Abstract
Background
The full reopening of schools in September 2020 was associated with an increase in COVID-19 cases and outbreaks in educational settings across England.
Methods
Primary and secondary schools reporting an outbreak (≥2 laboratory-confirmed cases within 14 days) to Public Health England (PHE) between 31 August and 18 October 2020 were contacted in November 2020 to complete an online questionnaire.
Interpretation
There were 969 school outbreaks reported to PHE, comprising 2% (n = 450) of primary schools and 10% (n = 519) of secondary schools in England. Of the 369 geographically-representative schools contacted, 179 completed the questionnaire (100 primary schools, 79 secondary schools) and 2,314 cases were reported. Outbreaks were larger and across more year groups in secondary schools than in primary schools. Teaching staff were more likely to be the index case in primary (48/100, 48%) than secondary (25/79, 32%) school outbreaks (P = 0.027). When an outbreak occurred, attack rates were higher in staff (881/17,362; 5.07; 95%CI, 4.75–5.41) than students, especially primary school teaching staff (378/3852; 9.81%; 95%CI, 8.90–10.82%) compared to secondary school teaching staff (284/7146; 3.97%; 95%CI, 3.79–5.69%). Secondary school students (1105/91,919; 1.20%; 95%CI, 1.13–1.28%) had higher attack rates than primary school students (328/39,027; 0.84%; 95%CI, 0.75–0.94%).
Conclusions
A higher proportion of secondary schools than primary schools reported a COVID-19 outbreak and experienced larger outbreaks across multiple school year groups. The higher attack rate among teaching staff during an outbreak, especially in primary schools, suggests that additional protective measures may be needed.
Funding
PHE
Keywords: SARS-CoV-2, COVID-19, Schools, Children, Transmission, Outbreak
Research In Context.
Evidence before this study
We searched PubMed for articles published between 01 January and 31 November 2020 with the terms “COVID-19″ or “SARS-CoV-2″ with “school”, “education”, “staff” or “student” to identify publications relating to COVID-19 cases and outbreaks in educational settings globally, with no language restrictions. Countries that kept their preschools and primary schools open early in the pandemic reported very few cases in school-aged children or outbreaks in educational settings. Similar experiences were reported by countries that reopened their schools after their national lockdown, when local community infection rates were low. A number of countries reported larger and more extensive COVID-19 outbreaks in secondary schools than in primary schools.
Added Value of this study
We rapidly investigated primary and secondary schools reporting a COVID-19 outbreak to Public Health England following the full reopening of educational settings during the autumn term in England. Unlike the summer half-term (June-July 2020), when very few cases and outbreaks were reported in educational settings, we found both an increase in the proportion of settings experiencing outbreaks, especially in secondary schools, and important differences in outbreak characteristics. While outbreaks were less common in primary schools, they were more likely to affect staff members. Compared to primary schools, outbreaks in secondary schools were larger, affecting more students than staff and across multiple year groups.
Implications of all the available evidence
Numerous mitigation processes have been recommended for the full reopening of schools, but little is known about the feasibility or implementation of these measures across different educational settings. We found significantly higher SARS-CoV-2 infection rates in staff compared to students, especially in primary schools. At the time in England, face coverings were optional for staff in primary schools and, in secondary schools, were recommended for staff and students in communal areas outside the classroom if physical distancing was difficult to maintain. Further studies are needed to identify the most effective interventions to protect staff and students against SARS-CoV-2 in educational settings.
Alt-text: Unlabelled box
1. Introduction
SARS-CoV-2, the virus responsible for COVID-19, first emerged in Wuhan, China, in December 2019 and spread rapidly worldwide, forcing many countries to implement national lockdown, which included school closures because the role of children in infection and transmission of SARS-CoV-2 was not known at the time [1]. Children represent only a small proportion of COVID-19 cases and generally develop a mild and transient illness – severe disease, hospitalization and deaths are rare in children [2]. School closure not only affects children's education, but has a wider negative impact on their physical, emotional and social well-being, with those from disadvantaged backgrounds likely to be the most affected [3,4].
In England, the first imported cases of SARS-CoV-2 were confirmed at the end of January 2020 and cases started increasing rapidly from March 2020 [5]. Schools were closed to all except children of keyworkers and vulnerable children from 20 March, with a wider national lockdown imposed from 23 March, which included home working and closure of non-essential shops and hospitality venues [6]. Cases of SARS-CoV-2 plateaued in mid-April and then declined gradually until end-May 2020 [5]. From 01 June 2020, preschools and some primary school years were allowed to physically re-open, followed by some secondary school years from 15 June, until the end of the summer half-term in mid-July 2020 [7]. During this period, the number of open educational settings increased from 20,500 to a peak of 23,500, and the number of students attending school increased from 475,000 to a peak of 1672,000 [8]. Physical distancing and infection control measures were put in place, including frequent hand washing, regular cleaning of classrooms and small class sizes restricted to 15 students and organised into discrete bubbles that did not physically or socially interact with each other [7]. These measures, along with low community SARS-CoV-2 infection rates, were associated with very few infections or outbreaks in educational settings [9].
