ABSTRACT
Background: The body-oriented therapeutic approach Somatic Experiencing® (SE) treats post-traumatic symptoms by changing the interoceptive and proprioceptive sensations associated with the traumatic experience. Filling a gap in the landscape of trauma treatments, SE has attracted growing interest in research and therapeutic practice, recently.
Objective: To date, there is no literature review of the effectiveness and key factors of SE. This review aims to summarize initial findings on the effectiveness of SE and to outline method-specific key factors of SE.
Method: To gain a first overview of the literature, we conducted a scoping review including studies until 13 August 2020. We identified 83 articles of which 16 fit inclusion criteria and were systematically analysed.
Results: Findings provide preliminary evidence for positive effects of SE on PTSD-related symptoms. Moreover, initial evidence suggests that SE has a positive impact on affective and somatic symptoms and measures of well-being in both traumatized and non-traumatized samples. Practitioners and clients identified resource-orientation and use of touch as method-specific key factors of SE. Yet, an overall studies quality assessment as well as a Cochrane analysis of risk of bias indicate that the overall study quality is mixed.
Conclusions: The results concerning effectiveness and method-specific key factors of SE are promising; yet, require more support from unbiased RCT-research. Future research should focus on filling this gap.
KEYWORDS: Somatic experiencing, bottom-up-therapy, trauma therapy, posttraumatic stress disorder, PTSD, scoping literature review
HIGHLIGHTS
This is to our knowledge the first literature review of the effectiveness and key factors of Somatic Experiencing (SE).
Results provide preliminary evidence that SE is an effective treatment of PSTD related symptoms and may be also usefull in the treatment of other disorders.
Short abstract
Antecedentes: Somatic Experiencing® (SE), abordaje terapéutico enfocado en el cuerpo, trata los síntomas postraumáticos mediante al modificación de las sensaciones interoceptivas y propioceptivas asociadas a la experiencia traumática. Al subsanar una brecha en el repertorio de tratamientos para el trauma, la ES ha atraído recientemente un creciente interés en investigación y en la práctica terapéutica.
Objetivo: A la fecha, no existe una revisión de la literatura sobre la efectividad y los factores clave de la ES. Esta revisión tiene por objetivo el resumir los hallazgos iniciales sobre la efectividad de la ES y describir los factores claves específicos del método aplicado en la ES.
Métodos: Para obtener un primer panorama general de la literatura, realizamos una revisión del alcance de la literatura incluyendo estudios publicados hasta el 13 de agosto del 2020. Identificamos 83 artículos, de los cuales 16 cumplían con los criterios de inclusión y fueron analizados de manera sistemática.
Resultados: Los hallazgos brindan evidencia preliminar sobre efectos positivos de la ES en síntomas relacionados al trastorno de estrés postraumático (TEPT). Asimismo, la evidencia inicial sugiere que la ES tiene un impacto positivo sobre síntomas afectivos y somáticos, y sobre indicadores de bienestar tanto en muestras de personas traumatizadas como en no traumatizadas. Los facultativos y los clientes identificaron recursos de orientación y el uso del tacto como los factores clave específicos del método aplicado en la ES. Sin embargo, tanto una evaluación general de la calidad de los estudios como un análisis Cochrane para el riesgo de sesgo mostraron que la calidad general del estudio es mixta.
Conclusiones: Los resultados relacionados a la efectividad y a los factores clave específicos del método aplicado en la ES son prometedores; no obstante, se requiere mayor sustento proveniente de ensayos clínicos aleatorizados sin sesgo. Las investigaciones futuras deberían enfocarse en subsanar esta brecha.
PALABRAS CLAVE: Experiencia somática, terapia de abajo hacia arriba, terapia de trauma, trastorno de estrés postraumático, TEPT, revisión del alcance de la literatura
Short abstract
背景: 躯体体验 ®(SE) 这一身体取向治疗方法通过改变创伤经历相关的内感觉和本体感觉来治疗创伤后症状。 SE填补了创伤治疗领域的空白, 最近在研究和治疗实践中引起了越来越多的兴趣。
目的: 至今尚无文献综述SE的有效性和关键因素。本综述旨在总结SE有效性的初步发现, 并概述SE方法特定关键因素。
方法: 为了获得第一篇文献综述, 我们进行了范围综述, 纳入直到2020年8月13日的研究。我们鉴定了83篇文章, 其中16篇符合纳入标准, 并进行了系统性分析。
结果: 这些发现为SE对PTSD相关症状的正性作用提供了初步证据。此外, 初步证据表明, SE对受创伤和未受创伤的样本的情感和躯体症状以及幸福感都有积极影响。从业者和客户将资源取向和使用触摸作为SE方法特定关键因素。然而, 总体研究质量评估以及偏倚风险的Cochrane分析表明总体研究质量混杂不齐。
结论: SE的有效性和方法特定关键因素的结果是有希望的; 但是, 需要来自无偏RCT研究的更多支持。未来研究应着重于填补这一空白。
关键词: 躯体体验, 自下而上疗法, 创伤疗法, 创伤后应激障碍, PTSD, 范围文献综述
In traumatic situations, people are pushed beyond the limits of their mental and physical capacity. These events trigger a strong stress reaction and may lead to serious psychological and physical illnesses such as post-traumatic stress disorder (PTSD; e.g. Brady, Killeen, Brewerton, & Lucerini, 2000). According to the DSM-V criteria (American Psychiatric Association [APA], 2014) the characteristic symptoms of PTSD can be classified into three symptom groups: intrusions (involuntary and stressful memories of the trauma), avoidance of the trauma associated stimuli, and persistent physiological hyperarousal. Unlike other mental disorders, PTSD has a particularly high persistence and low levels of spontaneous remission (Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995). Moreover, people with PTSD symptoms report high levels of suffering and have an increased chance of developing additional mental disorders (e.g. Stewart, Pihl, Conrod, & Dongier, 1998). Thus, it is important to identify effective interventions for the treatment of PTSD and to pursue new approaches that can successfully complement the existing ones.
A recent comparative effectiveness review reports a growing number of RCTs in the treatment of PTSD (O’Neil et al., 2020). By now, research on non-pharmacological approaches has focused primarily on cognitive-behavioural and exposure-based procedures to treat PTSD (e.g. Watts et al., 2013). These approaches address the dysfunctional cognitive and affective processing of traumatic experiences and try to teach a new way of dealing with the trauma. Numerous studies show that these procedures can lead to a significant reduction in post-traumatic symptoms (e.g. Watts et al., 2013). Cognitive-behavioural and exposure-based interventions can thus be an effective way to treat PSTD.
However, cognitive-behavioural and exposure-based interventions do not help all clients to reduce their PTSD-symptoms (e.g. Corrigan & Hull, 2015). Cognitive, language-based interventions require a substantial amount of cognitive processing. Yet, people who suffer from traumatic experiences show impaired cognitive functioning due to the increased negative affect that they are experiencing in trauma-related situation (Mujica-Parodi, Greenbag, & Kilpatrick, 2004; Van der Kolk, 2016). Thus, the trauma-related cognitive malfunction may reduce the efficacy of cognitive-behavioural treatments (Van der Kolk & Fisler, 1995). Additionally, exposure-based interventions frequently used in cognitive-behavioural therapy result in high drop-out rates due to the confrontational, aversive nature of the intervention (Lewis, Roberts, Gibson, & Bisson, 2020; Wald & Taylor, 2008). As a result, the last decade witnessed the development of complementing, body-oriented approaches aiming at changing the physiological and emotional processing of the traumatic experience in a ‘bottom-up’ instead of ‘top-down’ way (Van der Kolk, 1994, 2016). In contrast to top-down approaches, bottom-up procedures focus on the body and the ‘body memory’. In other words, these approaches emphasize the importance of subcortical brain levels, such as the brain stem and limbic system. Starting from these more ‘primitive’ brain structures and their embodied reactions, bottom-up approaches aim at changing the way the body responds to trauma experiences and are working upwards towards higher cortical systems (Levine, 1997; Van der Kolk, 2016).
1. Somatic experiencing
Among others, the ‘bottom-up’ approach Somatic Experiencing® (SE; Levine, 1997) has emerged as a promising intervention for the treatment of PSTD (see case reports: case of ‘Nancy’, Levine, 2008; case of ‘Simon’, Payne, Levine, & Crane-Godreau, 2015). It focuses on resolving the symptoms of chronic stress and post-traumatic stress (Payne et al., 2015). SE is a body-oriented therapeutic approach that focuses on the psychophysiological consequences of the traumatic event. SE is based on a generalized psychobiological model of resilience (Levine, 1997). According to SE, post-traumatic stress symptoms originate from a permanent overreaction of the innate stress system due to the overwhelming character of the traumatic event. In the traumatic situation, people are unable to complete the initiated psychological and physiological defensive reaction (e.g. prolonged freeze instead of fight or flight; Levine, 1997). This leads to a persistent somatic and emotional dysregulation of the nervous system and results in the chronically increased stress reaction that is observed in clients with PTSD.
