Abstract
University administrators and mental health clinicians have raised concerns about depression and anxiety among Ph.D. students, yet no study has systematically synthesized the available evidence in this area. After searching the literature for studies reporting on depression, anxiety, and/or suicidal ideation among Ph.D. students, we included 32 articles. Among 16 studies reporting the prevalence of clinically significant symptoms of depression across 23,469 Ph.D. students, the pooled estimate of the proportion of students with depression was 0.24 (95% confidence interval [CI], 0.18–0.31; I2 = 98.75%). In a meta-analysis of the nine studies reporting the prevalence of clinically significant symptoms of anxiety across 15,626 students, the estimated proportion of students with anxiety was 0.17 (95% CI, 0.12–0.23; I2 = 98.05%). We conclude that depression and anxiety are highly prevalent among Ph.D. students. Data limitations precluded our ability to obtain a pooled estimate of suicidal ideation prevalence. Programs that systematically monitor and promote the mental health of Ph.D. students are urgently needed.
Subject terms: Epidemiology, Anxiety, Depression, Health policy, Quality of life
Introduction
Mental health problems among graduate students in doctoral degree programs have received increasing attention1–4. Ph.D. students (and students completing equivalent degrees, such as the Sc.D.) face training periods of unpredictable duration, financial insecurity and food insecurity, competitive markets for tenure-track positions, and unsparing publishing and funding models5–12—all of which may have greater adverse impacts on students from marginalized and underrepresented populations13–15. Ph.D. students’ mental health problems may negatively affect their physical health16, interpersonal relationships17, academic output, and work performance18,19, and may also contribute to program attrition20–22. As many as 30 to 50% of Ph.D. students drop out of their programs, depending on the country and discipline23–27. Further, while mental health problems among Ph.D. students raise concerns for the wellbeing of the individuals themselves and their personal networks, they also have broader repercussions for their institutions and academia as a whole22.
Despite the potential public health significance of this problem, most evidence syntheses on student mental health have focused on undergraduate students28,29 or graduate students in professional degree programs (e.g., medical students)30. In non-systematic summaries, estimates of the prevalence of clinically significant depressive symptoms among Ph.D. students vary considerably31–33. Reliable estimates of depression and other mental health problems among Ph.D. students are needed to inform preventive, screening, or treatment efforts. To address this gap in the literature, we conducted a systematic review and meta-analysis to explore patterns of depression, anxiety, and suicidal ideation among Ph.D. students.
Results
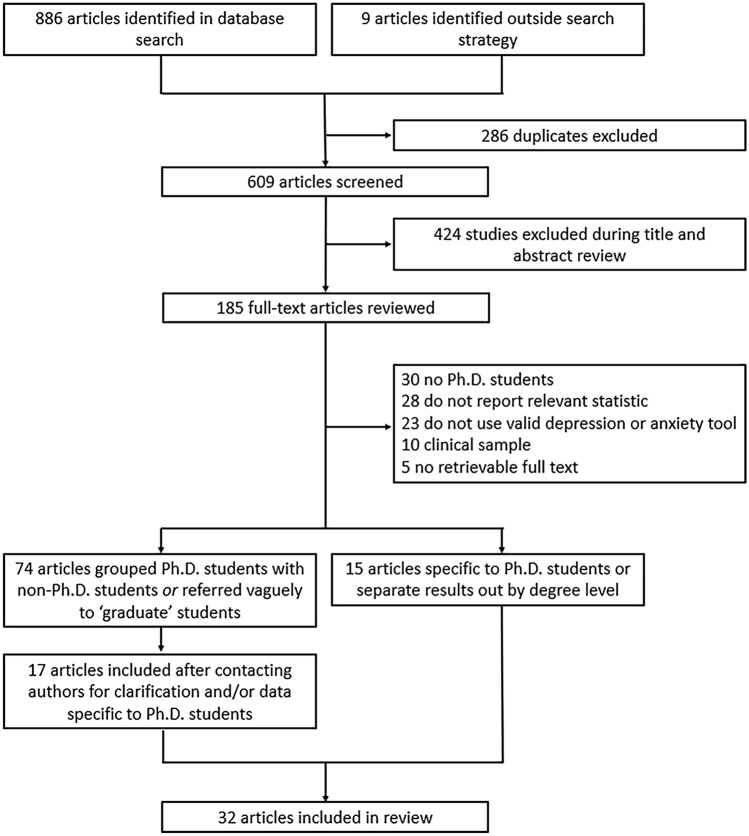
The evidence search yielded 886 articles, of which 286 were excluded as duplicates (Fig. 1). An additional nine articles were identified through reference lists or grey literature reports published on university websites. Following a title/abstract review and subsequent full-text review, 520 additional articles were excluded.
Figure 1.
Flowchart of included articles.
Of the 89 remaining articles, 74 were unclear about their definition of graduate students or grouped Ph.D. and non-Ph.D. students without disaggregating the estimates by degree level. We obtained contact information for the authors of most of these articles (69 [93%]), requesting additional data. Three authors clarified that their study samples only included Ph.D. students34–36. Fourteen authors confirmed that their study samples included both Ph.D. and non-Ph.D. students but provided us with data on the subsample of Ph.D. students37–50. Where authors clarified that the sample was limited to graduate students in non-doctoral degree programs, did not provide additional data on the subsample of Ph.D. students, or did not reply to our information requests, we excluded the studies due to insufficient information (Supplementary Table S1).
Ultimately, 32 articles describing the findings of 29 unique studies were identified and included in the review16,32–48,50–62 (Table 1). Overall, 26 studies measured depression, 19 studies measured anxiety, and six studies measured suicidal ideation. Three pairs of articles reported data on the same sample of Ph.D. students33,38,45,51,53,56 and were therefore grouped in Table 1 and reported as three studies. Publication dates ranged from 1979 to 2019, but most articles (22/32 [69%]) were published after 2015. Most studies were conducted in the United States (20/29 [69%]), with additional studies conducted in Australia, Belgium, China, Iran, Mexico, and South Korea. Two studies were conducted in cross-national settings representing 48 additional countries. None were conducted in sub-Saharan Africa or South America. Most studies included students completing their degrees in a mix of disciplines (17/29 [59%]), while 12 studies were limited to students in a specific field (e.g., biomedicine, education). The median sample size was 172 students (interquartile range [IQR], 68–654; range, 6–6405). Seven studies focused on mental health outcomes in demographic subgroups, including ethnic or racialized minority students37,41,43, international students47,50, and sexual and gender minority students42,54.
Table 1.
Summary of included articles.
