Abstract
The COVID-19 pandemic has imposed extraordinary and unpredictable changes on our lifestyle for an unknown duration. Consequently, core aspects of wellbeing including behavior, emotion, cognition, and social interactions are negatively affected. Sleep and circadian rhythms, with an extensive impact on physiology, behavior, emotion, and cognition are affected too. We provided an updated overview of the impact of the COVID-19 pandemic on circadian rhythms and sleep based on the results of published studies (n = 48) in three sections. First, we focus on circadian misalignment due to the pandemic in the general population (including shift workers, health staff, students) and COVID-19 patients and summarize the most critically contributing factors to circadian misalignment. Next, we address sleep difficulties and poor sleep quality during the pandemic, their contributing factors, rate and prevalence, and their effects on both the general population and COVID-19 patients. Finally, we summarize the currently applied/recommended interventions for aligning circadian rhythms and improving sleep quality in both, the general population, and COVID-19 patients during the pandemic situation. Briefly, circadian misalignment and sleep difficulties are common consequences of the pandemic in the general population (with elderly, students, children, health and night-work shifters as risk groups) and COVID-19 patients. Home confinement and its physiological, circadian, and psychological derivates are central to these difficulties. Symptoms severity, treatment progress, recovery duration, and even diagnosis of COVID-19 patients are considerably affected by circadian and sleep difficulties. Behavioral interventions for normalizing the factors that contribute to circadian and sleep difficulties are helpful.
Keywords: COVID-19, Sleep, Circadian disturbance, Home confinement, Brain, Cognition
1. Introduction
Known as the “once-in-a-century” pandemic [1], the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was first identified in December 2019 in Wuhan, China, leading to the COVID-19 disease. Since then, the disease has rapidly spread throughout the world afflicting more than 175,000,000 confirmed cases and more than 3,770,000 confirmed deaths worldwide to date (WHO: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 as of June 12th, 2021). The consequences of this extraordinary pandemic were not, however, limited to the disease-specific respiratory symptoms [2]. A full picture of the underlying mechanisms and immediate and late side effects is not completely understood yet. Serious consequences affect not only infected and recovered patients, but also the general population under the current pandemic. Lifestyle and mental health disruptions [3], neuropsychiatric disturbances [4], social isolation [5], emotional difficulties [6], behavioral problems [7,8], and cognitive deficits [9,10], are some of the consequences of the pandemic, affecting major aspects of our life as human beings (ie, mental, social, emotional, behavioral and cognitive).
A major consequence of the COVID-19 crisis is its effect on the sleep–wake cycle through lifestyle changes due to the pandemic [3,11]. Sleep is a ubiquitous physiological phenomenon with a huge, pervasive, and cyclical impact on our basic physiological processes (eg, metabolism, immune system), behavior, cognition, and emotion. Accordingly, any disruption of the sleep–wake cycle will have not only multifaceted acute but also long-term effects, depending on the duration of exposure. In this chapter organized in a semi-systematic review, we focus on how sleep and circadian rhythms, two interacting but also independent factors, are affected by the COVID-19 pandemic in infected patients and the general population, whose lifestyle has undergone unexpected changes. We aim to provide an updated overview of the COVID-19 impact on circadian rhythms and sleep quality based on findings reported by verified and reliable research articles. This is an important point to consider as there have been concerns over the methodological quality and validity of reported findings/perspectives related to the pandemic [12,13].
Before we discuss COVID-19 effects on circadian misalignment and sleep, we briefly describe their pervasive role in human brain functions, and cognition (as foundations for successful behavior and daily life performance), general health, and psychiatric disorders. This will allow us to better understand how circadian and sleep disruptions due to the COVID-19 pandemic can lead to their negative consequences.
2. Impact of sleep and circadian rhythms on brain and cognition, health and psychopathology
2.1. Brain physiology and cognition
Circadian rhythms and sleep–wake cycle are two closely interactive physiological phenomena. A well-known model for explaining the interaction of the circadian timing system (process C) and sleep–wake cycle (process S) is the “Two Process Model of Sleep Regulation” [14]. According to this model, the sleep–wake cycle (process S) increases during wakefulness, declines during sleep and this is entrained to day and night by the circadian pacemaker (process C) [15]. These two processes have extensive impacts on brain physiology and cognition [16,17] and are thus critical for adaptive behavior. The dependence of synaptic plasticity in the central nervous system [18], hippocampal long-term potentiation (LTP) [19], and structural synaptic plasticity [20] from circadian rhythms has been documented in previous animal studies. In humans, recent studies have also shown that cortical excitability and neuroplasticity in the brain are dependent on circadian rhythms and sleep [16,17,21,22]. In this line, negative effects of sleep difficulties on human cognition are well-documented [[23], [24], [25]]. Any disruption in the sleep–wake cycle and circadian rhythms affects cognitive abilities such as learning, memory, and attention [16,26] which are important for our daily normal functioning including job and academic performance [27,28].
2.2. Health and neuropsychiatric diseases
Circadian rhythms can be entrained or phase-shifted not only by our internal clock, but also external factors including social stimuli, auditory stimuli, exercise, and daily schedules or social rhythms. These triggers can disrupt social zeitgebers (external cues that function to entrain biological rhythms) which, in turn, derail biological rhythms [29]. In addition to being a risk factor for disease in the general and clinical populations (physical, psychiatric) [30], slight drifts from the circadian rhythm are associated with suboptimal functioning at behavioral and cognitive levels in healthy populations affecting our overall daily performance [31]. Circadian misalignment is proposed for explaining several clinical conditions, such as depression, bipolar, schizophrenia, and attention-deficit hyperactivity disorders as well [29,30,32]. In bipolar spectrum disorders for example, life events that disrupt social zeitgebers, can precipitate bipolar symptoms because they disturb circadian rhythms. In this line, it is shown that lockdown could expose patients with bipolar disorder to depressive relapse through dysregulation of biological rhythms [33]. With respect to the COVID-19 pandemic, which is a relevant modulator of circadian rhythms due to alterations of social zeitgebers caused by lockdowns, studies with a large number of participants have shown an increase in the prevalence of not only sleep-related disorders but also psychological and neuropsychiatric disorders in the general and clinical populations since the beginning of the outbreak [34,35].