From 31 August 2020, educational settings opened for all students in England. The same guidelines for physical distancing and other infection control measures remained in place but the large numbers of children attending school precluded small class sizes or organization into small bubbles. During September and October 2020, SARS-CoV-2 infection rates increased across all age-groups, including school-aged children, as did the number of COVID-19 outbreaks reported to Public Health England (PHE) [5]. We, therefore, initiated a rapid investigation of COVID-19 outbreaks reported to PHE during the first half of the autumn term in primary and secondary schools across England.
2. Methods
PHE initiated a rapid cross-sectional investigation of COVID-19 outbreaks occurring in the first half-term of the 2020/21 autumn term (31 August to 18 October 2020) in primary and secondary schools in England. Educational settings that re-opened during this period included 18,943 primary schools, 5,409 secondary schools, and 1,231 special schools. Schools that include both primary and secondary age pupils are counted seperately for primary and secondary schools in the denominator. (Source: Department for Education). The same physical distancing and infection control measures were implemented as in the summer half-term [7]. As per national guidance, face masks and face coverings were not recommended in classrooms, but staff and children in secondary schools were advised to wear them in communal areas outside the classroom if physical distancing was difficult to maintain, while primary schools had the discretion to recommend face masks or face coverings for staff or visitors [7].
Educational settings were advised to report SARS-CoV-2 cases and outbreaks to their local PHE Health Protection Teams (HPTs) for public health advice and support [9]. Owing to the volume of reported outbreaks after schools re-opened in September, however, a National Schools Advice Line opened on 17 September 2020, providing support and advice for smaller outbreaks of <5 cases. Arrangements were also made to allow some local authorities and other stakeholders to support HPTs with outbreak management. Schools were regularly provided with updated guidance on management of cases and contacts in educational settings [10,11]. Outbreaks reported to PHE are routinely recorded in HPZone, an online national case management system used by PHE HPTs to record events that require public health management [9]. HPZone, however, records limited data on individual outbreaks. The PHE national COVID-19 surveillance team use a weekly HPZone extract to report a summary of COVID19 outbreaks linked to educational and other settings [12]. To collect more detailed information on individual outbreaks in educational settings, PHE contacted headteachers or nominated Senior Management Team (SMT) members of primary and secondary schools reporting an outbreak during the first half of the autumn term and asked them to complete a secure online questionnaire developed using SnapSurvey v.11 or to provide the information over the telephone (Supplement Table S1). We aimed to contact as many schools as possible during the first two weeks of November 2020 and identified ~40% of schools in each PHE region using a purposive and pragmatic sampling strategy to achieve geographical representation of reported school outbreaks nationally.
2.1. Definitions
A case of COVID-19 was defined as any symptomatic individual testing positive for SARS-CoV-2 by RT-PCR on an upper respiratory tract swab. In England, all individuals have access to free testing for SARS-CoV-2 if they develop COVID-19 symptoms (fever, new continuous cough, loss of test/smell) [13]. Primary school and secondary school children were aged 4–11 and 11–18 years, respectively. Teaching staff were defined as any member of staff with a teaching role and included teachers, teaching assistants and specialist teachers, who were more likely to have direct close contact with students. Non-teaching staff were defined as members of staff in a non-teaching role, such as administrative and domestic staff. An outbreak was defined as two or more laboratory-confirmed cases of COVID-19 with illness onset dates, or test positivity dates if asymptomatic, within 14 days of each other.
2.2. Data management and analysis
Data collected through SnapSurvey were downloaded into Microsoft Excel 365 and Stata v.15 (Statacorp, Tx) for analysis. Outbreaks were categorised into primary or secondary schools in HPZone. After survey completion, some schools were subsequently identified as combined schools that hosted both primary and secondary school years on the same site; these were excluded from further analyses. Nurseries and Special Educational Needs and Disabilities (SEND) schools were excluded because they had very specific risk factors for SARS-CoV-2 infection, transmission and outbreaks. SARS-CoV-2 confirmation in the index case was used to identify the start of an outbreak. Data are mainly descriptive. Denominators for total student and staff numbers were reported by individual schools in the questionnaire. Continuous data that did not follow a normal distribution are described as medians with interquartile ranges. Proportions are presented with 95% binomial confidence intervals and compared using the chi-squared or Fisher's Exact test. Attack rates were calculated by dividing the number of cases by the population at risk (e.g. primary school teachers) and compared using Fishers Exact probability tests via the prop.test function in R studio (version 1.3.1056). Analyses were not adjusted for multiple comparisons.
2.3. Role of the funding source
This surveillance was internally funded by PHE and did not receive any specific grant funding from agencies in the public, commercial or not-for-profit sectors. All authors had access to the data; the first and final authors verified the data and had final responsibility for the decision to submit for publication.
