Abstract
Background:
Insurance status modifies healthcare access and inequities. The Affordable Care Act expanded Medicaid coverage for people with low incomes in the United States. This study assessed the consequences of this policy change for cancer care after expansion in 2014.
Methods:
National Cancer Database (NCDB) public benchmark reports were queried for each malignancy in 2013 and 2016. Furthermore, a systematic search [PubMed, Embase, Scopus and Cochrane] was performed. Data on insurance status, access to cancer screening and treatment, and socioeconomic disparities in these metrics was collected.
Results:
Two-tailed analysis of the NCDB revealed that 14 out of 18 eligible states had a statistically significant increase in Medicaid-insured patients with cancer after expansion. The average percentage increase was 51% (13.2–204%). From the systematic review, 229 studies were identified, 26 met inclusion. All 21 relevant articles reported lower uninsured rates. The average increase of Medicaid-insured patients was 77% (9.5–230%) and the average decrease of uninsured rates was 55% (13.4–73%). 15 out of 21 articles reported increased access to care. 16 out of 17 articles reported reductions in inequities.
Conclusion:
Medicaid expansion in 2014 increased the number of insured patients with cancer. Expansion also improved access to screening and treatment in most oncologic care, and reduced socioeconomic disparities. Further studies evaluating correlative survival outcomes are needed.
Policy Summary:
This study informs debates on expansion of Medicaid in state governments and electorates in the United States, and on health insurance reform broadly, by providing insight into how health insurance can benefit people with cancer while revealing how less insurance coverage could harm patients with cancer before and after their diagnosis. This study also contributes to discussions of health insurance mandates, subsidized coverage for people with low incomes, and covered healthcare services determinations by public and private health insurance providers in other countries.
Keywords: Patient Protection and Affordable Care Act, Health Insurance, Early Detection of Cancer, Health Services Accessibility, Healthcare Disparities
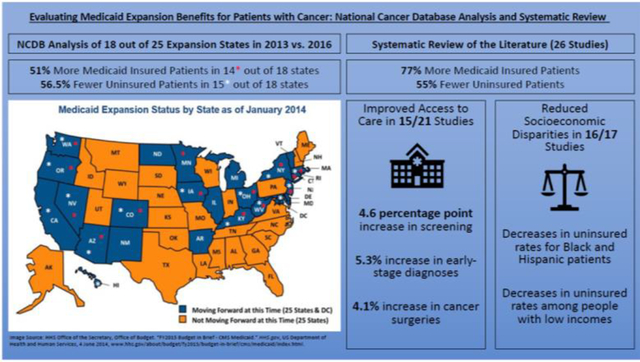
Graphical Abstract
Introduction
Cancer is a leading cause of mortality in the United States with an estimated 1,806,590 cases and 606,520 deaths in 2020 [1]. The all cancer five-year survival rate is 67.4% resulting in an estimated 15.5 million cancer survivors in America [1, 2]. Insurance status mediates access to care with relatively worse access for those without insurance [3–6]. As timely access to care influences cancer survival, insurance status impacts survival [7]. The percentage of uninsured cancer survivors decreased from 12.4% in 2012 to 7.7% in 2015 [8].
The Affordable Care Act (ACA) was largely implemented in 2014. The ACA provided federal funding for the expansion of Medicaid eligibility above previous state-set federal poverty level (FPL) limits to 138% FPL for nearly all adults, including childless nonelderly adults for the first time [9]. Due to the Supreme Court ruling National Federation of Independent Business v. Sebelius, states choose to expand [9]. As of November 2, 2020, 38 states and the District of Columbia have expanded Medicaid [9, 10]. Non-expansion states have income limits at or below 100% FPL, as low as 17% FPL, and an average cutoff of 46.2% FPL [11]. While few states variously expanded Medicaid soon after the ACA was passed, most expansion states implemented the expansion on January 1, 2014, per ACA regulations (Figure 1).
Figure 1.
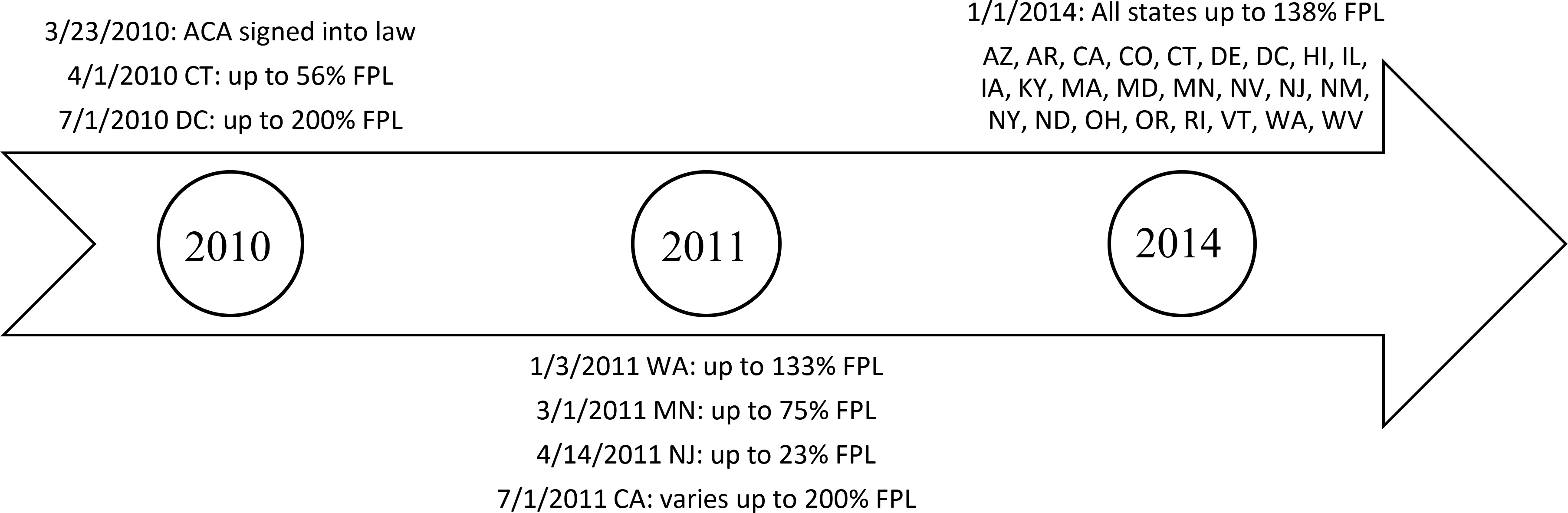
Timeline of when states implemented Medicaid expansions at particular Federal Poverty Level (FPL) eligibility cutoffs.
Expansion led to more people being insured via Medicaid and fewer people being uninsured [12–14]. However, people living in non-expansion states are more likely to be uninsured, especially if their income places them in a coverage gap [15, 16]. A major limitation of existing literature is the tendency to juxtapose expansion states against heterogenous non-expansion states as groups, rather than contrasting pre-expansion and post-expansion data for each singular specific expansion state. A recent article reviewed the outcomes of Medicaid expansion in patients with cancer after passage of the ACA [17]. However, the authors included studies featuring data from states that expanded Medicaid prior to 2014, at different FPL eligibility criteria, thereby limiting the generalizability of the study [17].
We used NCDB public benchmark reports to compare the insurance status distributions of patients diagnosed with common cancers in 2013 versus 2016 for each specific state that changed its FPL eligibility to 138% per the ACA on January 1, 2014. Then we performed a systematic review that only included data on the 2014 expansion to investigate the impact of Medicaid expansion on patients with cancer in terms of insurance status, access to care, and socioeconomic disparities. The hypothesis was that more people would be insured via Medicaid in 2016 with improved access to care and decreased socioeconomic disparities. Understanding the impact of Medicaid expansion on patients with cancer can help guide further policy development in promoting Medicaid expansion and universal coverage.
