Abstract
Background
A significant proportion of healthcare resource has been diverted to the care of those with COVID-19. This study reports the volume of surgical activity and the number of cancelled surgical procedures during the COVID-19 pandemic.
Methods
We used hospital episode statistics for all adult patients undergoing surgery between January 1, 2020 and December 31, 2020 in England and Wales. We identified surgical procedures using a previously published list of procedure codes. Procedures were stratified by urgency of surgery as defined by NHS England. We calculated the deficit of surgical activity by comparing the expected number of procedures from 2016 to 2019 with the actual number of procedures in 2020. Using a linear regression model, we calculated the expected cumulative number of cancelled procedures by December 31, 2021.
Results
The total number of surgical procedures carried out in England and Wales in 2020 was 3 102 674 compared with the predicted number of 4 671 338 (95% confidence interval [CI]: 4 218 740–5 123 932). This represents a 33.6% reduction in the national volume of surgical activity. There were 763 730 emergency surgical procedures (13.4% reduction) compared with 2 338 944 elective surgical procedures (38.6% reduction). The cumulative number of cancelled or postponed procedures was 1 568 664 (95% CI: 1 116 066–2 021 258). We estimate that this will increase to 2 358 420 (95% CI: 1 667 587–3 100 808) up to December 31, 2021.
Conclusions
The volume of surgical activity in England and Wales was reduced by 33.6% in 2020, resulting in more than 1.5 million cancelled operations. This deficit will continue to grow in 2021.
Keywords: anaesthesia, COVID-19, public policy, surgery, surgical activity, waiting list
Editor's key points.
-
•
COVID-19 has led to cancellations to elective surgery and changes in treatment options for those with acute surgical conditions, reducing surgical activity in countries around the world.
-
•
There is a marked growth of surgical waiting lists, which will add pressure to most national health systems.
-
•
It may take many years to clear the backlog of surgery as a result of COVID-19.
-
•
Widespread community vaccination is a necessary component of COVID-19 recovery.
The COVID-19 pandemic has fundamentally changed the delivery of healthcare worldwide. In many health systems, resources have been reallocated to the care of patients with COVID-19 and diverted away from routine healthcare services, including cancer care and chronic disease management.1,2 Critical care capacity was increased; staff and equipment were redeployed; and, in some cases, new hospitals were built.3, 4, 5 In England, the NHS postponed all non-urgent surgery (including the majority of cancer surgery) from April 15, 2020 to support the response to the first wave of the pandemic, with repetition of these delays from December 2020 in response to the second wave.6, 7, 8 This has had an enormous, but as yet uncharacterised, impact on the provision of surgery, resulting in the cancellation or delay of many operations, for almost an entire year.
In high-income countries, surgical services represent a large portion of healthcare activity.9 In the NHS, surgery accounts for more than 5 million hospital admissions every year.10,11 However, the exact number of surgical procedures that have been cancelled as a result of COVID-19 is unknown. During 2020, there was a phased reintroduction of urgent and elective surgery after the first lockdown. However, this was complicated by increased staff sickness, reduced operating theatre capacity, and lower throughput as a result of enhanced infection control policies. In the meantime, the waiting list for surgical procedures has continued to grow.12 In a previous study, we estimated that more than 2 million surgical procedures would have been cancelled in the NHS in England as a result of the first wave of the pandemic.13 However, this was modelled on previous years' data and anecdotally observed reductions in activity, and not accounting for a second wave of COVID-19 cases and further associated reductions in surgical activity. The true impact of COVID-19 on national surgical activity is, therefore, still unknown. It is crucial that we understand the total number of cancelled surgical procedures, the size of waiting list, and the priority of these cases, so that healthcare leaders and policymakers are able to plan the reintroduction of urgent and elective surgery.
Here, we report the results of a planned analysis of hospital episode data from the NHS in England and Wales. We describe the true national volume of surgical activity that occurred during the first wave of the COVID-19 pandemic and the initial recovery period, and also estimate the likely number of cancelled procedures until the end of 2021.
Methods
Study design and setting
This was a population-based epidemiological study describing all hospital admissions for a surgical procedure in the NHS in England and Wales between January 1, 2020 and December 31, 2020. We used data from January 1, 2016 until December 31, 2019 as a historical comparator period.
Data sources
We used Hospital Episode Statistics for Admitted Patient Care and Patient Episode Database for Wales, which describe every episode of hospital care in NHS in England and Wales, respectively. The NHS-funded treatments performed in the private sector are also captured. The databases include patient characteristics information (age, sex, and ethnicity), process information (dates of admission, start of episode, end of episode, reason for admission, and patient class), and procedural information (recorded using Office of Population Censuses and Surveys classification of interventions and procedures version 4.7 [OPCS-4.7] codes and associated dates).14,15
Data sharing
The data used in this study are derived from two data sources. It is not possible to share the raw patient-level data provided by NHS Digital describing NHS patients in England. Regarding data from NHS patients in Wales, the data used are available in the Secure Anonymised Information Linkage (SAIL) Databank at Swansea University, Swansea, Wales, UK, but as restrictions apply, they are not publicly available. All proposals to use SAIL data are subject to review by an independent Information Governance Review Panel (IGRP). Before any data can be accessed, approval must be given by the IGRP. The IGRP gives careful consideration to each project to ensure proper and appropriate use of SAIL data. When access has been granted, it is gained through a privacy-protecting safe haven and remote access system referred to as the SAIL Gateway. Furthermore, SAIL has established an application process to be followed by anyone who would like to access data via SAIL at https://www.saildatabank.com/application-process.
