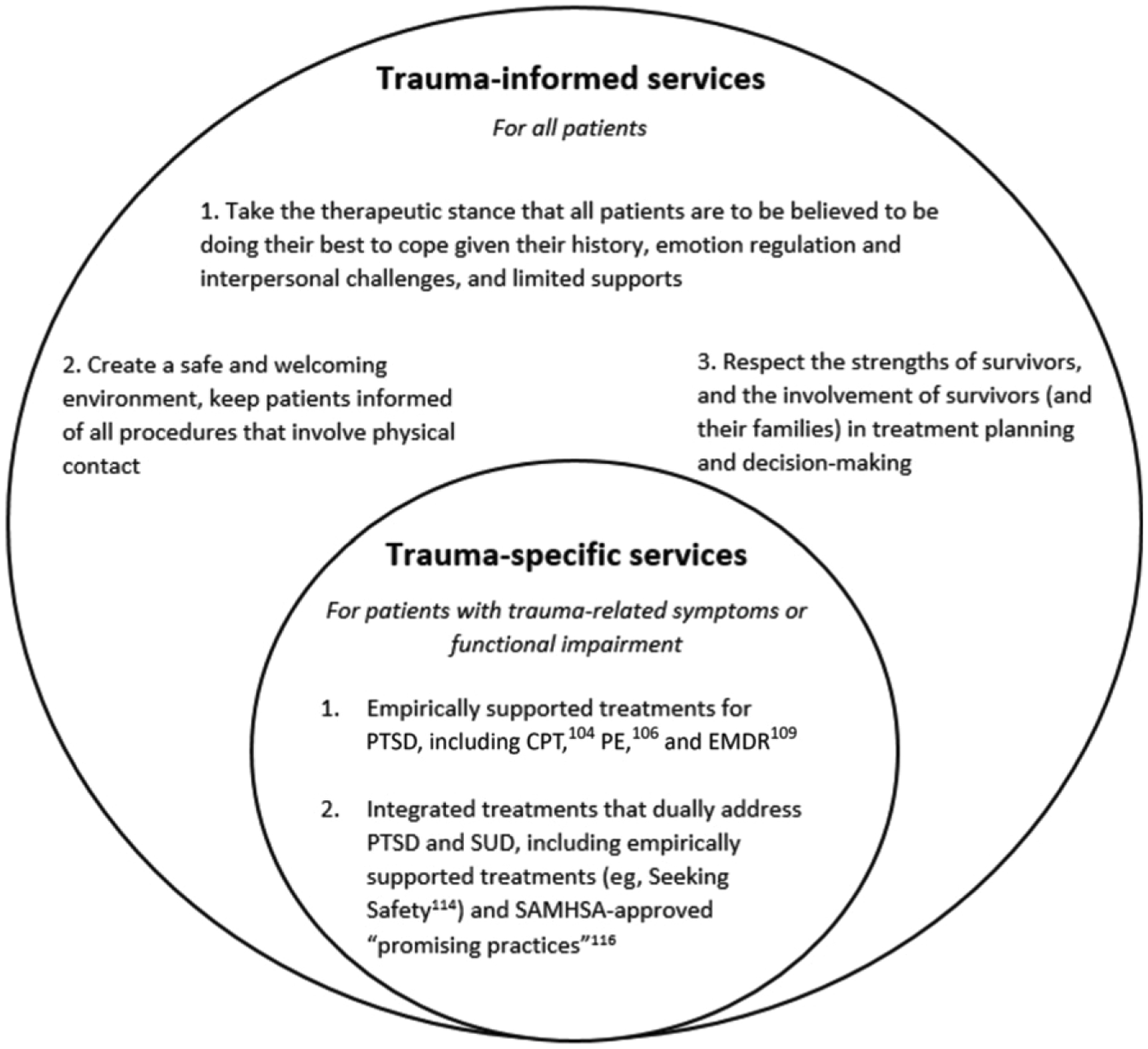
Schematic of trauma-informed and trauma-specific services for young adults with co-occurring substance use and psychiatric disorders. CPT, cognitive processing therapy; EMDR, eye movement desensitization and reprocessing; PE prolonged exposure therapy; SAMHSA, Substance Abuse and Mental Health Services Administration.