Materials and Methods
Analysis of the National Cancer Database
The National Cancer Database (NCDB) is a hospital-based registry featuring data from over 1,500 Commission on Cancer-accredited facilities with about 70% of newly diagnosed cases of cancer across all states in America [18, 19]. As 25 states (Figure 1) implemented the ACA-standardized Medicaid expansion on January 1, 2014, the NCDB public benchmark reports were queried for these states with 2013 representing pre-expansion counts and 2016 representing the most recent post-expansion counts for each state [20]. Adopters of expansion after January 1, 2014 were excluded due to different follow-up time. The variable of insurance status generated distributions of the type of insurance people had when initially diagnosed with, and/or initially treated for, a particular cancer in a particular state in a particular year. All diagnosis types and all hospital types were included. This process was done for every cancer in all of the 25 expansion states, and data for a cancer or a state was excluded if no one in that state with that cancer in that year was uninsured or Medicaid insured. The 12 eligible cancers were brain, breast, colon, corpus uteri, kidney and renal pelvis, lung or bronchus non-small cell carcinoma, lung or bronchus small cell carcinoma, melanoma of the skin, nodal non-Hodgkin’s lymphoma, pancreatic, thyroid, and urinary bladder cancers. Counts for each specific eligible malignancy were combined into an “all cancer” count, which was compared across insurance status between 2013 and 2016 for each eligible state. Percent change and averages were calculated. Chi square tests were performed to assess changes in the insurance status distributions. The number of Medicaid insured people with cancer diagnosed in 2013 was compared against the number of Medicaid insured cancer patients diagnosed in 2016 for a specific state via two-sided Fisher’s exact tests. Analysis was conducted using SAS 9.4 (Cary, North Carolina). Significance levels were denoted with a p<0.05.
Systematic Review
Framework followed Preferred Reporting Items for Systematic Review and Meta-Analysis guidelines (Supplement 1, 2) [21]. Search strategy was last utilized on 5/1/2020 to search PubMed, Embase, Cochrane Registry of Trials, and Scopus databases. Search terms were: (Medicaid expansion [Title/Abstract]) AND (cancer [Title/Abstract]) AND (Affordable Care Act [Text]). Filters used were: Humans, English, from 2014 – 2020. Included studies were peer-reviewed, quasi-experimental articles employing population-based sources such as large databases, registries, and national surveys. Selected articles presented quantitative results related to the 2014 Medicaid expansion and its impact on patients with a type(s) of cancer. Studies assessing pre-2014 Medicaid expansion and forms of Medicaid expansion outside of the domain of the ACA were excluded as Medicaid eligibility criteria differed. Surveillance reports, theoretical projections, and single institution studies were excluded. To limit heterogeneity, any study combining states that expanded Medicaid at different times was excluded. The Risk of Bias in Non-Randomized Studies of Interventions (ROBINS-I) standard was applied [22]. To evaluate quality, the National Institutes of Health Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies was employed [23]. Data extracted included outcome measures of insurance status, access to care in terms of screening and/or treatment and survival, if available, and inequities in these metrics influenced by race or income. Weighted averages of percent change in uninsured and Medicaid-insured rates were calculated.
Results
NCDB
18 out of 25 states were eligible for inclusion (Table 1). Pre-expansion insurance status distribution counts of 353,009 patients in 2013 were juxtaposed against post-expansion insurance status distribution counts of 370,810 patients in 2016. Fisher’s exact tests determined that 14 of 18 eligible states had a statistically significant increase in the number of Medicaid insured patients with cancer post-expansion (Table 1). The average percentage increase was 51% (13.2–204%). Chi square analysis revealed that 15 of 18 states also reported statistically significant changes in insurance distribution with an average percentage decrease in uninsured patients of 56.5% (14.6–83.8%) (Table 1).
Table 1.
NCDB results for 2013 and 2016 for selected Medicaid expansion states for all 12 eligible cancers (N = 723,819).
| State | Insurance Type | 2013 | 2016 | Percent Change (%) | Adjusted p-value for only Total Change | p-value for only Medicaid Change |
|---|---|---|---|---|---|---|
| Arizona | Uninsured | 89 | 76 | −14.61 | ||
| Private/Managed | 2237 | 2795 | +24.94 | |||
| Medicaid | 126 | 383 | +204.0 | <0.0001 | ||
| Medicare | 2624 | 3502 | +33.46 | |||
| Total | 5076 | 6756 | +33.10 | <0.0001 | ||
