Graphical abstract
Keywords: Autism spectrum disorder, Child, Behavior, COVID-19, Food supply
Abstract
Background
Research on the impact of the COVID-19 pandemic on behaviors of children with autism spectrum disorder (ASD) is lacking.
Aims
This study investigates the relationship between COVID-19 and behaviors of children with ASD living in the United States.
Methods and procedures
Parents and caregivers (n = 200) across the United States, as proxies for children 2–17 years of age with ASD, participated in an online survey querying changes in overall behavior and 15 specific behaviors during the COVID-19 pandemic. Logistic regression was used to assess the association of a moderate-to-large impact on the child’s overall behavior with household income level and food security status.
Outcomes and results
A majority of respondents reported a moderate-to-large impact on the child’s overall behavior (74 %) due to COVID-19. Several specific behaviors were also affected. Stratifying by income level and food security status revealed disparities in the impact on overall behavior and most specific behaviors. Compared to a household income ≥$100 K, an income <$50 K was associated with an increased risk of moderate-to-large impact on the child’s overall behavior (odds ratio (OR): 4.07, 95 % CI: 1.60, 10.38). Food insecurity also significantly impacted this risk, even after adjusting for potential confounding factors (OR: 3.31, 95 % CI: 1.13, 9.66).
Conclusions and implications
Our findings show a large proportion of caregivers reporting moderate-to-large changes post-COVID-19 in the behaviors of U.S. children with ASD, particularly in families with low income and/or food insecurity. This study highlights the effects of existing disparities on children with ASD and their families during this unprecedented time.
What this paper adds
There are very few studies reporting on the impact of the COVID-19 pandemic on behaviors of children with autism spectrum disorder, particularly in the United States. Further, there is a dearth of knowledge of the differential effects of the pandemic on ASD families by socioeconomic factors. Our study surveys caregivers across the U.S. to understand how ASD families are being affected by COVID-19 and its associated regulations. We report that the overall behavior as well as many specific behaviors of children with ASD have been greatly impacted. We further reveal that families living in low income or food insecure households had a significantly greater risk of reporting a moderate-to large-change in their child’s overall behavior when compared to families living in higher income or food secure households. Thus, this study sheds light on the added burden of the pandemic on ASD families experiencing socioeconomic disparities.
1. Introduction
The coronavirus disease 2019 (COVID-19) pandemic caused by the severe acute respiratory syndrome coronavirus 2 (SARS-Cov-2) has led to fundamental shifts in every sector of society around the world. Specifically, the pandemic has subjected most, if not all, people to navigate self-quarantines, social distancing, school and business closures, and interruption of services, especially in the healthcare sector. Children are a vulnerable population, and research has shown quarantine measures have resulted in anxiety, depression, irritability, and inattention (Panda et al., 2021). Additionally, research on the impacts of previous crises, such as the Middle East Respiratory Syndrome epidemic, has demonstrated their disproportionate negative effects on people with psychiatric and mental health disorders (Jeong et al., 2016). Thus, it is expected that drastic changes associated with the COVID-19 pandemic are particularly disrupting to children with psychiatric and neurodevelopmental disorders, including those with autism spectrum disorder (ASD) (Ameis et al., 2020; Colizzi et al., 2020; Palacio-Ortiz et al., 2020). However, only a handful of studies have reported on changes in moods and behaviors of children with ASD as a result of the pandemic (Amorim et al., 2020; Colizzi et al., 2020; Mutluer et al., 2020). Reported alterations of specific behaviors due to the pandemic among children with ASD include increased stereotypies and aggression, and changes in sleep and appetite (Mutluer et al., 2020).
ASD affects 1 in 54 children in the United States (Maenner et al., 2020) and is characterized by impairments in social communication and interaction along with restricted or repetitive behaviors (APA, 2013). Individuals living with ASD often prefer to follow structured routines and have individualized preferences and routines; for some, even minor disruptions can lead to heightened levels of stress and anxiety (Ameis et al., 2020; Baribeau et al., 2020). Feelings of anxiety or unease brought on by social isolation and confinement may lead to increased stereotypic behaviors, and behaviors during both structured activities and free time (Colizzi et al., 2020; Palacio-Ortiz et al., 2020). Further, the pandemic has caused disruptions in therapeutic treatments, specifically those in person – a great detriment to those with ASD (Palacio-Ortiz et al., 2020).
Recent work from Italy and Portugal has shown the COVID-19 pandemic has considerably affected the ASD community; however, these studies did not explore impacts on child behaviors or account for socioeconomic factors (Amorim et al., 2020; Colizzi et al., 2020). Only one study reported greater food insecurity (80 %) among ASD families living at or below the poverty level compared to those above the poverty level (35 %), but did not discuss the impacts on child behavior patterns (Vasudevan et al., 2020). A dearth of research exists on how the structural changes brought by the COVID-19 pandemic are affecting children with autism in the United States, especially among lower-resource subgroups.
Therefore, using a national web-based survey, we sought to characterize the relationship and severity of the global pandemic on families and children affected with ASD in the United States. Specifically, the goals of this study were twofold: 1) to describe the impact of the COVID-19 pandemic on adverse overall behavior, as well as fifteen specific behaviors, including hyperactivity, distractibility, and repetitive behavior, and 2) to explore if any changes in these behaviors were exhibited by demographic and socioeconomic characteristics, with an emphasis on low resource populations. Data from this study may be useful to tailor public health policy and interventions to mitigate the effects of the pandemic among vulnerable population subgroups within the autism community.