Therefore, the primary goal of SE is to modify the trauma-related stress response (Ogden & Minton, 2000). To achieve this, its major interventional strategy builds on bottom-up processing. Clients’ attention is directed to internal sensations, both visceral (interoception) and musculoskeletal (proprioception and kinaesthesis), rather than to primarily cognitive or emotional experiences. This is an important divergence from cognitive-behavioural therapy that focusses primarily on the cognitive and emotional experience associated with the trauma. In doing this, clients are trained to gradually reduce the arousal associated with the trauma by increasingly tolerating and accepting the inner physical sensations and related emotions and by activating internal and external resources, such as identifying parts of the body or memories that are associated with a positive and reassuring feeling. The resulting increase in interoceptive and proprioceptive awareness leads to a ‘discharge process’ after which the trauma-related activation is resolved (Brom et al., 2017; Payne et al., 2015). An important divergence from exposure-based therapy is that clients do not have to relive the whole traumatic event again to reduce the stress-reaction. The SE therapeutic intervention specifically avoids direct and intense evocation of traumatic memories. Trauma-related memories are approached indirectly and very gradually. Additionally, the generation of new corrective interoceptive experiences that physically contradict those of overwhelm and helplessness are facilitated (Payne et al., 2015). By this so-called process of ‘renegotiating’ (Levine, 1997) the clients’ traumatic stress reaction related to the trauma is modified in an adaptive and holistic manner.
As mentioned above, SE is based on a generalized psychobiological model of resilience (Levine, 1997). Thus, the psychophysiological dysregulation that occurs in a traumatic situation is expected to be associated with other mental disorders such as panic disorder, depression, or chronic pain (e.g. Carney, Freedland, & Veith, 2005; Chrousos, 2009; Cohen et al., 2000) as well. In these cases, the bottom-up approach aims to promote clients’ ability for self-regulation, thereby contributing to a stress-reduction and finally to an improvement in symptoms. Although originally developed to treat trauma-related disorders, SE is therefore increasingly used in clinical practice to treat other mental disorders as well (Foundation for Human Enrichment, 2007; Levine, 1997; Payne et al., 2015).
Moreover, some specific interventions are designed which are based on SE principles for application in specific settings. One example is the trauma resilience model (TRM). It was developed by Leitch and Miller-Karas as a brief, early intervention used for stabilization in disaster and emergency settings (Leitch & Miller-Karas, 2009).
2. The present study
Despite the high interest in clinical practice and a growing number of empirical studies on SE, there is still no literature overview of the current state of knowledge of SE. The aim of the present study is to provide a literature overview of research on SE with a focus on initial evidence for the effectiveness of this approach. Furthermore, we aimed to identify method-specific key factors of SE to outline avenues for future research.
3. Method
Considering the novelty of the research field regarding SE and the heterogeneity of the existing literature, we decided to apply a scoping review approach (Arksey & O’Malley, 2005). Arksey and O’Malley (2005) proposed that a scoping review is informative when a) a research field is still in its early stages of development, b) the overall aim is to cover a broader research question including many different study designs, and/or c), when the research field is less likely to address specific research questions.
3.1. Identifying the research questions
Arksey and O’Malley (2005) recommend to maintain a wide approach to cover a broad range of studies and topics. Consistently, in the initial stage, we conducted an exploratory literature research. After screening the results, we specified inclusion and exclusion criteria in an iterative process to focus on the two central research questions present in the field (for details, see Supplement Material Section I): What is known about the effectiveness of the SE approach? And what are method-specific key factors of SE?
3.2. Literature search strategy
We identified relevant studies using the databases PubPsych, Pubmed, PSYNDEX, PSYJournals, PsycINFO, and PsycARTICLES as well as Google Scholar and Google using the following search terms: ‘somatic experiencing’, ‘SE’, or in combination with ‘trauma’, ‘body therapy’ or ‘body trauma therapy’. The search was extended by tracking the references in identified hits and by checking the publication lists of authors, who published identified, relevant studies on SE. Additionally, the bibliography of the somatic experiencing training manual (Foundation for Human Enrichment, 2007) served as a supplementary source of information for potential articles. Finally, expert interviews with SE trainers were conducted, resulting in the identification of further valuable sources of literature.
3.3. Eligibility criteria
After screening the initial findings, we added relevant points to the criteria in several steps until we finally obtained a set of studies with sufficient methodological soundness and adequate content.
We included all studies that met the final inclusion criteria: 1) They were published in peer-reviewed journal articles, dissertations or clinical research project reports that were available in the above-mentioned databases up to and including 13 August 2020; and 2) were available in German or English. 3) The studies included quantitative and qualitative empirical analysis of SE with sample sizes of N > 1; and 4) tested SE as a therapeutic intervention in isolation or in combination with another therapeutic intervention. We excluded all studies that 1) investigated SE in combination with more than one other therapeutic method; 2) explained only theoretical aspects of SE; 3) placed SE in a new neuroscientific framework model; or 4) discussed theoretical differences between SE and another therapeutic approach.
We did not define any inclusion/exclusion criteria concerning outcome measures and intervention details (e.g. number of SE sessions or duration of treatment). Details of the search and selection process are reported in Figure 1 and in Sections I and II of the Supplemental Online Material.
Figure 1.
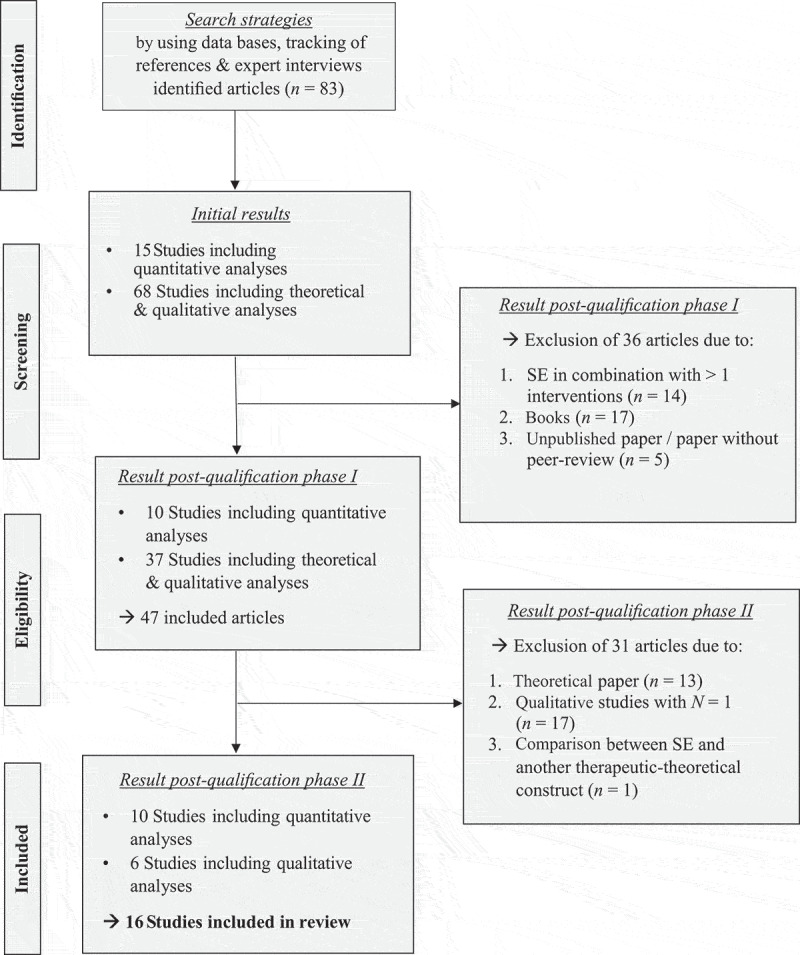
PRISMA flow diagram
3.4. Data analysis
The aim of the present scoping review was to present and summarize all data reviewed without seeking to quantitatively assess quality of evidence (Arksey & O’Malley, 2005). Still, a critical quality evaluation of the studies was conducted by implementing an overall quality assessment and a Cochrane risk of bias assessment (Higgins & Green, 2008).
We use descriptive data to summarize the studies (see Table 1), list the studies’ overall quality assessment (see Table 2) and the Cochrane risk of bias (see Tables 3 and 4), and, finally, document the reported effect sizes as well as other statistical information and results documented in the original quantitative studies (see Tables 5 and 6). We used counts and proportions to report all other data. No inferential statistical testing was performed in the present study.
Table 1.