| Author, Year | Country | Sample size (% Female) | Field | Depression | Anxiety | Suicidal ideation | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Scale (threshold and time frame) | Frequency (prevalence) | Mean (SD) | Scale (threshold and timeframe) | Frequency (prevalence) | Mean (SD) | Scale (timeframe) | Frequency (Prevalence) | Mean (SD) | ||||
| Bolotnyy, et al. 52 | USA | 513 (34.70%) | Economics | PHQ-9 (≥ 10, past 2 weeks) | 91 (17.74%) | NA | GAD-7 (≥ 10, past 2 weeks) | 90 (17.60%) | NA |
PHQ-9 (past 2 weeks) SBQR (past year) |
58 (11.30%) 61 (12.00%) |
NA |
| Baker and Chambers 44** | USA | 6 (100%) | Social Work | CES-D (≥ 16, past week) | 3 (50.00%) | NA | NA | NA | NA | NA | NA | NA |
|
Barry, et al. 53 Barry, et al. 51a a Reported a sample size of 82; adjusted scores are presented |
Australia |
81 (81.48%) 82 (81.71%) |
Mixed | DASS-42 (past week) | NA |
6.70 (6.00) 6.71 (5.98) |
DASS-42 (past week) | NA |
5.80 (6.90) 5.82 (6.92) |
NA | NA | NA |
| Boyle and McKinzie 54 | USA | 632 (NA) | Mixed | DASS-28 (past week) | NA | 5.97 (6.86) | DASS-28 (past week) | NA | 4.34 (5.65) | NA | NA | NA |
| Clark, et al. 37** | USA | 172 (NA) | School Psychology | BSI (past week) | NA | 1.51 (0.60) | BSI (past week) | NA | 1.47 (0.68) | NA | NA | NA |
| Corral-Frias, et al. 49** | Mexico | 7 (NA) | Mixed | MASQ-SF (past week) | NA | 20.00 (8.79) | MASQ-SF (past week) | NA | 20.00 (7.77) | NA | NA | NA |
|
Eisenberg, et al. 38** Golberstein, et al. 45a a Smaller overall sample size due to missing data |
USA | 654 (NA) | Mixed | PHQ-9 (≥ 10, past 2 weeks) | 91 (13.91%) | NA | PHQ GAD (past 4 weeks) | 25 (3.82%) | NA |
NCS-R (past 4 weeks) NCS-R (past 4 weeks – plan) |
11 (1.67%) 2 (0.30%) |
NA |
| Farrer, et al. 39** | Australia | 118 (NA) | Mixed | PHQ-9 (≥ 10, past 2 weeks) | 13 (11.02%) | 5.71 (4.46) | GAD-7 (≥ 10, past 2 weeks) | 10 (8.47%) | 3.79 (4.23) | NA | NA | NA |
| Garcia-Williams, et al. 34* | USA | 301 (77.08%) | Mixed | PHQ-9 (≥ 10, past 2 weeks) | 101 (33.55%) | 7.95 (5.16) | NA | NA | NA | 3-item measure (past 2 weeks) | 22 (7.31%) | NA |
| 3-item measure (lifetime—attempt) | 30 (9.97%) | |||||||||||
| Heinrich 55 | USA | 68 (NA) | Education | NA | NA | NA | STAI-trait (present) | NA | 33.43 (6.86) | NA | NA | NA |
| Hindman, et al. 46** | USA | 6 (100.00%) | Mixed | DASS-21 (past week) | NA | 3.00 (2.76) | DASS-21 (past week) | NA | 2.67 (2.42) | NA | NA | NA |
| Hirai, et al. 47** | USA | 46 (NA) | Mixed | DASS-21 (past week) | NA | 0.48 (0.59) | DASS-21 (past week) | NA | 0.45 (0.45) | NA | NA | NA |
|
Hish, et al. 56 Nagy, et al. 33 |
USA | 69 (60.87%) | Biomedicine | PHQ-9 (≥ 10, past 2 weeks) | 7 (10.14%) | 4.64 (4.84) | SCID-5-RV (past year) | 22 (31.88%) | NA | NA | NA | NA |
| Jamshidi, et al. 57 | Iran | 280 (NA) | Medical Sciences | GHQ-28 (past few weeks) | NA | 2.56 (4.07) | GHQ-28 (past few weeks) | NA | 4.43 (4.05) | NA | NA | NA |
| Lee and Jeong 48** | South Korea | 1,809 (NA) | Mixed | BDI (past week) | NA | 4.52 (5.15) | NA | NA | NA | NA | NA | NA |
| Levecque, et al. 32 | Belgium | 3,659 (52.01%) | Mixed | GHQ-12 (≥ 4, past few weeks) | 1,165 (31.84%) | NA | NA | NA | NA | NA | NA | NA |
| Lightstone, et al. 36* | USA | 116 (77.59%) | Medicine and Psychology | NA | NA | NA | STAI-trait (present) | NA | 38.19 (7.87) | NA | NA | NA |
| Lilly, et al. 41** | USA | 42 (NA) | Biomedicine | PHQ-2 (past 2 weeks) | 3 (7.14%) | NA | NA | NA | NA | NA | NA | NA |
|
Lipson, et al. 40** Lipson, et al. 43** Lipson, et al. 42**a aDue to some overlap in survey years across studies, data pooled (2007–2017) |
USA | Total: 13,912 (55.44%) | Mixed | PHQ-9 (≥ 10, past 2 weeks) | Total: 2377/13,912 (17.09%) | Total: 5.83 (4.89) |
2007–2012: PHQ GAD (past 4 weeks) 2013–2017: GAD-7 (≥ 10, past 2 weeks) |
2007–2012: 326/4,111 (7.93%) 2013–2017: 1,633/9,717 (16.81%) |
2007–2012: NA 2013–2017: 5.12 (4.72) |
Single-item (past year) | Total: 759/13,660 (5.56%) | NA |
| Liu, et al. 58 | China | 325 (60.31%) | Medicine | PHQ-9 (≥ 10, past 2 weeks) | 77 (23.70%) | NA | GAD-7 (≥ 10, past 2 weeks) | 65 (20.00%) | NA | NA | NA | NA |
| Meghani and Harvey 50 | USA | 32 (NA) | Mixed | Boston X 4 CES-D (≥ 10, past week) | 7 (21.88%) | 6.43 (5.66) | NA | NA | NA | NA | NA | NA |
| Richardson, et al. 62 | USA | 119 (85.71%) | Clinical and Counseling Psychology | IDAS-II (past 2 weeks) | NA | 46.09 (14.23) | NA | NA | NA | NA | NA | NA |
| Rummell 16 | Canada & USA | 119 (77.31%) | Clinical and Counseling Psychology | 35-item scale derived from DSM-5 (past 2 weeks) | 47 (39.29%) | NA | DSM-5 (past 2 weeks) | 58 (49.11%) | NA | NA | NA | NA |
| Sheldon 35* | USA | 35 (42.86%) | Physics and Ecology | NA | NA | NA | BSI (past week) | NA | 0.67 (NA) | NA | NA | NA |
| Sverdlik and Hall 59 | 54 Countries | 3,004 (79.36%) | Mixed | CES-D-10 (past week) | NA | 23.31 (4.53) | NA | NA | NA | NA | NA | NA |
| The Graduate Assembly 61 | USA | 529 (NA) | Mixed | CES-D (≥ 16, past week) | 249 (47.07%) | NA | NA | NA | NA | NA | NA | NA |
| University of California Office of the President 60 | USA | 3,190 (NA) | Mixed | CES-D-R (≥ 16, past 2 weeks) | 1,215 (38.09%) | NA | NA | NA | NA | NA | NA | NA |
Beck Depression Inventory (BDI), Brief Symptom Inventory (BSI), Center for Epidemiologic Studies–Depression (CES-D), Center for Epidemiologic Studies–Depression–Revised (CES-D-R), Depression Anxiety and Stress Subscales (DASS), Diagnostic and Statistical Manual (DSM), Generalized Anxiety Disorder (GAD), General Health Questionnaire (GHQ), Inventory of Depression and Anxiety Symptoms–Second Version (IDAS-II), Mood and Anxiety Symptom Questionnaire–Short Form (MASQ-SF), National Comorbidity Survey Replication, (NCS-R), Patient Health Questionnaire (PHQ), Suicide Behaviors Questionnaire-Revised (SBQR), State-Trait Anxiety Inventory (STAI), standard deviation (SD), Structured Clinical Interview for DSM-5 Axis I Disorders Research Version (SCID-5-RV).
*Author provided clarification—entire sample consisted of doctoral degree students.
**Author provided additional data—doctoral students reflect a subsample of the total number reported in the published article.
