Abstract
Social support (SS) predicts health outcomes among patients living with HIV. Systematic assessment of SS in routine HIV care is rare. We administered a brief, validated measure of SS, the Multifactoral Assessment of Perceived Social Support, within a patient-reported outcomes assessment of several health domains in routine HIV care at 4 U.S. clinics in English and Spanish (n=708). In univariate analysis, low SS was associated with poorer engagement in care, antiretroviral adherence, and health-related quality of life (HRQL); current methamphetamine/crystal use, depression, anxiety, and HIV stigma (all p<0.001); any use of either methamphetamines/crystal, illicit opioids, or cocaine/crack (p=0.001), current marijuana use (p=0.012), nicotine use (p=0.005), and concern for sexually transmitted infection (STI) exposure (p=0.001). High SS was associated with undetectable viral load (p=0.031). Multivariate analyses found low SS independently associated with depression (risk ratio (RR) 3.72, 95% CI 2.93-4.72), lower adherence (RR 0.76, 95% CI 0.64-0.89), poor engagement in care (RR 2.05, 95% CI 1.44-2.96), and having more symptoms (physical, psychological, and global distress) (RR 2.29, 95% CI 1.92-2.75). Medium SS was independently associated with depression (RR 2.59, 95% CI 2.00-3.36), poor engagement in care (RR 1.62, 95% CI 1.15-2.29) and having more symptoms (RR 1.75, 95% CI 1.44-2.13). SS assessment may help identify patients at risk for these outcomes, and set the stage for a multifaceted approach to improving health that takes the social dimension into account.
Introduction
Social support is an essential element of human health, protecting from mental ill-health (Gariepy, Honkaniemi, & Quesnel-Vallee, 2016), supporting healthful behaviors (Iribarren et al., 2017; Non et al., 2020; Watt et al., 2014) and improving immune, endocrine, and cardiac function (Cohen, 1988; Hawkley, Burleson, Berntson, & Cacioppo, 2003; Teoh & Hilmert, 2018; Uchino, Cacioppo, & Kiecolt-Glaser, 1996). Poor social support has been shown to increase the risk of morbidity and mortality (Holt-Lunstad, Smith, & Layton, 2010) through both physiological and psychosocial mechanisms (DiMatteo, 2004; Hawkley et al., 2003; Uchino et al., 1996) and has helped mitigate the emotional and practical impact of living with chronic conditions including cancer (Costa et al., 2017; Pinquart & Duberstein, 2010), diabetes (Pamungkas, Chamroonsawasdi, & Vatanasomboon, 2017; Spencer-Bonilla et al., 2017), and HIV (Iribarren et al., 2017).
Among people living with HIV (PLWH), social support plays a uniquely important role in health maintenance. This important role is due, in part, to the anticipation and experience of HIV-related stigma (Nyblade, 2006) which may render it difficult to establish and maintain adequate social support; indeed, HIV-related stigma has been found to be negatively correlated with social support (Smith, Rossetto, & Peterson, 2008). Evidence suggests that social support is protective for depression and HIV-related stigma (Larios, Davis, Gallo, Heinrich, & Talavera, 2009; Rao et al., 2012); it has also been associated with key outcomes in the HIV care continuum including earlier HIV diagnosis, better retention in care, and better adherence to antiretroviral therapy (ART) (Kelly, Hartman, Graham, Kallen, & Giordano, 2014). Insufficient social support, by contrast, has been associated with poorer ART adherence (Scheurer, Choudhry, Swanton, Matlin, & Shrank, 2012), unhealthy coping mechanisms (Iribarren et al., 2017), and denial of illness (Power et al., 2003) among PLWH. PLWH experience high rates of metabolic, cardiovascular, and immunologic complications (Deeks & Phillips, 2009; Willig & Overton, 2016), all of which may be further compromised by insufficient social support. As the population of PLWH grows older and the burden of morbidity and mortality for PLWH continues to shift from AIDS–defining illnesses to non-AIDS-related comorbidities (Justice & Braithwaite, 2012), identifying and addressing insufficient social support may yield broad health benefits.
There is little systematic assessment of patients’ social support in primary care, including primary HIV care. Given the strong association of the social dimension of life with health outcomes among PLWH, we incorporated a brief measure of perceived social support into routine HIV care. Using the Multifactoral Assessment of Perceived Social Support (MAPSS) (R. J. Fredericksen et al., 2019), a brief, validated measure of perceived functional social support for PLWH in care that is inclusive of concepts of social support prioritized highly by PLWH, we sought to characterize the relationship between social support and various health outcomes and behaviors in a population of PLWH.
Methods
Population
We administered the MAPSS to PLWH from four HIV primary care clinics within the Centers for AIDS Research Network of Integrated Clinical Systems (CNICS) in the United States which include: Fenway Community Health-Boston, MA; 1917 Clinic at the University of Alabama-Birmingham; Owen Clinic at the University of California-San Diego; and Madison Clinic at Harborview Medical Center/University of Washington-Seattle.
Procedure
In these clinics, as part of clinical care, patients complete a routine, self-administered assessment of patient-reported measures and outcomes (PROs) on touch-screen tablets immediately prior to seeing their provider (Crane et al., 2007; Lawrence et al., 2010). The PRO assessment includes self-reported measures of symptoms and health behaviors; we included the MAPSS as part of the assessment between January and August 2017. PLWH who appear intoxicated, have cognitive impairment, and/or are unable to read English, Spanish, or Amharic are not asked to complete the assessment. We administered the MAPSS to both English and Spanish-speaking patients, the two language groups for whom we have the largest numbers, in their respective languages.
Measures
Demographic data were elicited from the electronic health record (EHR) except sexual orientation and gender identity, which were collected with PRO measures. Other PRO measures included depression (PHQ-9) (Kroenke, Spitzer, & Williams, 2001; Spitzer, Kroenke, & Williams, 1999); anxiety (PHQ-5, three levels-high, some, and no anxiety) (Spitzer et al., 1999); adherence to ART using the Self-Rating Scale (Likert scale, very poor to excellent) and a 30-day visual analog scale (0-100% of medication taken in past month) (Chesney et al., 2000; Lu et al., 2008; Simoni et al., 2006); substance use (AUDIT/AUDIT-C for alcohol use, ASSIST for other substances) (Bradley et al., 2003; Bush, Kivlahan, McDonell, Fihn, & Bradley, 1998; Newcombe, Humeniuk, & Ali, 2005; 2002); current nicotine use; sexual risk behavior [Sexual Risk Behavior Inventory (R. J. Fredericksen et al., 2018), incorporating/using number of recent sex partners, self-reported concern for sexually transmitted infection (STI) exposure, and condomless sex in past three months]; HIV-related stigma (Earnshaw, Smith, Chaudoir, Amico, & Copenhaver, 2013) (5 point Likert scale, level of agreement with one or more of four stigma-related statements, score 1-5, higher score indicates worse stigma); HIV related symptoms (Justice et al., 2001) (number of symptoms for which ‘bothers some’ or ‘bothers a lot’ endorsed); and health-related quality of life (HRQL) (EuroQol, 1990) (EQ-5D, scoring range 5-13, lower score indicates better HRQL) and visual analog scale self-assessing health (0-100%, with 100% as best possible health). We used EHR data to determine viral load, CD4 cell count, the presence of hypertension or AIDS-defining illness, and frequency of missed visits. We defined poor engagement in care as one or more missed visits in two consecutive six-month intervals within a two-year time period.