Characteristics of the included studies
| Sample |
||||||||
|---|---|---|---|---|---|---|---|---|
| Study | Study Design | Research Question | Sample Size(n) | Inclusion Criteria | Gender Composition | Age (years) | Exclusion Criteria | Setting |
| [1] Brom et al. (2017)+ | Randomized controlled trial | Is SE effective in treating patients with PTSD? | 63 | PTSD diagnosis according to DSM-IV-TR (various types of trauma), fluent in either Hebrew or English, ≥ 18 years | EG: 15 f; 18 m CG: 17 f; 13 m | 40.51 (mean) | History of psychosis, brain damage, active suicidal tendencies, substance use, psychiatric comorbidity apart from depression, complex traumas (collected via SCID) | Israel |
| [2] Andersen et al. (2017)+ | Randomized controlled trial | Is SE effective in treating patients with chronic low back pain and comorbid PTSD? | 91 | Chronic low back pain, diagnosis of PTSD according to Harvard Trauma Questionnaire part IV (various types of trauma), ≥18 years | 54.2 % f 45.8 % m | 50.6 (mean) | Serious psychiatric comorbid diseases (bipolar, depression, psychosis or drug dependence) other ongoing psychotherapeutic interventions | Denmark |
| [3] Changaris (2010)+ | Case-control study | Is SE effective as a short-term intervention for the treatment of anxiety and depression symptoms in homeless adults? | 36 | Homeless adults living in a shelter in California | EG: 10 f; 8 m CG: 10 f; 8 m | EG: 48.2 (mean) CG: 49.2 (mean) |
No information | USA, California |
| [4] Parker, Doctor & Selvam (2008)+ | Uncontrolled field study | Is SE as a short-term intervention effective for the treatment of volunteers traumatized by a tsunami in India? | 150 | Survivors of the tsunami in South India, Tamil Nadu (2004), current experience of trauma symptoms (agreement in 8 of 17 items of the IES-R-A) | no information | 41.6 (mean) | No information | India, Tamil Nadu |
| [5] Leitch (2007)+ | Uncontrolled study | Is SE/TFA as a short-term intervention effective for the treatment of participants traumatized by a tsunami in Thailand? | 53 | Tsunami survivors in Thailand, Phang Nga (2004) | 64% f; 36 % m | Children: 3-15 (N = 9) Adults: 20-75 (N = 44) |
No information | Thailand, Phang Nga |
| [6] Leitch, Vanslyke & Allen (2009)+ | Case-control study | Is SE/TRM as a short-term intervention effective for the treatment of traumatizedd social workers working in crisis services? | 142 | Social workers who have experienced Hurricanes Katrina & Rita in New Orleans (2005) and are working in crisis management | 85.6 % f; 14.4 % m | 22-55 | No information | USA, New Orleans & Baton Rouge |
| [7] Leitch & Miller-Karas (2009)+ | Uncontrolled study | How is the TRM/SE training evaluated in the context of the earthquake relief project in China (2008)? | 350 | Doctors, nurses, teachers & consultants who had personally experienced the earthquake and were in professional contact with others affected | No information | 25-50 | No information | China |
| [8] Briggs, Hayes & Changaris (2018)+ | Uncontrolled study | Is SE effective in increasing the resilience in people with transgender identity in the face of discrimination and social injustice? | 7 | Participants with self-identification as transgender/gender non-conforming/gender variant, ≥ 18 years | No information | No information | No information | USA |
| [9] Winblad, Changaris & Stein (2018)+ | Uncontrolled longitudinal study | Does the three-year SE training lead to increased resilience & physical/mental health in the students? | 18 | Participants in the 3-year SE training course; psychologists, medical doctors, social workers, psychiatrists, physical therapists & other body oriented therapists | 16 f; 2 m | No information | No information | USA |
| [10] Rossi (2014) | Uncontrolled study | How does the SE beginning level of training affect the professional and personal lives of the students? | 54 | Students of the 3-year SE training course | 89 % f; 11 % m | 24-78 | No information | Brasil |
| [11] Olssen (2013) | Uncontrolled study | Why does SE work in the treatment of trauma in the view of mental health practitioners? | 10 | Mental health professionals, fully certified SE-training (N = 5) or in the second/third SE training years (N = 5) | 9 f; 1 m | No information | No information | USA |
| [12] McMahon (2017) | Uncontrolled study | How do traumatized patients benefit from SE from practitioner’s perspective & which clients are best suited for SE? | 3 | Mental health practitioners with fully certified SE-training | No information | No information | No information | USA |
| [13] Hays (2014) | Uncontrolled study | How does the therapeutic integration of SE and psychodynamic psychotherapy impact the work with traumatized clients from practitioner`s perspective? | 4 | Licensed psychotherapists with psychodynamic orientation & completed certified SE training; integrative use of both methods in therapeutic treatment of trauma | 1 f; 3 m | 40-68 | No information | USA |
| [14] Gomes (2014) | Case-control study | How does the inclusion of touch and movement elements in the SE therapy affect its success? | 10 | Women traumatised by experienced domestic violence, no previous psychotherapy, time of issue prevalence:1-3 years, no current sharing home with the aggressor | 10 f | 25-40 | No information | USA |
| [15] Nickerson (2015) | Uncontrolled study | Is SE effective in treating traumatized, politically persecuted Tibetan refugees? | 17 | Tibetan refugees; participants of the 1-year integration program of the GuChuSum association for former political prisoners | 7 f; 5 m | 18-80 | No information | India |
| [16] Ellegaard & Pedersen (2012)+ | Uncontrolled study | How does a combined intervention of SE- & Gestalt therapy influence a patient`s capacity to cope with chronic low back pain when its coupled with depression? | 6 | Patients with moderate depression score (BDI score of 23-30) & chronic low back pain (high pain score of 7-10 on scale 0-10) & attendance at 5-6 psychotherapeutic sessions | 4 f; 2 m | 20-33 | No information | Denmark |
| Intervention |
Measurement Points |
||||||
|---|---|---|---|---|---|---|---|
| Study | Experimental Group | Control Group | Instruments | pre | post | follow-up | follow-up II |
| [1] Brom et al. (2017)+ | 15 weekly individual SE-sessions (N = 30); Duration SE- sessions: 60 min | Waiting list (N=33) | (1) PTSD symptoms: CAPS & PDS; (2) Symptoms of depression: CES-D |
Yes | Yes | 15 weeks | No |
| [2] Andersen et al. (2017)+ | 6-12 individual SE-sessions + TAU (N = 45) Duration SE-sessions: 60 min. | TAU: 4-12 sessions of supervised exercises for low back pain by physiotherapists (N = 46) | (1) PTSD symptoms: HTQ-IV; (2) Kinesiophobia: TSK; (3) Disability related to low back pain: RMDQ; (4) Pain intensity: NRS; (5) Pain catastrophizing: PCS | Yes | No | 12 months | No |
| [3] Changaris (2010)+ | 1-3 individual SE-sessions + 4-weekly affect regulation skills workshop + TAU (N = 18); Duration SE-sessions: no information | TAU: multiple types of therapeutic activities of the shelter | (1) Anxiety symptoms: STAI; (2) Depression symptoms: BDI-II | Yes | No | 7-35 days | No |
| [4] Parker, Doctor & Selvam (2008)+ | 1 modified individual SE-session Duration SE-session: about 75 min | No information | (1) Emotional and bodily stress reactions: self-developed 17-item Post-Tsunami Symptom Checklist; (2) PTSD symptoms: IES-R-A (5 of the 17 items); (3) Presenting Post-Tsunami Symptoms: self-developed score based on the main symptoms of the participants & previous medical treatment | Yes | Yes | 4 months | 8 months |
| [5] Leitch (2007)+ | 1-3 individual SE/TFA-sessions; Duration SE-sessions: 40-60 min | No information | (1) Post-Tsunami-Symptom-tracking: self-developed checklist with demographic info & three (reported and observed) main symptoms; (2) Qualitative data about key interventions in an SE/TFA-session: Case-study form | Yes | Yes | 3-5 days | 12 months |
| [6] Leitch, Vanslyke & Allen (2009)+ | 1-2 individual SE/TRM-sessions + TAU (N = 91) Duration SE-sessions: 40-60 min | TAU: multiple types of therapeutic activities of the shelter, e.g. acupuncture, massage, work skills (N = 18) | (1) Coping: self-developed 4-Item-Skala (α = .79); (2) Physical & psychological symptomatology: SCL-90-R; (3) PTSD symptoms: PCL-C; (4) Resiliency: self-developed 7-Item-Skala (α = .85) | Yes | No | 3-4 months | No |
| [7] Leitch & Miller-Karas (2009)+ | Participation in the TRM/SE training course; Duration TRM/SE-training: 0.5-3 days; theory lectures & 1-2 days supervised field work with traumatised earthquake survivors | No information | (1) Training Relevance, Use, and Satisfaction: TRUSS; (2) Training Evaluation: TEF | No | Yes | No | No |
| [8] Briggs, Hayes & Changaris (2018)+ | 10 SE-group-sessions; Duration SE-sessions: 90 min | No information | (1) Stress, depression, anxiety & somatic symptoms: PHQ-SADS; (2) Quality of Life: WHOQoL-BREF | Yes | No | 10 weeks | No |
| [9] Winblad, Changaris & Stein (2018)+ | Participation in the SE training course Duration SE training: 3 years | No information | (1) Quality of Life: WHOQOL-BREF; (2) Stress, depression, anxiety & somatic symptoms: PHQ-SADS | Yes | No | 1 year | 2 & 3 years |
| [10] Rossi (2014) | Participation in the SE beginning level training courses Duration: 3 x four-day sessions | No information | (1) Influence of SE beginning training on professional & personal lives: self-developed questionnaire with open & closed questions | No | Yes | No | No |
| [11] Olssen (2013) | No information | No information | Individual interviews: Implementation: in person (N = 9) & by telephone (N = 1) Duration: 30-60 min; Data evaluation: content analysis using the open coding technique | No | Yes | No | No |
| [12] McMahon (2017) | No information | No information | Individual interviews: Implementation: in person; Duration: 45 - 60 min; Data evaluation: in the context of „Grounded Theory“ by using the open coding technique |
No | Yes | No | No |
| [13] Hays (2014) | No information | No information | Individual interviews: Implementation: in person; Duration: 30 min. – 2.5 h; Data evaluation: Case study analysis (within-case & cross-case analysis) |
No | Yes | No | No |
| [14] Gomes (2014) | One 90-minute individual SE-session + touch and movement protocols session (N = 5) | One 90-minute SE-session (N = 5) | (1) External ratings: Therapist labels own observations and clients’ remarks with adjectives; (2) Self-ratings: emotional/physiological well-being (on a scale from 0-10) | Yes | Yes | No | No |
| [15] Nickerson (2015) | 2-day workshop on the western concept of trauma & 2-6 SE-sessions (three months later) Duration SE-session: 60-75 min. | No information | Individual interviews (each after workshop & SE sessions), researcher observations, written field notes; Data evaluation: thematic content analysis | No | Yes | No | No |
| [16] Ellegaard & Pedersen (2012)+ | 5-6 individual psychotherapeutic sessions (SE + Gestalt therapy) Duration SE/Gestalt-session: no information | No information | Case reports: written field notes from each session; Data evaluation: Ricoeur-inspired method: naive reading, structural analysis & critical interpretation and discussion |
No | Yes | No | No |
Study: + = peer reviewed article; Sample: Sample sizes include initially included subjects; EG = experimental group; CG = control group; f = female; m = male. Interventions: TAU = Treatment as usual; SE = Somatic Experiencing; TFA = Trauma First Aide; TRM = Trauma Resiliency Model;/ = did not occur in the study. Measures: HTQ-IV = The Harvard Trauma Questionnaire part IV; CAPS = Clinician-Administered PTSD Scale; PDS = Posttraumatic Diagnostic Scale; CES-D = Center for Epidemiological Studies Depression Scale; TSK = Tampa Scale for Kinesiophobia; RMQD = Roland Morris Disability Questionnaire: NRS = Numerical Rating Scale for Pain Intensity; STAI = State-Trait Anxiety Inventory; BDI = Beck Depression Inventory; BDI-II – Beck Depression Inventory-II; PCS – Pain Catastrophizing Scale; IES-R-A – Impact of Events Scale-Revised-Abbreviated; SCL-90-R = Symptom Checklist-90-R; PCL-C = PTSD Checklist-Civilian version; TRUSS = Training Relevance, Use, and Satisfaction Scale; TEF = Training Evaluation Form; PHQ-SADS = Patient Health Questionnaire; WHOQOL-BREF = World Health Organization Quality of Life-Brief.