Having a history of trauma may make it difficult for some young adults to engage in treatment. Therefore, the working group agreed that repeated assessment of trauma exposure, symptoms, and reactions, as well as safety planning to reduce risk for additional trauma (eg, violence victimization), are critical aspects of quality SUD care for young adults. The working group emphasized that SUD providers should be aware that some aspects of care may produce heightened distress among trauma survivors and lead to treatment disengagement.43
Evidence
Trauma Exposure and ACEs
Trauma and ACEs, including physical or sexual abuse, neglect, or family dysfunction, are common in the general population. However, individuals who use substances are more likely to have been exposed to trauma and other ACEs and are more likely to develop subsequent physical and psychological consequences.44,45 An estimated 75% of adults in substance use treatment report interpersonal abuse and trauma histories.46 Whereas 13% of adults in the general population report exposure to 4 or more ACEs,47,48 84% of those with SUD report such exposure.49 Among the adult population, a dose-response relationship has been documented between number of ACEs and a range of negative health outcomes, including increased risk for SUDs, psychiatric disorders including depression, and suicide attempts.50,51 One study found that adults with 4 ACEs (versus none) were twice as likely to report heavy drinking and 3 times as likely to report alcohol problems in adulthood.52 ACEs and childhood trauma are associated with worse outcomes in substance use treatment, including higher severity of and shorter time to relapse.53–55
Assessment of Trauma History, ACEs, and Related Mental Health Problems
PTSD is one potential mental health consequence of traumatic events. Traumatic events are experiences meeting Criterion A for a diagnosis of PTSD (ie, exposure to life threat, serious injury, or sexual violence).46,56 Standardized tools to assess trauma exposure and related distress have been validated in populations with co-occurring substance use, but evidence suggests that they are seldom implemented in SUD treatment settings.57
Authors of 2 high-quality systematic reviews outline the best assessment tools for PTSD among adults and adolescents,58,59 including the PTSD Checklist for DSM-560 and the Life Events Checklist.61 The Primary Care PTSD Screen49 can be used as a brief screener for PTSD, followed by a diagnostic assessment.58,60 Standardized assessments also exist for ACEs, including the Centers for Disease Control and Prevention–Kaiser Permanente Adverse Childhood Experiences Questionnaire,62 Behavioral Risk Factor Surveillance System (BRFSS) ACE63 items, and the Center for Youth Wellness Adverse Childhood Experience Questionnaire (CYW ACEQ).64,65
Trauma-Informed Services
We are not aware of any randomized studies examining the efficacy of trauma-informed care; thus, our recommendation for trauma-informed services comes from observational data. The absence of data supporting trauma-informed services is largely due a lack of standardization of services or interventions, which leads to an inability to assess causal effects of specified approaches on clinical outcomes66 or to draw comparisons across studies. In practice, trauma-informed care typically involves staff trainings to promote awareness about biases and practice considerations for vulnerable populations. Findings from a systematic review suggest that these trainings improve provider knowledge across a variety of child-serving settings,66 but none has examined patient outcomes. Thus, there is a need to standardize trauma-informed services and test their effect on provider behaviors and patient outcomes.
Trauma-Specific Services
Several efficacy and effectiveness studies have found that treatment of PTSD can reduce substance use but that treating substance use has minimal impact on PTSD symptoms.67 For example, a treatment study in women with dual PTSD-SUD diagnoses found a temporal association between PTSD symptom reduction and number of days of substance use.67 Thus, PTSD-specific treatments may be warranted within substance use programs, and these may include established evidence-based PTSD treatments or dual PTSD-SUD treatments.
There are several evidence-based therapies for PTSD for adolescents and adults, based largely on cognitive behavioral therapy models, and there are several systematic reviews and meta-analyses on psychotherapies for PTSD.68 Common components across evidence-based therapies for PTSD include psychoeducation, relaxation training, exposure, and cognitive restructuring. PTSD treatments with the strongest evidence include cognitive processing therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing. Cognitive processing therapy and prolonged exposure therapy have demonstrated effectiveness for use with adolescent and young adults with PTSD,69,70 but there is scarce evidence on their use for co-occurring PTSD and SUD; only preliminary research exists in dually diagnosed adults.71–74 As an example of how treatments can be tailored for youth and young adults, developmentally adapted cognitive processing therapy includes a preparation phase to enhance motivation, emotion, and behavior management techniques for high risk behaviors, recognition of developmental tasks (ie, education about abusive partners, inclusion of social network), and a massed delivery of sessions (ie, >1 per week) to capitalize on fluctuations in motivation.75
Several integrated treatments have been developed recently to dually target substance use and PTSD symptoms,67 but only Seeking Safety has preliminary evidence for effectiveness with young adults.76 Seeking Safety is a present-focused therapy that focuses on cognitive, behavioral, and interpersonal coping skills and case management needs of clients.77 It can be delivered in individual or group format. Integrated treatment combines cognitive behavioral therapy components from evidence-based treatments for PTSD and SUD (eg, relapse prevention).78 There are several widely used, Substance Abuse and Mental Health Services Administration–approved integrated treatments considered “promising practices” without strong efficacy data.44,45 Programs should consult the National Trauma Consortium guidelines to stay abreast of current best practices.79
There are medications with moderate efficacy for PTSD symptoms but a limited number of studies in individuals with co-occurring disorders.80 The best evidence exists for selective serotonin reuptake inhibitors, which have been shown to reduce PTSD symptoms in adults with co-occurring alcohol use disorder and PTSD.81
Practice Considerations
Trauma survivors report distress in care settings related to themes of trust, safety, and sense of agency. In some cases, clinical experiences (such as physical touch, a provider’s physical appearance, or loud noises) may be reminders of a traumatic event and prompt distress. Therefore, providers should aim to develop trust over time, provide care in an unhurried fashion, talk about procedures before doing them, and validate and normalize concerns.43
Trauma-informed providers and systems may also establish procedures to reduce risk of additional trauma exposure in patients’ lives, especially in the context of familial or dating relationships. This could include addressing housing and financial circumstances that increase vulnerability to victimization or providing psychoeducation on healthy relationships (eg, to improve selection of partners with lower violence risk) and connection to additional community resources (eg, shelters, advocacy groups).
