Abstract
Aim
To understand the impact of COVID pandemic on the activity and patients’ care of the Head and Neck regional Unit, temporary moved in a COVID-free hospital.
Methods
We retrospectively analyzed the yearly activity of the “Head & Neck Cancer Unit” at the Azienda Ospedali Riuniti Marche Nord (Italy) during 2020 (COVID-19 pandemic) and we compared it with the one performed in 2019. Statistical analyses were performed using Chi-square.
Results
No significant differences were observed comparing the total number of patients treated for H&N squamous cell carcinoma (SCC) in 2019 with the ones in 2020. Moreover, no differences were identified in term of cancer stage at the moment of the surgery between 2019 and 2020. On the contrary, a significant reduction in the number of surgical procedures carried out for thyroid (p < 0.05) and skin (p < 0.001) malignancies was identified.
Conclusions
Despite Covid-19 limitations, our institution was able to preserve the number of major oncologic procedures without negative impact on patients’ care. We believe that the creation of specific COVID-free hospital can be the key preserve quality of care in epidemic emergency.
Keywords: Cancer, Head and neck, COVID-19, Multidisciplinary tumor board, Performance
Dear Editor,
The novel coronavirus 2019 (COVID-19) has having a severe impact on the health system due to the high likely of hospitalization and the risk of nosocomial transmission if not promptly and correctly diagnosed [1]. The needs of extensive pre-hospitalization screening prolonged the time of patients’ admission [1], [2]. Furthermore, to limit the risk of hospital virus spread, the number of accesses and procedures were limited, with the risk of a negative impact on patient’s health especially in case of head and neck malignancies [2].
Cancer surgery is generally considered non-elective, although there is a range of potential risks in which patients can occur if not promptly treated especially in case of head and neck malignancies. In fact, several upper aerodigestive tract malignancies can rapidly grow and quickly metastasize to locoregional lymph nodes [3], [4], [5], so a treatment delay over 20 days exposes patients to an increased risk of survival [3], [6].
Head and neck surgical procedures often require a relevant amount of healthcare resources in addition to potential infectious risks for healthcare workers, which may affect the decision to postpone or modify the surgery in case of financial restrictions or different use of economic/personnel resources (i.e. for Intensive Care Units or Covid Departments) [6], [7], [8], [9]. For example, free flap reconstructive surgery requires longer operative times and postoperative intensive care unit (ICU) occupancy [9]. Because nasopharynx and oropharynx are common location of Sars-CoV2, surgery in these districts expose healthcare workers (HCWs) to high risk of infection and has to be correctly managed to limit potential infection [7], [8], [9], [10].
The purpose of this study was to retrospectively analyze the activity of the “Head & Neck Cancer Group” at AORMN during the COVID-19 year (2020) comparing it to 2019 to understand the possible influence of COVID pandemic on the outcomes of patients affected by Head and Neck cancer. Notably, our region relocated the clinical and surgical activity separating it in COVID and COVID-free hospitals.
The study was approved by the Internal Review Board (IRB) of Azienda Ospedali Riuniti Marche Nord (AORMN), without release of an identification number following national laws for retrospective study. Medical records of patients in years 2019 and 2020 treated for any types of cancer in the Otolaryngology Department of AORMN were revised. Data about gender, age, location, type and severity of tumor were collected. Statistical analyses were performed using STATA ®. Chi Square was used to compare the data between 2019 and 2020. P was considered significant < 0.05.
