Abstract
Background
Multiligament knee injuries, though rare, can be profoundly disabling. Surgeons disagree about when to initiate rehabilitation after surgical reconstruction due to the conflicting priorities of postoperative stability and motion.
Questions/purposes
(1) Does early or late initiation of physical therapy after multiligament knee surgery result in fewer postoperative manipulations? (2) Does early versus late physical therapy compromise stability postoperatively? (3) Does early initiation of physical therapy result in improved patient-reported outcomes, as measured by the Multi-ligament Quality of Life (ML-QOL) score?
Methods
Between 2011 and 2016, 36 adults undergoing multiligament repair or reconstruction were prospectively enrolled in a randomized controlled trial and randomized 1:1 to either early rehabilitation or late rehabilitation after surgery. Eligibility included those with an injury to the posterior cruciate ligament (PCL) and at least one other ligament, as well as the ability to participate in early rehabilitation. Patients who were obtunded or unable to adhere to the protocols for other reasons were excluded. Early rehabilitation consisted of initiating a standardized physical therapy protocol on postoperative day 1 involving removal of the extension splint for quadriceps activation and ROM exercises. Late rehabilitation consisted of full-time immobilization in an extension splint for 3 weeks. Following this 3-week period, both groups engaged in the same standardized physical therapy protocol. All surgical reconstructions were performed at a single center by one of two fellowship-trained sports orthopaedic surgeons, and all involved allograft Achilles tendon PCL reconstruction. When possible, hamstring autograft was used for ACL and medial collateral ligament reconstructions, whereas lateral collateral ligament and posterolateral reconstruction was performed primarily with allograft. The primary outcome was the number of patients undergoing manipulation during the first 6 months. Additional outcomes added after trial registration were patient-reported quality of life scores (ML-QOL) at 1 year and an objective assessment of laxity through a physical examination and stress radiographs at 1 year. One patient from each group was not assessed for laxity or ROM at 1 year, and one patient from each group did not complete the ML-QOL questionnaires. No patient crossover was observed.
Results
With the numbers available, there was no difference in the use of knee manipulation during the first 6 months between the rehabilitation groups: 1 of 18 patients in the early group and 4 of 18 patients in the late group (p = 0.34). Similarly, there were no differences in knee ROM, stability, or patient-reported quality of life (ML-QOL) between the groups at 1 year.
Conclusion
With the numbers available in this study, we were unable to demonstrate a difference between early and late knee rehabilitation with regard to knee stiffness, laxity, or patient-reported quality of life outcomes. The results of this small, randomized pilot study suggest a potential role for early rehabilitation after multiligament reconstruction for knee dislocation, which should be further explored in larger multi-institutional studies.
Level of Evidence
Level II, therapeutic study.
Introduction
The treatment of the dislocated knee has been controversial. Surgical versus nonoperative management, reconstruction versus repair of torn ligaments, and early versus late surgery have all been subjects of debate [22, 26, 27]. However, several studies and systematic reviews have shown that operative intervention of multiligamentous knee injuries likely improves functional outcomes, with uncertain effects on instability, return to activity, and ROM [37, 39, 52, 54]. Likewise, anatomic reconstruction has been suggested to be superior to repair of ACL, posterior cruciate ligament (PCL), lateral collateral ligament (LCL), and midsubstance medial collateral ligament (MCL) injuries in terms of stability, return to activity, and flexion ROM [25, 30, 39]. However, evidence has emerged that bony avulsions of the fibular head, PCL, and MCL are best treated with repair [9, 16]. Still in question is whether a period of strict immobilization or early functional rehabilitation after multiligament knee surgery provides a better balance between instability and stiffness [20, 28, 33, 46].
This desired balance between laxity and stiffness has proven difficult to achieve after multiligament knee surgery [47]. To mitigate the risk of attenuation of reconstructed ligaments and resultant laxity, many surgeons prescribe a period of knee immobilization and nonweightbearing postoperatively, particularly after all-allograft reconstructions [11-14, 18, 32, 49]. However, studies examining postoperative complications have demonstrated that loss of ROM and arthrofibrosis are both more prevalent and more disabling than postoperative laxity [1, 3, 19, 29, 35, 36, 47, 48]. One systematic review postulates that stiffness after multiligament reconstruction could be caused or worsened by a period of postoperative immobilization [33]. Excessive arthrofibrosis often results in additional procedures, such as manipulation under anesthesia and arthroscopic lysis of adhesions, which expose patients to additional risks and further disability and increase healthcare system costs [4, 41]. To better understand the tradeoffs between early motion and immobilization in the setting of multiligamentous knee injuries associated with knee dislocation, we designed a randomized controlled pilot study.
We asked: (1) Does early or late initiation of physical therapy after multiligament knee surgery result in fewer postoperative manipulations? (2) Does early versus late physical therapy compromise stability postoperatively? (3) Does early initiation of physical therapy result in improved patient-reported outcomes, as measured by the Multi-ligament Quality of Life (ML-QOL) score?
Patients and Methods
Patient Eligibility and Selection
Between June 2011 and December 2016 (67 months), adults (older than 18 years) undergoing multiligament knee repair and/or reconstruction at a Level I trauma and tertiary referral academic hospital were screened for eligibility for our randomized controlled trial.
The inclusion criteria included MRI confirmation of a high-grade multiligament knee injury involving the PCL and, at a minimum, one other ligament treated with surgical fixation. Patients were required to have been ambulatory without aids before their injury. When possible, patients were encouraged to obtain full extension and 90° flexion before surgery. Patients were excluded if they had concurrent injuries or postinjury deficits impairing rehabilitation, ipsilateral vascular injuries treated with repair, or previous surgery of the affected knee.