| California | Uninsured | 1097 | 671 | −38.83 | ||
| Private/Managed | 27522 | 33468 | +21.60 | |||
| Medicaid | 5320 | 6195 | +16.45 | 0.12 | ||
| Medicare | 23437 | 25870 | +10.38 | |||
| Total | 57376 | 66204 | +15.39 | <0.0 001 | ||
| Colorado | Uninsured | 437 | 156 | −64.30 | ||
| Private/Managed | 6606 | 5875 | −11.07 | |||
| Medicaid | 748 | 1154 | +54.28 | <0.0001 | ||
| Medicare | 7057 | 6906 | −2.14 | |||
| Total | 14848 | 14091 | −5.10 | <0.0001 | ||
| Connecticut | Uninsured | 137 | 145 | +5.84 | ||
| Private/Managed | 6189 | 5880 | −4.99 | |||
| Medicaid | 1102 | 1285 | +16.61 | <0.0001 | ||
| Medicare | 7282 | 7390 | +1.48 | |||
| Total | 14710 | 14700 | −0.07 | 0.0002 | ||
| Delaware | Uninsured | 35 | 37 | +5.71 | ||
| Private/Managed | 1327 | 1315 | −0.09 | |||
| Medicaid | 143 | 159 | +11.19 | 0.52 | ||
| Medicare | 1779 | 1789 | 0.56 | |||
| Total | 3284 | 3300 | +0.49 | 0.91 | ||
| Hawaii | Uninsured | 37 | 6 | −83.78 | ||
| Private/Managed | 1602 | 1634 | +2.00 | |||
| Medicaid | 241 | 277 | +14.94 | 0.11 | ||
| Medicare | 1508 | 1723 | +14.26 | |||
| Total | 3388 | 3640 | +7.44 | 0.0001 | ||
| Iowa | Uninsured | 200 | 42 | −79.00 | ||
| Private/Managed | 2674 | 2981 | +11.48 | |||
| Medicaid | 300 | 376 | +25.33 | 0.04 | ||
| Medicare | 3356 | 3693 | +10.04 | |||
| Total | 6530 | 7092 | +8.61 | <0.0001 | ||
| Kentucky | Uninsured | 552 | 131 | −76.27 | ||
| Private/Managed | 5796 | 5656 | −2.42 | |||
| Medicaid | 1104 | 1827 | +65.49 | <0.0001 | ||
| Medicare | 8400 | 9312 | +10.86 | |||
| Total | 15852 | 16926 | +6.78 | <0.0001 | ||
| Massachusetts | Uninsured | 199 | 148 | −25.63 | ||
| Private/Managed | 13320 | 13821 | +3.76 | |||
| Medicaid | 1566 | 1952 | +24.65 | <0.0001 | ||
| Medicare | 12264 | 13702 | +11.73 | |||
| Total | 27349 | 29623 | +8.31 | <0.0001 | ||
| Maryland | Uninsured | 390 | 177 | −54.62 | ||
| Private/Managed | 7875 | 6595 | −16.25 | |||
| Medicaid | 709 | 624 | −11.99 | 0.53 | ||
| Medicare | 8073 | 7123 | −11.77 | |||
| Total | 17047 | 14519 | −14.83 | <0.0001 | ||
| Minnesota | Uninsured | 132 | 129 | −2.27 | ||
| Private/Managed | 13061 | 13647 | +4.49 | |||
| Medicaid | 973 | 1101 | +13.16 | 0.03 | ||
| Medicare | 8538 | 9107 | +6.70 | |||
| Total | 22704 | 23984 | +5.64 | 0.1251 | ||
| Nevada | Uninsured | 195 | 57 | −70.77 | ||
| Private/Managed | 1256 | 1245 | −0.88 | |||
| Medicaid | 152 | 232 | +52.63 | <0.0001 | ||
| Medicare | 1284 | 1458 | +13.55 | |||
| Total | 2887 | 2992 | +3.64 | <0.0001 | ||
| New Jersey | Uninsured | 1216 | 545 | −55.18 | ||
| Private/Managed | 11023 | 10991 | −0.29 | |||
| Medicaid | 830 | 1301 | +56.75 | <0.0001 | ||
| Medicare | 13445 | 13352 | −0.69 | |||
| Total | 26514 | 26189 | −1.23 | <0.0001 | ||
| New York | Uninsured | 591 | 463 | −21.66 | ||
| Private/Managed | 24281 | 23421 | −3.54 | |||
| Medicaid | 5210 | 6123 | +17.52 | <0.0001 | ||
| Medicare | 25192 | 25963 | +3.06 | |||
| Total | 55274 | 55970 | +1.26 | <0.0001 | ||
| Ohio | Uninsured | 1698 | 590 | −65.25 | ||
| Private/Managed | 17023 | 16723 | −1.76 | |||
| Medicaid | 2606 | 4140 | +58.86 | <0.0001 | ||
| Medicare | 21896 | 24260 | +10.80 | |||
| Total | 43223 | 45713 | +5.76 | <0.0001 | ||
| Oregon | Uninsured | 314 | 115 | −63.38 | ||
| Private/Managed | 4587 | 4360 | −4.95 | |||
| Medicaid | 676 | 1117 | +65.24 | <0.0001 | ||
| Medicare | 5593 | 6034 | +7.88 | |||
| Total | 11170 | 11626 | +4.08 | <0.0001 | ||
| Washington | Uninsured | 428 | 157 | −63.32 | ||
| Private/Managed | 8585 | 9157 | +6.70 | |||
| Medicaid | 1381 | 1987 | +43.88 | <0.0001 | ||
| Medicare | 10678 | 11536 | +8.04 | |||
| Total | 21072 | 22837 | +8.38 | <0.0001 | ||
| West Virginia | Uninsured | 127 | 37 | −70.87 | ||
| Private/Managed | 1557 | 1534 | −1.48 | |||
| Medicaid | 501 | 579 | +15.57 | 0.008 | ||
| Medicare | 2520 | 2498 | −0.87 | |||
| Total | 4705 | 4648 | −1.21 | <0.0001 |
Statistical analyses generated p-values only for the total change in insurance status distribution and change in the number of people with cancer insured by Medicaid. The 12 eligible cancers were brain, breast, colon, corpus uteri, kidney and renal pelvis, lung or bronchus non-small cell carcinoma, lung or bronchus small cell carcinoma, melanoma of the skin, nodal non-Hodgkin’s lymphoma, pancreatic, thyroid, and urinary bladder cancers.
Systematic Review Study Characteristics
229 articles were screened, of which 26 were included (Figure 2). All had “moderate” bias [22] based on ROBINS-I scores and 23 had “good” National Institutes of Health Study Quality Assessment [23] scores with 3 articles having “fair” scores [24–26]. 17 studies utilized national or multi-state databases [26–42] (Table 2). 24 studies compared expansion states against non-expansion states, whereas two articles studied Kentucky alone.
Figure 2.
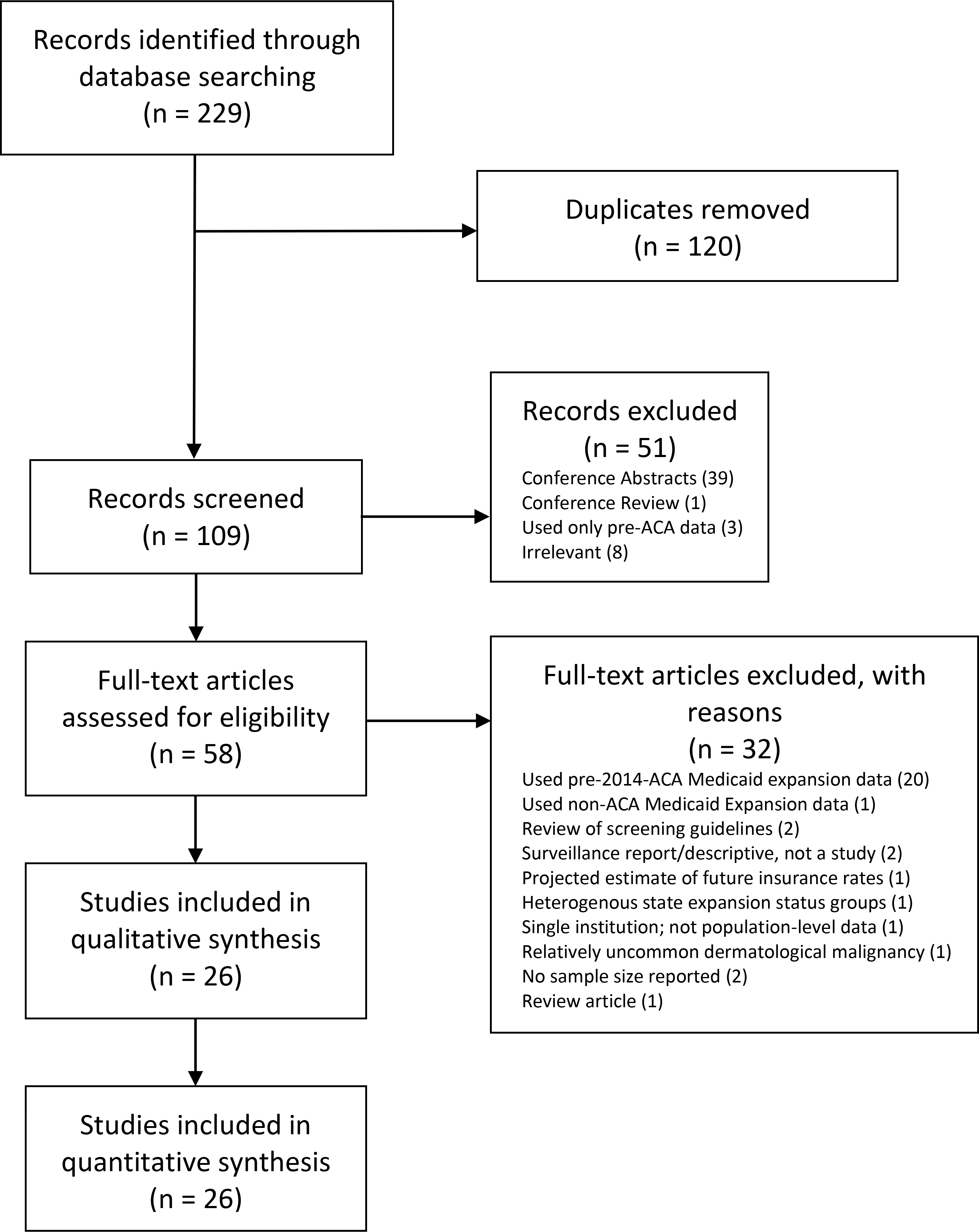
Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) flow diagram for systematic literature review.