Study population
All patients, of any age, undergoing surgical procedures in England and Wales in the study period were included. Surgical procedures were defined using a previously published definition of surgery identified using three-character OPCS-4.7 codes (Supplementary Appendix A).10,11
Outcomes
The primary outcome was the number of hospital admissions with an associated surgical procedure.
Data processing
Duplicate episodes were removed and procedures were restricted to primary procedures within each admission episode. This included finished consultant episodes only, which excludes hospital episodes, where a patient remains in hospital, or where data have not yet been submitted to NHS England/NHS Wales. Data were extracted from core data tables in the Data Access Environment (England) and the SAIL Databank (Wales). We selected all hospital episodes associated with defined OPCS-4.7 codes.10,11 We categorised each procedure according to urgency of the surgical procedure using four classes defined by NHS England (Supplementary Appendix B): emergency (required within 72 h), urgent (can be delayed for up to 4 weeks), semi-urgent (can be delayed for up to 3 months), and elective (can be delayed for more than 3 months).6 The OPCS-4.7 contributing to these classes were derived from average waiting times reported between 2014 and 2019, as described previously.16 We aggregated the data by anatomical location, month, and year of the procedure (Supplementary Appendix A).10,13
Statistical analysis
Volume of procedures
Descriptive statistics were used to characterise the volume of procedures performed during the historical comparative period (2016–9) and during 2020.
Estimation of the deficit of surgical volume
The expected monthly frequency of surgical activity from January 1, 2020 to December 31, 2020 was estimated using the surgical activity during the 4 yr before the study period (2016–9). A univariate time-series model that incorporated the monthly count of procedures from 2016 to 2019 was used to independently forecast the total monthly number of procedures and the monthly number of procedures for each of the aforementioned surgical classifications, alongside 95% confidence intervals (CIs). Because of the seasonal variation observed between 2016 and 2019, an exponential smoothing method was used.17
Modelling analysis
We calculated the deficit of surgical procedures up to December 31, 2020 with a 95% CI, based on the difference between the expected and actual number of cases that took place in the year to December 31, 2020. We used a linear regression model to determine the rate of surgical recovery between the first two waves of the pandemic (April to October 2020). We assumed that surgical services would remain disrupted until the end of March 2021, and extrapolated growth from that baseline using the linear model to determine when surgery would reach normal capacity. All data were extracted using Structured Query Language and analysed using IBM SPSS Statistics for Windows (released 2017, version 25.0; IBM Corp., Armonk, NY, USA). Graphs were made using ggplot2 package in R (version 4.0.1; R Core Team, R Foundation, Vienna, Austria). Statistical plans were developed a priori and published in the public domain (https://qmro.qmul.ac.uk/xmlui/handle/123456789/71298).
Research ethics approval
This analysis of routinely collected, pseudonymised data was approved prospectively by the Health Research Authority (20/HRA/3121). Analysis of NHS Wales data was approved by the SAIL independent IGRP project number 0911. Access to NHS England data was approved by the NHS Digital Independent Group Advising on the Release of Data (DARS-NIC-375669-J7M7F).
Public and patient involvement
A patient representative was consulted during the generation of the study concept and methodological design. Patient groups will be used in the dissemination of the study outcomes.
Results
We identified 3 102 674 admissions for a surgical procedure between January 1, 2020 and December 31, 2020 (Supplementary Appendix C). Of these, 2 981 161 (96%) were in England and 121 513 were in Wales (Supplementary Appendix D). The median age was 58 (inter-quartile range [IQR]: 38–73) yr, and 54% of the cohort were female patients.
