Abstract
People with chronic stroke (PwCS) demonstrate similar gait-slip fall-risk on both paretic and non-paretic side. Compensatory stepping and slipping limb control are crucial to reduce gait-slip fall-risk. Given the unpredictable intensities of real-life perturbations, this study aimed to determine whether recovery from paretic or non-paretic slips vary as a function of perturbation intensity among PwCS. Forty-four PwCS were assigned to non-paretic low intensity slip, non-paretic high intensity slip, paretic low intensity slip, or paretic high intensity slip group. Participants were subjected to a novel overground gait-slip with a distance of 24 cm (low) or 45 cm (high), under either limb. Recovery strategies, center of mass (CoM) state stability and slipping kinematics were analyzed. Both non-paretic high and low intensity groups demonstrated similar percentage of aborted and recovery stepping, however, paretic high intensity group demonstrated greater aborted stepping (p > 0.05). Both high and low intensity paretic slip groups demonstrated reduced post-slip CoM stability relative to the non-paretic slip groups (p < 0.05). Slip displacement was greater in paretic high group compared with non-paretic high group (p < 0.05). Greater slip displacement at higher intensity was noted only in paretic slip group (p < 0.05). The slip velocity was faster in paretic groups compared to non-paretic slip groups (p < 0.05). Paretic slips showed lower stability at both intensities associated with difficulty in modulating slipping kinematics and resorting to an increased aborted stepping strategy compared to non-paretic slip. These findings are suggestive of developing balance interventions for improving both compensatory non-paretic limb stepping and reactive control of slipping paretic limb for fall-risk reduction.
Keywords: Gait-slip, Stroke, Reactive balance, Perturbation intensity, Stability
1. Introduction
Falls in individuals with stroke contribute to long-term disability and mortality (Batchelor et al., 2012; Jørgensen et al., 2002). Fall incidence increases in people with chronic stroke (PwCS) after achieving community ambulation, due to increased exposure to external perturbations like slips or trips (Schmid et al., 2013; Weerdesteyn et al., 2008). Studies in healthy older adults show that recovery from external perturbations require intact reactive balance control, demanding execution of an effective rapid compensatory stepping response to prevent a fall (Maki and McIlroy, 1997; Maki et al., 2003). However, such reactive balance control is impaired in individuals with stroke (Handelzalts et al., 2019; Inness et al., 2014; Mansfield et al., 2015; Martinez et al., 2013). Strategies of reactive balance response are affected by perturbation intensity (velocity, acceleration and displacement) as shown by stance perturbation studies in healthy older adults (Bastian, 2008; Horak and Diener, 1994) and sensorimotor abilities of an individual demonstrated by perturbation studies in PwCS (Mansfield et al., 2012; Patel and Bhatt, 2016; Salot et al., 2016). This is evident by in-place versus change-in-support strategies exhibited during low and high magnitude perturbations, respectively (Horak and Nashner, 1986; Maki and McIlroy, 1997). Stroke related sensorimotor impairments may affect accurate encoding of contextual information or the ability to modify reactive motor responses, thereby increasing fall-risk in this population (Joshi et al., 2018; Lakhani et al., 2011; Mansfield et al., 2012; Salot et al., 2016). Thus, understanding the effect of perturbation intensity on recovery responses following paretic and non-paretic slips might provide insights into developing effective fall-risk assessments and balance interventions.
To examine recovery responses induced from environmental perturbations, researchers have now successfully induced real-life like laboratory perturbations in a safe and controlled environment (Allin et al., 2020; Kajrolkar et al., 2014; Okubo et al., 2018; Pai et al., 2014). Kajrolkar (2016) exposed PwCS to mid-sized laboratory overground gait-slips under each limb and demonstrated equal fall incidence on both paretic and non-paretic sides. Such similar fall incidence was attributed to reactive balance deficits of the paretic limb and an inability of the non-paretic limb to adequately compensate for those deficits, highlighting the need to effectively coordinate reactive responses from both limbs for successful recovery. Additionally, successful recovery from a perturbation is also based on the ability to modulate the slipping and stepping kinematics (Kajrolkar and Bhatt, 2016). In another study, although comparison between fallers vs. non-fallers among PwCS showed similar recovery strategies to split-belt based gait perturbations, fallers who responded with the paretic limb demonstrated lower stability compared with those who responded with the non-paretic limb, indicating difficulty in modulating paretic recovery step (Punt et al., 2017).
Literature shows that the central nervous system (CNS) exercises different motor strategies to counteract balance loss based on perturbation intensity (Imamizu et al., 2007). Patel et al. (2016) exposed PwCS to progressively increasing intensities of stance-slips. PwCS showed an increase in the multiple stepping response and decline in center of mass (CoM) stability with increasing perturbation intensity, suggesting an impaired ability to modulate reactive responses after stroke. However, the recovery strategies employed during stance (Joshi et al., 2018; Lakhani et al., 2011; Mansfield et al., 2011; Mansfield et al., 2012; Salot et al., 2016) and gait perturbations might be quite different (Kajrolkar and Bhatt, 2016; Kajrolkar et al., 2014). Further, in stance perturbations, PwCS predominantly perform a compensatory step with the preferred non-paretic limb (Joshi et al., 2018; Lakhani et al., 2011; Mansfield et al., 2012; Salot et al., 2016), therefore, it is challenging to examine specific contributions of each limb in reducing fall-risk. Additionally, as majority of falls in PwCS occur during walking (Batchelor et al., 2012; Schmid et al., 2013), it is crucial to study the effect of stroke impairments on the ability to modulate reactive balance responses to varying perturbation magnitudes during walking.