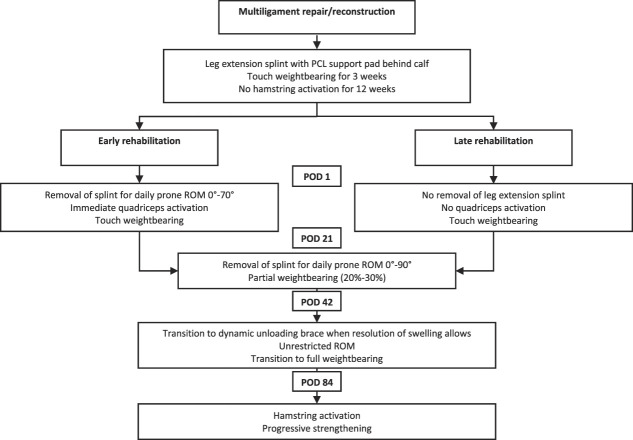
Over the 67 months during which the study was active, 82 patients were assessed for eligibility. Fifty-six percent (46 of 82) of the patients were excluded. The most common reasons for exclusion were no PCL injury (nine patients), associated fracture (eight patients), and concomitant vascular injury (six patients). Two patients refused participation (Fig. 1). This resulted in 36 patients being randomized, with 18 in each group.
Fig. 1.
This CONSORT diagram shows how patients were selected for inclusion in this study; PCL = posterior cruciate ligament; HTO = high tibial osteotomy.
Study Size and Randomization
Given the paucity of quality data describing the need for manipulation after modern multiligament knee reconstruction at the time of study design, we conducted a sample size calculation based on unpublished data from a survey of knee dislocation experts [27] at the 2010 Knee Dislocation Study Group meeting. The minimal clinically important reduction in manipulation was set to 40%, with an alpha of 0.05 and a power of 0.8, resulting in a targeted sample size of 35 patients per group after accounting for loss to follow-up. Because of the challenges with recruiting patients with these rare injuries, enrollment was stopped after 5 years, with 36 included patients and the study was analyzed as pilot-level data to inform future research.
Eligible patients were approached, provided informed consent, and were randomized at the time of the operation (via permuted blocks of varying size between two and four) in a 1:1 fashion to either early rehabilitation or late rehabilitation (Fig. 2). Thirty-five patients underwent reconstruction for ligamentous tears, and one patient in the early rehabilitation group underwent fixation of PCL avulsion. With the numbers available, we observed no differences between the groups with respect to age, gender, BMI, or Schenck injury classification (Table 1). Patient demographics and injury characteristics were collected preoperatively (see Table 1; Supplemental Digital Content 1, http://links.lww.com/CORR/A533). Injuries were graded using the Schenck Classification [42]. The treating surgeon, outcome assessors, and data analysts were blinded to the patients’ randomization (Fig. 1).
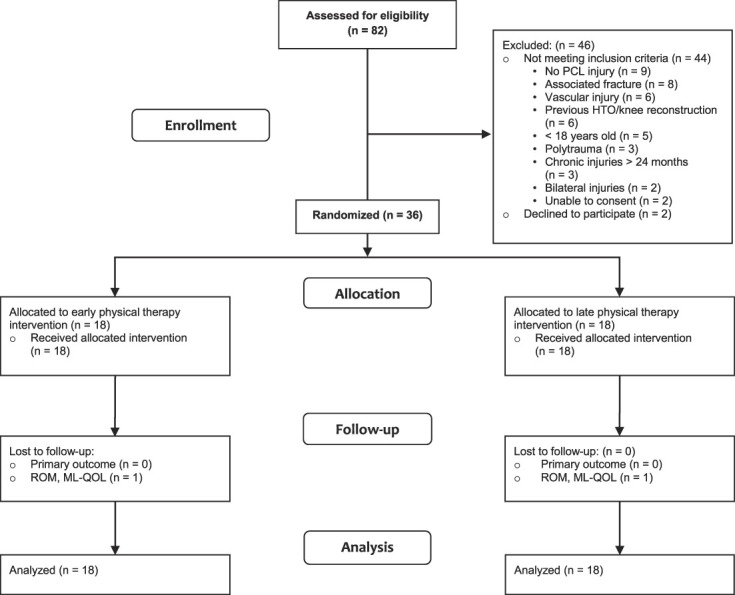
Fig. 2.
This flowchart depicts postoperative restrictions and the physical therapy plan; PCL = posterior cruciate ligament; POD = postoperative day.
Table 1.
Demographic and injury characteristics of the early rehabilitation and late rehabilitation groups
| Demographic and injury factors | Early rehabilitation (n = 18) | Late rehabilitation (n = 18) | p value |
| Age in years | 36 ± 12 | 36 ± 12 | 0.89a |
| Sex (male:female) | 12:6 | 16:2 | 0.11b |
| BMI in kg/m2 | 30 ± 7 | 28 ± 5 | 0.20a |
| Side (left:right) | 8:10 | 6:12 | 0.59c |
| Dislocation direction (medial: lateral: direct AP) | 6:11:1 | 6:11:1 | > 0.99b |
| Mechanism of injury (sports:low-energy:high-energy) | 9:1:7 | 9:3:6 | 0.72c |
| Schenck classification (1:2:3:4:5) | 3:0:15:1:0 | 2:0:14:1:0 | 0.70d |
| Days to surgery | 25 (18-146) | 19 (13-30) | 0.12e |
Data presented as mean ± SD or median (IQR).
t-test.
Fisher exact test.
Chi-square test.
Kruskal-Wallis test.
Mann-Whitney U test.
Surgery
All surgical interventions were performed at one tertiary academic center by one of two fellowship-trained orthopaedic sports surgeons (DBW, AN [not a study author]). High-grade ACL and PCL injuries, defined as those with clinical laxity grading greater than 2 and/or MRI evidence of complete tear, were reconstructed as single-bundle constructs. A tendoachilles allograft with a retained calcaneal bone block was used for all PCL reconstructions. ACL reconstructions were performed with hamstring autograft when possible (94% [29 of 31] of patients). In patients with injured hamstring tendons (one early rehabilitation) or request for all-allograft reconstruction (one late rehabilitation), a tendoachilles allograft was used for ACL reconstruction. ACL and PCL grafts were fixed primarily with an interference screw and secondarily with sutures from the graft tied around a post on both the femoral and tibial sides. Bony avulsions of the PCL were fixed directly with screw fixation (one early rehabilitation). MCL tibial avulsions were repaired using suture anchors and a double-row technique (two early rehabilitation and four late rehabilitation) [53]. MCL reconstruction was performed for midsubstance injuries or femoral avulsions without bone involvement using a hamstring autograft when possible (four early rehabilitation, three late rehabilitation), occasionally from the contralateral leg when the ipsilateral hamstring was used for ACL reconstruction (n = 3). One patient’s MCL was reconstructed using a tendoachilles allograft (early rehabilitation). MCL grafts were fixed to the femur with an interference screw for primary fixation and secondarily using sutures from the graft tied around a post. On the tibia, a screw-and-washer fixation method was used. Bony avulsions of the LCL were primarily repaired using imbricating and tensioning sutures to restore ligamentous length and integrity and subsequently fixed to bone with screws and soft-tissue washers (one late rehabilitation). LCL reconstructions were performed using either posterior tibial tendon allograft (seven early rehabilitation, eight late rehabilitation) or tendoachilles allograft (five early rehabilitation, three late rehabilitation), depending on availability. The posterolateral corner was reconstructed if a high-grade injury was confirmed via clinical examination and/or MRI. A modified LaPrade technique [43] using a single tendoachilles graft with bifid limbs was used for this when required (10 early rehabilitation, four late rehabilitation).