2. Methods
A total of 200 parents and caregivers across the United States participated in an anonymous one-time online survey formulated for understanding the impact of COVID-19 on food environments and eating behaviors in children with ASD. The survey also collected information on the impact of the pandemic on the overall behavior and specific behaviors of the children, which is the focus of the present study. Inclusion criteria were defined as any parent or caregiver over the age of 18 years with a child diagnosed with ASD between the ages of 2–17 years residing in the United States. The survey dates were inclusive of May 6 - June 23, 2020 – a time when most states were under a shelter in place or stay at home order (Chart: Each State’s COVID-19 Reopening and Reclosing Plans and Mask Requirements, 2020). We recruited exclusively through the Internet, advertising through social media channels, primarily Facebook, and did not query any personally identifying information from the participants.
All survey responses were self-reported by the caregiver or parent of a child with (reporter identified) ASD, and took on average under 15 min to complete. Respondents were asked about circumstances prior to and post-regulations brought about by the early phases of the COVID-19 pandemic in the U.S. context. As regulations varied by states and local governing bodies, the survey defined regulations as "shelter-in-place, stay at home, or similar order” by their state or regional legislations. Survey items included questions on respondent and child demographics, anthropometry, socioeconomic status, and the impact of COVID-19 on overall and specific behaviors.
The survey protocol and all materials were approved by the Purdue University Institutional Review Board (IRB-2020-646), and caregivers completed informed-consent procedures as proxies for their children prior to the collection of data. At the end of the survey, participants were given the option to enter an email address using a separatesurvey link (to ensure de-identification of the data reported) to enter a raffle for one of ten $20 Amazon.com gift cards.
2.1. Statistical analysis
Data were analyzed using Stata Statistical Software version 16 (College Station, TX: StataCorp LLC). Descriptive analysis was reported for the following characteristics: U.S. region (Northeast, Midwest, South, and West); shelter-in-place regulation at the time of survey response (yes/no); living with a spouse/partner (yes/no); number of children <18 years of age (n); respondent’s level of education and spouse/partner’s level of education (high school graduate or less, some college or associate degree, college degree, graduate degree or above); household income prior to regulations (<$50 K, $50 K–$100 K, ≥$100 K); household food insecurity status (yes/no); sex of the child (male/female), age of the child (years), age of ASD diagnosis (years), race/Hispanic origin of the child (Non-Hispanic White, Non-Hispanic Black, Hispanic or Latino, Mixed, or “Other” race); child’s weight status (underweight, healthy weight, overweight, or obese); and child’s current educational setting (attending school in person, home-schooled, receiving virtual instruction, or not receiving any instruction). For weight status, estimated weight (lb) and height (in) for each child were converted to metric units and used to calculate body mass index (BMI kg/m2). BMI percentiles were then utilized to categorize weight status as underweight (<5th percentile), healthy weight (5th to <85th percentile), overweight (85th to <95th percentile), or obese (≥95th percentile) according to the growth charts developed by the CDC for children 2–18 years of age (CDC, 2000).
As the primary behavioral outcome, caregivers were asked to rate the change in their child’s behavior as: no change, small change, moderate change, or large change. Descriptive characteristics were analyzed by the differential impact on this behavior outcome using two-tailed t-tests, chi-squared tests, and Fishers exact tests, when required. The outcome was also examined via logistic regression modeling income and food security status as predictors of moderate-to-large changes in overall behavior compared to no change or small changes. We presented these covariates in separate models, in the same model, and finally in the same model with additional defining characteristics including, sex (M/F), age (y), minority status (Y/N), living with a spouse or partner (Y/N), shelter regulations (Y/N), date of survey completion (continuous), rigidity or specificity in food selection or preference (Y/N), and special diet (Y/N). Though income and food security status were highly correlated, the variance inflation factors for all covariates in each model were <5. To improve the precision of our odds ratio estimates, we employed a bootstrap method with 10,000 replications for all models. This replication value was chosen by considering precision and computational demand (Papastergiou & Pappas, 2019; Pattengale et al., 2010).
Specific behaviors were also examined in relation to income level and food security status using two-tailed chi-squared tests, and Fishers exact tests, when required. To capture directionality, participants were asked to select whether they noticed an increase, decrease, or no change in these behaviors. The behaviors included, distractibility, arguing/stubbornness, hyperactivity, tantrums, disrupted sleep, crying, repetitive or restricted behaviors, clinginess, balance aggressiveness, compulsiveness, withdrawing behavior, scripting, obsessive thoughts or perseveration, self-injurious behaviors, and nightmares.