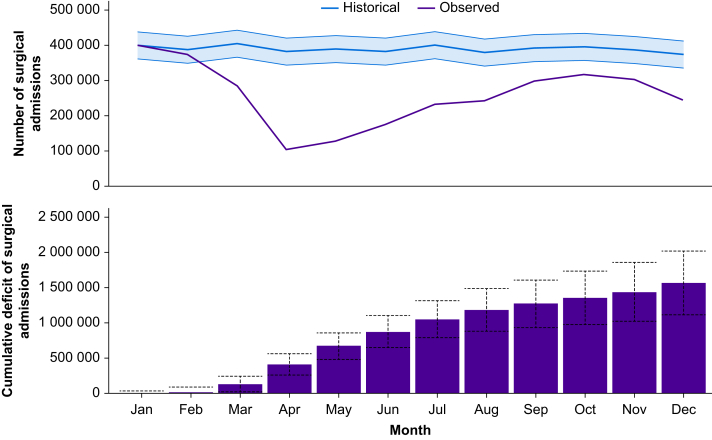
Comparison with the average annual activity, 2016–9
During the historical period (2016–9), there were a median of 4 685 106 admissions for surgery per year (IQR: 4 640 122–4 731 338). There was a median of 392 720.5 admissions per month (IQR: 376 400.3–406 084.3). The number of procedures expected to have been performed during 2020 was 4 671 338 (95% CI: 4 218 740–5 123 932). In 2020, the lowest number of surgical admissions was observed in April with 104 063 (compared with the expected number of 381 153 representing a 72.7% reduction in surgical activity during this month). The number of admissions during the pandemic period compared with the expected number of admissions is presented in Table 1 and Figure 1.
Table 1.
Observed number of procedures vs expected number of procedures. Class 1, emergency surgery within 72 h; Class 2, urgent surgery within 4 weeks; Class 3, semi-urgent surgery within 3 months; Class 4, elective surgery over 3 months. CI, confidence interval.
| Class 1 |
Class 2 |
Class 3 |
Class 4 |
|||||
|---|---|---|---|---|---|---|---|---|
| Observed, N | Percentage of expected (95% CI) | Observed, N | Percentage of expected (95% CI) | Observed, N | Percentage of expected (95% CI) | Observed, N | Percentage of expected (95% CI) | |
| January 2020 | 72 528 | 99.8 (92.6–108.2) | 35 067 | 106 (95.4–119.2) | 216 455 | 101.5 (91.6–113.7) | 75 195 | 98.0 (84.0–117.5) |
| February 2020 | 67 141 | 92.4 (85.7–100.1) | 31 839 | 96.2 (86.6–108.2) | 201 663 | 97.7 (87.9–110.0) | 72 343 | 90.3 (77.9–107.3) |
| March 2020 | 62 355 | 85.8 (79.6–93.0) | 29 629 | 89.5 (80.5–100.7) | 149 742 | 69.5 (62.8–77.8) | 44 496 | 57.3 (49.7–69.5) |
| April 2020 | 48 798 | 67.1 (62.3–72.8) | 16 525 | 49.9 (44.9–56.1) | 37 120 | 18.4 (16.5–20.7) | 1620 | 2.3 (1.9–2.7) |
| May 2020 | 59 597 | 82.0 (76.1–88.9) | 18 012 | 54.4 (48.9–61.2) | 47 274 | 22.9 (20.6–25.8) | 3542 | 4.5 (3.8–5.5) |
| June 2020 | 64 178 | 88.3 (82.0–95.7) | 21 772 | 65.7 (59.1–73.9) | 77 975 | 38.2 (34.4–43.1) | 11 033 | 14.1 (12.0–17.3) |
| July 2020 | 70 633 | 97.2 (90.2–105.3) | 24 988 | 75.4 (67.8–84.8) | 113 141 | 53.2 (48.0–59.6) | 23 619 | 30.3 (25.6–36.9) |
| August 2020 | 68 898 | 94.8 (88.0–102.8) | 23 183 | 69.9 (62.9–78.6) | 118 748 | 59.1 (53.0–66.8) | 31 785 | 40.7 (34.3–49.7) |
| September 2020 | 68 942 | 94.9 (88.0–102.8) | 27 145 | 81.8 (73.6–92.0) | 155 569 | 74.9 (67.5–84.3) | 46 239 | 59.2 (50.1–72.3) |
| October 2020 | 67 314 | 92.6 (86.0–100.4) | 27 933 | 84.1 (75.7–94.7) | 168 026 | 79.4 (71.6–89.1) | 53 518 | 68.6 (58.0–83.7) |
| November 2020 | 62 125 | 85.5 (79.3–92.6) | 27 007 | 81.3 (73.2–91.5) | 164 060 | 79.4 (71.4–89.4) | 50 154 | 64.2 (54.4–78.5) |
| December 2020 | 51 221 | 70.5 (65.4–76.2) | 24 313 | 73.2 (65.8–82.3) | 133 035 | 67.4 (60.4–76.3) | 35 179 | 45.1 (38.2–55.0) |
Fig 1.
Top panel: Surgical activity during 2020 (purple line) compared with expected surgical activity (blue line) based on the years 2016–9 (with 95% confidence intervals [CIs]). Bottom panel: cumulative deficit of surgical procedures throughout 2020 (95% CIs).
Deficit of surgical activity
The total cumulative deficit of hospital admissions for surgical procedures up to December 31, 2020 was 1 568 664 (95% CI: 1 116 066–2 021 258) procedures (Fig. 1). There were 763 730 emergency surgical procedures (13.4% reduction) compared with 2 338 944 elective surgical procedures (38.6% reduction). The majority of this deficit is represented by semi-urgent surgical procedures in Class 3 (904 761 of 1 568 664; 57.7%) and elective surgical procedures in Class 4 (481 150 of 1 568 664; 30.7%) (Table 2).
