Abstract
Klebsiella spp community-acquired meningitis caused by hypervirulent strains is well described as part of a distinct syndrome consisting of liver abscess and multiple septic metastatic lesions (Klebsiella pneumoniae invasive syndrome) occurring usually in diabetic, alcoholic, elderly or cancer patients, in Taiwan and other South-East Asian countries. In Western countries, these infections are very rare in natives and usually occur in patients of Asian origin. We report three cases of Filipino-origin patients, residents of Greece, with community-acquired invasive Klebsiella meningitis, who were treated in our ICU over a 10-year period.
LEARNING POINTS
Community-acquired Klebsiella spp meningitis has a very bad prognosis.
A physician must suspect an invasive Klebsiella infection in patients of Asian origin, even though they are residents of Western countries and have not visited their homeland recently.
Keywords: Meningitis, hypervirulent Klebsiella spp, liver abscess
INTRODUCTION
Some Klebsiella pneumoniae strains can cause community-acquired invasive infections (Klebsiella pneumoniae invasive syndrome) including liver abscess, pneumonia, meningitis/brain abscess, endophthalmitis and deep neck abscess, because they have the ability to metastatically spread, an unusual feature for enteric Gram-negative bacilli in the non-immunocompromised. These strains share common phenotypical features (hypermucoviscosity phenotype related to K1 and K2 capsular serotypes) and certain genetic plasmids (mucoviscosity-associated gene A (magA) and regulator of mucoid phenotype A (rmpA)). The hypermucoviscosity phenotype is confirmed by the string test (formation of a viscous string greater than 0.5 cm in length stretched by the inoculation loop).
The first cases were initially observed in Taiwan, where K. pneumoniae is one of the commonest pathogens of community-acquired bacterial meningitis. Subsequently, K. pneumoniae invasive syndrome has been reported in Hong Kong, Korea, Japan and other countries of the Asian Pacific Rim [1]. In Western countries, although an increasing number of cases are being reported, most occur in patients of Asian origin.
Host predisposing factors for acquiring invasive Klebsiella infection are diabetes, chronic liver disease, antibiotic use and alcoholism. The geographic distribution raises the possibility of genetic predisposition for gut colonization, as the prevalence of K. pneumoniae is higher in faecal samples from Asians than from Europeans.
These hypervirulent strains are generally susceptible to most antibiotics. Nevertheless, resistant isolates, including those that produce extended-spectrum beta-lactamases (ESBLs), have been reported. The emergence of such hypervirulent strains is a major concern [2, 3].
CASE DESCRIPTIONS
Over a period of 10 years, we have treated in our ICU three patients of Filipino descent who presented with community-acquired K. pneumoniae meningitis.
The presentations, clinical course and outcomes of these three patients are summarized below and in Table 1. The antibiotic susceptibility profiles of the Klebsiella spp isolates from the patients’ CSF are shown in Table 2. CT scan images of these patients are shown in Figs. 1–4
Table 1.
Patient presentation, clinical course and outcome
| Patient | 1 | 2 | 3 |
|---|---|---|---|
| Gender | Female | Male | Male |
| Age | 57 | 50 | 45 |
| Nationality | Filipino | Filipino | Filipino |
| Medical history | DM untreated, HbA1c: 15% | DM untreated, alcoholism | DM, illicit drug use, Klebsiella pneumoniae deep neck abscess successfully treated 9 months previously |
| Signs and symptoms | Fever, confusion, stiff neck, left hemiparesis | Fever, confusion, stiff neck, seizures | Fever, confusion, stiff neck |
| Blood glucose | 840 mg/dl | 443 mg/dl | 794 mg/dl |
| CSF analysis | WBC: 800 (90% PMN), Glu: 391 mg/dl, Prot.: 95 mg/dl |
WBC: 40,000 (98% PMN) Glu: 114 mg/dl, Prot.: 1,017 |
WBC: 290,000 (90% PMN), Glu 116 mg/dl, Prot.: 14,640 mg/dl |
| CSF culture | Klebsiella pneumoniae | K. pneumoniae | K. pneumoniae/ozaenae |
| Blood culture | K. pneumoniae | K. pneumoniae | Negative |
| Abdominal U/S | Not done | Not done | Negative for liver abscess |
| CT scan | Brain unremarkable (on admission and follow-up), abscesses in liver segment VII and spleen | Brain on admission unremarkable, at 48 h follow-up SAH/severe brain oedema. Abscesses in both lungs and liver segment VII | A few hypodense lesions of the brain stem and white matter |
| Antibiotic treatment on admission | Ceftriaxone, vancomycin, ampicillin/sulbactam + dexamethasone | Ceftriaxone, vancomycin, +dexamethasone | Meropenem, vancomycin, colistin+ dexamethasone |
| ICU LOS | 21 days | 4 days | 14 days |
| Final outcome | Death in ICU due to MOF | Death in ICU due to cerebral oedema | Death in ICU due to MOF |
DM, diabetes mellitus; CSF, cerebrospinal fluid; LOS, length of stay; MOF, multiple organ failure; SAH, subarachnoid haemorrhage.