Perioperative Care
Patients received weight-based dosing of an appropriate antibiotic before surgical incisions in accordance with our institutional guidelines on surgical prophylaxis. All patients were admitted to the hospital postoperatively. Intravenous antibiotics were continued for 24 hours postoperatively. Patients were subsequently transitioned to oral antibiotics for 7 days of total coverage, as has been described elsewhere [15]. All patients were given weight-based dosing of subcutaneous low-molecular-weight heparin as prophylaxis against deep vein thrombosis while in the hospital and following discharge for 3 weeks of total therapy. All patients were placed in a removable extension splint with a foam pad located posteriorly under the tibia for PCL support postoperatively. All patients were seen daily by the inpatient physical therapy department for exercise initiation (early rehabilitation group) and/or crutch training (both groups). Patients were discharged on postoperative day 2 or 3.
Rehabilitation Interventions
Early Rehabilitation
Patients began physical therapy on postoperative day 1 as an inpatient and were instructed to continue with in-person sessions at an outpatient center of their choice after discharge for a minimum of twice per week for the first 6 weeks and weekly thereafter. Patients were made touch weightbearing (foot flat, heel to toe gait) from weeks 0 to 3 in their extension splint and were permitted to remove the splint for passive ROM from 0° to 70° in the prone position (Fig. 2). This advanced in weeks 3 to 6 to partial weightbearing (20%-30%) and active and passive assisted ROM of 0° to 90° (still prone). During weeks 6 to 12, patients advanced to full weightbearing and were permitted unrestricted ROM in the supine position. A strengthening phase was initiated, predominantly with quadriceps activation. Hamstring activation was restricted until 12 weeks. After 3 months, patients worked on progressive strengthening activities and a graduated return to sports (Fig. 2). We ensured continuity and the patient’s adherence to physical therapy as an outpatient by requiring the first session to be arranged before hospital discharge, and we reviewed physical therapy notes at each follow-up appointment.
Late Rehabilitation
Patients were immobilized for 3 weeks postoperatively in a knee extension splint at all times and were allowed only touch weightbearing (foot flat, heel to toe gait), and no ROM or muscle activation was permitted to ensure compliance with full-time bracing. At 3 weeks postoperatively, patients began physical therapy at an outpatient center of their choice, for a minimum of two in-person sessions per week for the next 3 weeks and weekly thereafter (Fig. 2). This portion of the rehabilitation was identical to that of the early rehabilitation group, with patients permitted to remove their extension splint for exercises. We ensured that patients initiated and adhered to physical therapy as an outpatient by requiring the first session to be arranged before hospital discharge, and we reviewed physical therapy notes at each follow-up appointment.
Outcomes, Follow-up, and Data Acquisition
Follow-up appointments were scheduled as per typical practice at the 2-week, 6-week, 3-month, 6-month, 1-year, and 2-year postoperative timepoints. The 2-week appointment was a wound check and adverse event screen performed by the treating surgeon. An unblinded member of the team (an orthopaedic resident or fellow) screened physiotherapy notes at the 2- and 6-week appointments to assess for adherence and crossover. No crossover was observed between groups. From week 6 onward, ROM was assessed by a blinded advanced-practice physiotherapist at each clinic visit via goniometer measurement.
The primary outcome was manipulation under anesthesia or revision surgery. At the 3-month and 6-month follow-up appointments, patients were assessed to determine whether they should undergo manipulation, which included manipulation under anesthesia and arthroscopic debridement of arthrofibrosis. Objective indications for manipulation included any of the following: < 90° of flexion, > 10° of extension loss, and < 90° total arc of motion. Manipulation and arthroscopic debridement were recommended for patients meeting any of these indications at either the 3-month or 6-month appointment.
We added secondary endpoints including ROM, injury- specific patient-reported QOL, and clinically and radiographically graded stability after trial registration but before patient enrollment. For patient-reported outcomes, we used the ML-QOL tool, which is a reliable, validated, injury-specific patient questionnaire that consists of four domains to capture the multifaceted impact a knee dislocation can have on patients: physical impairments, emotional impairments, activity limitations, and societal involvement [5]. Scores were recorded at the 1-year follow-up visit.
At 1 year postoperatively, varus and valgus stress radiographs of the operated-on knee were obtained to assess coronal laxity, as previously described [23, 24, 31]. Sagittal laxity was assessed with Lachman and posterior drawer physical examination maneuvers. Stability was assessed by the treating surgeon, who was also blinded.
Complications including mortality, performance of revision surgery, deep venous thrombosis, or deep infection resulting in irrigation and debridement were recorded at each follow-up visit.
All 36 patients were assessed for the primary outcome of the study—performance of manipulation at 3 months and 6 months without any loss to follow-up. One patient in each group did not complete the ML-QOL questionnaires, and one patient from each group did not undergo assessment of their ROM or clinical laxity at 1 year postoperatively. There were no recorded major postoperative complications at 1 year, other than the documented need for manipulation.
Ethical Approval
The study was approved by the research ethics board (REB) at our home institution and registered at Clinicaltrials.gov with the identifier NCT01296750. Initial trial registration specified the primary outcome as manipulation within 6 months. The secondary outcomes of ROM, injury-specific patient-reported QOL, and clinical and radiographic laxity were added after trial registry but before enrollment of the first patient (March 2012). All amendments were submitted and approved by our institutional REB.