Table 2.
Monthly and cumulative deficit of number of surgical procedures. Class 1, emergency surgery within 72 h; Class 2, urgent surgery within 4 weeks; Class 3, semi-urgent surgery within 3 months; Class 4, elective surgery over 3 months. Each class was modelled separately, including the 'total' class, to improve model accuracy. The 'total' class cumulative deficit therefore varies slightly from the sum of all the cumulative deficits from all other classes.
| Total |
Class 1 |
Class 2 |
Class 3 |
Class 4 |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Monthly deficit | Cumulative deficit | Monthly deficit | Cumulative deficit | Monthly deficit | Cumulative deficit | Monthly deficit | Cumulative deficit | Monthly deficit | Cumulative deficit | |
| January | 863 | 863 | 150 | 150 | 0 | 0 | 0 | 0 | 1550 | 1550 |
| February | 14 055 | 14 918 | 5537 | 5687 | 1257 | 1257 | 4773 | 4773 | 7811 | 9361 |
| March | 118 492 | 133 410 | 10 323 | 16 010 | 3480 | 4737 | 65 692 | 70 465 | 32 291 | 41 652 |
| April | 277 090 | 410 500 | 23 880 | 39 890 | 16 597 | 21 334 | 165 060 | 235 525 | 70 055 | 111 707 |
| May | 261 176 | 671 676 | 13 081 | 52 971 | 15 123 | 36 457 | 159 167 | 394 692 | 74 522 | 186 229 |
| June | 207 880 | 879 556 | 8500 | 61 471 | 11 376 | 47 833 | 125 974 | 520 666 | 67 031 | 253 260 |
| July | 167 730 | 1 047 286 | 2045 | 63 516 | 8173 | 56 006 | 99 650 | 620 316 | 54 445 | 307 705 |
| August | 137 072 | 1 184 358 | 3780 | 67 296 | 9990 | 65 996 | 82 126 | 702 442 | 46 279 | 353 984 |
| September | 92 131 | 1 276 489 | 3736 | 71 032 | 6041 | 72 037 | 51 997 | 754 439 | 31 825 | 385 809 |
| October | 79 742 | 1 356 231 | 5364 | 76 396 | 5266 | 77 303 | 43 510 | 797 949 | 24 546 | 410 355 |
| November | 83 499 | 1 439 730 | 10 553 | 86 949 | 6205 | 83 508 | 42 533 | 840 482 | 27 910 | 438 265 |
| December | 128 934 | 1 568 664 | 21 457 | 108 406 | 8912 | 92 420 | 64 279 | 904 761 | 42 885 | 481 150 |
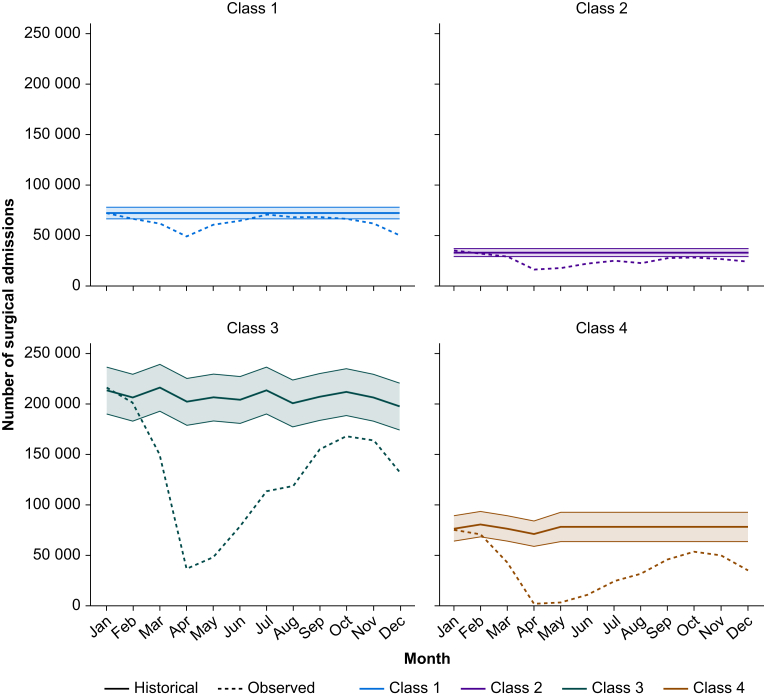
Number of surgical admissions by urgency of procedure
In 2020, the majority of surgical activity was Class 3 (1 582 808 of 3 102 674; 51.0%). The greatest reduction in activity compared with the historical cohort was seen in Class 4 procedures (448 723 of 929 873; a 51.8% reduction). The number of admissions in 2020 compared with the expected number of admissions categorised by class is presented in Table 1 and Figure 2.
Fig 2.