Provider-initiated assessment of trauma history is critical. Providers may be hesitant to ask about trauma because of concerns about upsetting patients or not having resources to offer after disclosure. However, requiring patients to be forthcoming about trauma history is problematic for multiple reasons. First, studies reveal patients are often unaware of the relationship between trauma exposure and current substance use.82 Therefore, patients may not mention past trauma because they do not recognize its relevance. Survivors may also be reluctant to disclose trauma because of shame and guilt, fear of judgment, or concern about resulting family discord.83 Reluctance to disclose trauma or engage in trauma-specific services may also be due to symptoms of PTSD, such as avoidance of the trauma memories and reminders.
For providers who have concerns about patients’ distress during these assessments, the literature provides some reassurance. One study found that even lengthy and sensitive trauma assessments were acceptable to most female subjects surveyed about assessments they had completed for a randomized controlled trial of PTSD treatment.84 Brief upset may occur for some patients but is not counterproductive. For example, Resick et al84 found that those who endorsed greater upset during assessments were more likely to complete PTSD-focused treatment, suggesting it may have facilitated insight-building about the importance of treatment.
PRINCIPLE 3: TREATMENT PROGRAMS SHOULD REGULARLY ASSESS AND RESPOND TO THE EVOLVING MENTAL HEALTH NEEDS, MOTIVATIONS, AND TREATMENT GOALS OF YOUNG ADULTS WITH CO-OCCURRING DISORDERS
Guidance
The working group noted that treatment needs, preferences, and priorities may be particularly dynamic among young adults, changing regularly on the basis of motivation for treatment, support from family and peers, and the evolution and episodic nature of symptoms and severity. Thus, all providers and systems who care for these patients should regularly reassess symptoms and treatment goals and remain attentive to patients’ changing motivations. Use of evidence-based and developmentally informed strategies that promote motivational enhancement and build therapeutic alliance is imperative for the challenge of engaging young adults in care and treatment planning for co-occurring conditions.85 Providers and systems should also work to address barriers to accurate assessment of young adults who may have co-occurring conditions, which include separating symptoms of an existing or emerging psychiatric disorder from sequelae of intoxication or withdrawal; lack of access to expert evaluation because of scarcity of specialists or high cost; and lack of patient motivation for evaluation (eg, due to the perception that evaluation is unnecessary, or to self and social stigma).86
Evidence
Ambivalence regarding behavior change and treatment is expected,87 and young adults face multiple unique barriers to engagement in care. Adolescence marks the beginning of a progression of health care disengagement.88 Young adults have the highest uninsured and unemployment rates in the United States of any age group and, thus, may experience more financial barriers to obtaining treatment.89,90 Adolescents and young adults, particularly males, may also hesitate to disclose symptoms or accept treatment due to fear of public stigma (societal and familial negative attitudes toward addiction and mental health treatment)91 and self stigma (internalized negative feelings toward oneself because of perception of public stigma).92,93 Young adults from immigrant and minority groups face cultural factors that heighten stigma, disparities in health care access and quality, and discrimination, inducing cultural stress and poor trust in health care.94
Therefore, providers should use evidence-based strategies designed to increase engagement in and motivation for care, including motivational interviewing (MI), motivational enhancement therapy (MET), and shared decision-making. MI is a treatment approach based on the stages of change theory that helps patients develop intrinsic motivation to change problematic behaviors.87 Although initially developed to target substance use, MI has shown promise for use with young adults with co-occurring psychiatric and SUD.95,96 For example, researchers in one randomized controlled trial found that an integrated model of MI and cognitive behavioral therapy for young adults with comorbid schizophrenia and SUD led to both reduction in positive symptoms of schizophrenia and an increase in abstinent days over a 12-month period.95 In another randomized study, psychiatrically hospitalized adolescents with co-occurring conditions who were randomly assigned to a 2-session MI intervention versus treatment as usual had both a longer latency to first use as well as less use in 6 months postdischarge.96
MET is another evidence-based technique for the treatment of SUD. MET includes MI plus formalized feedback to the patient on their current substance use42 and moves the young person toward identifying her own goals and values in treatment, desires for change, readiness, and expectations for achieving sobriety. Preliminary evidence suggests that MET could also benefit certain populations of adolescents and young adults with co-occurring disorders.97 For example, over 2 years, researchers in one randomized controlled trial found that adolescents ages 15 to 20 years with comorbid major depressive disorder and alcohol use disorder who received an intervention combining cognitive behavioral therapy and MET had significantly greater reduction in both depressive symptoms and alcohol use disorder compared with those who did not receive the intervention.97
Shared decision-making is an approach for partnering with patients and families to select medical treatments in a patient and family-centered manner, with evidence supporting its use for multiple medical conditions.98 Shared decision-making offers a structured process for collaboratively exploring the potential consequences of treatment options, and for making choices in the context of individual values and preferences.99 Although shared decision-making is a useful concept with evidence in other areas of medicine, there are limited data on its effectiveness in SUDs and mental illness.100 One randomized controlled trial found a reduction in both substance use and psychiatric symptoms with the use of a shared decision-making intervention compared with usual protocols for deciding treatment options.75
Practice Considerations
Developmentally, young adults undergo the major psychological task of recentering,101 referring to the change that individuals experience as their center of self-reference transitions from one of dependence (ie, on parents) to independence.101 During this stage, the young adult shifts from a receiver of guidance to a more independent and collaborative decision-maker. Treatment that is responsive to this developmental milestone by placing young adults at the center of decision-making may be important for engaging young adults with co-occurring disorders in care. At the same time, family and other loved ones can play a critical role in treatment. Providers can engage families by providing information about evidence-based options and orienting them to the importance of motivational approaches and shared decision-making. Families may need support and encouragement to give young adults space and time for weighing decisions, building trust with providers, overcoming stigma, and prioritizing care. Young adults have the authority to decide on the role of family and other loved ones in their care.