3. Methods
3.1. Eligibility criteria, information source, and search strategy
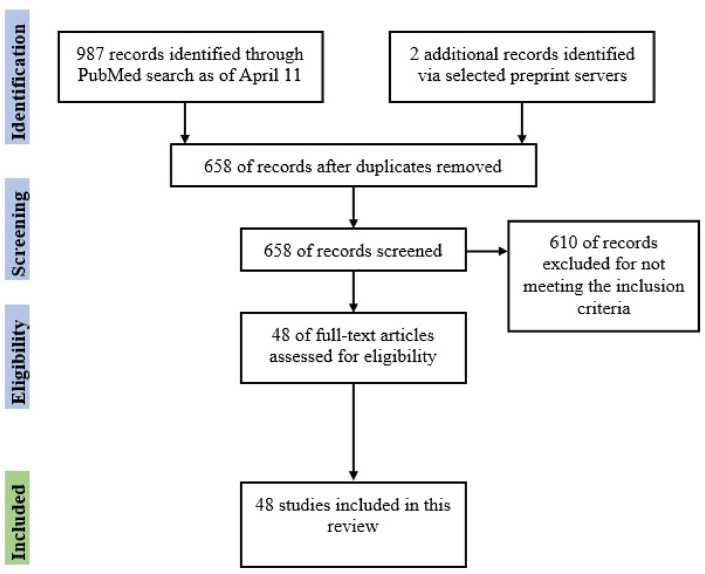
We aim to provide a comprehensive overview of the published literature on the COVID-19 impact on circadian rhythms and sleep difficulties. Inclusion criteria were peer-reviewed studies that are (1) published in English (2) in the PubMed database (3) and investigated sleep and/or circadian rhythms changes/difficulties in humans (4) during the COVID-19 pandemic (5). A search was conducted using the PubMed database with the final search updated on April 11th, 2021. Search terms included “COVID-19” OR “COVID-19 pandemic” AND “Circadian rhythms” OR “Circadian Misalignment” OR “Circadian Disorders” OR “Sleep Problems” OR “Sleep difficulties” OR “Sleep Quality”. The search was limited to journal articles written in English published between January 2020 up to April 2021. The search terms generated a total of 987 studies (88 + 5+83 + 103+261 + 447). Two reviewers (MAS & AA) screened the titles from the initial search, removed the duplicates and subsequently screened the abstracts to identify potential articles. After the initial title and abstract screen, duplicates were removed, and 48 studies were included in this review. We additionally checked medRxiv and the Lancet preprint servers for potentially relevant articles. The inclusion procedure is displayed in Fig. 1 . We also searched for the interventions applied or suggested in the included studies.
Fig. 1.
Flow diagram of included studies investigating the impact of COVID-19 pandemic on circadian rhythms difficulties and sleep problems.
3.2. Outcome variables
Variables related to sleep quality factors (eg, sleep time, awakening time, time to go to bed, time to get-up) and quality factors were the main outcome variables (using the Pittsburgh Sleep Quality Index). Sleep disorders (eg, insomnia, sleep apnea, narcolepsy, restless legs syndrome, nightmare), disorders of circadian rhythms, and mental health-related factors were among the outcome variables as well.
4. COVID-19 and circadian disturbances
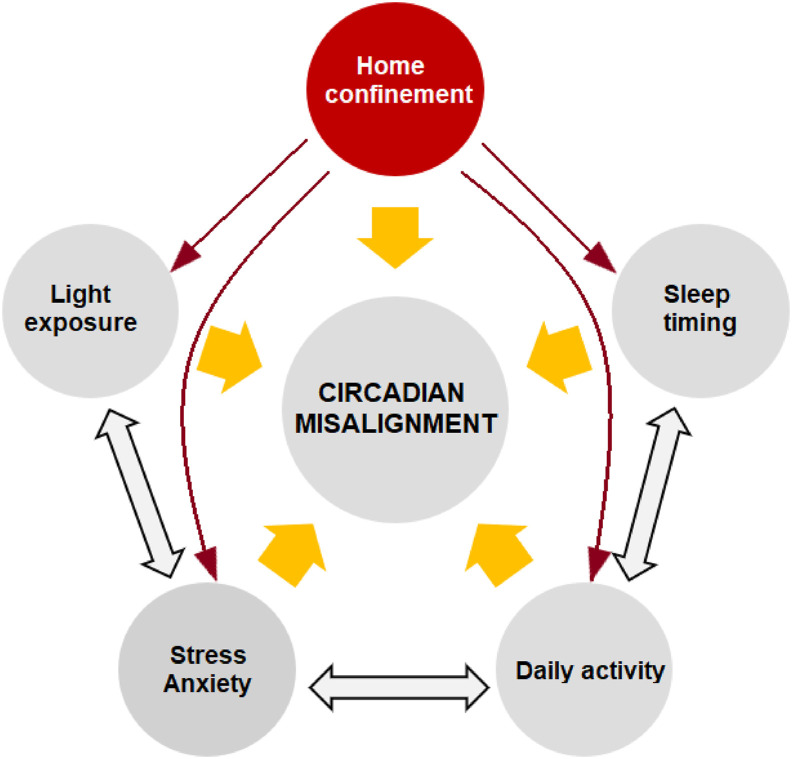
Circadian rhythms have a central role in coordinating daily physiological processes, including not only brain functions, but also the functions of innate and adaptive immunity, and thus have a profound impact on human health [36]. One major consequence of the COVID-19 pandemic has been home confinement/quarantine, which led to dramatic changes in the level of activity during daytime. This also affects exposure to light, which is a major pacemaker of circadian rhythms. As a result, circadian rhythms can deviate from their optimal pattern, which is known as “circadian misalignment”. The major factors contributing to circadian misalignment due to the COVID-19 pandemic based on the results of the included studies are displayed in Fig. 2 .
Fig. 2.
COVID-19 related contributors to circadian misalignment. Home confinement or quarantine due to COVID-19 is a central contributing factor with an impact on other factors.