Surgical activity by class for 2020 (dotted line) compared with expected surgical activity and 95% confidence interval (solid line and shading).
Number of surgical admissions by specialty
The number of admissions for surgery in 2020, stratified by anatomical surgical site, is provided in Supplementary Appendix E. The surgical specialty with the biggest reduction in activity in 2020 compared with the historical comparator was oral surgery (48 %).
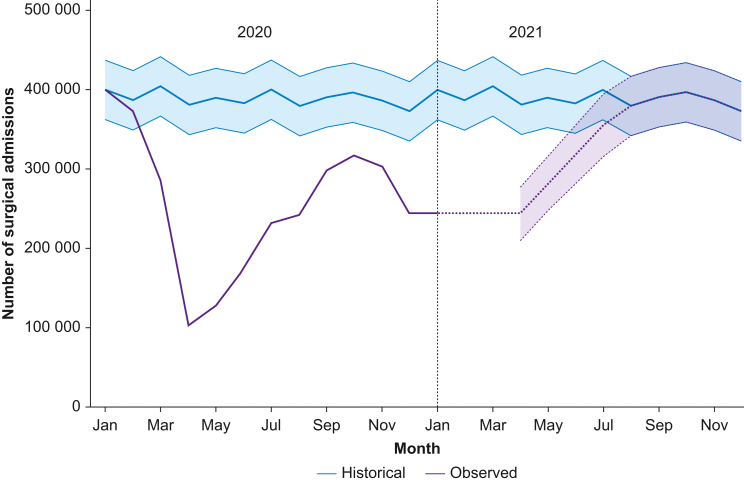
Predicted volume of surgical activity in 2021
If the reintroduction of surgical activity in March 2021 occurs at a similar rate to that observed between the first and second waves of the pandemic (April to October 2020), then surgical care will reach pre-pandemic activity levels by August 2021 (Fig. 3). We estimate a cumulative deficit of 2 384 200 (95% CI: 1 667 587–3 100 808) surgical procedures between January 1, 2020 and December 31, 2021 (Table 3). Based on the median monthly number of procedures performed from 2016 to 2019, this is equivalent to more than 6 months of pre-pandemic surgical activity.
Fig 3.
Predicted surgical activity for 2021 and return to pre-pandemic operative volume.
Table 3.
Modelled number of procedures, monthly deficit, and cumulative deficit in 2021. Data are counts of procedures with associated 95% confidence interval derived from a linear regression model.
| 2021 | Modelled number of procedures | Monthly deficit compared with historical period | Cumulative deficit (2021 only) |
|---|---|---|---|
| January | 243 748 (243 748–243 748) | 156 360 (118 644–194 076) | 156 360 (118 644–194 076) |
| February | 243 748 (243 748–243 748) | 143 293 (105 577–181 010) | 299 653 (224 221–375 086) |
| March | 243 748 (243 748–243 748) | 160 966 (123 249–198 682) | 460 619 (347 470–573 768) |
| April | 243 726 (210 656–276 797) | 137 427 (99 710–175 143) | 598 046 (447 180–748 911) |
| May | 281 040 (246 677–315 402) | 108 561 (70 845–146 278) | 706 607 (518 025–895 189) |
| June | 318 353 (281 817–354 890) | 64 485 (26 769–102 201) | 771 092 (544 794–997 390) |
| July | 355 667 (316 220–395 114) | 44 444 (6727–82 160) | 815 536 (551 521–1 079 550) |
| August | 379 686 (341 969–417 402) | 0 (0–0) | 815 536 (551 521–1 079 550) |
| September | 390 026 (352 309–427 742) | 0 (0–0) | 815 536 (551 521–1 079 550) |
| October | 396 533 (358 817–434 249) | 0 (0–0) | 815 536 (551 521–1 079 550) |
| November | 386 845 (349 129–424 561) | 0 (0–0) | 815 536 (551 521–1 079 550) |
| December | 372 682 (334 965–410 398) | 0 (0–0) | 815 536 (551 521–1 079 550) |
Discussion
The principal finding of this observational study is that the overall volume of surgical activity in England and Wales in 2020 was 33.6% lower than expected levels. This represents the cancellation or postponement of more than 1.5 million surgical procedures. The vast majority of the deficit of procedures is accounted for by semi-urgent and elective surgery (38.6%). However, there was a substantial reduction in the frequency of emergency surgery (13.4%), which has not yet returned to a pre-pandemic baseline. This may be because of a reduction in emergency surgical presentations, for example, fewer injuries requiring surgery because of lockdowns; it may represent an inflation of emergency case numbers before the pandemic (i.e. operations that were not true emergencies) or clinical management using non-surgical treatment (i.e. conservative or medical therapy). We predict that by the end of 2021, there will be 2.4 million surgical procedures outstanding, representing more than 6 months of normal surgical activity.