Social support measure (MAPSS)
The MAPSS is a brief, clinically relevant, unidimensional measure of perceived social support we designed in partnership with PLWH (R. Fredericksen et al., 2019). It incorporates concepts of social support prioritized highly by PLWH. The MAPSS has simple response options that are well-understood by both English and Spanish speakers (see Fig. 1). Items include content related to perceived functional support, such as, “How much do you feel loved, liked, or cared about?” and “How much do you feel that people in your personal life support your ability to stay healthy?” Response options are “not enough” and “enough or more than enough.” “Suboptimal” social support is defined as a ‘not enough’ response to any of the eight items, with endorsement of ‘not enough’ for 5-8 items scoring as low social support, 1-4 items as medium social support, and 0 items as high social support. Cronbach’s alpha for the MAPSS was calculated.
Figure 1.
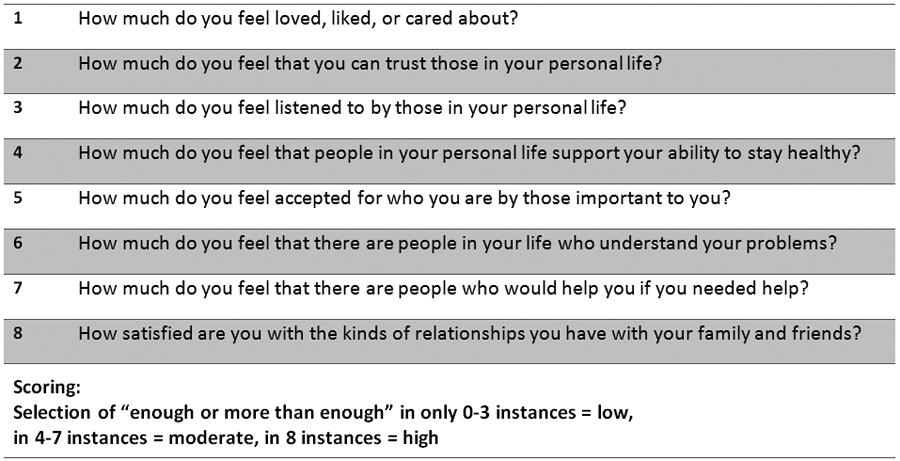
Multifactoral Assessment of Perceived Social Support (MAPSS)
CNICS data repository
The CNICS data repository integrates comprehensive clinical data including laboratory test results; ART use and other medications; diagnoses; demographic data; and historical information, including prior ART use, collected at initial clinic visits by standardized intake processes (Kitahata et al., 2008). The repository also includes the PRO data described here.
Data analysis
We divided participating PLWH into three groups based on their MAPSS scores: Low (0 – 3 points), Medium (4 – 7 points) and High (8 points) (R. Fredericksen et al., 2019). The groups were compared using ordinal logistic regression, with high social support as the reference category. Model fit and the assumption of proportional odds were tenable for all models.
In addition, we identified several recent, robust studies with large sample sizes with outcomes known or strongly suspected to be associated with social support. We performed multivariate analyses in CNICS data, based on the covariates and outcomes in these studies, with the addition of social support. Our goal was to better understand whether social support provided independent information about the outcome. We chose studies with the following outcomes: depression (Anagnostopoulos et al., 2015), engagement in care (Hightow-Weidman et al., 2017), medication adherence (Skalski et al., 2015), recent viral load (Rangarajan et al., 2016), health-related quality of life (HRQL) (Armon & Lichtenstein, 2012; Castro et al., 2019), recent drug use (Lightfoot et al., 2005), and number of symptoms (Harding et al., 2012; Lee et al., 2009). Symptoms in this latter category included symptoms of physical, psychological, and global distress as collected by either the Memorial Symptom Assessment Scale (in Lee et al) or its Short Form (in Harding et al)(Chang, Hwang, Feuerman, Kasimis, & Thaler, 2000; Portenoy et al., 1994). We constructed similar models with our data, with the addition of social support. We used Poisson regressions with robust standard errors to obtain risk ratios (RR). All models were controlled for age, sex, and race, in addition to outcome-specific covariates. High social support was the reference category.
Results
We administered the MAPSS to n=708 PLWH (48% age ≥50, 84% cisgender male, 29% nonwhite, 19% administered survey in Spanish) (see Table 1). Cronbach’s alpha for the MAPSS was 0.92. Table 2 summarizes demographic and behavioral characteristics by social support category determined from MAPSS responses. Data on stigma, condom use, and STI concern were only available for a subset of participants (n=201, n=433, and n=439, respectively). Algorithmic skip patterns allow stigma items to be assessed annually, and not at every assessment, to reduce patient burden; furthermore condom use/STI concern items are only asked when relevant, specifically of those having indicated sexual activity with a partner in the past 3 months. A higher proportion of PLWH who took the survey in English report lower levels of social support compared with those who took the survey in Spanish (p=0.015). We did not find differences in social support categories for other demographic groups (age, gender, race, ethnicity (Latino/non-Latino), sexual orientation, or study site).
Table 1.
Demographic and clinical characteristics of people living with HIV (n=708) who completed the MAPSS as part of routine clinical care visits in CNICS
| Characteristics | N (%) |
|---|---|
| Present sex male | 598 (84%) |
| Gender identity | |
| Male | 591 (83%) |
| Female | 101 (14%) |
| Transgender woman (male sex at birth) | 8 (1%) |
| Transgender man (female sex at birth) | 1 (0%) |
| Other/Unknown | 7 (1%) |
| Sexual orientation | |
| Lesbian/gay/other non-heterosexual identity | 464 (66%) |
| Straight or heterosexual | 158 (22%) |
| Bisexual | 54 (8%) |
| Something else | 10 (1%) |
| Don't know/unknown | 22 (3%) |
| Age | |
| <30 | 46 (7%) |
| 30-39 | 144 (20%) |
| 40-49 | 175 (25%) |
| ≥50 | 343 (48%) |
| Race | |
| White | 502 (71%) |
| Black | 130 (18%) |
| American Indian | 4 (1%) |
| Asian/Pacific Islander | 24 (3%) |
| Multiracial | 15 (2%) |
| Other/unknown | 33 (5%) |
| Hispanic | |
| Yes | 210 (30%) |
| No | 498 (70%) |
| Survey language Spanish | 136 (19%) |
| HIV risk factor | |
| MSM* | 473 (67%) |
| IDU** | 64 (9%) |
| MSM + IDU | 9 (1%) |
| Heterosexual | 129 (18%) |
| Other/unknown | 33 (5%) |
| Currently taking HIV medications | |
| Yes | 660 (93%) |
| No | 48 (6%) |
| Most recent CD4 count | |
| < 200 | 47 (7%) |
| 200 - 349 | 91 (13%) |
| ≥350 | 565 (80%) |
| Unknown | 5 (1%) |
| Recent viral load | |
| 0-400 | 646 (91%) |
| Over 400 | 52 (7%) |
| Unknown | 10 (1%) |
| Over 6 years in care | 358 (51%) |
men who have sex with men
injection drug user
Table 2.
