Abstract
A 46-year-old woman was admitted to our hospital because of high fever and lumbago. CT revealed increase in density of fat tissue around the aorta, suggesting retroperitoneal panniculitis. The following day, she reported of leg pain, pain in the mouth, painful urination and right eye pain that was exacerbated by eye movement. We observed erythema nodosum, aphthous stomatitis and genital ulceration. Ophthalmologic examination revealed mild right optic disc oedema. Visual acuity was normal in both eyes. MRI with gadolinium infusion revealed enhancement around the right optic nerve, suggesting optic nerve perineuritis (ONP). A diagnosis of Behçet’s disease was made. She was treated with prednisolone and colchicine with a favourable response. A warning sign of ONP is eye pain that is exacerbated by eye movement. MRI with gadolinium infusion should be performed immediately in such cases to prevent vision-threatening sequelae.
Keywords: eye, rheumatology
Background
Behçet’s disease is a systemic inflammatory disease of unknown aetiology, characterised by relapsing episodes of oral aphthous ulcers, genital ulcers, skin lesions and ocular lesions. However, Behçet’s disease can have variable presentations and is frequently misdiagnosed.
The eye is one of the most commonly involved organs in Behçet’s disease. The typical form of involvement is uveitis, which could be the initial manifestation of Behçet’s disease. The prevalence of uveitis in Behçet’s disease is as high as 48%. Optic nerve perineuritis (ONP) is a rare inflammatory disease, which specifically targets the optic nerve sheath. ONP might be idiopathic or occur as a manifestation of systemic diseases, such as Behçet’s disease.1–4
Erythema nodosum (EN) is a typical presentation of Behçet’s disease and the histopathological features of EN are classified as lobular panniculitis. Although panniculitis can occur in any fatty tissue, panniculitis in the abdominal cavity accompanied by Behçet’s disease is rarely reported.5 6
Here, we report a rare case of Behçet’s disease, in which the initial presentations included ONP and retroperitoneal panniculitis.
Case presentation
A 46-year-old woman was admitted to our hospital because of high fever and lumbago. She had been in good health until 3 days previously, when she developed fever with a temperature of over 38°C and lumbago, for which she visited our hospital.
On physical examination, her blood pressure was 104/58 mm Hg and pulse rate was 111 beats/min. Her body temperature was 38.9°C. There was tenderness in her gastric region, but there was no rebound tenderness or guarding. Her remaining physical examination was unremarkable, including that of her extremities. At this point, there were no ophthalmic complaints.
Investigations
Blood cell count showed leucocytosis: white blood cell counts 11.4×109 cells/L (normal range: 3.5–9.7×109 cells/L) and microcytic hypochromic anaemia (red blood cell count 4.35×1012 cells/L, haemoglobin 93 g/L and haematocrit 30.4%). Her C reactive protein level was elevated to 13.58 mg/dL (normal range: <0.5 mg/dL). Hepatic and renal functions were normal. CT scan revealed a focal increase in density of fat tissue around the abdominal aorta, suggesting retroperitoneal panniculitis (figure 1A). Gastrointestinal endoscopy revealed no abnormal findings.
Figure 1.
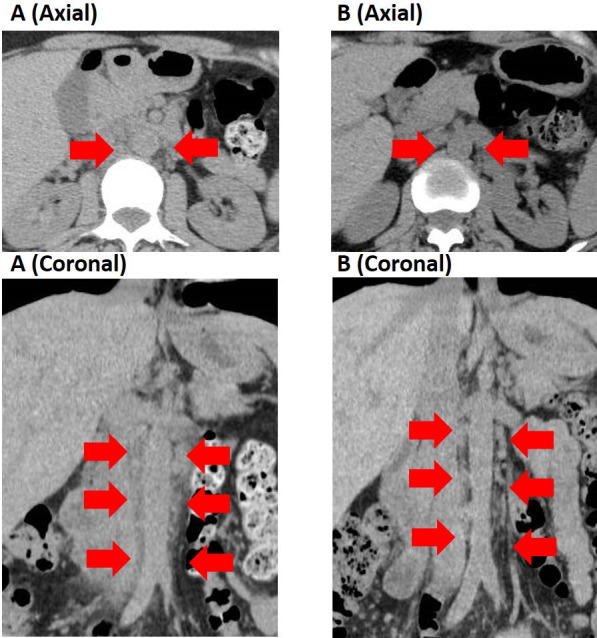
CT on admission revealed (A) increase in density of fat tissue around the aorta, suggesting retroperitoneal panniculitis. (B) The panniculitis improved after steroid and colchicine therapy.