CONCLUSIONS
Young adults with co-occurring psychiatric and SUDs present a vulnerable and difficult to engage, yet potentially resilient, population with appropriate treatment. Systems and providers should consider putting in place the necessary steps and supports to detect, monitor, and treat co-occurring conditions. These steps include partnerships with other providers and settings to deliver collaborative care; the use of both trauma-specific and trauma-informed interventions; and continual reassessment of symptoms and goals throughout treatment, facilitated by the use of motivationally-based and shared decision-making strategies. Research specifically with young adults is critical to further identify the most effective treatments for patients in this age group with co-occurring disorders, and how best to implement them.
FUNDING:
Dr Spencer received support from the National Institute of Mental Health (1K23 MH118478) and the Gordon and Betty Moore Foundation (5300). Dr Valentine received support from National Institute of Mental Health (1K23MH117221). Dr Yule received support from NIH grant K12DA000357. The funder/sponsor did not participate in the work. Funded by the National Institutes of Health (NIH).
ABBREVIATIONS
- ACE
adverse childhood experience
- A-CRA
Adolescent Community Reinforcement Approach
- MET
motivational enhancement therapy
- MI
motivational interviewing
- PCMH
patient-centered medical home
- PTSD
posttraumatic stress disorder
- SMI
severe mental illness
- SUD
substance use disorder
Footnotes
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
The guidelines and recommendations in this article are not American Academy of Pediatrics policy, and publication herein does not imply endorsement.
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
REFERENCES
- 1.Center for Behavioral Health Statistics and Quality. 2017 National Survey on Drug Use and Health: Detailed Tables. Substance Abuse and Mental Health Services Administration, Rockville, MD; 2018. Available at: https://www.samhsa.gov/data/nsduh/reports-detailed-tables-2017-NSDUH. Accessed November 18, 2019 [Google Scholar]
- 2.Swendsen J, Conway KP, Degenhardt L, et al. Mental disorders as risk factors for substance use, abuse and dependence: results from the 10-year follow-up of the National Comorbidity Survey. Addiction. 2010;105(6):1117–1128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.White AM, Jordan JD, Schroeder KM, et al. Predictors of relapse during treatment and treatment completion among marijuana-dependent adolescents in an intensive outpatient substance abuse program. Subst Abus. 2004;25(1):53–59 [DOI] [PubMed] [Google Scholar]
- 4.Reavley NJ, Cvetkovski S, Jorm AF, Lubman DI. Help-seeking for substance use, anxiety and affective disorders among young people: results from the 2007 Australian National Survey of Mental Health and Wellbeing. Aust N Z J Psychiatry. 2010;44(8):729–735 [DOI] [PubMed] [Google Scholar]
- 5.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602 [DOI] [PubMed] [Google Scholar]
- 6.Groenman AP, Janssen TWP, Oosterlaan J. Childhood psychiatric disorders as risk factor for subsequent substance abuse: a meta-analysis. J Am Acad Child Adolesc Psychiatry. 2017;56(7):556–569 [DOI] [PubMed] [Google Scholar]
- 7.Curry J, Silva S, Rohde P, et al. Onset of alcohol or substance use disorders following treatment for adolescent depression. J Consult Clin Psychol. 2012;80(2):299–312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Faraone SV, Wilens TE. Effect of stimulant medications for attention-deficit/hyperactivity disorder on later substance use and the potential for stimulant misuse, abuse, and diversion. J Clin Psychiatry. 2007;68(suppl 11):15–22 [PubMed] [Google Scholar]
- 9.Zonnevylle-Bender MJS, Matthys W, van de Wiel NMH, Lochman JE. Preventive effects of treatment of disruptive behavior disorder in middle childhood on substance use and delinquent behavior. J Am Acad Child Adolesc Psychiatry. 2007;46(1):33–39 [DOI] [PubMed] [Google Scholar]
- 10.Puleo CM, Conner BT, Benjamin CL, Kendall PC. CBT for childhood anxiety and substance use at 7.4-year follow-up: a reassessment controlling for known predictors. J Anxiety Disord. 2011;25(5):690–696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Miller S, Ringeisen H, Munoz B, et al. Correlates of mental health service use among young adults with mental illness: results from the national survey on drug use and health. Psychiatr Serv. 2016;67(6):642–649 [DOI] [PubMed] [Google Scholar]
- 12.Squeglia LM, Jacobus J, Tapert SF. The influence of substance use on adolescent brain development. Clin EEG Neurosci. 2009;40(1):31–38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marconi A, Di Forti M, Lewis CM, Murray RM, Vassos E. Meta-analysis of the association between the level of cannabis use and risk of psychosis. Schizophr Bull. 2016;42(5):1262–1269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gibbs M, Winsper C, Marwaha S, Gilbert E, Broome M, Singh SP. Cannabis use and mania symptoms: a systematic review and meta-analysis. J Affect Disord. 2015;171:39–47 [DOI] [PubMed] [Google Scholar]