These factors include changes in sleep timing and daily activity, limited exposure to light, and delayed chronotype (delay in the sleep–wake cycle) mostly caused by home confinement [[37], [38], [39]], and also increased levels of stress and anxiety over the current pandemic. An investigation of 3787 individuals who were in home confinement for an average of 65 days during the outbreak shows that around 67% of them shifted toward eveningness (evening person) at behavioral level during home confinement [40] which indicates a circadian misalignment. The problematic aspect here is that circadian misalignment has negative effects on not only general aspects of health but also on brain functions and cognition which are required for successful daytime performance. In what follows, we limit this discussion to health-related and sleep-related aspects of circadian misalignment.
4.1. Circadian misalignment and health
Many immune parameters oscillate rhythmically with the time of day, and thus the circadian clock is an important gatekeeper for reducing immunity-associated costs such as pathogens and noxious stimuli [41,42]. These immune system-related oscillations can be altered by an even short and transient shift of circadian rhythms [43]. Any disruption of the circadian rhythm and thereby immune cycle, due to intrinsic or extrinsic factors (eg, the current pandemic situation) can result in disorders of circadian function and/or alterations of regulation of waking adaptive behaviors [44]. Due to such pervasive impact, circadian misalignment can negatively affect hormonal, neurological, cognitive, and behavioral pathways and accordingly affect different aspects of health [30].
Additionally, circadian misalignment is a specific risk factor for viral diseases, including the COVID-19 disease. Emerging evidence suggests that people with a disrupted circadian clock owing to old age, working night shifts, jet lag or irregular sleeping and eating habits have a less vigorous immune system and thereby are more susceptible to viral respiratory diseases [36,45]. In this line, a recently published study shows that shift workers, particularly night shift workers that suffer from circadian misalignment, are at high risk of COVID-19 infection irrespective of their occupational group and based on data from UK Biobank participants who were tested for COVID-19 infection [46]. Furthermore, humans are more susceptible to infections at certain times of the day, because the immune system functionality follows a daily rhythmic pattern [41]. The COVID-19 disease, as a viral disease, is thus similarly affected. It is argued that infection severity of the COVID-19 disease is regulated by the circadian clock [36]. At the physiological level, different aspects of the disease process—from infection to pathology— are associated with circadian rhythmicity. This means that a misaligned circadian clock can intensify or prolong disease duration and the recovery process, while an undisturbed circadian clock can mitigate disease expression and the clinical course of COVID-19 [47].
In addition to infected patients, the general population will suffer from the consequence of circadian misalignment too. A nationwide school-based survey in 11,787 university students shows that circadian rhythm abnormalities caused by home quarantine affected up to 28% of participants and importantly, the prevalence of depression and anxiety were significantly higher in those with circadian rhythm abnormality [48]. Moreover, a dose–response relationship was found between the severity of circadian rhythm abnormality and psychological problems. Another international survey conducted on 11,431 adults from 40 countries showed that social restrictions due to the COVID-19 significantly changed the sleep–wake cycle and circadian alignment [49]. The health-related consequences of circadian misalignment can be severe in certain groups. Night shift workers [46,50], elderly [51], school and university students [48], and children [52] appear to be high-risk groups for circadian misalignment, though a respective risk applies for the general population [11,49]. This highlights the need for home-based interventions for the general population, and also hospital-based interventions for infected patients for re-aligning circadian rhythms, which will be discussed in the last section in some detail. A summary of the impact of circadian misalignment on the general population and patients and potential treatment approaches is in Table 1 .
Table 1.
The impact of circadian misalignment and sleep difficulties due to the COVID-19 pandemic on the general population and COVID infected patients and proposed interventions.
| Risk group | impact |
intervention |
|||
|---|---|---|---|---|---|
| COVID-19 patients | General population | COVID-19 patients | General population | ||
| Circadian misalignment | Elderly [53] | symptom severity [36] | sleep timing difficulties [38] | melatonin administration [47] | keeping regular sleep timing [37] |
| Night shift workers [46,50] | oscillation of immune components [47] | sleep habit changes [40] | chronopharmacology [47] | exposure to natural daylight [37,38] | |
| Students/youth [39,48] | medication efficacy [36] | regular exercise preferably in daytime [37] | |||
| Health care workers [54] | duration prolongation [36,47] | delaying sleep time in schoolers [55] | |||
| Sleep difficulties | COVID-19 patients [36] | duration prolongation [36,47] | higher rate of sleep disorders [[56], [57], [58], [59]] | progressive muscle relaxation [60] | CBT-I behavioral recommendations [37] |
| Health care workers [54,61] | delayed recovery [47,62] | anxiety and depression [4,63,64] | treatment time based on patients' internal clock [47] | regular daytime napping [65] | |
| Children/infants [52] | higher rate of depressed mood [66] | learning and working efficacy [65] | mindfulness techniques for child caregivers [52] | ||
| Students [67,68] | diagnosis [62] | cognitive decline [10,53] | |||
4.2. Circadian misalignment and sleep
One specific area that is bidirectionally affected by circadian misalignment is sleep, because of the prominent role of circadian rhythms in the sleep–wake cycle timing [69]. Accordingly, the need to sleep, time to sleep, and duration of sleep are closely related to circadian rhythms. In case of circadian misalignment, sleep onset and offset time and its duration are shifted from the normal cycle. In this line, it was shown that during the lockdown, circadian rhythms and chronotype, (ie, preference for earlier or later sleep onset/offset time) were delayed, and sleep duration was also decreased [39]. Another survey conducted in Italy indicated that sleep timing (time to go to bed and wake up) was significantly longer during the lockdown [70], a sign of circadian misalignment. Another study report longer sleep duration during home quarantine, and importantly this applied for people with early (ie, morning types) and late chronotype (evening types) [11]. Similarly, prolonged stays at home (>65 days) due to lookdown, shifted chronotype toward eveningness, which means a tendency for a later going to bedtime and delayed wake-up time [40]. This was associated with a change of sleep habits which is indicative of sleep rhythm misalignment.