Perioperative clinicians in the UK and worldwide will be familiar with changes to working patterns, reductions in operating theatre capacity, and increasing waiting lists for surgery.5,18 Several research groups have estimated the volume of cancelled surgical procedures.8,13,19 However, this is the first study, to our knowledge, to describe the impact of the COVID-19 pandemic on the volume of surgical activity at the level of national health systems. Our data represent the true reduction in surgical workload that occurred during the first wave of the pandemic in England and Wales, and the subsequent (incomplete) recovery of surgical services. In the early phase of the pandemic, there was a necessary trade-off between care of a large volume of patients with acute respiratory disease, many of whom required intensive care treatments, and continuation of services to treat surgical disease. This led to the almost complete cessation of all but the most emergent surgical treatment. The reintroduction of surgery after the first wave of the pandemic was complicated by several factors: first, concerns about the high risk of perioperative mortality amongst surgical patients with concomitant COVID-19 and the postponement of surgery on clinical grounds18,20; second, reduced availability of physical and human resources as a result of ongoing care of patients with COVID-19, which limited the capacity of surgical services21; and third, reduced throughput of surgery as a result of new infection control procedures to prevent nosocomial infection and to protect staff members. The consequences of the observed interruption to surgical treatment will be felt by millions of patients for many years to come. Delays in the diagnosis and the surgical management of cancer will undoubtedly lead to an increase in cancer-related mortality.22 For many patients waiting for semi-urgent and elective surgery, there is likely to be a worsening of their condition while waiting for surgery, which could make future treatment more difficult and less likely to succeed.23 Furthermore, these patients are likely to suffer worsening of their physical and mental health whilst while on the waiting list, placing additional burdens on primary and social care, reducing their productivity in the workplace.24 This represents a huge financial and human cost to society.
Dealing with the backlog of surgery will be a challenge to many health systems worldwide.25 We have previously demonstrated that ‘green pathway’ operating (in which elective patients are preoperatively screened for COVID-19, isolated in the preoperative period, and kept separate from acute admissions) is safe, with similar perioperative mortality amongst patients on green pathways compared with before the pandemic.20 Consequently, surgery should not be delayed or prevented if safeguards are put in place. However, this will require significant reorganisation of surgical services and financial commitment from central government. Green pathway operating will need dedicated space and staff to ensure safety, with routine COVID-19 testing for patients and staff. With limited personnel and physical resources, it may take many years of concerted effort to clear the backlog of surgery as a result of COVID-19. In the rush to limit harm to surgical patients and restart elective surgery as soon as possible, staff welfare should not be neglected. A high proportion of healthcare workers have experienced burn-out over the last year, and adequate time for staff recovery should be incorporated into any plan to tackle the waiting list for surgery.26 Asking staff that are already tired to work harder for longer periods of time may not be a sustainable solution to this problem.
This study has several strengths. We included data from all patients undergoing surgery in England and Wales during the first wave of the COVID-19 pandemic; thus, our results represent the true volume of surgery being performed. We included data from 2.5 million surgical patients, which represent one of the largest observational cohorts of surgical patients during the COVID-19 pandemic. A pre-pandemic cohort of more than 10 million patients was used to accurately identify the expected usual surgical activity within the NHS for comparison. Official routine data collection is also less open to bias, which can affect other data collection methods, such as clinician surveys. Furthermore, these data will be generalisable to other high-income countries, where similar reductions in surgical activity have been reported.27 The pandemic cohort time period was chosen for a number of reasons. Although the NHS response to COVID-19 began in early March 2020, there is evidence of community transmission within the UK before this.28 Furthermore, it is important that the winter months (January, February, and March) were included in this analysis, as operating volume is traditionally reduced because of other illnesses at this time of year. Our cohort cut-off of December 31, 2020 allowed us to analyse the first wave and subsequent recovery, leading into the second wave of the pandemic, whilst still allowing for data to feed through to national databases and be analysed in a timely manner. This study also has limitations. As with any population-based study using routinely collected data, there is the risk of incomplete or missing data, although from previous work, this is likely to be negligible in this setting. Furthermore, the second peak of the pandemic did not occur until February 2021 in the UK, so it is likely that surgical activity continued to decline after December. We deliberately took a conservative approach in our modelling by assuming December was the nadir of surgical activity after April 2020. We, however, accept that our total deficit in December 2021 is based on a number of assumptions used in our model, and therefore, the true number may be significantly different. Accurately predicting the impact of future waves is challenging because of the unknown impact of many issues, including the uptake and longer-term effectiveness of vaccines and future viral variants. Finally, these results might be less applicable to privately funded healthcare systems, where anecdotally privately funded surgery continued at more normal levels during the pandemic.
Conclusions
This study is the first to provide operational detail on surgical activity during the COVID-19 pandemic for an entire healthcare system. The volume of surgical activity in England and Wales in 2020 was 33.6% lower than historical data. More than 1.5 million surgical procedures have been cancelled as a result of COVID-19, and we predict that the deficit will increase to 2.4 million by the end of 2021. It is imperative that surgical patients are not the forgotten casualties of the pandemic. Further work must aim to identify ways to improve utilisation of all available capacity for surgical activity, with commitments by governments to make financing this work a priority.