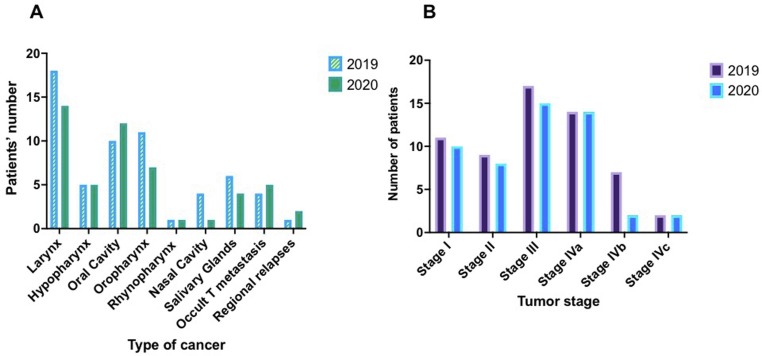
In 2019, 65 patients (42M, 23F, mean age 68 ± 13 years) completed the diagnostic and therapeutic procedures; 92.3% (60) patients suffered from head and neck squamous cell carcinoma (HNSCC), and 7.7% (5) had an advanced loco-regional relapse (node metastasis) arising from a previous head and neck skin cancer resection. In 2020, 56 subjects (38M, 18F, mean age 68 ± 10 years) completed the diagnostic and therapeutic procedures; 73.9% (51) subjects affected by HNSCC and 6.1% (5) had advanced loco-regional relapses (Fig. 1 a). No significant difference in patients’ cancer stage was noticed between 2019 and 2020 (Fig. 1b).
Fig. 1.
A) Comparison between patients treated for H&N squamous cell carcinoma in 2019 and 2020. B) Analysis of H&N squamous cell carcinomas stage of patients treated in 2019 and 2020.
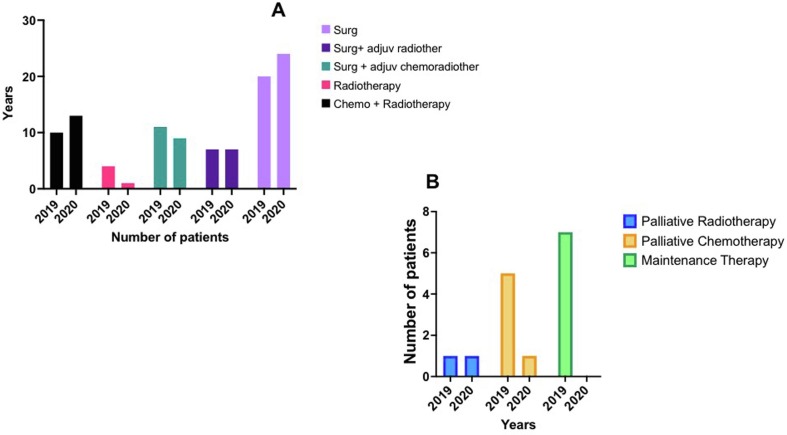
In 2019 patients underwent the following treatments: 30.8% (20) surgery only, 10.8% (7) surgery and adjuvant radiotherapy, 16.9% (11) surgery and adjuvant radio-chemotherapy, 6.1% (4) exclusive radiotherapy, 15.4% (10) radio-chemotherapy and 9.2% (6) radiotherapy or palliative chemotherapy. Maintenance therapy was performed in 10.8% (7) subjects, including 2 patients refusing the proposed treatment. The patients evaluated in 2020 underwent the following treatments: 42.8% (24) surgery only, 12.5% (7) surgery and adjuvant radiotherapy, 16.1% (9) surgery and adjuvant radio-chemotherapy, 1.8% (1) exclusive radiotherapy, 23.2% (13) radio-chemotherapy and 3.6% (2) radiotherapy or palliative chemotherapy (Fig. 2 ). When comparing 2020 data with those of 2019, we did not record a significant difference in the treatments performed.
Fig. 2.
A) Comparison among type of treatments performed in 2019 and 2020. B) Analysis of palliative and maintenance therapy performed in 2019 and 2020.