Thus, our study aimed to examine whether recovery from paretic or non-paretic slips vary as a function of perturbation intensity by exposing PwCS to a low intensity slip (slip distance 24 cm) and a high intensity slip (slip distance 45 cm) during walking, under either paretic limb or non-paretic limb. We hypothesized that regardless of the slipping side, both non-paretic and paretic gait-slips would demonstrate lower postural stability at high intensity slips due to the impaired ability of the paretic limb to effectively control slip kinematics and execute an appropriate recovery stepping response.
2. Methods
2.1. Participants
Forty-four community-dwelling PwCS participated in the study. The inclusion criteria were: 1) self-reported cortical stroke > 6 months ago (confirmed by their physician), and 2) ability to ambulate independently with or without an assistive device. Participants were excluded if they had: 1) cognitive impairment (Montreal Cognitive Assessment Scale score ≤ 26/30), 2) aphasia (Mississippi Aphasia Screening Test score of ≥ 71/100), 3) poor bone density (T score < −2 on the heel ultrasound), or 4) any other self-reported neurological, musculoskeletal, or cardiovascular conditions. Baseline assessments for severity of motor impairment, balance and mobility were performed. Participants were randomly assigned to either of the four groups: non-paretic low intensity slip, paretic low intensity slip, non-paretic high intensity slip and paretic high intensity slip. Depending on the assigned group, each participant was subjected to a single novel slip either under the non-paretic or paretic limbs and with a slip distance of either 45 cm (high intensity) or 24 cm (low intensity). Demographics and clinical characteristics of all the participants are presented in Table 1. All participants gave written informed consent approved by the Institutional Review Board of the University of Illinois at Chicago prior to enrollment.
Table 1.
Demographics and clinical outcome measures of study participants.
| Non-paretic low slip intensity |
Non-paretic high slip intensity | Paretic low slip intensity |
Paretic high slip intensity |
|
|---|---|---|---|---|
| n = 10 | n = 11 | n = 12 | n = 11 | |
| Age (years) | 56.6 ± 6.86 | 61.64 ± 9.41 | 59.17 ± 4.37 | 64.09 ± 13.58 |
| Chronicity (years) | 8.09 ± 6.29 | 8.36 ± 3.75 | 6.75 ± 5.58 | 8.27 ± 5.82 |
| Impairment level | ||||
| CMSA (Leg) (/7) | 5.33 ± 0.75 | 5.36 ± 0.98 | 4.7 ± 1.06 | 4.55 ± 1.16 |
| CMSA (Foot) (/7) | 2.67 ± 1.25 | 4.45 ± 1.16 | 3 ± 1.15 | 3.82 ± 1.27 |
| AFO/No AFO | ||||
| Balance (BBS) (/56) | 49.2 ± 3.54 | 49.82 ± 3.61 | 45.17 ± 6.13 | 45 ± 7.93 |
| TUG (s) | 15.3 ± 5.22 | 13.99 ± 4.28 | 14.59 ± 4.91 | 21.93 ± 14.79 |
CMSA: Chedoke-McMaster Stroke Assessment scale; AFO: Ankle foot orthosis; BBS: Berg Balance Scale; TUG: Timed up and go test; s: Seconds.
2.2. Laboratory based gait-slip protocol
Participants were secured in a safety harness to prevent from touching the ground in an event of fall. Participants were asked to walk at their preferred speed for few trials on an 8-meter instrumented walkway comprising of low-friction, moveable platform to familiarize them. Following baseline walking trials, participants were instructed that at any given time, with no prior warning, a slip may occur under either limbs and that they should try their best to recover balance and continue walking. A sudden unannounced slip was induced using a computer-controlled release mechanism. Depending on the assigned group, a slip was induced with a slip distance of 24 cm (low group) or 45 cm (high group) under either the non-paretic or paretic limb (Fig. 1a & 1b). Thus, participants were split into 4 different groups to prevent predictability of perturbation characteristics and also avoid any adaptation effects that could occur with repeated slip exposure, as previous studies have shown a strong ‘learning effect’ with a single slip exposure (i.e. First trial effect) (Liu et al., 2017; Marigold and Patla, 2002; Mcllroy and Maki, 1995).
Fig. 1.
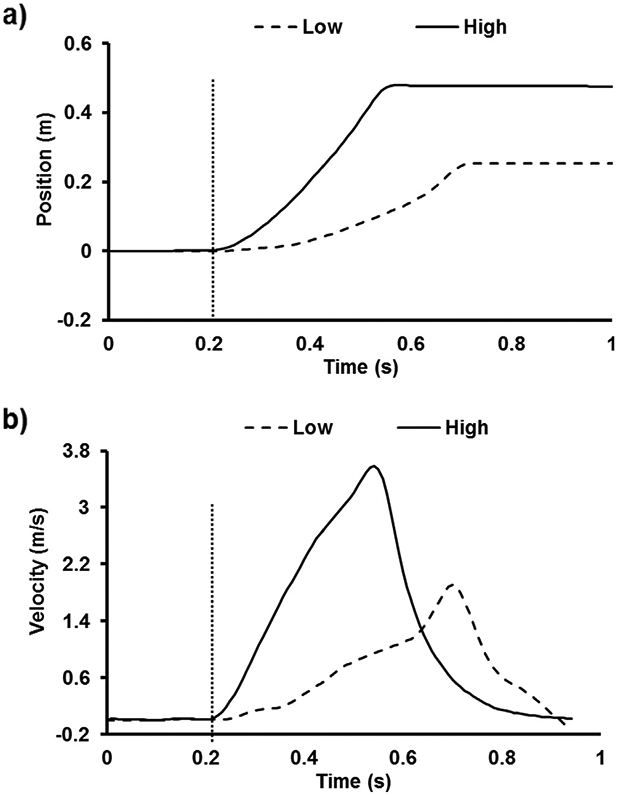
Time series data of the moveable platform (a) position in meters and (b) velocity in meter/second from representative participants from paretic high slip intensity group i.e. slip distance of 45 cm (solid line) and paretic low slip intensity group i.e. slip distance of 24 cm (dotted line) of overground gait-slip perturbations. The dotted vertical line indicates the instance of slip onset.