Table 2.
Summary of literature search results evaluating effects of Medicaid expansion for the three key domains of changes in insurance rates, cancer screening and access to care, and socioeconomic disparities.
| Citation, Author, Year | Sample | Cancer Type | Sample Size | More Insurance Coverage | More Screening & Treatment | Reduced Socioeconomic Disparities |
|---|---|---|---|---|---|---|
| 24. Okoro et al. 2017 | BRFSS. 18–64 years old. 2014. | Breast, cervical, colorectal | 277,734 | Not studied for cancer patients | Yes, greater breast (3ppt), cervical (1.5ppt), and colorectal (2.5ppt) cancer screening | Yes, reduced income gap in breast cancer screening, but not for cervical and colorectal cancer screening |
| 25. Lyu et al. 2019 | BRFSS. Low-income adults (<138% FPL). 18–64 years old. 2012 vs. 2016. | Breast, cervical, colorectal | 31,890 | Not studied. | Yes, greater breast (11.4ppt), cervical (6.9ppt), and colorectal (8.3ppt) cancer screening | Not studied. |
| 26. Mahal et al. 2020 | SEER. 18–64 years old. 2010–2014. | Breast, lung, and prostate | 108,864 | Yes, 71% fewer uninsured in Medicaid expansion states. | Not studied. | Yes, elimination of uninsured gap between Blacks (90.5% decrease) and Whites and between low-income (<138% FPL, 7% decrease) and high income people. |
| 27. Chino et al. 2017 | SEER. Radiation recipients. 18–64 years old. 2011–2014. | All Cancer | 197,290 | Yes, 53% fewer uninsured | Not studied. | Yes, greatest gains among Blacks (50%), high poverty areas (60% fewer uninsured) |
| 28. Jemal et al. 2017 | NCDB. 18–64 years old. 2011–2014. | All Cancer | 1,718,864 | Yes, 54.7% fewer uninsured | No, similar shift to earlier stage | Yes, reduced income gap in uninsured rate (62.5% fewer uninsured at <138%FPL) |
| 29. Moss et al. 2017 | SEER. Women. <65 years old. 2008–2014. | Cervical, uterine or ovarian | 90,192 | Yes, 50% fewer uninsured | No, shift toward later stage | Yes, reduced Black (by 50%) and low-income uninsured rate (by 72%) |
| 30. Cannon et al. 2018 | SEER. 19–64 years old. 2007–2014. | Head and Neck Squamous Cell Carcinoma | 89,038 | Yes, 52% fewer uninsured, 9.5% more via Medicaid | Not studied. | Not studied. |
| 31. Crocker et al. 2018 | HCUP-SID (Florida, Kentucky, Maryland, New Jersey, North Carolina). Cancer surgery patients. 18–64 years old. 2012–2015. | Colorectal, esophagogastric, hepatobiliary, lung, and urologic | 78,915 | Yes, 13.4% fewer uninsured | Yes, 4.1% increase in non-discretionary cancer surgeries (5.3% decrease in non-expansion states) | Not studied. |
| 32. Eguia et al. 2018 | HCUP-SID (Florida, Iowa, Maryland, New York). 18–64 years old. 2010–2014. | Pancreas, esophagus, prostate, bladder, colorectal, lung, and gastric | 317,858 | Yes, Medicaid insured increased: 12% for pancreatic, 14% for breast, 11% for colorectal, 34% for prostate, and 23% for gastric cancers (Expansion vs. non-expansion states) | Yes, cancer surgery rates up 30% for lung cancer, 25% for breast cancer, 25% for colorectal cancer in Medicaid Expansion states compared to non-expansion states | Yes, disparities in odds to undergo surgery between Medicaid and privately insured cancer patients of Black race and Hispanic race decreased after Medicaid expansion and increased in non-expansion states |
| 33. Han et al. 2018 | NAACCR (40 states). First primary malignant cancer. 18–64 years old. 2010–2014. | All Cancer | 2,471,154 | Yes, 50% fewer uninsured | Yes, 2.3% greater early-stage diagnosis: all cancers combined | Yes, reduced insurance disparities based on race (for Blacks and Hispanics), income, and rural residence |
| 34. Moss et al. 2018 | SEER. 0–64 years old. 2008–2014. | Breast, lung, and colon | 414,085 | Yes, fewer uninsured, more Medicaid insured: Colon (−50%,+38%) lung (−57%,+24%) breast (−33%,+14%) cancer | Yes, increase in early- stage diagnoses by 1.2% for breast, 6.4% for colon, but no change for lung cancer | Yes, uninsured rates decreased for all races except: American Indians/Alaskan Natives for lung & colon cancer, and except Blacks and American Indians/Alaskan Natives for breast cancer |
| 35. Soni et al. 2018 | SEER. First time cancer diagnosis. 19–64 years old. 2010–2014. | All Cancer | 3,055 | Not studied. | Yes, 6.4% increase in early-stage diagnoses | Not studied. |
| 36. Agarwal et al. 2019 | SEER. 0–64 years old. 2011–2015. Compared expansion states against non-expansion states. | All Cancer | 716,364 | Yes, 3% greater decrease in uninsured in expansion vs. non-expansion states | Not studied. | Yes, greatest decreases in uninsured among rural (−4.8%) & minorities except Asians and Pacific Islanders: Black (−3.4%), Hispanic (−3.9%) |
| 37. Crocker et al. 2019 | HCUP-SID (Florida, Kentucky, Maryland, New Jersey, North Carolina). Inpatient cancer surgery patients. 18–64 years old. 2012–2015 | Colorectal, esophagogastric, hepatobiliary, pancreatic, lung, urologic | 81,628 | Yes, 82.6% more insured via Medicaid in expansion states; 10.1% fewer Medicaid-insured in non-expansion states | Yes, 10.8% greater utilization by Medicaid & uninsured patients; 9.5% less in non-expansion states | Mixed Results. Expansion narrowed the income gap but not the race gap (Whites relative to Blacks and Hispanics) in cancer surgery utilization |
| 38. Spiegel et al. 2019 | SEER. New diagnosis. 19–64 years old. 2011–2014. | Breast, cervical, uterine, or prostate with brachytherapy | 15,497 | Yes, 38% fewer uninsured | Not studied. | Mixed Results. Expansion narrowed insurance income gap but not the race gap (Whites relative to Blacks and Hispanics) |
| 39. Huguet et al. 2019 | ADVANCE clinical data. Age-based screening cohorts from 21–64 years old. 2012–2015. | Cervical and colorectal | 329,126 | Yes, Medicaid visit rate up 56%, uninsured visit rate decreased 52% after Medicaid expansion | No, similar screening rates since increased in both states | Yes, narrowed race gap (Whites relative to Blacks and Hispanics) for cervical and colorectal cancer screening |
| 40. Mesquita-Neto et al. 2019 | SEER. All patients. 2007–2009 vs. 2014–2015. | Breast, colorectal, ovarian, lung, uterine, pancreatic, prostate, and liver | 293,028 | Yes, 50% fewer uninsured in Medicaid expansion states | Yes, 12.8% increase in early-stage diagnoses | Yes, 54.5% fewer uninsured & 3.8% greater access to surgery for people of low socioeconomic standing |
| 41. Sineshaw et al. 2020 | NCDB. 18–64 years old. 2010–2016. | Head and Neck Squamous Cell Carcinoma | 90,789 | Yes, 63% decrease in uninsured, 18% increase in Medicaid insured in Medicaid expansion states | Yes, 3.8% increase in early-stage diagnoses. Time to treatment initiation down 5.5 days for nonoropharyngeal head & neck squamous cell carcinoma, no difference for overall head & neck squamous cell carcinoma | Not studied. |
| 42. Takvorian et al. 2020 | NCDB. 40-64 years old. 2011–2016 | Breast, colon, non-small cell lung | 848,329 | Yes, 24% more Medicaid-insured and 55% fewer uninsured in Medicaid expansion states | Yes, 4.4% increase in early-stage diagnoses, 2.2% fewer late-stage diagnoses in expansion states. No time to treatment initiation difference between expansion and non-expansion states | Not studied. |