3. Results
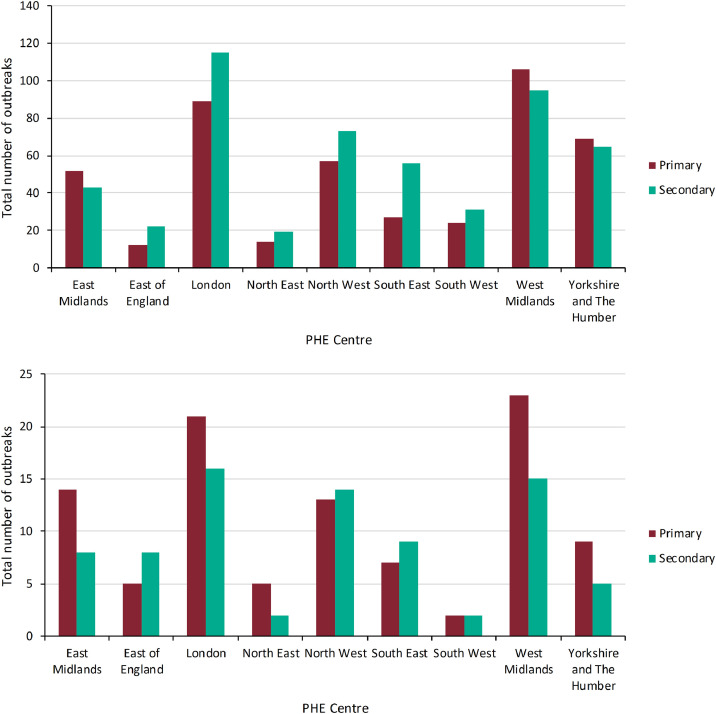
Between 31 August and 18 October 2020, 969 COVID-19 outbreaks in primary and secondary schools across England were reported to PHE (See Flowchart, Supplement Figure S2). Of these, 450 were in primary schools (2% of primary schools) and 519 in secondary schools (10% of secondary schools) (Fig. 1). Reported outbreaks increased rapidly after schools reopened, peaking during the week of 14–20 September 2020 and remained high until the end of the investigation period (week of 12–18 October 2020) (Supplement Figure S3). Outbreaks were reported across all English regions, with the greatest number of outbreaks reported in the London region and the West Midlands. Although there are nearly five times as many primary schools as secondary schools in England, there were more secondary than primary school outbreaks in six of the nine English regions (Fig. 1).
Fig. 1.
COVID-19 outbreaks by region that were (A) reported and (B) investigated by Public Health England during the first half of the autumn term (31 August to 18 October 2020) in England.Some outbreaks reported to PHE as occurring in primary or secondary schools were subsequently identified as combined schools that hosted both primary and secondary schools on the same site, which were excluded from further analyses.
In total, 369 schools reporting an outbreak (38% of reported outbreaks in educational settings) were contacted during the first two weeks of November 2020. Of these, 197 (53%) completed the survey. Five schools provided insufficient information, two were excluded because the outbreak occurred in a nursery attached to the primary school and 11 others were excluded because they were combined primary and secondary schools on the same site (Fig. 1). Therefore, 179 geographically-representative primary (n = 100, 56%) and secondary (n = 79, 44%) schools with confirmed COVID-19 outbreaks across England were included in the analysis (Supplement Figure S1).
3.1. Outbreaks
Outbreaks in primary schools involved 2–35 (median 6, IQR 4–10) cases compared to 2–100 (median 15, IQR 8.5–27) cases in secondary schools (P<0.001) (Table 1). Most outbreaks occurred across >1 year group in both primary and secondary schools, but 84%% (66/79) of secondary school outbreaks occurred across ≥3 year groups, compared to 25% (25/100) in primary schools (P<0.001). Outbreaks involving staff only were rare in both primary (6/100, 6%) and secondary schools (1/79, 1.3%) (Table 1). In total, 24 schools closed for up to 14 days (9 for ≤2 days, 9 for 3–13 days and 6 for 14 days) because of the outbreak, for multiple reasons, including deep cleaning, lack of staff, large numbers of contacts and to break the chain of transmission.
Table 1.
Summary of cases and size of outbreaks reported to Public Health England (PHE) during the first half of the autumn term (31 August to 18 October 2020) in England.
| School type |
||||
|---|---|---|---|---|
| Primary n (% in primary schools) | Secondary n (% in secondary schools) | Both settings n (%) | P value (primary vs secondary schools)* | |
| Total number of schools | 100 | 79 | 179 | |
| Total cases (% of cases across both settings) | 799 | 1515 | 2314 | |
| Student cases | 328 (41%) | 1105 (73%) | 1433 (62%) | P <0.001 |
| Staff cases | 471 (59%) | 410 (27%) | 881 (38%) | |
| Median (IQR) number of cases per outbreak | 6 (4–10) | 15 (8–28) | 9 (5–16) | P<0.001 |
| Mode number of cases per outbreak | 3 | 6 | 6 | |
| Total numbers of cases per outbreak | 2–35 | 2–100 | 2–100 | |
| Index case in the outbreak | ||||
| Teaching staff | 48 (48%) | 25 (32%) | 73 (41%) | P = 0.012 |
| Student | 35 (35%) | 47 (59%) | 82 (46%) | |
| Non-teaching staff | 9 (9%) | 6 (8%) | 15 (8%) | |
| Another source | 1 (1%) | 0 (0%) | 1 (1%) | |
| Not reported | 7 (7%) | 1 (1%) | 8 (4%) | |
| Groups affected by the outbreak | n (%) | n (%) | % | |
| Staff only | 6 (6%) | 1 (1%) | 7 (4%) | P<0.001 |
| 1 year group only | 39 (39%) | 5 (6%) | 44 (25%) | |
| 2 year groups | 30 (30%) | 7 (9%) | 37 (21%) | |
| 3 or more year groups | 25 (25%) | 66 (84%) | 91 (51%) | |
Proportions were compared using chi squared or Fishers Exact Test, medians with interquartile ranges were compared using the Mann-Whitney U Test.