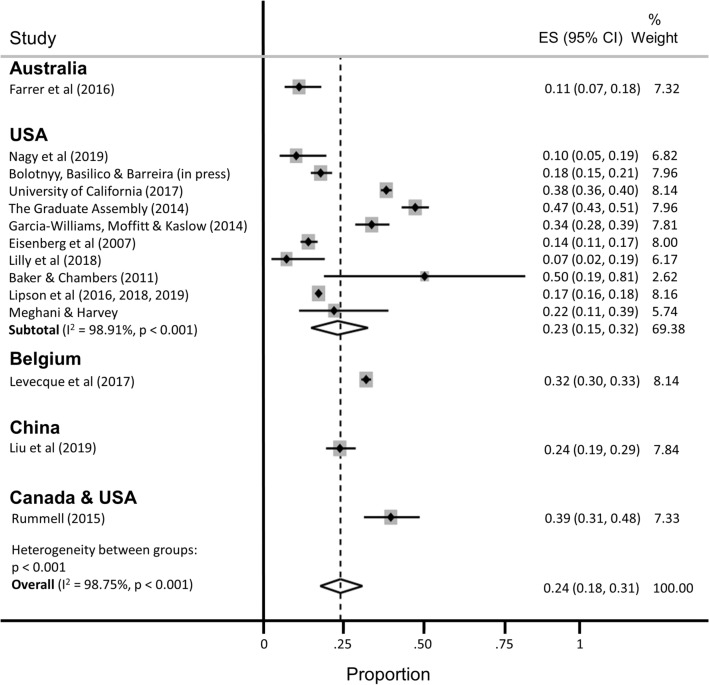
In all, 16 studies reported the prevalence of depression among a total of 23,469 Ph.D. students (Fig. 2; range, 10–47%). Of these, the most widely used depression scales were the PHQ-9 (9 studies) and variants of the Center for Epidemiologic Studies-Depression scale (CES-D, 4 studies)63, and all studies assessed clinically significant symptoms of depression over the past one to two weeks. Three of these studies reported findings based on data from different survey years of the same parent study (the Healthy Minds Study)40,42,43, but due to overlap in the survey years reported across articles, these data were pooled. Most of these studies were based on data collected through online surveys (13/16 [81%]). Ten studies (63%) used random or systematic sampling, four studies (25%) used convenience sampling, and two studies (13%) used multiple sampling techniques.
Figure 2.
Pooled estimate of the proportion of Ph.D. students with clinically significant symptoms of depression.
The estimated proportion of Ph.D. students assessed as having clinically significant symptoms of depression was 0.24 (95% confidence interval [CI], 0.18–0.31; 95% predictive interval [PI], 0.04–0.54), with significant evidence of between-study heterogeneity (I2 = 98.75%). A subgroup analysis restricted to the twelve studies conducted in the United States yielded similar findings (pooled estimate [ES] = 0.23; 95% CI, 0.15–0.32; 95% PI, 0.01–0.60), with no appreciable difference in heterogeneity (I2 = 98.91%). A subgroup analysis restricted to the studies that used the PHQ-9 to assess depression yielded a slightly lower prevalence estimate and a slight reduction in heterogeneity (ES = 0.18; 95% CI, 0.14–0.22; 95% PI, 0.07–0.34; I2 = 90.59%).
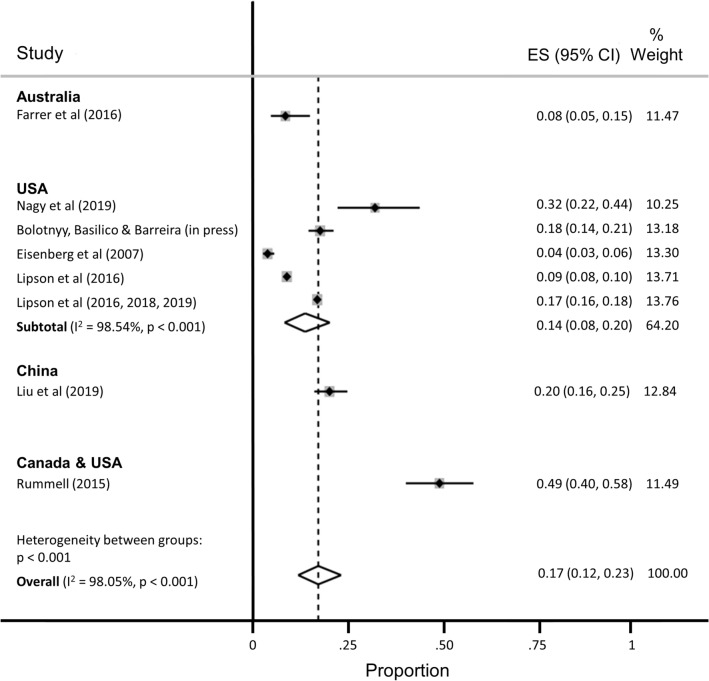
Nine studies reported the prevalence of clinically significant symptoms of anxiety among a total of 15,626 Ph.D. students (Fig. 3; range 4–49%). Of these, the most widely used anxiety scale was the 7-item Generalized Anxiety Disorder scale (GAD-7, 5 studies)64. Data from three of the Healthy Minds Study articles were pooled into two estimates, because the scale used to measure anxiety changed midway through the parent study (i.e., the Patient Health Questionnaire-Generalized Anxiety Disorder [PHQ-GAD] scale was used from 2007 to 2012 and then switched to the GAD-7 in 201340). Most studies (8/9 [89%]) assessed clinically significant symptoms of anxiety over the past two to four weeks, with the one remaining study measuring anxiety over the past year. Again, most of these studies were based on data collected through online surveys (7/9 [78%]). Five studies (56%) used random or systematic sampling, two studies (22%) used convenience sampling, and two studies (22%) used multiple sampling techniques.
Figure 3.
Pooled estimate of the proportion of Ph.D. students with clinically significant symptoms of anxiety.
The estimated proportion of Ph.D. students assessed as having anxiety was 0.17 (95% CI, 0.12–0.23; 95% PI, 0.02–0.41), with significant evidence of between-study heterogeneity (I2 = 98.05%). The subgroup analysis restricted to the five studies conducted in the United States yielded a slightly lower proportion of students assessed as having anxiety (ES = 0.14; 95% CI, 0.08–0.20; 95% PI, 0.00–0.43), with no appreciable difference in heterogeneity (I2 = 98.54%).
Six studies reported the prevalence of suicidal ideation (range, 2–12%), but the recall windows varied greatly (e.g., ideation within the past 2 weeks vs. past year), precluding pooled estimation.
Additional stratified pooled estimates could not be obtained. One study of Ph.D. students across 54 countries found that phase of study was a significant moderator of mental health, with students in the comprehensive examination and dissertation phases more likely to experience distress compared with students primarily engaged in coursework59. Other studies identified a higher prevalence of mental ill-health among women54; lesbian, gay, bisexual, transgender, and queer (LGBTQ) students42,54,60; and students with multiple intersecting identities54.
Several studies identified correlates of mental health problems including: project- and supervisor-related issues, stress about productivity, and self-doubt53,62; uncertain career prospects, poor living conditions, financial stressors, lack of sleep, feeling devalued, social isolation, and advisor relationships61; financial challenges38; difficulties with work-life balance58; and feelings of isolation and loneliness52. Despite these challenges, help-seeking appeared to be limited, with only about one-quarter of Ph.D. students reporting mental health problems also reporting that they were receiving treatment40,52.
Risk of bias
Twenty-one of 32 articles were assessed as having low risk of bias (Supplementary Table S2). Five articles received one point for all five categories on the risk of bias assessment (lowest risk of bias), and one article received no points (highest risk). The mean risk of bias score was 3.22 (standard deviation, 1.34; median, 4; IQR, 2–4). Restricting the estimation sample to 12 studies assessed as having low risk of bias, the estimated proportion of Ph.D. students with depression was 0.25 (95% CI, 0.18–0.33; 95% PI, 0.04–0.57; I2 = 99.11%), nearly identical to the primary estimate, with no reduction in heterogeneity. The estimated proportion of Ph.D. students with anxiety, among the 7 studies assessed as having low risk of bias, was 0.12 (95% CI, 0.07–0.17; 95% PI, 0.01–0.34; I2 = 98.17%), again with no appreciable reduction in heterogeneity.