Table 2.
Overall quality assessment of quantitative studies
| Criteria |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| RCT | CG & Matching | Follow-up | N ≥ 40 | N = constant | Test-instruments | Effect sizes | Therapy manual | Practi-tioners | |
| [1] Brom et al. (2017) | (+) | (+) | (+) | (+) | (+) | (+) | (+) | (+) | |
| [2] Andersen et al. (2017) | (+) | (+) | (+) | (+) | (+) | (+) | (+) | (+) | |
| [3] Changaris (2010) | (++) | (+) | |||||||
| [4] Parker et al. (2008) | (+) | (+) | (+) | (+) | (+) | (+) | |||
| [5] Leitch (2007) | (+) | (+) | (+) | ||||||
| [6] Leitch et al. (2009) | (++) | (+) | (+) | (+) | (+) | (+) | (+) | ||
| [7] Leitch and Miller-Karas (2009) | (+) | (+) | / | ||||||
| [8] Briggs et al. (2018) | (+) | (+) | (+) | (+) | |||||
| [9] Winblad et al. (2018) | (+) | (+) | / | / | |||||
| [10] Rossi (2014) | (+) | (+) | / | / | |||||
| n from total | 2 of 10 | 4 of 10 | 6 of 10 | 7 of 10 | 4 of 10 | 5 of 10 | 5 of 7 | 7 of 8 | 5 of 7 |
| Criteria fulfilled in % | 20% | 40% | 60% | 70% | 40% | 56% | 71% | 88% | 71% |
Assessment criteria: RCT: (+), if randomized controlled trial; CG & Matching: (+), if used; (++), if additional matching for EG & CG; Follow-up: (+), if follow-up after ≥ 3 months; N ≥ 40: (+), if N ≥ 40; N = constant: (+), if data collection without drop-outs; Measures: (+), if validity & reliability known; Effect sizes: (+), if calculated; Therapy manual: (+), if manual for SE-therapy used; Practitioners: (+), if SE-Practitioners had finished certified training. Further: RCT = randomized controlled trial; CG = control group;/ = criteria was not fulfilled because in this study examined differently.
Table 3.
Internal risk of bias assessment for randomized controlled trials
| Bias Domain |
||||||
|---|---|---|---|---|---|---|
| Study | Selection bias | Performance bias | Detection bias | Attrition bias | Reporting bias | Other bias |
| Brom et al. (2017) | Randomization: low RoB Allocation: unclear RoB | low RoB | low RoB | high RoB | unclear RoB | high RoB |
| Andersen et al. (2017) | Randomization: low RoB Allocation: low RoB | high RoB | low RoB | low RoB | unclear RoB | high RoB |
Table 4.
Internal risk of bias assessment for non-randomized studies
| Study |
Bias Domain |
||||||
|---|---|---|---|---|---|---|---|
| Time | Pre-interv. dom. | Pre-interv. dom. | At-interv. dom. | Post-interv. dom. | Post-interv. dom. | Post-interv. dom. | Post-interv. dom. |
| Confounding | Selection bias | Information bias | Confounding | Selection bias | Information bias | Reporting bias | |
| Changaris (2010) | moderate RoB | serious RoB | unclear RoB | low RoB | unclear RoB | critical RoB | serious RoB |
| Leitch et al. (2009) | moderate RoB | moderate RoB | moderate RoB | low RoB | moderate RoB | serious RoB | unclear RoB |
| Gomes Silva (2014) | moderate RoB | unclear RoB | moderate RoB | low RoB | low RoB | critical RoB | unclear RoB |
RoB = Risk of bias. Pre-interv. dom. = Pre-intervention domain. At-interv. dom. = At-intervention domain. Post-interv. dom. = Post-intervention domain.
Table 5.
Effectiveness of Somatic Experiencing (SE)
| Study | Instrument | Description | Overall Finding | Pre-Post Effect | Statistical Analysis |
|---|---|---|---|---|---|
| [1] Brom et al. (2017) | CAPS | PTSD | Significant positive effect of intervention compared to control group | Cohen’s d = 1.26 | Mixed model regression analysis |
| PDS | PTSD | Significant positive effect of intervention compared to control group | Cohen’s d = 1.18 | ||
| CES-D | Depression | Significant positive effect of intervention compared to control group | Cohen’s d = 1.08 | ||
| [2] Andersen et al. (2017) | HTQ-IV | PTSD | Significant positive effect of intervention over time in se-group only |
Cohen’s d = .46* | Repeated measures ANOVA |
| TSK | Kinesiophobia | Significant positive effect of intervention over time in se-group only |
Partial η2 = .07 | ||
| RMDQ | Disability related to low back pain | Significant positive effect for intervention & control group; no difference between groups | Partial η2 = .19 | ||
| NRS | Pain intensity | Significant positive effect for intervention & control group; no difference between groups | Partial η2 = .22 | ||
| PCS | Pain catastrophizing | significant positive effect for intervention & control group; no difference between groups | Partial η2 = .06 | ||
| [3] Changaris (2010) | STAI | State-Anxiety | significant positive effect for intervention compared to control | Not reported | Repeated measures ANOVA & independent groups t-test |
| Trait-Anxiety | No significant effect | Not reported | |||
| BDI-II | Depression (somatic symptoms) | Significant positive effect for intervention compared to control | Not reported | ||
| Depression (somatic symptoms) | Significant positive effect for intervention compared to control | Not reported | |||
| [4] Parker et al. (2008) | S.d. stress-checklist | Overall stress reaction | Significant positive effect of intervention over time (pre-post-4m-8m) |
Partial η2 = .09 | Repeated measures ANOVA |
| IES-R-A | PTSD | Significant positive effect of intervention over time (pre-4m-8m) | Not reported | ||
| S.d. symptom-score | Post-tsunami symptoms | Significant positive effect of intervention over time (pre-post-4m-8m) | Partial η2 = .2 | ||
| [6] Leitch et al. (2009) | S.d. coping-scale | Coping | No significant effect | η2 = .00 | One-way ANOVA |
| SCL-90-R | Psychological symptoms | Significant positive effect for intervention compared to control | η2 = .04 | ||
| Physical symptoms | No significant effect | η2 ≤ .00 | |||
| PCL-C | PTSD | Significant positive effect for intervention compared to control | η2 = .07 | ||
| S.d. resilience-scale | Resilience | Significant positive effect for intervention compared to control | η2 = .16 | ||
| [8] Briggs et al. (2018) | PHQ-SADS | Depression | Significant positive effect of intervention | Cohen’s d = 0.68 | One-group-t-test (pre-post-comparison) |
| Somatic symptoms | Significant positive effect of intervention | Cohen’s d = 0.72 | |||
| Anxiety | No significant effect | Not reported | |||
| WHOQOL-BREF | Psychological quality of life | Significant positive effect of intervention | Cohen’s d = 0.71 | ||
| Health related quality of life | No significant effect | Not reported | |||
| Social quality of life | No significant effect | Not reported | |||
| Environmental quality of life | No significant effect | Not reported |
| Non-comparative studies |
|||||||
|---|---|---|---|---|---|---|---|
| Study | Instrument | Overall Finding | |||||
| [5] Leitch (2007) | S.d. post-tsunami-symptom-checklist |
Post: partial/full reduction of reported (observed) symptoms in 67% (95%) of the subjects. follow-up I: partial/full reduction of reported (observed) symptoms in 90% (84%) of the subjects. follow-up II: partial/full reduction of reported (observed) symptoms in 90% (96%) of the subjects. |
|||||
| Qualitative case reports | 8 example comments on the death of family members & friends, the loss of house & fishing boats and growing fear & anxiety; example comment one year after tsunami: ‘Feels stronger, relies on her friends in the village for comfort because she knows she’s not the only one afraid. Would move far away if she had the money.’ | ||||||
| [7] Leitch and Miller-Karas (2009) | TRUSS | 97% rate the training as moderate to very helpful for their own work; 60% as useful for their own self-care | |||||
| TEF | 88% intend to use training frequently in the following two weeks; 82% agree that the training goals have been achieved; most helpful aspects: learning of specific trauma resilience models/SE methods & their application; aspects to be added in the future: practical exercises, demos & case studies | ||||||
| [9] Winblad et al. (2018) | PHQ-SADS | Sig. reduction for anxiety & somatic symptoms for pre & all 3 yearly follow-ups; no data evaluation for depression |
|||||
| WHOQOL-BREF | Sign. improvement of health-related quality of life between pre & all 3 follow-ups; sign. improvement of social quality of life at 3rd follow-up compared to all previous measurements | ||||||
| [10] Rossi (2014) | S.d. questionnaire (quantitative & qualitative evaluation) | 90.70% affirm self-experienced trauma; 90.70% affirm influence of training in professional life (1) getting or adding new tools, (2) using these tools to better help others, (3) ability to amplify the perception of the other, (4) deal better with present profession, (5) direct professional activities towards SE. 96.30% affirm influence of training in personal life: (1) self-perception, (2) self-regulation, (3) perception of patterns of behaviour, (4) new meaning to their life story, (5) perception of the other and of the surroundings, (6) relationships. |
|||||
Instrument: s.d. = self-developed; BDI-II – Beck Depression Inventory-II; CAPS = Clinician-Administered PTBS scale; CES-D = Center for Epidemiological Studies Depression Scale; HTQ-IV = The Harvard Trauma Questionnaire part IV; IES-R-A – Impact of Events Scale-Revised-Abbreviated; PCS – Pain Catastrophizing Scale; PCL-C = PTSD Checklist-Civilian version; PDS = Posttraumatic Diagnostic Scale; PHQ-SADS = Patient Health Questionnaire; PTSD Scale; TSK = Tampa Scale for Kinesiophobia; RMQD = Roland Morris Disability Questionnaire: NRS = Numerical Rating Scale for Pain Intensity; STAI = State-Trait Anxiety Inventory; SCL-90-R = Symptom Checklist-90-R; TEF = Training Evaluation Form; TRUSS = Training Relevance, Use, and Satisfaction Scale; WHOQOL-BREF = World Health Organization Quality of Life-Brief.