In addition to the stress and anxiety related to COVID-19, there are at least two major factors that contribute to increased sleep disturbances during the pandemic due to circadian misalignment: changes of daily routines and daily light exposure [38] which also affects the level of melatonin release, a hormone playing a key role in inducing sleepiness. Alterations of daily routines such as arising at a specific time, showing up at work, eating, exercising, and engaging in social/leisure activities are important timekeepers for our sleep–wake cycles and are synchronized with day (light) and night (dark) cycles. In the next section, we focus on sleep difficulties due to the COVID-19 crisis with more details.
5. COVID-19 and sleep difficulties
So far, we discussed how the COVID-19 pandemic led to circadian misalignment which in turn can result in health-related consequences and sleep difficulties. In this section, we specifically focus on sleep quality and how it is affected during the pandemic. The sleep difficulties addressed in the previous section involved quantitative factors (sleep onset/offset time, duration) related to circadian misalignment. Sleep quality can be affected by sleep timing and duration but includes other factors too such as sleep efficiency, subjective quality of sleep or daily disturbances due to poor sleep. Overall, studies have documented a strong negative impact of the COVID-19 pandemic on sleep quality in both infected patients and the general population. Different aspects related to the COVID-19 pandemic are suggested to be responsible for poor sleep quality according to the studies included in this review. These factors are summarized in Fig. 3 . The impact of the COVID-19 pandemic on sleep is also summarized in Table 1. In what follows, we summarize the currently available findings of sleep problems reported in the general population and patients with COVID-19.
Fig. 3.
COVID-19 related factors contributing to poor sleep. Based on the reported studies, there are at least 6 major factors that are bidirectionally related to poor sleep: home confinement/quarantine [11,37], lifestyle disruption [3,38], daylight exposure and melatonin level [37,38], circadian misalignment and delayed chronotype [11,39], emotion dysregulation [37,63,64], and increased levels of stress and anxiety with respect to disease vulnerability itself, but also financial, occupational and social consequences of the COVID-19 crisis [71,72]. Note: The factors contributing to poor sleep quality are not limited to those mentioned here.
5.1. Sleep difficulties rate during COVID-19 pandemic
A recent review and metanalysis of published studies showed that the prevalence rate of sleep problems among the general population in the pandemic was 35.7%, and patients with COVID-19 were the most affected group, with a pooled rate of 74.8% [73]. According to this review, health care workers and the general population had comparable rates of sleep problems, with rates of 36.0% and 32.3% respectively. Similarly, a recent systematic review found a pooled prevalence of 440% of sleep problems among healthcare workers [61]. Another survey-based study in mainly European countries shows that sleep problems affect children and infants too [52] and indeed these groups should be considered as high-risk groups. Here, the caregiver's stress level was a determining factor for sleep quality of children and infants. A detailed summary of sleep difficulties is displayed in Table 1.
5.2. Sleep difficulties in COVID-19 patients
The rate of sleep problems is reported almost two times more in the patients infected with COVID-19 compared to the general population [73]. More importantly, sleep problems in the patients are associated with different aspects of the disease, including diagnosis, pathology, duration, and also recovery period. A study conducted in COVID-19-positive vs COVID-19-negative individuals showed that self-report based, and polysomnographic sleep data can significantly predict the diagnosis of COVID-19 [62]. This demonstrates an important role of sleep in COVID-19 pathology but also suggests that the course of disease in these patients can be predicted by sleep-related parameters. In this line, a recent study conducted in hospitalized COVID-10 patients found that the duration of hospitalization and depression rate was significantly higher in the group exhibiting poor sleep quality (PSQI score ≥5) [74]. Another meta-analysis of 31 studies and 5153 COVID-19 patients found a pooled prevalence of sleep disturbances of 34% [66]. Importantly, this was associated with a 45% and 57% prevalence of depression and anxiety in these patients, respectively. Sleep problems continue after recovery in the patient too. An investigation of 125 patients recovered from the COVID-19 disease showed an insomnia rate of 26.45% after recovery [75]. Sleep Disorder Breathing including sleep apnea is also reported more frequently in COVID-19 patients due to the respiratory nature of the disease [56,76].
5.3. Sleep difficulties in the general population
A recent study shows that higher sleep quality positively predicts learning/working efficiency and exercise levels, while poor sleep quality negatively predicts the use of electronic devices and negative emotions [65]. This shows a critical role of healthy sleep for adaptive functioning. Aside from the overall negative impact of the current pandemic on sleep quality of the general population, specific subpopulations might face poorer sleep quality. Healthcare workers [54], children [52], and students, especially during stressful events [67], and elderly [53] are among these subpopulations, although some studies found no difference in the prevalence of sleep disorders between healthcare vs other professions workers [77]. Sleep problems interestingly led to experiences of COVID-like symptoms also in healthcare workers with negative infection test results [78]. The pandemic, however, does not equally affect sleep quality identically in everyone which is important for screening those at higher risk. A recent study showed that the effect of COVID -19 on sleep quality differed across participants and depended on pre-pandemic sleep quality. Pre-pandemic good sleepers most often experienced worse sleep during the lockdown [79]. On the other hand, some demographic and environmental factors appear to predict pandemic-related sleep difficulties including race, socioeconomic status, marital status, anxiety symptoms, depressive symptoms, physical somatization, and social loneliness, but not age, gender, or education although results regarding these variables have been mixed [63,64,80,81]. In addition to overall impaired sleep quality, specific sleep disorders are also reported to be enhanced during the COVID-19 pandemic, including insomnia [56,57,63], nightmares [58], sleep apnea [59], and restless legs syndrome [82]. In sum, despite partial inconsistency between studies in reporting correlates of poor sleep in the general population, higher sleep difficulties and sleep disorders are well-documented in the general population and COVID-19 patients.
6. Potential interventions
6.1. Interventions for circadian alignment
A recent physiological study showed potential protective effects of healthy sleep and aligned circadian rhythms for faster and efficient recovery in COVID-19 patients [47]. In this line, there are behavioral recommendations that are feasible at home and can help align circadian rhythms. Keeping a regular night-time and wake-up time, being exposed to natural daylight during the day, and trying to be more physically active during the day allows the circadian rhythms to be aligned [37]. In the current situation, we need a flexible working and schooling schedule to compensate for circadian misalignment. A recent study in adolescent pupils shows that delaying high school start times could be an effective way to extend sleep duration, improve sleep quality, reduce daytime sleepiness, and lower adolescents' stress during the school year [55] (Table 1).