Discussion
In our meta-analysis of 16 studies representing 23,469 Ph.D. students, we estimated that the pooled prevalence of clinically significant symptoms of depression was 24%. This estimate is consistent with estimated prevalence rates in other high-stress biomedical trainee populations, including medical students (27%)30, resident physicians (29%)65, and postdoctoral research fellows (29%)66. In the sample of nine studies representing 15,626 Ph.D. students, we estimated that the pooled prevalence of clinically significant symptoms of anxiety was 17%. While validated screening instruments tend to over-identify cases of depression (relative to structured clinical interviews) by approximately a factor of two67,68, our findings nonetheless point to a major public health problem among Ph.D. students. Available data suggest that the prevalence of depressive and anxiety disorders in the general population ranges from 5 to 7% worldwide69,70. In contrast, prevalence estimates of major depressive disorder among young adults have ranged from 13% (for young adults between the ages of 18 and 29 years in the 2012–2013 National Epidemiologic Survey on Alcohol and Related Conditions III71) to 15% (for young adults between the ages of 18 and 25 in the 2019 U.S. National Survey on Drug Use and Health72). Likewise, the prevalence of generalized anxiety disorder was estimated at 4% among young adults between the ages of 18 and 29 in the 2001–03 U.S. National Comorbidity Survey Replication73. Thus, even accounting for potential upward bias inherent in these studies’ use of screening instruments, our estimates suggest that the rates of recent clinically significant symptoms of depression and anxiety are greater among Ph.D. students compared with young adults in the general population.
Further underscoring the importance of this public health issue, Ph.D. students face unique stressors and uncertainties that may put them at increased risk for mental health and substance use problems. Students grapple with competing responsibilities, including coursework, teaching, and research, while also managing interpersonal relationships, social isolation, caregiving, and financial insecurity3,10. Increasing enrollment in doctoral degree programs has not been matched with a commensurate increase in tenure-track academic job opportunities, intensifying competition and pressure to find employment post-graduation5. Advisor-student power relations rarely offer options for recourse if and when such relationships become strained, particularly in the setting of sexual harassment, unwanted sexual attention, sexual coercion, and rape74–78. All of these stressors may be magnified—and compounded by stressors unrelated to graduate school—for subgroups of students who are underrepresented in doctoral degree programs and among whom mental health problems are either more prevalent and/or undertreated compared with the general population, including Black, indigenous, and other people of color13,79,80; women81,82; first-generation students14,15; people who identify as LGBTQ83–85; people with disabilities; and people with multiple intersecting identities.
Structural- and individual-level interventions will be needed to reduce the burden of mental ill-health among Ph.D. students worldwide31,86. Despite the high prevalence of mental health and substance use problems87, Ph.D. students demonstrate low rates of help-seeking40,52,88. Common barriers to help-seeking include fears of harming one’s academic career, financial insecurity, lack of time, and lack of awareness89–91, as well as health care systems-related barriers, including insufficient numbers of culturally competent counseling staff, limited access to psychological services beyond time-limited psychotherapies, and lack of programs that address the specific needs either of Ph.D. students in general92 or of Ph.D. students belonging to marginalized groups93,94. Structural interventions focused solely on enhancing student resilience might include programs aimed at reducing stigma, fostering social cohesion, and reducing social isolation, while changing norms around help-seeking behavior95,96. However, structural interventions focused on changing stressogenic aspects of the graduate student environment itself are also needed97, beyond any enhancements to Ph.D. student resilience, including: undercutting power differentials between graduate students and individual faculty advisors, e.g., by diffusing power among multiple faculty advisors; eliminating racist, sexist, and other discriminatory behaviors by faculty advisors74,75,98; valuing mentorship and other aspects of “invisible work” that are often disproportionately borne by women faculty and faculty of color99,100; and training faculty members to emphasize the dignity of, and adequately prepare Ph.D. students for, non-academic careers101,102.
Our findings should be interpreted with several limitations in mind. First, the pooled estimates are characterized by a high degree of heterogeneity, similar to meta-analyses of depression prevalence in other populations30,65,103–105. Second, we were only able to aggregate depression prevalence across 16 studies and anxiety prevalence across nine studies (the majority of which were conducted in the U.S.) – far fewer than the 183 studies included in a meta-analysis of depression prevalence among medical students30 and the 54 studies included in a meta-analysis of resident physicians65. These differences underscore the need for more rigorous study in this critical area. Many articles were either excluded from the review or from the meta-analyses for not meeting inclusion criteria or not reporting relevant statistics. Future research in this area should ensure the systematic collection of high-quality, clinically relevant data from a comprehensive set of institutions, across disciplines and countries, and disaggregated by graduate student type. As part of conducting research and addressing student mental health and wellbeing, university deans, provosts, and chancellors should partner with national survey and program institutions (e.g., Graduate Student Experience in the Research University [gradSERU]106, the American College Health Association National College Health Assessment [ACHA-NCHA], and HealthyMinds). Furthermore, federal agencies that oversee health and higher education should provide resources for these efforts, and accreditation agencies should require monitoring of mental health and programmatic responses to stressors among Ph.D. students.
Third, heterogeneity in reporting precluded a meta-analysis of the suicidality outcomes among the few studies that reported such data. While reducing the burden of mental health problems among graduate students is an important public health aim in itself, more research into understanding non-suicidal self-injurious behavior, suicide attempts, and completed suicide among Ph.D. students is warranted. Fourth, it is possible that the grey literature reports included in our meta-analysis are more likely to be undertaken at research-intensive institutions52,60,61. However, the direction of bias is unpredictable: mental health problems among Ph.D. students in research-intensive environments may be more prevalent due to detection bias, but such institutions may also have more resources devoted to preventive, screening, or treatment efforts92. Fifth, inclusion in this meta-analysis and systematic review was limited to those based on community samples. Inclusion of clinic-based samples, or of studies conducted before or after specific milestones (e.g., the qualifying examination or dissertation prospectus defense), likely would have yielded even higher pooled prevalence estimates of mental health problems. And finally, few studies provided disaggregated data according to sociodemographic factors, stage of training (e.g., first year, pre-prospectus defense, all-but-dissertation), or discipline of study. These factors might be investigated further for differences in mental health outcomes.
Clinically significant symptoms of depression and anxiety are pervasive among graduate students in doctoral degree programs, but these are understudied relative to other trainee populations. Structural and clinical interventions to systematically monitor and promote the mental health and wellbeing of Ph.D. students are urgently needed.
Methods
This systematic review and meta-analysis follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) approach (Supplementary Table S3)107. This study was based on data collected from publicly available bibliometric databases and did not require ethical approval from our institutional review boards.
Eligibility criteria
Studies were included if they provided data on either: (a) the number or proportion of Ph.D. students with clinically significant symptoms of depression or anxiety, ascertained using a validated scale; or (b) the mean depression or anxiety symptom severity score and its standard deviation among Ph.D. students. Suicidal ideation was examined as a secondary outcome.
We excluded studies that focused on graduate students in non-doctoral degree programs (e.g., Master of Public Health) or professional degree programs (e.g., Doctor of Medicine, Juris Doctor) because more is known about mental health problems in these populations30,108–110 and because Ph.D. students face unique uncertainties. To minimize the potential for upward bias in our pooled prevalence estimates, we excluded studies that recruited students from campus counseling centers or other clinic-based settings. Studies that measured affective states, or state anxiety, before or after specific events (e.g., terrorist attacks, qualifying examinations) were also excluded.