*Interaction group x time: partial η2 = .06.
Table 6.
Key factors of Somatic Experiencing (SE)
| Study | Overall Finding | ||
|---|---|---|---|
| [11] Olssen (2013) | (1) Increasing body awareness (the body leads; the body speaks; finish what the body started; the body survives) | (2) Treatment at the client’s pace (going slowly; client readiness & safety; client adjusted & settled within present environment; balancing moving forward with not flooding; educating & coaching) | (3) Client’s empowerment (building distress tolerance; developing a positive resource toolbox; quick & deep healing; increasing client independence; effective symptom management) |
| [12] McMahon (2017) | Importance of fit between client and practitioner (conceptualization of trauma; psychoeducation of the SE approach; clients not benefiting from SE; self-awareness of the SE practitioners) | ||
| [13] Hays (2014) | (1) Approach (Personal Rational & Background; Use of Touch; Psychoeducation & Supervision) | (2) Effects of integration (External client relational changes; Resolution/Reduction of symptoms; Value of integration; Risks & Deficits of integration) | (3) Evidence-Based Best Practices (Need for well-designed studies; Limitations & biases) |
| [14] Gomes Silva (2014) | (1) SE + touch & movement sessions show higher ratings on scale than classical SE sessions [from: Self-assessment (self-developed rating scale)] | (2) Stronger sensory-motor integration & more discharge energy in SE + touch & movement sessions than in classic SE sessions [from external assessment (adjectivations)] | |
| [15] Nickerson (2015) | Conclusion: Cultural understanding of the concept of trauma and therapy too different to be able to identify impact factors. | ||
| [16] Ellegaard and Pedersen (2012) | (1) Significance of previous experiences; | (2) Restrictions in everyday life; | (3) Restoration of inner resources |
4. Results
4.1. Study characteristics
Out of 83 articles identified at the beginning, 16 fulfilled the inclusion criteria. Table 1 reports details on the included studies. To facilitate reading, numbering in the Results section refers to Table 11: Ten quantitative studies [1–10] tested the effectiveness of SE and six qualitative analyses [11–16] investigated method-specific key factors of SE.
4.1.1. Study setting and participants
The included articles were published between 2007 and 2018. The majority of the studies were conducted in the USA (53%). Still, we found further studies conducted in Denmark (12%), India (12%), Brazil (6%), Thailand (6%), China (6%) and Israel (6%). Ten of them have been published in international peer-reviewed journals [1–9, 16]. The sample size varied between N = 3 and N = 350 (total N = 1014). All studies included samples of adult subjects; one study additionally investigated children and adolescents [5]. The following samples were examined: Victims of natural catastrophes such as a hurricanes or tsunamis [4, 5, 6]; students in/after classic [9, 10] or shortened SE training (Trauma Resilience Model; TRM; Leitch & Miller-Karas, 2009) [7]; practicing SE practitioners [11, 12, 13]; subjects with a diagnosis of PTSD due to diverse experienced traumas [1], subjects with chronic low back pain and comorbid PTSD [2] or comorbid depression [16]; homeless adults [3]; subjects with altered gender identity [8]; Tibetan refugees [15]; and women traumatized by domestic violence [14].
4.1.2. Outcome measurements
In the quantitative studies, a total of 24 different test instruments were used, of which only two instruments were used more than once (in two studies).
Overall, the 16 included studies show a great heterogeneity, not only in the type of sample but also in length and format (e.g. individual or group session) of the SE intervention, as well as the research objectives of the studies.
4.2. Quality of included quantitative studies
All ten quantitative studies were systematically analysed and critically evaluated. We derived the overall quality assessment criteria on the basis of the criteria used in previous reviews (e.g. Lemmens, Müller, Arntz, & Huibers, 2016). Additionally, we developed new criteria based on the methodological differences and deficiencies of the included studies. Table 2 provides a summary of studies’ overall quality. Further details on the assessment of overall study quality are provided in Section IV of the Supplemental Online Material.
Two studies [1, 2] were classified as randomized controlled trials, three [3, 6, 14] used a control group without randomization. For these five studies, we conducted a Cochrane risk of bias assessment (Higgins & Green, 2008) resulting in mixed evaluation of the risk of bias with different problems in each study (details see Tables 3 and 4).
4.3. Key findings
We grouped the results in two different sections structured by the two research questions. First, we outline results on the effectiveness of SE in the treatment of PTSD and other psychological disorders. Next, we focus on the results on method-specific key factors of SE.
4.4. Effectiveness
The results of the effectiveness analysis are presented in Table 5. Overall, we found ten studies reporting pre- to post-treatment changes in symptoms. In these ten studies, 24 different test instruments were collected. Only two instruments (WHOQOL-BREF; PHQ-SADS) were used twice in two different studies [8, 9]. The dependent variables were collected at one to four measurement points across all studies. The follow-up measurements covered a period between seven days and 12 months after the first measurement.
In six of the ten studies, the intervention consisted of individual SE sessions [1, 2, 3, 4, 5, 6] and in another of SE group sessions [8]. Studies provided between 1–3 sessions [3, 4, 5, 6] and 6–15 sessions [1, 2, 8]. In the three remaining cases, no SE sessions were held, instead participation in the SE training modules served as an intervention. In only four studies, a control group was established [1, 2, 3, 6]. We grouped the results on effectiveness depending on the dependent variables.
4.4.1. Posttraumatic stress symptoms
In four studies [1, 2, 4, 6], the effects of SE on posttraumatic stress symptoms were investigated. Positive effects of a SE treatment were found for all instruments assessing post-traumatic stress symptoms both in post-treatment and follow-up measurements up to one year. Three of the four studies included a control group and significant effects were found for the experimental group compared to the control group [1, 2, 6].
4.4.2. Depressive and anxiety symptoms
Two [1, 3] of four [1, 3, 8, 9] studies provide a sufficient data basis for a quantitative analysis of the effect of SE on depressive symptoms. Both studies report significant effects of SE in a pre-post comparison for the experimental group that were absent in the control group. Regarding anxiety symptoms, two [3, 9] out of three [3, 8, 9] studies found a significant reduction in anxiety symptoms due to an SE intervention in the follow-up measurements compared to baseline measurements [3, 9] and to control group [3]. The remaining study reported no improvement in anxiety through SE [8].
4.4.3. Specific symptom testing in the context of trauma
Two [4, 5] of three [4, 5, 6] studies analysing the effects of SE during natural disasters, such as tsunamis or hurricanes, showed positive effects of SE on all measures of symptoms assessed by self-developed instruments (post-tsunami symptom scores and stress symptom checklist in [4], descriptive reduction in [5]) between pre-post-follow-up measurements. In the third study [6], the significant reduction in symptoms was achieved on the psychological scale of SCL-R for the experimental group compared to the control group between post and follow-up measurement, while the physical symptom scale of this test showed no changes. Regarding pain-related symptoms in the context of trauma, one study [2] assessed the variables kinesiophobia, pain-related impairment, pain intensity, and pain-related catastrophizing. All assessed variables were significantly reduced in pre to follow-up comparisons. Differences in symptom reduction between experimental and control group were found only for the variable kinesiophobia.