| 43. Ajkay et al. 2018 | Kentucky Cancer Registry. Women. 20-64 years old. 2011–2016. | Breast | 1,315,965 | Yes, 73% fewer uninsured, 54% more via Medicaid | Yes, earlier stage (up 3.4%; 2.2ppt), earlier treatment (5.1% sooner) | Not studied. |
| 44. Cawley et al. 2018 | BRFSS. Low-income childless adults. 19–64 years old. 2010–2016 | Breast and cervical | 80,200 | Yes, 16.7% more insured | No screening change, but better access to care overall | Not studied. |
| 45. Nikpay et al. 2018 | BRFSS. All-Cancer survivors. 18–64 years old. 2011–2015 | All Cancer | 17,381 | Yes, 52.6% fewer uninsured | Yes, care (9ppt) & meds (14ppt) both more affordable | Not studied. |
| 46. Alharbi et al. 2019 | MEPS. Women. Low-income. <65 years old. 2012–2016. | Breast and cervical | 13,078 | Yes, 100% more insured via Medicaid | No, mammograms at the same rate and Papanicolaou tests at a lower rate | Not studied. |
| 47. Gan et al. 2019 | Kentucky Cancer Registry and Kentucky Hospital Discharge Database. 20+ years old. 2011–2016 | Colorectal | 930,176 | Yes, 230% increase in screened Medicaid insured | Yes, more diagnosed, earlier stage, better survival (Hazard Ratio = 0.73) | Yes, patients from Appalachian parts of Kentucky (rural) saw 199% increase in Medicaid and 77.7% decrease in uninsured. Early stage diagnosis increased 9.3% for Appalachians post-expansion |
| 48. Hendryx et al. 2018 | BRFSS. Low-income childless adults. 18–64 years old. 2012 vs. 2016. | Breast, cervical, and colorectal | 56,959 | Not studied. | Yes, greater screening rates: cervical (2ppt) and colorectal (3.2ppt) (Expansion vs. Non-expansion states) | Yes, helped reduced gap in screening between low and high income folks. |
| 49. Zerhouni et al. 2019 | BRFSS. White, Black, and Hispanic respondents with complete demographic answers. Age 50–64 years old. 2012–2016 | Colorectal | 341,350 | Not studied. | No, 8% more likely to get colorectal cancer screening in expansion states than non-expansion states, but no increase after 2014 Medicaid expansion | No, no statistically significant changes in disparities after 2014 Medicaid expansion. Statistically significant changes in race (Whites relative to Blacks and Hispanics) and income disparity reduction only seen in states that expanded Medicaid prior to 2014. |
| Summary | 17 from national/multi-state databases, 7 from national surveys, 2 from Kentucky databases | All Cancer (6), Breast (11), Gastrointestinal (11), Gynecologic (9), Lung (7), Squamous Cell Carcinoma (2), Urologic (6) | 10,928,809 | 21 out of 21 articles | 15 out of 21 articles | 16 out of 17 articles |
Abbreviations: ADVANCE (Accelerating Data Value Across a National Community Health Center Network), BRFSS (Behavioral Risk Factor Surveillance System), HCUP-SID (Healthcare Cost and Utilization Project - State Inpatient Databases), MEPS (Medical Expenditure Panel Survey), NAACR (North American Association of Cancer Registries), NCDB (National Cancer Database), SEER (Surveillance, Epidemiology, and End Results Program); ppt (Percentage Point); FPL (Federal Poverty Level).
Summary of Literature Search
Insurance Status
21 articles studied insurance status of people with cancer after Medicaid expansion, and all reported increases in the number of Medicaid insured and/or decreases in the number of uninsured patients with cancer in expansion states compared to non-expansion states [26–34, 36–47] (Table 2). Among the articles that report a relative percentage decrease in uninsured patients, the weighted average decrease was 55% (13.4–73%) after expansion [26–31, 33, 34, 36–38, 40–43, 45]. For studies that report a relative percentage increase in the number of patients with Medicaid, the weighted average increase was 77% (9.5–230%) [30, 32, 39, 41–44, 46, 47].
Access to Care
21 articles evaluated access to care in terms of screening, stage at diagnosis, and treatment rates (Table 2). One study evaluated survival [47]. 15 of these 21 articles reported a result indicating a statistically significant increase in one or more metric in expansion states compared to non-expansion states [24, 25, 31–35, 37, 40–43, 45, 47, 48]. 11 of these 15 articles specifically reported relatively higher screening rates and/or earlier stage of cancer at diagnosis in expansion states [24, 25, 33–35, 40–43, 47, 48]. The average increase in screening rates was 4.6 percentage points (1.5–11.4ppt) across three articles [24, 25, 48]. The percent increase in neoplasms diagnosed at an earlier stage following Medicaid expansion averaged to be 5.3% (2.3–12.8%) between seven studies [33–35, 40–43]. Heterogenous reporting precluded further quantitative analysis. Six studies described increased access to care as improved affordability of care and medications, reduced time to treatment, increases in non-discretionary cancer surgeries, greater utilization, and better survival in Medicaid expansion states [31, 32, 37, 41, 45, 47]. The six articles that did not find improved access to care reported varying observations, including earlier stage diagnosis for all cancers, later stage of diagnosis for cervical, uterine, or ovarian cancers, and no changes in screening [28, 29, 39, 44, 46, 49].
Socioeconomic Disparities
16 of the 17 studies that characterized changes in socioeconomic inequities along the continuum of care of patients with cancer reported reductions in disparities after expansion [24, 26–29, 32–34, 36–40, 48] (Table 2). The specific differences partially relieved included uninsured rates, and lower screening and surgery rates. Alleviation of differences based on race was observed in eight of 16 articles [26, 27, 29, 32–34, 36, 39], and narrowing of gaps based on income was reported in 10 of 16 studies [24, 26, 27, 29, 32, 33, 37, 38, 40, 48]. Depending on the study, the decrease in uninsured rates among Black patients ranged from 3.4–90.5% [26, 27, 29, 36]. The reduction in the proportion of uninsured people from low-income, high poverty, and/or rural backgrounds averaged to be 47% (4.8–77.7%) [26–29, 36, 47]. Five studies [26, 27, 29, 32, 33] reported simultaneous benefits for both minority (Black and/or Hispanic) and low-income populations, whereas three articles [37, 38, 40] reported that disparities in income but not race were reduced following expansion.
Discussion
We conducted a descriptive analysis of the NCDB and performed a systematic literature review to evaluate the influence Medicaid expansion in 2014 had on the insurance status of people with cancer. This was previously unclear, as no prior study evaluated pre-expansion and post-expansion data for each specific state that changed its Medicaid eligibility to 138% FPL at the same time on January 1, 2014. For patients with one of twelve common malignancies, expansion led to statistically significant increases in the number of Medicaid-insured patients, and decreases in the number of uninsured patients. Systematic review of existing literature supported these observations. This shift in insurance status is critically important for people with cancer as insurance status impacts access to care throughout the continuum of care, influencing outcomes [3, 4, 47].