If articles described the study sample in general terms (i.e., without clarifying the degree level of the participants), we contacted the authors by email for clarification. Similarly, if articles pooled results across graduate students in doctoral and non-doctoral degree programs (e.g., reporting a single estimate for a mixed sample of graduate students), we contacted the authors by email to request disaggregated data on the subsample of Ph.D. students. If authors did not reply after two contact attempts spaced over 2 months, or were unable to provide these data, we excluded these studies from further consideration.
Search strategy and data extraction
PubMed, Embase, PsycINFO, ERIC, and Business Source Complete were searched from inception of each database to November 5, 2019. The search strategy included terms related to mental health symptoms (e.g., depression, anxiety, suicide), the study population (e.g., graduate, doctoral), and measurement category (e.g., depression, Columbia-Suicide Severity Rating Scale) (Supplementary Table S4). In addition, we searched the reference lists and the grey literature.
After duplicates were removed, we screened the remaining titles and abstracts, followed by a full-text review. We excluded articles following the eligibility criteria listed above (i.e., those that were not focused on Ph.D. students; those that did not assess depression and/or anxiety using a validated screening tool; those that did not report relevant statistics of depression and/or anxiety; and those that recruited students from clinic-based settings). Reasons for exclusion were tracked at each stage. Following selection of included articles, two members of the research team extracted data and conducted risk of bias assessments. Discrepancies were discussed with a third member of the research team. Key extraction variables included: study design, geographic region, sample size, response rate, demographic characteristics of the sample, screening instrument(s) used for assessment, mean depression or anxiety symptom severity score (and its standard deviation), and the number (or proportion) of students experiencing clinically significant symptoms of depression or anxiety.
Risk of bias assessment
Following prior work30,65, the Newcastle–Ottawa Scale111 was adapted and used to assess risk of bias in the included studies. Each study was assessed across 5 categories: sample representativeness, sample size, non-respondents, ascertainment of outcomes, and quality of descriptive statistics reporting (Supplementary Information S5). Studies were judged as having either low risk of bias (≥ 3 points) or high risk of bias (< 3 points).
Analysis and synthesis
Before pooling the estimated prevalence rates across studies, we first transformed the proportions using a variance-stabilizing double arcsine transformation112. We then computed pooled estimates of prevalence using a random effects model113. Study specific confidence intervals were estimated using the score method114,115. We estimated between-study heterogeneity using the I2 statistic116. In an attempt to reduce the extent of heterogeneity, we re-estimated pooled prevalence restricting the analysis to studies conducted in the United States and to studies in which depression assessment was based on the 9-item Patient Health Questionnaire (PHQ-9)117. All analyses were conducted using Stata (version 16; StataCorp LP, College Station, Tex.). Where heterogeneity limited our ability to summarize the findings using meta-analysis, we synthesized the data using narrative review.
Supplementary Information
Acknowledgements
We thank the following investigators for generously sharing their time and/or data: Gordon J. G. Asmundson, Ph.D., Amy J. L. Baker, Ph.D., Hillel W. Cohen, Dr.P.H., Alcir L. Dafre, Ph.D., Deborah Danoff, M.D., Daniel Eisenberg, Ph.D., Lou Farrer, Ph.D., Christy B. Fraenza, Ph.D., Patricia A. Frazier, Ph.D., Nadia Corral-Frías, Ph.D., Hanga Galfalvy, Ph.D., Edward E. Goldenberg, Ph.D., Robert K. Hindman, Ph.D., Jürgen Hoyer, Ph.D., Ayako Isato, Ph.D., Azharul Islam, Ph.D., Shanna E. Smith Jaggars, Ph.D., Bumseok Jeong, M.D., Ph.D., Ju R. Joeng, Nadine J. Kaslow, Ph.D., Rukhsana Kausar, Ph.D., Flavius R. W. Lilly, Ph.D., Sarah K. Lipson, Ph.D., Frances Meeten, D.Phil., D.Clin.Psy., Dhara T. Meghani, Ph.D., Sterett H. Mercer, Ph.D., Masaki Mori, Ph.D., Arif Musa, M.D., Shizar Nahidi, M.D., Ph.D., Arthur M. Nezu, Ph.D., D.H.L., Angelo Picardi, M.D., Nicole E. Rossi, Ph.D., Denise M. Saint Arnault, Ph.D., Sagar Sharma, Ph.D., Bryony Sheaves, D.Clin.Psy., Kennon M. Sheldon, Ph.D., Daniel Shepherd, Ph.D., Keisuke Takano, Ph.D., Sara Tement, Ph.D., Sherri Turner, Ph.D., Shawn O. Utsey, Ph.D., Ron Valle, Ph.D., Caleb Wang, B.S., Pengju Wang, Katsuyuki Yamasaki, Ph.D.
Author contributions
A.C.T. conceptualized the study and provided supervision. T.K. conducted the search. E.N.S. contacted authors for additional information not reported in published articles. E.N.S. and T.K. extracted data and performed the quality assessment appraisal. E.N.S. and A.C.T. conducted the statistical analysis and drafted the manuscript. T.K., M.V.K., R.A., S.C., H.L., X.L., C.H.L., I.R., S.S., M.T. and M.Y. contributed to the interpretation of the results. All authors provided critical feedback on drafts and approved the final manuscript.
Funding
A.C.T. acknowledges funding from the Sullivan Family Foundation. This paper does not reflect an official statement or opinion from the County of San Mateo.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Emily N. Satinsky, Email: satinsky@usc.edu
Alexander C. Tsai, Email: actsai@partners.org
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-021-93687-7.
References
- 1.Woolston C. Why mental health matters. Nature. 2018;557:129–131. doi: 10.1038/d41586-018-04998-1. [DOI] [Google Scholar]
- 2.Woolston C. A love-hurt relationship. Nature. 2017;550:549–552. doi: 10.1038/nj7677-549a. [DOI] [Google Scholar]
- 3.Woolston C. PhD poll reveals fear and joy, contentment and anguish. Nature. 2019;575:403–406. doi: 10.1038/d41586-019-03459-7. [DOI] [PubMed] [Google Scholar]
- 4.Byrom N. COVID-19 and the research community: The challenges of lockdown for early-career researchers. Elife. 2020;9:e59634. doi: 10.7554/eLife.59634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alberts B, Kirschner MW, Tilghman S, Varmus H. Rescuing US biomedical research from its systemic flaws. Proc. Natl. Acad. Sci. USA. 2014;111:5773–5777. doi: 10.1073/pnas.1404402111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McDowell GS, et al. Shaping the future of research: A perspective from junior scientists. F1000Res. 2014;3:291. doi: 10.12688/f1000research.5878.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Petersen AM, Riccaboni M, Stanley HE, Pammoli F. Persistence and uncertainty in the academic career. Proc. Natl. Acad. Sci. USA. 2012;109:5213–5218. doi: 10.1073/pnas.1121429109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Leshner AI. Rethinking graduate education. Science. 2015;349:349. doi: 10.1126/science.aac9592. [DOI] [PubMed] [Google Scholar]
- 9.National Academies of Sciences Engineering and Medicine . Graduate STEM Education for the 21st Century. National Academies Press; 2018. [Google Scholar]
- 10.Charles ST, Karnaze MM, Leslie FM. Positive factors related to graduate student mental health. J. Am. Coll. Health. 2021 doi: 10.1080/07448481.2020.1841207. [DOI] [PubMed] [Google Scholar]
- 11.Riddle ES, Niles MT, Nickerson A. Prevalence and factors associated with food insecurity across an entire campus population. PLoS ONE. 2020;15:e0237637. doi: 10.1371/journal.pone.0237637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Soldavini J, Berner M, Da Silva J. Rates of and characteristics associated with food insecurity differ among undergraduate and graduate students at a large public university in the Southeast United States. Prev. Med. Rep. 2019;14:100836. doi: 10.1016/j.pmedr.2019.100836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Clark US, Hurd YL. Addressing racism and disparities in the biomedical sciences. Nat. Hum. Behav. 2020;4:774–777. doi: 10.1038/s41562-020-0917-7. [DOI] [PubMed] [Google Scholar]
- 14.Gardner SK. The challenges of first-generation doctoral students. New Dir. High. Educ. 2013;2013:43–54. doi: 10.1002/he.20064. [DOI] [Google Scholar]
- 15.Seay SE, Lifton DE, Wuensch KL, Bradshaw LK, McDowelle JO. First-generation graduate students and attrition risks. J. Contin. High. Educ. 2008;56:11–25. doi: 10.1080/07377366.2008.10400158. [DOI] [Google Scholar]
- 16.Rummell CM. An exploratory study of psychology graduate student workload, health, and program satisfaction. Prof. Psychol. Res. Pract. 2015;46:391–399. doi: 10.1037/pro0000056. [DOI] [Google Scholar]
- 17.Salzer MS. A comparative study of campus experiences of college students with mental illnesses versus a general college sample. J. Am. Coll. Health. 2012;60:1–7. doi: 10.1080/07448481.2011.552537. [DOI] [PubMed] [Google Scholar]
- 18.Hysenbegasi A, Hass S, Rowland C. The impact of depression on the academic productivity of university students. J. Ment. Health Policy Econ. 2005;8:145–151. [PubMed] [Google Scholar]
- 19.Harvey S, et al. Depression and work performance: An ecological study using web-based screening. Occup. Med. (Lond.) 2011;61:209–211. doi: 10.1093/occmed/kqr020. [DOI] [PubMed] [Google Scholar]
- 20.Eisenberg D, Golberstein E, Hunt JB. Mental health and academic success in college. BE J. Econ. Anal. Policy. 2009;9:40. [Google Scholar]
- 21.Lovitts, B. E. Who is responsible for graduate student attrition--the individual or the institution? Toward an explanation of the high and persistent rate of attrition. In: Annual Meeting of the American Education Research Association (New York, 1996). Available at: https://eric.ed.gov/?id=ED399878.