4.4.4. Resilience
In addition, three studies addressed the influence of SE on resilience [6, 8, 9]. Two of them collected the general quality of life (by using the WHOQOL-BREF). There were significant improvements in the social, physical [9] and psychological [8] domains, but not in the environmental domain [8, 9] of the general quality of life questionnaire in pre to follow-up comparisons. These two studies [8, 9] show also a significant [9] or marginally significant [8] improvement in the somatic symptom scale of PHQ-SADS following SE intervention. Beyond that, significant improvements were achieved in a further study [6] on an in-house developed resilience scale in pre to follow-up comparison between control and experimental group, while there were no significant improvements in an in house-developed coping scale of the same study.
4.4.5. User perspective
Finally, two studies evaluated the SE training by implementing one post-measurement after the completed training modules [9, 10]. In both studies, descriptively positive effects of the training on the professional and personal life of the SE trainees could be shown. Consistently, in a third study [7], therapists who worked in crisis areas reported that they benefitted in their work and in their own self-care from an SE/TRM-training on a descriptive level. In these three studies, trainees did not receive an SE-treatment themselves. Thus, they do not inform about the effectiveness of the SE-treatment and method-specific key factors and are excluded from further discussion. Still, it might be an interesting avenue for future research to investigate whether SE leads to positive outcomes for both clients and professionals.
4.5. Method-specific key factors
Six studies addressed the key factors of SE by interviewing both practitioners [11, 12, 13] and clients [14, 15, 16]. The study specific results are listed in detail in Table 6. Further information is reported in Section III of the Supplemental Online Material.
4.5.1. Practitioners’ perspective on method-specific key factors of SE
In the following, we report only the key factors that are considered key aspects for the success of SE across studies and samples.
Physiological conceptualization of trauma
All interviewed practitioners agreed with SE’s basic idea that traumatic events are ‘stored’ in the nervous system and can be resolved by integrating non-verbal, physiological impulses into the therapeutic process. Practitioners proposed that clients who do not agree with this trauma-concept were non-compliant with SE therapy and preferred a standard PTSD-treatment [11, 12, 13].
The importance of psychoeducation
Furthermore, practitioners from all three studies considered the simplicity of the theoretical approach of SE as a key factor of its effectiveness. The theoretical approach provides an easy, comprehensive approach to understand the origin of a trauma and the need for treating symptoms at both the psychological and the physiological level [11, 12, 13].
Establishment of trust and security
Finally, practitioners emphasized that building trust and security in clients is a central factor for a successful SE treatment of trauma. It is of particular importance that clients trust both the therapeutic approach of SE and their own body with its survival mechanisms. In addition, there should be a basic feeling of security before dealing with the trauma [11, 12, 13].
4.5.2. Clients’ perspective on key factors
Reviewing clients’ perspectives on key factors of SE, we quickly realized that studies‘ results were too heterogeneous in terms of sample composition and intervention methods to be able to draw comprehensive conclusions about method-specific key factors [14, 15, 16].
4.5.3. Cross-category key factors
We decided to summarize the key factors that were found both in the reports of practitioners and clients. We identified two method-specific key factors that were reported consistently in three studies [11, 13, 16 & 12, 13, 14] by both clients and practitioners.
Building up resources
Both practitioners and clients reported that the development and work with internal and external resources is an important key factor for the effectiveness of SE. Some qualitative analyses highlight that it is important to perceive the body itself as a central resource. Thus, practitioners should support clients in their ability to regulate and relax themselves. In addition, some analysis outlined that the successful establishment of internal and external resources is a prerequisite for treating the trauma-related experiences [11, 13, 16].
Use of touch in SE
A second overarching factor mentioned by practitioners and clients is the use of touch – either self-touch or soft touch by the therapist – in therapy. In a one-year advanced course, SE practitioners learned techniques for the integrative use of touch in therapy (e.g. a hand contact on a shoulder to provide gentle support and endorse a feeling of safety). According to the theory behind SE (Levine, 1997), touch can be an important key factor in trauma healing as it can support a feeling of safety which is a key to overcoming trauma symptoms. Consistently, the majority of practitioners and clients across three studies rated touch as a supporting factor and as a helpful, effective enhancer in therapeutic treatment [12, 13, 14].
5. Discussion
In recent years, there has been a growing interest in body-oriented psychotherapeutic approaches, especially for the treatment of trauma-related disorders (e.g. Kim, Schneider, Kravitz, Mermier, & Burge, 2013; Metcalf et al., 2016). Among others, Somatic Experiencing® (SE; Levine, 1997) has emerged as a promising approach that focuses on the integration and modification of trauma-related somatic reactions. The aim of the present review was to examine the initial empirical findings on the effectiveness and method-specific key factors of SE.
5.1. Findings on the effectiveness of SE
5.1.1. PTSD
SE was originally developed for the treatment of trauma-related stress symptoms. Consistently, the majority of the studies that were reviewed focused on the effectiveness of SE in the treatment of PTSD. Overall, four of the five studies on PTSD showed significant symptom reductions for all eight dependent variables (Andersen, Lahav, Ellegaard, & Manniche, 2017; Brom et al., 2017; Leitch, Vanslyke, & Allen, 2009; Parker, Doctor, & Selvam, 2008). The fifth study (descriptively evaluated) supports these findings (Leitch, 2007). The identified effects were shown for experimental compared to control group (Andersen et al., 2017; Brom et al., 2017; Leitch et al., 2009), in comparisons between pre- and post-measurement (Brom et al., 2017; Leitch, 2007; Parker et al., 2008) and remained stable in the follow-up measurements (Andersen et al., 2017; Brom et al., 2017; Leitch, 2007; Leitch et al., 2009; Parker et al., 2008). The three studies using a control group (Andersen et al., 2017; Brom et al., 2017; Leitch et al., 2009) showed these effects in experimental-control group comparisons. Three out of four studies evaluated by inferential statistics reported a large beneficial effect of SE (Andersen et al., 2017; Brom et al., 2017; Parker et al., 2008), the fourth (Leitch et al., 2009) a small effect (Cohen, 1988). Taken together, there are initial, but promising findings suggesting a significant, long-term symptom reduction due to SE treatment.
Moreover, these findings show that SE can successfully treat trauma sequelae in different settings and under different conditions. The available studies varied considerably in the duration of the intervention (between 1–2 and 6–15 sessions), the sample characteristics (e.g. age, culture, socioeconomic status), as well as the complexity and cause of the traumatization (e.g. natural disasters, terrorist attacks, car accidents). Still, SE led to a significant symptom reduction in nearly all of the reviewed studies.
5.1.2. Comorbidities
In addition, the present body of research suggests that SE leads to an improvement of comorbid symptoms. We found studies reporting positive effects of SE on comorbid depression symptoms (Brom et al., 2017), pain-related symptoms (Andersen et al., 2017), and post-treatment resilience (Leitch et al., 2009). The effect of SE on pain-related symptoms was shown for the variables kinesiophobia, pain-related impairment, pain intensity, and pain-related catastrophizing. These effects are limited by the fact that the symptom reduction for the last three variables was evident in both experimental and control group. Overall, findings correspond with SE’s objective of a symptom-spanning treatment of PTSD ranging from cognitive and affective to somatic symptoms (Levine, 1997; Payne et al., 2015).
5.1.3. Further symptomatology
An additional focus of the reviewed studies was the treatment of affective symptoms and the enhancement of well-being. In two studies, SE led to a reduction of depressive (Briggs, Hayes, & Changaris, 2018; Changaris, 2010) and anxiety symptoms (Changaris, 2010) that were unrelated to trauma. Two studies showed positive effects on quality of life and somatic symptoms (Briggs et al., 2018; Winblad, Changaris, & Stein, 2018).
5.2. Evaluation of the effectiveness of SE
The available results provide initial, but promising evidence that SE is an effective treatment of PTSD and comorbid symptoms. Moreover, results suggest that SE also has a positive effect on general well-being outside PTSD treatment and may be effective in the treatment of affective and somatic symptoms.
5.2.1. PTSD
Yet, the present findings are limited in several ways. First, by now, there is only a very limited number of studies (n = 5) addressing the effectiveness of SE in the treatment of PTSD with sufficient scientific rigour. Second, two out of five studies on PTSD did not compare SE treatments to adequate control groups. Moreover, these studies used self-developed symptom checklists as dependent variables (Leitch, 2007; Parker et al., 2008). The authors report that they had to adapt the questionnaires to the severe traumatization of the subjects in the investigated crisis areas and thus could not refer to validated standard questionnaires used in PTSD research. The special survey conditions of some studies also resulted in only two out of five studies including exclusively subjects with a confirmed PTSD diagnosis (Andersen et al., 2017; Brom et al., 2017). Furthermore, the assessment of the risk of bias (Higgins & Green, 2008) indicates that the risk of bias is mixed throughout the experimental studies. The overall study quality assessment points out the high heterogeneity of the included studies. Thus, the field of SE research is urging for strong experimental research designs. Still, regarding these limitations, it is important to notice that SE is statistically most effective in the methodologically high-quality randomized controlled trials (Andersen et al., 2017; Brom et al., 2017). Results suggest that the positive effects of SE found in these studies were reduced rather than inflated due to methodological shortcomings.
5.2.2. Further symptomatology
Beyond the treatment of PTSD, it is also apparent that (a) the effects of SE were not stable across all dependent variables, (b) the studies had small sample sizes (Briggs et al., 2018) and (c) a control group was only collected in one of the studies (Changaris, 2010). Due to the small number of available studies (n = 3) and the methodological deficiencies mentioned, findings can therefore be considered only preliminary evidence for the effectiveness of SE outside PTSD.