3. Results
In total, 200 parents and caregivers completed the survey and were relatively evenly distributed across all four regions of the U.S. (Table 1 ). This was a convenience sample with 39 of 50 states represented and 32 % represented by Indiana, Illinois, California, and Pennsylvania. Most respondents (77 %) reported a shelter in place or stay at home order at the time of the survey response. Over 76 % of children were male, the mean age of the child was 7.7 years (range 2–17 years), and the mean age of ASD diagnosis was 3.7 years. The majority of children were non-Hispanic White (62 %) followed by Hispanic or Latino (14 %), mixed race (10 %), non-Hispanic Black (7 %), and “other” race (7 %). Of those that disclosed information on anthropometry, 42 % were classified as healthy weight; the remaining 16 %, 16 %, and 26 % were classified as underweight, overweight, and obese, respectively. Most of the adults sampled reported living with a spouse or partner (75 %), with on average two children living in the home. Respondent and spouse/partner education levels were highly correlated (r = 0.63, p < 0.001, data not shown) with 39 % of respondents having some college or an associate degree and 27 % having a graduate degree or higher. Most families (46 %) reported a household income of less than $50 K, compared to 33 % who reported an income of $50 K – <$100 K and 21 % who reported an income of ≥$100 K. Just over 60 % of respondents reported living in a food insecure household post-COVID-19. Most children were homeschooled or receiving virtual instruction (70 %), while 30 % were not receiving any instruction at the time of survey participation.
Table 1.
Household and child characteristics.
| Total |
Impact on Overall Behavior |
||||
|---|---|---|---|---|---|
| None to Small N = 51 |
Moderate to Large N = 148 |
||||
| Household characteristics | N = 200 | n (%) | n (%) | n (%) | P–value |
| U.S. Region | 198 | ||||
| Midwest | 56 (28.3) | 18 (35.3) | 38 (25.9) | ||
| Northeast | 43 (21.7) | 7 (13.7) | 36 (24.5) | ||
| South | 54 (27.3) | 17 (33.3) | 37 (25.2) | ||
| West | 45 (22.7) | 9 (17.7) | 36 (24.5) | 0.18 | |
| Shelter regulationsa | 196 | ||||
| Yes | 151 (77.0) | 39 (78.0) | 112 (76.7) | ||
| No | 39 (19.9) | 11 (22.0) | 28 (19.2) | ||
| Don’t know | 6 (3.1) | 0 (0.0) | 6 (4.1) | 0.76 | |
| Living with spouse/partner | 199 | ||||
| Yes | 149 (74.9) | 44 (86.3) | 105 (71.0) | ||
| No | 50 (25.1) | 7 (13.7) | 43 (29.1) | 0.03 | |
| Children <18y in home, mean (SD) | 192 | 2.1 (1.0) | 2.3 (1.0) | 2.0 (1.0) | 0.08 |
| Respondent educationb | 183 | ||||
| High school graduate or less | 17 (9.3) | 3 (6.3) | 14 (10.4) | ||
| Some college/associate degree | 71 (38.8) | 13 (27.1) | 58 (43.0) | ||
| College degree | 45 (24.6) | 16 (33.3) | 29 (21.5) | ||
| Graduate degree or above | 50 (27.3) | 16 (33.3) | 34 (25.2) | 0.12 | |
| Spouse/partner educationb | 133 | ||||
| High school graduate or less | 19 (14.3) | 4 (9.8) | 15 (16.3) | ||
| Some college/associate degree | 51 (38.4) | 15 (36.6) | 36 (39.1) | ||
| College degree | 30 (22.6) | 8 (19.5) | 22 (23.9) | ||
| Graduate degree or above | 33 (24.8) | 14 (34.2) | 19 (20.7) | 0.38 | |
| Loss of employment reduced pay (either or both caregiver) | 144 | ||||
| Yes | 54 (37.5) | 7 (17.1) | 47 (45.6) | ||
| No | 90 (62.5) | 34 (82.9) | 56 (54.4) | 0.001 | |
| Receiving food resources | 198 | ||||
| Yes | 71 (35.9) | 12 (23.5) | 59 (40.1) | ||
| No | 127 (64.1) | 39 (76.5) | 88 (59.9) | 0.03 | |
| Household income (pre-COVID) | 163 | ||||
| <$50K | 75 (46.0) | 11 (26.2) | 64 (52.9) | ||
| $50 K - <$100K | 54 (33.1) | 17 (40.5) | 37 (30.6) | ||
| ≥$100K | 34 (20.9) | 14 (33.3) | 20 (16.5) | 0.01 | |
| Food Insecurity (post-COVID) | 198 | ||||
| Yes | 119 (60.1) | 18 (36.0) | 101 (68.2) | ||
| No | 79 (39.9) | 32 (64.0) | 47 (31.8) | <0.001 | |
| Child characteristics | N | n (%) | n (%) | n (%) | |
| Sex | 197 | ||||
| Male | 150 (76.1) | 43 (84.3) | 107 (73.3) | ||
| Female | 47 (23.9) | 8 (15.7) | 39 (26.7) | 0.11 | |
| Age, mean (SD)c | 198 | 7.7 (4.1) | 7.4 (4.4) | 7.9 (4.0) | 0.44 |
| Age of diagnosis, mean (SD)c | 193 | 3.7 (2.4) | 3.7 (2.4) | 3.7 (2.4) | 0.96 |
| Race | 195 | ||||
| Non-Hispanic White | 121 (62.1) | 32 (62.8) | 89 (61.8) | ||
| Non-Hispanic Black | 14 (7.2) | 2 (3.9) | 12 (8.3) | ||
| Hispanic or Latino | 27 (13.9) | 7 (13.7) | 20 (13.9) | ||
| Mixed | 19 (9.7) | 7 (13.7) | 12 (8.3) | ||
| Other | 14 (7.2) | 3 (5.9) | 11 (7.6) | 0.71 | |
| Weight status | 103 | ||||
| Underweight | 16 (16.5) | 6 (24.0) | 10 (12.8) | ||
| Healthy weight | 43 (41.8) | 10 (40.0) | 33 (76.7) | ||
| Overweight | 16 (15.5) | 3 (12.0) | 13 (16.7) | ||
| Obese | 27 (26.2) | 6 (24.0) | 22 (28.2) | 0.59 | |
| Educational settingd | 166 | ||||
| Attending school in person | 1 (0.6) | 0 (0.0) | 1 (0.8) | ||
| Homeschooled | 12 (7.2) | 2 (5.1) | 10 (7.9) | ||
| Receiving virtual instruction | 104 (62.7) | 26 (66.7) | 78 (61.4) | ||
| Not receiving any instruction | 49 (29.5) | 32 (62.8) | 89 (61.8) | 0.91 | |
Note: Some percentages may not add up to 100 % due to rounding; Fisher’s exact p-value reported where applicable. Bolded values = p<0.05.