- 22.Gardner SK. Student and faculty attributions of attrition in high and low-completing doctoral programs in the United States. High. Educ. 2009;58:97–112. doi: 10.1007/s10734-008-9184-7. [DOI] [Google Scholar]
- 23.Lovitts BE. Leaving the Ivory Tower: The Causes and Consequences of Departure from Doctoral Study. Rowman & Littlefield Publishers; 2001. [Google Scholar]
- 24.Rigler Jr, K. L., Bowlin, L. K., Sweat, K., Watts, S. & Throne, R. Agency, socialization, and support: a critical review of doctoral student attrition. In: Proceedings of the Third International Conference on Doctoral Education: Organizational Leadership and Impact, University of Central Florida, Orlando, (2017).
- 25.Golde CM. The role of the department and discipline in doctoral student attrition: Lessons from four departments. J. High. Educ. 2005;76:669–700. doi: 10.1353/jhe.2005.0039. [DOI] [Google Scholar]
- 26.Council of Graduate Schools . PhD Completion and Attrition: Analysis of Baseline Program Data from the PhD Completion Project. Council of Graduate Schools; 2008. [Google Scholar]
- 27.National Research Council . A Data-Based Assessment of Research-Doctorate Programs in the United States. The National Academies Press; 2011. [PubMed] [Google Scholar]
- 28.Akhtar P, et al. Prevalence of depression among university students in low and middle income countries (LMICs): A systematic review and meta-analysis. J. Affect. Disord. 2020;274:911–919. doi: 10.1016/j.jad.2020.03.183. [DOI] [PubMed] [Google Scholar]
- 29.Mortier P, et al. The prevalence of suicidal thoughts and behaviours among college students: A meta-analysis. Psychol. Med. 2018;48:554–565. doi: 10.1017/S0033291717002215. [DOI] [PubMed] [Google Scholar]
- 30.Rotenstein LS, et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: A systematic review and meta-analysis. JAMA. 2016;316:2214–2236. doi: 10.1001/jama.2016.17324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tsai JW, Muindi F. Towards sustaining a culture of mental health and wellness for trainees in the biosciences. Nat. Biotechnol. 2016;34:353–355. doi: 10.1038/nbt.3490. [DOI] [PubMed] [Google Scholar]
- 32.Levecque K, Anseel F, De Beuckelaer A, Van der Heyden J, Gisle L. Work organization and mental health problems in PhD students. Res. Policy. 2017;46:868–879. doi: 10.1016/j.respol.2017.02.008. [DOI] [Google Scholar]
- 33.Nagy GA, et al. Burnout and mental health problems in biomedical doctoral students. CBE Life Sci. Educ. 2019;18:1–14. doi: 10.1187/cbe.18-09-0198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Garcia-Williams A, Moffitt L, Kaslow NJ. Mental health and suicidal behavior among graduate students. Acad. Psychiatry. 2014;28:554–560. doi: 10.1007/s40596-014-0041-y. [DOI] [PubMed] [Google Scholar]
- 35.Sheldon KM. Emotionality differences between artists and scientists. J. Res. Pers. 1994;28:481–491. doi: 10.1006/jrpe.1994.1034. [DOI] [Google Scholar]
- 36.Lightstone SN, Swencionis C, Cohen HW. The effect of bioterrorism messages on anxiety levels. Int. Q. Community Health Educ. 2006;24:111–122. doi: 10.2190/1YWV-JEDN-BQFP-NEXH. [DOI] [PubMed] [Google Scholar]
- 37.Clark CR, Mercer SH, Zeigler-Hill V, Dufrene BA. Barriers to the success of ethnic minority students in school psychology graduate programs. School Psych. Rev. 2012;41:176–192. doi: 10.1080/02796015.2012.12087519. [DOI] [Google Scholar]
- 38.Eisenberg D, Gollust SE, Golberstein E, Hefner JL. Prevalence and correlates of depression, anxiety, and suicidality among university students. Am. J. Orthopsychiatry. 2007;77:534–542. doi: 10.1037/0002-9432.77.4.534. [DOI] [PubMed] [Google Scholar]
- 39.Farrer LM, Gulliver A, Bennett K, Fassnacht DB, Griffiths KM. Demographic and psychosocial predictors of major depression and generalised anxiety disorder in Australian university students. BMC Psychiatry. 2016;16:241. doi: 10.1186/s12888-016-0961-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lipson SK, Zhou S, Wagner B, III, Beck K, Eisenberg D. Major differences: Variations in undergraduate and graduate student mental health and treatment utilization across academic disciplines. J. Coll. Stud. Psychother. 2016;30:23–41. doi: 10.1080/87568225.2016.1105657. [DOI] [Google Scholar]
- 41.Lilly FRW, et al. The influence of racial microaggressions and social rank on risk for depression among minority graduate and professional students. Coll. Stud. J. 2018;52:86–104. [Google Scholar]
- 42.Lipson SK, Raifman J, Abelson S, Reisner SL. Gender minority mental health in the U.S.: Results of a national survey on college campuses. Am. J. Prev. Med. 2019;57:293–301. doi: 10.1016/j.amepre.2019.04.025. [DOI] [PubMed] [Google Scholar]
- 43.Lipson SK, Kern A, Eisenberg D, Breland-Noble AM. Mental health disparities among college students of color. J. Adolesc. Health. 2018;63:348–356. doi: 10.1016/j.jadohealth.2018.04.014. [DOI] [PubMed] [Google Scholar]
- 44.Baker AJL, Chambers J. Adult recall of childhood exposure to parental conflict: Unpacking the black box of parental alienation. J. Divorce Remarriage. 2011;52:55–76. doi: 10.1080/10502556.2011.534396. [DOI] [Google Scholar]
- 45.Golberstein E, Eisenberg D, Gollust SE. Perceived stigma and mental health care seeking. Psychiatr. Serv. 2008;59:392–399. doi: 10.1176/ps.2008.59.4.392. [DOI] [PubMed] [Google Scholar]
- 46.Hindman RK, Glass CR, Arnkoff DB, Maron DD. A comparison of formal and informal mindfulness programs for stress reduction in university students. Mindfulness. 2015;6:873–884. doi: 10.1007/s12671-014-0331-1. [DOI] [Google Scholar]
- 47.Hirai R, Frazier P, Syed M. Psychological and sociocultural adjustment of first-year international students: Trajectories and predictors. J. Couns. Psychol. 2015;62:438–452. doi: 10.1037/cou0000085. [DOI] [PubMed] [Google Scholar]
- 48.Lee JS, Jeong B. Having mentors and campus social networks moderates the impact of worries and video gaming on depressive symptoms: A moderated mediation analysis. BMC Public Health. 2014;14:1–12. doi: 10.1186/1471-2458-14-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Corral-Frias NS, Velardez Soto SN, Frias-Armenta M, Corona-Espinosa A, Watson D. Concurrent validity and reliability of two short forms of the mood and anxiety symptom questionnaire in a student sample from Northwest Mexico. J. Psychopathol. Behav. Assess. 2019;41:304–316. doi: 10.1007/s10862-019-09738-x. [DOI] [Google Scholar]
- 50.Meghani DT, Harvey EA. Asian Indian international students' trajectories of depression, acculturation, and enculturation. Asian Am. J. Psychol. 2016;7:1–14. doi: 10.1037/aap0000034. [DOI] [Google Scholar]
- 51.Barry KM, Woods M, Martin A, Stirling C, Warnecke E. A randomized controlled trial of the effects of mindfulness practice on doctoral candidate psychological status. J. Am. Coll. Health. 2019;67:299–307. doi: 10.1080/07448481.2018.1515760. [DOI] [PubMed] [Google Scholar]
- 52.Bolotnyy, V., Basilico, M. & Barreira, P. Graduate student mental health: lessons from American economics departments. J. Econ. Lit. (in press).