Table 2.
Antibiotic susceptibility profile of Klebsiella spp isolated in patient CSF
| Patient | Patient | ||||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 1 | 2 | 3 | ||
| Amikacin | S | S | S | Imipenem | S | S | S |
| Amoxicillin/clavulanic acid | S | R | S | Levofloxacin | S | S | |
| Ampicillin | R | R | R | Meropenem | S | S | S |
| Ampicillin/sulbactam | R | R | Minocycline | S | |||
| Aztreonam | S | R | S | Moxifloxacin | S | ||
| Cefalotin | S | R | Nalidixic acid | S | |||
| Cefepime | S | R | S | Netilmicin | S | ||
| Cefixime | R | Nitrofurantoin | R | ||||
| Cefotaxime | R | Norfloxacin | S | ||||
| Cefoxitin | S | R | S | Ofloxacin | S | ||
| Ceftazidime | S | R | S | ||||
| Ceftriaxone | S | R | S | Piperacillin/tazobactam | S | S | S |
| Cefuroxime | S | R | S | Tetracycline | S | S | |
| Cefuroxime axetil | R | Ticarcillin | R | ||||
| Chloramphenicol | S | Tigecycline | S | S | |||
| Ciprofloxacin | S | S | S | Tobramycin | S | ||
| Colistin | S | S | S | Trimethoprim | S | ||
| Gentamicin | S | S | S | Trimethoprim/sulfamethoxazole | S | S | S |
| ESBL positive | + | ||||||
CSF, Cerebrospinal fluid; ESBL, extended spectrum beta lactamase; S, susceptible; R, resistant
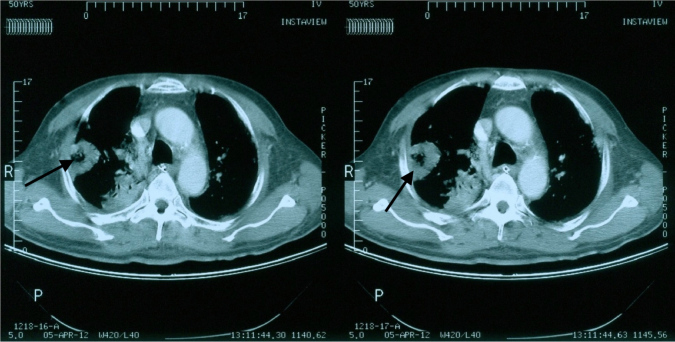
Figure 1.

CT scan of patient 1 showing a hypodense segment VII liver lesion (abscess) and multiple bile stones
Figure 2.
A CT scan of patient 2 showing cavitating pulmonary consolidation
Figure 3.
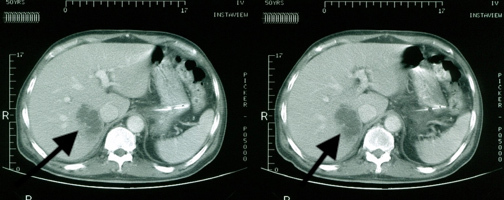
A CT scan of patient 2 showing a hypodense liver lesion compatible with a liver abscess
Figure 4.
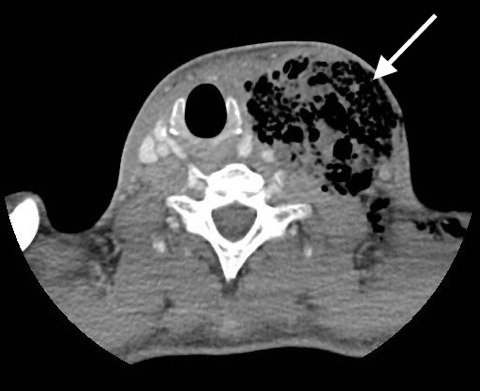
Cervical CT of patient 3 some 9 months before admission showing a neck abscess. The abscess was successfully drained and the pus culture yielded Klebsiella ozaenae
All patients were intubated and required noradrenaline on admission in the emergency department because of a low Glasgow Coma Scale score and septic shock.