The following day, she reported of leg pain, pain in the mouth, painful urination and right eye pain that was exacerbated by eye movement. There were tender and red nodules on both lower extremities, suggesting EN (figure 2) and aphthous stomatitis on the oral mucosa. Examination by a gynaecologist revealed genital ulceration. Best corrected visual acuity indicated an acuity of 20/20 in both eyes. Funduscopic examination revealed mild right optic disc oedema. However, there were no signs of uveitis. MRI with gadolinium infusion revealed enhancement around the right optic nerve, suggesting ONP (figure 3A).
Figure 2.
There were tender and red nodules on both lower extremities, suggesting erythema nodosum.
Figure 3.
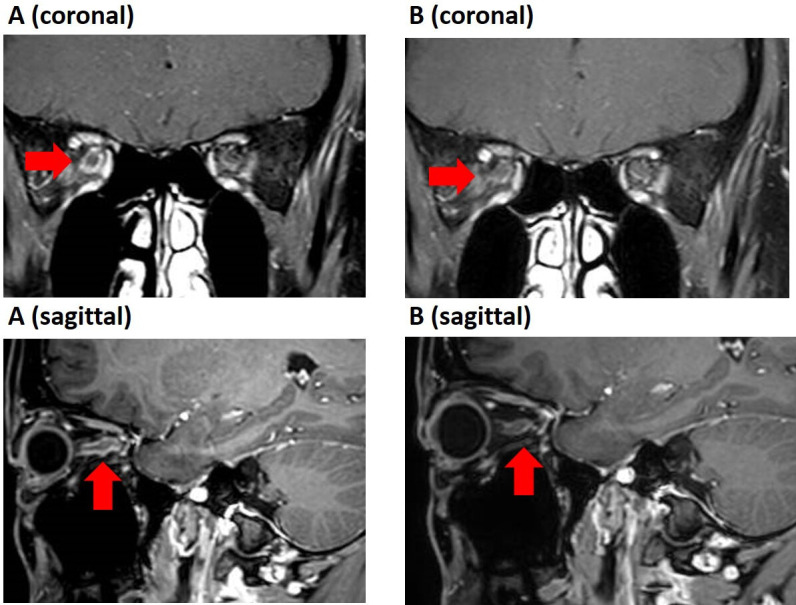
MRI with gadolinium infusion revealed (A) enhancement around the right optic nerve, suggesting optic nerve perineuritis. (B)The perineuritis disappeared after therapy.
Differential diagnosis
Behçet’s disease was diagnosed based on the International Criteria for Behçet’s Disease (at least five points for genital aphthosis, oral aphthosis and skin lesions). The differential diagnosis included autoimmune diseases such as IgG4-related disease, granulomatous polyangiitis and systemic lupus erythematosus (SLE). However, these diseases were excluded because serum IgG4 levels were normal (17 mg/dL) and proteinase 3 antineutrophil cytoplasmic antibody (ANCA), myeloperoxidase ANCA and antinuclear antibody were negative. An infectious aetiology was ruled out because blood culture was negative for bacteria and she did not respond to antibiotic therapy.
Treatment
She was treated with 30 mg oral prednisolone and 1 mg of colchicine daily with a favourable response. Leg pain, pain in the mouth, painful urination and right eye pain disappeared the following day, as did EN. The right optic disc oedema also resolved.
CT performed 18 days after the initiation of therapy revealed improvement of the increase in density of fat tissue around the aorta (figure 1B). MRI performed 20 days after the initiation of therapy revealed disappearance of abnormal enhancement around the right optic nerve (figure 3B).
Outcome and follow-up
The dose of prednisolone was gradually tapered and she is treated as an outpatient for 6 months at the moment without recurrence of the disease.
Discussion
ONP is a rare inflammatory disease that specifically targets the optic nerve sheath. In 2001, Purvin et al7 reviewed clinical and radiographic features of 14 cases of idiopathic ONP. In their review, all patients had visual loss, eye pain or both. The eye pain was commonly exacerbated by eye movement. Visual acuity was 20/20 or better in eight of the 15 eyes. MRI demonstrated enhancement around, rather than within, the optic nerve (‘tram-track’ sign on axial views and ‘doughnut’ sign on coronal views).
In 2011, Hickman1 reviewed cases of secondary ONP and found that the cause of ONP with autoimmune diseases included Behçet’s disease (10 cases), granulomatous polyangiitis (5 cases) and Crohn’s disease (1 case). In 2021, Hongyang et al3 reported that the causes of ONP with autoimmune diseases included Graves’ disease (12 cases), IgG4-related disease (10 cases), granulomatous polyangiitis (4 cases), SLE (2 cases), sarcoidosis, rheumatoid arthritis, scleroderma, Behçet’s disease and gout.