- 53.Barry KM, Woods M, Warnecke E, Stirling C, Martin A. Psychological health of doctoral candidates, study-related challenges and perceived performance. High. Educ. Res. Dev. 2018;37:468–483. doi: 10.1080/07294360.2018.1425979. [DOI] [Google Scholar]
- 54.Boyle KM, McKinzie AE. The prevalence and psychological cost of interpersonal violence in graduate and law school. J. Interpers. Violence. 2021;36(13-14):6319–6350. doi: 10.1177/0886260518816329. [DOI] [PubMed] [Google Scholar]
- 55.Heinrich DL. The causal influence of anxiety on academic achievement for students of differing intellectual ability. Appl. Psychol. Meas. 1979;3:351–359. doi: 10.1177/014662167900300307. [DOI] [Google Scholar]
- 56.Hish AJ, et al. Applying the stress process model to stress-burnout and stress-depression relationships in biomedical doctoral students: A cross-sectional pilot study. CBE Life Sci. Educ. 2019;18:1–11. doi: 10.1187/cbe.19-03-0060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Jamshidi F, et al. A cross-sectional study of psychiatric disorders in medical sciences students. Mater. Sociomed. 2017;29:188–191. doi: 10.5455/msm.2017.29.188-191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Liu C, et al. Prevalence and associated factors of depression and anxiety among doctoral students: The mediating effect of mentoring relationships on the association between research self-efficacy and depression/anxiety. Psychol. Res. Behav. Manag. 2019;12:195–208. doi: 10.2147/PRBM.S195131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sverdlik A, Hall NC. Not just a phase: Exploring the role of program stage on well-being and motivation in doctoral students. J. Adult Contin. Educ. 2019;26:1–28. [Google Scholar]
- 60.University of California Office of the President . The University of California Graduate student Well-Being Survey Report. University of California; 2017. [Google Scholar]
- 61.The Graduate Assembly . Graduate Student Happiness & Well-Being Report. University of California at Berkeley; 2014. [Google Scholar]
- 62.Richardson CM, Trusty WT, George KA. Trainee wellness: Self-critical perfectionism, self-compassion, depression, and burnout among doctoral trainees in psychology. Couns. Psychol. Q. 2020;33(2):187–198. doi: 10.1080/09515070.2018.1509839. [DOI] [Google Scholar]
- 63.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977;1:385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- 64.Spitzer RL, Kroenke K, Williams JBW, Lowe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 65.Mata DA, et al. Prevalence of depression and depressive symptoms among residents physicians: A systematic review and meta-analysis. JAMA. 2015;314:2373–2383. doi: 10.1001/jama.2015.15845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gloria CT, Steinhardt MA. Flourishing, languishing, and depressed postdoctoral fellows: Differences in stress, anxiety, and depressive symptoms. J. Postdoct. Aff. 2013;3:1–9. [Google Scholar]
- 67.Levis B, et al. Patient Health Questionnaire-9 scores do not accurately estimate depression prevalence: Individual participant data meta-analysis. J. Clin. Epidemiol. 2020;122:115–128.e111. doi: 10.1016/j.jclinepi.2020.02.002. [DOI] [PubMed] [Google Scholar]
- 68.Tsai AC. Reliability and validity of depression assessment among persons with HIV in sub-Saharan Africa: Systematic review and meta-analysis. J. Acquir. Immune Defic. Syndr. 2014;66:503–511. doi: 10.1097/QAI.0000000000000210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Baxter AJ, Scott KM, Vos T, Whiteford HA. Global prevalence of anxiety disorders: A systematic review and meta-regression. Psychol. Med. 2013;43:897–910. doi: 10.1017/S003329171200147X. [DOI] [PubMed] [Google Scholar]
- 70.Ferrari A, et al. Global variation in the prevalence and incidence of major depressive disorder: A systematic review of the epidemiological literature. Psychol. Med. 2013;43:471–481. doi: 10.1017/S0033291712001511. [DOI] [PubMed] [Google Scholar]
- 71.Hasin DS, et al. Epidemiology of adult DSM-5 major depressive disorder and its specifiers in the United States. JAMA Psychiatry. 2018;75:336–346. doi: 10.1001/jamapsychiatry.2017.4602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.US Substance Abuse and Mental Health Services Administration . Key Substance Use and Mental Health Indicators in the United States: Results from the 2019 National Survey on Drug Use and Health. Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; 2020. [Google Scholar]
- 73.Kessler RC, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 74.Working Group report to the Advisory Committee to the NIH Director . Changing the Culture to End Sexual Harassment. U. S. National Institutes of Health; 2019. [Google Scholar]
- 75.National Academies of Sciences Engineering and Medicine . Sexual Harassment of Women: Climate, Culture, and Consequences in Academic Sciences, Engineering, and Medicine. The National Academies Press; 2018. [PubMed] [Google Scholar]
- 76.Wadman M. A hidden history. Science. 2018;360:480–485. doi: 10.1126/science.360.6388.480. [DOI] [PubMed] [Google Scholar]
- 77.Hockfield S, Magley V, Yoshino K. Report of the External Review Committee to Review Sexual Harassment at Harvard University. External Review Committee to Review Sexual Harassment at Harvard University; 2021. [Google Scholar]
- 78.Bartlett T, Gluckman N. She left Harvard. He got to stay. Chronicle High. Educ. 2021;64:A14. [Google Scholar]
- 79.Tseng M, et al. Strategies and support for Black, Indigenous, and people of colour in ecology and evolutionary biology. Nat. Ecol. Evol. 2020;4:1288–1290. doi: 10.1038/s41559-020-1252-0. [DOI] [PubMed] [Google Scholar]
- 80.Williams DR, et al. Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: Results from the National Survey of American Life. Arch. Gen. Psychiatry. 2007;64:305–315. doi: 10.1001/archpsyc.64.3.305. [DOI] [PubMed] [Google Scholar]
- 81.Wu AH. Gender bias in rumors among professionals: An identity-based interpretation. Rev. Econ. Stat. 2020;102:867–880. doi: 10.1162/rest_a_00877. [DOI] [Google Scholar]
- 82.Kessler RC. Epidemiology of women and depression. J. Affect. Disord. 2003;74:5–13. doi: 10.1016/S0165-0327(02)00426-3. [DOI] [PubMed] [Google Scholar]
- 83.Mattheis A, Cruz-Ramirez De Arellano D, Yoder JB. A model of queer STEM identity in the workplace. J. Homosex. 2020;67:1839–1863. doi: 10.1080/00918369.2019.1610632. [DOI] [PubMed] [Google Scholar]