Shelter in place or stay at home order from any governing body; p-value for this variable excluded the “don’t know” category.
High school graduate including GED or other equivalent.
Age in years.
P–value for this variable excluded the “attending school in person” category.
3.1. Primary outcome
Close to three quarters (74 %) of respondents reported a moderate-to-large change in the overall behavior of their child post-COVID 19 regulations, compared to those reporting no change or a small change in overall behavior (Table 1). While most household characteristics did not significantly differ by the impact of the pandemic on overall behavior, there were a few socioeconomic factors that did reflect this contrast. Fewer respondents living with a spouse or partner reported a moderate-to-large change in overall behavior compared to those who did not live with a spouse or partner (p = 0.03). Significant differences were also seen by level of household income (p < 0.01), with 53 % of respondents reporting moderate-to-large changes in overall behavior living with household incomes <$50 K compared to 26 % of respondents reporting the same with household incomes ≥$100 K. Similarly, a greater percentage of caregivers reporting a moderate-to-large impact on the child’s overall behavior reported living in food insecure households (68 %) when compared with those living in food secure households (36 %), and this difference was highly significant (p < 0.001).
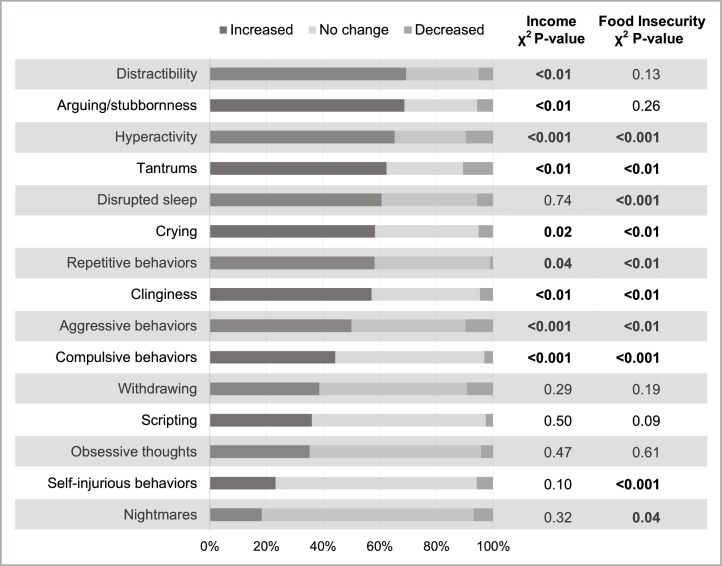
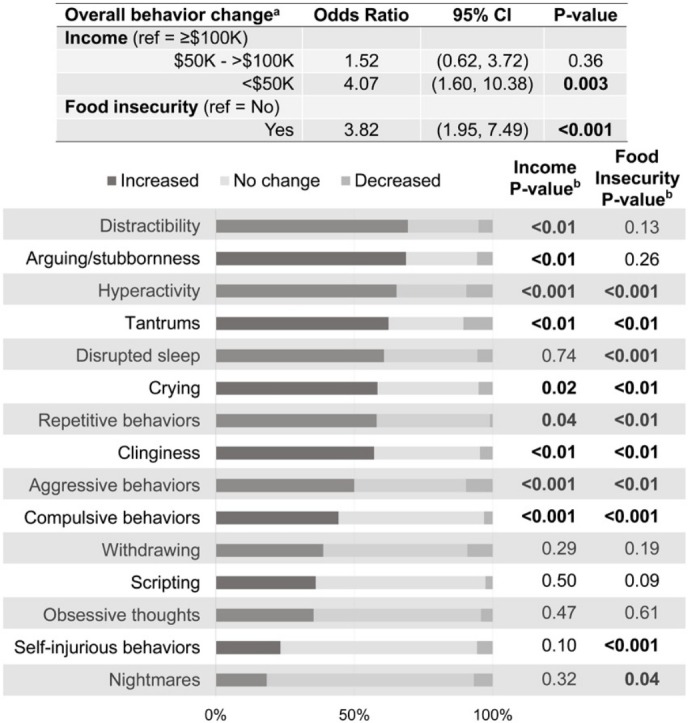
In addition to the impact on overall behavior, a large proportion of caregivers also reported changes in specific behaviors of the children. Close to 70 % of respondents reported increases in distractibility and arguing or stubbornness, followed by hyperactivity, tantrums, and disrupted sleep patterns, each reported by over 60 % of participants (Fig. 1 ). Increases in self-injurious behaviors and nightmares were reported by less than 30 %. However, not all respondents reported increased behaviors; decreased tantrums, hyperactivity, aggressive behaviors, and withdrawing were all reported by around 10 % of the respondents (Fig. 1).