NCDB Analysis
Evaluation of NCDB data reveals the insurance status of patients with cancer at their point of care. The increase in Medicaid enrollment for patients with cancer after expansion among these 14 states averages to be 51% (13.2–204%), outpacing the gain in Medicaid signups throughout the country between 2013 and 2016 of 13% for the general population [50]. Furthermore, the decrease in the number of uninsured patients with cancer after expansion in the 15 states with significant changes in insurance distribution averaged to be 56.5% (14.6–83.8%). For these 15 states the average percent decrease in the number of uninsured people among the general population between 2013 and 2016 was 6.3% [50]. Therefore, cancer patients in these Medicaid expansion states had greater gains in Medicaid insurance and lower rates of being uninsured compared to the general population since Medicaid expansion in 2014.
Systematic Review
The trend from the NCDB correlated with the systematic review, as all relevant articles reported increased Medicaid coverage and decreased uninsured rates after expansion in 2014. These sequelae are important to confirm as insurance status modifies cancer patient outcomes [51]. People who are uninsured when newly diagnosed with a malignancy tend to be diagnosed at a later stage compared to people with insurance and are less likely to receive timely and appropriate treatment, contributing to worse survival for uninsured people with cancer [51, 52]. Moreover, Medicaid patients report having a usual source of care, having a healthcare visit in the last year, and not forgoing care or medications due to cost at greater rates than uninsured patients [51].
Therefore, the next domain we evaluated was access to care. The most common improvements after expansion were higher screening rates and/or earlier stage of cancer at diagnosis in expansion states relative to non-expansion states. Importantly, this increase in detecting neoplasms early was observed for malignancies for which screening is routinized via guidelines such as breast and colorectal cancers, and for all cancers in general. However, six articles report no relative shift in stage of diagnosis or change in screening rates for both frequently-screened and general malignancies, with one study even describing a decrease in Papanicolaou tests. Lyu et al. [25] observed that ACA-mediated Medicaid expansions were associated with increased cancer screening for breast, cervical, and colorectal cancers only in states with a high supply of primary care providers to meet the demand of more patients with Medicaid. In states with limited supply of primary providers, such limited cancer screening may be more pronounced with increased competition for appointments among a larger insured population following ACA implementation. Clinics may have also rejected newly enrolled Medicaid patients as Medicaid pays less than other insurance [53]. Indeed, a study found greater availability of appointments for Medicaid enrollees between 2012 and 2014, when the ACA increased Medicaid reimbursement rates to Medicare levels [54]. These findings reveal a role for policy to increase the availability of primary care providers. Loan forgiveness and increased reimbursement rates for primary care providers may help achieve the goals of health insurance reform and expansion.
Diagnosing malignancies earlier and starting treatment earlier are main reasons why more people are surviving cancer [51, 55]. Indeed, three studies specifically noticed statistically significant increases in cancer surgery rates after expansion while others noted better affordability of care and medications. Thus, the increase in screening and earlier detection of neoplasms in people residing in states that expanded Medicaid could facilitate improved survival. This finding was made by Gan et al. [47] who saw that Medicaid expansion in Kentucky led to greater diagnosis of colorectal cancer, more early-stage diagnoses, and better survival.
We also noted reductions in socioeconomic disparities after Medicaid expansion in 2014. Income and race were the determinants of health most consistently evaluated in selected studies. Eligibility for Medicaid is based on a low modified adjusted gross income; thus, it is intuitive that increasing the income limit to 138% FPL will increase eligibility. Nonetheless, it is important to demonstrate that the income gap in insurance status did narrow following Medicaid expansion since this can influence cancer survival. O’Connor et al. [56] found that the mean cancer death rate was 185.9 per 100,000 person-years in high-income counties, compared with 204.9 and 229.7 per 100,000 person-years in medium- and low-income counties, respectively.
In addition, multiple studies reported gains in insurance and increases in screening for racial minorities, particularly African-Americans after Medicaid expansion. However, in one study the only minority group to not see a decrease in uninsured rates was American Indians/Alaska Natives [34], and in another study Asians and Pacific Islanders were the one group to not experience a decrease in uninsured rates [36]. Moreover, while Zerhouni et al. [49] reported an 8.1% increase in colorectal cancer screening for African-Americans after Medicaid expansion, they also observed that Latinx people experienced no increase in colorectal cancer screening. Despite these shortcomings, the progress in reducing disparities for the African-American population is certainly noteworthy, especially as increased screening may lead to earlier detection, which may translate to a reduction in the health disparity of differential colorectal cancer survival by race [47, 57]. Prior to Medicaid expansion, African-Americans were 4.9% less likely to receive timely cancer therapy relative to Whites, the greatest delay in time to treatment for cancer for any minority group [57]. After expansion, Adamson et al. [57] no longer observed this inequity. Eguia et al. [32] also noted a narrowed gap in odds to undergo surgery for Medicaid-insured Black and Hispanic patients after expansion. Therefore, these gains in Medicaid insurance enrollment, screening, odds to undergo surgery for cancer, and timely cancer treatment rates collectively indicate reductions in socioeconomic disparities for people with cancer.
The current systematic review features data from Surveillance, Epidemiology, and End Results (SEER) reports [36], Behavioral Risk Factor Surveillance System (BRFSS) surveys [44], and other sources, and was corroborated with the NCDB. Even though including data from different sources invites heterogeneity, using multiple sizable and diverse population-based methods makes the results more generalizable [58]. Increasing the broad relevance of findings from this analysis, six of the 26 studies included all cancers in their samples rather than limiting selected malignancies to neoplasms that are more detectable by screening or too uncommon. Moreover, the total sample size of 10,928,809 people for these 26 studies surpasses many datasets.
While differing in study design and included studies, our findings are similar to a recent review by Moss et al. [17]. They included studies on Medicaid expansions that occurred before 2014, which can be problematic since only a few states participated in Medicaid expansion between 2010 and 2014 [17, 59] at drastically different income eligibility limits ranging from 23%−200% FPL (Figure 1). The current study was restricted to states that expanded Medicaid in January 2014 at the same 138% FPL eligibility. Thereby, the results would be a more accurate representation of the effects of Medicaid expansion in its current form as regulated by the ACA.
Limitations
There are important limitations to acknowledge regarding use of the NCDB. As the NCDB is a hospital-based registry, it is not representative of the United States population, limiting the external validity. Therefore, the results were also corroborated across multiple data sources via systematic review. The NCDB is also susceptible to selection bias, as only patients with access to care are diagnosed with cancer, and those with greater access to care tend to be insured. This may underrepresent uninsured patients, and overrepresent insured patients compared to the general population. However, our analysis did not focus on the general population, but instead evaluated trends in insurance status of patients when first diagnosed and/or treated for cancer. The simultaneous downward trends in population uninsured rates and uninsured rates for newly diagnosed cancer patients are nevertheless reassuring. Ultimately, the NCDB was chosen since it has data from all states whereas other datasets such as SEER only have data from a few states [60].
Though the systematic review utilizes various sources, relying on select databases such as SEER for eight out of 26 articles can limit the generalizability of the data, and surveys are susceptible to response bias [61]. Incomplete retrieval of identified research and reporting bias are also potential limitations. In our analysis, we also merged multiple measured outcomes into three domains, inviting conflation and mixed findings. For example, it can be debated if findings in one study of alleviation of inequities by income but not race demonstrate that Medicaid expansion facilitates decreases in socioeconomic inequities. Moreover, the paucity of alternative variables to characterize social determinants of health reflects a limitation of the literature. Only three studies looked at rural location, and only Mesquita-Neto et al. [40] created a nuanced socioeconomic standing metric that added area unemployment rate and education level to income measures. Thus, insight into the effect of Medicaid expansion on health disparities is primarily restricted to the roles of race and income along the continuum of care. This review may not capture changes in survival given the recency of Medicaid expansion implementation in 2014. Therefore, we cannot characterize the impact of Medicaid expansion on health disparities, but rather on inequities in factors that can influence health such as insurance status and access to care. This short time window also limited the number of studies overall.