6.2. Interventions for healthy sleep
A study found that sleep quality is affected on a daily base and night-to-night change of sleep quality during the pandemic predicts how individuals cope with daily challenges induced by home confinement [72]. Accordingly, a relatively poorer night sleep predicts increased rumination, psychotic-like experiences, and somatic complaints the following day. This indicates the importance of early interventions for treatment and or prevention of sleep difficulties during the pandemic. The Cognitive-Behavioral Therapy (CBT) Academy for insomnia recently published a list of feasible practical recommendations that are helpful for enhancing sleep hygiene during the pandemic [37]. These recommendations suggest avoiding over-attention to stressful news about the pandemic, expressing stress/anxiety with friends or the social medial, doing regular exercise, receiving natural daylight, and keeping regular night-time and wake-up time. Moreover, digital CBT for insomnia treatment that was received before the pandemic, increased health resilience during the actual COVID-19 pandemic in adults with a history of insomnia and ongoing mild to moderate mental health symptoms [83]. Another study showed that online mindfulness training via videoconferencing may be a useful intervention for stress reduction, but not sleep improvement during times when traditional in-person training is not feasible [84]. Finally, a recent metanalysis showed that non-pharmacological interventions (eg, muscle relaxation, respiratory muscle-related rehabilitation, online psychotherapy) can improve the sleep status of COVID-19 patients [85].
For COVID-19 patients, chronopharmacology is suggested as a potential intervention and especially during the hospitalization period. This approach has two major aspects: conducting general disease- and symptom-related interventions (eg, medication) during the optimal time of the day to guarantee maximum efficacy, and administration of modulators of circadian rhythms such as corticosteroids and melatonin [47,86]. Increased exposure to environmental zeitgebers (eg, light) of COVID-19 patients hospitalized in the intensive care unit has is also suggested for expediting the recovery process and alleviating symptoms severity [47]. This study also suggests determining the circadian profile of the patient (rhythmic/nonrhythmic amplitude and phase) and to assess the individual time of the largest risk for complications, and that of optimal medication dosing schedules (Table 1).
7. Conclusion
We provided an updated overview of the impact of the COVID-19 pandemic on circadian rhythms and sleep in the general population and COVID-19 patients. Home confinement seems to be a central factor in driving not only circadian misalignment but also poor sleep quality. On the other hand, sleep difficulties and circadian disruption have a critical role in the diagnosis, pathology, disease prolongation and recovery of COVID-19 patients. Despite such a pervasive role, the role of sleep problems is underestimated with respect to health-related behavior in the general population and infected patients. Behavioral interventions for balancing the factors contributing to circadian misalignment and poor sleep quality are available, which should be considered by health professionals and policymakers.
CRediT author contributions
MAS: Investigation, Conceptualization, Methodology, Writing - Original Draft, Writing - Review & Editing. AA: Investigation, Writing - Review & Editing. E.GH: Investigation, Visualization, Writing - Review & Editing. MAN: Writing - Review & Editing.
Acknowledgments
The authors received no financial support for the research, authorship, and/or publication of this solicited article.
Footnotes
Authors declare no competing interests.
The ICMJE Uniform Disclosure Form for Potential Conflicts of Interest associated with this article can be viewed by clicking on the following link: https://doi.org/10.1016/j.sleep.2021.07.011.
Conflict of interest
The following is the supplementary data related to this article:
Multimedia component 1
References
- 1.Gates B. Responding to covid-19—a once-in-a-century pandemic? N Engl J Med. 2020;382:1677–1679. doi: 10.1056/NEJMp2003762. [DOI] [PubMed] [Google Scholar]
- 2.Menni C., Valdes A.M., Freidin M.B., et al. Real-time tracking of self-reported symptoms to predict potential COVID-19. Nat Med. 2020;26:1037–1040. doi: 10.1038/s41591-020-0916-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Giuntella O., Hyde K., Saccardo S., et al. Lifestyle and mental health disruptions during COVID-19. Proc Natl Acad Sci Unit States Am. 2021;118 doi: 10.1073/pnas.2016632118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rogers J.P., Chesney E., Oliver D., et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry. 2020;7:611–627. doi: 10.1016/S2215-0366(20)30203-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Armitage R., Nellums L.B. COVID-19 and the consequences of isolating the elderly. The Lancet Public Health. 2020;5:e256. doi: 10.1016/S2468-2667(20)30061-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bogin B., Varea C. COVID-19, crisis, and emotional stress: a biocultural perspective of their impact on growth and development for the next generation. Am J Hum Biol. 2020;32:e23474. doi: 10.1002/ajhb.23474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wise T., Zbozinek T.D., Michelini G., et al. Vol. 7. Royal Society Open Science; 2020. Changes in risk perception and self-reported protective behaviour during the first week of the COVID-19 pandemic in the United States; p. 200742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jiao W.Y., Wang L.N., Liu J., et al. Behavioral and emotional disorders in children during the COVID-19 epidemic. J Pediatr. 2020;221:264–266.e1. doi: 10.1016/j.jpeds.2020.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Martín-Jiménez P., Muñoz-García M.I., Seoane D., et al. Cognitive impairment is a common comorbidity in deceased COVID-19 patients: a hospital-based retrospective cohort study. J Alzheimers Dis. 2020;78:1367–1372. doi: 10.3233/JAD-200937. [DOI] [PubMed] [Google Scholar]