2.3. Data collection and analysis
Kinematics from a full body marker set (30 retro-reflective markers) were recorded by an eight-camera motion capture system (Motion Analysis Corporation, Santa Rosa, CA). Kinematic data were sampled at 120 Hz and synchronized with the force plate and load cell data, which was collected at 600 Hz. The instances of recovery step liftoff and touchdown during walking were determined from the vertical ground reaction forces using a custom written Matlab program.
2.4. Outcome measures
Perturbation outcome and recovery strategies:
Perturbation outcome on a novel slip resulted either in a backward loss of balance (BLOB), characterized by the need to execute a compensatory stepping response or no loss of balance which was identified when participants continued to maintain their regular walking pattern with the trailing limb landing ahead of the slipping limb. A BLOB was associated with recovery strategies which were aborted and recovery step. An aborted step was identified as unloading followed by sudden loading of the stepping limb without complete toe clearance (Bhatt et al., 2005; Espy et al., 2010). The immediate post-slip step with the trailing (stepping) limb that landed posterior to the slipping limb was identified as a recovery step.
Pre- and post-slip CoM state stability:
The CoM state stability was calculated as the shortest distance of the CoM state (instantaneous CoM position and velocity) to the computational threshold against BLOB during slipping (Pai and Iqbal, 1999). Center of mass position was computed using a 12 segment body representation (de Leva, 1996) and was expressed relative to the posterior most base of support (BOS) and normalized by participant’s foot length. Center of mass velocity was expressed as the first order derivative of the absolute CoM position, normalized by a dimensionless fraction of (g = acceleration due to gravity, h = participant’s height), and then expressed relative to the BOS. The CoM position and velocity were measured at pre-slip touchdown of slipping limb, post-slip lift off, and the instant right before touchdown (prerecovery) of the contralateral limb. We computed the stability at the specific pre-slip and post-slip instances. Stability values < 0 indicated greater likelihood of BLOB as shown in Fig. 3a, whereas, stability values > 0 indicated decreased likelihood of BLOB. Values for CoM position < 0 indicated that the CoM was outside (behind) the posterior boundary of BOS signifying backward instability and greater likelihood of backward balance los. A CoM position > 1 indicated that the CoM was outside (ahead of) the anterior boundary of the BOS signifying forward instability and greater likelihood of forward balance loss (Pai and Patton, 1997). Values for CoM velocity < 0 indicated that the CoM was traveling slower than the BOS, and values > 0 indicated that the CoM was moving faster than the BOS (McMahon, 1984).
Fig. 3.
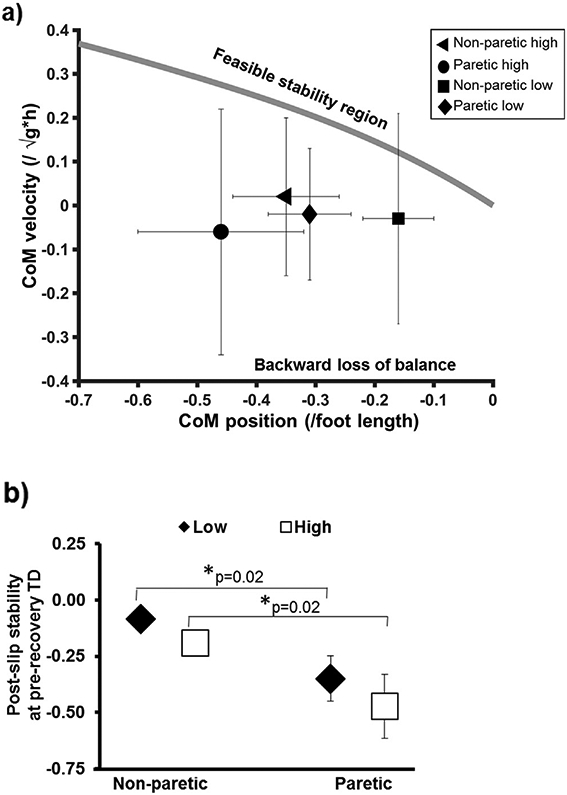
Comparison of means (±standard deviation) of (a) post-slip CoM stability at lift off plotted for all the 4 groups against the predicted stability threshold for BLOB (Pai and Iqbal, 1999) showing all the values to be negative and lying outside of the feasible stability region, beyond the backward stability threshold indicative of BLOB, and (b) post-slip CoM stability at pre-recovery touchdown for all four non-paretic high, non-paretic low, paretic high and paretic low groups. CoM stability < 0 indicative of greater possibility of BLOB while CoM stability > 0 indicative of lower possibility of BLOB. Significant differences are indicated with * p < 0.05. CoM: Center of mass; TD: touchdown; Low: low intensity slip group (slip distance 24 cm); High: high intensity slip group (slip distance 45 cm).
Slipping kinematics:
Peak slip displacement and velocity were calculated as the maximum displacement (i.e. the distance covered by the slipping foot heel marker) and maximum velocity (computed as first order derivative of slip displacement) of the moveable platform between the pre-slip touchdown of the slipping limb and post-slip liftoff of the stepping limb.