Statistical Analysis
The statistical analyses were performed using SAS version 9.4 (SAS Institute Inc). All tests were two-sided, with p values of < 0.05 considered statistically significant.
Descriptive statistics were used to summarize patient demographics as well as injury and surgical characteristics. Categorical variables are presented as counts. Continuous variables were evaluated for normality using a visual inspection of histograms and the Komolgorov-Smirnov test of normality. Continuous variables with highly skewed distributions are presented as medians and interquartile ranges. Continuous variables with normal distributions are presented as means with SDs. Between-group differences were evaluated using univariate analyses. Categorical variables were assessed using the chi-square or the Fisher exact test where appropriate. Continuous variables were assessed using two-tailed t-tests or the Mann-Whitney U tests where appropriate, based on distribution. Ordinal variables were assessed using the Kruskal-Wallis tests.
Outcomes were evaluated similarly. Categorical variables were assessed using the chi-square or the Fisher exact test where appropriate. Continuous variables were assessed using two-tailed t-tests or Mann-Whitney U tests where appropriate, based on distribution. Ordinal variables were assessed using the Kruskal-Wallis tests.
Results
Timing of Initiation of Rehabilitation and Postoperative Manipulations
With the numbers available, there were no differences between the groups in terms of the proportion of patients who underwent manipulation under anesthesia after the index reconstructive procedure. In the early rehabilitation group, 1 of 18 patients underwent manipulation (6% [95% CI 0% to 27%]) and in the late rehabilitation group, 4 of 18 patients did (22% [95% CI 6% to 48%]; p = 0.34). However, we acknowledge that we were underpowered on the important findings of this study.
Timing of Rehabilitation and Knee Stability
In this small study, there was no difference in knee laxity on physical examination for ACL (early rehabilitation median [range] grading 1 [0 to 1]; late rehabilitation median grading 1 (0 to 2); median difference 0; p = 0.82) and PCL reconstructions (early rehabilitation median grading 1 [0 to 3]; late rehabilitation median grading 1 [0 to 2]; median difference 0; p = 0.96) (Table 2). Likewise, coronal-plane stress radiographs did not demonstrate any difference between the early rehabilitation and late rehabilitation groups in terms of varus stress for lateral-sided injuries (early rehabilitation mean 1 ± 4 mm; late rehabilitation mean 2 ± 3 mm; mean difference -1 mm [95% CI -4 to 2]; p = 0.58) or valgus stress for medial-sided injuries (early rehabilitation mean 0 ± 1 mm; late rehabilitation mean 0 ± 2 mm; mean difference 0 mm [95% CI -2 to 3]; p = 0.93) (Fig. 3). Patient-level stress radiograph data for lateral-sided injuries were reported specifically for clarity (see Table 2; Supplemental Digital Content 2, http://links.lww.com/CORR/A534). We found no differences in total ROM (early rehabilitation mean 130° ± 8°; late rehabilitation mean 129° ± 10°; mean difference 1° [95% CI -5° to 7°]; p = 0.77), flexion deficits (early rehabilitation median 5° [IQR 5° to 10°]; late rehabilitation median 5° [IQR 0° to 10°]; median difference 0°; p = 0.74), or extension deficits (early rehabilitation median 2° [IQR 1° to 5°]; late rehabilitation median 0° [IQR 0° to 2°]; median difference 2°; p = 0.18) between the two groups, compared with the contralateral leg (Table 2). With regard to this secondary outcome, one patient from each group did not undergo an assessment of ROM or stability.
Table 2.
Outcomes of the early rehabilitation and late rehabilitation groups
| Outcome | Early rehabilitation (n = 18) | Late rehabilitation (n = 18) | Difference of medians or mean difference (95% CI) | p value |
| Manipulation | 0.34b | |||
| Yes | 1 | 4 | ||
| No | 17 | 14 | ||
| ACL grade | ||||
| 0 | 6 | 8 | ||
| 1 | 11 | 7 | ||
| 2 | 0 | 2 | 0 (0-0) | 0.82c |
| 3 | 0 | 0 | ||
| 4 | 0 | 0 | ||
| PCL grade | ||||
| 0 | 7 | 7 | ||
| 1 | 7 | 7 | ||
| 2 | 2 | 3 | 0 (-1 to 1) | 0.96c |
| 3 | 1 | 0 | ||
| 4 | 0 | 0 | ||
| ROM in degrees | 130 ± 8 | 129 ± 10 | 1 (-5 to 7) | 0.77d |
| Flexion deficita in degrees | 5 (5-10) | 5 (0-10) | 0 (-5 to 5) | 0.74e |
| Extension deficita in degrees | 2 (1-5) | 0 (0-2) | 2 (0-2) | 0.18e |
| Varus stress radiography (lateral injury)a in millimeters | 1 ± 4 | 2 ± 3 | -1 (-4 to 2) | 0.58d |
| Valgus stress radiography (medial injury)a in millimeters | 0 ± 1 | 0 ± 2 | 0 (-2 to 3) | 0.93d |
| ML-QOL physical impairments | 15.8 (9.2-23.7) | 21.1 (7.9-33.6) | -5.3 (-14.5 to 7.9) | 0.58e |
| ML-QOL emotional impairments | 35.0 (11.7-41.7) | 28.3 (15.0-50.0) | 6.7 (-12.9 to 20.0) | 0.80e |
| ML-QOL activity limitations | 18.8 (8.3-29.2) | 27.1 (16.7-33.3) | -8.3 (-16.7 to 4.2) | 0.24e |
| ML-QOL societal involvement | 20.8 (8.3-25.0) | 22 (16.7-33.3) | -1.2 (-16.7 to 12.5) | 0.46e |
Data presented as mean ± SD or median (IQR).
Compared with contralateral leg.
Fisher exact test.
Kruskal-Wallis test.
t-test.
Mann-Whitney U test.
95% CIs for Kruskal-Wallis and Mann Whitney-U tests generated using Hodges Lehmann estimation.
Fig. 3.