- 10.Hampshire A., Trender W., Chamberlain S.R., et al. Cognitive deficits in people who have recovered from COVID-19 relative to controls: an N=84,285 online study. medRxiv. 2020 doi: 10.1016/j.eclinm.2021.101044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Salehinejad M.A., Majidinezhad M., Ghanavati E., et al. Negative impact of COVID-19 pandemic on sleep quantitative parameters, quality, and circadian alignment: implications for health and psychological well-being. EXCLI Journal. 2020;19:1297–1308. doi: 10.17179/excli2020-2831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alexander P.E., Debono V.B., Mammen M.J., et al. COVID-19 coronavirus research has overall low methodological quality thus far: case in point for chloroquine/hydroxychloroquine. J Clin Epidemiol. 2020;123:120–126. doi: 10.1016/j.jclinepi.2020.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jung R.G., Di Santo P., Clifford C., et al. Methodological quality of COVID-19 clinical research. Nat Commun. 2021;12:943. doi: 10.1038/s41467-021-21220-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Borbély A.A. A two process model of sleep regulation. Hum Neurobiol. 1982;1:195–204. [PubMed] [Google Scholar]
- 15.Borbély A.A., Daan S., Wirz-Justice A., et al. The two-process model of sleep regulation: a reappraisal. J Sleep Res. 2016;25:131–143. doi: 10.1111/jsr.12371. [DOI] [PubMed] [Google Scholar]
- 16.Salehinejad M.A., Ghanavati E., Reinders J., et al. Sleep-dependent upscaled excitability and saturated neuroplasticity in the human brain: from brain physiology to cognition. bioRxiv. 2021 doi: 10.7554/eLife.69308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Salehinejad M.A., Wischnewski M., Ghanavati E., et al. Cognitive functions and respective parameters of human brain physiology are chronotype-dependent. bioRxiv. 2021 doi: 10.1038/s41467-021-24885-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barnes C., McNaughton B., Goddard G., et al. Circadian rhythm of synaptic excitability in rat and monkey central nervous system. Science. 1977;197:91–92. doi: 10.1126/science.194313. [DOI] [PubMed] [Google Scholar]
- 19.Gerstner J.R., Yin J.C. Circadian rhythms and memory formation. Nat Rev Neurosci. 2010;11:577. doi: 10.1038/nrn2881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Appelbaum L., Wang G., Yokogawa T., et al. Circadian and homeostatic regulation of structural synaptic plasticity in hypocretin neurons. Neuron. 2010;68:87–98. doi: 10.1016/j.neuron.2010.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ly J.Q.M., Gaggioni G., Chellappa S.L., et al. Circadian regulation of human cortical excitability. Nat Commun. 2016;7:11828. doi: 10.1038/ncomms11828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gaggioni G., Ly J.Q.M., Muto V., et al. Age-related decrease in cortical excitability circadian variations during sleep loss and its links with cognition. Neurobiol Aging. 2019;78:52–63. doi: 10.1016/j.neurobiolaging.2019.02.004. [DOI] [PubMed] [Google Scholar]
- 23.Zare Khormizi H., Salehinejad M.A., Nitsche M.A., et al. Sleep-deprivation and autobiographical memory: evidence from sleep-deprived nurses. J Sleep Res. 2019;28 doi: 10.1111/jsr.12683. [DOI] [PubMed] [Google Scholar]
- 24.Schmidt C., Collette F., Cajochen C., et al. A time to think: circadian rhythms in human cognition. Cogn Neuropsychol. 2007;24:755–789. doi: 10.1080/02643290701754158. [DOI] [PubMed] [Google Scholar]
- 25.Yaffe K., Falvey C.M., Hoang T. Connections between sleep and cognition in older adults. Lancet Neurol. 2014;13:1017–1028. doi: 10.1016/S1474-4422(14)70172-3. [DOI] [PubMed] [Google Scholar]
- 26.Wright K., Lowry C., LeBourgeois M. Circadian and wakefulness-sleep modulation of cognition in humans. Front Mol Neurosci. 2012;5 doi: 10.3389/fnmol.2012.00050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goldin A.P., Sigman M., Braier G., et al. Interplay of chronotype and school timing predicts school performance. Nature Human Behaviour. 2020;4:387–396. doi: 10.1038/s41562-020-0820-2. [DOI] [PubMed] [Google Scholar]
- 28.Musshafen L.A., Tyrone R.S., Abdelaziz A., et al. Associations between sleep and academic performance in US adolescents: a systematic review and meta-analysis. Sleep Med. 2021;83:71–82. doi: 10.1016/j.sleep.2021.04.015. [DOI] [PubMed] [Google Scholar]
- 29.Grandin L.D., Alloy L.B., Abramson L.Y. The social zeitgeber theory, circadian rhythms, and mood disorders: review and evaluation. Clin Psychol Rev. 2006;26:679–694. doi: 10.1016/j.cpr.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 30.Baron K.G., Reid K.J. Circadian misalignment and health. Int Rev Psychiatr. 2014;26:139–154. doi: 10.3109/09540261.2014.911149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chellappa S.L., Morris C.J., Scheer F.A.J.L. Daily circadian misalignment impairs human cognitive performance task-dependently. Sci Rep. 2018;8:3041. doi: 10.1038/s41598-018-20707-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Alloy L.B., Nusslock R., Boland E.M. The development and course of bipolar spectrum disorders: an integrated reward and circadian rhythm dysregulation model. Annu Rev Clin Psychol. 2015;11:213–250. doi: 10.1146/annurev-clinpsy-032814-112902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Carta M.G., Ouali U., Perra A., et al. Living with bipolar disorder in the time of covid-19: biorhythms during the severe lockdown in cagliari, Italy, and the moderate lockdown in tunis, Tunisia. Front Psychiatr. 2021;12:634765. doi: 10.3389/fpsyt.2021.634765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Partinen M. Sleep research in 2020: COVID-19-related sleep disorders. Lancet Neurol. 2021;20:15–17. doi: 10.1016/S1474-4422(20)30456-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yao H., Chen J.-H., Xu Y.-F. Patients with mental health disorders in the COVID-19 epidemic. The Lancet Psychiatry. 2020;7:e21. doi: 10.1016/S2215-0366(20)30090-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ray S., Reddy A.B. COVID-19 management in light of the circadian clock. Nat Rev Mol Cell Biol. 2020;21:494–495. doi: 10.1038/s41580-020-0275-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Altena E., Baglioni C., Espie C.A., et al. Dealing with sleep problems during home confinement due to the COVID-19 outbreak: practical recommendations from a task force of the European CBT-I Academy. J Sleep Res. 2020;29 doi: 10.1111/jsr.13052. [DOI] [PubMed] [Google Scholar]