2.5. Statistical analysis
The Kruskal-Wallis test was used to analyze the differences in recovery strategies (aborted stepping and recovery stepping) between the non-paretic low intensity, paretic low intensity, non-paretic high intensity, and paretic high intensity slip groups. Any significant main effects were followed-up with planned comparisons using the Mann-Whitney U test to compare differences between the two groups. A one-way analysis of variance was performed to compare the variables: (1) pre-slip stability, (2) post-slip stability at pre-recovery touchdown, (3) peak slip displacement and (4) peak slip velocity. Significant effects were followed-up with planned comparisons using independent t-test. For all outcome measures, to examine the effect of perturbation intensity on the slip side, the planned comparisons performed were: 1) paretic low intensity versus paretic high intensity slip groups and 2) non-paretic low intensity versus non-paretic high intensity slip groups. To examine the effect of slip side at each slip intensity, the planned comparisons performed were: 1) paretic low intensity versus non-paretic low intensity slip groups and 2) paretic high intensity versus non-paretic high intensity slip groups. All analyses were performed using SPSS version 24 with a significance level of 0.05.
To determine the sample size for this study, a priori power analysis was performed using an estimated effect size of 1.26 for post-slip stability at touchdown (primary outcome measure) based on the findings from Kajrolkar (2016) and considering power of >0.75 with a level of significance as 0.05. The resulting sample size was 10 participants in each group.
3. Results
3.1. Perturbation outcome and recovery strategies
Participants from all the four groups demonstrated a BLOB following overground gait-slips. The recovery strategies associated with the BLOB demonstrated no significant differences between the four groups, (X2 = 5.64, p = 0.13) (Fig. 2a). For the paretic slip groups, the high intensity slip group demonstrated greater proportion of aborted stepping strategy (36%) versus low intensity slip group (8%); however, the difference was not significant (U = 47.5, p = 0.11). For the non-paretic slip groups, there was no difference in proportion of the aborted stepping strategy between the low intensity (40%) and high intensity (55%) slip groups (U = 47, p = 0.51). At low intensity slips, there was a near significant difference in the aborted stepping strategies between the non-paretic (40%) and paretic (8%) slip groups (U = 41, p = 0.08). At high intensity slips, there was no difference in aborted stepping strategy between the non-paretic (55%) and paretic (36%) slip groups (U = 49.5, p = 0.40).
Fig. 2.
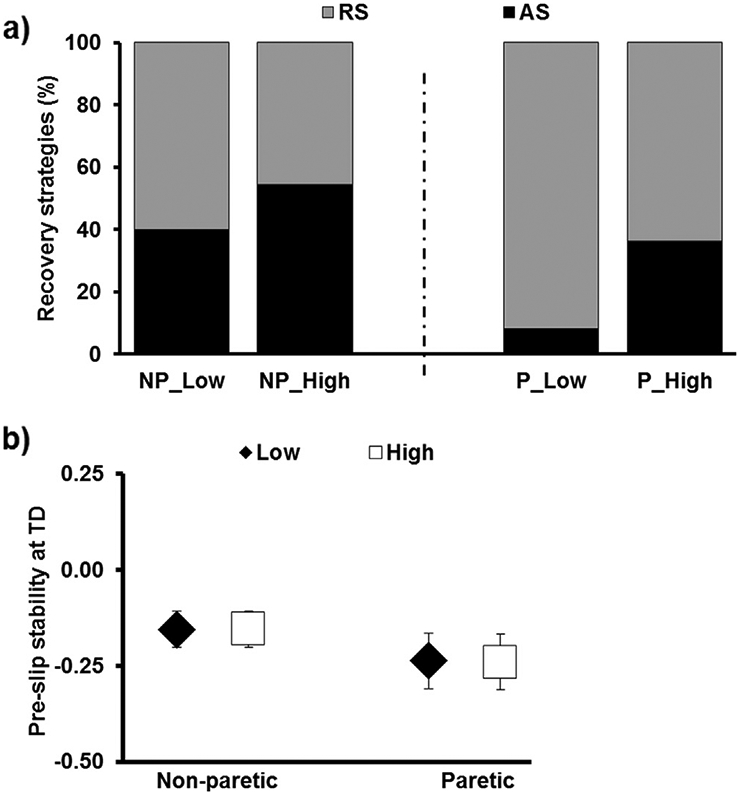
(a) Percentage of recovery strategies shown by non-paretic high, non-paretic low, paretic high and paretic low groups exposed to a single, novel slip either under non-paretic or paretic limb with a slip distance of either 24 cm (low) or 45 cm (high), and (b) pre-slip CoM stability at touchdown. CoM stability < 0 indicative of greater possibility of backward loss of balance while CoM stability > 0 indicative of lower possibility of backward loss of balance. Significant differences are indicated with * p < 0.05. NP_Low: non-paretic low intensity slip group, NP_High: non-paretic high intensity slip group, P_Low: paretic low intensity slip group, P_High: paretic high intensity slip group, RS: recovery step; AS: aborted step; TD: touchdown; Low: low intensity slip group (slip distance 24 cm); High: high intensity slip group (slip distance 45 cm).
3.2. Stability
There was no significant difference in pre-slip stability [F3, 43 = 2.01, p = 0.12] (Fig. 2b) between the four groups. The post-slip stability at liftoff was below the computational threshold for BLOB indicated by negative mean stability values for all the 4 groups [(non-paretic high intensity slip group (−0.17), paretic high intensity slip group (−0.30), non-paretic low intensity slip group (−0.12) and paretic low intensity slip group (−0.19)] as shown in Fig. 3a. Post-slip stability at pre-recovery touchdown demonstrated significant difference among all four groups [F3, 43 = 4.7, p = 0.007]. For the non-paretic slip groups, there was no difference in stability at pre-recovery touchdown between the low and high intensity slip groups (p = 0.30, 95% CI = −0.1, 0.31) (Fig. 3b). Similarly, for the paretic slip groups, there was no difference in stability at pre-recovery touchdown between the low and high intensity slip groups (p = 0.30, 95% CI = −0.12, 0.36). At low slip intensity, the non-paretic and paretic slip groups showed significant difference in stability at pre-recovery touchdown (p = 0.02, 95% CI = 0.03, 0.49) (Fig. 3b). Similarly, at high slip intensity, the non-paretic and paretic slip groups showed significant difference in stability at pre-recovery touchdown (p = 0.02, 95% CI = 0.04, 0.51).