- 15.Substance Abuse and Mental Health Services Administration. Report to Congress on the Treatment and Prevention of Co-Occurring Substance Abuse and Mental Disorders. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2002 [Google Scholar]
- 16.McGovern MP, Clark RE, Samnaliev M. Co-occurring psychiatric and substance use disorders: a multistate feasibility study of the quadrant model. Psychiatr Serv. 2007;58(7):949–954 [DOI] [PubMed] [Google Scholar]
- 17.McDonell MG, Kerbrat AH, Comtois KA, Russo J, Lowe JM, Ries RK. Validation of the co-occurring disorder quadrant model. J Psychoactive Drugs. 2012;44(3):266–273 [DOI] [PubMed] [Google Scholar]
- 18.Drake RE, Essock SM, Shaner A, et al. Implementing dual diagnosis services for clients with severe mental illness. Psychiatr Serv. 2001;52(4):469–476 [DOI] [PubMed] [Google Scholar]
- 19.Salloum IM, Brown ES. Management of comorbid bipolar disorder and substance use disorders. Am J Drug Alcohol Abuse. 2017;43(4):366–376 [DOI] [PubMed] [Google Scholar]
- 20.Sterling S, Chi F, Hinman A. Integrating care for people with co-occurring alcohol and other drug, medical, and mental health conditions. Alcohol Res Health. 2011;33(4):338–349 [PMC free article] [PubMed] [Google Scholar]
- 21.Asarnow JR, Rozenman M, Wiblin J, Zeltzer L. Integrated medical-behavioral care compared with usual primary care for child and adolescent behavioral health: a meta-analysis. JAMA Pediatr. 2015;169(10):929–937 [DOI] [PubMed] [Google Scholar]
- 22.Goodrich DE, Kilbourne AM, Nord KM, Bauer MS. Mental health collaborative care and its role in primary care settings. Curr Psychiatry Rep. 2013;15(8):383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.American Psychiatric Association. Learn about the collaborative care model. Available at: https://www.psychiatry.org/psychiatrists/practice/professional-interests/integrated-care/get-trained/about-collaborative-care. Accessed February 17, 2019
- 24.Young J, Gilwee J, Holman M, Messier R, Kelly M, Kessler R. Mental health, substance abuse, and health behavior intervention as part of the patient-centered medical home: a case study. Transl Behav Med. 2012;2(3):345–354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alford DP, LaBelle CT, Kretsch N, et al. Five year experience with collaborative care of opioid addicted patients using buprenorphine in primary care. Arch Intern Med. 2011;171(5):425–431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Knight JR, Sherritt L, Shrier LA, Harris SK, Chang G. Validity of the CRAFFT substance abuse screening test among adolescent clinic patients. Arch Pediatr Adolesc Med. 2002;156(6):607–614 [DOI] [PubMed] [Google Scholar]
- 27.Chan Y-F, Huang H, Sieu N, Unützer J. Substance screening and referral for substance abuse treatment in an integrated mental health care program. Psychiatr Serv. 2013;64(1):88–90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.US Preventive Services Task Force. Draft recommendation statement: unhealthy drug use: screening. 2019. https://www.uspreventiveservicestaskforce.org/uspstf/draft-recommendation/drug-use-illicit-screening#fullrecommendationstart. Accessed July 1, 2020
- 30.Salvo N, Bennett K, Cheung A, et al. ; Evidence on Tap Concurrent Disorders Collaborative Team. Prevention of substance use in children/adolescents with mental disorders: a systematic review. J Can Acad Child Adolesc Psychiatry. 2012;21(4):245–252 [PMC free article] [PubMed] [Google Scholar]
- 31.Godley SH, Hunter BD, Fernández-Artamendi S, Smith JE, Meyers RJ, Godley MD. A comparison of treatment outcomes for adolescent community reinforcement approach participants with and without co-occurring problems. J Subst Abuse Treat. 2014;46(4):463–471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pettinati HM, Oslin DW, Kampman KM, et al. A double-blind, placebo-controlled trial combining sertraline and naltrexone for treating co-occurring depression and alcohol dependence. Am J Psychiatry. 2010;167(6):668–675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wilens TE, Gignac M, Swezey A, Monuteaux MC, Biederman J. Characteristics of adolescents and young adults with ADHD who divert or misuse their prescribed medications. J Am Acad Child Adolesc Psychiatry. 2006;45(4):408–414 [DOI] [PubMed] [Google Scholar]
- 34.Posternak MA, Mueller TI. Assessing the risks and benefits of benzodiazepines for anxiety disorders in patients with a history of substance abuse or dependence. Am J Addict. 2001;10(1):48–68 [DOI] [PubMed] [Google Scholar]
- 35.Hu HM, Kline A, Huang FY, Ziedonis DM. Detection of co-occurring mental illness among adult patients in the New Jersey substance abuse treatment system. Am J Public Health. 2006;96(10):1785–1793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Padwa H, Guerrero EG, Braslow JT, Fenwick KM. Barriers to serving clients with co-occurring disorders in a transformed mental health system. Psychiatr Serv. 2015;66(5):547–550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kuehn BM. Integrated care key for patients with both addiction and mental illness. JAMA. 2010;303(19):1905–1907 [DOI] [PubMed] [Google Scholar]