The reported index case in each outbreak varied by educational setting (P = 0.012). Teaching staff were more likely to be the index case in primary schools (48/100, 48%) than in secondary schools (25/79, 32%; P = 0.027) (Table 1). Most outbreaks involved both staff and students, irrespective of the educational setting or whether the index case was a staff member or a student. While some outbreaks in secondary schools involved only students, reported outbreaks in primary schools always involved staff and students (Table 2). The source of infection was not known for most index cases. The most common reason for SARS-CoV-2 testing in the first four cases involved in the outbreak was presence of COVID-19 symptoms in 68% (433/635) with 6% (36/635) tested because they were contacts of a confirmed case in school, while 18% (112/635) reported contact with a household case (Supplement Table S4).
Table 2.
Involvement of students and staff according to the index cases in outbreaks reported to Public Health England (PHE) during the first half of the autumn term in England.
| School type | ||||
|---|---|---|---|---|
| Index case | Group affected | Primary schools | Secondary schools | Both settings |
| Teaching staff | Staff only | 4/48 (8%) | 0/25 (-) | 4/73 (5%) |
| Student only | 0/48 (-) | 0/25 (-) | 0/73 (-) | |
| Both | 44/48 (92%) | 25/25 (100%) | 69/73 (95%) | |
| Student | Staff only | 0/35 (-) | 1/47 (2%) | 1/82 (1%) |
| Student only | 10/35 (29%) | 6/47 (13%) | 16/82 (20%) | |
| Both | 25/35 (71%) | 40/47 (85%) | 65/82 (79%) | |
| Non-teaching staff | Staff only | 2/9 (22%) | 0/6 (-) | 2/15 (13%) |
| Student only | 0/9 (-) | 0/6 (-) | 0/15 (-) | |
| Both | 7/9 (78%) | 6/6 (100%) | 13/15 (87%) | |
3.2. Attack rates in staff and students
There were 2314 SARS-CoV-2 cases reported across the 179 schools, including 799 cases in primary schools and 1515 cases in secondary schools (Table 1). In students, SARS-CoV-2 attack rates increased with increasing school academic year, peaking in academic year 11 (15–16 year-olds) (Supplement Figure S5). Attack rates in secondary school students (1.20%; 95%CI, 1.13–1.28%) were significantly higher than in primary school students (0.84%; 95%CI, 0.75–0.94%) (P<0.001) (Table 3), while attack rates in staff members (5.07%; 95%CI, 4.75–5.41%) were almost five times higher than in students (1.09%; 95%CI, 1.04–1.15%) (P<0. 001). Additionally, teaching staff (6.02%; 95%CI, 5.59–6.48%) had higher attack rates than non-teaching staff (3.44%; 95%CI, 3.01–3.93%) (P<0.001) (Table 3). Within an outbreak setting, primary school teaching staff had the highest attack rate (9.81%; 95%CI, 8.90–10.82%). Teaching staff in secondary schools by comparison had an attack rate of 3.97% (95%CI, 3.54–4.46%) (P<0.001), while non-teaching staff had the lowest attack rate (2.98%; 95%CI, 2.07–4.26%) (Table 3).
Table 3.
Attack rate with 95% confidence intervals by education setting for staff and students in primary and secondary schools reporting a COVID-19 outbreak during the first half of the autumn term (31 August to 18 October 2020) in England.
| School type | |||
|---|---|---|---|
| Primary | Secondary | Both settings | |
| Total number of schools | 100 | 79 | 179 |
| Student cases | 328 | 1105 | 1433 |
| Total students | 39,027 | 91,919 | 130,946 |
| Student attack rate,% (95% CI) | 0.84% (0.75–0.94%) | 1.20 (1.13–1.28%) | 1.09% (1.04–1.15%) |
| Staff cases | 471 | 410 | 881 |
| Total staff | 5852 | 11,510 | 17,362 |
| Staff attack rate,% (95% CI) | 8.05% (7.37–8.78%) | 3.56% (3.24–3.92%) | 5.07% (4.75–5.41%) |
| Teaching staff cases | 378 | 284 | 662 |
| Total teaching staff | 3852 | 7146 | 10,998 |
| Teaching staff attack rate,% (95% CI) | 9.81% (8.90–10.82%) | 3.97% (3.54–4.46%) | 6.02% (5.59–6.48%) |
| Non-teaching staff cases | 93 | 126 | 219 |
| Total non-teaching staff | 2000 | 4364 | 6364 |
| Non-teaching staff attack rate,% (95% CI) | 4.65% (3.79–5.69%) | 2.89% (2.42–3.44%) | 3.44% (3.01–3.93%) |
| All cases | 799 | 1515 | 2314 |
| Total population (staff & students) | 44,879 | 103,429 | 148,308 |
| Attack rate,% (95% CI) | 1.78% (1.66–1.91%) | 1.46% (1.39–15.4%) | 1.56% (1.50 −1.62%) |
When assessed by index case status, attack rates in primary and secondary school students were low, irrespective of whether the index case was a student or a staff member. In contrast, when the index case was a staff member, attack rates were high among other staff members, being highest among primary school teaching staff (250/1832, 13.65%; 95% CI, 12.12–15.32%) (Table 4). Where a student was the index case, attack rates were higher for teaching staff in primary schools (86/1300, 6.62%; 95% CI, 5.35–8.14%) than secondary schools (144/4678, 3.08%; 95% CI, 2.61–3.62%) (P<0.001) (Table 4).