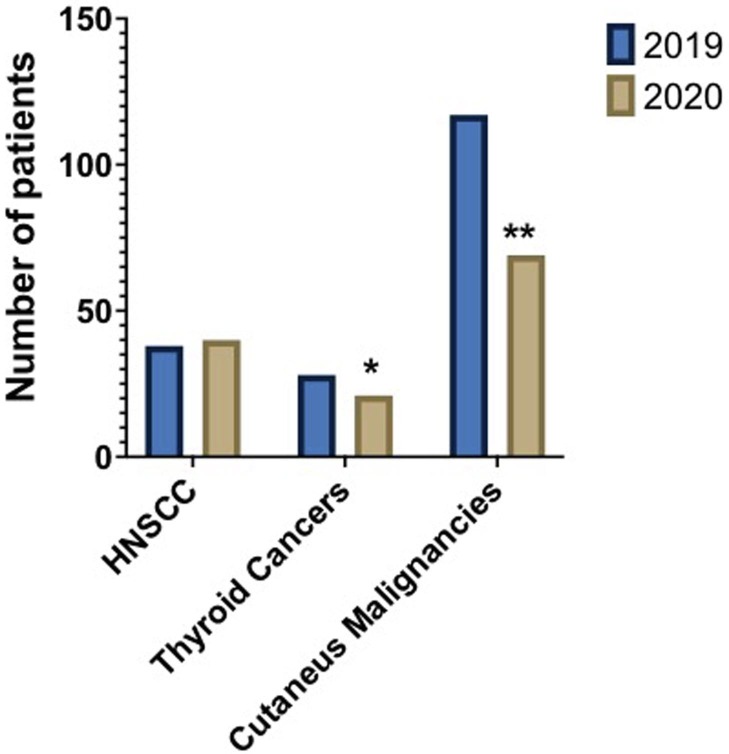
38 surgical procedures for H&N cancer were performed in 2019 and 40 in 2020. Thyroid surgery for cancer was statistically significant reduced (25% less) comparing 2020 with 2019 (p < 0.05). Same statistically significant differences were observed looking at surgical procedures carried out for cutaneous malignancies (p < 0.001). In 2020, these procedures were reduced of 41% compared with 2019 (69 vs 117) (Fig. 3 ).
Fig. 3.
Surgical procedures performed for malignancies of the H&N in 2019 and 2020 (*: p < 0.05; **: p < 0.001).
AORMN includes three hospitals that were adapted to manage COVID pandemic without excessively reduction of medical and surgical activities. Two hospitals were exclusively dedicated to patients with COVID-19 and one devoted to continue standard medical and surgical treatment including emergencies (COVID-free).
Despite we observed a consistent reduction of surgery for thyroid [11] and skin cancers [12], maybe related to the poor symptomatology and symptoms underestimation by patients, the subdivision of the activity in three different hospital allowed us to treat head and neck cancers without any negative impact on patients care. In the COVID-free hospital, the procedure for admitting patients were standardized and extremely restricted both for patients and healthcare professional [13]. This rigorous method allowed to manage the treatment of head and neck malignancies exactly as in non-pandemic era [12].
During COVID-19 pandemic, the management of patients with cancer has becoming more challenging; in fact, they represent a high-risk group because more vulnerable to the infections due to their underlying disease and their immunosuppressed state, which implies a greater risk of serious bacterial/viral complications during and post-surgery [14]. Sars-CoV2 can be potentially fatal in these patients, so any type of methods to leave the virus out have to be used. Based on our experience a complete separation of the activities can be a successful way to protect these patients.
We think that due to the increased risk of new-pandemic, the healthcare system should be organized to promptly divide clinical and surgical activity to avoid delay in the treatment of the cancer; in fact, a tardive treatment could expose patients to high risk of death, another long-term – despite underestimated – effect of COVID-19 pandemic.
Financial support
None.