- 38.White PH, Cooley WC, Cooley WC, Sagerman PJ; Transitions Clinical Report Authoring Group; American Academy of Pediatrics; American Academy of Family Physicians; American College of Physicians. Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics. 2018;142(5):e20182587. [DOI] [PubMed] [Google Scholar]
- 39.Adams SH, Park MJ, Irwin CE Jr.. Adolescent and young adult preventive care: comparing national survey rates. Am J Prev Med. 2015;49(2):238–247 [DOI] [PubMed] [Google Scholar]
- 40.Richardson LP, McCarty CA, Radovic A, Suleiman AB. Research in the integration of behavioral health for adolescents and young adults in primary care settings: a systematic review. J Adolesc Health. 2017;60(3):261–269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Clark HW, Power AK. Women, co-occurring disorders, and violence study: a case for trauma-informed care. J Subst Abuse Treat. 2005;28(2):145–146 [DOI] [PubMed] [Google Scholar]
- 42.Serafini K, Decker S, Kiluk BD, et al. Outcome expectations and associated treatment outcomes in motivational enhancement therapy delivered in English and Spanish. Am J Addict. 2015;24(8):732–739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yedidia MJ. Competencies for engaging high-needs patients in primary care. Healthc (Amst). 2018;6(2):122–127 [DOI] [PubMed] [Google Scholar]
- 44.Brady K, Hien DA, Haynes L, Killeen T. Post Traumatic Stress Disorder in Patients with Substance Use Disorders. In: Nunes EV, Levounis P, Davis P, eds. Substance Dependence and Co-Occurring Psychiatric Disorders. Kingston, NJ: Civic Research Institute; 2010:2–27 [Google Scholar]
- 45.Substance Abuse and Mental Health Services Administration. Treatment Improvement Protocol (TIP) Series 57: Trauma-Informed Care in Behavioral Health Services. Rockville, MD: HHS publication No. (SMA) 13–4801; 2014 [PubMed] [Google Scholar]
- 46.Ouimette PC, Kimerling R, Shaw J, Moos RH. Physical and sexual abuse among women and men with substance use disorders. Alcohol Treat Q. 2000;18(3):7–17 [Google Scholar]
- 47.Fothergill KE, Ensminger ME, Green KM, Crum RM, Robertson J, Juon H-S. The impact of early school behavior and educational achievement on adult drug use disorders: a prospective study. Drug Alcohol Depend. 2008;92(1–3):191–199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Centers for Disease Control and Prevention. About the CDC-Kaiser ACE study: major findings. Available at: https://www.cdc.gov/violenceprevention/childabuseandneglect/acestudy/about.html. Accessed March 8, 2019
- 49.Prins A, Ouimette P, Kimerling R, et al. The primary care PTSD screen (PC-PTSD): development and operating characteristics. Prim Care Psychiatry. 2003;9(1):9–14 [Google Scholar]
- 50.Kalmakis KA, Chandler GE. Health consequences of adverse childhood experiences: a systematic review. J Am Assoc Nurse Pract. 2015;27(8):457–465 [DOI] [PubMed] [Google Scholar]
- 51.Austin AE, Shanahan ME, Zvara BJ. Association of childhood abuse and prescription opioid use in early adulthood. Addict Behav. 2018;76:265–269 [DOI] [PubMed] [Google Scholar]
- 52.Dube SR, Anda RF, Felitti VJ, Edwards VJ, Croft JB. Adverse childhood experiences and personal alcohol abuse as an adult. Addict Behav. 2002;27(5):713–725 [DOI] [PubMed] [Google Scholar]
- 53.Cloitre M, Stolbach BC, Herman JL, et al. A developmental approach to complex PTSD: childhood and adult cumulative trauma as predictors of symptom complexity. J Trauma Stress. 2009;22(5):399–408 [DOI] [PubMed] [Google Scholar]
- 54.Curran E, Adamson G, Stringer M, Rosato M, Leavey G. Severity of mental illness as a result of multiple childhood adversities: US National Epidemiologic Survey. Soc Psychiatry Psychiatr Epidemiol. 2016;51(5):647–657 [DOI] [PubMed] [Google Scholar]
- 55.Van Dam NT, Rando K, Potenza MN, Tuit K, Sinha R. Childhood maltreatment, altered limbic neurobiology, and substance use relapse severity via trauma-specific reductions in limbic gray matter volume. JAMA Psychiatry. 2014;71(8):917–925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 3rd ed. Washington, DC: American Psychiatric Association; 2013 [Google Scholar]
- 57.Gielen N, Krumeich A, Havermans RC, Smeets F, Jansen A. Why clinicians do not implement integrated treatment for comorbid substance use disorder and posttraumatic stress disorder: a qualitative study. Eur J Psychotraumatol. 2014;5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lancaster CL, Teeters JB, Gros DF, Back SE. Posttraumatic stress disorder: overview of evidence-based assessment and treatment. J Clin Med. 2016;5(11):105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Leigh E, Yule W, Smith P. Measurement Issues: measurement of posttraumatic stress disorder in children and young people - lessons from research and practice. Child Adolesc Ment Health. 2016;21(2):124–135 [DOI] [PubMed] [Google Scholar]