Table 4.
Attack rates with 95% confidence intervals in students and staff according to the index case in outbreaks reported to Public Health England (PHE) during the first half of the autumn term in England.
| Attack Rate | ||||
|---|---|---|---|---|
| Index Case | Group affected | Primary Schools | Secondary Schools | Both Settings |
| Student | Students | 167/13,967 (1.20%; 1.03 - 1.39%) | 700/56,418 (1.24%; 1.15 - 1.34%) | 867/70,385 (1.23%; 1.15 - 1.32%) |
| Teaching staff | 86/1300 (6.62%; 5.35 - 8.14%) | 144/4678 (3.08%; 2.61 - 3.62%) | 230/5978 (3.85%; 3.38 - 4.97%) | |
| Non-teaching staff | 16/747 (2.14%; 1.27 - 3.53%) | 56/2708 (2.07%; 1.58 - 2.70%) | 72/3455 (2.08%; 1.65 - 2.63%) | |
| Total (all staff/students) | 269/16,014 (1.68%; 1.49 - 1.89%) | 900/63,804 (1.41%; 1.32 - 1.51%) | 1169/79,818 (1.46%; 1.39 - 1.55%) | |
| Teaching staff | Students | 127/18,083 (0.70%; 0.59 - 0.84%) | 330/27,119 (1.22%; 1.09 - 1.36%) | 457/45,202 (1.01%; 0.92 - 1.10%) |
| Teachers | 250/1832 (13.65%; 12.12 - 15.32%) | 123/1786 (6.89%; 5.78 - 8.19%) | 373/3618 (10.31%; 4.22 - 6.13%) | |
| Non-teaching staff | 53/890 (5.96%; 4.53 - 7.77%) | 57/1269 (4.49%; 3.45 - 5.82%) | 110/2159 (5.09%; 4.22 - 6.13%) | |
| Total (all staff/students) | 430/20,805 (2.07%; 1.88 - 2.27%) | 510/30,174 (1.69%; 1.55 - 1.84%) | 940/50,979 (1.84%; 1.73 - 1.97%) | |
| Non-teaching staff | Students | 13/3853 (0.34%; 0.19 - 0.59%) | 65/6556 (0.99%; 0.77 - 1.27%) | 78/10,409 (0.75%; 0.60 - 0.94%) |
| Teaching staff | 21/356 (5.90%; 3.78 - 9.01%) | 17/532 (3.20%; 1.93 - 5.17%) | 38/888 (4.28%;3.09 - 5.88%) | |
| Non-teaching staff | 16/197 (8.12; 4.86 – 13.08%) | 13/337 (3.86%; 2.16 - 6.67%) | 29/534 (5.43%; 3.73 – 7.79%) | |
| Total (staff and students) | 50/4406 (1.13%; 0.85 - 1.51%) | 95/7425 (1.28%; 1.04 - 1.57%) | 145/11,831 (1.23%; 1.04 - 1.44%) | |
4. Discussion
The reopening of all schools after 31 August 2020 was associated with nearly 1000 primary and secondary school outbreaks of COVID-19 reported to PHE during the first half of the autumn term. These represented 2% of primary schools and 10% of secondary schools across England, and 32% of all outbreaks reported to PHE across all settings (care homes, hospital, prisons, workplaces, food outlets and other) [12]. Detailed follow-up of 179 schools reporting an outbreak identified 2314 cases among staff and students. When an outbreak occurred, teaching staff were more likely to be affected than non-teaching staff, with the highest rates reported in primary school teachers, who were also more likely to be the index case in primary schools than students. Among students, secondary school students had higher attack rates than primary school students and were more likely to be the index case in secondary schools than teaching or non-teaching staff. Outbreaks were larger and across multiple year groups in secondary schools compared to primary schools, but, reassuringly, attack rates in students were very low in both settings, irrespective of the source of the index case. Most outbreaks involved both staff and students across both educational settings, although some outbreaks in secondary schools involved students only.