5.3. Method-specific key factors of SE
Six studies investigated method-specific key factors (Ellegaard & Pedersen, 2012; Gomes Silva, 2014; Hays, 2014; McMahon, 2017; Nickerson, 2015; Olssen, 2013). Across the three studies from practitioner’s perspective, all the practitioners who were interviewed emphasized the following three method-specific key factors: Physiological conceptualization of trauma, psychoeducation, and the establishment of security and trust (Hays, 2014; McMahon, 2017; Olssen, 2013). Moreover, both practitioners and clients emphasized that resource activation (Ellegaard & Pedersen, 2012; Hays, 2014; Olssen, 2013) and the use of touch (Gomes Silva, 2014; Hays, 2014; McMahon, 2017) are method-specific key factors in SE.
These findings are again limited by the fact that studies on key factors in SE (n = 6) are still scarce. Furthermore, these studies are very heterogenous in both study design and study objective. For instance, two out of six studies investigating the key factors of SE analysed a combination of SE with another therapeutic intervention suggesting that the identified key factors in these studies may not be attributed to the SE intervention alone (Ellegaard & Pedersen, 2012; Gomes Silva, 2014).
Still, results provide a first overview of method-specific key factors of SE outlining avenues for future research on SE.
5.4. Limitations and future directions
In the present scoping review, we investigated the state of literature on the effectiveness and key factors of Somatic Experiencing (SE), a body-oriented approach to treat PTSD (Levine, 1997): Overall, the present findings are consistent with previous findings on body-oriented PTSD interventions. In a comprehensive field review, Kim et al. (2013) showed that body-oriented procedures are effective interventions for the treatment of PTSD symptoms and have a positive effect on comorbid symptoms, as well. Consistently, we found preliminary evidence suggesting that SE is an effective approach to treat PTSD and comorbid symptoms (Andersen et al., 2017; Brom et al., 2017; Leitch, 2007; Leitch et al., 2009; Parker et al., 2008). Taken together, findings suggest that body-oriented interventions are a promising approach to treat trauma-related disorders and may complement other interventions in this area.
This review is, to our knowledge, the first literature review of studies on SE. The aim was therefore to provide a comprehensive and broad overview of existing research. For this reason, in addition to checking the databases and search engines, a number of expert interviews were conducted and additional hits were identified by tracking references.
The included studies report promising effects of SE in the treatment of PTSD symptoms. Moreover, the present findings also provide initial evidence that SE may be useful as a body-oriented approach beyond trauma therapy (Briggs et al., 2018; Changaris, 2010; Ellegaard & Pedersen, 2012; Winblad et al., 2018). Consistent with the underlying model of SE to treat PTSD as a psychobiological phenomenon (Levine, 1997), the positive effects of SE treatment were found for diverse outcome measures ranging from affective symptoms to psychosomatic symptoms such as pain.
However, the results must be interpreted with caution. Only few of the studies meet the rigorous methodological criteria (e.g. RCT design) necessary for a robust proof of both efficacy and effectiveness of a clinical treatment.
Therefore, we encourage future research to replicate the previous findings in randomized controlled trials with satisfactory sample sizes to evaluate SE’s efficacy. For this purpose, the development of a standardized therapeutic manual is recommended. Training practitioners in a manualized therapy would reduce the heterogeneity of the interventions examined in the empirical studies. By ensuring a high methodological standard of the SE interventions, future studies may evaluate the efficacy and effectiveness of SE more precisely. In a following step, SE should be compared with other interventions.
A second focus of the present review was to investigate the key factors in SE (Ellegaard & Pedersen, 2012; Gomes Silva, 2014; Hays, 2014; McMahon, 2017; Nickerson, 2015; Olssen, 2013). Consistent with the theoretical foundation of SE (Levine, 1997) and previous reports from SE users, we identified resource activation (Ellegaard & Pedersen, 2012; Hays, 2014; Olssen, 2013) and the use of touch (Gomes Silva, 2014; Hays, 2014; McMahon, 2017) (by both clients and practitioners) as well as physiological conceptualization of trauma, the importance of psychoeducation, and the establishment of security and trust (Hays, 2014; McMahon, 2017; Olssen, 2013) (by practitioners) as method-specific key factors.
The latter represents a key factor that is exclusively used in body-oriented approaches. Thus, we encourage future research to investigate the influence of these key factors and therapeutic outcomes in randomized control-trials and to outline potential implications for standard approaches in trauma therapy.
Although SE was developed as an intervention in the context of trauma therapy, there are reports that practitioners have successfully implemented SE in the treatment of other psychological disorders (Briggs et al., 2018; Changaris, 2010; Ellegaard & Pedersen, 2012; Winblad et al., 2018). In the present scoping review, we found that SE is often used in combination with other treatment procedures (Changaris, 2010; Ellegaard & Pedersen, 2012; Hays, 2014; Nickerson, 2015). Findings suggest that SE is easily integrated in existing therapeutic approaches (e.g. as a supplement to Gestalt therapy (Ellegaard & Pedersen, 2012)). In future studies, the ability to combine SE with other procedures could be systematically investigated. This would make SE useful for the broad field of application and enable synergy effects.
Finally, the present study identified the duration of SE intervention as a potentially important moderating key factor of the effectiveness of SE treatments. Studies with the longest SE interventions (6–12 sessions) also provided the greatest effects in the treatment of posttraumatic stress (Andersen et al., 2017; Brom et al., 2017). Consistently, Changaris (2010) notes that a significant reduction in depressive symptoms with SE was only found after controlling for the number of SE sessions. We suggest that future studies may consider the number of sessions as a moderating factor for the treatment effects on both simple and complex trauma.
6. Conclusion
The present scoping review provides a very first overview of the existing empirical studies on SE. Findings show that research on SE is in an early stage. So far, it provides promising findings indicating that SE might be effective in reducing traumatic stress, affective disorders, and somatic symptoms and in improving life quality. In addition, first method-specific key factors of SE have been identified. SE seems to be characterized in particular by its cross-cultural applicability and its combinability with other therapeutic procedures. The latter might be one of the reasons why SE attracts growing interest in clinical application despite the lack of empirical research. Yet, the current evidence base is weak and does not (yet) fully accomplish the high standards for clinical effectiveness research. Thus, we hope that this review encourages future research to focus on extensive, methodologically rigorous studies to ensure the efficacy and effectiveness of SE in the treatment of trauma-related disorders.
Supplementary Material
Funding Statement
The present study received no funding.
Notes
In addition, a study protocol of a randomized controlled trial, which will be published in full at a later date: Andersen, Ellegaard, Schiøttz-Christensen, and Manniche (2018).
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Since all data is already listed in the paper or the supplement, there is no additional material left to be provided online.
Ethics statement
Due to the nature of a literature review, no new data was collected and no ethics statement is required.
Supplementary material
Supplemental data for this article can be accessed here.
References
References marked with * include all studies that are the result of the scoping review and are presented in Table 1.