Demographic, clinical and behavioral attributes by levels of social support among people living with HIV in CNICS; n (%) or median (interquartile range).
| Total (n=708) |
Social Support | p-valuea | |||
|---|---|---|---|---|---|
| Low (0 – 3 points) (n=105) |
Medium (4-7 points) (n=146) |
High (8 points) (n=457) |
|||
| Survey language Spanish | 0.015 | ||||
| Yes | 136 (19%) | 15 (14%) | 21 (14%) | 100 (22%) | |
| No | 572 (81%) | 90 (86%) | 125 (86%) | 357 (78%) | |
| 5 years or less since initial visit | 0.64 | ||||
| Yes | 304 (43%) | 49 (47%) | 61 (42%) | 194 (43%) | |
| No | 404 (57%) | 56 (53%) | 85 (58%) | 263 (58%) | |
| Most recent viral load | 0.031 | ||||
| Detectable | 52 (8%) | 11 (11%) | 15 (11%) | 26 (6%) | |
| Undetectable | 646 (93%) | 93 (89%) | 128 (90%) | 425 (94%) | |
| Recent CD4 | |||||
| <200 | 47 (7%) | 12 (11%) | 4 (3%) | 31 (7%) | 0.39 |
| 200 to <30 | 91 (13%) | 18 (17%) | 19 (13%) | 54 (12%) | |
| 350+ | 565 (80%) | 75 (71%) | 122 (84%) | 368 (81%) | |
| Any AIDS-defining illness | 0.95 | ||||
| Yes | 204 (29%) | 32 (328%) | 40 (27%) | 132 (29%) | |
| No | 504 (71%) | 73 (70%) | 106 (73%) | 325 (71%) | |
| Any hypertension diagnosis | 0.8 | ||||
| Yes | 180 (25%) | 23 (22%) | 44 (30%) | 113 (25%) | |
| No | 528 (75%) | 82 (78%) | 102 (70%) | 344 (75%) | |
| Engagement in care | < 0.001 | ||||
| Yes | 528 (75%) | 61 (58%) | 97 (66%) | 370 (81%) | |
| No | 180 (25%) | 44 (42%) | 49 (34%) | 87 (19%) | |
| Adherence to ART*
(Self-rating scale) |
0.001 | ||||
| Very poor–fair | 37 (6%) | 12 (13%) | 9 (7%) | 16 (4%) | |
| Good-Excellent | 621 (94%) | 81 (87%) | 125 (93%) | 415 (96%) | |
| Adherence (VAS**) | 99 (95–100) | 96 (90-99) | 98 (93-100) | 99 (96.5-100) | < 0.001 |
| Number of symptoms bothered by, some or a lot | 1 (0-4) | 5 (1-9) | 2 (0-7) | 0 (0-3) | < 0.001 |
| HRQL*** (VAS**) | 80 (67–91) | 66 (47-80) | 75 (61-90) | 86 (70-95) | < 0.001 |
| HRQL (EQ-5D) | 6 (5-7) | 7 (6-8.5) | 6 (5-7) | 5 (5-7) | < 0.001 |
| Depression (PHQ-9) | 3 (0.5-8) | 8.5 (5-15) | 6 (2-11) | 2 (0-5) | < 0.001 |
| Anxiety (PHQ-5) | < 0.001 | ||||
| None | 528 (75%) | 58 (56%) | 92 (63%) | 378 (83%) | |
| Some | 94 (13%) | 18 (17%) | 30 (21%) | 46 (10%) | |
| High | 82 (12%) | 28 (27%) | 23 (16%) | 31 (7%) | |
| HIV stigma | 1.5 (1-2.5) | 2.5 (1.5-3.5) | 2 (1.5-3) | 1 (1-2) | <0.001 |
| Current smoke or vape | 0.005 | ||||
| Yes | 218 (31%) | 42 (40%) | 51 (35%) | 125 (27%) | |
| No | 487 (69%) | 62 (60%) | 94 (65%) | 331 (73%) | |
| Any cocaine/crack past 3 months | 0.51 | ||||
| Yes | 34 (5%) | 5 (5%) | 9 (6%) | 20 (5%) | |
| No | 657 (95%) | 94 (95%) | 134 (94%) | 429 (96%) | |
| Any methamphetamines/crystal past 3 months | < 0.001 | ||||
| Yes | 72 (11%) | 20 (19%) | 25 (18%) | 27 (6%) | |
| No | 615 (90%) | 83 (81%) | 115 (82%) | 417 (94%) | |
| Any heroin past 3 months | 0.002 | ||||
| Yes | 7 (1%) | 3 (3%) | 4 (3%) | 0 (0%) | |
| No | 671 (99%) | 95 (97%) | 134 (97%) | 442(100%) | |
| Any prescription opioids taken not as prescribed past 3 months | 0.95 | ||||
| Yes | 11 (2%) | 1 (1%) | 3 (2%) | 7 (2%) | |
| No | 670 (98%) | 100 (99%) | 135 (98%) | 435 (98%) | |
| Used any of the above drugs, past 3 months | 0.001 | ||||
| Yes | 224 (33%) | 43 (42%) | 56 (40%) | 125 (29%) | |
| No | 458 (67%) | 60 (58%) | 84 (60%) | 314 (72%) | |
| Any sedatives past 3 months | 0.21 | ||||
| Yes | 147 (21%) | 24 (24%) | 35 (24%) | 88 (20%) | |
| No | 546 (79%) | 78 (77%) | 109 (76%) | 359 (80%) | |
| Any prescription stimulants past 3 months | 0.47 | ||||
| Yes | 89 (13%) | 13 (13%) | 22 (15%) | 54 (12%) | |
| No | 600 (87%) | 87 (87%) | 121 (85%) | 392 (88%) | |
| Any marijuana past 3 months | 0.012 | ||||
| Yes | 205 (29%) | 34 (33%) | 54 (38%) | 117 (26%) | |
| No | 429 (71%) | 68 (67%) | 89 (62%) | 335 (74%) | |
| Alcohol risk, AUDIT | 0.65 | ||||
| No drinking | 233 (34%) | 38 (37%) | 44 (31%) | 151 (34%) | |
| Not high risk | 338 (49%) | 47 (46%) | 67 (48%) | 224 (50%) | |
| High risk | 120 (17%) | 17 (17%) | 30 (21%) | 73 16(%) | |
| Approximately how many sex partners, past 3 months | 0.008 | ||||
| None | 261 (37%) | 40 (39%) | 52 (36%) | 169 (37%) | |
| 1 | 271 (39%) | 33 (32%) | 45 (31%) | 193 (42%) | |
| 2 to 5 | 144 (20%) | 26 (25%) | 39 (27%) | 79 (17%) | |
| ≥6 | 28 (4%) | 4 (4%) | 10 (7%) | 14 (3%) | |
| Concerned might have been exposed to STI**** or re-exposed to HIV | 0.001 | ||||
| Yes | 80 (18%) | 18 (29%) | 23 (25%) | 39 (14%) | |
| No | 359 (82%) | 45 (71%) | 69 (75%) | 245 (86%) | |
| Any unprotected vaginal or anal sex | 0.08 | ||||
| Yes | 228 (53%) | 36 (59%) | 52 (58%) | 140 (50%) | |
| No | 205 (47%) | 25 (41%) | 38 (42%) | 142 (50%) | |
Univariate p-value from ordinal logistic regression.