Purvin et al7 reported a dramatic response to corticosteroid therapy, with most patients typically demonstrating dramatic pain relief within hours of initiating treatment, and all demonstrating relief within days of treatment initiation. Visual loss also showed prompt recovery. However, 4 of 14 patients relapsed with lowering of the steroid dose. In that study, two patients were treated successfully with indomethacin as opposed to corticosteroids. Furthermore, a refractory case was treated successfully with radiation therapy and azathioprine. However, the role of non-steroidal anti-inflammatory medication or radiation in long-term prevention of relapse is unclear. In contrast to idiopathic cases, ONP in Behçet’s disease is more likely to demonstrate initial rapid progression of visual loss and more severe loss at presentation. Patients show less recovery of vision in response to corticosteroids, but carry a lower rate of subsequent relapse.2 The prognosis of visual loss in ONP is excellent if treated by corticosteroids promptly after the onset of visual loss. However, a delay in treatment results in poor visual outcomes. Thus, early diagnosis and prompt treatment are essential for improving visual outcomes.
Panniculitis in the abdominal cavity is a rare and benign inflammatory condition. Although it predominantly affects the mesenteric fat of the small and large intestines, it rarely involves retroperitoneal fat.8 Causes of abdominal panniculitis include idiopathic, infectious, neoplastic and autoimmune diseases, such as Behçet’s disease. EN is a typical presentation of Behçet’s disease, and the histopathological features of EN are classified as lobular panniculitis. Although histological examination was not performed in this case, it is speculated that similar histological changes were present in the retroperitoneal fat tissue.
In summary, we experienced a patient with Behçet’s disease in whom the initial presentations included ONP and retroperitoneal panniculitis. Behçet’s disease can have variable presentations and can be frequently misdiagnosed. Physicians should be aware of these rare presentations of Behçet’s disease.
Learning points.
We report a rare case of Behçet’s disease, in which the initial presentations included optic nerve perineuritis (ONP) and retroperitoneal panniculitis.
Early diagnosis and prompt treatment of ONP are essential for improving visual outcomes because a delay in treatment results in poor visual outcomes, especially in patient with Behçet’s disease. A warning sign of ONP is eye pain that is exacerbated by eye movement. MRI with gadolinium infusion should be performed immediately in such cases to prevent vision threatening sequelae.
Although erythema nodosum is a typical presentation of Behçet’s disease, retroperitoneal panniculitis could be the first manifestation of Behçet’s disease.
Footnotes
Contributors: KY: reviewed medical records, interpreted data and drafted the manuscript. EM: reviewed medical records, interpreted data and supervised the study.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Obtained.
References
- 1.Hickman SJ. Optic perineuritis. Curr Neurol Neurosci Rep 2016;16:16. 10.1007/s11910-015-0617-2 [DOI] [PubMed] [Google Scholar]
- 2.Lai C, Sun Y, Wang J, et al. Optic perineuritis in Behçet disease. J Neuroophthalmol 2015;35:342–7. 10.1097/WNO.0000000000000264 [DOI] [PubMed] [Google Scholar]
- 3.Li H, Zhou H, Sun J, et al. Optic perineuritis and its association with autoimmune diseases. Front Neurol 2020;11:627077. 10.3389/fneur.2020.627077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Purvin V, Kawasaki A. Optic perineuritis secondary to Wegener's granulomatosis. Clin Exp Ophthalmol 2009;37:712–7. 10.1111/j.1442-9071.2009.02122.x [DOI] [PubMed] [Google Scholar]
- 5.Issa I, Baydoun H. Mesenteric panniculitis: various presentations and treatment regimens. World J Gastroenterol 2009;15:3827–30. 10.3748/wjg.15.3827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nordstrom E, Fischer M. The great masquerader: Behcet’s disease. Case Reports 2014;2014:bcr2013202919. 10.1136/bcr-2013-202919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Purvin V, Kawasaki A, Jacobson DM. Optic perineuritis: clinical and radiographic features. Arch Ophthalmol 2001;119:1299–306. 10.1001/archopht.119.9.1299 [DOI] [PubMed] [Google Scholar]
- 8.Terada N, Tanaka T, Fujimoto T, et al. Retroperitoneal panniculitis. BMJ Case Rep 2015;2015:bcr2015212670. 10.1136/bcr-2015-212670 [DOI] [PMC free article] [PubMed] [Google Scholar]