Fig. 1.
Changes in specific child behaviors by level of household income (pre-COVID) and food insecurity (post-COVID).
Noted disparities by household income and food security status were observed for overall behavior and for most specific behaviors. Increased hyperactivity, tantrums, crying, repetitive behaviors or interests, clinginess, aggressiveness, and compulsivity were significantly associated with both lower levels of income and with food insecurity (Fig. 1). For example, 79 % of respondents with a household income <$50 K reported increased hyperactivity compared to 63 % among those with an income of $50 K – <$100 K, and 32 % among those with an income of ≥$100 K (p < 0.001). Similarly, 77 % of those living in food insecure households reported increased hyperactivity in their child post-pandemic while only 48 % of respondents reported increased hyperactivity in food secure households (p < 0.001). Distractibility and arguing/stubbornness were also significantly associated with income level, with over 70 % of families earning <$50 K reporting increased levels of each; however, these behaviors were not significantly associated with food security status. In contrast, increases in disrupted sleep, self-injurious behaviors, and nightmares were significantly associated with food insecurity but not with income status. There were no differences in withdrawing, scripting, or obsessive behaviors based on household income level or food security status. As a check, we compared the responses to changes in overall behavior to changes in specific behaviors using chi squared tests, and each comparison was significant.
Overall, children living in households with lower incomes had a higher risk of negative changes in overall behavior as a result of the pandemic. Regression analysis revealed that having a household income <$50 K (prior to COVID-19 regulations) was significantly associated with an increased risk of moderate-to-large impact of COVID-19 on the child’s overall behavior (crude odds ratio (OR): 4.07; 95 % confidence interval (CI): 1.60, 10.38) when compared to a household income ≥$100 K (Table 2 ). There was no significant difference in the impact on overall behavior between household incomes of $50 K – <$100 K and ≥$100 K. Food insecurity status was also significantly related to the risk of negative impacts on overall behavior – children living in food insecure homes had an increased risk for moderate-to large-changes in overall behavior post-COVID-19 compared to those living in food secure homes (crude OR: 3.82;95 % CI: 1.95, 7.49). When both were added to the same model, however, only food security retained significance. With the addition of other potential confounding factors, including sociodemographic characteristics, food insecurity continued to remain significantly associated with moderate-to-large impact on overall behavior (OR: 3.68; 95 % CI: 1.14, 11.89).
Table 2.
Associations of moderate-to-large impact of post-COVID-19 regulations on overall behavior among children with ASD with income and food insecurity.a
| Odds Ratio | 95 % CI | P–value | |
|---|---|---|---|
| Model I (N = 163) | |||
| Income | |||
| ≥$100K | (ref) | – | – |
| $50 K - >$100K | 1.52 | (0.59, 3.92) | 0.38 |
| <$50K | 4.07 | (1.50, 11.04) | 0.006 |
| Model II (N = 198) | |||
| Food insecurity | |||
| No | (ref) | – | – |
| Yes | 3.82 | (1.92, 7.62) | <0.001 |
| Model III (N = 162) | |||
| Income | |||
| ≥$100K | (ref) | – | – |
| $50 K - >$100K | 1.23 | (0.47, 3.25) | 0.67 |
| <$50K | 2.12 | (0.75, 6.03) | 0.16 |
| Food insecurity | |||
| No | (ref) | – | – |
| Yes | 3.19 | (1.42, 7.18) | 0.005 |
| Model IV (N = 120) | |||
| Sex | |||
| Female | (ref) | – | – |
| Male | 2.32 | (0.53, 10.17) | 0.28 |
| Age | 1.07 | (0.93, 1.23) | 0.33 |
| Minority race | 0.57 | (0.15, 2.09) | 0.35 |
| Shelter regulations | 0.40 | (0.10, 1.66) | 0.17 |
| Loss of employmentb | 3.46 | (0.84, 14.23) | 0.06 |
| Food resourcesc | 0.62 | (0.09, 4.02) | 0.61 |
| Income | |||
| ≥$100K | (ref) | – | – |
| $50 K - >$100K | 1.19 | (0.33, 4.25) | 0.87 |
| <$50K | 3.18 | (0.37, 27.54) | 0.27 |
| Food insecurity | |||
| No | (ref) | – | – |
| Yes | 3.84 | (1.05, 14.00) | 0.04 |
Bolded values = p<0.05.
Child overall behavior defined as none to small (ref) vs. moderate-to-large; logistic regression models with income prior to COVID-19 and food security post-onset of COVID-19.
Loss of employment or reduced pay for one or both caregivers.