antiretroviral treatment
visual analog scale
health-related quality of life
sexually transmitted infection
Among HIV-specific health outcomes, a higher proportion of PLWH indicating the highest levels of social support had detectable viral loads with >400 copies/mL (p=0.031). A higher proportion of people who reported lower levels of social support were less engaged in care, defined as 1 or more missed visits in two consecutive six-month periods over the past two years (p<0.001), reporting more missed doses of ART (p<0.001), and reported “very poor” or “fair” ability to take all of their HIV medication (p=0.001). PLWH reporting less social support reported a higher number of symptoms that were bothersome as reported from the systems review.
Depression, anxiety, poorer reported HRQL, and reported HIV stigma were each associated with lower social support (p<0.001 for each). Poor social support was associated with several types of substance use. It was lower among those who reported smoking/vaping nicotine (p=0.005), current methamphetamine users (p<0.001), current marijuana users (p=0.012), and those indicating any use of methamphetamines, illicit opioids, or cocaine/crack (p=0.001). Notably, there was no association found between perceived social support and current alcohol use.
Social support may have a relationship with sexual risk behavior. Among those reporting having been sexually active in the past 3 months, a higher proportion of PLWH reporting higher levels of social support reported having just one sex partner in the past three months (p=0.008) and a smaller proportion reported being concerned about exposure to STI (p=.001).
In the multivariate replication models, social support was independently associated with many of the seven outcomes (Table 3). Low social support was independently associated with depression (RR 3.72, 95% CI 2.93-4.72), lower adherence (RR 0.76, 95% CI 0.64-0.89), poor engagement in care (RR 2.05, 95% CI 1.44-2.96), and having more symptoms (physical, psychological, and global distress) (RR 2.29, 95% CI 1.92-2.75). Medium social support was independently associated with depression (RR 2.59, 95% CI 2.00-3.36), poor engagement in care (RR 1.62, 95% CI 1.15-2.29) and having more symptoms (RR 1.75, 95% CI 1.44-2.13). Social support did not provide significant additional explanation for drug use or recent viral load.
Table 3.
Risk ratios (RR) (with 95% confidence intervals) for adding social support to models similar to those found in recent selected robust studies. All models were controlled for age, sex, and race and covariates in the right column. High social support was the reference category.
| Association of Social Support with outcome in PLWH in CNICS cohort | Example study from the literature |
Covariates | |||
|---|---|---|---|---|---|
| Outcome | High | Medium | Low | ||
| Depression (PHQ9; 4 categories) | Ref | 2.59 (2.00, 3.36) | 3.72 (2.93, 4.72) | Anagnostopoulos 2015 | Viral load, recent cd4 count, drug use, sexually active, alcohol use |
| Poor engagement in care | 1.62 (1.15, 2.29) | 2.05 (1.44, 2.96) | Hightow-Weidman 2017 | Depression, substance use | |
| Adherence (4 categories) | 0.91 (0.81, 1.01) | 0.76 (0.64, 0.89) | Skalski 2015 | Depression, substance use | |
| Recent viral load undetectable* | 1.01 (0.94, 1.11) | 1.00 (0.90, 1.10) | Rangarajan 2016 | Depression, stigma, substance use, adherence, engagement in care | |
| Health-related quality of life (4 categories) | 0.97 (0.89, 1.05) | 0.86 (0.75, 0.97) | Armon 2012 | Substance use, recent CD4 cell count, symptoms, depression | |
| Health-related quality of life (4 categories) | 0.97 (0.89, 1.06) | 0.85 (0.75, 0.97) | Castro 2018 | Depression, substance use, viral load, recent cd4 count | |
| Recent drug use | 1.11 (0.84, 1.46) | 1.11 (0.81, 1.52) | Lightfoot 2005 | Depression, health-related quality of life | |
| Number of symptoms (4 categories) | 1.75 (1.44, 2.13) | 2.29 (1.92, 2.75) | Lee 2009, Harding 2012 | Recent CD4 cell count, viral load | |
A model for recent viral load that did not control for adherence or engagement in care gave similarly null findings for social support, with RR of 0.97 (0.86, 1.08) for medium support and 0.97 (0.86, 1.10) for low.
Discussion
Perceived social support was significantly associated with health outcomes, consistent with findings among PLWH and other populations (Broadhead et al., 1983; Cassel, 1976; Cohen, 1988; Cohen & Wills, 1985; Hawkley et al., 2003; Iribarren et al., 2017; Kelly et al., 2014; Scheurer et al., 2012; Uchino et al., 1996; Watt et al., 2014). Lower perceived social support was associated with poorer engagement in care, poorer ART adherence, more bothersome symptoms, worse HIV stigma, worse perceived HRQL, depression, anxiety, and the use of most substances, with the exception of alcohol. In addition, lower social support was associated with a higher number of sex partners in the past three months and higher likelihood of concern regarding exposure to STI. Multivariate analyses found lower social support to be associated with higher depression, higher symptom burden, lower engagement in care, lower medication adherence, and lower HRQL.
While the direction of these associations are not known due to the cross-sectional nature of this study, our findings highlight the extent to which the social lives of PLWH intertwine with health behaviors and outcomes. Longitudinal studies can help determine whether changes corresponding to improvements in perceived social support are associated with improvements in these health outcomes. This hypothesis is plausible, as positive changes in social support among PLWH may support reductions in health behaviors that impact viral replication, such as poor adherence to ART and substance use, as well as supporting behaviors that reduce the risk of HIV/STI transmission.