- American Psychiatric Association . (2014). Diagnostisches und statistisches manual psychischer Störungen–DSM-5. Göttingen: Hogrefe Verlag. [Google Scholar]
- Andersen, T. E., Ellegaard, H., Schiøttz-Christensen, B., & Manniche, C. (2018). Somatic experiencing® for patients with low back pain and comorbid posttraumatic stress disorder–protocol of a randomized controlled trial. BMC Complementary and Alternative Medicine, 18(1), 308. DOI: 10.1186/s12906-018-2370-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Andersen, T. E., Lahav, Y., Ellegaard, H., & Manniche, C. (2017). A randomized controlled trial of brief somatic experiencing for chronic low back pain and comorbid post-traumatic stress disorder symptoms. European Journal of Psychotraumatology, 8(1), 1–17. DOI: 10.1080/20008198.2017.1331108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arksey, H., & O’Malley, L. (2005). Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology, 8(1), 19–32. DOI: 10.1080/1364557032000119616 [DOI] [Google Scholar]
- Brady, K. T., Killeen, T. K., Brewerton, T., & Lucerini, S. (2000). Comorbidity of psychiatric disorders and posttraumatic stress disorder. The Journal of Clinical Psychiatry, 61(Suppl7), 22–32. https://www.psychiatrist.com/wp-content/uploads/2021/02/24280_comorbidity-psychiatric-disorders-posttraumatic-stress.pdf [PubMed] [Google Scholar]
- *Briggs, P. C., Hayes, S., & Changaris, M. (2018). Somatic experiencing informed therapeutic group for the care and treatment of biopsychosocial effects upon a gender diverse identity. Frontiers in Psychiatry, 9, 1–18. DOI: 10.3389/fpsyt.2018.00053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Brom, D., Stokar, Y., Lawi, C., Nuriel‐Porat, V., Ziv, Y., Lerner, K., & Ross, G. (2017). Somatic experiencing for posttraumatic stress disorder: A randomized controlled outcome study. Journal of Traumatic Stress, 30(3), 304–312. DOI: 10.1002/jts.22189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carney, R. M., Freedland, K. E., & Veith, R. C. (2005). Depression, the autonomic nervous system, and coronary heart disease. Psychosomatic Medicine, 67, 29–33. DOI: 10.1097/01.psy.0000162254.61556.d5 [DOI] [PubMed] [Google Scholar]
- *Changaris, M. C. (2010). Assessing the efficacy of somatic experiencing for reducing symptoms of anxiety and depression (Unpublished Dissertation). John F. Kennedy University. [Google Scholar]
- Chrousos, G. P. (2009). Stress and disorders of the stress system. Nature Reviews. Endocrinology, 5(7), 374–381. DOI: 10.1038/nrendo.2009.106 [DOI] [PubMed] [Google Scholar]
- Cohen, H., Benjamin, J., Geva, A. B., Matar, M. A., Kaplan, Z., & Kotler, M. (2000). Autonomic dysregulation in panic disorder and in post-traumatic stress disorder: Application of power spectrum analysis of heart rate variability at rest and in response to recollection of trauma or panic attacks. Psychiatry Research, 96(1), 1–13. DOI: 10.1016/S0165-1781(00)00195-5 [DOI] [PubMed] [Google Scholar]
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale, NJ: Earlbaum. [Google Scholar]
- Corrigan, F. M., & Hull, A. M. (2015). Neglect of the complex: Why psychotherapy for post-traumatic clinical presentations is often ineffective. BJPsych Bulletin, 39(2), 86–89. DOI: 10.1192/pb.bp.114.046995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Ellegaard, H., & Pedersen, B. D. (2012). Stress is dominant in patients with depression and chronic low back pain. A qualitative study of psychotherapeutic interventions for patients with non-specific low back pain of 3–12 months’ duration. BMC Musculoskeletal Disorders, 13(1), 166. DOI: 10.1186/1471-2474-13-166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foundation for Human Enrichment . (2007). Studienbuch, Somatic Experiencing (SE), Basiskonzept zur Traumabewältigung nach Peter Levine, Ph.D [Study book, Somatic Experiencing (SE), basic concept for coping with trauma according to Peter Levine, Ph.D]. Boulder, CO: Somatic Experiencing Trauma Institute. [Google Scholar]
- *Gomes Silva, S. (2014). Engaging touch and movement in somatic experiencing trauma resolution approach (Unpublished Doctoral Dissertation). International University for Graduate Studies. [Google Scholar]
- *Hays, J. T. (2014). Healing trauma in the psyche-soma: Somatic experiencing in psychodynamic psychotherapy (Unpublished Doctoral Dissertation). Pacifica Graduate Institute. [Google Scholar]
- Higgins, J. P., & Green, S. (2008). Cochrane handbook for systematic reviews of interventions. New Jersey, USA: Wiley-Blackwell. [Google Scholar]
- Kessler, R. C., Sonnega, A., Bromet, E., Hughes, M., & Nelson, C. B. (1995). Posttraumatic stress disorder in the national comorbidity survey. Archives of General Psychiatry, 52(12), 1048–1060. DOI: 10.1001/archpsyc.1995.03950240066012 [DOI] [PubMed] [Google Scholar]
- Kim, S. H., Schneider, S. M., Kravitz, L., Mermier, C., & Burge, M. R. (2013). Mind-body practices for posttraumatic stress disorder. Journal of Investigative Medicine, 61(5), 827–834. DOI: 10.2310/JIM.0b013e3182906862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Leitch, L., & Miller-Karas, E. (2009). A case for using biologically-based mental health intervention in post-earthquake China: Evaluation of training in the trauma resiliency model. Emergency Mental Health, 11(4), 221–233. https://www.researchgate.net/profile/laurie_leitch/publication/44650492_a_case_for_using_biologically-based_mental_health_intervention_in_post-earthquake_china_evaluation_of_training_in_the_trauma_resiliency_model [PubMed] [Google Scholar]
- *Leitch, M. L. (2007). Somatic experiencing treatment with tsunami survivors in Thailand: Broadening the scope of early intervention. Traumatology, 13(3), 11–20. DOI: 10.1177/1534765607305439 [DOI] [Google Scholar]
- *Leitch, M. L., Vanslyke, J., & Allen, M. (2009). Somatic experiencing treatment with social service workers following Hurricanes Katrina and Rita. Social Work, 54(1), 9–18. DOI: 10.1093/sw/54.1.9 [DOI] [PubMed] [Google Scholar]
- Lemmens, L. H., Müller, V. N., Arntz, A., & Huibers, M. J. (2016). Mechanisms of change in psychotherapy for depression: An empirical update and evaluation of research aimed at identifying psychological mediators. Clinical Psychology Review, 50, 95–107. DOI: 10.1016/j.cpr.2016.09.004 [DOI] [PubMed] [Google Scholar]
- Levine, P. A. (1997). Waking the tiger: Healing trauma. The innate capacity to transform overwhelming experiences. Berkeley, CA: North Atlantic Books. [Google Scholar]
- Levine, P. A. (2008). Trauma healing. A pioneering program for restoring the wisdom of your body. Boulder, CO: Sounds True. [Google Scholar]
- Lewis, C., Roberts, N. P., Gibson, S., & Bisson, J. I. (2020). Dropout from psychological therapies for post-traumatic stress disorder (PTSD) in adults: Systematic review and meta-analysis. European Journal of Psychotraumatology, 11(1), 1709709. DOI: 10.1080/20008198.2019.1709709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *McMahon, S. (2017). The body recovers: Practitioner perspective on somatic experiencing (Unpublished Clinical Research Paper). St. Catherine University. [Google Scholar]
- Metcalf, O., Varker, T., Forbes, D., Phelps, A., Dell, L., DiBattista, A., … O’Donnell, M. (2016). Efficacy of fifteen emerging interventions for the treatment of posttraumatic stress disorder: A systematic review. Journal of Traumatic Stress, 29(1), 88–92. DOI: 10.1002/jts.22070 [DOI] [PubMed] [Google Scholar]
- Mujica-Parodi, L. R., Greenbag, T., & Kilpatrick, J. F. (2004). A multi-modal study of cognitive processing under negative emotional arousal. Proceedings of the Annual Meeting of the Cognitive Science Society, 26(26), 30–35. https://escholarship.org/content/qt16c8r6ww/qt16c8r6ww.pdf [Google Scholar]
- *Nickerson, G. L. (2015). Getting to the root of suffering: Dialogues with Tibetan refugee expolitical prisoners on what heals psychological and somatic sequelae of trauma (Unpublished Doctoral Dissertation). Pacifica Graduate Institute. [Google Scholar]
- O’Neil, M. E., Cheney, T. P., Hsu, F. C., Carlson, K. F., Hart, E. L., Holmes, R. S., … Lewis, M. (2020). Pharmacologic and nonpharmacologic treatments for posttraumatic stress disorder: An update of the ptsd-repository evidence base. Rockville, MD: Agency for Healthcare Research and Quality (US). [PubMed] [Google Scholar]
- Ogden, P., & Minton, K. (2000). Sensorimotor psychotherapy: One method for processing traumatic memory. Traumatology, 6(3), 149–173. DOI: 10.1177/153476560000600302 [DOI] [Google Scholar]
- *Olssen, M. C. (2013). Mental health practitioners’ views on why somatic experiencing works for treating trauma (Unpublished Clinical Research Paper). St. Catherine University. [Google Scholar]
- *Parker, C., Doctor, R. M., & Selvam, R. (2008). Somatic therapy treatment effects with tsunami survivors. Traumatology, 14(3), 103–109. DOI: 10.1177/1534765608319080 [DOI] [Google Scholar]
- Payne, P., Levine, P. A., & Crane-Godreau, M. A. (2015). Somatic experiencing: Using interoception and proprioception as core elements of trauma therapy. Frontiers in Psychology, 6(93), 1–18. DOI: 10.3389/fpsyg.2015.00093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Rossi, C. P. (2014). SE beginning level training effects on professional and personal life of students (Unpublished Doctoral Dissertation). Charisma University. [Google Scholar]
- Stewart, S. H., Pihl, R. O., Conrod, P. J., & Dongier, M. (1998). Functional associations among trauma, PTSD, and substance-related disorders. Addictive Behaviors, 23(6), 797–812. DOI: 10.1016/S0306-4603(98)00070-7 [DOI] [PubMed] [Google Scholar]
- Van der Kolk, B. (2016). Verkörperter Schrecken. Lichtenau: G. P. Probst Verlag. [Google Scholar]
- Van der Kolk, B. A. (1994). The body keeps the score: Memory and the evolving psychobiology of posttraumatic stress. Harvard Review of Psychiatry, 1(5), 253–265. DOI: 10.3109/10673229409017088 [DOI] [PubMed] [Google Scholar]
- Van der Kolk, B. A., & Fisler, R. (1995). Dissociation and the fragmentary nature of traumatic memories: Overview and exploratory study. Journal of Traumatic Stress, 8(4), 505–525. DOI: 10.1002/jts.2490080402 [DOI] [PubMed] [Google Scholar]
- Wald, J., & Taylor, S. (2008). Responses to interoceptive exposure in people with posttraumatic stress disorder (PTSD): A preliminary analysis of induced anxiety reactions and trauma memories and their relationship to anxiety sensitivity and PTSD symptom severity. Cognitive Behaviour Therapy, 37(2), 90–100. DOI: 10.1080/16506070801969054 [DOI] [PubMed] [Google Scholar]
- Watts, B. V., Schnurr, P. P., Mayo, L., Young-Xu, Y., Weeks, W. B., & Friedman, M. J. (2013). Meta-analysis of the efficacy of treatments for posttraumatic stress disorder. The Journal of Clinical Psychiatry, 74(6), 541–550. DOI: 10.4088/JCP.12r08225 [DOI] [PubMed] [Google Scholar]
- *Winblad, N. E., Changaris, M., & Stein, P. K. (2018). Effect of somatic experiencing resiliency-based trauma treatment training on quality of life and psychological health as potential markers of resilience in treating professionals. Frontiers in Neuroscience, 12(70), 1–10. DOI: 10.3389/fnins.2018.00070 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Since all data is already listed in the paper or the supplement, there is no additional material left to be provided online.