3.3. Slipping kinematics (peak slip displacement and velocity)
There was a significant difference in peak slip displacement [F3, 43 = 2.91, p = 0.04], and velocity [F3, 43 = 4.28, p = 0.01] between all the four groups. For the non-paretic slip groups, peak slip displacement (p = 0.54, 95% CI = −0.16, 0.08), and peak slip velocity (p = 0.44, 95% CI = −0.58, 0.27) showed a trend of being greater in the high intensity slip group than the low intensity slip group (Fig. 4a & 4b). For the paretic slip groups, the peak slip displacement was greater in the high intensity slip group versus the low intensity slip group (p = 0.03, 95% CI = −0.21, −0.007) (Fig. 4a); however, there was no difference in the peak slip velocity (p = 0.57, 95% CI = −0.75, 0.42) between low and high intensity paretic slip groups (Fig. 4b). At high intensity slips, there was a significant difference in peak slip displacement between the non-paretic and paretic slip groups (p = 0.02, 95% CI = −0.22, −0.01); however, at low intensity slips, there was no difference in peak slip displacement between the paretic and non-paretic slip groups (p = 0.47, 95% CI = −0.16, 0.08) (Fig. 4a). At high intensity slips, the peak slip velocity was significantly different between non-paretic and paretic slip groups (p = 0.01, 95% CI = −1.12, −0.11) (Fig. 4b). Similarly, at low slip intensity, significant different in peak slip velocity between the non-paretic and paretic slip groups (p = 0.02, 95% CI = −1.15, −0.07) was noted.
Fig. 4.
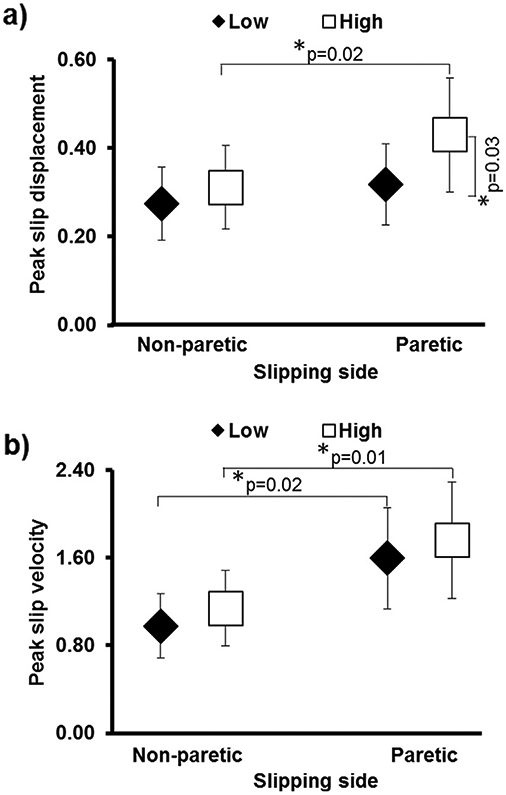
Comparison of means (±standard deviation) of post-slip (a) peak slip displacement and (b) peak slip velocity for all four non-paretic high, non-paretic low, paretic high and paretic low groups. Significant differences are marked with *p < 0.05. Low: low intensity slip group (slip distance 24 cm); High: high intensity slip group (slip distance 45 cm).
4. Discussion
Our study examined whether recovery after experiencing a gait-slip under the paretic or non-paretic limb vary as a function of slip intensity. For this, we exposed PwCS to low and high intensity gait-slips under their paretic or the non-paretic limb during regular walking. Specifically, we determined the effect of slip intensity on gait-slip outcomes, recovery strategies, and postural stability between non-paretic and paretic slips among PwCS. The results were partially supportive of our hypothesis, demonstrating that the paretic limb was associated with reduced reactive CoM stability especially at high intensity slips due to the inability to alter slipping kinematics.
Although all participants experienced a BLOB upon experiencing an unexpected slip, the recovery strategies differed between the four groups. At high intensity slips, the non-paretic and paretic slip groups demonstrated a near equal preference for recovery stepping and aborted stepping strategies (Fig. 2a). In contrast, at low intensity slips, the paretic slip group showed a greater proportion of recovery stepping responses compared to the non-paretic slip group (p = 0.08). With regards to the impact of slip intensity, recovery strategy for the paretic slip groups differed with slip intensity. The aborted stepping strategy increased from 8% in the paretic low intensity slip group (24 cm) to 36% in the paretic high intensity slip group (45 cm). Despite differences in recovery strategies, we found no difference in pre-slip CoM stability (proactive) between all four groups (Fig. 2b). This was expected as all groups received uniform instructions regarding knowledge of the novel slip resulting in somewhat similar anticipatory changes which may have only a minimal effect on stability among all four groups.
In line with previous gait-slip studies (Bhatt et al., 2012; Espy et al., 2010; Kajrolkar et al., 2014; Pai et al., 2010), the post-slip onset stability at liftoff in all the groups demonstrated a posterior shift in the CoM position relative to the anteriorly displacing BOS and also a slower velocity than the forward moving BOS. Based on the dynamic CoM model (Pai and Iqbal, 1999), such posterior shifting contributes to a CoM state stability (computed from CoM position and velocity) below the computational threshold for BLOB (Fig. 3a). This led to negative reactive stability values validating the BLOB outcomes evidenced in all four groups after gait-slips.