Our findings build on those of prior studies across the life span linking health behaviors and outcomes to the dimension of social support (Hawkley et al., 2003; Hussen et al., 2017; Mackin, Perlman, Davila, Kotov, & Klein, 2017; Watt et al., 2014). These include several studies comprised primarily of HIV-uninfected populations, yet relevant to PLWH, such as the positive impact of practical social support on medication adherence (Scheurer et al., 2012) and the benefit of social support on cardiovascular, endocrine, and immune functioning (Uchino et al., 1996). Studies specific to PLWH have found higher social support to be linked to both cognitive and behavioral resilience (Hussen et al., 2017) and, that among the newly diagnosed, the positive relationship between social support and earlier diagnosis, timely linkage to care, and ART adherence (Kelly et al., 2014).
The strength of these associations prompts us to ask: what factors influence one’s perceived level of social support, and to what extent can providers in a clinical setting help modify these factors? Identification and treatment of depression is one clear opportunity: depressive disorders, highly prevalent among PLWH (Rabkin, 2008), are characterized by the presence of several symptoms that may increase social isolation, such as diminished interest in pleasurable activity, as well as feelings of worthlessness (American Psychiatric Association, 2013). Low self-worth may cause PLWH to feel diminished social connections and friendships, or to perceive such relationships as inauthentic. Antidepressants are known to improve self-perceptions of social functioning (Venditti et al., 2000; Young, Moskowitz, & aan het Rot, 2014), and evidence suggests that cognitive behavioral therapy may improve perceptions of social support (Berkman et al., 2003; Stice, Rohde, Gau, & Ochner, 2011), supporting an argument for routine screening for clinical depression in HIV care and its subsequent treatment. It is also possible that low social support may, in itself, trigger or exacerbate depression in vulnerable PLWH. Directly targeting perceptions of available social support with psychotherapy, group therapy, or other formalized peer-based support may more directly improve perceived social support.
We considered three sub-populations of PLWH who may particularly benefit from standardized assessment of social support: the elderly, the disabled, and those that are newly diagnosed with HIV. Among elderly PLWH, inadequate social support may have a more profound health impact relative to other populations given the higher prevalence and earlier onset of chronic comorbidities (Gallant, Hsue, Shreay, & Meyer, 2017; Guaraldi et al., 2011). Among the general population of physically disabled adults, inadequate social support is a common problem (Burholt, Windle, Morgan, & team, 2017; Scope, 2017); again, health impacts among physically disabled PLWH may be more severe. PLWH recently diagnosed with HIV may also benefit from at least initial assessment of social support, given that the social dimension of living with HIV is complicated by the anticipation and experience of HIV-related stigma. For newly-diagnosed PLWH, assessing and managing the social dimension of living with HIV has been described as an overwhelming and isolating experience (R. J. Fredericksen et al., 2015). Newly diagnosed PLWH suddenly face myriad decisions surrounding disclosure of their HIV status: who to tell, at what point, in what way, and at what potential cost. The health burden of such pressures have been associated with feelings of worthlessness, depressive symptoms, increased sexual risk behavior, substance use, poorer social functioning, and lower overall quality of life (Logie & Gadalla, 2009; Vanable, Carey, Blair, & Littlewood, 2006; Wolitski, Pals, Kidder, Courtenay-Quirk, & Holtgrave, 2009). Identifying lower levels of social support among newly diagnosed PLWH may lead to actions that lessen these outcomes at a particularly challenging time.
Referrals to support groups and clinic-based interventions that address coping with anticipated and actual HIV-related stigma may help bolster social support, both by generating community among newly-diagnosed PLWH, as well as helping to develop strategies and skills for navigating outside relationships. PLWH have noted that addressing social issues (i.e., HIV-related stigma) in the context of HIV care is essential to help address adverse health behaviors (R. J. Fredericksen et al., 2015), for example, in reducing a perceived need to use drugs or alcohol to cope with social isolation.
Both HIV-related stigma and social support have been top concerns among PLWH relative to other health-related topics (R. Fredericksen et al., 2016; R. J. Fredericksen et al., 2015). Assessment of perceived social support and HIV-related stigma, in conjunction with assessment of depression, drug and alcohol use, medication adherence and HIV/STI transmission risk behavior may help initiate conversations with PLWH about the interrelationships between these factors, and help set the stage for a multifaceted approach to improving health outcomes that takes the social dimension into account.
Strengths
We included a geographically, clinically, and demographically diverse patient sample from multiple sites across the US. In addition, we selected a measure that was developed with careful consideration of PLWH priorities and that is brief enough to potentially incorporate into clinical care visits.
Limitations
Due to the cross-sectional nature of this study, it is not possible to determine the directionality of cause/effect between social support and outcomes or if there may be a different cause. We identified in multivariate models the importance of factors such as depression and HRQL, but it is difficult to determine from this data whether these factors impact social support, the reverse, or both. Future studies with longitudinal data may focus on exploring this directionality.
Only one of the sites included in this study was located in the southern United States, which is currently the area of highest incidence of HIV as well as a region with the highest number of deaths in PLWH (CDC, 2017). The interplay of social support and HIV infection in this region merits further investigation.
Conclusions
Low social support is a common issue among PLWH and is associated with poor health outcomes. The use of the MAPSS, a well-tolerated and brief patient-reported measure of perceived social support that can be completed by PLWH electronically at the beginning of provider visits, may help identify PLWH at risk for these outcomes. Availing PLWH of resources for bolstering social support may help improve health outcomes.
Acknowledgements
We thank our patients, as well as the Madison Clinic Patient Panel for guidance in domain selection and development of the measure. This work was funded by the Patient Centered Outcomes Research Institute (PCORI) SC14-1403-14081 with additional support from the National Institute of Allergy and Infectious Diseases (NIAID) [CNICS R24 AI067039, UW CFAR NIAID Grant P30 AI027757; and UAB CFAR grant P30 AI027767].
Footnotes
Disclosure Statement
The authors declare no conflicts of interest.