In England, the reopening of schools in the autumn term was a very different experience compared to the summer half-term, when national lockdown was still in place. In June, community SARS-CoV-2 infection rates were very low, only a few academic years were allowed back in school (mainly in preschool and primary school years), class sizes were restricted to small numbers and staff to student ratios were higher than usual [7]. Additionally, staff and students were segregated into distinct bubbles that did not interact with each other and could easily be identified for self-isolation if a case was confirmed in the bubble [7]. Consequently, there were very few confirmed cases and outbreaks of COVID-19 reported in schools during the summer half-term, and a large proportion of confirmed outbreaks involved staff members only, with more than half the outbreaks involving only two cases [9]. At that time, the experience in England was consistent with reports from the few countries that had kept their preschools and primary schools open throughout the first wave of pandemic in the spring of 2020 [4], and with schools that re-opened after their national lockdown in the summer of 2020 [4,[14], [15], [16], [17]]. There were, however, reports of higher numbers of cases and outbreaks in secondary schools than in primary schools in the same region (i.e. areas where both educational setting types had the same community infection risk) [18], [19], [20]. In the Netherlands, public health investigations found that just over half the cases in secondary school clusters were acquired outside school, mainly during intensive contact with friends or classmates in their free time [16]. Additionally, infections in secondary schools were seen mainly in small groups of students and separately in teachers. Accordingly, the Netherlands does not recommend self-isolation for classmates unless they had intensive contact with a confirmed case [16]. In our outbreak investigation, we also observed an increasing risk of infection with age, which is consistent with national data in England [5], and there were some secondary school outbreaks that were restricted to students only. Older children appear to be at increased risk of SARS-CoV-2 infection [21], may be more efficient transmitters of the virus [22], and have increased social contacts and mixing patterns than younger children, which may all increase the risk of more widespread infection in this group.
Compared to the students, however, SARS-CoV-2 infection rates during school outbreaks were significantly higher in school staff, especially teaching staff. This was particularly the case for teaching staff in primary schools, who were also more likely to be the index case in primary school outbreaks. In primary schools, attack rates were also highest among teaching staff when the index case was also a member of the teaching staff. For both staff and students, SARS-CoV-2 may have been acquired in the community or within the educational setting. Cases in staff members, however, are more concerning because adults are more likely to develop severe disease, require hospitalization, intensive care and die of COVID-19 compared to children [23,24]. We were unable to ascertain the potential source of infection for the reported cases because outbreak information was obtained from Headteacher/SMT interviews. Notably though, most cases in the outbreaks were tested because they were symptomatic for COVID-19, with fewer than 10% tested because they were contacts of a confirmed case in school. In addition, the offer of testing in these outbreaks followed national guidelines and was mainly restricted to symptomatic individuals [25]. We were, therefore, unable to assess the role of asymptomatic infection and transmission among staff and students.
The higher infection rates in primary compared to secondary school staff during outbreaks could be due to difficulties in maintaining physical distancing between staff and students (and among the students themselves)because they are usually physically smaller than secondary schools. Another important difference is that face coverings are discretionary for staff or students in primary schools but, in secondary schools, are recommended for use in communal areas outside the classroom [7]. Reassuringly, though, recent ONS analysis found no evidence of differences in infection positivity rates between primary and secondary school teachers, other key workers and other professions between 02 September and 16 October 2020, although the confidence intervals around the point estimates were wide because of small numbers [26]. This could be a reflection of the extensive infection control practices in educational settings compared to other places of employment.
4.1. Strengths and limitations
The strength of this analysis lies in the real-time national surveillance undertaken by PHE of outbreaks in institutional settings, including schools, with daily updates through a national online electronic data management system. However, because of the large numbers of cases and outbreaks reported to PHE at the start of the autumn term, smaller outbreaks were subsequently managed by the schools themselves, with support from the National Schools Advice line and other partners such as Local Authorities, without input from PHE. Smaller outbreaks may, therefore, not have been recorded on HPZone. Currently, for example, the London region only records outbreaks involving more than five cases on HPZone, the North East only reports complex outbreaks, and the North West and East of England only report outbreaks which require public health intervention. In addition, the investigated outbreaks relied on passive identification and notification of confirmed cases and, because wider testing was not performed, it is not possible to assess the extent of asymptomatic spread among other staff and students attending affected settings.
Another limitation is that the investigations was limited to a sample of 20% of the outbreaks reported during the period of interest, although these were geographically representative of total reported outbreaks. Of the contacted schools, 47% did not participate due to lack of time/capacity to complete the survey and general survey fatigue. Additionally, this was a retrospective interview rather than a detailed prospective investigation and, therefore, the data collected were limited by the information available to the interviewee. Specific limitations include limited demographic, symptoms and outcome data collected for staff and students, lack of information on the source of infection in the index case, and lack of wider testing of contacts and their household members to better understand asymptomatic infection and transmission within educational settings as well as between schools and households. Because of the lack of viral genomic data, too, it was not possible to determine whether these were genuine outbreaks caused by the same SARS-CoV-2 strain or a result of multiple separate introductions into the school. We were also unable to assess adherence to nationally recommended infection control measures in the schools reporting an outbreak. Factors affecting the risk and size of COVID-19 outbreaks within educational settings include not only the use of facemasks and face covering but also the size of the school and individual classes, ability to maintain physical distancing inside school premises, implementation and adherence to other infection control measures such as frequent hand washing and sanitization of high-touch contact surfaces, items and equipment. Factors outside the educational settings are also likely to be important, including local community infection rates, population density and indices of deprivation, as well as household characteristics, such as number of children and adults in the household and occupation of adults.