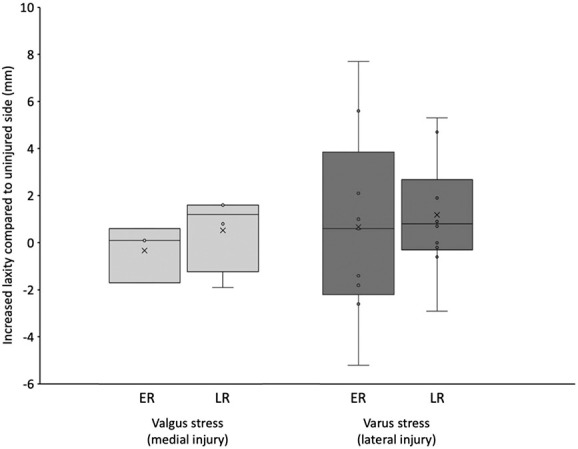
This graph shows an assessment of coronal stability using varus and valgus stress radiographs. Lateral-sided injuries were assessed with varus stress, and medial-sided injuries were assessed with valgus stress. The total distance between the relevant articular surfaces was measured and compared with that of the contralateral, uninjured leg. Radiographs were taken at the 1-year follow-up visit by the primary surgeon. Images were evaluated by a blinded assessor; ER = early rehabilitation; LR = late rehabilitation.
Timing of Rehabilitation and Patient-reported Outcomes (ML-QOL Scores)
At 1 year, there was no difference between the treatment groups with respect to the four ML-QOL domains: physical impairments (early rehabilitation median 16 [IQR 9 to 24]; late rehabilitation median 21 [IQR 8 to 34]; median difference -5; p = 0.58), emotional impairments (early rehabilitation median 35 [IQR 12 to 42]; late rehabilitation median 28 [IQR 15 to 50]; median difference 7; p = 0.80), activity limitations (early rehabilitation median 19 [IQR 8 to 29]; late rehabilitation median 27 [IQR 17 to 33]; median difference -8; p = 0.24), and societal involvement (early rehabilitation median 21 [IQR 8 to 25]; late rehabilitation median 22 [IQR 17 to 33]; median difference -1; p = 0.46), with the numbers available (Fig. 4). One patient from each group did not complete the ML-QOL by the final follow-up visit at 24 months (Table 2).
Fig. 4.
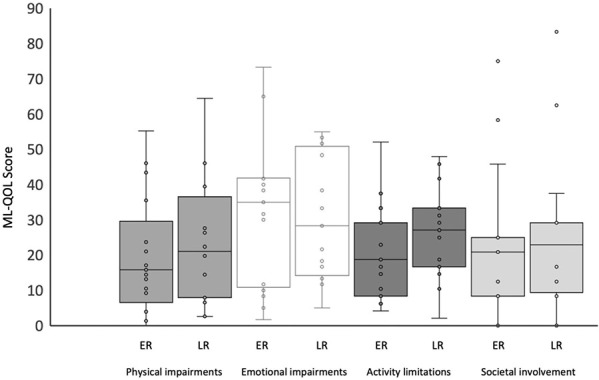
This graph demonstrates that there were no differences between early rehabilitation and late rehabilitation regarding ML-QOL scores; ER = early rehabilitation; LR = late rehabilitation.
Discussion
Rehabilitation after multiligament knee reconstruction for knee dislocation provides significant challenges for both patients and providers, as a balance between postoperative stiffness and laxity is sought to provide optimal function. Both excess stiffness or instability can be substantially disabling and may be influenced by the timing of postoperative physical therapy. We sought to establish whether early rehabilitation or a period of immobilization followed by rehabilitation resulted in improved outcomes after multiligamentous knee reconstruction after dislocation. With the numbers available, our study was unable to demonstrate a difference in the performance of manipulation, knee stability, or patient-reported outcomes between these two approaches. This evidence suggests a potential role for early rehabilitation in this complicated patient population. Following this study, all multiligamentous knee reconstruction patients operated on at our institution are now treated with early physical therapy after surgery.
Limitations
Our study has a number of limitations. Due to challenges in enrolling patients, the study was terminated prematurely, and thus, our findings are potentially subject to Type II error and are underpowered to evaluate our target outcomes. In our findings, there was a proportional difference of 17% when comparing the number of manipulations required between the late rehabilitation group (four) and the early rehabilitation group (one). Based on our sample size of 36 patients, a proportional difference of 47% between groups would have been required to deem the two groups different, with a power of 0.8. However, the similarities between groups in the laxity and ROM findings at 1 year suggest that even with an underpowered small sample, the possibility of late rehabilitation resulting in a clinically important benefit that warrants delaying physiotherapy is less likely. We believe that viewing this study as a pilot study will be helpful in determining the effect size and providing a framework for future trials. A second limitation of our study is the selection of our secondary outcomes after registration of the trial protocol. Our initial registration did not include any intended secondary outcomes, and the endpoints of ROM, clinical and radiographic laxity, and injury-specific patient-reported quality of life were added to the protocol after this due to their importance and relevance to our study question. These were specified in protocol amendments and submitted to our institution’s REB before enrollment of the first patient (March 2012). A further limitation results from the use of unpublished expert opinion survey data for our sample size calculation. This was motivated by a lack of quality evidence at the time of study creation reporting incidence of postoperative arthrofibrosis in knee dislocation patients using modern techniques. If a more accurate calculation could have been performed, the feasibility of reaching our target enrollment may have changed. Accordingly, the results of this pilot study can be used in such a fashion for future trials evaluating knee dislocation patients with our reported postoperative outcomes. The small sample size is also prone to the potential limitations of heterogeneity between the two groups. Although we did not observe baseline differences in age, sex, BMI, injury classification, or method of reconstruction between the rehabilitation groups, it is difficult to say how minor or unmeasured differences between these groups could have affected the outcome in a small sample size. Our use of autograft in most reconstructions may impact the generalizability of these results to all-allograft multiligament reconstructions, which could have a different propensity for developing postoperative arthrofibrosis, though this has not been evident in the evidence [7, 44]. Furthermore, the conclusions of this study might be limited by the follow-up duration because stress radiographs and patient-reported outcomes were collected at 1 year postoperatively. Although these short-term results provide value, recovery from multiligament knee reconstruction is a lengthy process, and future studies with longer-term follow-up will help strengthen our conclusions and inform treatment.
Given the rare nature of this injury [34], a trial of adequate power would likely require a multicenter, possibly even international, design. To date, no such study has been conducted in patients with multiligament knee injuries, although the STaR Trial examining early and delayed surgery is ongoing and may provide insights into the best treatment of these patients (clinicaltrials.gov: NCT03543098).