Receiving food resources including, SNAP, WIC, food stamps, mobile meals, food pantry, school meals, meals for elderly, etc.
4. Discussion
More than half of families reported negative changes in behavior of children living with ASD as a result of the COVID-19 pandemic; these negative changes disproportionately impacted families with food insecurity and those living with annual incomes <$50 K. Given few studies have characterized the specific needs of ASD families in the United States during COVID-19, our results shed initial light on the overall and specific behavioral challenges families are encountering. A majority of the caregivers in our study reported moderate-to-large impacts of COVID-19 on the overall behavior of their child. Our estimate of 74 % for these changes in overall behavior parallels a recent estimate from Italy, where 76 % of respondents indicated difficulties managing structured activities (Colizzi et al., 2020), and another from Portugal in which 77 % of children were reported as having worsened behavior problems (Amorim et al., 2020).
We also observed changes in child behaviors that may increase risk for adverse health outcomes. For example, behaviors such as distractibility, hyperactivity, and disruptive sleep, commonly reported in our study, are characteristic of attention deficit hyperactivity disorder (ADHD), a disorder highly co-morbid with ASD (Antshel & Russo, 2019). Proper sleep is a cornerstone for human health, and inadequacies have been shown to exacerbate already existing adverse symptoms and behaviors in individuals with ASD (Becker & Gregory, 2020). Recent research shows changes in sleep patterns due to the COVID-19 pandemic may result in aggression and anxiety among children with ASD (Ameis et al., 2020). Furthermore, research on the impacts of the COVID-19 pandemic on children with ADHD illustrates increased conduct problems (Nonweiler et al., 2020) as well as increased risk of infection with the virus among young people with ADHD compared to controls (Merzon et al., 2020). Our results for increased arguing or stubbornness (69 %), and withdrawing behavior (40 %) mirror research showing decreased prosocial behaviors among children with ASD compared with controls post-COVID-19 (Nonweiler et al., 2020). A recent study in Turkey also reported significantly increased hyperactivity, aggression, sleep disturbances, stereotypic behavior, and withdrawing behavior, which were all reported by our respondents to varying degrees (Mutluer et al., 2020). However, while caregivers reported increases in adverse behaviors such as hyperactivity, tantrums, withdrawing, and aggressive behaviors in our study, around 10 % reported decreases in these specific behaviors, suggesting that not all families are experiencing the pandemic similarly. While these findings are not surprising given the heterogeneity of ASD phenotypes, they may have also been due to positive changes in diet, increased time spent with family, or other structural changes that should be explored in future research (Ameis et al., 2020).
Most importantly, our results illuminate how COVID-19 is differentially impacting families by those experiencing food insecurity, despite level of income and other potentially confounding factors. Food insecurity is defined by the Unites States Department of Agriculture as “a household-level economic and social condition of limited or uncertain access to adequate food” (Coleman-Jensen et al., 2020). At even marginal levels (one or two indicators), food insecurity is associated with behavioral, emotional, and academic problems from early childhood to adolescence, adjusting for potential confounding factors (Shankar et al., 2017). Food insecurity can also be detrimental to the cognitive development of children, especially those with neurodevelopmental disorders including ASD (Althoff et al., 2016). The percentage of food insecurity status in our study (55–60 %) is comparable to a recent larger study by Autism Speaks that examined food security status among ASD families in November and December, 2020 (52 %) (Vasudevan et al., 2021). Furthermore, while this recent study reported differences in demographic and socioeconomic characteristics by food security status among these families, associations with behavior changes were not examined.
Low-income children are more likely to live in food insecure households (Coleman-Jensen et al., 2013); however, as our study suggests, while both and low income and food insecurity may have an impact on adverse outcomes in children, income level alone does not fully describe these effects. For example, previous research has shown that living in a low-income household without food insecurity did not have an adverse impact on inattention/ hyperactivity and that the effect was specifically related to household food insecurity status (Melchior et al., 2012). It is interesting to note that changes in disruptive sleep have also been shown to be significantly associated with household food insecurity but not with income level in our study (Kalousová et al., 2019; Na et al., 2020). Thus, while food insecurity is an issue across the board, and particularly during this pandemic, our findings reveal the disproportional weight of this circumstance on ASD families and their children.
Our study was not without limitations. As this was a cross-sectional study, we could not report on differences before and after the onset of the pandemic other than self-report, which may have led to recall and information biases. This study also only examined ASD families and did not consider a control group. Lastly, a limitation of which to be mindful is the difference in sample sizes of the regression models. For example, the sample size for the income level model was smaller compared to the food security status model (n = 163 vs 198) as was the fully adjusted model (n = 120).
Our finding that food security status was a significant factor, even after adjusting for socioeconomic and demographic factors, calls for more food policies and interventions to effect change in the pandemic’s impact on overall behavior of children with ASD. Research on the impacts of COVID-19 have revealed food insecurity has intensified among families across the US (Adams et al., 2020; Pereira & Oliveira, 2020). Financial assistance may be one way to assist these families, including supplemental grants and funding specifically targeting food access. Basic infrastructure and services, availability of markets with high-quality foods, quality of school meals and school-based services, and household access to food all need to be addressed. To effect changes for these low-resource ASD families, systems-level and civil society approaches must take place.