4.2. Implications of findings
There is increasing evidence that SARS-CoV-2 infections in educational settings are strongly associated with community infection rates in adults [27]. We have previously shown that the risk of school outbreaks correlated with regional SARS-CoV-2 infection rates during the summer half-term in England [9]. Maintaining low community infection rates is, therefore, critical for reducing the risk of virus introduction into educational settings. Additionally, despite the challenges in implementing national recommendations for the large numbers of students returning to school (as evidenced by most outbreaks involving both staff and students), it is highly likely that the implemented measures have helped reduce SARS-CoV-2 transmission within schools. This may explain why only 2% of primary schools and 10% of secondary schools reported an outbreak to PHE during the first half of the autumn term. The reopening of all schools on 08 March 2021 In England, the emergence and rapid spread of a more transmissible SARS-CoV-2 variant B.1.1.7 led to a third national lockdown, including school closures, in December 2020. Cases increased rapidly throughout December 2020 and then declined during January and February 2021 [5], allowing all schools to reopen from 08 March 2021, with new infection control guidance including use of facemasks or face coverings by secondary school students in classroom and by primary school staff and visitors in situations where social distancing between adults is not possible.29 Given that both these groups were identified as high-risk in our investigation, it is hoped that these new guidelines will help reduce the risk of SARS-CoV-2 infection and outbreaks in the coming months.
Further studies are needed to understand the contribution of in-school and outside-school transmission to SARS-CoV-2 spread and especially the role of asymptomatic infection and transmission among staff and students. These should include detailed prospective outbreak investigations with genomic sequencing of SARS-CoV-2 strains to determine whether the same strain is responsible for the reported outbreaks, as well as antibody testing to capture asymptomatic infections and define the true spread of an outbreak. Such studies are currently underway in the School Infection Survey (SIS) in England,30 which should provide important data to help keep educational settings open and allow staff and students to attend school safely during the current pandemic.
Ethical approval
PHE has legal permission, provided by Regulation 3 of The Health Service (Control of Patient Information) Regulations 2002, to process patient confidential information for national surveillance of communicable diseases and as such, individual patient consent is not required.
Role of the funding source
This surveillance was internally funded by PHE and did not receive any specific grant funding from agencies in the public, commercial or not-for-profit sectors. All authors had access to the data; the first and final authors verified the data and had final responsibility for the decision to submit for publication.
Data sharing
Applications for relevant anonymised data should be submitted to the Public Health England Office for Data Release: https://www.gov.uk/government/publications/accessing-public-health-england-data/about-the-phe-odr-and-accessing-data.
Contributions
FA, SL, VS were responsible for conceptualization and study design/methodology.
FA, AM, KM, CO, AV, SJ, AP, JF, JB, LL, SL, ZA, JL, IH, SN, VS contributed to project administration.
SL, FA, KM, AM and VS contributed to the original draft and SL FA AM and KM conducted the formal analysis. KM, AM and FA were responsible for data validation.
All authors contributed to reviewing and editing the manuscripts.
Declaration of interests
The authors declare no conflicts of interest.
Acknowledgements
The authors would like to thank all the participating school staff for kindly completing the survey. The authors are also grateful to PHE Staff who helped with the surveillance: Alpa Shah, Corinne Whillock, Paul Charter, Dawn Phillips, Deborah Cohen, Emily-Jane Picton, Francine Stalham, Julie Brough, Michael Lattimore, Oliver Martin, Shahin Parmar, and Teresa Gibbs
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.lanepe.2021.100120.
Appendix. Supplementary materials
References
- 1.Viner R.M., Russell S.J., Croker H. School closure and management practices during coronavirus outbreaks including COVID-19: a rapid systematic review. Lancet Child Adolesc Health. 2020;4(5):397–404. doi: 10.1016/S2352-4642(20)30095-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ladhani S.N., Amin-Chowdhury Z., Davies H.G. COVID-19 in children: analysis of the first pandemic peak in England. Arch Dis Child. 2020;105(12):1180–1185. doi: 10.1136/archdischild-2020-320042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Viner R.M., Bonell C., Drake L. Reopening schools during the COVID-19 pandemic: governments must balance the uncertainty and risks of reopening schools against the clear harms associated with prolonged closure. Arch Dis Child. 2020 doi: 10.1136/archdischild-2020-319963. Aug 3:archdischild-2020-319963. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Levinson M., Cevik M., Lipsitch M. Reopening Primary Schools during the Pandemic. N Engl J Med. 2020 doi: 10.1101/2020.07.19.20157362. 2020 Jul 24;2020.07.19.20157362Preprint. [DOI] [PubMed] [Google Scholar]
- 5.Public Health England (PHE). Weekly coronavirus disease 2019 (COVID-19) surveillance report: summary of COVID-19 surveillance systems. Avaliable at:https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/880925/COVID19_Epidemiological_Summary_w17.pdf. Accessed 25 February 2021.
- 6.Prime Minister's Office. Prime Minister's statement on coronavirus (COVID-19): 23 march 2020. Avaliable at: https://www.gov.uk/government/speeches/pm-address-to-the-nation-on-coronavirus-23-march-2020. Accessed 05 August 2020.
- 7.Deapartment for Education (DfE) 27 July 2020. Guidance for full opening: schools.https://www.gov.uk/government/publications/actions-for-schools-during-the-coronavirus-outbreak/guidance-for-full-opening-schools Avaliable at: [Google Scholar]
- 8.Department for Education (DfE). Attendance in education and early years settings during the coronavirus (COVID-19) outbreak: 23 March to 9 July 2020. Avaliable at:https://www.gov.uk/government/statistics/attendance-in-education-and-early-years-settings-during-the-coronavirus-covid-19-outbreak-23-march-to-9-july-2020. Accessed 05 August 2020.