Timing of Initiation of Rehabilitation and Postoperative Manipulations
With the numbers available, there was no difference in the primary outcome of this study—the need for manipulation—between early and late rehabilitation groups. Previously, recommendations for rehabilitation after multiligament knee reconstruction included immobilizing the knee in full extension from 4 weeks to 12 weeks postoperatively to protect the reconstruction [21, 40]. The motivation for this delay may have come in part from a lack of confidence in fixation techniques, graft size and structure, nonanatomic surgical reconstructions, and the desire to have repaired and/or reconstructed tendons provisionally heal before stressing the construct [40]. In the current era of allograft use [38, 51], as well as with the evolution of anatomic reconstruction techniques, fixation devices, and an improved understanding of ligamentous healing [6], we suggest that many of these concerns have been addressed. Therefore, we believe early initiation of physical therapy can be explored in an effort to reduce postoperative stiffness and improve outcomes. This suggestion mirrors the evolution of other postoperative knee protocols, such as in TKA and ACL reconstruction, which have progressively moved toward early rehabilitation with mounting evidence for reduction in stiffness and improved outcomes [2, 8, 45]. The less than 6% rate of manipulation and a mean ROM arc of 130° in our early rehabilitation group is encouraging. Our study, though small, provides a first step in establishing evidence for early rehabilitation after multiligament knee reconstruction.
Timing of Rehabilitation and Knee Stability
Despite challenges in obtaining an adequate sample size and a resultant small study population, important secondary findings related to stability are to be highlighted. In our study, early rehabilitation did not lead to worsened laxity in either the sagittal or coronal planes, which is thought to be the primary concern related to early initiation of physical therapy in these patients [28]. However, even though the measured laxity on varus stress radiographs for lateral-sided injuries did not differ substantially in measures of central tendency between groups, the range of values in the early rehabilitation group was large (-5 to 8 mm). Although this could be viewed as concerning for instability, the early and late rehabilitation groups both had three patients with more than 2 mm of increased laxity and two patients with more than 4 mm of increased laxity on stress radiographs. Thus, the lack of difference in coronal laxity between the early and late rehabilitation groups, particularly in those with medial-sided injuries, is also reassuring to practitioners who wish to implement early rehabilitation protocols in this high-risk group. This assertion is further strengthened by the results of a meta-analysis by Mook et al. [33], which pooled knee dislocation patients from observational studies with varied postoperative protocols and demonstrated a reduction in coronal laxity among those treated with early rehabilitation. Taken together, this evidence tends to refute the notion that early initiation of physical therapy after multiligament knee reconstruction results in laxity. However, further research with larger prospective studies is required to determine whether early rehabilitation could improve stability, as suggested by Mook et al. [33].
Timing of Rehabilitation and Patient-reported Outcomes (ML-QOL Score)
In our small study, at 1 year after surgery, we found no difference between early and late rehabilitation groups in any of the four ML-QOL domains (physical impairments, emotional impairments, activity limitations, and societal involvement). Similar to our other outcomes, this study was likely underpowered to accurately evaluate differences between ML-QOL scores of the two treatment groups. Despite this, our findings are consistent with a previous study comparing pooled patient-reported outcomes across studies with either early or late rehabilitation protocols after multiligament reconstruction, which also found no difference between groups [33]. However, previous orthopaedic studies have demonstrated improved patient-reported outcomes with early initiation of physical therapy in total joint arthroplasty [17], ankle ligament reconstruction [50], and meniscal repair [10]. Further prospective studies examining the factors that affect patient quality of life after multiligament knee injury, including postoperative rehabilitation protocols, are needed.
Conclusion
With the numbers available in this study, we were unable to demonstrate a difference between early and late knee rehabilitation with regard to knee stiffness, laxity, or patient-reported quality of life outcomes. The results of this small, randomized pilot study suggest a potential role for early rehabilitation after multiligament reconstruction for knee dislocation, which should be further explored in larger multiinstitutional studies.
Supplementary Material
Acknowledgments
We thank Dr. Aaron Nauth MD, MSc, FRCSC, who contributed two surgical procedures to the study.
Footnotes
The institution of one or more of the authors (DBW) has received, during the study period, funding from Physicians’ Services Incorporated Foundation.
Each author certifies that neither he nor she, nor any member of his or her immediate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Ethical approval for this study was obtained from St. Michael’s Hospital, Toronto, ON, Canada (approval number 10-0382). The trial was registered at Clinicaltrials.gov with the identifier NCT01296750.
This work was performed at St. Michael’s Hospital, Toronto, ON, Canada.
Contributor Information
Matthew Rubacha, Email: mattrubacha@gmail.com.
Jaskarndip Chahal, Email: jchahal@utosm.com.
Ryan Khan, Email: ryan.khan@unityhealth.to.
Bheeshma Ravi, Email: bheeshma.ravi@sunnybrook.ca.
Daniel B. Whelan, Email: daniel.whelan@unityhealth.to.