Authors' contributions
Study design: TEA, TDD, AJF, RMP
Data collection: JAGG, AJF, FT, RG, RAL
Data analysis: JAGG, AJF
Data interpretation: TDD, TEA, JAGG, AJF
Writing of first draft of paper: TDD, TEA
Revising of paper for important intellectual content: all authors
Approval of final version: all authors
AJF and JAGG had full access to the data and act as guarantors.
Acknowledgements
This work used data provided by patients and collected by the NHS as part of their care and support. The authors would like to acknowledge all data providers, who make anonymised data available for research, and the collaborative partnership that enabled acquisition and access to the de-identified data, which led to this output. The collaboration was led by the Swansea University Health Data Research UK team under the direction of the Welsh Government Technical Advisory Cell, and includes the following groups and organisations: the Secure Anonymised Information Linkage (SAIL) Databank, Administrative Data Research Wales, NHS Wales Informatics Service, Public Health Wales, NHS Shared Services, and the Welsh Ambulance Service NHS Trust. All research conducted has been completed under the permission and approval of the SAIL independent Information Governance Review Panel project number 0911. The Welsh data source was supported by Health Data Research UK, which receives its funding from HDR UK Ltd (HDR-9006) funded by the UK Medical Research Council, Engineering and Physical Sciences Research Council, Economic and Social Research Council, Department of Health and Social Care (England), Chief Scientist Office of the Scottish Government Health and Social Care Directorates, Health and Social Care Research and Development Division (Welsh Government), Public Health Agency (Northern Ireland), British Heart Foundation, and the Wellcome Trust. The funding sources had no role in the study design, data collection, analysis, interpretation, or writing of this paper.
Handling editor: Paul Myles
Footnotes
This article is accompanied by an editorial: COVID 19 and the challenges of the surgery backlog: the greatest healthcare innovation would be to do what we know by Monty G. Mythen, Br J Anaesth 2021:127:192–195, doi: 10.1016/j.bja.2021.05.021
Supplementary data to this article can be found online at https://doi.org/10.1016/j.bja.2021.05.001.
Declarations of interest
AJF holds a National Institute for Health Research Doctoral Research Fellowship (DRF-2018-11-ST2-062). TDD reports funding from the Welsh Clinical Academic Training Fellowship. ISW is the surgical Specialty Lead for Health and Care Research Wales, and reports active grants from the American Association of Plastic Surgeons and the European Association of Plastic Surgeons. ISW is an editor for Frontiers in Surgery, associate editor for the Annals of Plastic Surgery, and editorial board of BMC Medicine, and has numerous other editorial board roles. RMP has received honoraria or research grants from Edwards Lifesciences, Intersurgical, and GlaxoSmithKline within the last 5 yr, and holds editorial roles with the British Journal of Anaesthesia, the British Journal of Surgery, and BMJ Quality & Safety. TEA is a member of the associate editorial board of the British Journal of Anaesthesia and has received consultancy fees from MSD unrelated to this work. All other authors report no financial relationships with any organisations that might have an interest in the submitted work in the previous 3 yr, and no other relationships or activities that could appear to have influenced the submitted work.
Funding
Barts Charity (MGU0545); Medical Research Council (MR/V028367/1)
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Morris E.J.A., Goldacre R., Spata E. Impact of the COVID-19 pandemic on the detection and management of colorectal cancer in England: a population-based study. Lancet Gastroenterol Hepatol. 2021;6:199–208. doi: 10.1016/S2468-1253(21)00005-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Flint S.W., Brown A., Tahrani A.A., Piotrkowicz A., Joseph A.C. Cross-sectional analysis to explore the awareness, attitudes and actions of UK adults at high risk of severe illness from COVID-19. BMJ Open. 2020;10 doi: 10.1136/bmjopen-2020-045309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Soreide K., Hallet J., Matthews J.B. Immediate and long-term impact of the COVID-19 pandemic on delivery of surgical services. Br J Surg. 2020;107:1250–1261. doi: 10.1002/bjs.11670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abu Hilal M., Besselink M.G., Lemmers D.H.L., Taylor M.A., Triboldi A. Early look at the future of healthcare during the COVID-19 pandemic. Br J Surg. 2020;107:e197. doi: 10.1002/bjs.11666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.COVIDSurg Collaborative Global guidance for surgical care during the COVID-19 pandemic. Br J Surg. 2020;107:1097–1103. doi: 10.1002/bjs.11646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Royal College of Surgeons of England . 2020. Clinical guide to surgical prioritisation during the coronavirus pandemic.https://www.rcseng.ac.uk/coronavirus/surgical-prioritisation-guidance/ Available from: [Google Scholar]