4.1. Effect of intensity on non-paretic gait-slips
We found that the stability at pre-recovery touchdown in the non-paretic slip groups was not influenced by slip intensity (Fig. 3b). At both slip intensities, non-paretic groups showed significantly greater pre-recovery touchdown stability compared to their corresponding paretic slip groups. Perhaps, the non-paretic slipping limb could easily control the moveable plate velocity contributing to better reactive control of slipping kinematics at each slip intensity relative the paretic slip groups. Superior slipping kinematics in the non-paretic slip groups was characterized by lower slip displacement and velocity (Fig. 4a, b), that may have reduced the slip intensity and in turn improved reactive stability at pre-recovery touchdown. Our results concur with previous studies in healthy adults indicating that better reactive control of slipping limb kinematics is related with lower incidence of balance loss (Marigold and Patla, 2002; Pavol and Pai, 2002).
PwCS minimized slip induced instability by adopting either an aborted or recovery stepping strategy (Fig. 2a) (Kajrolkar and Bhatt, 2016). A recovery step that allows to increase BOS and arrest slip-induced backward CoM movement (Maki and McIlroy, 1997), might have been a strategy of choice for individuals who were able to initiate and execute a recovery step with the paretic limb. Thus, if the non-paretic limb continues to slip (with a longer slip distance) once the paretic limb touchdown occurs, there is at least one stable BOS point to re-establish stability and prevent a split fall or vertical descent (Yang et al., 2012). On the other hand, an aborted stepping response might reduce the time in single stance under conditions of threat and allow time to “ride” out the perturbation (i.e. till perturbation termination) before continuing with the next forward gait step (Kajrolkar and Bhatt, 2016). If paretic trailing limb is unable to demonstrate effective compensatory stepping due to motor impairments, aborted step might be a best alternative strategy to regain stability. In case of a finite slip, an aborted step might lead to achievement of maximum stability at the cost of mobility. The impaired CNS may choose an aborted stepping response to augment postural stability, until the perturbation stops, thereby demonstrating the ‘posture first strategy’ (Doumas et al., 2008; Kajrolkar et al., 2014). We argue that as the non-paretic limb might exert a better control on slipping limb kinematics than the paretic limb, PwCS showed equal preference for recovery step and aborted step strategies regardless of slip intensity.
4.2. Effect of intensity on paretic gait-slips
Among all groups, paretic high intensity slip group demonstrated the most negative post-slip CoM stability at pre-recovery touchdown and higher peak slip velocity compared with the other groups (Fig. 3b and 4b). Further, the slip intensity influenced the peak slip displacement in the paretic slip groups. This was evidenced by a higher peak slip displacement in paretic high intensity slip group compared with paretic low intensity slip group. Evidence suggests that feedforward adjustments in the form of flat foot landing and increased knee flexion would provide a braking impulse (Bhatt et al., 2006; Cham and Redfern, 2002; Lockhart et al., 2003; Marigold and Patla, 2002). Such braking impulse assists in lowering perturbation intensity by reducing the slip velocity and displacement. Recently, Wang et al. (2020) found that a greater knee flexor moment during proactive (before slip onset) and early reactive phases (from slip onset to recovery limb liftoff) could shorten the distance between the CoM and slipping foot, thereby reducing slip intensity and lowering the risk of BLOB. Our findings could be indicative of impaired ability of the paretic limb to reactively control the slip kinematics (displacement and velocity) by generating sufficient post-slip knee flexion moment, especially at high intensity slips.
We found no difference in the reactive (post-slip) stability between the paretic low and high intensity slip groups. A potential explanation is that the greater instability in the paretic high intensity slip group could have been mitigated by the choice of recovery strategy adopted by this group. Despite the intact ability of the non-paretic stepping limb to execute a recovery step, the increased aborted stepping adopted by the non-paretic limb at high intensity slips could be a strategy to enhance stability. Sensing an increased perceived threat with faster peak slip velocity, the CNS may have chosen to avoid the risk associated with a single stance phase especially on the paretic limb and adopted a sudden reloading of the non-paretic stepping limb (aborted stepping) while gaining time to work on modulating slipping kinematics to reduce slip intensity.
Similar to PwCS, perturbation studies in older adults have shown greater percentage of aborted stepping to enhance stability and prevent a fall (Espy et al., 2010; Yang et al., 2012). Although the aborted step strategy may be beneficial to re-gain stability for ‘finite’ smaller slip distances, such a stepping strategy might result in a split-fall in case of an infinite slip resulting from a continuous forward movement of the slipping limb and irreversible hip descent (Yang et al., 2012). Thus, there might be a substantial increase in fall-risk with increased slip intensity during paretic slips compared with non-paretic slips due to the poor reactive control of CoM stability demonstrated by the paretic slip groups in our study.
5. Clinical application and limitation
Despite the ability to ambulate independently in community, PwCS have persistent deficits in reactive balance control, more evident at high intensity paretic gait-slips. Our results demonstrate a lower postural stability during paretic slips compared with non-paretic slips, regardless of slip intensity. Thus, balance training interventions in clinical settings could be designed to improve compensatory non-paretic limb stepping and reactive control of slipping paretic limb for reducing fall risk among PwCS. Furthermore, incorporating fall-risk assessment at high intensity perturbations under safe, controlled conditions could mimic the challenges faced upon exposure to real-life environmental gait-slips and help in better identification of PwCS at a risk of falling. Our results must be interpreted considering its limitations. Our study was performed with relatively high functioning PwCS and our present results may not be generalized to individuals with limited ability to ambulate. Moreover, such lower postural stability on paretic slip than non-paretic slip might be associated not only with the impaired motor function but also with the impaired somatosensory input resulting in an inability to accurately detect instability or perturbation intensity. Future studies in PwCS should examine the influence of impaired somatosensory function on reactive balance during gait-slips.