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). [Google Scholar]
- Anagnostopoulos A, Ledergerber B, Jaccard R, Shaw SA, Stoeckle M, Bernasconi E, … Swiss, H. I. V. C. S. (2015). Frequency of and Risk Factors for Depression among Participants in the Swiss HIV Cohort Study (SHCS). PLoS One, 10(10), e0140943–e0140943. doi: 10.1371/journal.pone.0140943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armon C, & Lichtenstein K (2012). The associations among coping, nadir CD4+ T-cell count, and non-HIV-related variables with health-related quality of life among an ambulatory HIV-positive patient population. Qual Life Res, 21(6), 993–1003. doi: 10.1007/s11136-011-0017-2 [DOI] [PubMed] [Google Scholar]
- Berkman LF, Blumenthal J, Burg M, Carney RM, Catellier D, Cowan MJ, … Enhancing Recovery in Coronary Heart Disease Patients, I. (2003). Effects of treating depression and low perceived social support on clinical events after myocardial infarction: the Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) Randomized Trial. Jama, 289(23), 3106–3116. doi: 10.1001/jama.289.23.3106 [DOI] [PubMed] [Google Scholar]
- Bradley KA, Bush KR, Epler AJ, Dobie DJ, Davis TM, Sporleder JL, … Kivlahan DR (2003). Two brief alcohol-screening tests From the Alcohol Use Disorders Identification Test (AUDIT): validation in a female Veterans Affairs patient population. Arch Intern Med, 163(7), 821–829. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=12695273 [DOI] [PubMed] [Google Scholar]
- Broadhead WE, Kaplan BH, James SA, Wagner EH, Schoenbach VJ, Grimson R, … Gehlbach SH (1983). The epidemiologic evidence for a relationship between social support and health. Am J Epidemiol, 117(5), 521–537. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/6342368 [DOI] [PubMed] [Google Scholar]
- Burholt V, Windle G, Morgan DJ, & team, C. W. (2017). A Social Model of Loneliness: The Roles of Disability, Social Resources, and Cognitive Impairment. Gerontologist, 57(6), 1020–1030. doi: 10.1093/geront/gnw125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bush K, Kivlahan DR, McDonell MB, Fihn SD, & Bradley KA (1998). The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med, 158(16), 1789–1795. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=9738608 [DOI] [PubMed] [Google Scholar]
- Cassel J (1976). The contribution of the social environment to host resistance: the Fourth Wade Hampton Frost Lecture. Am J Epidemiol, 104(2), 107–123. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/782233 [DOI] [PubMed] [Google Scholar]
- Castro R, De Boni RB, Luz PM, Velasque L, Lopes LV, Medina-Lara A, … Veloso VG (2019). Health-related quality of life assessment among people living with HIV in Rio de Janeiro, Brazil: a cross-sectional study. Qual Life Res, 28(4), 1035–1045. doi: 10.1007/s11136-018-2044-8 [DOI] [PubMed] [Google Scholar]
- CDC. (2017). Diagnoses of HIV infection in the United States and dependent areas. Retrieved from
- Chang VT, Hwang SS, Feuerman M, Kasimis BS, & Thaler HT (2000). The memorial symptom assessment scale short form (MSAS-SF). Cancer, 89(5), 1162–1171. doi: [DOI] [PubMed] [Google Scholar]
- Chesney MA, Ickovics JR, Chambers DB, Gifford AL, Neidig J, Zwickl B, & Wu AW (2000). Self-reported adherence to antiretroviral medications among participants in HIV clinical trials: the AACTG adherence instruments. Patient Care Committee & Adherence Working Group of the Outcomes Committee of the Adult AIDS Clinical Trials Group (AACTG). AIDS Care, 12(3), 255–266. doi: 10.1080/09540120050042891 [DOI] [PubMed] [Google Scholar]
- Cohen S (1988). Psychosocial models of the role of social support in the etiology of physical disease. Health Psychol, 7(3), 269–297. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/3289916 [DOI] [PubMed] [Google Scholar]
- Cohen S, & Wills TA (1985). Stress, social support, and the buffering hypothesis. Psychol Bull, 98(2), 310–357. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/3901065 [PubMed] [Google Scholar]
- Costa ALS, Heitkemper MM, Alencar GP, Damiani LP, Silva RMD, & Jarrett ME (2017). Social Support Is a Predictor of Lower Stress and Higher Quality of Life and Resilience in Brazilian Patients With Colorectal Cancer. Cancer Nurs, 40(5), 352–360. doi: 10.1097/NCC.0000000000000388 [DOI] [PubMed] [Google Scholar]
- Crane HM, Lober W, Webster E, Harrington RD, Crane PK, Davis TE, & Kitahata MM (2007). Routine collection of patient-reported outcomes in an HIV clinic setting: the first 100 patients. Current HIV Research, 5(1), 109–118. Retrieved from http://offcampus.lib.washington.edu/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=cmedm&AN=17266562&site=ehost-live [DOI] [PubMed] [Google Scholar]
- Deeks SG, & Phillips AN (2009). HIV infection, antiretroviral treatment, ageing, and non-AIDS related morbidity. BMJ, 338, a3172. doi: 10.1136/bmj.a3172 [DOI] [PubMed] [Google Scholar]
- DiMatteo MR (2004). Social support and patient adherence to medical treatment: a meta-analysis. Health Psychol, 23(2), 207–218. doi: 10.1037/0278-6133.23.2.207 [DOI] [PubMed] [Google Scholar]
- Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, & Copenhaver MM (2013). HIV stigma mechanisms and well-being among PLWH: a test of the HIV stigma framework. AIDS Behav, 17(5), 1785–1795. doi: 10.1007/s10461-013-0437-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- EuroQol G (1990). EuroQol--a new facility for the measurement of health-related quality of life. Health Policy, 16(3), 199–208. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/10109801 [DOI] [PubMed] [Google Scholar]
- Fredericksen R, Fitzsimmons E, Gibbons L, Dougherty S, Loo S, Shurbaji S, … Crane H (2019). Development and content validation of the Multifactoral Assessment of Perceived Social Support (MAPSS), a brief, patient-reported measure of social support for use in HIV care. AIDS Care, In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredericksen R, Fitzsimmons E, Gibbons L, Loo S, Avendano-Soto S, Anderson W, … Crane H (2016). Prioritization of domain content areas to address in HIV clinical care among patients living with HIV and HIV care providers in the United States. Paper presented at the International Society of Quality of Life Copenhagen, Denmark. [Google Scholar]