- 60.Weather F, Blake DD, Schnurr PP, Kaloupek D, Marx B, Keane T. Clinician-administered PTSD scale for DSM-5 (CAPS-5). Available at: https://www.ptsd.va.gov/professional/assessment/adult-int/caps.asp. Accessed February 4, 2019 [DOI] [PMC free article] [PubMed]
- 61.Gray MJ, Litz BT, Hsu JL, Lombardo TW. Psychometric properties of the life events checklist. Assessment. 2004;11(4):330–341 [DOI] [PubMed] [Google Scholar]
- 62.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245–258 [DOI] [PubMed] [Google Scholar]
- 63.Ege MA, Messias E, Thapa PB, Krain LP. Adverse childhood experiences and geriatric depression: results from the 2010 BRFSS. Am J Geriatr Psychiatry. 2015;23(1):110–114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Koita K, Long D, Hessler D, et al. Development and implementation of a pediatric adverse childhood experiences (ACEs) and other determinants of health questionnaire in the pediatric medical home: a pilot study. PLoS One. 2018;13(12):e0208088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Halfon N, Mendonca A, Berkowitz G. Health status of children in foster care. The experience of the Center for the Vulnerable Child. Arch Pediatr Adolesc Med. 1995;149(4):386–392 [DOI] [PubMed] [Google Scholar]
- 66.Hanson RF, Lang J. A critical look at trauma-informed care among agencies and systems serving maltreated youth and their families. Child Maltreat. 2016;21(2):95–100 [DOI] [PubMed] [Google Scholar]
- 67.Hien DA, Jiang H, Campbell ANC, et al. Do treatment improvements in PTSD severity affect substance use outcomes? A secondary analysis from a randomized clinical trial in NIDA’s Clinical Trials Network. Am J Psychiatry. 2010;167(1):95–101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Watkins LE, Sprang KR, Rothbaum BO. Treating PTSD: a review of evidence-based psychotherapy interventions. Front Behav Neurosci. 2018;12:258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Zandberg L, Kaczkurkin AN, McLean CP, Rescorla L, Yadin E, Foa EB. Treatment of adolescent PTSD: the impact of prolonged exposure versus client-centered therapy on co-occurring emotional and behavioral problems. J Trauma Stress. 2016;29(6):507–514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Rosner R, Rimane E, Frick U, et al. Effect of developmentally adapted cognitive processing therapy for youth with symptoms of posttraumatic stress disorder after childhood sexual and physical abuse: a randomized clinical trial. JAMA Psychiatry. 2019;76(5):484–491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Belleau EL, Chin EG, Wanklyn SG, Zambrano-Vazquez L, Schumacher JA, Coffey SF. Pre-treatment predictors of dropout from prolonged exposure therapy in patients with chronic posttraumatic stress disorder and comorbid substance use disorders. Behav Res Ther. 2017;91:43–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Schäfer I, Chuey-Ferrer L, Hofmann A, Lieberman P, Mainusch G, Lotzin A. Effectiveness of EMDR in patients with substance use disorder and comorbid PTSD: study protocol for a randomized controlled trial. BMC Psychiatry. 2017;17(1):95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Markus W, de Weert-van Oene GH, Becker ES, DeJong CAJ. A multi-site randomized study to compare the effects of Eye Movement Desensitization and Reprocessing (EMDR) added to TAU versus TAU to reduce craving and drinking behavior in alcohol dependent outpatients: study protocol. BMC Psychiatry. 2015;15:51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Valiente-Gómez A, Moreno-Alcázar A, Radua J, et al. A multicenter phase II rater-blinded randomized controlled trial to compare the effectiveness of Eye movement desensitization reprocessing therapy vs. treatment as usual in patients with substance use disorder and history of psychological trauma: a study design and protocol. Front Psychiatry. 2019;10:108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Joosten EA, de Jong CA, de Weert-van Oene GH, Sensky T, van der Staak CP. Shared decision-making reduces drug use and psychiatric severity in substance-dependent patients. Psychother Psychosom. 2009;78(4):245–253 [DOI] [PubMed] [Google Scholar]
- 76.Bougard KG, Laupola TMT, Parker-Dias J, Creekmore J, Stangland S. Turning the tides: coping with trauma and addiction through residential adolescent group therapy. J Child Adolesc Psychiatr Nurs. 2016;29(4):196–206 [DOI] [PubMed] [Google Scholar]
- 77.Najavits L Seeking Safety: A Treatment Manual for PTSD and Substance Abuse. New York, NY: Guilford Publications; 2002 [Google Scholar]
- 78.Carroll KM, Rounsaville BJ, Gordon LT, et al. Psychotherapy and pharmacotherapy for ambulatory cocaine abusers. Arch Gen Psychiatry. 1994;51(3):177–187 [DOI] [PubMed] [Google Scholar]
- 79.Finkelstein N, VandeMark N, Fallot R, Brown V, Cadiz S, Heckman J. Enhancing Substance Abuse Recovery through Integrated Trauma Treatment. Sarasota, FL: National Trauma Consortium, Center for Substance Abuse Treatment; 2004 [Google Scholar]