References
- 1.Barrett IJ, Krych AJ, Pareek A, et al. Short- to mid-term outcomes of anatomic MCL reconstruction with Achilles tendon allograft after multiligament knee injury. Knee Surg Sports Traumatol Arthrosc. 2018;26:2952-2959. [DOI] [PubMed] [Google Scholar]
- 2.Beynnon BD, Johnson RJ, Abate JA, Fleming BC, Nichols CE. Treatment of anterior cruciate ligament injuries, part 2. Am J Sports Med. 2005;33:1751-1767. [DOI] [PubMed] [Google Scholar]
- 3.Billieres J, Labruyere C, Steltzlen C, et al. Multiligament knee injuries treated by one-stage reconstruction using allograft: postoperative laxity assessment using stress radiography and clinical outcomes. Orthop Traumatol Surg Res. 2020;106:937-944. [DOI] [PubMed] [Google Scholar]
- 4.Bodendorfer BM, Keeling LE, Michaelson EM, et al. Predictors of knee arthrofibrosis and outcomes after arthroscopic lysis of adhesions following ligamentous reconstruction: a retrospective case-control study with over two years' average follow-up. J Knee Surg. 2019;32:536-543. [DOI] [PubMed] [Google Scholar]
- 5.Chahal J, Whelan DB, Jaglal SB, et al. The multiligament quality of life questionnaire: development and evaluation of test-retest reliability and validity in patients with multiligament knee injuries. Am J Sports Med. 2014;42:2906-2916. [DOI] [PubMed] [Google Scholar]
- 6.Chahla J, Nitri M, Civitarese D, Dean CS, Moulton SG, LaPrade RF. Anatomic double-bundle posterior cruciate ligament reconstruction. Arthrosc Tech. 2016;5:e149-156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cook S, Ridley TJ, McCarthy MA, et al. Surgical treatment of multiligament knee injuries. Knee Surg Sports Traumatol Arthrosc. 2015;23:2983-2991. [DOI] [PubMed] [Google Scholar]
- 8.den Hertog A, Gliesche K, Timm J, Muhlbauer B, Zebrowski S. Pathway-controlled fast-track rehabilitation after total knee arthroplasty: a randomized prospective clinical study evaluating the recovery pattern, drug consumption, and length of stay. Arch Orthop Trauma Surg. 2012;132:1153-1163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Desai VS, Wu IT, Camp CL, Levy BA, Stuart MJ, Krych AJ. Midterm outcomes following acute repair of grade III distal MCL avulsions in multiligamentous knee injuries. J Knee Surg. 2020;33:785-791. [DOI] [PubMed] [Google Scholar]
- 10.Dias JM, Mazuquin BF, Mostagi FQ, et al. The effectiveness of postoperative physical therapy treatment in patients who have undergone arthroscopic partial meniscectomy: systematic review with meta-analysis. J Orthop Sports Phys Ther. 2013;43:560-576. [DOI] [PubMed] [Google Scholar]
- 11.Edson CJ. Conservative and postoperative rehabilitation of isolated and combined injuries of the medial collateral ligament. Sports Med Arthrosc Rev. 2006;14:105-110. [DOI] [PubMed] [Google Scholar]
- 12.Edson CJ, Fanelli GC, Beck JD. Rehabilitation after multiple-ligament reconstruction of the knee. Sports Med Arthrosc Rev. 2011;19:162-166. [DOI] [PubMed] [Google Scholar]
- 13.Fanelli GC. Posterior cruciate ligament rehabilitation: how slow should we go? Arthroscopy. 2008;24:234-235. [DOI] [PubMed] [Google Scholar]
- 14.Fanelli GC, Beck JD, Edson CJ. Combined PCL-ACL lateral and medial side injuries: treatment and results. Sports Med Arthrosc Rev. 2011;19:120-130. [DOI] [PubMed] [Google Scholar]
- 15.Fanelli GC, Edson CJ. Surgical treatment of combined PCL-ACL medial and lateral side injuries (global laxity): surgical technique and 2- to 18-year results. J Knee Surg. 2012;25:307-316. [DOI] [PubMed] [Google Scholar]
- 16.Geeslin AG, Moulton SG, LaPrade RF. A systematic review of the outcomes of posterolateral corner knee injuries, part 1: surgical treatment of acute injuries. Am J Sports Med. 2016;44:1336-1342. [DOI] [PubMed] [Google Scholar]
- 17.Haas R, Sarkies M, Bowles KA, O'Brien L, Haines T. Early commencement of physical therapy in the acute phase following elective lower limb arthroplasty produces favorable outcomes: a systematic review and meta-analysis examining allied health service models. Osteoarthritis Cartilage. 2016;24:1667-1681. [DOI] [PubMed] [Google Scholar]
- 18.Harner CD, Waltrip RL, Bennett CH, Francis KA, Cole B, Irrgang JJ. Surgical management of knee dislocations. J Bone Joint Surg Am. 2004;86:262-273. [DOI] [PubMed] [Google Scholar]
- 19.Hegyes MS, Richardson MW, Miller MD. Knee dislocation. Complications of nonoperative and operative management. Clin Sports Med. 2000;19:519-543. [DOI] [PubMed] [Google Scholar]
- 20.Hunter RE, Mastrangelo J, Freeman JR, Purnell ML, Jones RH. The impact of surgical timing on postoperative motion and stability following anterior cruciate ligament reconstruction. Arthroscopy. 1996;12:667-674. [DOI] [PubMed] [Google Scholar]
- 21.Irrgang JJ, Fitzgerald GK. Rehabilitation of the multiple-ligament-injured knee. Clin Sports Med. 2000;19:545-571. [DOI] [PubMed] [Google Scholar]
- 22.Jiang W, Yao J, He Y, Sun W, Huang Y, Kong D. The timing of surgical treatment of knee dislocations: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2015;23:3108-3113. [DOI] [PubMed] [Google Scholar]
- 23.Laprade RF, Bernhardson AS, Griffith CJ, Macalena JA, Wijdicks CA. Correlation of valgus stress radiographs with medial knee ligament injuries: an in vitro biomechanical study. Am J Sports Med. 2010;38:330-338. [DOI] [PubMed] [Google Scholar]
- 24.LaPrade RF, Heikes C, Bakker AJ, Jakobsen RB. The reproducibility and repeatability of varus stress radiographs in the assessment of isolated fibular collateral ligament and grade-III posterolateral knee injuries. An in vitro biomechanical study. J Bone Joint Surg Am. 2008;90:2069-2076. [DOI] [PubMed] [Google Scholar]
- 25.Levy BA, Dajani KA, Morgan JA, Shah JP, Dahm DL, Stuart MJ. Repair versus reconstruction of the fibular collateral ligament and posterolateral corner in the multiligament-injured knee. Am J Sports Med. 2010;38:804-809. [DOI] [PubMed] [Google Scholar]
- 26.Levy BA, Dajani KA, Whelan DB, et al. Decision making in the multiligament-injured knee: an evidence-based systematic review. Arthroscopy. 2009;25:430-438. [DOI] [PubMed] [Google Scholar]