Conclusions
Through a descriptive analysis of the National Cancer Database and a systematic review of the literature, we found that people with cancer experienced lower uninsured rates, increased Medicaid insurance rates, increased access to care in terms of screening and surgery, and alleviation of socioeconomic disparities in these metrics following Medicaid expansion in 2014. These findings serve as comprehensive evidence of the sustained consequences of Medicaid expansion throughout the continuum of care for patients with cancer. Moreover, this review and analysis highlight areas for future in-depth studies to track these results and further evaluate the impact on health disparities and survival. These studies can ultimately inform government action to increase insurance coverage.
Supplementary Material
Highlights:
Medicaid expansion in 2014 reduced the number of uninsured patients with cancer
Expansion increased the number of Medicaid-insured patients with cancer
Expansion increased screening, earlier detection, and treatment of cancer
Expansion decreased socioeconomic disparities in cancer care
Acknowledgements:
This research was supported by the Keck School of Medicine of USC Summer Research Fellowship to NHN; and the National Center for Advancing Translational Science of the United States National Institutes of Health [grant numbers UL1TR001855 and UL1TR000130] to LD; and the National Institutes of Health Southern California Clinical and Translational Science Institute KL2 Clinical and Translational Research Scholar Award [grant number KL2 TR001854-04] to FJA.
Footnotes
Declarations of interest: Disclosed in ICMJE Conflict of Interest forms submitted to journal.
Disclaimer: The American College of Surgeons and the Commission on Cancer have not verified and are not responsible for the analytic or statistical methodology used or for the conclusions drawn from these data by the investigator. It is the policy of the National Cancer Database (NCDB) that facility-specific survival data obtained from NCDB cannot be published.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Howlader N, et al. , SEER Cancer Statistics Review, 1975–2017. National Cancer Institute, 2019. [Google Scholar]
- 2.Rohan EA, et al. , Comprehensive cancer control: promoting survivor health and wellness. Cancer Causes & Control, 2018. 29(12): p. 1277–1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kehl KL, et al. , Access to accredited cancer hospitals within federal exchange plans under the Affordable Care Act. Journal of Clinical Oncology, 2017. 35(6): p. 645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kehl KL, et al. , Insurance networks and access to affordable cancer care. Journal of Clinical Oncology, 2019: p. JCO. 19.01484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nguyen KH and Sommers BD, Access and quality of care by insurance type for low-income adults before the Affordable Care Act. American journal of public health, 2016. 106(8): p. 1409–1415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tarazi WW, et al. , Medicaid expansion and access to care among cancer survivors: a baseline overview. Journal of Cancer Survivorship, 2016. 10(3): p. 583–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cortes J, et al. , Enhancing global access to cancer medicines. CA: A Cancer Journal for Clinicians, 2020. [DOI] [PubMed] [Google Scholar]
- 8.Davidoff AJ, et al. , Changes in health insurance coverage associated with the affordable care act among adults with and without a cancer history: population-based national estimates. Medical care, 2018. 56(3): p. 220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rosenbaum S and Westmoreland TM, The Supreme Court’s surprising decision on the Medicaid expansion: how will the federal government and states proceed? Health Affairs, 2012. 31(8): p. 1663–1672. [DOI] [PubMed] [Google Scholar]
- 10.Kaiser Family Foundation. Status of state action on the Medicaid expansion decision. 2020. [cited 2020 March 13]; Available from: https://www.kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D.
- 11.Brooks T, Roygardner L, and Artiga S, Medicaid and CHIP eligibility, enrollment, and cost sharing policies as of January 2019: Findings from a 50-state survey. Georgetown University Center for Children and Families, available at https://www.kff.org/medicaid/report/medicaid-and-chip-eligibility-enrollment-and-cost-sharing-policies-asof-january-2019-findings-from-a-50-state-survey, 2019. [Google Scholar]
- 12.Mazurenko O, et al. , The effects of Medicaid expansion under the ACA: a systematic review. Health Affairs, 2018. 37(6): p. 944–950. [DOI] [PubMed] [Google Scholar]
- 13.Decker SL, Lipton BJ, and Sommers BD, Medicaid expansion coverage effects grew in 2015 with continued improvements in coverage quality. Health Affairs, 2017. 36(5): p. 819–825. [DOI] [PubMed] [Google Scholar]
- 14.Soni A, Hendryx M, and Simon K, Medicaid expansion under the Affordable Care Act and insurance coverage in rural and urban areas. The Journal of Rural Health, 2017. 33(2): p. 217–226. [DOI] [PubMed] [Google Scholar]
- 15.Choi S, Lee S, and Matejkowski J, The Effects of State Medicaid Expansion on Low-Income Individuals’ Access to Health Care: Multilevel Modeling. Population health management, 2018. 21(3): p. 235–244. [DOI] [PubMed] [Google Scholar]
- 16.Garfield R, Orgera K, and Damico A, The coverage gap: Uninsured poor adults in states that do not expand Medicaid (Issue Brief). Retrieved from Henry J. Kaiser Family Foundation; website: https://www.kff.org/medicaid/issue-brief/the-coverage-gapuninsured-poor-adults-in-states-that-do-not-expandmedicaid, 2019. [Google Scholar]
- 17.Moss HA, et al. , The Affordable Care Act’s Medicaid Expansion and Impact along the Cancer-Care Continuum: A Systematic Review. JNCI: Journal of the National Cancer Institute, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.American College of Surgeons. About the National Cancer Database. 2019. [cited 2020 April 22]; Available from: https://www.facs.org/quality-programs/cancer/ncdb/about.
- 19.Mallin K, et al. , Incident cases captured in the National Cancer Database compared with those in US population based central cancer registries in 2012–2014. Annals of surgical oncology, 2019. 26(6): p. 1604–1612. [DOI] [PubMed] [Google Scholar]
- 20.National Cancer Database, Public Benchmark Reports. American College of Surgeons, 2019; Available from: https://reportsncdb.facs.org/BMPub/
- 21.Moher D, et al. , Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals of internal medicine, 2009. 151(4): p. 264–269. [DOI] [PubMed] [Google Scholar]
- 22.Sterne JA, et al. , ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. bmj, 2016. 355: p. i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.National Heart, Lung, and Blood Institute. Study quality assessment tools. 2018; Available from: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools.