Policies to address these issues are necessary, not only for minimizing impacts on challenging behaviors in children with ASD; they are also needed for providing adequate and equitable care for ASD families especially given the differential impact of food security status (Ameis et al., 2020). For example, some countries have provided financing for farmers to meet the demands of their local communities and have incentivized the distribution of high quality foods to vulnerable populations (Pereira & Oliveira, 2020). Monitoring food prices in urban areas that have been hardest hit by the pandemic and planning for social protections, including food security are additional approaches (Pereira & Oliveira, 2020). For ASD families specifically, providing extra behavioral supports to families with food insecurity may also be required as they will likely have residual challenging behaviors even with these protections in place. For example, programs that deploy telehealth-based behavioral supports could help families manage the challenges that are coming up around food-related routines and changes. Providing wraparound social work and/or mental health support for caregivers could also be another source of support for these families.
4.1. Conclusion
The COVID-19 pandemic has brought forth many significant public health challenges. Children with ASD who tend to have more structured preferences and patterns are disproportionately at risk for adverse outcomes. In this cross-sectional study, our findings show a large proportion of caregivers reporting moderate-to-large changes in overall and specific behaviors, with greatest impact among low income and food insecure households. The types of challenges families experienced varied across income, suggesting public health policies and interventions should be customized to the diverse needs of families. Together, our results may inform future policy and interventions to reduce the negative impacts of COVID-19 on individuals with ASD and their families.
CRediT authorship contribution statement
Anita A. Panjwani and Bridgette L. Kelleher were involved in the conception, design, and methodology. All authors were involved in the analysis and interpretation of the data. Anita A. Panjwani drafted the initial manuscript, Regan L. Bailey and Bridgette L. Kelleher reviewed the manuscript, and all authors approved of the final manuscript.
Declaration of Competing Interest
The authors have no conflicts of interest to declare.
Acknowledgements
The authors are sincerely thankful to all the study participants for the time and energy they put forth to support this research study. We also thank Shinyoung Jun, Ph.D. (Department of Nutrition Sciences, Purdue University) for her insights and contribution to this manuscript.
This work was supported by Purdue University through the Discovery Park Big Idea Challenge Grant (PI Kelleher), USA and the National Institute of Mental Health (K23MH111955, PI Kelleher), USA.
Number of reviews completed is 2
References
- Adams E.L., Caccavale L.J., Smith D., Bean M.K. Food insecurity, the home food environment, and parent feeding practices in the era of COVID-19. Obesity (Silver Spring) 2020;28(November (11)):2056–2063. doi: 10.1002/oby.22996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Althoff R.R., Ametti M., Bertmann F. The role of food insecurity in developmental psychopathology. Preventive Medicine. 2016;92:106–109. doi: 10.1016/j.ypmed.2016.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ameis S.H., Lai M.C., Mulsant B.H., Szatmari P. Coping, fostering resilience, and driving care innovation for autistic people and their families during the COVID-19 pandemic and beyond. Molecular Autism. 2020;11(1):61. doi: 10.1186/s13229-020-00365-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amorim R., Catarino S., Miragaia P., Ferreras C., Viana V., Guardiano M. The impact of COVID-19 on children with autism spectrum disorder. Revista de Neurologia. 2020;71(8):285–291. doi: 10.33588/rn.7108.2020381. (Impacto de la COVID-19 en niños con trastorno del espectro autista.) [DOI] [PubMed] [Google Scholar]
- Antshel K.M., Russo N. Autism Spectrum disorders and ADHD: Overlapping phenomenology, diagnostic issues, and treatment considerations. Current Psychiatry Reports. 2019;21(5):34. doi: 10.1007/s11920-019-1020-5. [DOI] [PubMed] [Google Scholar]
- APA . American Psychiatric Association; 2013. Diagnostic and statistical manual of mental disorders. [Google Scholar]
- Baribeau D.A., Vigod S., Pullenayegum E., Kerns C.M., Mirenda P., Smith I.M., Vaillancourt T., Volden J., Waddell C., Zwaigenbaum L., Bennett T., Duku E., Elsabbagh M., Georgiades S., Ungar W.J., Zaidman-Zait A., Szatmari P. Repetitive behavior severity as an early Indicator of risk for elevated anxiety symptoms in autism Spectrum disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2020;59(7):890–899. doi: 10.1016/j.jaac.2019.08.478. e893. [DOI] [PubMed] [Google Scholar]
- Becker S.P., Gregory A.M. Editorial Perspective: Perils and promise for child and adolescent sleep and associated psychopathology during the COVID-19 pandemic. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 2020;61(7):757–759. doi: 10.1111/jcpp.13278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC . 2000. A SAS program for the CDC growth charts.http://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm Retrieved October 12, 2020, from. [Google Scholar]