- 84.Semlyen J, King M, Varney J, Hagger-Johnson G. Sexual orientation and symptoms of common mental disorder or low wellbeing: Combined meta-analysis of 12 UK population health surveys. BMC Psychiatry. 2016;16:1–19. doi: 10.1186/s12888-016-0767-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lark JS, Croteau JM. Lesbian, gay, and bisexual doctoral students' mentoring relationships with faculty in counseling psychology: A qualitative study. Couns. Psychol. 1998;26:754–776. doi: 10.1177/0011000098265004. [DOI] [Google Scholar]
- 86.Jaremka LM, et al. Common academic experiences no one talks about: Repeated rejection, imposter syndrome, and burnout. Perspect Psychol Sci. 2020;15:519–543. doi: 10.1177/1745691619898848. [DOI] [PubMed] [Google Scholar]
- 87.Allen HK, et al. Substance use and mental health problems among graduate students: Individual and program-level correlates. J. Am. Coll. Health. 2020 doi: 10.1080/07448481.2020.1725020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Turner A, Berry T. Counseling center contributions to student retention and graduation: A longitudinal assessment. J. Coll. Stud. Dev. 2000;41:627–636. [Google Scholar]
- 89.Dyrbye LN, Thomas MR, Shanafelt TD. Medical student distress: Causes, consequences, and proposed solutions. Mayo Clin. Proc. 2005;80:1613–1622. doi: 10.4065/80.12.1613. [DOI] [PubMed] [Google Scholar]
- 90.Tija J, Givens JL, Shea JA. Factors associated with undertreatment of medical student depression. J. Am. Coll. Health. 2005;53:219–224. doi: 10.3200/JACH.53.5.219-224. [DOI] [PubMed] [Google Scholar]
- 91.Dearing R, Maddux J, Tangney J. Predictors of psychological help seeking in clinical and counseling psychology graduate students. Prof. Psychol. Res. Pract. 2005;36:323–329. doi: 10.1037/0735-7028.36.3.323. [DOI] [Google Scholar]
- 92.Langin K. Amid concerns about grad student mental health, one university takes a novel approach. Science. 2019 doi: 10.1126/science.caredit.aay7113. [DOI] [Google Scholar]
- 93.Guillory, D. Combating anti-blackness in the AI community. arXiv, arXiv:2006.16879 (2020).
- 94.Galan CA, et al. A call to action for an antiracist clinical science. J. Clin. Child Adolesc. Psychol. 2021;50(1):12–57. doi: 10.31234/osf.io/xqwr4. [DOI] [PubMed] [Google Scholar]
- 95.Wyman PA, et al. Effect of the Wingman-Connect upstream suicide prevention program for air force personnel in training: A cluster randomized clinical trial. JAMA Netw Open. 2020;3:e2022532. doi: 10.1001/jamanetworkopen.2020.22532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Knox KL, et al. The US Air Force Suicide Prevention Program: Implications for public health policy. Am. J. Public Health. 2010;100:2457–2463. doi: 10.2105/AJPH.2009.159871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Inclusive Climate Subcommittee of the Government Department Climate Change Committee . Government Department Climate Change: Final Report and Recommendations. Government Department, Harvard University; 2019. [Google Scholar]
- 98.Inclusive Climate Subcommittee of the Government Department Climate Change Committee . Government Department Climate Survey Report. Government Department, Harvard University; 2019. [Google Scholar]
- 99.Magoqwana B, Maqabuka Q, Tshoaedi M. "Forced to care" at the neoliberal university: Invisible labour as academic labour performed by Black women academics in the South African university. S. Afr. Rev. Sociol. 2019;50:6–21. doi: 10.1080/21528586.2020.1730947. [DOI] [Google Scholar]
- 100.Jones HA, Perrin PB, Heller MB, Hailu S, Barnett C. Black psychology graduate students' lives matter: Using informal mentoring to create an inclusive climate amidst national race-related events. Prof. Psychol. Res. Pract. 2018;49:75–82. doi: 10.1037/pro0000169. [DOI] [Google Scholar]
- 101.Mathur A, Meyers FJ, Chalkley R, O'Brien TC, Fuhrmann CN. Transforming training to reflect the workforce. Sci. Transl. Med. 2015;7:285. doi: 10.1126/scitranslmed.aaa8200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Scharff V. Advice: Prepare your Ph.D.s for diverse career paths. Chronicle High. Educ. 2018;65:30. [Google Scholar]
- 103.Beattie TS, Smilenova B, Krishnaratne S, Mazzuca A. Mental health problems among female sex workers in low- and middle-income countries: A systematic review and meta-analysis. PLoS Med. 2020;17:e1003297. doi: 10.1371/journal.pmed.1003297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Ismail Z, et al. Prevalence of depression in patients with mild cognitive impairment: A systematic review and meta-analysis. JAMA Psychiatry. 2017;74:58–67. doi: 10.1001/jamapsychiatry.2016.3162. [DOI] [PubMed] [Google Scholar]
- 105.Lim GY, et al. Prevalence of depression in the community from 30 countries between 1994 and 2014. Sci. Rep. 2018;8:1–10. doi: 10.1038/s41598-018-21243-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Jones-White DR, Soria KM, Tower EKB, Horner OG. Factors associated with anxiety and depression among U.S. doctoral students: Evidence from the gradSERU survey. J. Am. Coll. Health. 2021 doi: 10.1080/07448481.2020.1865975. [DOI] [PubMed] [Google Scholar]
- 107.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 2009;151:264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 108.Helmers KF, Danoff D, Steinert Y, Leyton M, Young SN. Stress and depressed mood in medical students, law students, and graduate students at McGill University. Acad. Med. 1997;72:708–714. doi: 10.1097/00001888-199708000-00018. [DOI] [PubMed] [Google Scholar]
- 109.Rabkow N, et al. Facing the truth: A report on the mental health situation of German law students. Int. J. Law Psychiatry. 2020;71:101599. doi: 10.1016/j.ijlp.2020.101599. [DOI] [PubMed] [Google Scholar]
- 110.Bergin A, Pakenham K. Law student stress: Relationships between academic demands, social isolation, career pressure, study/life imbalance and adjustment outcomes in law students. Psychiatr. Psychol. Law. 2015;22:388–406. doi: 10.1080/13218719.2014.960026. [DOI] [Google Scholar]
- 111.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 2010;25:603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 112.Freeman MF, Tukey JW. Transformations related to the angular and the square root. Ann. Math. Stat. 1950;21:607–611. doi: 10.1214/aoms/1177729756. [DOI] [Google Scholar]
- 113.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin. Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 114.Wilson EB. Probable inference, the law of succession, and statistical inference. J. Am. Stat. Assoc. 1927;22:209–212. doi: 10.1080/01621459.1927.10502953. [DOI] [Google Scholar]
- 115.Newcombe RG. Two-sided confidence intervals for the single proportion: Comparison of seven methods. Stat. Med. 1998;17:857–872. doi: 10.1002/(SICI)1097-0258(19980430)17:8<857::AID-SIM777>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 116.Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 117.Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.