Patient 1 had a good response after 72 hours of treatment, fever resolved, a new CSF culture was sterile, and noradrenaline was discontinued. The empiric antibiotic regimen was de-escalated to ceftriaxone as soon as the CSF culture report was available. On the 6th day, a blood culture yielded Candida tropicalis and Staphylococcus aureus. Micafungin and vancomycin were prescribed. A CT scan of the abdomen was performed as part of the candidemia diagnostic work-up and showed a liver abscess and bile stones. On the 10th day, fever relapsed and shock developed. Meropenem and tigecycline were prescribed and ceftriaxone stopped. Percutaneous drainage of the abscess was attempted, but the patient had a cardiac arrest during the procedure. After stabilization, a laparotomy was performed. The gallbladder was removed and surgical drainage performed. There was no improvement and the patient died after 2 days. A blood culture yielded a KPC susceptible only to colistin, cefepime and gentamicin and a pandrug-resistant Providencia stuartii.
Patient 2 developed signs of brain herniation (bilateral mydriasis, with no reaction to light, diabetes insipidus) after 48 hours. A CT scan showed severe brain oedema and subarachnoid haemorrhage. He died on day 4.
Patient 3 did not improve even though the antibiotic regimen was effective against K. pneumoniae/ozaenae, and died in the ICU.
DISCUSSION
The diagnosis of invasive Klebsiella infection in our patients was based solely on clinical grounds (liver abscess, metastatic spread, CNS involvement) as laboratory confirmation (serotyping, string test) was not available. The antibiotic susceptibility pattern of the Klebsiella spp isolates differed from the national Greek pattern (KPC 66.5%) [4] and was consistent with the pattern reported for the hypervirulent strains (cephalosporine, carbapenem sensitive, rarely ESBL+).
Patients 1 and 2 fulfilled the clinical definition criteria proposed by Siu et al. [5]. The abdominal US of patient 3 was negative for abscess. The liver involvement of patient 1 was not identified on admission because invasive Klebsiella infection was not suspected. Nevertheless, the empiric treatment was effective, but the patient died from secondary infections.
The K. pneumoniae of patient 2 was ESBL+, resistant to the empirical treatment. This treatment failure may explain the patient’s rapid deterioration.
To the best of our knowledge, these are the only published cases of this infection in Greece and some of the first reports in patients of Filipino descent worldwide.
In summary, invasive K. pneumoniae infection with CNS involvement has a bad prognosis. Aggressive diagnostic work-up should be done in order to identify occult metastatic spread.
Footnotes
Conflicts of Interests: The authors declare there are no competing interests.
REFERENCES
- 1.Chang W-N, Huang C-R, Lu C-H, Chien C-C. Adult Klebsiella pneumoniae meningitis in Taiwan: an overview. Acta Neurol Taiwan. 2012;21(2):87–96. [PubMed] [Google Scholar]
- 2.Ku Y-H, Chuang Y-C, Chen C-C, Lee M-F, Yang Y-C, Tang H-J, et al. Klebsiella pneumoniae isolates from meningitis: epidemiology, virulence and antibiotic resistance. Sci Rep. 2017;16:1–10. doi: 10.1038/s41598-017-06878-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jun J-B. Klebsiella pneumoniae liver abscess. Infect Chemother. 2018;50(3):210–219. doi: 10.3947/ic.2018.50.3.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Galani I, Karaiskos I, Karantani I, Papoutsaki V, Maraki S, Papaioannou V, et al. Epidemiology and resistance phenotypes of carbapenemase-producing Klebsiella pneumoniae in Greece, 2014 to 2016. Eurosurveillance. 2018;23(31) doi: 10.2807/1560-7917.ES.2018.23.30.1700775. [DOI] [PubMed] [Google Scholar]
- 5.Siu LK, Yeh K-M, Lin J-C, Fung C-P, Chang F-Y. Klebsiella pneumoniae liver abscess: a new invasive syndrome. Lancet Infect Dis. 2012;12(11):881–887. doi: 10.1016/S1473-3099(12)70205-0. [DOI] [PubMed] [Google Scholar]