- 24.Okoro CA, et al. , Surveillance for health care access and health services use, adults aged 18–64 years—Behavioral Risk Factor Surveillance System, United States, 2014. MMWR Surveillance Summaries, 2017. 66(7): p. 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lyu W and Wehby GL, The impacts of the ACA medicaid expansions on cancer screening use by primary care provider supply. Medical care, 2019. 57(3): p. 202–207. [DOI] [PubMed] [Google Scholar]
- 26.Mahal AR, et al. , Early impact of the Affordable Care Act and medicaid expansion on racial and socioeconomic disparities in cancer care. American Journal of Clinical Oncology, 2020. 43(3): p. 163–167. [DOI] [PubMed] [Google Scholar]
- 27.Chino F, et al. , Healthcare disparities in cancer patients receiving radiation: changes in insurance status after medicaid expansion under the affordable care act. International Journal of Radiation Oncology• Biology• Physics, 2017. 99(5): p. 1320–1321. [DOI] [PubMed] [Google Scholar]
- 28.Jemal A, et al. , Changes in insurance coverage and stage at diagnosis among nonelderly patients with cancer after the Affordable Care Act. Journal of Clinical Oncology, 2017. 35(35): p. 3906–3915. [DOI] [PubMed] [Google Scholar]
- 29.Moss HA, Havrilesky LJ, and Chino J, Insurance coverage among women diagnosed with a gynecologic malignancy before and after implementation of the Affordable Care Act. Gynecologic oncology, 2017. 146(3): p. 457–464. [DOI] [PubMed] [Google Scholar]
- 30.Cannon RB, et al. , Association of the Patient Protection and Affordable Care Act with insurance coverage for head and neck cancer in the SEER database. JAMA Otolaryngology–Head & Neck Surgery, 2018. 144(11): p. 1052–1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Crocker AB, et al. , The Affordable Care Act’s Medicaid expansion and utilization of discretionary vs. non-discretionary inpatient surgery. Surgery, 2018. 164(6): p. 1156–1161. [DOI] [PubMed] [Google Scholar]
- 32.Eguia E, et al. , Impact of the Affordable Care Act (ACA) Medicaid expansion on cancer admissions and surgeries. Annals of surgery, 2018. 268(4): p. 584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Han X, et al. , Comparison of insurance status and diagnosis stage among patients with newly diagnosed cancer before vs after implementation of the Patient Protection and Affordable Care Act. JAMA oncology, 2018. 4(12): p. 1713–1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Moss HA, et al. , Trends in insurance status among patients diagnosed with cancer before and after implementation of the Affordable Care Act. Journal of oncology practice, 2018. 14(2): p. e92–e102. [DOI] [PubMed] [Google Scholar]
- 35.Soni A, et al. , Effect of Medicaid expansions of 2014 on overall and early-stage cancer diagnoses. American journal of public health, 2018. 108(2): p. 216–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Agarwal A, Katz AJ, and Chen RC, The Impact of the Affordable Care Act on Disparities in Private and Medicaid Insurance Coverage Among Patients Under 65 With Newly Diagnosed Cancer. International Journal of Radiation Oncology* Biology* Physics, 2019. 105(1): p. 25–30. [DOI] [PubMed] [Google Scholar]
- 37.Crocker AB, et al. , Expansion coverage and preferential utilization of cancer surgery among racial and ethnic minorities and low-income groups. Surgery, 2019. 166(3): p. 386–391. [DOI] [PubMed] [Google Scholar]
- 38.Spiegel DY, et al. , Changes in insurance coverage for cancer patients receiving brachytherapy before and after enactment of the Affordable Care Act. Brachytherapy, 2019. 18(1): p. 115–121. [DOI] [PubMed] [Google Scholar]
- 39.Huguet N, et al. , Cervical and colorectal cancer screening prevalence before and after Affordable Care Act Medicaid expansion. Preventive medicine, 2019. 124: p. 91–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mesquita-Neto JWB, et al. , Disparities in access to cancer surgery after Medicaid expansion. The American Journal of Surgery, 2020. 219(1): p. 181–184. [DOI] [PubMed] [Google Scholar]
- 41.Sineshaw HM, et al. , Association of Medicaid Expansion Under the Affordable Care Act With Stage at Diagnosis and Time to Treatment Initiation for Patients With Head and Neck Squamous Cell Carcinoma. JAMA Otolaryngology–Head & Neck Surgery, 2020. 146(3): p. 247–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Takvorian SU, et al. , Association of Medicaid expansion under the Affordable Care Act with insurance status, cancer stage, and timely treatment among patients with breast, colon, and lung cancer. JAMA network open, 2020. 3(2): p. e1921653–e1921653. [DOI] [PubMed] [Google Scholar]
- 43.Ajkay N, et al. , Early impact of medicaid expansion and quality of breast cancer care in Kentucky. Journal of the American College of Surgeons, 2018. 226(4): p. 498–504. [DOI] [PubMed] [Google Scholar]
- 44.Cawley J, Soni A, and Simon K, Third year of survey data shows continuing benefits of medicaid expansions for low-income childless adults in the US. Journal of general internal medicine, 2018. 33(9): p. 1495–1497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nikpay SS, Tebbs MG, and Castellanos EH, Patient Protection and Affordable Care Act Medicaid expansion and gains in health insurance coverage and access among cancer survivors. Cancer, 2018. 124(12): p. 2645–2652. [DOI] [PubMed] [Google Scholar]
- 46.Alharbi AG, et al. , Impact of Medicaid coverage expansion under the Affordable Care Act on mammography and pap tests utilization among low-income women. PloS one, 2019. 14(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gan T, et al. , Impact of the Affordable Care Act on colorectal cancer screening, incidence, and survival in Kentucky. Journal of the American College of Surgeons, 2019. 228(4): p. 342–353. e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hendryx M and Luo J, Increased cancer screening for low-income adults under the Affordable Care Act Medicaid expansion. Medical care, 2018. 56(11): p. 944–949. [DOI] [PubMed] [Google Scholar]
- 49.Zerhouni YA, et al. , Effect of Medicaid expansion on colorectal cancer screening rates. Diseases of the Colon & Rectum, 2019. 62(1): p. 97–103. [DOI] [PubMed] [Google Scholar]
- 50.Barnett JC and Berchick ER, Health insurance coverage in the United States: 2016. Current population reports. Washington DC: US Government Printing Office, 2017: p. P60–260. [Google Scholar]
- 51.Ward E, et al. , Association of insurance with cancer care utilization and outcomes. CA: a cancer journal for clinicians, 2008. 58(1): p. 9–31. [DOI] [PubMed] [Google Scholar]
- 52.Halpern MT, et al. , Association of insurance status and ethnicity with cancer stage at diagnosis for 12 cancer sites: a retrospective analysis. The lancet oncology, 2008. 9(3): p. 222–231. [DOI] [PubMed] [Google Scholar]
- 53.Zuckerman S, Skopec L, Epstein M. Medicaid physician fees after the ACA primary care fee bump. Washington, DC: Urban Institute. 2017. [Google Scholar]
- 54.Polsky D, Richards M, Basseyn S, et al. Appointment availability after increases in Medicaid payments for primary care. New England Journal of Medicine. 2015;372(6):537–545. [DOI] [PubMed] [Google Scholar]
- 55.Miller KD, et al. , Cancer treatment and survivorship statistics, 2016. CA: a cancer journal for clinicians, 2016. 66(4): p. 271–289. [DOI] [PubMed] [Google Scholar]
- 56.O’Connor JM, et al. , Factors associated with cancer disparities among low-, medium-, and high-income US counties. JAMA network open, 2018. 1(6): p. e183146–e183146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Adamson BJ, et al. , Affordable Care Act (ACA) Medicaid expansion impact on racial disparities in time to cancer treatment. Journal of Clinical Oncology, 2019. [Google Scholar]
- 58.Jairam V and Park HS, Strengths and limitations of large databases in lung cancer radiation oncology research. Translational lung cancer research, 2019. 8(Suppl 2): p. S172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Barnes JM, et al. , Associations of Early Medicaid Expansion With Insurance Status and Stage at Diagnosis Among Cancer Patients Receiving Radiation Therapy. Practical radiation oncology, 2019. [DOI] [PubMed] [Google Scholar]
- 60.Surveillance, Epidemiology, and End Results Program, Overview of the SEER Program. 2018; Available from: https://seer.cancer.gov/about/factsheets/SEER_Overview.pdf
- 61.Behavioral Risk Factor Surveillance Survey. About BRFSS. 2014. [cited 2020 April 24]; Available from: https://www.cdc.gov/brfss/about/index.htm.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