- Chart: Each State’s COVID-19 Reopening and Reclosing Plans and Mask Requirements . 2020. The national academy for state health policy.https://www.nashp.org/governors-prioritize-health-for-all/ Retrieved November 5, 2020, from. [Google Scholar]
- Coleman-Jensen A., Nord M., Singh A. 2013. Household food security in the United States in 2012 (ERR-155)https://www.ers.usda.gov/webdocs/publications/45129/39937_err-155.pdf?v=42199 Retrieved November 23, 2020, from. [Google Scholar]
- Coleman-Jensen A., Rabbitt M.P., Gregory A.C. Economic Research Service, United States Department of Agriculture; 2020. Definitions of food security.https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/definitions-of-food-security/ [Google Scholar]
- Colizzi M., Sironi E., Antonini F., Ciceri M.L., Bovo C., Zoccante L. Psychosocial and behavioral impact of COVID-19 in autism Spectrum disorder: An online parent survey. Brain Sciences. 2020;10(6) doi: 10.3390/brainsci10060341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeong H., Yim H.W., Song Y.J., Ki M., Min J.A., Cho J., Chae J.H. Mental health status of people isolated due to Middle East Respiratory Syndrome. Epidemiology and Health. 2016;38 doi: 10.4178/epih.e2016048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalousová L., Xiao B., Burgard S.A. Material hardship and sleep: Results from the Michigan Recession and Recovery Study. Sleep Health. 2019;5(2):113–127. doi: 10.1016/j.sleh.2018.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maenner M.J., Shaw K.A., Baio J., Washington A., Patrick M., DiRienzo M., Christensen D.L., Wiggins L.D., Pettygrove S., Andrews J.G., Lopez M., Hudson A., Baroud T., Schwenk Y., White T., Rosenberg C.R., Lee L.C., Harrington R.A., Huston M.…Dietz P.M. Prevalence of autism Spectrum disorder among children aged 8 years - autism and developmental disabilities monitoring network, 11 sites, United States, 2016. Morbidity and Mortality Weekly Report Surveillance Summaries. 2020;69(4):1–12. doi: 10.15585/mmwr.ss6904a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melchior M., Chastang J.F., Falissard B., Galéra C., Tremblay R.E., Côté S.M., Boivin M. Food insecurity and children’s mental health: A prospective birth cohort study. PloS One. 2012;7(12) doi: 10.1371/journal.pone.0052615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merzon E., Manor I., Rotem A., Schneider T., Vinker S., Golan Cohen A., Lauden A., Weizman A., Green I. ADHD as a risk factor for infection with Covid-19. Journal of Attention Disorders. 2020 doi: 10.1177/1087054720943271. 1087054720943271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mutluer T., Doenyas C., Aslan Genc H. Behavioral implications of the Covid-19 process for autism Spectrum disorder, and individuals’ comprehension of and reactions to the pandemic conditions. Frontiers in Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.561882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Na M., Eagleton S.G., Jomaa L., Lawton K., Savage J.S. Food insecurity is associated with suboptimal sleep quality, but not sleep duration, among low-income Head Start children of pre-school age. Public Health Nutrition. 2020;23(4):701–710. doi: 10.1017/s136898001900332x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nonweiler J., Rattray F., Baulcomb J., Happé F., Absoud M. Prevalence and associated factors of emotional and behavioural difficulties during COVID-19 pandemic in children with neurodevelopmental disorders. Children. 2020;7(9) doi: 10.3390/children7090128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palacio-Ortiz J.D., Londoño-Herrera J.P., Nanclares-Márquez A., Robledo-Rengifo P., Quintero-Cadavid C.P. Psychiatric disorders in children and adolescents during the COVID-19 pandemic. Revista Colombiana de Psiquiatria. 2020;49(October–December (4)):279–288. doi: 10.1016/j.rcp.2020.05.006. English, Spanish. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panda P.K., Gupta J., Chowdhury S.R., Kumar R., Meena A.K., Madaan P., Sharawat I.K., Gulati S. Psychological and behavioral impact of lockdown and quarantine measures for COVID-19 pandemic on children, adolescents and caregivers: A systematic review and meta-analysis. Journal of Tropical Pediatrics. 2021;67(January (1)) doi: 10.1093/tropej/fmaa122. fmaa122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papastergiou A., Pappas V. A comparison of sighted and visually impaired children’s text comprehension. Research in Developmental Disabilities. 2019;85:8–19. doi: 10.1016/j.ridd.2018.10.003. [DOI] [PubMed] [Google Scholar]
- Pattengale N.D., Alipour M., Bininda-Emonds O.R., Moret B.M., Stamatakis A. How many bootstrap replicates are necessary? Journal of Computational Biology: A Journal of Computational Molecular Cell Biology. 2010;17(3):337–354. doi: 10.1089/cmb.2009.0179. [DOI] [PubMed] [Google Scholar]
- Pereira M., Oliveira A.M. Poverty and food insecurity may increase as the threat of COVID-19 spreads. Public Health Nutrition. 2020;23(December (17)):3236–3240. doi: 10.1017/S1368980020003493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shankar P., Chung R., Frank D.A. Association of food insecurity with children’s behavioral, emotional, and academic outcomes: A systematic review. Journal of Developmental and Behavioral Pediatrics: JDBP. 2017;38(2):135–150. doi: 10.1097/dbp.0000000000000383. [DOI] [PubMed] [Google Scholar]
- Vasudevan V., Karpur A., Shih A., Frazier T. Food insecurity in households of people with autism spectrum disorder during the COVID-19 pandemic. medRxiv. 2021 doi: 10.1101/2021.03.30.21254339. 2021.2003.2030.21254339. [DOI] [Google Scholar]