- 9.Ismail S., Saliba V., Lopez-Bernal J., Ramsay M., Ladhani S. SARS-CoV-2 infection and transmission in educational settings: cross-sectional analysis of clusters and outbreaks in England. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30882-3. Dec 8;S1473-3099(20)30882-3Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Department for Education (DfE) Published: 2 July 2020. Guidance: actions for schools during the coronavirus outbreak. What all schools will need to do during the coronavirus (COVID-19) outbreak.https://www.gov.uk/government/publications/actions-for-schools-during-the-coronavirus-outbreak Last updated 22 February 2021. Avaliable at: [Google Scholar]
- 11.Department for Education (DfE). Schools coronavirus (COVID-19) operational guidance, February 2021. Avaliable at:https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/964351/Schools_coronavirus_operational_guidance.pdf. Accessed 01 February 2021.
- 12.Public Health England (PHE) 8 October 2020. Official statistics: national flu and COVID-19 surveillance reports. National influenza and COVID-19 report, monitoring COVID-19 activity, seasonal flu and other seasonal respiratory illnesses.https://www.gov.uk/government/statistics/national-flu-and-covid-19-surveillance-reports (updated 17 December 2020). Avaliable at: [Google Scholar]
- 13.UK Government. Get a free NHS test to check if you have coronavirus, 2020. Avaliable at: https://www.gov.uk/get-coronavirus-test. Accessed 25 February 2021.
- 14.Otte I.M., Kampe E., Lehfeld A.S., Buda S., Buchholz U., Haas W. Surveillance of COVID-19 school outbreaks, Germany, March to August 2020. Euro Surveillance. 2020;25(38) doi: 10.2807/1560-7917.ES.2020.25.38.2001645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Macartney K., Quinn H.E., Pillsbury A.J. Transmission of SARS-CoV-2 in Australian educational settings: a prospective cohort study. Lancet Child Adolesc Health. 2020;4(11):807–816. doi: 10.1016/S2352-4642(20)30251-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.National Institute for Public Health and the Environment (RIVM) TN . 2020. Children and COVID-19.https://www.rivm.nl/en/novel-coronavirus-covid-19/children-and-covid-19 Avaliable at: [Google Scholar]
- 17.Couzin-Frankel J., Vogel G., Weiland M. Not open and shut. Science. 2020;369(6501):241–245. doi: 10.1126/science.369.6501.241. [DOI] [PubMed] [Google Scholar]
- 18.Stein-Zamir C., Abramson N., Shoob H. A large COVID-19 outbreak in a high school 10 days after schools' reopening, Israel, May 2020. Euro Surveillance. 2020;25(29) doi: 10.2807/1560-7917.ES.2020.25.29.2001352. doi: 2001310.2002807/2001560-2007917.ES.2002020.2001325.2001329.2001352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fontanet A., Tondeur L., Madec Y. Cluster of COVID-19 in northern France: a retrospective closed cohort study. MedRxiv. 23 April 2020 doi: 10.1101/2020.04.18.20071134. [DOI] [Google Scholar]
- 20.Fontanet A., Grant R., Tondeur L. SARS-CoV-2 infection in primary schools in northern France: a retrospective cohort study inan area of high transmission. MexRxIV. 29 June 2020 doi: 10.1101/2020.06.25.20140178. [DOI] [Google Scholar]
- 21.Viner R.M., Mytton O.T., Bonell C. Susceptibility to and transmission of COVID-19 amongst children and adolescents compared with adults: a systematic review and meta-analysis. JAMA Pediatr. 2020 doi: 10.1001/jamapediatrics.2020.4573. Sep 25Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Park Y.J., Choe Y.J., Park O. Contact tracing during coronavirus disease outbreak, South Korea, 2020. Emerg Infect Dis J. 2020;26(10):2465–2468. doi: 10.3201/eid2610.201315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Castagnoli R., Votto M., Licari A. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in children and adolescents: a systematic review. JAMA Pediatr. 2020;174(9):882–889. doi: 10.1001/jamapediatrics.2020.1467. Sep 1. [DOI] [PubMed] [Google Scholar]
- 24.Ludvigsson J.F. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. 2020;109(6):1088–1095. doi: 10.1111/apa.15270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Department of Health and Social Care (DHSC) 15 April 2020. Coronavirus (COVID-19): getting tested. Guidance on coronavirus testing, including who is eligible for a test and how to get tested.https://www.gov.uk/guidance/coronavirus-covid-19-getting-tested (updated 14 December 2020); Avaliable at: [Google Scholar]
- 26.Office for National Statistics (ONS). Coronavirus (COVID-19) infection survey, UK: 6 November 2020. Avaliable at: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/coronaviruscovid19infectionsurveypilot/6november2020#age-analysis-of-the-number-of-people-in-england-who-had-covid-19. Accessed 12 December 2020.
- 27.Mensah A., Sinnathamby M., Zaidi A. SARS-CoV-2 Infections in Children Following the Re-Opening of Schools and the Impact of National Lockdown during Autumn 2020: prospective, National Observational Cohort Surveillance, England. J Infect. 2021 doi: 10.1016/j.jinf.2021.02.022. Feb 25; S0163-4453(21)00093-1Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.