6. Conclusion
Our findings demonstrated that impaired reactive control of the paretic limb to alter slipping kinematics of the BOS contributed to increased slip intensity and resulted in high fall-risk among PwCS. Such difficulty in modulating slipping kinematics became more evident at high intensity paretic gait-slip. Thus, it is essential to develop fall-risk assessment and training paradigms specifically emphasizing on both compensatory stepping with non-paretic limb and reactive control of slipping with paretic limb at high intensity gait-slips among PwCS.
Acknowledgements
The authors would like to thank Riddhi Panchal, MS PT, and Lakshmi Kannan, MS PT for assistance with data collection and Shuaijie Wang, PhD for assistance with data analysis. This study was funded by the American Heart Association (12SDG12170022) and National Institute of Health (NIH) [1R01HD088543-01A1] awarded to Dr. Tanvi Bhatt.
References
- Allin LJ, Brolinson PG, Beach BM, Kim S, Nussbaum MA, Roberto KA, Madigan ML, 2020. Perturbation-based balance training targeting both slip- and trip-induced falls among older adults: a randomized controlled trial. BMC Geriatrics 20, 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bastian AJ, 2008. Understanding sensorimotor adaptation and learning for rehabilitation. Curr. Opin. Neurol 21, 628–633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batchelor FA, Hill KD, Mackintosh SF, Said CM, Whitehead CH, 2012. Effects of a multifactorial falls prevention program for people with stroke returning home after rehabilitation: a randomized controlled trial. Arch. Phys. Med. Rehabil 93, 1648–1655. [DOI] [PubMed] [Google Scholar]
- Bhatt T, Wening J, Pai Y-C, 2006. Adaptive control of gait stability in reducing slip-related backward loss of balance. Exp. Brain Res 170, 61–73. [DOI] [PubMed] [Google Scholar]
- Bhatt T, Wening JD, Pai YC, 2005. Influence of gait speed on stability: recovery from anterior slips and compensatory stepping. Gait Posture 21, 146–156. [DOI] [PubMed] [Google Scholar]
- Bhatt T, Yang F, Pai YC, 2012. Learning to resist gait-slip falls: long-term retention in community-dwelling older adults. Arch. Phys. Med. Rehabil 93, 557–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cham R, Redfern MS, 2002. Changes in gait when anticipating slippery floors. Gait & posture 15, 159–171. [DOI] [PubMed] [Google Scholar]
- de Leva P, 1996. Adjustments to Zatsiorsky-Seluyanov’s segment inertia parameters. J. Biomech 29, 1223–1230. [DOI] [PubMed] [Google Scholar]
- Doumas M, Smolders C, Krampe RT, 2008. Task prioritization in aging: effects of sensory information on concurrent posture and memory performance. Exp. Brain Res 187, 275–281. [DOI] [PubMed] [Google Scholar]
- Espy DD, Yang F, Bhatt T, Pai YC, 2010. Independent influence of gait speed and step length on stability and fall risk. Gait Posture 32, 378–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Handelzalts S, Steinberg-Henn F, Levy S, Shani G, Soroker N, Melzer I, 2019. Insufficient Balance Recovery Following Unannounced External Perturbations in Persons With Stroke. Neurorehabilitation and neural repair 33, 730–739. [DOI] [PubMed] [Google Scholar]
- Horak FB, Diener HC, 1994. Cerebellar control of postural scaling and central set in stance. J. Neurophysiol 72, 479–493. [DOI] [PubMed] [Google Scholar]
- Horak FB, Nashner LM, 1986. Central programming of postural movements: adaptation to altered support-surface configurations. J. Neurophysiol 55, 1369–1381. [DOI] [PubMed] [Google Scholar]
- Imamizu H, Sugimoto N, Osu R, Tsutsui K, Sugiyama K, Wada Y, Kawato M, 2007. Explicit contextual information selectively contributes to predictive switching of internal models. Exp. Brain Res 181, 395–408. [DOI] [PubMed] [Google Scholar]
- Inness EL, Mansfield A, Lakhani B, Bayley M, McIlroy WE, 2014. Impaired reactive stepping among patients ready for discharge from inpatient stroke rehabilitation. Phys. Ther 94, 1755–1764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jørgensen L, Engstad T, Jacobsen BK, 2002. Higher incidence of falls in long-term stroke survivors than in population controls: depressive symptoms predict falls after stroke. Stroke 33, 542–547. [DOI] [PubMed] [Google Scholar]
- Joshi M, Patel P, Bhatt T, 2018. Reactive balance to unanticipated trip-like perturbations: a treadmill-based study examining effect of aging and stroke on fall risk. International Biomechanics 5, 75–87. [Google Scholar]
- Kajrolkar T, Bhatt T, 2016. Falls-risk post-stroke: Examining contributions from paretic versus non paretic limbs to unexpected forward gait slips. J. Biomech 49, 2702–2708. [DOI] [PubMed] [Google Scholar]
- Kajrolkar T, Yang F, Pai YC, Bhatt T, 2014. Dynamic stability and compensatory stepping responses during anterior gait-slip perturbations in people with chronic hemiparetic stroke. J. Biomech 47, 2751–2758. [DOI] [PubMed] [Google Scholar]
- Lakhani B, Mansfield A, Inness EL, McIlroy WE, 2011. Compensatory stepping responses in individuals with stroke: a pilot study. Physiotherapy Theory Practice 27, 299–309. [DOI] [PubMed] [Google Scholar]