Author contribution
LD: clinical care, data analyses, manuscript idea, writing and final approval; GL: clinical care, data acquisition and analyses, manuscript idea, writing and final approval; MP: clinical care, data acquisition and analyses, manuscript idea, writing and final approval; CB, FB, FM, EM, AR, LG, AP,AS,GL, BR,AS and PA : clinical care, manuscript writing and final approval; MC: clinical care and organization, manuscript writing and final approval, LI: clinical care, data acquisition, manuscript idea, writing and final approval; ADS: study design and supervision, data analysis, definition of conclusion writing and final approval.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Armocida B., Formenti B., Ussai S., Palestra F., Missoni E. The Italian health system and the COVID-19 challenge. Lancet Public Health. 2020;5(5):e253. doi: 10.1016/S2468-2667(20)30074-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jensen A.R., Nellemann H.M., Overgaard J. Tumor progression in waiting time for radiotherapy in head and neck cancer. Radiother Oncol. 2007;84(1):5–10. doi: 10.1016/j.radonc.2007.04.001. [DOI] [PubMed] [Google Scholar]
- 3.Xing Y., Zhang J., Lin H., Gold K.A., Sturgis E.M., Garden A.S., et al. Relation between the level of lymph node metastasis and survival in locally advanced head and neck squamous cell carcinoma. Cancer. 2016;122(4):534–545. doi: 10.1002/cncr.29780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Di Stadio A., Gradoni P., Cingolani C., Battisti E., Pandolfini M., Milazzo E., et al. Björk Flap Tracheotomy for COVID-19 Pneumonia With Massive Thyroid Struma: A Stable Airway to Expedite Ventilator Weaning. Ear Nose Throat J. 2020 doi: 10.1177/0145561320968931. 145561320968931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Graboyes E.M., Kompelli A.R., Neskey D.M., Brennan E., Nguyen S., Sterba K.R., et al. Association of treatment delays with survival for patients with head and neck cancer: a systematic review. JAMA Otolaryngol Head Neck Surg. 2019;145(2):166. doi: 10.1001/jamaoto.2018.2716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.D'Ascanio L., Pandolfini M., Cingolani C., Latini G., Giardini D. Letter to the editor regarding “How to avoid nosocomial spread during tracheostomy for Covid-19 patients”. Head Neck. 2020;42(9):2768–2769. doi: 10.1002/hed.26333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.D'Ascanio L., Pandolfini M., Capalbo M., Tempesta M. Minimizing Healthcare Worker Contamination Risk During Tracheostomy. J Am Coll Surg. 2020;231(2):299–300. doi: 10.1016/j.jamcollsurg.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.D'Ascanio L., Latini G., Pandolfini M., Giardini D. Corona-steps for tracheotomy in COVID-19 patients: A staff-safe method for airway management. Oral Oncol. 2020;106:104731. doi: 10.1016/j.oraloncology.2020.104731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Prachand V.N., Milner R., Angelos P., Posner M.C., Fung J.J., Agrawal N., et al. Medically necessary, time-sensitive procedures: scoring system to ethically and efficiently manage resource scarcity and provider risk during the COVID-19 Pandemic. J Am Coll Surg. 2020;231(2):281–288. doi: 10.1016/j.jamcollsurg.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.De Luca P., Scarpa A., Ralli M., De Vincentiis M., Cassandro E., Chiarella G., et al. Nasal, pharyngeal, and laryngeal endoscopy procedures during COVID-19 pandemic: available recommendations from national and international societies. Eur Arch Otorhinolaryngol. 2020;277(7):2151–2153. doi: 10.1007/s00405-020-06028-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.van Gerwen M., Alpert N., Sinclair C., Kale M., Genden E., Taioli E. Assessing non-aggressiveness of untreated, local and regional, papillary thyroid cancer. Oral Oncol. 2020;105:104674. doi: 10.1016/j.oraloncology.2020.104674. [DOI] [PubMed] [Google Scholar]
- 12.Maranzano M., D'Ascanio L., Ricci G., Omer H., Di Stadio A. Misinterpretation of head and neck masses can delay the correct diagnosis. A two-step demolitive-reconstruction surgery for saving patient's life. Oral Oncol. 2021:105197. doi: 10.1016/j.oraloncology.2021.105197. [DOI] [PubMed] [Google Scholar]
- 13.Riva G., Pizzo C., Fassone E., Pecorari G. Head and neck cancer surgery in COVID-19 pandemic in Northern Italy. Oral Oncol. 2020;107:104835. doi: 10.1016/j.oraloncology.2020.104835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Perri F., Ionna F., Longo F., Della Vittoria Scarpati G., De Angelis C., Ottaiano A., et al. Immune response against head and neck cancer: biological mechanisms and implication on therapy. TranslOncol. 2020;13(2):262–274. doi: 10.1016/j.tranon.2019.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]