- Fredericksen RJ, Edwards TC, Merlin JS, Gibbons LE, Rao D, Batey DS, … Patrick DL (2015). Patient and provider priorities for self-reported domains of HIV clinical care. AIDS Care, 27(10), 1255–1264. doi: 10.1080/09540121.2015.1050983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredericksen RJ, Fitzsimmons E, Gibbons LE, Dougherty S, Loo S, Shurbaji S, … Crane HM (2019). Development and content validation of the Multifactoral assessment of perceived social support (MAPSS), a brief, patient-reported measure of social support for use in HIV care. AIDS Care, 31(sup1), 1–9. doi: 10.1080/09540121.2019.1612005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredericksen RJ, Mayer KH, Gibbons LE, Edwards TC, Yang FM, Walcott M, … Crane HM (2018). Development and Content Validation of a Patient-Reported Sexual Risk Measure for Use in Primary Care. J Gen Intern Med. doi: 10.1007/s11606-018-4496-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallant J, Hsue PY, Shreay S, & Meyer N (2017). Comorbidities Among US Patients With Prevalent HIV Infection-A Trend Analysis. J Infect Dis, 216(12), 1525–1533. doi: 10.1093/infdis/jix518 [DOI] [PubMed] [Google Scholar]
- Gariepy G, Honkaniemi H, & Quesnel-Vallee A (2016). Social support and protection from depression: systematic review of current findings in Western countries. Br J Psychiatry, 209(4), 284–293. doi: 10.1192/bjp.bp.115.169094 [DOI] [PubMed] [Google Scholar]
- Guaraldi G, Orlando G, Zona S, Menozzi M, Carli F, Garlassi E, … Palella F (2011). Premature age-related comorbidities among HIV-infected persons compared with the general population. Clin Infect Dis, 53(11), 1120–1126. doi: 10.1093/cid/cir627 [DOI] [PubMed] [Google Scholar]
- Harding R, Selman L, Agupio G, Dinat N, Downing J, Gwyther L, … Higginson IJ (2012). Prevalence, burden, and correlates of physical and psychological symptoms among HIV palliative care patients in sub-Saharan Africa: an international multicenter study. J Pain Symptom Manage, 44(1), 1–9. doi: 10.1016/j.jpainsymman.2011.08.008 [DOI] [PubMed] [Google Scholar]
- Hawkley LC, Burleson MH, Berntson GG, & Cacioppo JT (2003). Loneliness in everyday life: cardiovascular activity, psychosocial context, and health behaviors. J Pers Soc Psychol, 85(1), 105–120. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/12872887 [DOI] [PubMed] [Google Scholar]
- Hightow-Weidman L, LeGrand S, Choi SK, Egger J, Hurt CB, & Muessig KE (2017). Exploring the HIV continuum of care among young black MSM. PLoS One, 12(6), e0179688. doi: 10.1371/journal.pone.0179688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad J, Smith TB, & Layton JB (2010). Social relationships and mortality risk: a meta-analytic review. PLoS Med, 7(7), e1000316. doi: 10.1371/journal.pmed.1000316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussen SA, Harper GW, Rodgers CRR, van den Berg JJ, Dowshen N, & Hightow-Weidman LB (2017). Cognitive and Behavioral Resilience Among Young Gay and Bisexual Men Living with HIV. LGBT Health, 4(4), 275–282. doi: 10.1089/lgbt.2016.0135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iribarren S, Siegel K, Hirshfield S, Olender S, Voss J, Krongold J, … Schnall R (2017). Self-Management Strategies for Coping with Adverse Symptoms in Persons Living with HIV with HIV Associated Non-AIDS Conditions. AIDS Behav. doi: 10.1007/s10461-017-1786-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Justice AC, & Braithwaite RS (2012). Lessons learned from the first wave of aging with HIV. AIDS, 26 Suppl 1, S11–18. doi: 10.1097/QAD.0b013e3283558500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Justice AC, Holmes W, Gifford AL, Rabeneck L, Zackin R, Sinclair G, … Wu AW (2001). Development and validation of a self-completed HIV symptom index. J Clin Epidemiol, 54 Suppl 1, S77–90. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=11750213 [DOI] [PubMed] [Google Scholar]
- Kelly JD, Hartman C, Graham J, Kallen MA, & Giordano TP (2014). Social support as a predictor of early diagnosis, linkage, retention, and adherence to HIV care: results from the steps study. J Assoc Nurses AIDS Care, 25(5), 405–413. doi: 10.1016/j.jana.2013.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitahata MM, Rodriguez B, Haubrich R, Boswell S, Mathews WC, Lederman MM, … Saag MS (2008). Cohort profile: the Centers for AIDS Research Network of Integrated Clinical Systems. Int J Epidemiol, 37(5), 948–955. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=18263650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JB (2001). The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med, 16(9), 606–613. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=11556941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larios SE, Davis JN, Gallo LC, Heinrich J, & Talavera G (2009). Concerns about stigma, social support and quality of life in low-income HIV-positive Hispanics. Ethn Dis, 19(1), 65–70. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/19341165 [PubMed] [Google Scholar]
- Lawrence ST, Willig JH, Crane HM, Ye J, Aban I, Lober W, … Schumacher JE (2010). Routine, self-administered, touch-screen, computer-based suicidal ideation assessment linked to automated response team notification in an HIV primary care setting. Clin Infect Dis, 50(8), 1165–1173. doi: 10.1086/651420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee KA, Gay C, Portillo CJ, Coggins T, Davis H, Pullinger CR, & Aouizerat BE (2009). Symptom experience in HIV-infected adults: a function of demographic and clinical characteristics. J Pain Symptom Manage, 38(6), 882–893. doi: 10.1016/j.jpainsymman.2009.05.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lightfoot M, Rogers T, Goldstein R, Rotheram-Borus MJ, May S, Kirshenbaum S, … Morin SF (2005). Predictors of substance use frequency and reductions in seriousness of use among persons living with HIV. Drug Alcohol Depend, 77(2), 129–138. doi: 10.1016/j.drugalcdep.2004.07.009 [DOI] [PubMed] [Google Scholar]
- Logie C, & Gadalla T (2009). Meta-analysis of health and demographic correlates of stigma towards people living with HIV. AIDS Care, 21(6), 742–753. [DOI] [PubMed] [Google Scholar]
- Lu M, Safren SA, Skolnik PR, Rogers WH, Coady W, Hardy H, & Wilson IB (2008). Optimal recall period and response task for self-reported HIV medication adherence. AIDS Behav, 12(1), 86–94. doi: 10.1007/s10461-007-9261-4 [DOI] [PubMed] [Google Scholar]
- Mackin DM, Perlman G, Davila J, Kotov R, & Klein DN (2017). Social support buffers the effect of interpersonal life stress on suicidal ideation and self-injury during adolescence. Psychol Med, 47(6), 1149–1161. doi: 10.1017/S0033291716003275 [DOI] [PubMed] [Google Scholar]
- Newcombe DA, Humeniuk RE, & Ali R (2005). Validation of the World Health Organization Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): report of results from the Australian site. Drug Alcohol Rev, 24(3), 217–226. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=16096125 [DOI] [PubMed] [Google Scholar]
- Non AL, Roman JC, Clausing ES, Gilman SE, Loucks EB, Buka SL, … Kubzansky LD (2020). Optimism and Social Support Predict Healthier Adult Behaviors Despite Socially Disadvantaged Childhoods. Int J Behav Med, 27(2), 200–212. doi: 10.1007/s12529-020-09849-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyblade LC (2006). Measuring HIV stigma: existing knowledge and gaps. Psychology Health & Medicine, 11(3), 335–345. [DOI] [PubMed] [Google Scholar]