- 38.Morin C.M. Carrier J, Bastien C, Godbout R, on behalf of the Canadian S, Circadian N. Sleep and circadian rhythm in response to the COVID-19 pandemic. Can J Public Health. 2020;111:654–657. doi: 10.17269/s41997-020-00382-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Leone M.J., Sigman M., Golombek D.A. Effects of lockdown on human sleep and chronotype during the COVID-19 pandemic. Curr Biol. 2020;30:R930. doi: 10.1016/j.cub.2020.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rome O., Sinai L., Sevitt R., et al. Owls and larks do not exist: COVID-19 quarantine sleep habits. Sleep Med. 2020;77:177–183. doi: 10.1016/j.sleep.2020.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Man K., Loudon A., Chawla A. Immunity around the clock. Science. 2016;354:999–1003. doi: 10.1126/science.aah4966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Scheiermann C., Kunisaki Y., Frenette P.S. Circadian control of the immune system. Nat Rev Immunol. 2013;13:190–198. doi: 10.1038/nri3386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cuesta M., Boudreau P., Dubeau-Laramée G., et al. Simulated night shift disrupts circadian rhythms of immune functions in humans. J Immunol. 2016;196:2466–2475. doi: 10.4049/jimmunol.1502422. [DOI] [PubMed] [Google Scholar]
- 44.Robert Y., Moore M. Circadian rhythms: basic neurobiology and clinical applications. Annu Rev Med. 1997;48:253–266. doi: 10.1146/annurev.med.48.1.253. [DOI] [PubMed] [Google Scholar]
- 45.Edgar R.S., Stangherlin A., Nagy A.D., et al. Cell autonomous regulation of herpes and influenza virus infection by the circadian clock. Proc Natl Acad Sci Unit States Am. 2016;113:10085–10090. doi: 10.1073/pnas.1601895113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fatima Y, Bucks RS, Mamun AA, et al. Shift work is associated with increased risk of COVID-19: findings from the UK Biobank cohort. J Sleep Res. 2021:e13326. [DOI] [PMC free article] [PubMed]
- 47.Haspel J., Kim M., Zee P., et al. A timely call to arms: COVID-19, the circadian clock, and critical care. J Biol Rhythm. 2021 doi: 10.1177/0748730421992587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tao S., Wu X., Li S., et al. 2020. Associations of circadian rhythm abnormalities caused by home quarantine during the COVID-19 outbreak and mental health in Chinese undergraduates: evidence from a nationwide school-based survey. Available at: SSRN 3582851. [Google Scholar]
- 49.Korman M., Tkachev V., Reis C., et al. COVID-19-mandated social restrictions unveil the impact of social time pressure on sleep and body clock. Sci Rep. 2020;10:22225. doi: 10.1038/s41598-020-79299-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Silva FRd, Guerreiro RdC., Andrade HdA., et al. Does the compromised sleep and circadian disruption of night and shiftworkers make them highly vulnerable to 2019 coronavirus disease (COVID-19)? Chronobiol Int. 2020;37:607–617. doi: 10.1080/07420528.2020.1756841. [DOI] [PubMed] [Google Scholar]
- 51.Cardinali D.P., Brown G.M., Reiter R.J., et al. Elderly as a high-risk group during COVID-19 pandemic: effect of circadian misalignment, sleep dysregulation and melatonin administration. Sleep and vigilance. 2020:1–7. doi: 10.1007/s41782-020-00111-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Markovic A, Mühlematter C, Beaugrand M, et al. Severe effects of the COVID-19 confinement on young children's sleep: a longitudinal study identifying risk and protective factors. J Sleep Res. 2021:e13314. [DOI] [PMC free article] [PubMed]
- 53.De Pue S., Gillebert C., Dierckx E., et al. The impact of the COVID-19 pandemic on wellbeing and cognitive functioning of older adults. Sci Rep. 2021;11:4636. doi: 10.1038/s41598-021-84127-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Simonetti V., Durante A., Ambrosca R., et al. Anxiety, sleep disorders and self-efficacy among nurses during COVID-19 pandemic: a large cross-sectional study. J Clin Nurs. 2021;30:1360–2137. doi: 10.1111/jocn.15685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gruber R., Saha S., Somerville G., et al. The impact of COVID-19 related school shutdown on sleep in adolescents: a natural experiment. Sleep Med. 2020;76:33–35. doi: 10.1016/j.sleep.2020.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tasnim S., Rahman M., Pawar P., et al. Epidemiology of sleep disorders during COVID-19 pandemic: a systematic scoping review. medRxiv. 2020 [Google Scholar]
- 57.Lin L-y, Wang J., Ou-yang X-y, et al. The immediate impact of the 2019 novel coronavirus (COVID-19) outbreak on subjective sleep status. Sleep Med. 2021;77:348–354. doi: 10.1016/j.sleep.2020.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gorgoni M., Scarpelli S., Alfonsi V., et al. Pandemic Dreams: quantitative and qualitative features of the oneiric activity during the lockdown due to COVID-19 in Italy. Sleep Med. 2021;81:20–32. doi: 10.1016/j.sleep.2021.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Thorpy M., Figuera-Losada M., Ahmed I., et al. Management of sleep apnea in New York City during the COVID-19 pandemic. Sleep Med. 2020;74:86–90. doi: 10.1016/j.sleep.2020.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Liu K., Chen Y., Wu D., et al. Effects of progressive muscle relaxation on anxiety and sleep quality in patients with COVID-19. Compl Ther Clin Pract. 2020;39:101132. doi: 10.1016/j.ctcp.2020.101132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Marvaldi M., Mallet J., Dubertret C., et al. Anxiety, depression, trauma-related, and sleep disorders among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Neurosci Biobehav Rev. 2021;126:252–264. doi: 10.1016/j.neubiorev.2021.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Quer G., Radin J.M., Gadaleta M., et al. Wearable sensor data and self-reported symptoms for COVID-19 detection. Nat Med. 2021;27:73–77. doi: 10.1038/s41591-020-1123-x. [DOI] [PubMed] [Google Scholar]