- 27.Levy BA, Fanelli GC, Whelan DB, et al. Controversies in the treatment of knee dislocations and multiligament reconstruction. J Am Acad Orthop Surg. 2009;17:197-206. [DOI] [PubMed] [Google Scholar]
- 28.Lynch AD, Chmielewski T, Bailey L, et al. Current concepts and controversies in rehabilitation after surgery for multiple ligament knee injury. Curr Rev Musculoskelet Med. 2017;10:328-345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Manske RC, Hosseinzadeh P, Giangarra CE. Multiple ligament knee injury: complications. N Am J Sports Phys Ther. 2008;3:226-233. [PMC free article] [PubMed] [Google Scholar]
- 30.Mariani PP, Santoriello P, Iannone S, Condello V, Adriani E. Comparison of surgical treatments for knee dislocation. Am J Knee Surg. 1999;12:214-221. [PubMed] [Google Scholar]
- 31.McDonald LS, Waltz RA, Carney JR, et al. Validation of varus stress radiographs for anterior cruciate ligament and posterolateral corner knee injuries: a biomechanical study. Knee. 2016;23:1064-1068. [DOI] [PubMed] [Google Scholar]
- 32.Medvecky MJ, Zazulak BT, Hewett TE. A multidisciplinary approach to the evaluation, reconstruction and rehabilitation of the multi-ligament injured athlete. Sports Med. 2007;37:169-187. [DOI] [PubMed] [Google Scholar]
- 33.Mook WR, Miller MD, Diduch DR, Hertel J, Boachie-Adjei Y, Hart JM. Multiple-ligament knee injuries: a systematic review of the timing of operative intervention and postoperative rehabilitation. J Bone Joint Surg Am. 2009;91:2946-2957. [DOI] [PubMed] [Google Scholar]
- 34.Nielsen AB, Yde J. Epidemiology of acute knee injuries: a prospective hospital investigation. J Trauma. 1991;31:1644-1648. [DOI] [PubMed] [Google Scholar]
- 35.Noyes FR, Barber-Westin SD. Reconstruction of the anterior and posterior cruciate ligaments after knee dislocation. Use of early protected postoperative motion to decrease arthrofibrosis. Am J Sports Med. 1997;25:769-778. [DOI] [PubMed] [Google Scholar]
- 36.Ogata K, McCarthy JA. Measurements of length and tension patterns during reconstruction of the posterior cruciate ligament. Am J Sports Med. 1992;20:351-355. [DOI] [PubMed] [Google Scholar]
- 37.Peskun CJ, Whelan DB. Outcomes of operative and nonoperative treatment of multiligament knee injuries: an evidence-based review. Sports Med Arthrosc Rev. 2011;19:167-173. [DOI] [PubMed] [Google Scholar]
- 38.Petre BM, Smith SD, Jansson KS, et al. Femoral cortical suspension devices for soft tissue anterior cruciate ligament reconstruction: a comparative biomechanical study. Am J Sports Med. 2013;41:416-422. [DOI] [PubMed] [Google Scholar]
- 39.Richter M, Bosch U, Wippermann B, Hofmann A, Krettek C. Comparison of surgical repair or reconstruction of the cruciate ligaments versus nonsurgical treatment in patients with traumatic knee dislocations. Am J Sports Med. 2002;30:718-727. [DOI] [PubMed] [Google Scholar]
- 40.Rodeo SA, Arnoczky SP, Torzilli PA, Hidaka C, Warren RF. Tendon-healing in a bone tunnel. A biomechanical and histological study in the dog. J Bone Joint Surg Am. 1993;75:1795-1803. [DOI] [PubMed] [Google Scholar]
- 41.Saini P, Trikha V. Manipulation under anesthesia for post traumatic stiff knee-pearls, pitfalls and risk factors for failure. Injury. 2016;47:2315-2319. [DOI] [PubMed] [Google Scholar]
- 42.Schenck RC., Jr. The dislocated knee. Instr Course Lect. 1994;43:127-136. [PubMed] [Google Scholar]
- 43.Serra Cruz R, Mitchell JJ, Dean CS, Chahla J, Moatshe G, LaPrade RF. Anatomic posterolateral corner reconstruction. Arthrosc Tech. 2016;5:e563-572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shapiro MS, Freedman EL. Allograft reconstruction of the anterior and posterior cruciate ligaments after traumatic knee dislocation. Am J Sports Med. 1995;23:580-587. [DOI] [PubMed] [Google Scholar]
- 45.Shaw T. Accelerated rehabilitation following anterior cruciate ligament reconstruction. Phys Ther Sport. 2002;3:19-26. [Google Scholar]
- 46.Shelbourne KD, Nitz P. Accelerated rehabilitation after anterior cruciate ligament reconstruction. Am J Sports Med. 1990;18:292-299. [DOI] [PubMed] [Google Scholar]
- 47.Sheth U, Sniderman J, Whelan DB. Early surgery of multiligament knee injuries may yield better results than delayed surgery: a systematic review. Journal of ISAKOS. 2019;4:26-32. [Google Scholar]
- 48.Sisto DJ, Warren RF. Complete knee dislocation. A follow-up study of operative treatment. Clin Orthop Relat Res. 1985;198:94-101. [PubMed] [Google Scholar]
- 49.Skendzel JG, Sekiya JK, Wojtys EM. Diagnosis and management of the multiligament-injured knee. J Orthop Sports Phys Ther. 2012;42:234-242. [DOI] [PubMed] [Google Scholar]
- 50.Vopat ML, Tarakemeh A, Morris B, et al. Early versus delayed mobilization postoperative protocols for lateral ankle ligament repair: a systematic review and meta-analysis. Orthop J Sports Med. 2020;8:2325967120925256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Walsh MP, Wijdicks CA, Parker JB, Hapa O, LaPrade RF. A comparison between a retrograde interference screw, suture button, and combined fixation on the tibial side in an all-inside anterior cruciate ligament reconstruction: a biomechanical study in a porcine model. Am J Sports Med. 2009;37:160-167. [DOI] [PubMed] [Google Scholar]
- 52.Werier Keating JF, Meek RN. Complete dislocation of the knee - the long-term results of ligamentous reconstruction. Knee. 1998;5:255-260. [Google Scholar]
- 53.Whelan D, Leiter J, Sasyniuk T, et al. Double-row repair of the distal attachment of the superficial medial collateral ligament: a basic science pilot study. Knee Surg Sports Traumatol Arthrosc. 2015;23:2820-2824. [DOI] [PubMed] [Google Scholar]
- 54.Wong CH, Tan JL, Chang HC, Khin LW, Low CO. Knee dislocations-a retrospective study comparing operative versus closed immobilization treatment outcomes. Knee Surg Sports Traumatol Arthrosc. 2004;12:540-544. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.