- Pamungkas RA, Chamroonsawasdi K, & Vatanasomboon P (2017). A Systematic Review: Family Support Integrated with Diabetes Self-Management among Uncontrolled Type II Diabetes Mellitus Patients. Behav Sci (Basel), 7(3). doi: 10.3390/bs7030062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinquart M, & Duberstein PR (2010). Associations of social networks with cancer mortality: a meta-analysis. Crit Rev Oncol Hematol, 75(2), 122–137. doi: 10.1016/j.critrevonc.2009.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Portenoy RK, Thaler HT, Kornblith AB, Lepore JM, Friedlander-Klar H, Kiyasu E, … et al. (1994). The Memorial Symptom Assessment Scale: an instrument for the evaluation of symptom prevalence, characteristics and distress. Eur J Cancer, 30A(9), 1326–1336. doi: 10.1016/0959-8049(94)90182-1 [DOI] [PubMed] [Google Scholar]
- Power R, Koopman C, Volk J, Israelski DM, Stone L, Chesney MA, & Spiegel D (2003). Social support, substance use, and denial in relationship to antiretroviral treatment adherence among HIV-infected persons. AIDS Patient Care STDS, 17(5), 245–252. doi: 10.1089/108729103321655890 [DOI] [PubMed] [Google Scholar]
- Rabkin JG (2008). HIV and depression: 2008 review and update. Curr HIV/AIDS Rep, 5(4), 163–171. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/18838056 [DOI] [PubMed] [Google Scholar]
- Rangarajan S, Donn JC, Giang le T, Bui DD, Hung Nguyen H, Tou PB, … West G (2016). Factors associated with HIV viral load suppression on antiretroviral therapy in Vietnam. J Virus Erad, 2(2), 94–101. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/27482442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao D, Chen WT, Pearson CR, Simoni JM, Fredriksen-Goldsen K, Nelson K, … Zhang F (2012). Social support mediates the relationship between HIV stigma and depression/quality of life among people living with HIV in Beijing, China. Int J STD AIDS, 23(7), 481–484. doi: 10.1258/ijsa.2009.009428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheurer D, Choudhry N, Swanton KA, Matlin O, & Shrank W (2012). Association between different types of social support and medication adherence. Am J Manag Care, 18(12), e461–467. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/23286676 [PubMed] [Google Scholar]
- Scope. (2017). Nearly half of disabled people chronically lonely. Retrieved from https://www.scope.org.uk/press-releases/nearly-half-of-disabled-people-chronically-lonely?utm_content=bufferc7c3d&utm_medium=social&utm_source=twitter&utm_campaign=buffer
- Simoni JM, Kurth AE, Pearson CR, Pantalone DW, Merrill JO, & Frick PA (2006). Self-report measures of antiretroviral therapy adherence: A review with recommendations for HIV research and clinical management. AIDS Behav, 10(3), 227–245. doi: 10.1007/s10461-006-9078-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skalski LM, Watt MH, MacFarlane JC, Proeschold-Bell RJ, Stout JE, & Sikkema KJ (2015). Mental Health and Substance Use Among Patients in a North Carolina HIV Clinic. N C Med J, 76(3), 148–155. doi: 10.18043/ncm.76.3.148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith R, Rossetto K, & Peterson BL (2008). A meta-analysis of disclosure of one's HIV-positive status, stigma and social support. AIDS Care, 20(10), 1266–1275. doi: 10.1080/09540120801926977 [DOI] [PubMed] [Google Scholar]
- Spencer-Bonilla G, Ponce OJ, Rodriguez-Gutierrez R, Alvarez-Villalobos N, Erwin PJ, Larrea-Mantilla L, … Montori VM (2017). A systematic review and meta-analysis of trials of social network interventions in type 2 diabetes. BMJ Open, 7(8), e016506. doi: 10.1136/bmjopen-2017-016506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, & Williams JB (1999). Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. Jama, 282(18), 1737–1744. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=10568646 [DOI] [PubMed] [Google Scholar]
- Stice E, Rohde P, Gau J, & Ochner C (2011). Relation of depression to perceived social support: results from a randomized adolescent depression prevention trial. Behav Res Ther, 49(5), 361–366. doi: 10.1016/j.brat.2011.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teoh AN, & Hilmert C (2018). Social support as a comfort or an encouragement: A systematic review on the contrasting effects of social support on cardiovascular reactivity. Br J Health Psychol, 23(4), 1040–1065. doi: 10.1111/bjhp.12337 [DOI] [PubMed] [Google Scholar]
- Uchino BN, Cacioppo JT, & Kiecolt-Glaser JK (1996). The relationship between social support and physiological processes: a review with emphasis on underlying mechanisms and implications for health. Psychol Bull, 119(3), 488–531. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/8668748 [DOI] [PubMed] [Google Scholar]
- Vanable PA, Carey MP, Blair DC, & Littlewood RA (2006). Impact of HIV-related stigma on health behaviors and psychological adjustment among HIV-positive men and women. AIDS And Behavior, 10(5), 473–482. Retrieved from http://offcampus.lib.washington.edu/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=cmedm&AN=16604295&site=ehost-live [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venditti LN, Arcelus A, Birnbaum H, Greenberg P, Barr CE, Rowland C, & Williamson T (2000). The impact of antidepressant use on social functioning: reboxetine versus fluoxetine. Int Clin Psychopharmacol, 15(5), 279–289. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/10993130 [DOI] [PubMed] [Google Scholar]
- Watt RG, Heilmann A, Sabbah W, Newton T, Chandola T, Aida J, … Tsakos G (2014). Social relationships and health related behaviors among older US adults. BMC Public Health, 14, 533. doi: 10.1186/1471-2458-14-533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO ASSIST Working Group. (2002). The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): development, reliability and feasibility. Addiction, 97(9), 1183–1194. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=12199834 [DOI] [PubMed] [Google Scholar]
- Willig AL, & Overton ET (2016). Metabolic Complications and Glucose Metabolism in HIV Infection: A Review of the Evidence. Curr HIV/AIDS Rep, 13(5), 289–296. doi: 10.1007/s11904-016-0330-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolitski RJ, Pals SL, Kidder DP, Courtenay-Quirk C, & Holtgrave DR (2009). The effects of HIV stigma on health, disclosure of HIV status, and risk behavior of homeless and unstably housed persons living with HIV. AIDS And Behavior, 13(6), 1222–1232. doi: 10.1007/s10461-008-9455-4 [DOI] [PubMed] [Google Scholar]
- Young SN, Moskowitz DS, & aan het Rot M (2014). Possible role of more positive social behaviour in the clinical effect of antidepressant drugs. J Psychiatry Neurosci, 39(1), 60–65. doi: 10.1503/jpn.130165 [DOI] [PMC free article] [PubMed] [Google Scholar]