- 7.Spinelli A., Pellino G. COVID-19 pandemic: perspectives on an unfolding crisis. Br J Surg. 2020;107:785–787. doi: 10.1002/bjs.11627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.CovidSurg Collaborative Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg. 2020;107:1440–1449. doi: 10.1002/bjs.11746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weiser T.G., Haynes A.B., Molina G. Estimate of the global volume of surgery in 2012: an assessment supporting improved health outcomes. Lancet. 2015;385:S11. doi: 10.1016/S0140-6736(15)60806-6. [DOI] [PubMed] [Google Scholar]
- 10.Abbott T.E.F., Fowler A.J., Dobbs T.D., Harrison E.M., Gillies M.A., Pearse R.M. Frequency of surgical treatment and related hospital procedures in the UK: a national ecological study using hospital episode statistics. Br J Anaesth. 2017;119:249–257. doi: 10.1093/bja/aex137. [DOI] [PubMed] [Google Scholar]
- 11.Fowler A.J., Abbott T.E.F., Prowle J., Pearse R.M. Age of patients undergoing surgery. Br J Surg. 2019;106:1012–1018. doi: 10.1002/bjs.11148. [DOI] [PubMed] [Google Scholar]
- 12.Griffin S. Covid-19: waiting times in England reach record highs. BMJ. 2020;370:m3557. doi: 10.1136/bmj.m3557. [DOI] [PubMed] [Google Scholar]
- 13.Fowler A.J., Dobbs T.D., Wan Y.I. Estimated surgical requirements in England after COVID-19: a modelling study using hospital episode statistics. Br J Surg. 2021 Jan 27;108:97–103. doi: 10.1093/bjs/znaa012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.NHS . 2020. OPCS classification of interventions and procedures. NHS Model and data dictionary.https://datadictionary.nhs.uk/supporting_information/opcs_classification_of_interventions_and_procedures.html Available from: [Google Scholar]
- 15.Herbert A., Wijlaars L., Zylbersztejn A., Cromwell D., Hardelid P. Data resource profile: hospital episode statistics admitted patient care (HES APC) Int J Epidemiol. 2017;46 doi: 10.1093/ije/dyx015. 1093-i. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fowler A.J., Dobbs T.D., Wan Y.I. Resource requirements for reintroducing elective surgery during the COVID-19 pandemic: modelling study. Br J Surg. 2020;108:97–103. doi: 10.1093/bjs/znaa012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Soyiri I.N., Reidpath D.D. An overview of health forecasting. Environ Health Prev Med. 2013;18:1–9. doi: 10.1007/s12199-012-0294-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.COVIDSurg Collaborative Delaying surgery for patients with a previous SARS-CoV-2 infection. Br J Surg. 2020;107:e601–e602. doi: 10.1002/bjs.12050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.CRC COVID Research Collaborative Colorectal cancer services during the COVID-19 pandemic. Br J Surg. 2020;107:e255–e256. doi: 10.1002/bjs.11706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abbott T.F., Fowler A.J., Dobbs T.D. Mortality after surgery with SARS-CoV-2 infection in England: a population-wide epidemiological study. medrxiv. 2021 doi: 10.1101/2021.02.17.21251928. Preprint published on February 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fowler A., Abbott T.E.F., Pearse R.M. Can we safely continue to offer surgical treatments during the COVID-19 pandemic? BMJ Qual Saf. 2021 Apr;30:268–270. doi: 10.1136/bmjqs-2020-01254. [DOI] [PubMed] [Google Scholar]
- 22.Maringe C., Spicer J., Morris M. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncol. 2020;21:1023–1034. doi: 10.1016/S1470-2045(20)30388-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wijeysundera D.N., Pearse R.M., Shulman M.A. Assessment of functional capacity before major non-cardiac surgery: an international, prospective cohort study. Lancet. 2018;391:2631–2640. doi: 10.1016/S0140-6736(18)31131-0. [DOI] [PubMed] [Google Scholar]
- 24.Wan Y.I., McGuckin D., Fowler A.J., Prowle J.R., Pearse R.M., Moonesinghe S.R. Socioeconomic deprivation and long-term outcomes after elective surgery: analysis of prospective data from two observational studies. Br J Anaesth. 2021;126:642–651. doi: 10.1016/j.bja.2020.10.019. [DOI] [PubMed] [Google Scholar]
- 25.Mayol J., Fernandez Perez C. Elective surgery after the pandemic: waves beyond the horizon. Br J Surg. 2020;107:1091–1093. doi: 10.1002/bjs.11688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tan Y.Q., Wang Z., Yap Q.V. Psychological health of surgeons in a time of COVID-19: a global survey. Ann Surg. 2021 doi: 10.1097/SLA.0000000000004775. Online ahead of print published on January 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bedard N.A., Elkins J.M., Brown T.S. Effect of COVID-19 on hip and knee arthroplasty surgical volume in the United States. J Arthroplasty. 2020;35:S45–S48. doi: 10.1016/j.arth.2020.04.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Scally G., Jacobson B., Abbasi K. The UK’s public health response to covid-19. BMJ. 2020;369:m1932. doi: 10.1136/bmj.m1932. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.