- 63.Dzierzewski J.M., Dautovich N.D., Ravyts S.G., et al. Insomnia symptoms during the COVID-19 pandemic: an examination of biopsychosocial moderators. Sleep Med. 2021 doi: 10.1016/j.sleep.2021.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hyun S., Hahm H.C., Wong G.T.F., et al. Psychological correlates of poor sleep quality among U.S. young adults during the COVID-19 pandemic. Sleep Med. 2021;78:51–56. doi: 10.1016/j.sleep.2020.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Dai W., Zhou J., Li G., et al. Maintaining normal sleep patterns, lifestyles and emotion during the COVID-19 pandemic: the stabilizing effect of daytime napping. J Sleep Res. 2021:e13259. doi: 10.1111/jsr.13259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Deng J., Zhou F., Hou W., et al. Annals of the New York Academy of Sciences; 2020. The prevalence of depression, anxiety, and sleep disturbances in COVID-19 patients: a meta-analysis. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Du C., Zan M.C.H., Cho M.J., et al. Health behaviors of higher education students from 7 countries: poorer sleep quality during the COVID-19 pandemic predicts higher dietary risk. Clocks & sleep. 2021;3:12–30. doi: 10.3390/clockssleep3010002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Marelli S., Castelnuovo A., Somma A., et al. Impact of COVID-19 lockdown on sleep quality in university students and administration staff. J Neurol. 2021;268:8–15. doi: 10.1007/s00415-020-10056-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Dijk D., Czeisler C. Contribution of the circadian pacemaker and the sleep homeostat to sleep propensity, sleep structure, electroencephalographic slow waves, and sleep spindle activity in humans. J Neurosci. 1995;15:3526–3538. doi: 10.1523/JNEUROSCI.15-05-03526.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Cellini N., Canale N., Mioni G., et al. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J Sleep Res. 2020;29 doi: 10.1111/jsr.13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Jiang Z., Zhu P., Wang L., et al. Psychological distress and sleep quality of COVID-19 patients in Wuhan, a lockdown city as the epicenter of COVID-19. J Psychiatr Res. 2020;136:595–602. doi: 10.1016/j.jpsychires.2020.10.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Simor P., Polner B., Báthori N., et al. Home confinement during the COVID-19: day-to-day associations of sleep quality with rumination, psychotic-like experiences, and somatic symptoms. Sleep. 2021;44:zsab029. doi: 10.1093/sleep/zsab029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Jahrami H., BaHammam A.S., Bragazzi N.L., et al. Sleep problems during the COVID-19 pandemic by population: a systematic review and meta-analysis. J Clin Sleep Med. 2021;17:299–313. doi: 10.5664/jcsm.8930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Akıncı T., Melek Başar H. Relationship between sleep quality and the psychological status of patients hospitalised with COVID-19. Sleep Med. 2021;80:167–170. doi: 10.1016/j.sleep.2021.01.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Xu F., Wang X., Yang Y., et al. Depression and insomnia in COVID-19 survivors: a cross-sectional survey from Chinese rehabilitation centers in Anhui province. Sleep Med. 2021 doi: 10.1016/j.sleep.2021.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Labarca G., Henriquez-Beltran M., Llerena F., et al. Undiagnosed sleep disorder breathing as a risk factor for critical COVID-19 and pulmonary consequences at the midterm follow-up. Sleep Med. 2021 doi: 10.1016/j.sleep.2021.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Janati Idrissi A., Lamkaddem A., Benouajjit A., et al. Sleep quality and mental health in the context of COVID-19 pandemic and lockdown in Morocco. Sleep Med. 2020;74:248–253. doi: 10.1016/j.sleep.2020.07.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Amra B., Salmasi M., Soltaninejad F., et al. Healthcare workers' sleep and mood disturbances during COVID-19 outbreak in an Iranian referral center. Sleep & breathing = Schlaf & Atmung. 2021:1–8. doi: 10.1007/s11325-021-02312-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kocevska D., Blanken T.F., Van Someren E.J.W., et al. Sleep quality during the COVID-19 pandemic: not one size fits all. Sleep Med. 2020;76:86–88. doi: 10.1016/j.sleep.2020.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Duran S., Ö Erkin. Psychologic distress and sleep quality among adults in Turkey during the COVID-19 pandemic. Prog Neuro Psychopharmacol Biol Psychiatr. 2021;107:110254. doi: 10.1016/j.pnpbp.2021.110254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Paiva T., Reis C., Feliciano A., et al. Sleep and awakening quality during COVID-19 confinement: complexity and relevance for health and behavior. Int J Environ Res Publ Health. 2021:18. doi: 10.3390/ijerph18073506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Franco B., Morais M.A., Holanda A.S.S., et al. Impact of Covid-19 on the restless legs syndrome. Sleep science (Sao Paulo, Brazil) 2020;13:186–190. doi: 10.5935/1984-0063.20200031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Cheng P., Casement M.D., Kalmbach D.A., et al. Digital cognitive behavioral therapy for insomnia promotes later health resilience during the coronavirus disease 19 (COVID-19) pandemic. Sleep. 2021;44:zsaa258. doi: 10.1093/sleep/zsaa258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lim J., Leow Z., Ong J., et al. JMIR mental health; 2021. The effects of online group mindfulness training on stress and sleep quality during the COVID-19 pandemic in Singapore: a retrospective equivalence analysis. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ding H., He F., Lu Y.G., et al. Effects of non-drug interventions on depression, anxiety and sleep in COVID-19 patients: a systematic review and meta-analysis. Eur Rev Med Pharmacol Sci. 2021;25:1087–1096. doi: 10.26355/eurrev_202101_24679. [DOI] [PubMed] [Google Scholar]
- 86.Cardinali D.P., Brown G.M., Pandi-Perumal S.R. Can melatonin Be a potential “silver bullet” in treating COVID-19 patients? Diseases. 2020;8:44. doi: 10.3390/diseases8040044. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Multimedia component 1