- Liu X, Bhatt T, Wang S, Yang F, Pai Y-CC, 2017. Retention of the “first-trial effect” in gait-slip among community-living older adults. Geroscience 39, 93–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lockhart TE, Woldstad JC, Smith JL, 2003. Effects of age-related gait changes on the biomechanics of slips and falls. Ergonomics 46, 1136–1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maki BE, McIlroy WE, 1997. The role of limb movements in maintaining upright stance: the “change-in-support” strategy. Phys. Ther 77, 488–507. [DOI] [PubMed] [Google Scholar]
- Maki BE, Mcilroy WE, Fernie GR, 2003. Change-in-support reactions for balance recovery. IEEE Eng. Med. Biol. Mag 22, 20–26. [DOI] [PubMed] [Google Scholar]
- Mansfield A, Inness EL, Komar J, Biasin L, Brunton K, Lakhani B, McIlroy WE, 2011. Training rapid stepping responses in an individual with stroke. Phys. Ther 91, 958–969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mansfield A, Inness EL, Lakhani B, McIlroy WE, 2012. Determinants of limb preference for initiating compensatory stepping poststroke. Arch. Phys. Med. Rehabil 93, 1179–1184. [DOI] [PubMed] [Google Scholar]
- Mansfield A, Wong JS, McIlroy WE, Biasin L, Brunton K, Bayley M, Inness EL, 2015. Do measures of reactive balance control predict falls in people with stroke returning to the community?. Physiotherapy 101, 373–380. [DOI] [PubMed] [Google Scholar]
- Marigold DS, Patla AE, 2002. Strategies for dynamic stability during locomotion on a slippery surface: effects of prior experience and knowledge. J. Neurophysiol 88, 339–353. [DOI] [PubMed] [Google Scholar]
- Martinez KM, Mille M-L, Zhang Y, Rogers MW, 2013. Stepping in persons poststroke: comparison of voluntary and perturbation-induced responses. Arch. Phys. Med. Rehabil 94, 2425–2432. [DOI] [PubMed] [Google Scholar]
- Mcllroy W, Maki B, 1995. Adaptive changes to compensatory stepping responses. Gait & posture 3, 43–50. [Google Scholar]
- McMahon TA, 1984. Muscles, reflexes, and locomotion. Princeton University Press. [Google Scholar]
- Okubo Y, Brodie MA, Sturnieks DL, Hicks C, Carter H, Toson B, Lord SR, 2018. Exposure to trips and slips with increasing unpredictability while walking can improve balance recovery responses with minimum predictive gait alterations. PLoS ONE 13, e0202913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pai Y-C, Bhatt T, Yang F, Wang E, Kritchevsky S, 2014. Perturbation training can reduce community-dwelling older adults’ annual fall risk: a randomized controlled trial. J. Gerontology Series A: Biomedical Sci. Medical Sciences 69, 1586–1594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pai Y-C, Patton J, 1997. Center of mass velocity-position predictions for balance control. J. Biomech 30, 347–354. [DOI] [PubMed] [Google Scholar]
- Pai YC, Bhatt T, Wang E, Espy D, Pavol MJ, 2010. Inoculation against falls: rapid adaptation by young and older adults to slips during daily activities. Arch. Phys. Med. Rehabil 91, 452–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pai YC, Iqbal K, 1999. Simulated movement termination for balance recovery: can movement strategies be sought to maintain stability in the presence of slipping or forced sliding?. J. Biomech 32, 779–786. [DOI] [PubMed] [Google Scholar]
- Patel PJ, Bhatt T, 2016. Does aging with a cortical lesion increase fall-risk: Examining effect of age versus stroke on intensity modulation of reactive balance responses from slip-like perturbations. Neuroscience 333, 252–263. [DOI] [PubMed] [Google Scholar]
- Pavol MJ, Pai YC, 2002. Feedforward adaptations are used to compensate for a potential loss of balance. Exp. Brain Res 145, 528–538. [DOI] [PubMed] [Google Scholar]
- Punt M, Bruijn SM, Roeles S, van de Port IG, Wittink H, van Dieën JH, 2017. Responses to gait perturbations in stroke survivors who prospectively experienced falls or no falls. J. Biomech 55, 56–63. [DOI] [PubMed] [Google Scholar]
- Salot P, Patel P, Bhatt T, 2016. Reactive balance in individuals with chronic stroke: biomechanical factors related to perturbation-induced backward falling. Phys. Ther 96, 338–347. [DOI] [PubMed] [Google Scholar]
- Schmid AA, Yaggi HK, Burrus N, McClain V, Austin C, Ferguson J, Fragoso C, Sico JJ, Miech EJ, Matthias MS, 2013. Circumstances and consequences of falls among people with chronic stroke. [DOI] [PubMed] [Google Scholar]
- Wang S, Wang Y, Pai Y-CC, Wang E, Bhatt T, 2020. Which Are the Key Kinematic and Kinetic Components to Distinguish Recovery Strategies for Overground Slips Among Community-Dwelling Older Adults?. J. Appl. Biomechanics 1, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weerdesteyn V, de Niet M, van Duijnhoven HJ, Geurts AC, 2008. Falls in individuals with stroke. J. Rehabil. Res. Dev 45, 1195–1213. [PubMed] [Google Scholar]
- Yang F, Espy D, Bhatt T, Pai YC, 2012. Two types of slip-induced falls among community dwelling older adults. J. Biomech 45, 1259–1264. [DOI] [PMC free article] [PubMed] [Google Scholar]