- 80.Verplaetse TL, McKee SA, Petrakis IL. Pharmacotherapy for co-occurring alcohol use disorder and post-traumatic stress disorder: targeting the opioidergic, noradrenergic, serotonergic, and GABAergic/glutamatergic systems. Alcohol Res. 2018;39(2):193–205 [PMC free article] [PubMed] [Google Scholar]
- 81.Hien DA, Levin FR, Ruglass LM, et al. Combining seeking safety with sertraline for PTSD and alcohol use disorders: a randomized controlled trial. J Consult Clin Psychol. 2015;83(2):359–369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Chandler GE, Kalmakis KA, Murtha T. Screening adults with substance use disorder for adverse childhood experiences. J Addict Nurs. 2018;29(3):172–178 [DOI] [PubMed] [Google Scholar]
- 83.Crisma M, Bascelli E, Paci D, Romito P. Adolescents who experienced sexual abuse: fears, needs and impediments to disclosure. Child Abuse Negl. 2004;28(10):1035–1048 [DOI] [PubMed] [Google Scholar]
- 84.Resick PA, Iverson KM, Artz CE. Participant reactions to a pretreatment research assessment during a treatment outcome study for PTSD. J Trauma Stress. 2009;22(4):316–319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Mistler LA, Sheidow AJ, Davis M. Transdiagnostic motivational enhancement therapy to reduce treatment attrition: use in emerging adults. Cognit Behav Pract. 2016;23(3):368–384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Flynn PM, Brown BS. Co-occurring disorders in substance abuse treatment: issues and prospects. J Subst Abuse Treat. 2008;34(1):36–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.DiClemente CC, Corno CM, Graydon MM, Wiprovnick AE, Knoblach DJ. Motivational interviewing, enhancement, and brief interventions over the last decade: a review of reviews of efficacy and effectiveness. Psychol Addict Behav. 2017;31(8):862–887 [DOI] [PubMed] [Google Scholar]
- 88.Rice SM, Purcell R, McGorry PD. Adolescent and young adult male mental health: transforming system failures into proactive models of engagement. J Adolesc Health. 2018;62(suppl 3):S9–S17 [DOI] [PubMed] [Google Scholar]
- 89.Salaheddin K, Mason B. Identifying barriers to mental health help-seeking among young adults in the UK: a cross-sectional survey. Br J Gen Pract. 2016;66(651):e686–e692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.US Census Bureau. Another look at health insurance coverage rates for young adults. 2018. Available at: https://www.census.gov/newsroom/blogs/random-samplings/2018/09/another_look_at_heal.html. Accessed November 8, 2019
- 91.Mason-Jones AJ, Crisp C, Momberg M, Koech J, De Koker P, Mathews C. A systematic review of the role of school-based healthcare in adolescent sexual, reproductive, and mental health. Syst Rev. 2012;1:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Latalova K, Kamaradova D, Prasko J. Perspectives on perceived stigma and self-stigma in adult male patients with depression. Neuropsychiatr Dis Treat. 2014;10:1399–1405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Lynch L, Long M, Moorhead A. Young men, help-seeking, and mental health services: exploring barriers and solutions. Am J Men Health. 2018;12(1):138–149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Alegria M, Carson NJ, Goncalves M, Keefe K. Disparities in treatment for substance use disorders and co-occurring disorders for ethnic/racial minority youth. J Am Acad Child Adolesc Psychiatry. 2011;50(1):22–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Barrowclough C, Haddock G, Wykes T, et al. Integrated motivational interviewing and cognitive behavioural therapy for people with psychosis and comorbid substance misuse: randomised controlled trial. BMJ. 2010;341:c6325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Brown RA, Abrantes AM, Minami H, et al. Motivational interviewing to reduce substance use in adolescents with psychiatric comorbidity. J Subst Abuse Treat. 2015;59:20–29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Cornelius JR, Douaihy A, Bukstein OG, et al. Evaluation of cognitive behavioral therapy/motivational enhancement therapy (CBT/MET) in a treatment trial of comorbid MDD/AUD adolescents. Addict Behav. 2011;36(8):843–848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Hamann J, Leucht S, Kissling W. Shared decision making in psychiatry. Acta Psychiatr Scand. 2003;107(6):403–409 [DOI] [PubMed] [Google Scholar]
- 99.Elwyn G, Frosch D, Thomson R, et al. Shared decision making: a model for clinical practice. J Gen Intern Med. 2012;27(10):1361–1367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Friedrichs A, Spies M, Härter M, Buchholz A. Patient preferences and shared decision making in the treatment of substance use disorders: a systematic review of the literature. PLoS One. 2016;11(1):e0145817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Tanner JL. Recentering during Emerging Adulthood: A Critical Turning Point in Life Span Human Development. In: Arnett JJ, Tanner JL, eds. Emerging Adults in America: Coming of Age in the 21st Century. Washington, DC: American Psychological Association; 2006:21–55 [Google Scholar]


